Abstract
Annual influenza vaccination is strongly recommended for patients with chronic pulmonary diseases, such as bronchial asthma, chronic obstructive pulmonary disease (COPD), and interstitial pulmonary diseases. However, many of these patients regularly receive systemic and/or inhaled corticosteroid therapy, and the impact of corticosteroid therapy on influenza vaccine efficacy and safety is unclear. Patients with chronic pulmonary diseases were enrolled in the study and divided into three groups based on their maintenance therapy: (A) without corticosteroid therapy (17 males, three females; mean age, 72.3 ± 7.9), (B) oral corticosteroid therapy (four males, seven females; mean age, 66.1 ± 10.6), and (C) inhaled corticosteroid therapy (eight males, nine females; mean age, 62.4 ± 16.0). All patients received influenza vaccine, and serum hemagglutination inhibition (HI) antibodies against influenza strains A/H1N1, A/H3N2, and B were measured at baseline (before vaccination) and 4-6 weeks after vaccination. Sufficient antibody titers or significant increases were observed after vaccination compared with titers before vaccination in all three groups. No systemic reactions were reported. Long-term oral/inhaled corticosteroid therapy was not associated with vaccination side effects and did not affect the immune response to the influenza vaccine.
Keywords: corticosteroid, influenza vaccine, chronic pulmonary disease
Introduction
Influenza is a major public health problem that causes significant morbidity and mortality worldwide (Lambert and Fauci, 2010[8]; Igarashi et al., 2011[4]). Yearly vaccination prevents influenza-related complications and reduces influenza prevalence (Nichol et al., 2007[11]). Elderly patients with chronic pulmonary diseases such as bronchial asthma, chronic obstructive pulmonary disease (COPD), and interstitial pulmonary diseases are strongly recommended to receive an annual influenza vaccine to prevent disease symptom exacerbation or loss of pulmonary function due to respiratory tract infection (Nichol et al., 2007[11]; Inoue et al., 2003[5], 2009[6]). However, many patients with chronic pulmonary diseases regularly receive systemic or inhaled corticosteroid, and it is well known that systemic corticosteroid administration restrains immune responses, such as antibody production (Baxter and Harris, 1975[1]). Despite this, few studies have investigated the influence of steroid therapy on influenza vaccine efficacy and safety, and the effects of regular oral or inhaled corticosteroids on these parameters were unclear. In this study, we evaluated the efficacy and safety of the influenza vaccine in elderly patients with chronic pulmonary diseases who were receiving oral or inhaled corticosteroids.
Materials and Methods
Patient characteristics
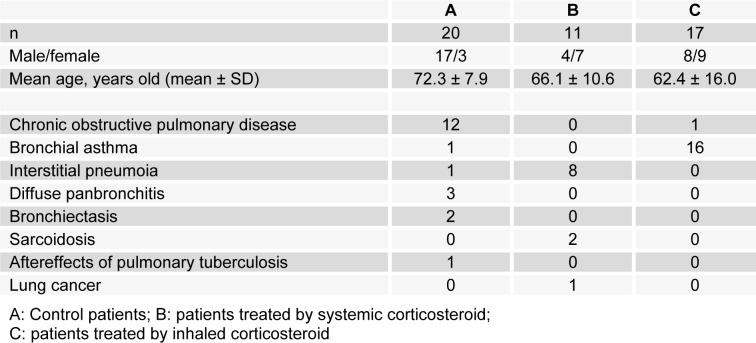
This prospective study was carried out between October 2004 and April 2005. A total of 48 patients with chronic respiratory diseases, with or without oral or inhaled corticosteroid treatment, were recruited from Yamaguta University Hospital and enrolled in the study (those who received both oral and inhaled corticosteroid were excluded). The patients were classified into three groups based on their maintenance therapy: (A) without corticosteroid therapy (17 males, three females; mean age, 72.3 ± 7.9), (B) oral corticosteroid therapy (four males, seven females, mean age, 66.1 ± 10.6; median corticosteroid dose: 10.0 mg/ day (2.5-25 mg/day), equivalent to prednisolone), or (C) inhaled corticosteroid therapy (eight males, nine females; mean age, 62.4 ± 16.0; median inhaled corticosteroid dose: 800 μg/day (400-1600 μg/day), equivalent to budesonide). All patients with chronic respiratory diseases were stable before receiving vaccination. Patient characteristics are summarized in Table 1(Tab. 1).
