Abstract
Mothers of preterm infants experience significant psychological distress, with elevated levels of inter-correlated depressive symptoms, stress, anxiety and post-traumatic stress symptoms. In a sample of racially and ethnically diverse mothers of preterm infants, we identified differing patterns of psychological distress during infant hospitalization and examined the effect of these psychological distress patterns on longitudinal trajectories of each psychological distress measure and on maternal perceptions of the child over the first year of the infant’s life. Mothers of preterm infants (N = 232) completed five questionnaires assessing depressive symptoms, anxiety, post-traumatic stress symptoms, stress due to infant appearance, and stress due to parental role alteration during enrollment in the neonatal hospitalization, discharge, and at 2, 6, and 12 months of age adjusted for prematurity. Latent class analysis on the enrollment psychological distress variables allowed us to identify five sub-groups of mothers exhibiting similar patterns of psychological distress, differing primarily in degree and type: low distress, moderate distress, high NICU-related distress, high depressive and anxiety symptoms, and extreme distress. These classes continued to show different longitudinal trajectories for the psychological distress measures through 12 months corrected age. Mothers in the extreme distress class and, to a lesser degree, mothers in the high depressive and anxiety symptom class remained at risk of significant psychological distress one year after discharge and had less positive perceptions of their child (greater worry and higher perceptions of child vulnerability). In conclusion, distinctive subgroups of mothers during hospitalization had different patterns of psychological distress throughout the 12-month period and may require different interventions in the NICU.
Keywords: Maternal psychological distress, prematurity, depression, anxiety, stress
1. Introduction
Prematurity affects about 11.5% of all births in the United States.1 Mothers of preterm infants experience significant psychological distress as evidenced by elevated levels of depressive, stress, anxiety and post-traumatic stress symptoms,2 which are often inter-correlated.2–4 The purpose of this study was to identify sub-groups of mothers who showed different patterns of psychological distress (specifically, stress due to infant illness and appearance in the neonatal intensive care unit (NICU), stress due to parental role alteration in the NICU, depressive symptoms, state anxiety, and post-traumatic stress symptoms), to determine whether these sub-groups differed on maternal and infant characteristics and to examine how early psychological distress sub-groups are longitudinally related to psychological distress measures and maternal perceptions of the child throughout the first year after hospital discharge.
Mothers of preterm infants experience marked psychological distress during infant hospitalization.2,4,5 They fear that the infant may not survive and grieve over the infant’s immaturity and frequent health crises.6,7 In addition, the loss of the expected maternal role due to infant illness and separation from the infant during hospitalization is a major source of stress.8,9 Almost 50% of mothers of premature infants have high levels of anxiety and/or depressive symptoms during infant hospitalization.6,9–12 The severity of psychological distress may be related to severity of the infant illness,3 although findings are inconsistent.13,14 In addition, this distress may be worsened by other factors in the mothers’ lives such as daily stressors or post-partum depression.2,15
Elevated levels of maternal psychological distress may continue for months or even years after hospital discharge. The severity of psychological distress after discharge is related to the severity of psychological distress while the infant is hospitalized.2,16 Many mothers of preterm infants continue to have high levels of anxiety and/or depressive symptoms for months after infant hospital discharge,6,9–12 and some show post-traumatic stress symptoms related to the NICU experience and infant illness severity.2,13,17,18
The various types of psychological distress in mothers of preterm infants are inter-correlated, both during hospitalization and after infant discharge.2–4 Yet most studies continue to examine single psychological distress outcomes and do not account for potential response differences within sub-group of mothers,6,12,13,16 with one exception. In a study that only dealt with African-American mothers of preterm infants, researchers identified sub-groups of mothers who had different patterns of psychological distress defined as a composite of six measures of psychological distress.2 However, a comprehensive psychological distress profile for mothers of diverse ethnic groups has not been available to researchers and clinicians. Expanding knowledge to comprehensively understand differences in psychological distress among a diverse population may help us develop ways of identifying sub-groups of mothers with high vulnerability and important periods during the first years to pinpoint effective times for interventions and target resources to ameliorate maternal psychological distress and in turn minimizing poor health outcomes for mothers and their offspring.
This study estimated the inter-correlations between depressive symptoms, state anxiety, post-traumatic stress symptoms, stress due to infant appearance and behavior, and stress due to parental role alteration in a multi-ethnic sample of mothers of pre-term infants during initial hospitalization. We conducted a latent class analysis based on the five measures of maternal psychological distress and examined whether psychological distress class membership was related to characteristics of the mother or infant. Finally, the study tested the effect of psychological distress class membership on longitudinal trajectories of each psychological distress measure over the first year of the infant’s life, maternal worry about child health, parenting stress after-discharge, and maternal perceptions of child vulnerability at 12 months.
2. Methods
The study employed a longitudinal repeated measure design as part of a randomized controlled trial testing the effects of two maternally administered interventions for preterm infants on infant health and development, maternal psychological well-being, and the maternal-infant relationship.19,20 In the parent study the interventions had no effect on maternal psychological distress. The focus on the current analysis was on the psychological distress measures collected at study enrollment, which were measured before the intervention begun and were unlikely to be affected by later psychological distress treatment. Yet the effect of the intervention was included in all longitudinal models to eliminate any possible confounding of intervention effects with the sub-group patterns that are the focus of this report.
