This conference report was provided by Aditi Nerurkar, MD, MPH, an integrative medicine physician at Harvard Medical School and the medical director of the Cheng-Tsui Integrated Health Center at Beth Israel Deaconess Medical Center, Boston, Massachusetts. She specializes in mind-body medicine, stress management, and lifestyle medicine. She is also a contributor to The Atlantic and The Huffington Post.
BACKGROUND AND INTRODUCTION
Until recently, the basic assumption was that the enteric system and central nervous system functioned independently of each other with little communication. But emerging research suggests there exists a rich and dynamic interrelationship between these 2 seemingly disparate entities. Referred to as the gut-brain axis, this innovative construct offers us a new window into understanding the mind-body connection. In the context of gastrointestinal (GI) illness in particular, it may help to elucidate the complex mechanisms contributing to chronic pain in patients with functional GI disorders, organic GI disorders, and behavioral disorders that cause GI somatization.
The mechanistic features of the gut-brain axis are comprised of a complex set of interconnected pathways linking the enteric system to the nervous system (Figure). The brain receives a continual stream of afferent information from the gut, integrates this information with internal cues in the body and external signals from the environment, and sends a response back to specific target cells in the GI tract. This dialogue is imperceptible in most people, but in patients with GI illness, this communication can cause a host of negative sequelae, which may include the recurrent discomfort of irritable bowel syndrome (IBS), the psychological and behavioral disturbances leading to abdominal pain in anorexia nervosa, the intestinal inflammation in patients with Crohn's disease, autoimmune-meditated intestinal changes in those with celiac disease, and tissue degeneration from tumor formation in patients with GI malignancies. Yet irrespective of their variable initial etiologies, these downstream consequences often lead to significant physiological and psychosocial dysfunction, both of which can adversely impact a patient's quality of life. Historically, the management of these aforementioned consequences has focused mainly on treating the underlining disease, and to date, little has been done to understand why the gut-brain dialogue exists in the first place.
Figure.
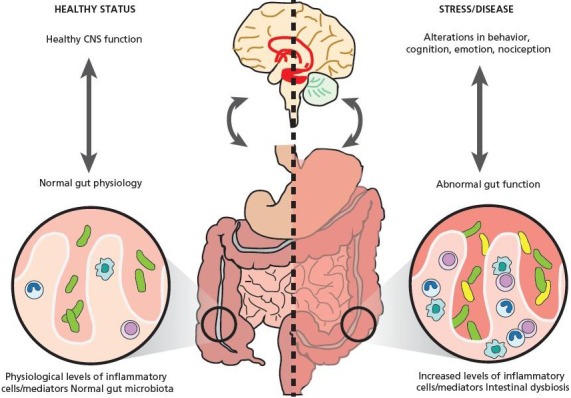
Components of the gut-brain axis: a schematic. Reproduced with permission from: Grenham S, Clarke G, Cryan JF, Dinan TG. Brain–gut–microbe communication in health and disease. Front Physio. 2011;2:94.
To help gain greater insight into the nature of this innate, bidirectional pathway of communication, the symposium “The Gut-Brain Axis: How to Manage Pain Caused by this Cross-talk” was held on May 4, 2015, in Salerno, Italy. Sponsored by the European Biomedical Research Institute of Salerno, the Medical Association of Salerno, and the Institute for Integrative Health, the symposium sought to elucidate how conventional and complementary medical systems currently understand this bidirectional cross-talk and how an integrative approach blending these 2 medical spheres might provide a new and innovative therapeutic perspective in the management of chronic pain in GI illness. The symposium featured 38 speakers from numerous academic institutions in 5 different countries (Table), and the symposium's presenters represented a wide range of medical specialties including gastroenterology, internal medicine, pediatrics, adolescent medicine, neurology, psychiatry, and integrative medicine.
Table.
