Background
Few studies report estimates of cardiovascular disease (CVD) or major adverse cardiovascular events (MACE) in patients with psoriatic arthritis (PsA).
Objective
To estimate rates of incident CVD and MACE in patients with PsA compared to patients without PsA.
Methods
Using the Clinical Practice Research Datalink, we conducted 2 cohort studies of patients with PsA compared to patients without PsA or psoriasis matched on age, sex, general practice, and calendar time: 1 study of CVD and 1 study of MACE. In each study, we excluded patients who had a study outcome before cohort entry. Cases were patients with a first-time diagnosis of CVD or MACE recorded during follow-up. We estimated incidence rates (IRs) and incidence rate ratios (IRRs) with 95% confidence intervals (95% CI) and stratified results in the PsA cohort by exposure to systemic PsA treatments.
Results
The IR of CVD was higher in the patients with PsA compared to those without PsA (12.8/1000 person-years [PYs] [95% CI, 11.9–13.7] and 9.6/1000 PYs [95% CI, 9.3–9.0]; IRR, 1.33 [95% CI, 1.23–1.44]). The IR of MACE was slightly higher in the PsA compared to the non-PsA cohort (4.6/1000 PYs [95% CI, 4.1–5.1] and 3.5/1000 PYs [95% CI, 3.4–3.7]; IRR, 1.30 [95% CI, 1.15–1.47]). Among the patients with PsA, IRs were higher for those who received PsA treatments for both outcomes but did not differ significantly by type of treatment received.
Conclusions
The rates of CVD and MACE were slightly higher in the patients with PsA compared to the patients without PsA. Among the patients with PsA, rates of both outcomes were higher among those who received prescriptions for systemic PsA treatments.
Key Words: cardiovascular disease, major adverse cardiovascular events, psoriatic arthritis
Psoriatic arthritis (PsA) and psoriasis have been associated with an increased prevalence of cardiovascular disease (CVD); however, few published studies have examined the risk of incident CVD in patients with PsA, whereas only 1 recent analysis presented data on major adverse cardiovascular events (MACE).
A systematic review of the literature by Tobin et al found 5 relevant studies on cardiovascular events in patients with PsA. Overall, rates of CVD were higher in the PsA population as compared to non-PsA comparison group.1 A more recent systematic review2 of available literature of PsA and cardiovascular morbidity and mortality found similar results as Tobin et al after reviewing 28 similar and more recent studies. Overall mortality ranged from 8% to 16%, whereas cardiovascular death ranged from 25% to 50% of overall deaths in the study populations.2 An analysis of a US claims database also reported a significant increased risk of cardiovascular events among 3066 patients with PsA compared to matched patients without PsA.3 Prevalence ratios ranged from 1.3 to 1.5 for hypertension, ischemic heart disease, and congestive heart failure.3 A study that prospectively followed 648 patients with PsA enrolled through the main PsA clinic in Toronto for selected cardiovascular events found that the prevalence ratio of myocardial infarction, angina, and hypertension were all approximately 2-fold higher in the PsA population compared to those without PsA.4 More recently, 3 population-based cohort studies reported conflicting results.5–7 A large cohort study reported a marginally increased adjusted hazard ratio (HR) for incident MACE among 4174 patients with PsA without prescriptions for disease-modifying antirheumatic drugs (DMARDs) compared to patients without PsA (HR, 1.24).5 Another study reported that the 10-year cumulative incidence of cardiovascular events was 17% among 126 patients with PsA with no history of CVD.6 However, the Nord-Trøndelag Health Study reported no difference in 10-year risk of fatal cardiovascular events between 338 patients with PsA and 50,468 patients without PsA, although the patients with PsA had higher prevalence of CVD than those without PsA.7
The objective of this study was to estimate the rate of incident CVD and MACE among patients with PsA compared to matched patients without PsA or psoriasis using the United Kingdom (UK) Clinical Practice Research Datalink (CPRD).
MATERIALS AND METHODS
Data Source
The UK CPRD is a large, longitudinal, population-based electronic medical record database that contains data on approximately 10 million people. The UK National Health Service provides universal coverage; therefore, the database contains a representative sample of the UK general population.8 Participating general practitioners (GPs) contribute data in an anonymous format including medical diagnoses, physical findings, symptoms, details of hospital stays and specialist visits, and deaths. Several validation studies have been published on the accuracy of information recorded in the CPRD,8–11 which indicates that the data are of high accuracy with regard to recorded clinical diagnoses with more than 90% of information from the manual medical records present in the GP’s office recorded on the computer.