2.1. Participants
Participants were 232 mothers of preterm infants weighing less than 1750 grams at birth, who had enrollment data. Mothers and infants were recruited from the neonatal intensive care units (NICUs) of four hospitals (two in a Southeastern state and two in a Midwestern state). The two Southeastern hospitals served suburban and rural populations of diverse socioeconomic status; whereas the two Midwestern hospitals served inner city populations. Recruitment occurred when the infant was no longer critically ill (not on the ventilator or continuous positive airway pressure, not in immediate danger of needing these treatments), without an umbilical artery catheter, and able to be held outside the incubator. Randomization was stratified by recruitment hospital and singleton vs multiple birth infants. Mother-infant dyads were randomized to the intervention groups using a randomization plan pre-determined by the study statistician based on random numbers.
Exclusion criteria included mothers who did not have custody of the infant, whose infants had congenital neurological problems (e.g., congenital hydrocephalus, Down Syndrome) or symptoms of substance exposure, who would have difficulty participating in the study (age less than 15; history of HIV; psychosis or bipolar disease; current diagnosis of major depression; ongoing critical illness; or non-English speaking), or for whom follow-up for 12 months was unlikely (out-of-state mothers). Non-English speaking mothers were excluded because many of the instruments have not been validated for use with monolingual Spanish speakers. All other infants were eligible, including those with postnatal neurological insults or substance exposure without symptoms. For multiple birth infants, one infant from each set was randomly selected for the study. Characteristics of mothers and infants in the sample are presented in Table 1.
Table 1.
Characteristics of the 232 Mothers and Their Preterm Infants
| Mean | (SD) | % | |
|---|---|---|---|
| Maternal Age in Years | 27.0 | (6.1) | |
| % Married | 32.3% | ||
| Maternal Education: Years | 13.4 | (2.3) | |
| Race: % White | 19.8% | ||
| % Black | 69.8% | ||
| % Hispanic | 8.1% | ||
| % Other | 1.9% | ||
| % First-Time Mothers | 55.1% | ||
| % on Public Assistance | 20.3% | ||
| Gestational Age in Weeks | 27.2 | (2.9) | |
| Birthweight in Grams | 1006.2 | (326) | |
| % Small for Gestational Age | 18.7% | ||
| Sex of Child: % Male | 46.1% | ||
| % Multiple Births | 18.3% | ||
| Mechanical Ventilation (days) | 16.7 | (26.7) | |
| % Surgery | 36.1% | ||
| % Patent Ductus Arteriosus | 41.0% | ||
| % Infection | 75% | ||
| % Necrotizing Enterocolitis | 17.6% | ||
| % Intraventricular Hemorrhage | 32.6% | ||
| Neurological Insultsa | 4.1 | (3.7) |
Neurobiologic Risk Scale (NBRS)
2.3. Measures
Infant clinical information was obtained at baseline (when the infant was no longer critically ill) from a review of medical records, including gestational age, multiple birth, size, Apgar score at five minutes, intraventricular hemorrhage, and mechanical ventilation. Maternal sociodemographic information was obtained from questionnaires at baseline, including maternal age, ethnicity, education, marital status, first time mothers, public assistance, and recruitment site. Questionnaires about maternal psychological distress and perceptions of the child were also administered at the same points in time. All the questionnaires have been used and validated with mothers of preterm infants.2
2.3.1. Psychological Distress Measures
The Center for Epidemiologic Studies Depression Scale (CESD) measures the frequency of 20 depressive symptoms, on a 4-point Likert scale, from “rarely or none of the time (less than 1 day in the past week)” to “most or all of the time (5–7 days).”21 Scores range from 0 to 60, with higher scores indicating more depressive symptoms. The CESD cut-off score of 16 is related to a diagnosis of depression though it does not necessarily imply a diagnosis.22 The CESD has good test-retest reliability.21 Cronbach’s alphas in this sample were 0.90 at enrollment, 0.89 at discharge, 0.86 at 2 months, 0.87 at 6 months, and 0.86 at 12 months.
The state sub-scale of the State-Trait Anxiety Inventory (STAI), which measures maternal situational anxiety, includes 20 items and has been found to be sensitive to changes in anxiety levels.23 Total scores range from 20 to 80, with higher scores correlating with greater anxiety.23 Stability coefficients of the state sub-scale range from .16 to .53, as would be expected since it was designed to be influenced by situational factors.23 Cronbach’s alphas in this sample were 0.93 at enrollment, 0.92 at discharge, 0.88 at 2 months, 0.90 at 6 months, and 0.91 at 12 months.
The Perinatal Post-Traumatic Stress Symptom Questionnaire (PPQ) measured the extent to which mothers experience post-traumatic stress symptoms in response to the birth of a high-risk infant and the NICU experience.17 The PPQ has 14 yes-no items that measure intrusive thoughts (e.g., bad dreams of giving birth), avoidance or numbing (e.g., inability to remember parts of the hospitalization), and increased arousal (e.g., increased irritability or anger). The “yes” answers are summed. Scores of 6 or greater are indicative of elevated PTSD symptoms. Test-retest reliability over 2 to 4 weeks was .92.17 Cronbach’s alphas in this sample were 0.79 at enrollment, 0.85 at discharge, 0.81 at 2 months, 0.86 at 6 months, and 0.83 at 12 months.
Parental Stress Scale: NICU (PSS: NICU), administered only at study enrollment, measured the degree of stress experienced by mothers from alterations in their parental role during neonatal hospitalization and the appearance and behavior of their child.8 The PSS: NICU asks how stressful the experience has been to date using 28 items on a 5-point scale ranging from “not at all stressful” to “extremely stressful”. Item scores are summed, and higher scores indicate more stress. Cronbach’s alphas in this sample were 0.91 at enrollment for the infant appearance and behavior subscale, and 0.90 for the parental role alteration subscale.
