Summary
A major change is needed in the entrenched culture of routinely administering high-concentration oxygen to acutely ill patients regardless of need.
Oxygen is a drug that should be prescribed for specific indications. There should be a documented target range for oxygen saturation, and regular monitoring of the patient’s response.
There are risks from unrelieved hypoxaemia due to insufficient oxygen therapy, and from provoked hyperoxaemia due to excessive oxygen therapy. Oxygen therapy should therefore be titrated so that the saturation is within a range that avoids these risks.
If oxygen requirements are increasing, the clinician should review the patient and consider transfer to a higher level of care. If oxygen requirements are decreasing, consider reducing or discontinuing oxygen therapy.
Key words: chronic obstructive pulmonary disease, hypercapnia, hypoxaemia, oxygen inhalation therapy
Introduction
Management of the acutely hypoxaemic patient requires evaluation and treatment of the underlying cause of the hypoxaemia. Oxygen therapy relieves hypoxaemia, but not the underlying cause.
Oxygen is a drug and it should be prescribed for specific indications. This prescription should include the target range for oxygen saturation. The response to oxygen administration requires regular monitoring.1-3
Identifying the need for oxygen
In the first assessment of an unwell patient, oxygen saturations can be determined by pulse oximetry. However, clinicians need to be aware that the accuracy of pulse oximetry is variable in clinical practice.4 Arterial blood gases should be measured in patients who are critically unwell, when an oximetry reading cannot be obtained or when hypercapnia is suspected. In view of the widespread use of venous blood gas measurements, clinicians need to be aware that this method cannot accurately determine arterial carbon dioxide.5
Oxygen therapy is indicated in patients with oxygen saturations below the target saturation range. It is not indicated for the treatment of breathlessness in patients with adequate oxygen saturations, apart from certain patients with carbon monoxide poisoning and with pneumothorax.3,6
Prescribing the appropriate dose
Just like any other drug, oxygen should be prescribed at the appropriate dose, to achieve a desired outcome. For oxygen this is the designated saturation range. This approach is important because unrelieved hypoxaemia due to insufficient oxygen therapy, and provoked hyperoxaemia due to excessive oxygen therapy, are both associated with adverse clinical outcomes.7-10
Target oxygen saturation ranges
The recommended target saturation range should be included as part of the patient’s oxygen prescription on the drug chart.
COPD and conditions associated with chronic respiratory failure
In the treatment of exacerbations of chronic obstructive pulmonary disease (COPD), oxygen should be titrated to achieve a target oxygen saturation range of 88–92%. This results in a greater than twofold reduction in mortality, compared with the routine administration of high-concentration oxygen therapy (see Box).9
Box. Evidence for a target oxygen saturation of 88–92% in acute exacerbations of chronic obstructive pulmonary disease9.
In a randomised controlled trial, ambulances were allocated to treat patients having an acute exacerbation of chronic obstructive pulmonary disease with either:
titrated oxygen therapy – oxygen delivered by nasal cannulae as required to achieve target pulse oximetry saturations of 88–92% and bronchodilators delivered by an air-driven nebuliser
or
high-concentration oxygen therapy – 8 L/min via a non-rebreather mask, regardless of oxygen saturation, and bronchodilators given by an oxygen-driven nebuliser.
Key findings were:
mortality was over two times higher in patients who received routine high-concentration oxygen compared with those who received titrated oxygen therapy
the number needed to harm (death) with the routine use of high-concentration oxygen was 14 (one additional person died for every 14 treated).
Uncontrolled oxygen therapy for patients with COPD can cause hypercapnia. Due to concerns that the risks of high-concentration oxygen therapy may also apply in other conditions that place patients at risk of hypercapnic respiratory failure (cystic fibrosis, neuromuscular disorders, chest wall disorders, morbid obesity), the saturation target of 88–92% has also been recommended for these patients.3
Other acute medical conditions
Due to limited evidence from randomised controlled trials to guide clinical practice, it has been difficult to set a target saturation range for other acute medical conditions, such as asthma, pneumonia and acute coronary syndrome.8,11-13 A pragmatic guide is to only give oxygen if saturations are under 92%, with a target saturation range of 92–96%.
