Summary
Stable angina pectoris is characterised by typical exertional chest pain that is relieved by rest or nitrates.
Risk stratification of patients is important to define prognosis, to guide medical management and to select patients suitable for revascularisation.
Medical treatment aims to relieve angina and prevent cardiovascular events. Beta blockers and calcium channel antagonists are first-line options for treatment. Short-acting nitrates can be used for symptom relief.
Low-dose aspirin and statins are prescribed to prevent cardiovascular events.
Key words: beta blockers, calcium channel antagonists, glyceryl trinitrate, stable angina
Introduction
Cardiovascular disease is the leading cause of death in Australia. Angina pectoris affects more than 353 000 Australians and accounts for approximately 72 000 hospital admissions annually.1
Angina is caused by myocardial ischaemia. Chronic stable angina has a consistent duration and severity, and is provoked by a predictable level of exertion. It can also be provoked by emotional stress. The pain is relieved by rest or short-acting nitrates.2
The aim of medical therapy is to minimise symptoms and retard disease progression. This requires lifestyle modification as well as drug treatment.3-6
Diagnosis
The diagnosis of angina is usually suspected from a thorough history and examination. Patients should have an ECG and undergo assessment for cardiovascular risk factors such as diabetes7 and hyperlipidaemia.4 An echocardiograph can help with the assessment of left ventricular function.8 Once the clinical diagnosis of stable coronary artery disease is established, the patient’s risk of future cardiovascular events is evaluated.
Risk stratification
In patients with stable coronary artery disease the risk of cardiovascular mortality may be predicted by clinical and demographic variables. These include gender,9 left ventricular function,8,9 the provocation of myocardial ischaemia with stress testing,10,11 and the severity of coronary artery disease seen on angiography.3,5,8,12,13 Patients at high risk of cardiovascular events may need revascularisation14,15 as well as medical therapy.
Clinical evaluation
The history, examination, ECG and laboratory tests provide important prognostic information. Increasing age, chronic kidney disease, diabetes, hypertension, current smoking, previous myocardial infarction, hypercholesterolaemia and heart failure are predictive of adverse outcomes.9
Echocardiography
Echocardiography provides information about left ventricular function, and regional wall motion abnormalities that may be related to infarction or ischaemia. In patients with stable coronary artery disease, left ventricular ejection fraction is the strongest predictor of long-term survival. The 12-year survival of medically treated patients with ejection fractions greater than 50% is 73%, and 54% if the ejection fraction is between 35% and 49%. Survival is only 21% if the ejection fraction is less than 35%.8
Stress testing
Stress testing on a treadmill or bicycle is recommended for patients with normal resting ECGs who can exercise.2,10 Symptoms such as chest discomfort and dyspnoea, exercise workload, blood pressure response and ECG changes consistent with ischaemia are recorded as the patient exercises.10 Abnormalities present at rest such as atrial fibrillation, left ventricular hypertrophy, intraventricular conduction abnormalities and ECG changes related to electrolyte imbalance or digoxin will result in more frequent false-positive results. Stress testing is also used to evaluate the efficacy of revascularisation and medical treatment, and to direct the prescription of exercise.2,3,16
Exercise or pharmacological stress echocardiography may be necessary to demonstrate ischaemic changes in left ventricular systolic function in patients whose resting ECGs5 are abnormal or unable to be interpreted (because of left bundle branch block, paced rhythm). Exercise echocardiography provides information about cardiac structure and function, exercise workload, heart rate and rhythm and blood pressure response. Pharmacological testing may be necessary in patients who cannot exercise.3,5 Myocardial perfusion scintigraphy is an alternative for those with uninterpretable ECGs or inability to exercise.11
Imaging of coronary arteries
Computed tomography (CT) of the coronary arteries without contrast injection can show coronary calcification,17 although correlation with the degree of luminal narrowing is poor.
Intravenous injection of a contrast agent allows visualisation of the vessel lumen. The severity and extent of the lesions determine the risk of a cardiovascular event (Table 1).12,16,18-20 CT angiography exposes patients to radiation. It should be reserved for those who are not overweight, without excessive coronary calcium (Agatston score <400) and who are in sinus rhythm with resting heart rates of 65 beats/minute or less, with or without medication.