Symposium Attendees
| Title | Speaker/Discussant | Institution | Medical Specialty |
|---|---|---|---|
| Professor | Paolo Barone | University of Salerno | Neurology |
| Doctor | Paolo Marchettini | Hospital San Raffaele, Milan | Neurology |
| Doctor | Marco Ruggero Lacerenza | Nursing Home S. Pio X; “Opera San Camillo” Foundation | Neurology |
| Associate Professor | Rosario Cuomo Federico II | University Hospital School of Medicine | Gastroenterology |
| Doctor | Carlo Di Lorenzo | Nationwide Children's Hospital Columbus OH USA | Pediatrics |
| Professor | Justin Wu | The Institute of Digestive Disease The ChineseUniversity of Hong Kong | Gastroenterology |
| Doctor | Francesco Cardini | Regional Health Agency of Emilia Romagna | Gynecology and obstetrics |
| Professor | Carmelina Loguercio | University of Naples | Gastroenterology |
| Professor | Alessio Maria Monteleone | University of Salerno | Psychiatry |
| Associate Professor | Umberto Volpe | University of Naples | Psychiatry |
| Professor | Valdo Ricca | University hospital of Careggi, Florence | Psychiatry |
| Associate Professor | Carlo Catassi | University Politecnica Marche | Pediatrics |
| Professor | Carolina Ciacci | University of Salerno | Gastroenterology |
| Associate Professor | Gerard Mullin | Johns Hopkins Hospital, Baltimore, Maryland | Gastroenterology |
| Doctor | Brian Berman | University of Maryland School of Medicine | Family and community medicine, integrative medicine |
| Professor | Basilio Malamisura | Azienda Ospedaliera Salerno | PediatricGastroenterology |
| Doctor | Annamaria Staiano | University of Naples, Federico II | Pediatrics |
| Professor | Jost Langhorst | University Duisburg-Essen, Germany | Gastroenterology |
| Professor | Fabio Cominelli | Case Western Reserve University, Cleveland, Ohio | Gastroenterology |
| Doctor | Marina Aloi | University Sapienza, Rome | Pediatrics |
| Associate Professor | Gabriele Riegler | University of Naples | Psychiatry |
| Associate Professor | Marco Romano | University of Naples | Gastroenterology |
| Assistant Professor | Jun Mao | University of Pennsylvenia | Family medicine |
| Professor | Claudia Witt | University of Zurich Switzerland | Epidemiology, integrative medicine |
| Professor | Renato Gammaldi | University Hospital “San Giovanni e Ruggi”, Salerno | Intensive care |
| Doctor | Giulio Corrivetti | Salerno Health Authority | Psychiatry |
| Professor | Alessio Fasano | MassGeneral Hospital for Children | Pediatrics |
| Doctor | Elio Rossi | Homeopathic Clinic, Hospital of Lucca | Homeopathy/integrative medicine |
| Title | Moderator | Institution | Medical Specialty |
| Associate Professor | Vajro Pietro | Department of Medicine of the University of Salerno | Pediatrics |
| Director department neonatology | Lopardo Beatrice | Neonatology, Salerno | Neonatology |
| Professor | Ronald Kleinman | MassGeneral Hospital for Children | Pediatric Gastroenterology and nutrition |
| Professor | Palmiero Monteleone | University of Salerno | Psychiatry |
| Doctor | Riccardo Troncone | University of Salerno | Pediatrics |
| Professor | Allan Walker | Harvard Medical School | PediatricGastroenterology |
| Doctor | Mario Colucci | Salerno Health Authority | Infectious diseases |
| Doctor | Armando De Martino | Salerno Health Authority | Emergency medicine |
| Stefano Pepe | Telethon Institute of Genetics and Medicine, Naples | Genetics | |
| Tiziana Salvati | Psychology | ||
| Title | organizer | Institution | Medical Specialty |
| Professor | Brian Berman | Center for Integrative Medicine, University of Maryland School of Medicine, Baltimore, Maryland | Family and community medicine, integrative medicine |
| Professor | Alessio Fasano | MassGeneral Hospital for Children | Pediatric gastroenterology and nutrition |
| Doctor | Giulio Corrivetti | Salerno Health Authority | Psychiatry |
| Executive director | Susan Berman | Institute for Integrative Health, Baltimore, Maryland | |
| Professor | Claudia Witt | Complementary and Integrative Medicine, Zurich, Switzerland | Integrative medicine |
KEYNOTE PRESENTATIONS: ADDRESSING THE COMPLEXITIES IN UNDERSTANDING AND TREATING PAIN MODULATED BY THE GUT-BRAIN AXIS
The event began with 2 keynote presentations given by Drs Paolo Marchettini and Marco Lacerenza, respectively. These talks provided an initial framework for the symposium and introduced the audience to key terminology as well as broader concepts that were used throughout the event. The keynote addresses defined which structures comprise the gut-brain axis, classified the types of pain variants, and explained what constitutes the gut microbiome and metabolome and their impact on the gut-brain cross-talk. They also introduced larger, conceptual topics such as the biopsychosocial model of pain, the emotional implications for affected patients, and the impact of pain on the doctor-patient relationship. The keynote talks concluded with a phrase that was echoed throughout the symposium by the speakers who followed: Pain is a complex condition with multifactorial inputs and therefore requires a complex and multifactorial approach in its management.
