Summary
The first aid for burns is to run cold water over the burn for 20 minutes. This is effective for up to three hours after the injury.
Assess the affected body surface area using the rule of nines. Consult a burn unit if more than 5% of the total body surface area is burnt in a child or if more than 10% in an adult.
Extensive or deep burns and burns to special areas, such as the hands, should be referred. Chemical or electrical burns should also be assessed by a burn unit.
For minor burns, antimicrobial dressings are recommended, but oral antibiotics should be avoided unless there are signs of infection. As burns are tetanus prone, check the patient’s immunisation status.
Burns that become infected or are slow to heal should be discussed with a burn unit. The burn unit can also provide advice if there are uncertainties about how to manage a patient.
Key words: dressings, first aid, skin, burns
Introduction
Burns affect at least 1% of Australians each year,1 although the number is probably higher due to the under-reporting of minor burn injuries. Pharmacists and GPs may be asked about managing minor burns. The majority of injuries are caused by scalds from hot liquids, contact with hot objects and fire. However mechanisms such as friction burns, for example from treadmills, are becoming more prevalent.1-3
Determining the severity of a burn injury
The significance of a burn injury depends on its depth and the percentage of total body surface area affected. The depth of the injury is determined by the temperature of the heat source and the duration of contact with that source.1
The rule of nines is a practical method to quantify the area affected by the burn.4 For a person at least 10 years old, the head is equal to 9%, each upper limb 9%, the anterior trunk 18%, the posterior trunk 18% and each lower limb 18% (see Fig.).1,4 In children under 10 years old, the rule varies slightly, as the head represents a larger proportion of their body surface area. In addition, the palm and fingers of the patient of all ages can be used to estimate 1% total body surface area, which is useful when calculating scattered burn injuries.1
Fig.
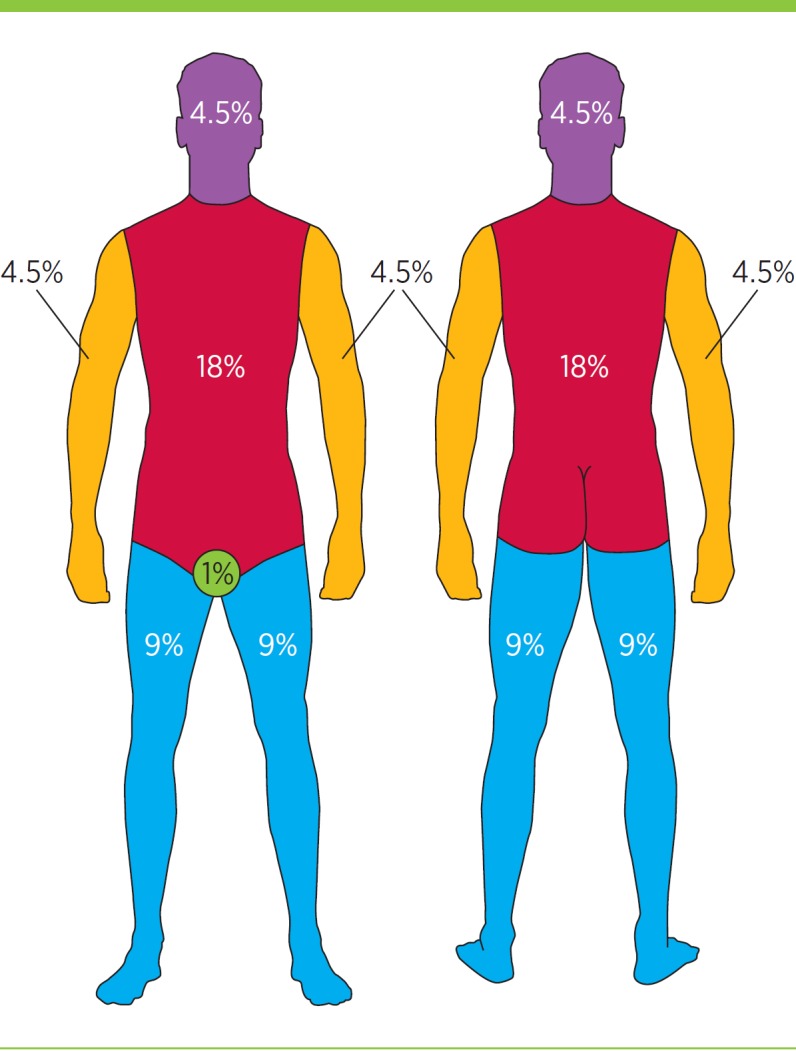
The rule of nines, for burns in people at least 10 years old
Percentages represent proportions of total body surface area.