Table 1. Risk stratification by CT coronary angiography 12,16,18-20.
| Risk of cardiovascular event | Angiographic findings |
|---|---|
| High | Disease of left main or left anterior descending coronary artery, three-vessel disease with proximal stenoses |
| Intermediate | Significant lesion in large and proximal coronary artery, but no high-risk features |
| Low | Normal coronary artery or non-obstructive plaques |
If patients have a high risk of cardiovascular events or if their symptoms are not adequately controlled, invasive coronary angiography may be indicated. It helps define prognosis5 and options for revascularisation. The 12-year survival rate in medically treated patients is 74% for single-vessel disease, 59% for two-vessel disease and 50% for three-vessel coronary disease.12 Severe stenosis of the left main coronary artery or proximal left anterior descending artery has a poor prognosis if not revascularised.8 Conversely, the exclusion of significant obstructive disease on angiography is reassuring.19
Lifestyle modification
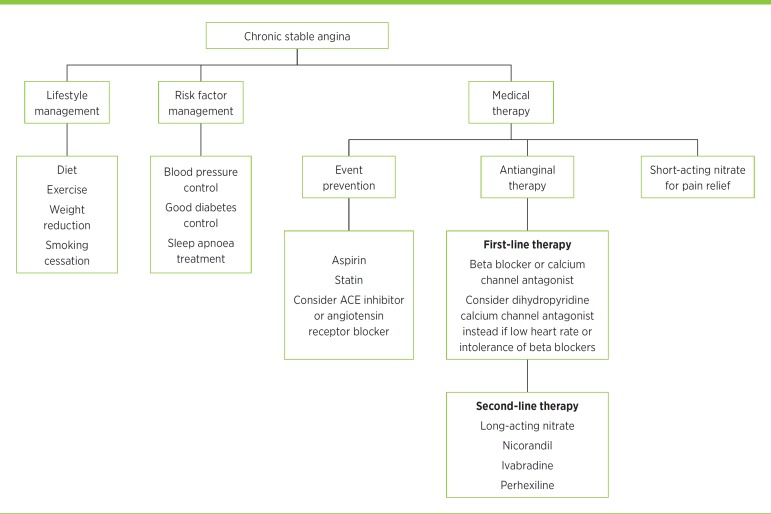
The management of cardiovascular risk factors plays an important role in the overall care of patients with chronic stable angina (Fig.). Modifiable cardiovascular risk factors include hypertension, hypercholesterolaemia, smoking, diabetes, obesity and sedentary lifestyle. Regular exercise, a healthy diet and maintenance of ideal weight reduce the risk of adverse cardiovascular events. Smoking is a strong and independent risk factor for coronary artery disease so efforts to quit should be encouraged and supported. Control of blood pressure and diabetes is paramount to reducing cardiovascular morbidity and mortality. Patients should be screened for sleep apnoea. Annual influenza vaccination is recommended.21,22
Fig.
Management of chronic stable angina
Prevention of cardiovascular events
Low-dose aspirin reduces major cardiac events by up to 30% and should be prescribed to patients with coronary artery disease.3 Clopidogrel is an alternative option for patients intolerant of aspirin. Patients with established coronary artery disease should be prescribed statin therapy irrespective of their lipid profile to slow the progression or even promote regression of coronary atherosclerosis.4
Angiotensin converting enzyme (ACE) inhibitors should be prescribed for patients with stable angina, particularly those who have hypertension, left ventricular dysfunction, diabetes6 or chronic kidney disease. Adverse effects include a persistent cough, hyperkalaemia and, rarely, angioedema. Angiotensin receptor antagonists may be used for those who do not tolerate ACE inhibitors.3
Drug therapy
The aim of drug therapy (Table 2)2,3,5,23 is to minimise symptoms and prevent progression of coronary artery disease. Short-acting nitrates are prescribed to relieve acute symptoms or anticipated angina. Drug therapy aims to reduce myocardial oxygen demand or increase coronary blood supply. The choice of drugs is influenced by factors such as comorbidities, tolerance and adverse effects.