Parental Stress Scale: Prematurely Born Child (PSS: PBC), administered at 2, 6, and 12 months infant age-corrected for prematurity, measured mother’s perception of the stress related to parenting her infant after hospital discharge.8 This scale includes 20 items, such as “getting my baby/child to sleep through the night,” and asks mothers to rate the amount of stress caused by each item on a 5-point scale, ranging from “not at all stressful” to “extremely stressful.” Item scores are summed and range from 20 to 100; higher score indicates higher parental stress. Cronbach’s alphas in this sample were 0.91 at 2 months, 0.91 at 6 months, and 0.90 at 12 months.
The parental stress scales (PSS: NICU, PSS: PBC) used in this study are not measures of parenting behavior or parental interaction, which are beyond the scope of this manuscript. These measures were selected to explore psychological distress related to having a preterm infant.2
2.3.2. Maternal perception of the child
The worry index and the vulnerable child scale were used to measure maternal perceptions of the child. They are not measures of parenting behavior or parental interactions. The Worry Index measured the degree to which a mother worries about her preterm infant in seven areas (e.g., medical problems, rehospitalization, the infant getting enough to eat).24 Worry reflects the mother’s ongoing perception of the child’s risk for problems. Items are rated on a 5-point scale, from “not at all” to “very much.” Cronbach’s alphas in this study were .88 at enrollment, 0.87 at discharge, 0.83 at 2 months, 0.85 at 6 months, and 0.85 at 12 months.
The Vulnerable Child Scale measured the mother’s perception of her toddler’s vulnerability to health problems25 and was administered only at 12 months. Sixteen items using a 4-point scale that ranges from “definitely true” to “definitely false” are then summed. Total scores range from 16 to 64 with lower scores indicating a greater sense of vulnerability. Cronbach’s alpha for this study was 0.80.
2.4. Procedures
The institutional review committees for protection of human subjects for all study sites approved the study. Mothers provided informed consent for their infant’s and their own participation. Mothers completed self-reported questionnaires at enrollment in the hospital, at hospital discharge, and at 2 and 6 months corrected age at home, and at 12 months corrected age at the neonatal follow-up clinic.
2.5. Data Analyses
Inter-correlations among psychological distress scores at enrollment were estimated. Then, each mother was placed in a psychological distress class using latent profile analysis, appropriate when indicators (CESD, STAI, PPQ, and PSS:NICU) are continuous.26 The optimal number of latent profile classes at enrollment was determined by fitting models with varying numbers of classes and varying within-class covariance structures and comparing the Bayesian information criteria (BIC) between models. Latent profile analysis does not assign participants to classes but rather estimates class membership probabilities for each participant. In this study, each mother was placed in the profile class for which she showed the highest probability of membership.
Next, each psychological distress variable was dichotomized based on either published cut-point scores (depressive symptoms, state anxiety, post-traumatic stress symptoms) or median at enrollment where no cut-off scores have been published (both infant appearance and behavior stress and parental role alteration stress).2 The percent of mothers in each class whose scores were elevated (at-or-above the clinical cut-point versus below the clinical cut-point) were calculated.
Then, we tested the relationship between the mother’s class membership at enrollment (independent variable) and each maternal and infant characteristic at enrollment (dependent variable). For categorical variables, we calculated a Chi Square test of independence or for continuous variables, we calculated an F test for an analysis of variance.
We also examined the relationship between the mother’s class membership at enrollment and the predicted trajectories of each longitudinal measure of psychological distress over the first year: depressive symptoms, state anxiety, post-traumatic stress symptoms, and parenting stress. Each psychological distress measure was examined in a separate longitudinal model to see whether the classes continue to differ over time and in what manner.27 The psychological distress measure was the dependent variable, and time and latent class of the mother were the primary independent variables. Intervention group and intervention by time were included as covariates. We did not include recruitment site because previous analyses found that only one psychological distress variable, post-traumatic stress, was affected by site and then only site had only a minor effect.20 Within maternal variation in psychological distress was modeled by including a random intercept and slope component.27 Statistically significant time by class interactions were decomposed by the derivation of the effect of time for each class. None of the mothers were receiving treatment for psychological distress at study enrollment so we did not account for this variable in the analysis.
3. Results
3.1. Correlations of Maternal Psychological Distress Measures
All five measures of maternal psychological distress were significantly correlated (p < .001) with correlation coefficients ranging from 0.43 (infant appearance and behavior stress and state anxiety) to 0.69 (depressive symptoms and state anxiety).
3.2. Maternal Psychological Distress Classes
The mean and standard deviation (SD) of maternal psychological distress scores of the five classes are presented in Table 2; we named the latent classes based on the most salient mean psychological distress scores of mothers assigned to each class.2 The 52 mothers in the low distress class averaged low scores on all measures. The 57 mothers in the moderate distress class averaged moderate scores on all measures. The 78 high NICU-related distress mothers had elevated scores on infant appearance and behavior stress and parental role stress and moderate scores on the other measures. The 20 mothers in the high depressive and anxiety symptom class had elevated scores on depressive symptoms and anxiety, and moderate to low scores on the rest of the measures. The 25 mothers in the extreme distress class had extreme elevated scores on all measures.
Table 2.
