Abstract
Lumbar disc herniations are rare in pregnancy, with an incidence of 1:10 000. Less than 2% of these herniations result in cauda equina syndrome (CES). Diagnosing CES in pregnant patients can be difficult because changes in bladder and bowel habits are common in normal pregnancies. We present the case of a 29-year-old woman, with a history of lumbar radiculopathy, who presented at 39 weeks gestation with severe lower back and bilateral lower limb radiculopathy. Symptoms of CES began to develop only after the onset of labour. Diagnostic MRI was obtained following delivery and the patient was treated by microdiscectomy. Following surgery, bladder and bowel function began to normalise and at 3 months follow-up, she had made a full recovery. To the best of our knowledge, CES has never been reported to present during labour. This case highlights the diagnostic dilemma and need for a high index of suspicion.
Background
Lumbar disc herniations are rare in pregnancy, with an incidence of 1:10 000.1 Fewer than 2% of such disc herniations result in cauda equina syndrome (CES).2 Missed diagnosis can have disastrous effects on the quality of life of affected patients, and yet the characteristic features of CES can be masked by those of normal pregnancy, and particularly labour, making diagnosis difficult.3–5 Few cases of CES during pregnancy have been reported in the literature, however, this case is, to the best of our knowledge, unique in that the characteristic features of the condition began to develop only after the induction of labour; also, this is the first such case reported in the literature.
Case presentation
A 29-year-old woman (gravidity 1, parity 0) presented at 39 weeks gestation with a 1 week history of severe lower back pain and bilateral radicular leg pain. On examination, there was no neurological abnormality and her rectal examination was entirely normal. The patient had presented to the hospital with similar symptoms 1 week previously and she was sent home. While the fetus was considered to be not at risk, with normal obstetric examination and cardiotocography (CTG), it was decided to proceed with induction of labour so that a MRI could be performed and possible treatment of her back and leg started.
The patient developed progressive difficulty in passing urine and the sensation of incomplete bladder emptying in the 12 h following the induction of labour. This was associated with a change in her neurological examination, with reduced sensation in the right L5 dermatome and the perineal region, raising the concern about possible development of CES. A urinary catheter was sited and drained 400 mL of residual urine. An initial decision was made to allow labour to progress, without requesting a MRI. Unfortunately, within the next 2 h fetal distress was indicated by pathological CTG traces and a category two lower segment caesarean section was performed. The caesarean section was performed under general anaesthesia, which is not normal practice in our institution, to avoid a spinal anaesthesia clouding the clinical picture in the mother, who was suspected of having CES. A healthy baby girl weighing 3270 g was delivered, with Apgar scores of 9 at both 1 and 5 min.
Investigations
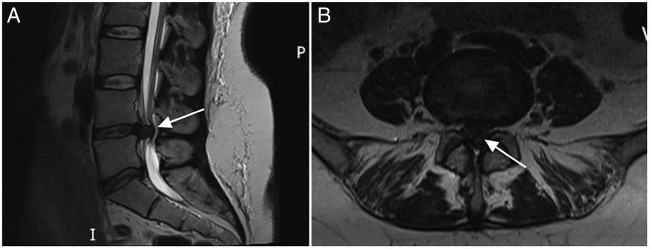
Following recovery from general anaesthesia, an MRI was obtained, which revealed a large L4/5 central intervertebral disc extrusion compressing the cauda equina (figure 1).
Figure 1.
(A) Sagittal and (B) axial sections of T2-weighted MRI demonstrating a large, central intervertebral disc extrusion (arrow) at the level of L4–5 compressing and displacing the thecal sac and nerve roots posteriorly.
Differential diagnosis
Prior to obtaining the MRI, the clinical presentation could have been explained by a smaller intervertebral disc extrusion causing back and leg symptoms. Congestion of Batson’s venous system during labour could have worsened these symptoms mimicking the presentation of CES. The changes to bladder and bowel function could have been consistent with normal pregnancy and labour.
Treatment
A diagnosis of incomplete CES was made and a bilateral L4/5 microdiscectomy was performed under general anaesthesia, with the patient placed prone on a Montreal mattress. Particular care was taken with positioning due to the previous anterior abdominal wall incision from the caesarean section. The extruded disc fragment was removed, and at the end of the procedure the dural tube and traversing L5 nerve roots were fully mobile to the midline bilaterally. There were no complications and there was no neurological deterioration following surgery.
Outcome and follow-up
The patient's radicular leg pain resolved immediately following surgery and her bladder control gradually normalised such that she was discharged home on the 12th postoperative day, without a urinary catheter.
At 3 months follow-up the patient reported normal bladder and bowel control, no leg pain and improving right L5 sensation.
