Abstract
Cleidocranial dysplasia (CCD), an autosomal dominant disorder with a prevalence of 1 in 1 000 000 individuals, presents with a wide range of variability. Dentists are often the first to encounter patients with CCD, some of whom do not show typical manifestations. Since it has similar features to other pathologies, CCD is misdiagnosed as other conditions. A 10-year-old boy suffering from CCD was misdiagnosed as having rickets and was referred for non-eruption of a few permanent teeth along with an unaesthetic facial appearance. Clinically and radiologically, a diagnosis of CCD was made. Currently, management of this patient's orofacial manifestations is underway.
Background
Cleidocranial dysplasia (CCD) is an inherited skeletal dysplasia with characteristic clinical findings in which the skull, clavicles and dentition are primarily affected. This autosomal dominant disease has been reported to be caused by mutations in the RUNX2 gene (the gene required for osteoblastic differentiation) on chromosome 6p21.1 2 More recently, a frame-shift mutation of 884delC corresponding to the cDNA sequence was found in exon five of the CBFA1/RUNX2 gene in a Chinese family.3 Skeletal, dental and other features of CCD include a brachycephalic skull, widely open calvarial sutures, frontal and occipital bossing, clavicular aplasia/hypoplasia, wormian bones, delayed ossification of pelvic bones and distal phalanges, bell-shaped thorax, short stature, hypertelorism, hearing loss, recurrent mid-ear infections, supernumerary teeth, narrow high arched palate and prolonged retention of primary dentition/delayed eruption of permanent dentition. The adverse general health effects of CCD are not very severe and there is no associated impairment in cognitive or intellectual functioning in those affected.4 The variety of dental problems leads to crowding and malocclusion, which makes dental management an important aspect of the healthcare of affected people.5 We report a case of a 10-year-old boy who was referred for non-eruption of a few permanent teeth along with an unaesthetic facial appearance. Clinically and radiologically, a diagnosis of CCD was performed.
Case presentation
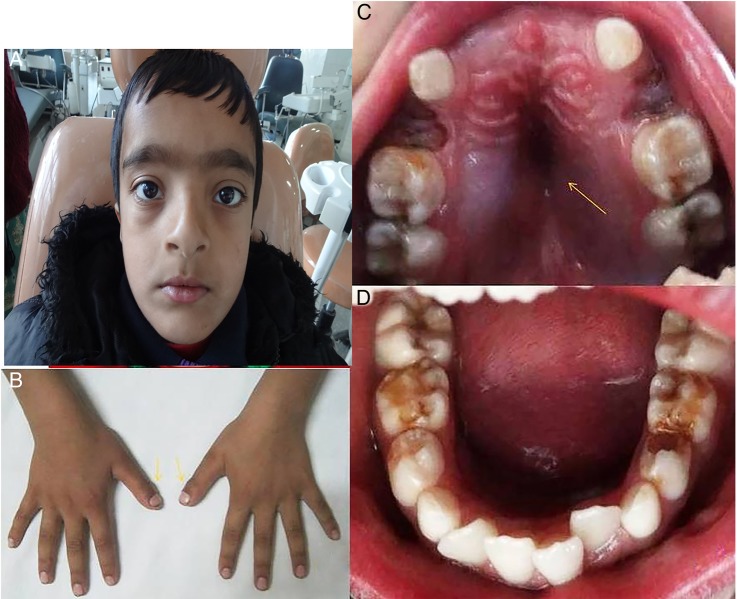
A 10-year-old boy diagnosed with rickets was referred to our dental department for non-eruption of a few permanent teeth and an ensuing unaesthetic facial appearance. He had no history of trauma to the facial region. Family history and examination revealed the presence of a similar condition in the patient's father, however, no other family members were affected. The patient had a short stature. He was well oriented, with an unimpaired intellect. His hand examination showed abnormalities including brachydactyly, tapering fingers and short, broad thumbs; his hearing was normal and he had no history of mid-ear infections. Extraoral examination revealed frontal bossing with a brachycephalic skull, hypertelorism, depressed and flattened nasal bridge, and a deficient mid-face. Intraoral examination showed unerupted maxillary permanent incisors, a narrow maxillary arch with high arched palate and multiple decayed teeth. The mandibular anterior teeth showed crowding (figure 1A–D).
Figure 1.