After these initial keynote presentations, the symposium continued with a systems-based approach; there were 5 individual sessions, each with a disease-specific focus. IBS, inflammatory bowel disease (IBD), celiac disease, GI malignancies, and anorexia nervosa were systematically discussed in the context of pain modulated by the gut-brain axis. Each session began with a clinical case and was followed by 3 distinct types of presentations; the first described the conventional approach to treating pain in that condition, the second discussed strategies for pain control using complementary medicine, and the third offered a combined integrative approach to pain for that condition utilizing the expertise of 2 discussants, 1 from the conventional medical sphere and the other from the complementary medical sphere. This 3-step presentation model allowed for a unique forum and an open, mutually respectful dialogue among thought leaders from both the biomedical and integrative medicine communities.
While each individual session highlighted best practices for pain management in the specific medical condition being discussed, several overarching themes emerged across all sessions irrespective of disease context (Box). These unifying themes were alluded to throughout the 5 corresponding sessions and helped to create a deeper, more nuanced understanding of evidence-based biomedical and integrative strategies in managing pain modulated by the gut-brain axis.
SUMMARY OF SESSIONS
Session 1: Irritable Bowel Syndrome as a Quintessential Disorder of the Gut-Brain Axis
The first session discussed IBS, a functional GI disorder quintessential of the gut-brain axis. The clinical vignette introducing IBS focused on 2 key clinical aspects of the syndrome: its variable symptomology delineated by the Rome Criteria and the need for a tailored approach to treatment depending on the dominant symptoms. The case also elucidated the dietary connection to serotonin and other neurotransmitters: increased acetylcholine in constipation-predominant IBS and increased norepinephrine in diarrhea-predominant IBS. Conventional treatment modalities for IBS were presented including lifestyle changes, a low-FODMAP (fermentable oligo-dimonosaccharides and polyols) diet, psychotherapy, stress management, cognitive behavioral therapy, psychopharmacology, and pharmacotherapy such as a low-dose tricyclic antidepressant, while the integrative approach offered traditional Chinese medicine and acupuncture as potential adjunctive treatments.
Session 2: Anorexia Nervosa as a Mind-Body Disorder
The second session introduced anorexia nervosa as a disorder of the gut-brain axis. The clinical vignette presented a young woman with classic features of anorexia and highlighted the importance of an early diagnosis and subsequent treatment using a multidisciplinary team, which included a primary care physician, psychiatrist, psychologist, and nutritionist. While several presenters mentioned the limited role that pharmacotherapy such as olanzapine or selective serotonin reuptake inhibitors could play in treatment, the majority of the discussion centered around the complex bio-psychosocial forces involved in this condition. Interestingly, nearly all presenters approached anorexia nervosa as a mind-body disorder and offered evidence to support the use of integrative modalities such as mind-body medicine, acupuncture, traditional Chinese medicine, and homeopathy in its management.
Common Themes In Pain Management In The Context Of The Gut-Brain Axis
Pain is a complex disorder with numerous biopsychosocial forces involved.
Paint treatment requires a highly coordinated, multidisciplinary, team-baased approach.