Discussion
Back pain is a very common complaint during pregnancy, affecting >50% of pregnant women.6 7 The incidence of new lumbar disc herniations during pregnancy is 1:10 000. The diagnosis should be considered in any pregnant patient presenting with severe lower back or leg pain.1 8 CES results from compression of the nerve roots distal to the conus medullaris and complicates fewer than 2% of disc herniations.2 Pregnancy itself is not considered an independent risk factor for disc disease.9 However, as the prevalence of other recognised risk factors, such as high body mass index and increased age, continue to rise in the pregnant population, physicians should expect to encounter more cases of lumbar disc herniations than they may have in the past.10
CES is a clinical diagnosis characterised by sphincteric dysfunction. Individual patients can present with some or all of the following ‘red flag’ symptoms:2 11
Disturbance of bladder, bowel and/or sexual function
Saddle anaesthesia (sensory disturbance of the buttocks, posterior thighs and perineal region)
Bilateral radicular leg pain.
The preservation or loss of executive bladder control allows classification into two clinical categories.11 CES with retention (CESR) is characterised by painless urinary retention and eventual overflow incontinence. Patients with incomplete CES (CESI) maintain some sphincteric function despite altered urinary sensation, loss of desire to void and/or poor urinary stream. Our patient displayed these features. Although the usefulness of this distinction has been contested,12 it does hold prognostic value as patients with CESI at the time of surgery typically have more favourable outcomes than those with CESR.11
On examination, reduced perianal sensation, reduced resting anal tone and reduced voluntary anal contraction are hallmark features. Lower limb lower motor neurone signs (reduced power, sensation and reflexes) may also be present. Suspicion of CES should prompt thorough neurological examination, and MRI not only to confirm diagnosis, but also to identify the level, aetiology and extent of pathology.11 In our case, the patient was in labour before she presented with symptoms of progressive bladder dysfunction.
A decision was made to delay the MRI until after delivery, given that the pregnancy was initially thought to be progressing adequately. Pregnancy is not a contraindication for MRI, and has proven to be safe in the second and third trimesters.13 The potential risks presented to the fetus in the first trimester are currently inadequately understood, however, if CES is suspected, then the risks are outweighed by the maternal benefits.10 13
As demonstrated in our case, it is important to note that patients’ symptoms can change or progress over time and that sphincteric dysfunction is a feature of pregnancy, posing a diagnostic dilemma. Therefore, patients should be advised to report new or progressive symptoms, particularly changes in motor function, micturition and bowel incontinence and be re-examined regularly.10
CES is a surgical emergency, as failure to expediently decompress affected nerve roots can result in permanent neurological deficit, and loss of ureteric and anal sphincter control.2 11 However, because of the low incidence of occurrence of CES and the similarity of its features to the normal physiological changes during pregnancy and labour, misdiagnosis has been reported.3–5 Mohapatra and Patra5 published a case in which a patient at 20 weeks gestation presented with a 25-day history of lower back pain and urinary retention manifesting as a watery vaginal discharge. The true diagnosis of CES was misdiagnosed by both an orthopaedic surgeon and obstetrician as leaking membranes and pregnancy-related retention, respectively. At 7 months, the patient continued to experience urinary and faecal incontinence, which the authors suggested would probably persist for life.
Performing spinal surgery on pregnant patients can be challenging. Optimal access to the spine is permitted in the prone position. Beyond the first trimester, prone positioning and resultant abdominal compression can incite preterm labour.8 Surgery is therefore undertaken in either the lateral decubitus position, or with the use of frames that allow the gravid abdomen to hang freely.14 15 Beyond 34 weeks, the risk of preterm labour during surgery rises, while the risk of neonatal pulmonary compromise decreases. Therefore, in late pregnancy, delivery of the fetus prior to surgery may be preferable.16 17
In our case, emergency caesarean section had already been performed prior to spinal surgery, and therefore patient positioning with respect to fetal safety was not a concern. Care was taken to minimise the pressure applied to the Pfannenstiel wound, to prevent dehiscence, by placing additional gel padding on top of the Montreal mattress. Al-areibi et al16 highlighted the potential for major blood loss when operating in the immediate postpartum period as a result of engorged epidural veins. Therefore, standard precautions for expectant blood loss were taken, including performing blood grouping and sample-saving prior to surgery, and having cell salvage available in theatre.
Learning points.
Cauda equina syndrome (CES) is a rare cause of back pain in pregnancy and labour that should be considered when any of the ‘red flag’ symptoms are present.
Diagnosing CES in pregnant patients can be difficult, as bladder and bowel symptoms often resemble those of normal pregnancy and labour.
The clinical picture can evolve over time. Regular assessment of the clinical signs reduces the likelihood of missing a diagnosis of CES.