(A) Broad head, frontal depression on the forehead, hypertelorism, broad and flat nasal bridge. (B) brachydactyly, tapering fingers and broad thumbs. (C) High arched palate and tooth size—arch size discrepancy. (D) Occlusal view of mandible.
Provisional diagnosis
The diagnosis was CCD.
Differential diagnosis
Rickets, pyknodysostosis, mandibuloacral dysplasia (MAD), Yunis Varon syndrome.
Investigations
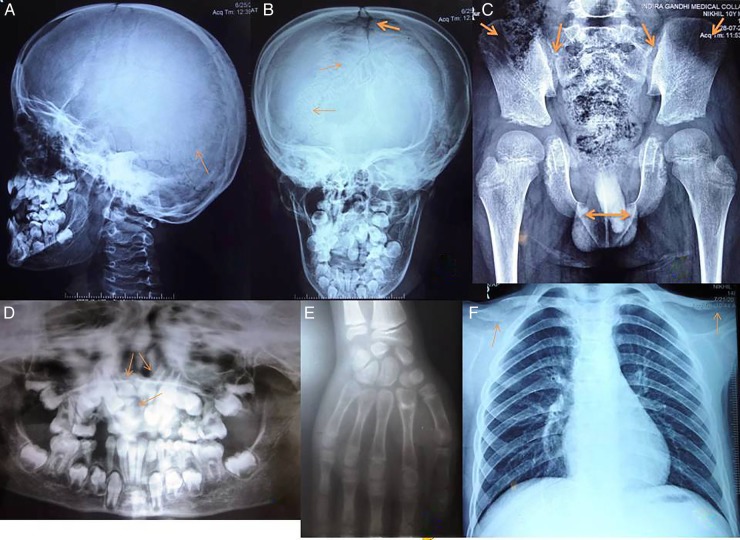
Radiographic investigations were carried out and showed open skull sutures, a number of wormian bones present between sutures, hypoplastic bilateral acromial ends of the clavicles, malunion of an old fracture of the acromial end of the right clavicle, hypoplastic phalanges of the hand, hypoplastic iliac wings, a wide sacroiliac joint and pubic symphysis, impacted maxillary permanent incisors with presence of twin tooth-like structures in the vicinity and delayed root formation of permanent teeth (figure 2).
Figure 2.
Radiographic examination: (A and B) Broad sagittal and metopic sutures and Wormian bones between sutures. (C) Hypoplastic iliac wings and wide sacroiliac joint and pubic symphysis. (D) Impacted 11, 21 and retarded root formation of permanent teeth. (E) Hypoplastic phalanges. (F) Hypoplastic clavicles (acromial ends) and bell-shaped rib cage.
Further biochemical tests were advised, including a thyroid function test, and checking of serum calcium, serum phosphate and serum alkaline phosphatase levels; all were found to be within normal range.
Confirmatory diagnosis
Based on the findings, a diagnosis of CCD was performed.
Treatment and follow-up
The non-eruption of permanent maxillary central incisors was addressed first. A full thickness mucoperiosteal flap was raised in the region and the two tooth-like structures were removed and sutures placed (figure 3). The extracted tooth-like structures were later diagnosed histopathologically as compound odontomes. The decayed teeth were restored and the patient was kept under regular follow-up to evaluate the eruption of permanent teeth. Treatment with calcium and vitamin D supplementation was started as bone density was assessed to be below normal, and also because preventive treatment for osteoporosis should be initiated at a young age. Multidisciplinary treatment with dental and medical intervention is presently proceeding (figure 4).
Figure 3.
(A–C) Raised mucoperiosteal flap and extraction of two compound odontomes followed with placement of 3–0 silk sutures. (D and E) Compound odontomes. (F) One month postoperative photograph.
Figure 4.
Multidisciplinary treatment to restore proper aesthetics and function.