Table 2. Drugs for angina 2,3,5,23.
| Drug | Indications | Mechanism | Adverse effects | Precautions |
|---|---|---|---|---|
| Nitrates (short- and long-acting) | Relief of acute or anticipated pain (short-acting) Prevention of angina (long-acting) |
Systemic and coronary vasodilation | Headache Hypotension Syncope Reflex tachycardia |
Avoid sildenafil and similar drugs Tolerance with long-acting nitrates |
| Beta blockers | First-line therapy for exertional angina and after myocardial infarction | Reduce blood pressure, heart rate and contractility Prolongs diastolic filling time |
Fatigue Altered glucose Bradycardia Heart block Impotence Bronchospasm Peripheral vasoconstriction Hypotension Insomnia or nightmares |
Avoid with verapamil because of risk of bradycardia Avoid in asthma, 2nd and 3rd degree heart block and acute heart failure |
| Dihydropyridine calcium channel antagonists (e.g. amlodipine, felodipine, nifedipine) | Alternative, or in addition, to a beta blocker Coronary spasm |
Systemic and coronary vasodilator | Hypotension Peripheral oedema Headache Palpitations Flushing |
Avoid short-acting nifedipine because of reflex tachycardia and increased mortality in ischaemia |
| Non-dihydropyridine calcium channel antagonists (e.g. verapamil, diltiazem) | Alternative, or in addition, to a beta blocker | Arteriolar vasodilator Centrally acting drugs reduce heart rate, blood pressure, contractility, and prolong diastole |
Negative inotropic effect Bradycardia Heart block Constipation Hypotension Headache |
Avoid verapamil in heart failure and in combination with a beta blocker |
| Nicorandil | Angina | Systemic and coronary vasodilator | Headache Dizziness Nausea Hypotension Gastrointestinal ulceration |
Avoid sildenafil and similar drugs Metformin may reduce efficacy |
| Ivabradine | Angina Chronic heart failure |
Reduces heart rate | Visual disturbances Headache Dizziness Bradycardia Atrial fibrillation Heart block |
Caution with drugs that induce or inhibit cytochrome P450 3A4 Avoid in renal or hepatic failure |
| Perhexiline | Refractory angina | Favours anaerobic metabolism in active myocytes | Headache Dizziness Nausea, vomiting Visual change Peripheral neuropathy |
Narrow therapeutic range Need to monitor adverse effects and drug concentrations |
Beta blockers
Beta blockers are first-line therapy to reduce angina and improve exercise tolerance by limiting the heart rate response to exercise.3,5 Although they reduce the risk of cardiovascular death and myocardial infarction by 30% in post-infarct patients, their benefits in those with stable coronary artery disease are less certain.3,24 The drugs most widely used for angina in the context of normal left ventricular function are the beta1-selective drugs such as metoprolol and atenolol.
Adverse effects include fatigue, altered glucose, bronchospasm, bradycardia, impotence and postural hypotension. Switching to a less lipophilic beta blocker such as atenolol may alleviate symptoms such as insomnia or nightmares. They are usually well tolerated in patients with emphysema who have predominantly fixed airways disease. Beta blockers should not be stopped abruptly due to the risk of rebound hypertension or ischaemia.
Calcium channel antagonists
Calcium channel antagonists improve symptoms of angina via coronary and peripheral vasodilation. They are indicated for those who cannot tolerate or have insufficient control of ischaemic symptoms on beta blockers alone.
Non-dihydropyridine drugs such as verapamil and diltiazem also reduce heart rate and contractility. Verapamil has comparable antianginal activity to metoprolol and can be useful for treatment of supraventricular arrhythmias and hypertension. However, verapamil should be avoided in patients taking beta blockers owing to the risk of heart block, and in those with heart failure because of its negative inotropic effect. Diltiazem has a low adverse effect profile with a modest negative inotropic effect. Care should be taken when prescribing in combination with a beta blocker and in patients with left ventricular dysfunction.
The dihydropyridines such as amlodipine, felodipine and lercanidipine have greater vascular selectivity and minimal negative inotropic properties. They are therefore safer in patients with left ventricular dysfunction. Amlodipine is an effective once-daily antianginal drug that can be used in combination with a beta blocker. Long-acting nifedipine is a proven antianginal drug and is most effective when used in conjunction with a beta blocker.25
Contraindications to nifedipine use include severe aortic stenosis, obstructive cardiomyopathy and heart failure. Short-acting nifedipine is rarely used as monotherapy due to reflex tachycardia, which can worsen ischaemia and has been associated with a dose-related increase in mortality. It should therefore be avoided.