Means (SD and % Elevated) Scores on the Five Maternal Distress Measures for the Five Classes at Enrollment
| Low Distress N = 52 Mean (SD) % |
Moderate Distress N = 57 Mean (SD) % |
High NICU Stress N = 78 Mean (SD) % |
High Depr/Anx N = 20 Mean (SD) % |
Extreme Distress N = 25 Mean (SD) % |
|
|---|---|---|---|---|---|
| Depressive Symptoms | 4.1 (2.1) 0% | 13.8 (5.2) 31.6% | 16.9 (8.0) 53.8% | 31.8 (6.5) 100% | 36.6 (7.4) 100% |
| State Anxiety | 27.2 (6.3) 9.6% | 37.8 (7.8) 52.6% | 42.9 (10.6) 67.9% | 54.3 (6.2) 100% | 59.4 (10.2) 100% |
| Post-Traumatic Stress | 1.1 (1.1) 0% | 3.1 (2.0) 12.3% | 5.8 (2.4) 57.7% | 7.7 (1.8) 85% | 9.3 (1.9) 96% |
| Infant Appear. Stress | 21.7 (13.4) 17.3% | 25.5 (9.5) 10.5% | 51.6 (11.2) 93.6% | 30.4 (7.5) 20% | 63.0 (10.7) 100% |
| Parental Role Stress | 20.3 (10.4) 13.5% | 23.8 (10.9) 29.8% | 38.2 (9.1) 80.8% | 29.8 (9.0) 45% | 46.1 (4.9) 100% |
Note: Depr/Anxiety = depressive and anxiety symptom. Appear.= appearance.
3.3. Elevated Maternal Psychological Distress in Each Class
Next we examined the extent to which the five classes displayed elevated scores on each psychological distress measure (Table 2). A mean of 0.4 measures were elevated for the low distress class, 2.5 for the moderate distress class, 3.5 for the high NICU-related distress class, 3.6 for the high depressive and anxiety symptom class, and 4.8 for the extreme distress class. Thus, mothers in the low distress class were unlikely to show elevated scores on any measure and mothers in the extreme distress class showed elevated scores on virtually all measures. The mothers in the other three classes had intermediate scores.
3.4. Class Differences in Maternal and Infant Characteristics at Enrollment
Among maternal characteristics, the classes did not differ statistically on age, marital status, first-time motherhood, or public assistance (Table 3). The low distress class had the second lowest mean educational level, the highest percentage of African American mothers, and lowest amount of worry about their infant. The high depressive and anxiety symptoms and the extreme distress classes had the highest educational levels. The high depressive and anxiety symptom class had the highest percentage of Hispanics and the second highest amount of worry. The extreme distress class had the lowest percentage of African Americans and the greatest worry about their infants.
Table 3.
Class Differences on Maternal and Infant Characteristics and Infant Illness Severity Variables.
| Maternal Characteristics |
Low Distress Mean (SD) (n = 52) |
Moderate Distress Mean (SD) (n = 57) |
Hi NICU Stress Mean (SD) (n = 78) |
High Depr/Anx Mean (SD) (n = 20) |
Extreme Distress Mean (SD) (n = 25) |
|---|---|---|---|---|---|
| Maternal Age | 26.0 (5.5) | 27.6 (5.7) | 27.1 (6.3) | 26.6 (6.2) | 27.8 (7.1) |
| Ethnicity** | |||||
| White, non-Hispanic | 9.6% | 24.6% | 15.4% | 20% | 44% |
| Black, non-Hispanic | 80.8% | 72.9% | 65.4% | 75% | 52% |
| Hispanic | 9.6% | 1.7% | 15.4% | 5% | 4% |
| Other | 0% | 1.7% | 0% | 0% | 3.8% |
| Education in Years* | 12.8 (1.7) | 13.5 (2.3) | 13.9 (2.3) | 12.0 (1.6) | 13.9 (2.6) |
| Marital Status | |||||
| Single | 76.9% | 58.9% | 61.5% | 61.1% | 64% |
| Married | 21.1% | 37.5% | 35.9% | 33.3% | 32% |
| Divorced | 1.9% | 3.6% | 1.3% | 5.6% | 4% |
| Separated | 0% | 0% | 1.3% | 0% | 0% |
| First Time Mothers | 43.1% | 55.8% | 63% | 42.1% | 65.2% |
| Public Assistance | 25% | 24.5% | 17.9% | 15% | 12% |
| Worry About Child*** | 14.8 (5.8) | 17 (6.5) | 23 (6.9) | 22 (7.1) | 28.4 (7.1) |
|
Infant Characteristics |
|||||
| Gestational Age** | 27.5 (3) | 27.4 (2.7) | 27.2 (3) | 27.9 (2.6) | 25.1 (1.9) |
| Multiple Birth | 9.6% | 14.8% | 24.3% | 20% | 24% |
| Percent SGA | 11.76% | 16.7% | 23% | 15% | 16% |
| Intraventricular | 6.6% | 6.6% | 12.3% | 2.2% | 4.8% |
| Hemorrhage | |||||
| Apgar 5*** | 7.8 (1.3) | 7.4 (1.3) | 6.9 (1.6) | 7.8 (1.8) | 5.9 (2.1) |
| Mechanical | 11.5 (18.8) | 11.8 (15.0) | 16.4 (19.8) | 14.9 (20.1) | 39.9 (57.0) |
| Ventilation a*** | |||||
| Percent Infections*** | 1.4 (1.5) | 1.6 (1.3) | 1.7 (1.4) | 1.9 (1.8) | 3.2 (2.2) |
| Percent Surgery*** | 0.4 (1.0) | 0.6 (1.0) | 0.7 (1.2) | 0.4 (0.7) | 1.6 (2.0) |
| Recruitment Site** | |||||
| Midwestern | 53.8% | 61.4% | 37.2% | 60% | 28% |
| Southeastern | 46.1% | 38.5% | 62.8% | 40% | 72% |
Note: Hi NICU Stress= high NICU-related distress. Depr/Anxiety= depressive and anxiety symptom.