Discussion
CCD, an autosomal dominant disorder with a prevalence of 1 in 1 000 000 individuals, presents with a wide range of variability.6 The disease gene has been mapped to chromosome 6p21 within a region containing core-binding factor subunit α-1, a member of the runt family of transcription factors—runt-related transcription factor 2 (RUNX2)7—which is essential for osteoblasts and odontoblasts differentiation as well as for bone and tooth formation. Molecular genetic testing of RUNX2 detects mutations in 60%–70% of individuals with a clinical diagnosis of CCD.8
Several pathologies closely mimic cleidocranial dysplasia clinically, causing even an astute physician to initially wrongly diagnosis it. Below are descriptions of these conditions/pathologies mentioned along with their differentiating features:
Rickets—Vitamin D resistant rickets share common clinical features with CCD, such as short stature, brachycephaly and delayed eruption of teeth. In the present case, the physician initially misdiagnosed the patient as having rickets, because of the features mentioned above; however, a careful evaluation proved otherwise. Table 1 summarises several differentiating features from CCD.
Pyknodysostosis is a clinical condition similar to CCD; it exhibits calvarial and clavicular changes but can be differentiated by absence of supernumerary teeth and increased bone density on roentgenographic film, in contrast to CCD (Maroteaux and Lamy, 1962).
MAD is an autosomal recessive disorder and can be differentiated from CCD by progressive stiffening of joints and acro-osteodysplasia of the fingers and toes, with delayed ossification of the carpal bones on radiographs (Novelli et al, 2002).
Yunis Varon syndrome can be differentiated by absence of a distal phalanx of the great toe, poorly delineated lips and fewer pronounced dental findings.
Other syndromes that share similar clinical features are osteopetrosis, Paget's disease, CDAGS syndrome, Crane-Heise syndrome, hypophosphatasia and Holt-Oram syndrome or TAR syndrome.
Table 1.
Factors that differentiate cleidocranial dysplasia from rickets
| Cleidocranial dysplasia | Vitamin D resistant rickets | |
|---|---|---|
| Family history | Usually an autosomal dominant linkage | Usually sex-linked dominant linkage |
| Dental findings |
|
|
| Radiographic findings |
|
|
| Histological findings | Normal structure of enamel, dentin and bone |
|
| Laboratory findings | Normal levels of calcium, phosphorous and vitamin D |
|
Dentists are often the first to encounter patients with CCD, some of whom do not show typical manifestations. The main features of CCD include a short stature, clavicular hypoplasia/aplasia, open sutures and fontanelle, frontal and parietal bossing, supernumerary teeth and open pubic symphysis. There are four reported types of CCD: the first has typical clinical manifestations and a history of heredity; the second has typical clinical manifestations without a history of heredity; the third has atypical clinical manifestations and a history of heredity; the fourth has neither typical clinical manifestations nor a history of heredity.9 10 The fourth type of CCD is relatively difficult to diagnose only on the basis of clinical and radiographic findings.
The typical bilateral absence of clavicles is only observed in 10% of cases of CCD; whereas hypoplastic acromial ends of the clavicle are more commonly seen,11 12 as was noticed in the present case. The widened pubic symphysis and sacroiliac joint, as was seen in this case, are due to delayed ossification. The combination of frontal bossing and open metopic sutures results in an apparent deformity in the calvaria. If the cranial vault defect is significant, the head should be protected from blunt trauma; helmets may be advised for high-risk activities. In these cases, evaluation by a craniofacial surgeon and rehabilitation services are indicated.8 The conservative cranioplasty technique can be performed for the reduction of the frontal bossing and subsequent filling of the metopic suture defect with autogenous bone chips.13
Individuals with CCD have abnormalities in the orofacial complex in the form of a deficient mid-face, underdeveloped paranasal sinuses, high arched palate, delayed eruption of teeth and supernumerary teeth. Up to 94% of people with CCD have dental findings including supernumerary teeth (70%) and eruption failure of permanent teeth.14–16 In addition to RUNX2 mutation, other non-genetic factors, such as those of an epigenetic origin, modifier genes, copy number variations and environmental factors are believed to be involved in the formation of supernumerary teeth in CCD.17–19 Delayed eruption of teeth is seen due to a less but not entirely absent eruptive potential.20 The various factors involved in delayed tooth eruption in CCD are supernumerary teeth, lack of cellular cementum, lack of appropriate inflammatory response, an inadequate expression of some cytokines, increased bone density impeding resorption and underlying defects in bone.21 These orodental features are in accordance with the findings in our case, except for the presence of supernumerary teeth. Presence of odontomes along with CCD has not been reported earlier. Early diagnosis is crucial for the timely commencement of appropriate treatment.22 Treatment of patients with CCD requires an interdisciplinary approach and collaboration among specialists, the patient and the patient's family,22 with the goal of improving appearance and providing a functioning masticatory mechanism. Presently, orthodontic and orthopaedic management is being undertaken for this patient.