Nitrates
Sublingual glyceryl trinitrate tablets or nitroglycerin spray remain the treatment of choice for rapid relief of acute symptoms and anticipated angina. Sublingual glyceryl trinitrate tablets are absorbed in the sublingual mucosa and take effect within a couple of minutes. The tablet can be discarded with resolution of chest pain to minimise adverse effects such as headache. Glyceryl trinitrate spray is equally effective and, due to its longer shelf-life, is more convenient for those with infrequent symptoms of angina.
Isosorbide dinitrate undergoes hepatic conversion to mononitrate, resulting in an onset of action of 3–4 minutes. It can provide an antianginal effect for up to one hour. Less commonly it is used as a chronic antianginal drug but requires multiple dosing, and tolerance limits its usefulness. It is often used up to three times per day with a nitrate-free period of up to 14 hours to minimise tolerance.
Long-acting nitrates such as oral isosorbide mononitrate or transdermal patches are effective in relieving angina and can improve exercise tolerance. Chronic nitrate therapy is limited by the development of nitrate tolerance. A nitrate-free period of at least eight hours may reduce this problem. The mechanism of nitrate tolerance is not well established but involves attenuation of the vascular effect of the drug rather than altered pharmacokinetics.26 A nitrate-free period restores the vascular reactivity of the vessel. Transdermal patches are generally used for 12 consecutive hours with a 12-hour nitrate-free period. There is no evidence that nitrates improve survival.
Common adverse effects include headache, hypotension and light-headedness. Nitrates should not be prescribed for patients taking phosphodiesterase-5 inhibitors such as sildenafil due to the risk of profound hypotension. Other contraindications include severe aortic stenosis and hypertrophic cardiomyopathy.
Nicorandil
Nicorandil is a potassium channel activator that improves coronary flow as a result of both arterial and venous dilation. It may be used in addition to beta blockers and calcium channel antagonists to control angina or in patients who are intolerant of nitrates. Nicorandil has been shown to reduce cardiovascular events by 14% in patients with chronic stable angina.27 Its use has been associated with headaches, hypotension, painful ulcers and genital and gastrointestinal fistulae.28
Ivabradine
Ivabradine can be considered for patients intolerant of, or insufficiently responsive to, other drugs. It acts on If channels in the sinus node to lower the heart rate of patients in sinus rhythm without affecting blood pressure, conduction or myocardial contractility.29 Ivabradine has been shown to reduce a composite primary end point of cardiovascular death and hospitalisation with myocardial infarction or heart failure. However, a recent placebo-controlled trial involving 19 102 patients with stable coronary artery disease found that adding ivabradine to standard therapy did not improve a composite outcome of death from cardiovascular causes, or non-fatal myocardial infarction.30 Ivabradine has been used in combination with beta blockers.31
Perhexiline
Perhexiline promotes anaerobic metabolism of glucose in active myocytes. Its use is limited by a narrow therapeutic window and high pharmacokinetic variability.23 Given its potential for toxic effects such as peripheral neuropathy and hepatic damage, it is usually reserved for patients whose angina is refractory to other therapies. It may be used safely with conscientious monitoring of clinical effects and regular measurement of plasma drug concentrations.32
Conclusion
Stable angina is typically provoked by exertion and relieved by rest or nitrate therapy.2 Risk stratification should be done to define prognosis, guide management and select appropriate patients for revascularisation.3,5,19 The aims of medical therapy are to control symptoms, improve quality of life and prevent cardiovascular events.2,5 Beta blockers and calcium channel antagonists remain first-line options for treatment. Short-acting nitrates can be used for symptoms.