Capillary refill is a good indicator of the depth of the burn. Any burn that is only erythematous and does not have blisters or a break in the skin is superficial.
Any burn with brisk capillary refill is also likely to be superficial. Burns with slow capillary refill, or that are white, mottled or cherry red in appearance, are likely to be deep.1
When to refer
In general terms, if more than 10% of the total body surface area is burnt in children, and more than 20% in adults, the injuries are severe and must be referred to a specialist burn unit, as emergency management and fluid resuscitation are required (see Box).1 This is due to the release of inflammatory mediators which leads to a systemic inflammatory response and potential shock.1
Box. Burn unit referral criteria1.
Burns >10% total body surface area
Full thickness burns >5% total body surface area
Paediatric burns >5% total body surface area
Burns to the face, hands, feet, genitalia, perineum and major joints
Chemical burns
Electrical burns including lightning injuries
Burns with associated trauma
Burns with inhalation injury
Circumferential burns of the limbs or chest
Burns in patients with pre-existing medical conditions
Burns with suspected non-accidental injury, assault or self-inflicted
Burns during pregnancy
Burns in the extremes of age – infants and elderly
Infected burns (although not an Australian and New Zealand Burn Association criterion, we recommend that infected burns be referred to a burn unit)
Burns of 5–10% total body surface area in children and 10–20% in adults still require referral as the patients may require admission for management of problems such as pain.1,5
Patients should also be referred to a burn unit if the injury involves the airway, face or neck, or affects the hands, feet or perineum.5 Patients with significant medical comorbidities such as diabetes, those who are immunocompromised, very young or very old patients, and those with associated trauma should also be referred.1
All patients with burn injuries from chemical or electrical sources should be referred to a burn unit.5 Chemical burns often cause very deep injuries and may require specific decontamination or urgent debridement. Electrical injuries, while potentially appearing innocuous, may require cardiac monitoring due to the risk of cardiac arrhythmia.1
Any burn that crosses a joint should be referred as it may lead to significant scar contracture irrespective of size.1 Circumferential burns and burns with the potential to compromise circulation or respiratory effort should be referred immediately for consideration of escharotomy.1
Small burns and those localised to specialised areas can be significant. For example friction burns from treadmills to the fingers of a toddler often require skin grafting, leave permanent scarring and have a risk of lifelong morbidity due to scar contracture.2
Some burns that do not initially meet the criteria for referral to a tertiary hospital may still need consultation with a burn unit if the wound takes longer than 10 days to heal. Burns that take longer than 14 days to heal may scar and any burn that takes longer than 21 days will very likely scar.6 Burn units not only look after acute burn injuries but also provide management of scarring if required.
Any burn more than the size of a 20 cent piece, or deep burns that are smaller, need to be reviewed by a medical practitioner for advice and potential referral.
What can be managed in the community?
Small superficial burns that do not meet the criteria for referral can be managed by GPs. A pharmacist may provide first aid and advice on wound dressing, but has a key role in recommending medical attention when required.
Burn units are always available for consultation. Photographs can be sent for advice if necessary. They can also be used to monitor healing.
First aid
If someone is on fire, it is important for them to stop, drop, cover their face and roll. Clothing, nappies and jewellery must be removed, as they can continue to burn and store heat. If, however, the clothing is firmly stuck to the skin, cut around the area leaving adherent cloth in place.1 This will require removal in hospital.