Conclusion
Family history and dental, radiographic, laboratory and histological findings, are valuable tools for differentiating CCD from vitamin D-resistant rickets.
Learning points.
Cleidocranial dysplasia mimics other conditions based on clinical features; investigations help in accurately diagnosing the condition.
Early diagnosis is of paramount importance in decreasing skeletal and dental morbidity.
A multidisciplinary approach is required in treating the condition.
Footnotes
Contributors: Cleidocranial dysplasia syndrome (CCD) with unusual finding in a young patient—A Case Report Contributors. PS, AS, CJ, AB, We certify that we have participated sufficiently in the intellectual content, conception and design of this work or the analysis and interpretation of the data (when applicable), as well as the writing of the manuscript, to take public responsibility for it and have agreed to have our names listed as contributors. We believe the manuscript represents valid work. Neither this manuscript nor one with substantially similar content under our authorship has been published or is being considered for publication elsewhere, except as described in the covering letter. We certify that all the data collected during the study are presented in this manuscript and no data from the study have been or will be published separately. We attest that, if requested by the editors, we will provide the data/information or will cooperate fully in obtaining and providing the data/information on which the manuscript is based, for examination by the editors or their assignees. Financial interests, direct or indirect, that exist or may be perceived to exist for individual contributors in connection with the content of this paper have been disclosed in the cover letter. Sources of outside support of the project are named in the cover letter. We hereby transfer, assign, or otherwise convey all copyright ownership, including any and all rights incidental thereto, exclusively to the BMJ CASE REPORTS, in the event that such work is published by the BMJ CASE REPORTS. The Indian Journal of Dental Science shall own the work, including (1) copyright; (2) the right to grant permission to republish the article in whole or in part, with or without fee; (3) the right to produce preprints or reprints and translate into languages other than English for sale or free distribution; and (4) the right to republish the work in a collection of articles in any other mechanical or electronic format. We give the rights to the corresponding author to make necessary changes as per the request of the journal, to carry out the rest of the correspondence on our behalf and, he/she will act as the guarantor for the manuscript on our behalf. All persons who have made substantial contributions to the work reported in the manuscript, but who are not authors, are named in the Acknowledgment and have given us their written permission to be named. If we do not include an Acknowledgment, that means we have not received substantial contributions from non-authors and no author has been omitted.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Mundlos S, Otto F, Mundlos C et al. Mutations involving the transcription factor CBFA1 cause cleidocranial dysplasia. Cell 1997;89:773–9. 10.1016/S0092-8674(00)80260-3 [DOI] [PubMed] [Google Scholar]
- 2.Otto F, Thornell AP, Crompton T et al. CBFA1, a candidate gene for cleidocranial dysplasia syndrome, is essential for osteoblast differentiation and bone development. Cell 1997;89:765–71. 10.1016/S0092-8674(00)80259-7 [DOI] [PubMed] [Google Scholar]
- 3.Wang S, Zhang S, Wang Y et al. Cleidocranial dysplasia syndrome: clinical characteristics and mutation study of a Chinese family. Int J Clin Exp Med 2013;6:900–7. [PMC free article] [PubMed] [Google Scholar]
- 4.Cooper SC, Flaitz CM, Johnston DA et al. A natural history of cleidocranial dysplasia. Am J Med Genet 2001;104:1–6. 10.1002/ajmg.10024 [DOI] [PubMed] [Google Scholar]