Measured in days.
Classes differ, p < .05.
Classes differ, p < .01.
Classes differ, p < .001.
Among infant characteristics, maternal psychological distress classes did not differ statistically on multiple births, small-for-gestational-age, or intraventricular hemorrhage. Infants in the low distress class had the shortest time on mechanical ventilation, and the fewest infections. Infants in the low distress and high depressive and anxiety symptom classes had the highest Apgar scores. Infants in the extreme maternal psychological distress class had the lowest Apgar scores, spent the longest time on mechanical ventilation, had the most infections, and had the highest rate of surgery. Mothers from the Midwestern recruitment sites made up the greatest percentages of the low, moderate, and high depressive and anxiety symptom classes. Southeastern mothers were most common in the other two classes. However, mothers from both states were in each maternal psychological distress class.
3.5. Class Differences in Distress Over Time
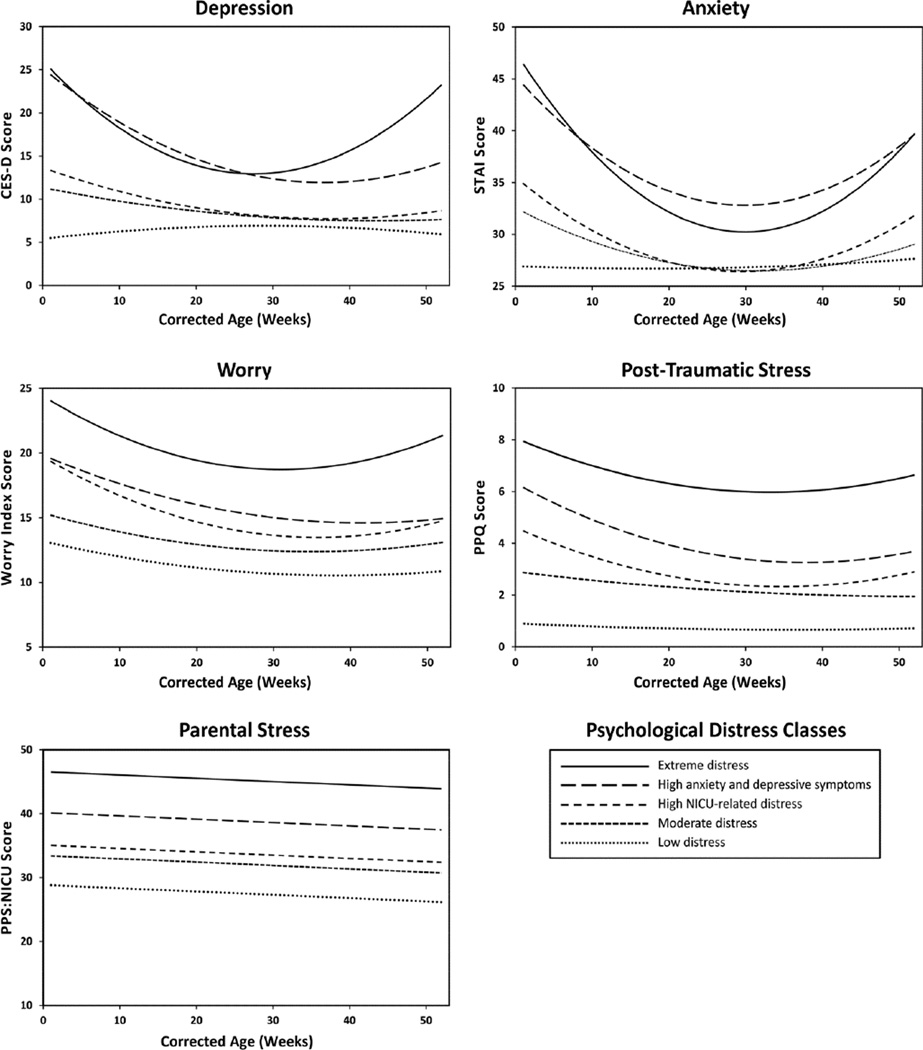
We next examined the longitudinal trajectory of each maternal psychological distress measure. The intervention had no significant effect on the psychological distress measures over time. Except for the parental stress measure for which interactions were not examined because it was only measured at 3 time points, the trajectories of each psychological distress measure over the first 12 months differed by psychological distress class, as reflected in statistically significant parameters for both linear and quadratic components of the age by class interactions. The type III fixed effect for the quadratic components of the age by class interaction were F(4,667) = 19.35, p < .001 for depressive symptoms, F(4,467) = 14.15, p < .001 for anxiety, and F(4,463) = 4.78, p < .001 for post-traumatic stress symptoms. Using the estimated fixed effect parameters yielded by our program (SAS, PROC MIXED), we calculated simple effects28 for age for each class for each psychological distress measure. These are plotted in Figure 1.
Figure 1.
Estimated Simple Effects of Age on Each Distress Measure and Worry for the Five Latent Classes
Estimated class specific trajectories for depressive symptoms and anxiety had similar patterns. The extreme distress and high depressive and anxiety symptom classes had trajectories that differed from those of the other three classes. Because of the differences in estimated quadratic effects of age on depressive symptoms, the extreme distress and high depressive and anxiety symptom class decreased over the first 24–30 weeks post-term then began to increase. The other three classes also decreased over the first 24–30 weeks at which point their trajectories became indistinguishable. Similar differences in the linear and quadratic effects of age were seen in the class-specific trajectories of anxiety.
