Abstract
Abdominal pain in a teenage girl is common; however, thorough history and examination can often distinguish a more rare or sinister diagnosis. We present a case of a 15-year-old girl presenting with abdominal pain, who was subsequently diagnosed with double intussusception secondary to her previously unrecognised Peutz-Jeghers syndrome (PJS).
Background
This case demonstrates an unusual surgical emergency, with a rare syndrome underlying the presentation itself. The report emphasises the importance of thorough history taking and examination as the clues to a diagnosis may be subtle.
Case presentation
A 15-year-old girl presented to the emergency department of a district general hospital, with a 5-day history of abdominal pain. This pain was described as intermittent and cramping, and had been worsening in severity since its onset. She reported having had similar pain in the past few years, however, this had always resolved without intervention. On the day of presentation, she reported two episodes of bilious vomiting, and had absolute constipation, with bowels last open 2 days previously. She denied urinary symptoms, and was currently menstruating. The medical history was significant for dysmenorrhoea and menorrhagia, for which she had been taking mefenamic acid and buscopan. She also had been investigated for non-epileptiform complex partial seizures as a child; these had since resolved.
Investigations
On presenting examination, the patient appeared dehydrated, with tachycardia of 121 bpm and tachypnoea of 28 breaths/min, blood pressure was stable at 113/67 mm Hg and oxygen saturations were 100% on room air. Examination revealed a distended but soft abdomen with tenderness around the umbilicus. Omeprazole and paracetamol were administered in the emergency department and intravenous fluid resuscitation was started. Bloods revealed C reactive protein of 156 mg/L but a white cell count within normal limits. There was no anaemia and biochemistry was normal. Abdominal X-ray (figure 1) demonstrated numerous central dilated loops of bowel. On a working diagnosis of small bowel obstruction, an nasogastric tube was sited. A CT scan was organised for the following morning (figure 2). This demonstrated apparent telescoping of the bowel within a distal segment at two separate sites, one in the upper left quadrant and another in the pelvis. The patient was discussed with a children's tertiary referral hospital and an urgent transfer was arranged.
Figure 1.

Plain abdominal radiograph.
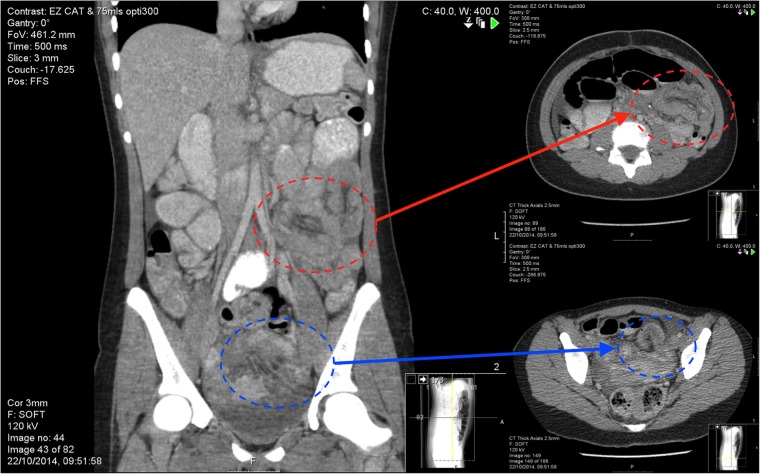
Figure 2.
Coronal section CT scan clearly identifying two intussusceptions—also shown in transverse section.
Differential diagnosis
In a patient with double-site intussusception, the diagnosis is likely to be limited to a small group of conditions affecting the intestine at multiple points. PJS and other polyposis syndromes such as juvenile polyposis syndrome, familial adenomatous polyposis and the PTEN (phosphatase and tensin homologue) hamartoma tumour syndromes, should be considered.
Malignancy, most commonly lymphoma in the younger patient, should also be included in the differential, as should intestinal tuberculosis.
Treatment
On arrival, the girl was taken to theatre for laparotomy. Intraoperative findings were those of grossly inflamed small bowel and free fluid in the pelvis. The two apparent sites of intussusception, identified on CT scan, had since resolved, however there were haemorrhagic areas throughout the small bowel mucosa. In the mid-jejunum, a large, partially obstructing polypoid lesion was palpated through the bowel wall; two smaller polyps were also felt in the distal ileum. Two small bowel resections were performed with primary anastomosis.
Outcome and follow-up
Histological analysis of the resected specimen showed pedunculated polypoid lesions with a nodular surface. Microscopic examination revealed villous architecture lined by normal small intestinal type epithelium. Arborisation of smooth muscle fibres was noted—giving the characteristic ‘Christmas Tree’ appearance to the hamartomatous polyp.
There was epithelial misplacement within the muscularis propria but no evidence of dysplasia or true invasion, ruling out the possibility of an intestinal malignancy.