Footnotes
Conflict of interest: none declared
References
- 1.Australian Institute of Health and Welfare. Cardiovascular disease: Australian facts 2011. Cardiovascular disease series no 35. Cat. No. CVD 53. Canberra: AIHW; 2011. www.aihw.gov.au/publication-detail/?id=10737418510 [cited 2015 Jul 1]
- 2.Abrams J. Clinical practice. Chronic stable angina. N Engl J Med 2005;352:2524-33. [DOI] [PubMed] [Google Scholar]
- 3.Montalescot G, Sechtem U, Achenbach S, Andreotti F, Arden C, Budaj A, et al. Task Force Members. ESC Committee for Practice Guidelines. Document Reviewers . 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J 2013;34:2949-3003. [DOI] [PubMed] [Google Scholar]
- 4.Catapano AL, Reiner Z, De Backer G, Graham I, Taskinen MR, Wiklund O, et al. European Society of Cardiology (ESC) European Atherosclerosis Society (EAS) . ESC/EAS Guidelines for the management of dyslipidaemias: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Atherosclerosis 2011;217:3-46. [DOI] [PubMed] [Google Scholar]
- 5.Fihn SD, Gardin JM, Abrams J, Berra K, Blankenship JC, Dallas AP, et al. American College of Cardiology Foundation. American Heart Association Task Force on Practice Guidelines. American College of Physicians. American Association for Thoracic Surgery. Preventive Cardiovascular Nurses Association. Society for Cardiovascular Angiography and Interventions. Society of Thoracic Surgeons . 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol 2012;60:e44-164. [DOI] [PubMed] [Google Scholar]
- 6.Heart Outcomes Prevention Evaluation Study Investigators . Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: results of the HOPE study and MICRO-HOPE substudy [Erratum in: Lancet 2000;356:860]. Lancet 2000;355:253-9. [PubMed] [Google Scholar]
- 7.Norhammar A, Lagerqvist B, Saleh N. Long-term mortality after PCI in patients with diabetes mellitus: results from the Swedish Coronary Angiography and Angioplasty Registry. EuroIntervention 2010;5:891-7. [PubMed] [Google Scholar]
- 8.Emond M, Mock MB, Davis KB, Fisher LD, Holmes DR, Jr, Chaitman BR, et al. Long-term survival of medically treated patients in the Coronary Artery Surgery Study (CASS) Registry. Circulation 1994;90:2645-57. [DOI] [PubMed] [Google Scholar]
- 9.Hjemdahl P, Eriksson SV, Held C, Forslund L, Näsman P, Rehnqvist N. Favourable long term prognosis in stable angina pectoris: an extended follow up of the angina prognosis study in Stockholm (APSIS). Heart 2006;92:177-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ashley EA, Myers J, Froelicher V. Exercise testing in clinical medicine. Lancet 2000;356:1592-7. [DOI] [PubMed] [Google Scholar]
- 11.Schinkel AF, Bax JJ, Geleijnse ML, Boersma E, Elhendy A, Roelandt JR, et al. Noninvasive evaluation of ischaemic heart disease: myocardial perfusion imaging or stress echocardiography? Eur Heart J 2003;24:789-800. [DOI] [PubMed] [Google Scholar]
- 12.Califf RM, Armstrong PW, Carver JR, D’Agostino RB, Strauss WE. 27th Bethesda Conference: matching the intensity of risk factor management with the hazard for coronary disease events. Task Force 5. Stratification of patients into high, medium and low risk subgroups for purposes of risk factor management. J Am Coll Cardiol 1996;27:1007-19. [DOI] [PubMed] [Google Scholar]
- 13.Prasad A, Rihal C, Holmes DR, Jr. The COURAGE trial in perspective. Catheter Cardiovasc Interv 2008;72:54-9. [DOI] [PubMed] [Google Scholar]
- 14.Rihal CS, Raco DL, Gersh BJ, Yusuf S. Indications for coronary artery bypass surgery and percutaneous coronary intervention in chronic stable angina: review of the evidence and methodological considerations. Circulation 2003;108:2439-45. [DOI] [PubMed] [Google Scholar]
- 15.Hemingway H, Crook AM, Feder G, Banerjee S, Dawson JR, Magee P, et al. Underuse of coronary revascularization procedures in patients considered appropriate candidates for revascularization. N Engl J Med 2001;344:645-54. [DOI] [PubMed] [Google Scholar]