Table 1. Patients' profiles.
Study protocol
All patients received a single subcutaneous inoculation of the trivalent influenza vaccine from the same lot containing hemagglutinin of influenza HA1 (A/Beijing), HA2 (A/Taiwan), and HB (B/Panama), from Mitsubishi Tanabe Pharma Co. Osaka, Japan. Blood samples were collected to measure antibody titers against influenza A and B antigens before vaccination and 4-6 weeks after vaccination.
Serum antibody titers were measured with hemagglutination inhibition (HI) assays. The serum samples were serially diluted and co-incubated with influenza antigen and 0.5 % chicken red blood cells. The HI titter was determined as the reciprocal of the highest serum dilution resulting in nonagglutination of red blood cells. Vaccination efficacy was evaluated by seroconversion, defined as a pre-vaccination HI titer < 1:10 and a post-vaccination HI titer ≥ 1:40 or a pre-vaccination HI titer ≥ 1:10 and a minimum four-fold rise in post-vaccination HI antibody titer and seroprotection, defined as a post-vaccination HI titer of ≥ 1:40 (Chotirosniramit et al., 2012[2]).
Statistical analysis
Data are shown as mean ± standard deviation (SD). Pre- and post-vaccination HI titers were compared with paired t tests. Possible influences of oral or inhaled steroid therapy were evaluated with Chi-squared tests.
Results
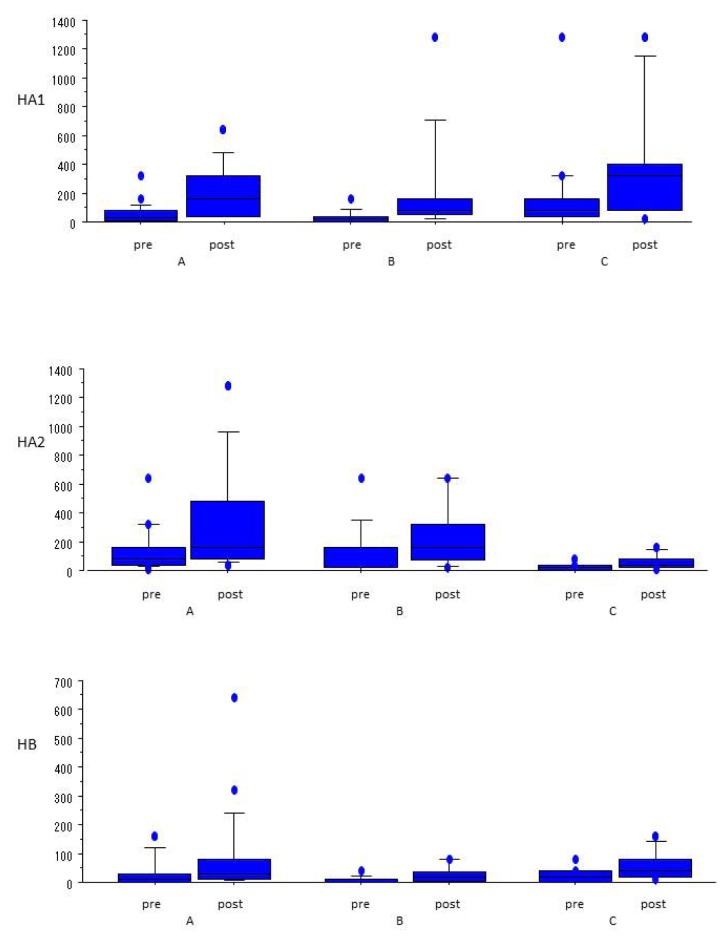
Serum antibody responses against influenza vaccine antigens were increased from baseline values in all three groups (Figure 1(Fig. 1)). In group A, we observed significant increases in HA1 and HA2 titers. Although there was no significant difference in HB antibody HI titer between pre- and post-vaccination, HB antibody HI titers were sufficient for seroprotection. Group B exhibited significant increases in HI titers for HA2 and HB. Although there was no significant difference in HA1 antibody HI titer between the two time points, the HI titers were high enough for seroprotection. In group C, significant increases in HI titers against HA1 and HB were noted. Although we did not observe a significant difference in HA2 antibody HI titer levels between pre- and post-vaccination, the levels were high enough to confer seroprotection.