The class specific effects of time on the post-traumatic stress symptoms indicated five distinct trajectories. However, the quadratic component of these trajectories is much larger for the extreme distress class (.002), the high depressive and anxiety symptom class (.002), and the high NICU-related distress (.002), than for the other two classes (.0002 and .0003).
3.6. Class Differences in Maternal Perceptions of the Child Over Time
Worry about child health decreased over time for all classes (see Figure 1). However, the extreme distress class remained significantly higher than all others and the estimated trajectory appeared to reverse directions more than the other classes. This is reflected in an estimated quadratic coefficient for age that was much larger than that for the other classes. It also had statistically significant age squared by class interaction (F(4,471) = 3.02, p = .01)
Maternal perceptions of child vulnerability were only measured at 12 months and differed significantly between the classes (F(4,284) = 13.99, p < .001). Higher scores on this scale indicated less perception of vulnerability. The mean ranged from 54.4 (SD = 7.0) in the low distress class to 48.1 (SD = 9.1) in the extreme distress class. The moderate distress and high stress classes had means of 51.8 (SD = 5.6) and 51.2 (SD = 6.2), respectively. The high depressive and anxiety symptom class showed a lower mean score 49.0 (SD = 8.7).
4. Discussion
This study showed that five maternal psychological distress measures during neonatal hospitalization of preterm infants (depressive symptoms, state anxiety, post-traumatic stress symptoms, stress due to the infant appearance and behavior, and stress due to parental role alterations) were significantly interrelated. Mothers were grouped into five latent classes (low distress, moderate distress, high stress, high depressive and anxiety symptom class and extreme distress) according to their differing degrees and types of psychological distress. Class membership, as determined at enrollment in the NICU, continued to be related to the trajectories of each psychological distress measure through one-year corrected for prematurity. The mothers in the extreme distress class and, to a lesser degree, the high depressive and anxiety symptom class, remained at risk of significant psychological distress one year after discharge and also had less positive perceptions of the infants as evidenced by elevated worry scores and high perceptions of child vulnerability. This study replicated findings of an earlier study that psychological distress patterns identified in NICU could predict maternal psychological distress for at least a year.2
Our findings of five psychological distress classes were similar to the four class solution found in the previous study with 177 African Americans from a Southeastern state, in which the authors created psychological distress classes based on the composite of depressive symptoms, state anxiety, post-traumatic stress, infant appearance and behavior stress, stress related to parental role alteration in the NICU, and daily hassles.2 Both studies had a low distress class, an extreme distress class, and two intermediate classes–one high on NICU-related distress and one high on anxiety and depressive symptoms. The fifth class in the current study had moderate scores on all measures and appeared to be intermediate between the low distress and the high stress classes. In both studies, the trajectory of the classes showed significant decline in symptoms over time except for the low distress class, which already had low scores. However, in the current study, most of the trajectories of the extreme distress classes showed declines in symptoms over the first six months postpartum but then increases in these symptoms. This finding may suggest that mothers in this class might be at higher risk for chronic psychological distress. Thus, healthcare professionals should assess mothers’ psychological distress over time and support them on their psychological response that may continue to be relevant at least throughout the first year postpartum. This study shows that mothers’ risk for ongoing psychological distress can be predicted during the infant’s neonatal hospitalization.
The present study and the earlier one of African Americans differed in the distribution of the total sample across classes: 32% of the original sample was in the low distress class versus 47% of our current sample in the low and moderate distress classes, and 41% of the African American sample was in either the extreme distress or high depressive and anxiety symptom class as compared to only 20% of our current sample.2 These sample distribution differences might be related to site differences, specifically the inclusion of the Midwestern sites in the current study. The African American study was conducted in the same Southeastern state as the present study but the infants were recruited from different hospitals than the infants in the current study.2 We have previously reported that the Midwestern mothers in the current sample were more likely to be younger, African American or Hispanic, unmarried, and on public assistance than Southeastern mothers.20 Our Southeastern sample was more diverse in race and socioeconomic status than the Midwestern sample, which was recruited from an inner city population living in poverty.20
Researchers have suggested that differences in mothers’ depressive symptoms are not the function of specific racial or ethnic group membership but a reflection of sociodemographic risk and family support.29 Researchers also argue that the lack of social support and distressful social context can have an impact on depressive symptoms among low income and ethnic minority women.30 Therefore, it is possible that the mothers living in inner city poverty experienced so much chronic stress in their lives that the addition of a critically ill preterm infant did not greatly increase their psychological distress. However, because ethnic differences in our study were confounded by study site differences, additional research is needed to determine how maternal psychological distress is related to ethnic group and geographic location.
Race and clinical factors were noteworthy in the most and least distressed classes. For example, the extreme distress class had the lowest percentage of African Americans and the greatest worry about their infants. Infants in the extreme distress class had the most problems in the NICU with the longest time on mechanical ventilation, most infections, and highest rate of surgery. This class most commonly came from the Southeastern state sites, which were diverse in race and socioeconomic status and less exposed to inner city poverty than the Midwestern mothers.20 Also, Southeastern infants were smaller and sicker than Midwestern infants because one Southeastern hospital was a children’s hospital that was a referral center for surgery.20 By contrast, mothers in the low distress class, who were more likely to be Midwestern, had the lowest mean educational level, were more likely to be African American, and had lowest amount of worry about their infant.20 Their infants were the healthiest, with the highest Apgar scores, the shortest time on mechanical ventilation, and fewest infections.