For all thermal burns, 20 minutes of cold running water (2–15° C) has been proven to reduce the area and depth of the burn.7 Consequently, this reduces the area requiring skin grafting.8,9 Cold running water should ideally be applied within an hour of the injury, but is useful up to three hours post injury.10 It may also have an analgesic effect.10 Copious cold running water should be used to decontaminate chemical burns.1 Ice is never appropriate first aid for burns, as it can deepen these injuries and cause hypothermia.7
Care must be taken with cooling to avoid hypothermia. This is particularly important in people with large surface area burns, young children and older people. These patients must be kept warm by covering unaffected areas as much as possible.1
Hydrogels containing tea tree oil have also been shown to have an analgesic effect, and sheet hydrogels may be useful as a temporary wound cover.11 They do not, however, replace the need for 20 minutes of cold running water, and hypothermia is also a risk.11
Wound management for minor burns
Following the application of cold running water, wound management depends on the integrity of the skin. If the skin is intact and not blistered, wound coverage is not necessary and the application of a simple moisturiser is recommended.1 If the skin is blistered or broken, an assessment of wound size and depth should be undertaken. Consultation with a burn unit should be considered.
Burns are tetanus prone. Tetanus immunisation status and subsequent immunisation or provision of tetanus immunoglobulins should be considered.1
Dressings
A large range of dressings can be applied to burns.12 The most important principles are to keep the wound clean and moist during healing.1 If blisters are present, or have been broken, use a protective dressing.1 An antimicrobial dressing is generally recommended. Silver dressings, which come in many forms (e.g. nanocrystalline silver sheets, silver impregnated foam, hydrofibre) or products such as chlorhexidine-impregnated tulle gras can be useful for their antimicrobial properties. If any signs of infection develop, patients should be referred to a burn unit.
Dressings should be applied according to the manufacturers’ recommendations. The frequency of dressing changes can vary from daily to weekly, and is determined by the product used and the amount of wound exudate. While health practitioners may favour a less expensive dressing, they should be aware that less frequent dressing changes and a lower chance of infection may make some relatively expensive antimicrobial dressings more cost-effective. As burns are very painful, fewer dressing changes, and therefore less associated procedural pain and distress, are highly desirable and may expedite healing.13,14
The length of treatment depends on the time to healing. This is generally indicated by a pink, fully epithelialised wound surface.
Silver sulfadiazine cream
In the recent past, creams containing silver sulfadiazine were commonly used for burn injuries.15,16 While an effective antimicrobial, silver sulfadiazine requires daily dressing changes, which can be labour intensive and distressing for patients. Silver sulfadiazine produces a pseudo-eschar, which makes burns assessment difficult and may be implicated in reduced rates of wound re-epithelialisation.15,16 With the advent of new dressing technologies, the role of silver sulfadiazine should be limited to treating infected burns.
If it is used on an infected burn, silver sulfadiazine cream should be applied onto a sterile cloth or tulle gras. This ensures that it remains in contact with the wound bed.15 Infected burns should be referred to a burn unit as soon as possible as early debridement and intravenous antibiotics may be indicated.
Moisturising creams
Burn injuries often lead to dry skin and pruritus so moisturisers are commonly recommended. There are many moisturising products available, but a simple water-based sorbolene cream is very efficacious and cost-effective.1 In patients with intact, non-blistered skin, a moisturising cream can be used for primary wound management.1 Dry skin and pruritus can sometimes persist for many months after the burn has healed. Regular application of a water-based moisturising cream is recommended. However, moisturising products containing sodium lauryl sulphate, such as aqueous cream, are not recommended as they have been shown in some instances to worsen dryness.17,18 There is little evidence that adding vitamin E to sorbolene cream results in scar reduction but such creams are commonly used.19
Soaps
Generally, soaps should be avoided due to their drying nature, sometimes for up to 12 months post injury. Washing with a moisturising cream or a non-soap-based product is recommended.
Oils
Oils are generally discouraged in the initial months after a burn, especially in children, as they are not readily absorbed into the skin. They may interfere with the integrity of pressure garments which are prescribed for scar management in some patients.