In cases where CES is suspected but MRI is not possible until after delivery, epidural anaesthesia is advised against as this could cloud the clinical picture and make monitoring the progression of symptoms difficult.
Footnotes
Contributors: CSJ, SP, WG-J and OMS were responsible for conception and design. CSJ, SP, WG-J and OMS were responsible for interpretation of data. CSJ and SP were responsible for drafting of article. WG-J and OMS were responsible for revising the article critically for important intellectual content. CSJ, SP, WG-J and OMS were responsible for approving the final manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.LaBan M, Perrin J, Latimer F. Pregnancy and the herniated lumbar disc. Arch Phys Med Rehabil 1983;64:319–21. [PubMed] [Google Scholar]
- 2.Gitelman A, Hishmeh S, Morelli B et al. . Cauda equina syndrome: a comprehensive review. Am J Orthop 2008;37:556–62. [PubMed] [Google Scholar]
- 3.Timothy J, Anthony R, Tyagi A et al. . A case of delayed diagnosis of the cauda equina syndrome in pregnancy. Aust N Z J Obstet Gynaecol 1999;39: 260–1. 10.1111/j.1479-828X.1999.tb03389.x [DOI] [PubMed] [Google Scholar]
- 4.Ashkan K, Casey A, Powell M et al. . Back pain during pregnancy and after childbirth: an unusual cause not to miss. J R Soc Med 1998;91:88–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mohapatra R, Patra R. Cauda equina syndrome in pregnancy due to disc prolapse. JIACM 2008;9:140–2. [Google Scholar]
- 6.Bhardwaj A, Nagandla K. Musculoskeletal symptoms and orthopaedic complications in pregnancy: pathophysiology, diagnostic approaches and modern management. Postgrad Med J 2014;90:450–60. 10.1136/postgradmedj-2013-132377 [DOI] [PubMed] [Google Scholar]
- 7.Stapleton D, MacLennan A, Kristiansson P. The prevalence of recalled low back pain during and after pregnancy: a South Australian population survey. Aust N Z J Obstet Gynaecol 2002;42:482–5. 10.1111/j.0004-8666.2002.00482.x [DOI] [PubMed] [Google Scholar]
- 8.Abou-Shameh M, Dosani D, Gopal S et al. . Lumbar discectomy in pregnancy. Int J Gynaecol Obstet 2006;92:167–9. 10.1016/j.ijgo.2005.09.028 [DOI] [PubMed] [Google Scholar]
- 9.Weinreb J, Wolbarsht L, Cohen J et al. . Prevalence of lumbosacral intervertebral disk abnormalities on MR images in pregnant and asymptomatic non-pregnant women. Radiology 1989;170:125–8. 10.1148/radiology.170.1.2521192 [DOI] [PubMed] [Google Scholar]
- 10.Curtin P, Rice J. Cauda equina syndrome in early pregnancy: a case report. Acta Obset Gynecol Scand 2007;86:758–9. 10.1080/00016340500438447 [DOI] [PubMed] [Google Scholar]
- 11.Gardner A, Gardner E, Morley T. Cauda equina syndrome: a review of the current clinical and medico-legal position. Eur Spine J 2011;20:690–7. 10.1007/s00586-010-1668-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Germon T, Ahuja S, Casey A et al. . British Association of Spine Surgeons standards of care for cauda equina syndrome. Spine J 2015;15:S2–4. 10.1016/j.spinee.2015.01.006 [DOI] [PubMed] [Google Scholar]
- 13.Patenaude Y, Pugash D, Lim K et al. . The use of magnetic resonance imaging in the obstetric patient. J Obstet Gynaecol Can 2014;36:349–63. [DOI] [PubMed] [Google Scholar]
- 14.Han I, Kuh S, Kim J et al. . Clinical approach and surgical strategy for spinal diseases in pregnant women. Spine 2008;33:e614–19. 10.1097/BRS.0b013e31817c6c7d [DOI] [PubMed] [Google Scholar]
- 15.Brookfield K, Brown M. How should pregnant women with spinal disease be managed? Nat Clin Pract Neurol 2008;4:652–3. 10.1038/ncpneuro0952 [DOI] [PubMed] [Google Scholar]
- 16.Al-areibi A, Coveney L, Singh S et al. . Case report: anesthetic management for sequential cesarean delivery and laminectomy. Can J Anesth 2007;54:471–4. 10.1007/BF03022034 [DOI] [PubMed] [Google Scholar]
- 17.Brown M, Brookfield K. Lumbar disc excision and cesarean delivery during the same anesthesia. A case report. J Bone Joint Surg Am 2004;86:2030–2. [DOI] [PubMed] [Google Scholar]