Figure 1. Pre- and post-vaccination antibody titers against HA1, HA2, and HB. Group A, patients without corticosteroid therapy; Group B, patients with oral corticosteroid therapy; and Group C, patients with inhaled corticosteroid therapy.
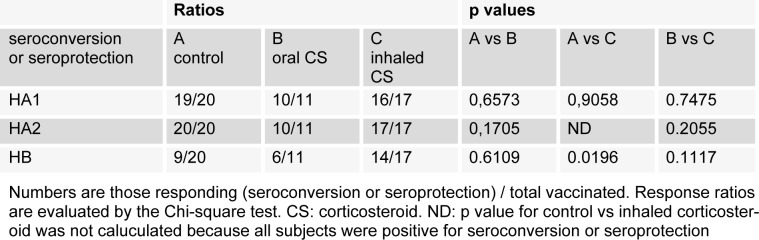
Vaccination effectiveness findings are summarized in Table 2(Tab. 2). In patients who received inhaled corticosteroid therapy, the ratio of seroconversion or seroprotection for HB was significantly higher than in patients without corticosteroid therapy. A local reaction was observed at the injection site within several days after vaccination in one patient, but no systemic reactions were observed.
Table 2. The ratio of seroconversion or seroprotection after vaccination.
Discussion
We investigated the efficacy and safety of the influenza vaccine in elderly patients with chronic pulmonary diseases receiving oral or inhaled corticosteroid therapy. Maintenance treatment with oral or inhaled corticosteroid therapy in this population did not reduce the serological response to influenza vaccination. In fact, Table 2(Tab. 2) shows that the serological response to HB was significantly reduced in patients without corticosteroid therapy. Overall, nine of 20 control patients (without corticosteroid therapy) did not show a serological response after vaccination. Our findings suggest that inhaled corticosteroid did not exert a significant immunosuppressive effect.
In patients with chronic pulmonary disease, respiratory tract infection is the most prevalent cause of acute symptom exacerbation (Inoue et al., 2003[5], 2009[6]). This is especially true in COPD patients; respiratory tract infections due to influenza virus or rhinovirus induce secondary bacterial infection and severe respiratory failure (Igarashi et al., 2011[4]; McManus et al., 2008[10]). Patients with chronic pulmonary diseases are strongly urged to receive an annual influenza vaccination, and many of them also receive oral and/or inhaled corticosteroid treatment. We did not find any significant differences in antibody production against influenza strains between patients with or without corticosteroid therapy. A few studies have investigated the influence of corticosteroids on influenza vaccine-induced antibody production (Kubiet et al., 1996[7]; Hanania et al., 2004[3]), but ours is the first report that shows effective antibody production against influenza in elderly patients with chronic pulmonary diseases who were receiving oral or inhaled corticosteroid.
It is well known that long-term systemic corticosteroid therapy is immunosuppressive (Lipworth, 1999[9]). Indeed, we found that pre-vaccination antibody titers were lower in patients treated with oral or inhaled corticosteroid compared to patients without steroid therapy. Despite this observation, there were no significant post-vaccination differences between the groups. These results suggest that vaccinating patients with chronic pulmonary diseases who receive corticosteroid treatment against influenza is effective.