Selecting the appropriate delivery method
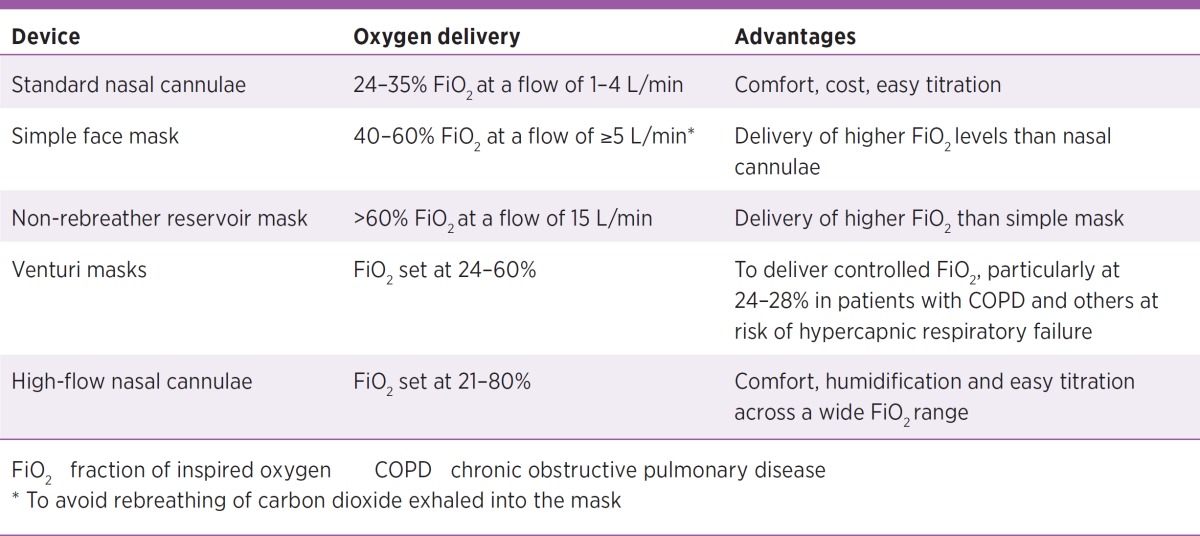
Oxygen can be delivered through a number of devices (Table). For most patients, standard nasal cannulae are the preferred method of delivery. The flow rate is varied to achieve the target oxygen saturation.
Table. Oxygen-delivery devices.
Nebulisers
In patients with COPD, titration of oxygen therapy should continue during bronchodilator administration, if required, to achieve the 88–92% target oxygen saturation range. This can be done by giving titrated oxygen through nasal cannulae and giving the bronchodilator through an air-driven nebuliser. There is evidence from a randomised controlled trial for this approach (see Box).9
An alternative to nebulisation that allows for the ongoing titration of oxygen therapy is to give the bronchodilator from a metered dose inhaler via a spacer. If an oxygen-driven nebuliser must be used, the duration of each nebulisation should be limited.3
Patients who improve
If the patient’s clinical condition improves to the extent that their oxygen saturation exceeds the target oxygen saturation range, this is an indication to reduce the concentration of inspired oxygen. Monitoring of oxygen saturations should be continued to detect subsequent deterioration of the underlying condition and the requirement to increase or resume oxygen therapy.
Patients who deteriorate
If oxygen saturations fall or increasing oxygen concentrations are required to maintain oxygen saturation within the target range, review the patient and consider measurement of their arterial blood gases.
In hospital a need for a fraction of inspired oxygen (FiO2) greater than 40% should trigger a review by a senior clinician. If the patient requires an FiO2 greater than 50%, consultation with intensive care is recommended. Increased monitoring and non-invasive or invasive ventilation should be considered.
If oxygen-induced hypercapnia develops, oxygen therapy should not be abruptly stopped. This may lead to rebound hypoxaemia (with a fall in oxygen saturation to below the level seen before oxygen was given).14,15 Oxygen should be gradually down-titrated and non-invasive ventilation considered.
Prophylactic oxygen therapy
There are risks in the practice of administering prophylactic oxygen to a breathless patient who is not currently hypoxaemic, in the belief that it may prevent hypoxaemia if the underlying condition deteriorates. This practice has the potential to cause delay in recognising clinical deterioration and reduce the time available to start additional treatment.16
Conclusion
A major shift is occurring in the use of oxygen therapy. This shift is based on the recognition that the routine administration of high-concentration oxygen to acutely unwell patients has the potential to cause harm. Oxygen therapy should be titrated to ensure patients have an oxygen saturation within a target range. This reduces the risks of both hypoxaemia and hyperoxaemia.