The patient belongs at the center of the treatment plan.
Session 3: Celiac Disease and Migraine Pain: Elucidating the Crosstalk in the Gut-Brain Axis
The third session discussed the gut-brain axis in the context of celiac disease and its association with migraine headaches. Led by a case presentation, the discussion centered around the role that the gut microbiome plays in this linkage. Several proposed mechanisms of action were presented, including small intestine bacterial overgrowth (SIBO) promoting a proinflammatory cascade and compromised gut-immune barrier, thereby contributing to increased gut permeability and bacterial translocation. Strategies for pain management in patients with celiac disease and migraines included novel approaches like mind-body therapies, functional medicine, probiotics, and emerging vaccine formulations.
Session 4: Inflammatory Bowel Disease and the “Exposome”
The fourth session focused on IBD pain and the gut-brain axis. The clinical vignette described a pediatric patient with a new diagnosis of IBD and introduced disease activity indices such as the PUAIC and Pediatric Quality of Life Inventory. The subsequent discussion highlighted the management of both adult and pediatric patients with IBD. Various pathways in the pathophysiology of IBD were presented, including the microbiome, gut-immune barrier, and “exposome.” In discussing IBD treatment, presenters highlighted the fact that disease management was synonymous with pain management, since disease activity correlated directly with intestinal inflammation that subsequently led to pain. An effective strategy for disease management, and thereby pain management, in IBD was a multidisciplinary approach using conventional pharmacotherapy along with nonpharmacological approaches such as mindfulness meditation, yoga, and stress management, among others.
Session 5: Gastrointestinal Malignancies and Their Varied Pain Syndromes
The fifth session illustrated the gut-brain axis in the context of GI malignancies, particularly of the colon and pancreas. In this clinical vignette, the characteristics of the patient's neoplastic pain were complex and multifactorial: nociceptive and neuropathic pain caused by tumor growth and metastatic disease, as well as psychogenic pain related to the cancer diagnosis. Presenters discussed the conventional approach to pain management in cancer patients, which included employing an “analgesic ladder” of nonsteroidal anti-inflammatories, opiates, antidepressants, anticonvulsants, local anesthetics, celiac plexus block, and in some cases, neurolysis. There was also considerable discussion on integrative approaches such as mindfulness meditation, yoga, and acupuncture within the framework of a multidisciplinary, team-based, patient-centered approach to care.
Panel Discussion: Next Steps in Managing Pain in the Context of the Gut-Brain Axis
The symposium's final session was a panel discussion on insights, lessons learned, and next steps from the day-long event. Discussants agreed that the gut-brain axis was a true paradigm shift in the understanding of chronic pain in GI illness and the symposium was an important first step in elucidating this novel yet not well-understood construct. They called for a greater need for research on the mechanisms of pain in the context of the gut-brain axis, additional research on the mechanisms of action of both biomedical and integrative therapies in modulating pain, and further studies in comparative effectiveness, including “-omics” trials, to better understand whether specific subsets of patients may gain greater benefits from specific treatments.
CLOSING REMARKS: REFLECTIONS FROM THE SYMPOSIUM ORGANIZERS
The symposium officially concluded with closing remarks from Drs Brian Berman and Alessio Fasano. They remarked on the unprecedented nature of this gathering with respect to the type of content discussed, the range of medical specialties represented, and the rare confluence of the biomedical and integrative medical models—all for the common goal of gaining a better understanding of the gut-brain axis and its impact on pain. They reflected that while the crosstalk between the enteric and nervous systems has not yet been well-understood, its presence calls into question an outdated assumption that the mind and body, vis-à-vis the gut and brain, are separate. They encouraged the need for pragmatic randomized clinical trials, basic science research, and translational research to elucidate the underlying mechanisms of pain and its treatment, using the combination of biomedical and integrative therapies as a new approach to personalized medicine. In concluding their remarks, they stated that as the approach to understanding disease etiology is changing, so too is the approach to disease management. A multidisciplinary, team-based, patient-centered approach using the best of conventional and integrative therapies, with shared decision-making with the patient, is the future of pain therapy, irrespective of disease context.