- 5.Roberts T, Stephen L, Beighton P. Cleidocranial dysplasia: a review of the dental, historical, and practical implications with an overview of the South African experience. Oral Surg Oral Med Oral Pathol Oral Radiol 2013; 115:46–55. 10.1016/j.oooo.2012.07.435 [DOI] [PubMed] [Google Scholar]
- 6.Mundlos S. Cleidocranial dysplasia: clinical and molecular genetics. J Med Genet 1999;36:177–82. [PMC free article] [PubMed] [Google Scholar]
- 7.Yoshida T, Kanegane H, Osato M et al. Functional analysis of RUNX2 mutations in Japanese patients with cleidocranial dysplasia demonstrates novel genotype-phenotype correlations. Am J Hum Genet 2002;71:724–38. 10.1086/342717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mendoza-Londono R, Lee B. Cleidocranial Dysplasia. In: Pagon RA, Adam MP, Ardinger HH et al. eds GeneReviews®. Seattle, WA: University of Washington, Seattle, 1993–2014. 2006 Jan 3 (Updated 2013 August 29). [PubMed] [Google Scholar]
- 9.Chitayat D, Hodgkinson KA, Azouz EM. Intrafamilial variability in cleidocranial dysplasia: a three generation family. Am J Med Genet 1992;42:298–303. 10.1002/ajmg.1320420307 [DOI] [PubMed] [Google Scholar]
- 10.Zhou G, Chen Y, Zhou L et al. CBFA1 mutation analysis and functional correlation with phenotypic variability in cleidocranial dysplasia. Hum Mol Genet 1999;8:2311–16. 10.1093/hmg/8.12.2311 [DOI] [PubMed] [Google Scholar]
- 11.Mehta DN, Vachhani RV, Patel MB. Cleidocranial dysplasia: a report of two cases. J Indian Soc Pedod Prev Dent 2011;29:251–4. 10.4103/0970-4388.85836 [DOI] [PubMed] [Google Scholar]
- 12.Karagüzel G, Aktürk FA, Okur E et al. Cleidocranial dysplasia: a case report. J Clin Res Pediatr Endocrinol 2010;2:134–6. 10.4274/jcrpe.v2i3.134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McGuire TP, Gomes PP, Lam DK et al. Cranioplasty for midline metopic suture defects in adults with cleidocranial dysplasia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;103:175–9. 10.1016/j.tripleo.2006.02.014 [DOI] [PubMed] [Google Scholar]
- 14.Bufalino A, Paranaíba LM, Gouvêa AF et al. Cleidocranial dysplasia: oral features and genetic analysis of 11 patients. Oral Dis 2012;18:184–90. 10.1111/j.1601-0825.2011.01862.x [DOI] [PubMed] [Google Scholar]
- 15.Golan I, Baumert U, Hrala BP et al. Dentomaxillofacial variability of cleidocranial dysplasia: clinicoradiological presentation and systematic review. Dentomaxillofac Radiol 2003;32:347–54. 10.1259/dmfr/63490079 [DOI] [PubMed] [Google Scholar]
- 16.Golan I, Baumert U, Hrala BP et al. Early craniofacial signs of cleidocranial dysplasia. Int J Paediatr Dent 2004;14:49–53. 10.1111/j.1365-263X.2004.00501.x [DOI] [PubMed] [Google Scholar]
- 17.Ryoo HM, Kang HY, Lee SK et al. RUNX2 mutations in cleidocranial dysplasia patients. Oral Dis 2010;16:55–60. 10.1111/j.1601-0825.2009.01623.x [DOI] [PubMed] [Google Scholar]
- 18.Suda N, Hamada T, Hattori M et al. Diversity of supernumerary tooth formation in siblings with cleidocranial dysplasia having identical mutation in RUNX2: Possible involvement of non-genetic or epigenetic regulation. Orthod Craniofac Res 2007;10:222–5. 10.1111/j.1601-6343.2007.00404.x [DOI] [PubMed] [Google Scholar]
- 19.Suda N, Hattori M, Kosaki K et al. Correlation between genotype and supernumerary tooth formation in cleidocranial dysplasia. Orthod Craniofac Res 2010;13:197–202. 10.1111/j.1601-6343.2010.01495.x [DOI] [PubMed] [Google Scholar]
- 20.Jensen BL, Kreiborg S. Development of the dentition in cleidocranial dysplasia. J Oral Pathol Med 1990;19:89–93. 10.1111/j.1600-0714.1990.tb00803.x [DOI] [PubMed] [Google Scholar]
- 21.Suri L, Gagari E, Vastardis H. Delayed tooth eruption: Pathogenesis, diagnosis, and treatment. A literature review. Am J Orthod Dentofacial Orthop 2004;126:432–45. 10.1016/j.ajodo.2003.10.031 [DOI] [PubMed] [Google Scholar]
- 22.Gömleksiz C, Arslan E, Arslan S et al. Delayed diagnosis of cleidocranial dysplasia in an adult: A case report. Acta Medica Academica 2014;43:92–6. 10.5644/ama2006-124.106 [DOI] [PubMed] [Google Scholar]