In the longer term, bath oils may be of benefit to some individuals. Some bath oils are infused with colloidal oatmeal which may relieve itch. Products such as Bio-Oil or vitamin E oil can be used for scar management, however evidence of their effectiveness is limited and conflicting.19
Sun protection
Sun protection is essential. Sun exposure in the initial 12 months after injury is anecdotally known to increase the risk of skin pigmentation. In the longer term, burned skin is at higher risk of malignancy than unburned skin.20 When choosing a product, those for sensitive skin are preferred. In the initial post-burn period, creams may be too irritant or too oily. Other measures such as protective clothing should therefore be strongly recommended.1
Antipruritics
Pruritus is commonly experienced after a burn, particularly by patients with larger injuries. Itching and consequent scratching can be extremely detrimental to wound healing. In many instances antihistamines may be required.21 Topical preparations such as moisturising cream or colloidal oatmeal may also have a role.22 In patients with larger burn injuries, and pruritus resistant to first-line treatments, drugs such as gabapentin may be considered by burn or pain specialists.23,24
Oral antibiotics
The prescribing of prophylactic oral antibiotics within the community setting is an area of increasing concern. The inappropriate use of antibiotics leads to high incidences of multi-resistant organisms.25 Multi-resistant Staphylococcus aureus and multi-resistant Pseudomonas aeruginosa are becoming increasingly prevalent and difficult to treat.26 Usually, antimicrobial dressings can keep wound colonisation to a minimum.
Wounds should only be treated with antibiotics if they are clinically infected or a wound swab shows moderate to heavy colonisation despite antimicrobial dressing management, or there is clinical evidence of systemic infection.27 Prescribing of oral antibiotics should align with microbiology results where possible. Any infected burn should be referred to a burn unit for ongoing advice and management.
Conclusion
While some burns require specialist management, vast numbers of injuries present to pharmacists and GPs. Burn units and some plastic surgery units are useful resources if advice regarding management is required. The nearest burn unit28 should be contacted if the patient meets referral criteria.
Footnotes
Conflict of interest: none declared
REFERENCES
- 1.Emergency Management of Severe Burns Manual. 17th ed. The Education Committee of the Australian and New Zealand Burns Association Ltd; 2013. [Google Scholar]
- 2.Kim LH, Maze DA, Adams S, Guitonich S, Connolly S, Darton A, et al. Paediatric treadmill injuries: an increasing problem. Med J Aust 2009;191:516. [DOI] [PubMed] [Google Scholar]
- 3.Jeremijenko L, Mott J, Wallis B, Kimble R. Paediatric treadmill friction injuries. J Paediatr Child Health 2009;45:310-2. [DOI] [PubMed] [Google Scholar]
- 4.Knaysi GA, Crikelair GF, Cosman B. The role of nines: its history and accuracy. Plast Reconstr Surg 1968;41:560-3. [PubMed] [Google Scholar]
- 5.Australian and New Zealand Burn Association. ANZBA referral criteria. 2015. www.anzba.org.au/care/referral-criteria[cited 2015 Jul 1]
- 6.Cubison TC, Pape SA, Parkhouse N. Evidence for the link between healing time and the development of hypertrophic scars (HTS) in paediatric burns due to scald injury. Burns 2006;32:992-9. [DOI] [PubMed] [Google Scholar]
- 7.Cuttle L, Kempf M, Kravchuk O, Phillips GE, Mill J, Wang XQ, et al. The optimal temperature of first aid treatment for partial thickness burn injuries. Wound Repair Regen 2008;16:626-34. [DOI] [PubMed] [Google Scholar]
- 8.Bartlett N, Yuan J, Holland AJ, Harvey JG, Martin HC, La Hei ER, et al. Optimal duration of cooling for an acute scald contact burn injury in a porcine model. J Burn Care Res 2008;29:828-34. [DOI] [PubMed] [Google Scholar]
- 9.Yuan J, Wu C, Holland AJ, Harvey JG, Martin HC, La Hei ER, et al. Assessment of cooling on an acute scald burn injury in a porcine model. J Burn Care Res 2007;28:514-20. [DOI] [PubMed] [Google Scholar]
- 10.Rajan V, Bartlett N, Harvey JG, Martin HC, La Hei ER, Arbuckle S, et al. Delayed cooling of an acute scald contact burn injury in a porcine model: is it worthwhile? J Burn Care Res 2009;30:729-34. [DOI] [PubMed] [Google Scholar]
- 11.ANZBA Use of hydrogels consensus statement. Australian and New Zealand Burns Association; 2012 May.