The patient underwent genetic analysis and was revealed to carry a defect in the STK11/LKB1 gene, a germline mutation known to give rise to PJS.
On close examination in follow-up clinic, subtle areas of pigmentation were identifiable on the buccal mucosa (figure 3.) Summatively, this evidence confirmed a diagnosis of PJS. Once discharged from the surgical team, the patient will continue to be followed up by the paediatric and adult gastroenterologists.
Figure 3.

Subtle pigmentation of the buccal mucosa.
Current guidance from the British Society of Gastroenterology suggests surveillance with extended upper gastrointestinal (GI) endoscopy and colonoscopy (or flexible sigmoidoscopy with contrast enema) every 2–3 years.1 The purpose of this is both to identify and remove any large polyps as well as form part of the cancer surveillance. There is no evidence-based start point for this surveillance process, however, general consensus seems to be from the onset of symptoms, or from mid-late adolescence in the asymptomatic patient.
Discussion
Double intussusception is rare; in this case, we found the lead points of both intussusceptions were hamartomatous polyps. A unifying diagnosis in such cases would point towards polyposis syndrome, of which PJS represents one of few that present in childhood. Incidences of double-site intussusception in PJS have only been reported a handful of times, to the authors’ knowledge.2–4
Double intussusception can be a confusing term; double can refer to two intussuscepta within a single intussuscipiens—either contiguous intestinal segments or, more rarely, two separate portions through the same distal portion.
Simultaneous intussusceptions at two separate sites also have been classified as ‘double intussusception’, but could perhaps be more definitively named ‘double-site intussusceptions’. Clearly, in these examples, a more widespread intestinal pathological process, such as polyposis syndrome, should be considered.
As mentioned, current recommendation for long-term management of PJS involves regular endoscopic surveillance of polyps. GI cancers are expected in approximately 1 in every 50 patients; these may present at any point among the GI tract. Although hamartomata in PJS are not in themselves malignant, there is a proposed increased propensity for adenoma formation and transformation owing to the underlying genetic mutation of the STK11/LKB 1 tumour suppressor gene. This same genetic defect is also thought to bring about an identified increased risk of malignancies of the pancreas, lung, breast, uterus, ovary, cervix and testis. With the exception of the sex organ tumours, these would predominantly be of an adenocarcinoma in tissue type.
Since the syndrome affects the length of the gut, surgery tends to be withheld until a surgical emergency presents itself, such as obstruction.5 The advent of double-balloon endoscopy has opened up the feasibility of polyp surveillance and snaring throughout the GI tract without necessitating surgery. If surgery is performed, palpation of the length of the gut and removal of any identified polyps should be performed.
A comprehensive review by Beggs and colleagues collated a number of recently made recommendations to produce a further recommendation of annual haemoglobin levels, as well as biannual abdominal ultrasound to examine for pancreatic masses, annual gynaecological/testicular examination and 6-monthly breast examination.5 Of note to paediatric surgeons, testicular cancer in PJS has an average age of onset of 8 years.
Learning points.
In the older child presenting with double site intussusception, multiple lead points limit the potential causes to very few diagnoses.
Peutz-Jeghers syndrome should be suspected and can be diagnosed preoperatively due to cutaneous manifestations.
Diagnosis of Peutz-Jeghers syndrome ought to prompt a more thorough exploration of the abdomen at the time of surgery in order to resect any other polyps.
Footnotes
Contributors: JD performed the literature review and was the principle author of the report. NJW was the principle reviewer. DK was the supervising reviewer and gave final approval of the article.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Dunlop M, British Society for Gastroenterology; Association of Coloproctology for Great Britain and Ireland. Guidance on gastrointestial surveillance for hereditary non-polyposis colorectal cancer, familial adenomatous polyposis, juvenile polyposis, and Peutz-Jeghers syndrome. Gut 2002;51:v21–7. doi:10.1136/gut.51.suppl_5.v21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Choi S, Chung S, Kim S et al. A case of Peutz-Jeghers syndrome associated with jejunojejunal and colocolic intussusception. Chonnam Med J 1999;35:407–12. [Google Scholar]
- 3.Marschall J, Hayes P. Intussusceptions in a man with Peutz-Jeghers syndrome. CMAJ 2003;168:315–16. [PMC free article] [PubMed] [Google Scholar]
- 4.Motie M, Amouzeshi A, Jalali A. Multiple intussusceptions as primary manifestation of Peutz-Jeghers syndrome: report of a case. Iran J Pediatr 2009;19:313–16. [Google Scholar]
- 5.Beggs AD, Latchford AR, Vasen HF et al. Peutz-Jeghers syndrome: a systematic review and recommendations for management. Gut 2010;59:975–86. doi:10.1136/gut.2009.198499 [DOI] [PubMed] [Google Scholar]