Our findings suggest that mothers in the high depressive and anxiety symptom class and the extreme distress class had the sickest infants. A recent meta-analysis showed that parents report more stress for infants with lower gestational ages and lower birth weights. 5 However, the authors argue that prematurity can best be regarded as one of the possible complications of birth, and not as a source of stress in itself.5 A limitation of this meta-analysis was that the authors considered the outcomes of only two stress questionnaires: Parenting Stress Index (PSI Short Form), and the PSS: NICU, which are administered at different time points. Another study showed that parenting stress in mothers of preterm infants was significantly greater than stress in mothers of term infants at one year of age.31 Maternal stress during hospitalization and worry about the infant’s health and development were significantly related to maternal depressive symptoms over time.6 As our findings show that the psychological distress measures are interrelated, it is clinically important to do a thorough assessment of maternal psychological distress during neonatal hospitalization.
Several factors may limit the generalizability of this study. First, mothers in this study participated in a randomized controlled trial testing two maternally administered interventions for preterm infants on infant health and development, maternal psychological well-being, and the maternal-infant relationship.20 However, the interventions were unlikely to influence the mother’s psychological distress class because the classes were defined using the scores at the study enrollment before the intervention began. Second, we did not have data to inform whether psychological distress symptoms were present before study enrollment, but mothers with a diagnosis of psychosis or bipolar diagnosis or taking anti-depressants at enrollment were excluded from the study. Identifying sub-groups of mothers experiencing similar patterns of psychological distress will serve to improve clinical detection and treatment of these symptoms in the postpartum period. Third, ethnic differences were likely confounded by study site differences. However, this limitation was somewhat off-set because the multi-site nature of our study increased the potential generalizability of our findings. Additional research is needed to determine how maternal psychological distress is related to ethnic group and geographic location. Fourth, this study only followed the mothers for one year postpartum. Previous research has shown that class membership may have effects for more than two years postpartum.2 Additional research exploring the relationship between psychological distress class and parent-infant interactions and infant outcomes would provide better information on the utility of these classes to target interventions. Despite these limitations, the identification of similar latent classes of maternal psychological distress across multiple studies suggests that psychological distress is an important clinical phenomenon that needs to be further explored to illuminate the need for intervention that help decrease maternal psychological distress over time with routine support.
In conclusion, our findings identified the existence of distinct sub-groups of mothers exhibiting different trajectories of maternal psychological distress in a multi-ethnic group of mothers of preterm infants. This suggests that there may be a need for different interventions for different sub-groups of mothers in the NICU. These sub-groups cannot be identified purely based on maternal or infant characteristics. Therefore, mothers need to be assessed for their patterns of psychological distress, which can be used to predict their psychological distress response over time, and in turn their perception of the child and parenting stress. This information should be of great value to help define need for interventions to ameliorate maternal psychological distress and parenting response of mothers of preterm infants.
Highlights.
Mothers of preterm infants often experience marked psychological distress over time
Sub-groups of mothers experience distinctive patterns of psychological distress
Mothers’ risk for ongoing distress can be predicted during infant’s hospitalization
Acknowledgements
This research was funded by R01 NR009418 from the National Institute for Nursing Research, NIH and the Harris Foundation. The authors wish to thank Donna Ryan, Paula Anderson, Paula Anderson, Anna Arens, Jada Brooks, Emily Chin, Kristy Coe, Lindsey Garfield, Donna Harris, Francia Marin, Sarah Pelizzari, Nancy Peters, Shana Salik, Julia Shannon and Teresa Shaw for technical assistance and John Boling for statistical consultation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.WHO. Born too soon: The global action report on preterm birth. Geneva: 2012. [Google Scholar]
- 2.Holditch-Davis D, Miles MS, Weaver MA, et al. Patterns of distress in African-American mothers of preterm infants. J Dev Behav Pediatr. 2009;30(3):193–205. doi: 10.1097/DBP.0b013e3181a7ee53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singer LT, Salvator A, Guo S, Collin M, Lilien L, Baley J. Maternal psychological distress and parenting stress after the birth of a very low-birth-weight infant. JAMA. 1999;281(9):799–805. doi: 10.1001/jama.281.9.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jubinville J, Newburn-Cook C, Hegadoren K, Lacaze-Masmonteil T. Symptoms of acute stress disorder in mothers of premature infants. Adv Neonatal Care. 2012;12(4):246–253. doi: 10.1097/ANC.0b013e31826090ac. [DOI] [PubMed] [Google Scholar]