There are some limitations in our study. First, it was performed at a single center, so the number of subjects enrolled was not large. Second, the dose of systemic steroid was relatively low in this study population, so the effects of high-dose corticosteroid treatment on antibody production against influenza is still unknown. Third, only one patient treated with inhaled corticosteroid was infected with influenza A, and one patient without corticosteroid therapy was infected with influenza B during the study period. As such, we could not investigate any potential preventative effect of the corticosteroid treatment on influenza infection. Fourth, most patients had received the flu vaccine for multiple consecutive years, and many exhibited high antibody titers before vaccination; therefore, we cannot ignore the influence of previous vaccinations on antibody titer levels.
In conclusion, influenza vaccination is safe and effectively stimulates antibody production even in patients treated with oral or inhaled corticosteroid. Further investigation in a much larger population will be necessary to confirm our results.
References
- 1.Baxter JD, Harris AW. Mechanism of glucocorticoid action: general features, with reference to steroid-mediated immunosuppression. Transplant Proc. 1975;7:55–65. [PubMed] [Google Scholar]
- 2.Chotirosniramit N, Sugandhavesa P, Aurpibul L, Thetket S, Kosashunhanan N, Supindham T, et al. Immune response to. 2009 H1N1 vaccine in HIV-infected adults in Northern Thailand. Hum Vaccin Immunother. 2012;8:1854–1859. doi: 10.4161/hv.21820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hanania NA, Sockrider M, Castro M, Holbrook JT, Tonascia J, Wise R, et al. Immune response to influenza vaccination in children and adults with asthma: effect of corticosteroid therapy. J Allergy Clin Immunol. 2004;113:717–724. doi: 10.1016/j.jaci.2003.12.584. [DOI] [PubMed] [Google Scholar]
- 4.Igarashi A, Tokairin Y, Hirono O, Kato T, Kubota I. Two cases of mixed infection following. 2009 H1N1 influenza pneumonia [article in Japanese] Nihon Kokyuki Gakkai Zasshi. 2011;49:226–231. [PubMed] [Google Scholar]
- 5.Inoue S, Nakamura H, Otake K, Saito H, Terashita K, Sato J, et al. Impaired pulmonary inflammatory responses are a prominent feature of streptococcal pneumonia in mice with experimental emphysema. Am J Respir Crit Care Med. 2003;167:764–770. doi: 10.1164/rccm.2105111. [DOI] [PubMed] [Google Scholar]
- 6.Inoue S, Nakamura H, Shibata Y, Abe S, Takabatake N, Sata M, et al. Effect of antibiotic therapy on the inflammatory responses during streptococcal pneumonia in emphysematous mice. EXCLI J. 2009;8:50–57. [Google Scholar]
- 7.Kubiet MA, Gonzalez-Rothi RJ, Cottey R, Bender BS. Serum antibody response to influenza vaccine in pulmonary patients receiving corticosteroids. Chest. 1996;110:367–370. doi: 10.1378/chest.110.2.367. [DOI] [PubMed] [Google Scholar]
- 8.Lambert CL, Fauci AS. Influenza vaccines for the future. N Engl J Med. 2010;363:2036–2044. doi: 10.1056/NEJMra1002842. [DOI] [PubMed] [Google Scholar]
- 9.Lipworth BJ. Systemic adverse effects of inhaled corticosteroid therapy: A systematic review and meta-analysis. Arch Intern Med. 1999;159:941–955. doi: 10.1001/archinte.159.9.941. [DOI] [PubMed] [Google Scholar]
- 10.McManus TE, Marley AM, Baxter N, Christie SN, O'Neill HJ, Elborn JS, et al. Respiratory viral infection in exacerbations of COPD. Respir Med. 2008;102:1575–1580. doi: 10.1016/j.rmed.2008.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nichol KL, Nordin JD, Nelson DB, Mullooly JP, Hak E. Effectiveness of influenza vaccine in the community-dwelling elderly. N Engl J Med. 2007;357:1373–1381. doi: 10.1056/NEJMoa070844. [DOI] [PubMed] [Google Scholar]