Footnotes
The Medical Research Institute of New Zealand has received research funding from Fisher and Paykel Healthcare (the manufacturer of high-flow nasal cannula devices).
Reference
- 1.Thomson AJ, Webb DJ, Maxwell SR, Grant IS. Oxygen therapy in acute medical care. BMJ 2002;324:1406-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beasley R, McNaughton A, Robinson G. New look at the oxyhaemoglobin dissociation curve. Lancet 2006;367:1124-6. [DOI] [PubMed] [Google Scholar]
- 3.O’Driscoll BR, Howard LS, Davison AG, British Thoracic Society . BTS guideline for emergency oxygen use in adult patients. Thorax 2008;63 Suppl 6:vi1-68. [DOI] [PubMed] [Google Scholar]
- 4.Young IH. Oximetry. Aust Prescr 2003;26:132-5. [Google Scholar]
- 5.Byrne AL, Bennett M, Chatterji R, Symons R, Pace NL, Thomas PS. Peripheral venous and arterial blood gas analysis in adults: are they comparable? A systematic review and meta-analysis. Respirology 2014;19:168-75. [DOI] [PubMed] [Google Scholar]
- 6.MacDuff A, Arnold A, Harvey J, BTS Pleural Disease Guideline Group . Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. Thorax 2010;65 Suppl 2:ii18-31. [DOI] [PubMed] [Google Scholar]
- 7.Cameron L, Pilcher J, Weatherall M, Beasley R, Perrin K. The risk of serious adverse outcomes associated with hypoxaemia and hyperoxaemia in acute exacerbations of COPD. Postgrad Med J 2012;88:684-9. [DOI] [PubMed] [Google Scholar]
- 8.Sjöberg F, Singer M. The medical use of oxygen: a time for critical reappraisal. J Intern Med 2013;274:505-28. [DOI] [PubMed] [Google Scholar]
- 9.Austin MA, Wills KE, Blizzard L, Walters EH, Wood-Baker R. Effect of high flow oxygen on mortality in chronic obstructive pulmonary disease patients in prehospital setting: randomised controlled trial. BMJ 2010;341:c5462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McHugh G, Freebairn R. Optimal oxygen therapy in the critically ill patient with respiratory failure. Curr Respir Med Rev 2010;6:229-37. [Google Scholar]
- 11.Ranchord AM, Argyle R, Beynon R, Perrin K, Sharma V, Weatherall M, et al. High-concentration versus titrated oxygen therapy in ST-elevation myocardial infarction: a pilot randomized controlled trial. Am Heart J 2012;163:168-75. [DOI] [PubMed] [Google Scholar]
- 12.Perrin K, Wijesinghe M, Healy B, Wadsworth K, Bowditch R, Bibby S, et al. Randomised controlled trial of high concentration versus titrated oxygen therapy in severe exacerbations of asthma. Thorax 2011;66:937-41. [DOI] [PubMed] [Google Scholar]
- 13.Wijesinghe M, Perrin K, Healy B, Weatherall M, Beasley R. Randomized controlled trial of high concentration oxygen in suspected community-acquired pneumonia. J R Soc Med 2012;105:208-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kane B, Turkington PM, Howard LS, Davison AG, Gibson GJ, O’Driscoll BR. Rebound hypoxaemia after administration of oxygen in an acute exacerbation of chronic obstructive pulmonary disease. BMJ 2011;342:d1557. [DOI] [PubMed]
- 15.Rudolf M, Turner JA, Harrison BD, Riordan JF, Saunders KB. Changes in arterial blood gases during and after a period of oxygen breathing in patients with chronic hypercapnic respiratory failure and in patients with asthma. Clin Sci (Lond) 1979;57:389-96. [DOI] [PubMed] [Google Scholar]
- 16.Beasley R, Aldington S, Robinson G. Is it time to change the approach to oxygen therapy in the breathless patient? Thorax 2007;62:840-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Further reading
- Beasley R, Chien J, Douglas J, Eastlake L, Farah C, King G, et al. TSANZ Oxygen guidelines for acute oxygen use in adults; swimming between the flags. Respirology. Forthcoming 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy R, Driscoll P, O’Driscoll R. Emergency oxygen therapy for the COPD patient. Emerg Med J 2001;18:333-9. [DOI] [PMC free article] [PubMed] [Google Scholar]