- 5.Schappin R, Wijnroks L, Uniken Venema MM, Jongmans MJ. Rethinking stress in parents of preterm infants: a meta-analysis. PLoS One. 2013;8(2):e54992. doi: 10.1371/journal.pone.0054992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miles MS, Holditch-Davis D, Schwartz TA, Scher M. Depressive symptoms in mothers of prematurely born infants. J Dev Behav Pediatr. 2007;28(1):36–44. doi: 10.1097/01.DBP.0000257517.52459.7a. [DOI] [PubMed] [Google Scholar]
- 7.Smith S. Physiologic stability of intubated VLBW infants during skin-to-skin care and incubator care. Advances in Neonatal Care. 2001;1(1):28–40. [Google Scholar]
- 8.Miles MS, Funk SG, Carlson J. Parental Stressor Scale: neonatal intensive care unit. Nurs Res. 1993;42(3):148–152. [PubMed] [Google Scholar]
- 9.Miles MS, Funk SG, Kasper MA. The stress response of mothers and fathers of preterm infants. Res Nurs Health. 1992;15(4):261–269. doi: 10.1002/nur.4770150405. [DOI] [PubMed] [Google Scholar]
- 10.Davis L, Edwards H, Mohay H, Wollin J. The impact of very premature birth on the psychological health of mothers. Early Hum Dev. 2003;73(1–2):61–70. doi: 10.1016/s0378-3782(03)00073-2. [DOI] [PubMed] [Google Scholar]
- 11.Mew AM, Holditch-Davis D, Belyea M, Miles MS, Fishel A. Correlates of depressive symptoms in mothers of preterm infants. Neonatal Netw. 2003;22(5):51–60. doi: 10.1891/0730-0832.22.5.51. [DOI] [PubMed] [Google Scholar]
- 12.Zelkowitz P, Bardin C, Papageorgiou A. Anxiety affects the relationship between parents and their very low birth weight infants. Infant Mental Health Journal. 2007;28(3):296–313. doi: 10.1002/imhj.20137. [DOI] [PubMed] [Google Scholar]
- 13.Shaw RJ, Lilo EA, Storfer-Isser A, et al. Screening for symptoms of postpartum traumatic stress in a sample of mothers with preterm infants. Issues Ment Health Nurs. 2014;35(3):198–207. doi: 10.3109/01612840.2013.853332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rogers CE, Kidokoro H, Wallendorf M, Inder TE. Identifying mothers of very preterm infants at-risk for postpartum depression and anxiety before discharge. J Perinatol. 2013;33(3):171–176. doi: 10.1038/jp.2012.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beck CT. Recognizing and screening for postpartum depression in mothers of NICU infants. Adv Neonatal Care. 2003;3(1):37–46. doi: 10.1053/adnc.2003.50013. [DOI] [PubMed] [Google Scholar]
- 16.Northrup TF, Evans PW, Stotts AL. Depression among mothers of high-risk infants discharged from a neonatal intensive care unit. MCN Am J Matern Child Nurs. 2013;38(2):89–94. doi: 10.1097/NMC.0b013e318270f8b8. [DOI] [PubMed] [Google Scholar]
- 17.DeMier RL, Hynan MT, Harris HB, Manniello RL. Perinatal stressors as predictors of symptoms of posttraumatic stress in mothers of infants at high risk. J Perinatol. 1996;16(4):276–280. [PubMed] [Google Scholar]
- 18.Chronicity of maternal depressive symptoms, maternal sensitivity, and child functioning at 36 months. NICHD Early Child Care Research Network. Dev Psychol. 1999;35(5):1297–1310. doi: 10.1037//0012-1649.35.5.1297. [DOI] [PubMed] [Google Scholar]
- 19.White-Traut R, Wink T, Minehart T, Holditch-Davis D. Frequency of Premature Infant Engagement and Disengagement Behaviors During Two Maternally Administered Interventions. Newborn Infant Nurs Rev. 2012;12(3):124–131. doi: 10.1053/j.nainr.2012.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holditch-Davis D, White-Traut RC, Levy JA, O’Shea TM, Geraldo V, David RJ. Maternally administered interventions for preterm infants in the NICU: Effects on maternal psychological distress and mother-infant relationship. Infant Behav Dev. 2014;37(4):695–710. doi: 10.1016/j.infbeh.2014.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Radloff LS. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- 22.Roberts RE, Vernon SW. The Center for Epidemiologic Studies Depression Scale: its use in a community sample. Am J Psychiatry. 1983;140(1):41–46. doi: 10.1176/ajp.140.1.41. [DOI] [PubMed] [Google Scholar]
- 23.Spielberger C. Manual for the State-Trait Anxiety Inventory. Palo Alto: Consulting Psychologists Press; 1983. [Google Scholar]
- 24.Miles MS, Holditch-Davis D. Compensatory parenting: how mothers describe parenting their 3-year-old, prematurely born children. J Pediatr Nurs. 1995;10(4):243–253. doi: 10.1016/s0882-5963(05)80021-1. [DOI] [PubMed] [Google Scholar]
- 25.Perrin EC, West PD, Culley BS. Is my child normal yet? Correlates of vulnerability. Pediatrics. 1989;83(3):355–363. [PubMed] [Google Scholar]
- 26.Muthén BO. Beyond SEM: General latent variable modeling. Behaviormetrika. 2002;29:81–117. [Google Scholar]
- 27.Diggle PPH, Liang K-Y, Zeger S. Analysis of Longitudinal Data. Second ed. Oxford University Press; 2002. [Google Scholar]
- 28.Aiken L, West S. Multiple Regression: Testing and interpreting interactions. Thousand Oaks, California: Sage Publications; 1991. [Google Scholar]
- 29.Poehlmann J, Schwichtenberg AJ, Bolt D, Dilworth-Bart J. Predictors of depressive symptom trajectories in mothers of preterm or low birth weight infants. J Fam Psychol. 2009;23(5):690–704. doi: 10.1037/a0016117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McGrath E, Keita GP, Strickland BR, Russo NF. Women and depression: Risk factors and treatment issues: Final report of the American Psychological Association’s National Task Force on Women and Depression. Washigton, DC: American Psychological Association; 1990. [Google Scholar]
- 31.Gray PH, Edwards DM, O’Callaghan MJ, Cuskelly M, Gibbons K. Parenting stress in mothers of very preterm infants -- influence of development, temperament and maternal depression. Early Hum Dev. 2013;89(9):625–629. doi: 10.1016/j.earlhumdev.2013.04.005. [DOI] [PubMed] [Google Scholar]