- 12.Pharmaceutical Society of Australia. Australian Pharmaceutical Formulary and Handbook. 22nd ed. Canberra: Pharmaceutical Society of Australia; 2012. [Google Scholar]
- 13.Brown NJ, Kimble RM, Gramotnev G, Rodger S, Cuttle L. Predictors of re-epithelialization in pediatric burn. Burns 2014;40:751-8. [DOI] [PubMed] [Google Scholar]
- 14.Brown NJ, Kimble RM, Rodger S, Ware RS, McWhinney BC, Ungerer JP, et al. Biological markers of stress in pediatric acute burn injury. Burns 2014;40:887-95. [DOI] [PubMed] [Google Scholar]
- 15.Murphy PS, Evans GR. Advances in wound healing: a review of current wound healing products. Plast Surg Int 2012;2012:190436. [DOI] [PMC free article] [PubMed]
- 16.Atiyeh BS, Costagliola M, Hayek SN, Dibo SA. Effect of silver on burn wound infection control and healing: review of the literature. Burns 2007;33:139-48. [DOI] [PubMed] [Google Scholar]
- 17.Mohammed D, Matts PJ, Hadgraft J, Lane ME. Influence of Aqueous Cream BP on corneocyte size, maturity, skin protease activity, protein content and transepidermal water loss. Br J Dermatol 2011;164:1304-10. [DOI] [PubMed] [Google Scholar]
- 18.Danby SG, Al-Enezi T, Sultan A, Chittock J, Kennedy K, Cork MJ. The effect of aqueous cream BP on the skin barrier in volunteers with a previous history of atopic dermatitis. Br J Dermatol 2011;165:329-34. [DOI] [PubMed] [Google Scholar]
- 19.Zurada JM, Kriegel D, Davis IC. Topical treatments for hypertrophic scars. J Am Acad Dermatol 2006;55:1024-31. [DOI] [PubMed] [Google Scholar]
- 20.Zuo KJ, Tredget EE. Multiple Marjolin’s ulcers arising from irradiated post-burn hypertrophic scars: a case report. Burns 2014;40:e21-5. [DOI] [PubMed] [Google Scholar]
- 21.Baker RA, Zeller RA, Klein RL, Thornton RJ, Shuber JH, Marshall RE, et al. Burn wound itch control using H1 and H2 antagonists. J Burn Care Rehabil 2001;22:263-8. [DOI] [PubMed] [Google Scholar]
- 22.Matheson JD, Clayton J, Muller MJ. The reduction of itch during burn wound healing. J Burn Care Rehabil 2001;22:76-81. [DOI] [PubMed] [Google Scholar]
- 23.Ahuja RB, Gupta GK. A four arm, double blind, randomized and placebo controlled study of pregabalin in the management of post-burn pruritus. Burns 2013;39:24-9. [DOI] [PubMed] [Google Scholar]
- 24.Ahuja RB, Gupta R, Gupta G, Shrivastava P. A comparative analysis of cetirizine, gabapentin and their combination in the relief of post-burn pruritus. Burns 2011;37:203-7. [DOI] [PubMed] [Google Scholar]
- 25.Barajas-Nava LA, López-Alcalde J, Roqué i Figuls M, Solà I, Bonfill Cosp X. Antibiotic prophylaxis for preventing burn wound infection. Cochrane Database Syst Rev 2013;6:CD008738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Branski LK, Al-Mousawi A, Rivero H, Jeschke MG, Sanford AP, Herndon DN. Emerging infections in burns. Surg Infect (Larchmt) 2009;10:389-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.NSW Agency for Clinical Innovation. Clinical Practice Guidelines: Summary of Evidence. ACI Statewide Burn Injury Service. 2014 May.
- 28.Australian and New Zealand Burn Association. Burn units. 2015. http://anzba.org.au/resources/burn-units/ [cited 2015 Jul 1]