- 16.Lin FY, Dunning AM, Narula J, Shaw LJ, Gransar H, Berman DS, et al. Impact of an automated multimodality point-of-order decision support tool on rates of appropriate testing and clinical decision making for individuals with suspected coronary artery disease: a prospective multicenter study. J Am Coll Cardiol 2013;62:308-16. [DOI] [PubMed] [Google Scholar]
- 17.Raggi P, Gongora MC, Gopal A, Callister TQ, Budoff M, Shaw LJ. Coronary artery calcium to predict all-cause mortality in elderly men and women. J Am Coll Cardiol 2008;52:17-23. [DOI] [PubMed] [Google Scholar]
- 18.Min JK, Dunning A, Lin FY, Achenbach S, Al-Mallah M, Budoff MJ, et al. CONFIRM Investigators . Age- and sex-related differences in all-cause mortality risk based on coronary computed tomography angiography findings results from the International Multicenter CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter Registry) of 23,854 patients without known coronary artery disease. J Am Coll Cardiol 2011;58:849-60. [DOI] [PubMed] [Google Scholar]
- 19.Jacq L, Chabredier-Paquot C, Pezzano M, Caussin C, Habis M, Schaison F, et al. [Prognostic value of normal coronary angiography] [French.]. Ann Cardiol Angeiol (Paris) 2001;50:404-7. [DOI] [PubMed] [Google Scholar]
- 20.Ostrom MP, Gopal A, Ahmadi N, Nasir K, Yang E, Kakadiaris I, et al. Mortality incidence and the severity of coronary atherosclerosis assessed by computed tomography angiography. J Am Coll Cardiol 2008;52:1335-43. [DOI] [PubMed] [Google Scholar]
- 21.Nichol KL, Nordin J, Mullooly J, Lask R, Fillbrandt K, Iwane M. Influenza vaccination and reduction in hospitalizations for cardiac disease and stroke among the elderly. N Engl J Med 2003;348:1322-32. [DOI] [PubMed] [Google Scholar]
- 22.Ciszewski A, Bilinska ZT, Brydak LB, Kepka C, Kruk M, Romanowska M, et al. Influenza vaccination in secondary prevention from coronary ischaemic events in coronary artery disease: FLUCAD study. Eur Heart J 2008;29:1350-8. [DOI] [PubMed] [Google Scholar]
- 23.Horowitz JD, Mashford ML. Perhexiline maleate in the treatment of severe angina pectoris. Med J Aust 1979;1:485-8. [DOI] [PubMed] [Google Scholar]
- 24.Bangalore S, Bhatt DL, Steg PG, Weber MA, Boden WE, Hamm CW, et al. β-blockers and cardiovascular events in patients with and without myocardial infarction: post hoc analysis from the CHARISMA trial. Circ Cardiovasc Qual Outcomes 2014;7:872-81. [DOI] [PubMed] [Google Scholar]
- 25.Furberg CD, Psaty BM, Meyer JV. Nifedipine. Dose-related increase in mortality in patients with coronary heart disease. Circulation 1995;92:1326-31. [DOI] [PubMed] [Google Scholar]
- 26.Parker JD, Parker JO. Nitrate therapy for stable angina pectoris. N Engl J Med 1998;338:520-31. [DOI] [PubMed] [Google Scholar]
- 27.IONA Study Group . Effect of nicorandil on coronary events in patients with stable angina: the Impact Of Nicorandil in Angina (IONA) randomised trial. Lancet 2002;359:1269-75. [DOI] [PubMed] [Google Scholar]
- 28.McDaid J, Reichl C, Hamzah I, Fitter S, Harbach L, Savage AP. Diverticular fistulation is associated with nicorandil usage. Ann R Coll Surg Engl 2010;92:463-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fox K, Ford I, Steg PG, Tendera M, Ferrari R, BEAUTIFUL Investigators . Ivabradine for patients with stable coronary artery disease and left-ventricular systolic dysfunction (BEAUTIFUL): a randomised, double-blind, placebo-controlled trial. Lancet 2008;372:807-16. [DOI] [PubMed] [Google Scholar]
- 30.Fox K, Ford I, Steg PG, Tardif JC, Tendera M, Ferrari R, SIGNIFY Investigators . Ivabradine in stable coronary artery disease without clinical heart failure. N Engl J Med 2014;371:1091-9. [DOI] [PubMed] [Google Scholar]
- 31.Tardif JC, Ponikowski P, Kahan T, ASSOCIATE Study Investigators . Efficacy of the I(f) current inhibitor ivabradine in patients with chronic stable angina receiving beta-blocker therapy: a 4-month, randomized, placebo-controlled trial. Eur Heart J 2009;30:540-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ashrafian H, Horowitz JD, Frenneaux MP. Perhexiline. Cardiovasc Drug Rev 2007;25:76-97. [DOI] [PubMed] [Google Scholar]