Study Design and Base Population
This cohort study was conducted using CPRD data from January 1, 1988 through December 31, 2012. We identified all patients in the CPRD with a diagnosis of PsA who had at least 1 year of recorded medical history in their record before the first PsA diagnosis code. One year of history was required to ensure that we identified patients with new diagnoses of PsA that were not diagnosed before the start of the patient’s record. The cohort entry date was the date of the first recorded PsA diagnosis. For each patient with PsA, up to 10 patients with no recorded diagnoses of psoriasis or PsA (henceforth referred to as non-PsA) were matched on age, sex, and general practice attended. All patients without PsA were required to be present in the database on the cohort entry date of their matched patient with PsA, and the cohort entry date of each patient with PsA was assigned to the matched patients without PsA.
Cohorts and Outcomes of Interest
Separate cohorts were identified for each outcome of interest (ie, CVD, MACE). In each cohort, patient follow-up began at the cohort entry date and continued until the end of the study period, end of registration with the practice, death, or until they developed the outcome of interest. The accumulated time was expressed as person-years (PYs) at risk. Diagnoses of interest were identified using automated searches of the electronic record of all patients in each cohort. Cohort and outcome definition are described in the succeeding subsections.
CVD Cohort
Cardiovascular diseases under study included arrhythmias, ischemic heart disease, angina, myocardial infarction, stroke, pericardial disease, pulmonary hypertension, and sudden death. Any patient who had one of these diagnoses recorded before the cohort entry date was excluded from this cohort. All patients who had a first-time record of one of these diagnoses after the cohort entry date were considered cases. If a patient had more than one of these outcomes, we included the first only. The electronic records for a sample of identified cases were reviewed to assess the accuracy.
MACE Cohort
Major adverse cardiovascular events were comprised of all myocardial infarctions, strokes, and sudden deaths. Any patient who had one of these diagnoses recorded before the cohort entry date was excluded from the MACE cohort. A patient was considered a case if they had a first-time record for one of these diagnoses after the cohort entry date. If a patient had more than one of these outcomes, we included the first only. The electronic records for a sample of identified cases were reviewed to assess accuracy. Each case of sudden death was reviewed to confirm that the patient died from a cardiovascular event.
Stratification by Exposure to PsA Systemic Therapy
Among those with PsA, we stratified the results by person-time of exposure to systemic therapies to treat PsA and non-exposed time. The systemic therapies included DMARDs/biologics (eg, methotrexate, sulfasalazine, and adalimumab), immunosuppressants (eg, azathioprine and leflunomide), and corticosteroids (codes are available upon request), which were treated as time-varying covariates during follow-up. Person-time of exposure to these drugs was accrued between the dates of the prescription issued through 3 months after the end of the supply (based on the amount prescribed divided by the number of times per day). Otherwise, the follow-up time was treated as not exposed to the systemic therapies. To assess the appropriateness of this exposure time window definition, we conducted sensitivity analyses where the period after the end of supply was varied from 1 month to 6 months.
Statistical Analysis
Within each cohort, we estimated incidence rates (IRs) per 1000 PYs and incidence rate ratios (IRRs) with 95% confidence intervals (CIs) for PsA compared to non-PsA cohorts, and stratified by sex and age (<30, 30–49, 50–69, and ≥70 years). We estimated the risk (cumulative hazard function) of each study outcome using the Kaplan-Meier method and tested the differences using log-rank test. In the PsA cohort, the results were stratified by person-time of exposure or nonexposure to systemic PsA therapy and by type of drug prescribed. Statistical analyses were carried out using SAS Release 9.2 (SAS Institute Inc, Cary NC).
The protocol for this study was reviewed and approved by the Independent Scientific Advisory Committee of the CPRD.
RESULTS
Cardiovascular Disease
We identified 7982 patients with PsA and 74,583 patients without PsA in the CVD cohort after exclusions. Their characteristics are presented in Table 1. The rate of incident CVD was marginally higher in the PsA cohort compared to the non-PsA cohort (12.8/1000 PYs [95% CI, 11.9–13.7] and 9.6/1000 PYs [95% CI, 9.3–9.9], respectively; IRR, 1.33 [95% CI, 1.23–1.44]; Table 2). Rates were higher in men compared to women and increased with increasing age in both the PsA and non-PsA cohorts. Rates were higher in the PsA cohort at every age stratum. Rates were consistently higher in the PsA cohort compared to the non-PsA cohort at each time point after cohort entry (P < 0.0001; Fig. 1).
TABLE 1.
Distribution of Characteristics of Patients With and Without PsA, by Subcohort
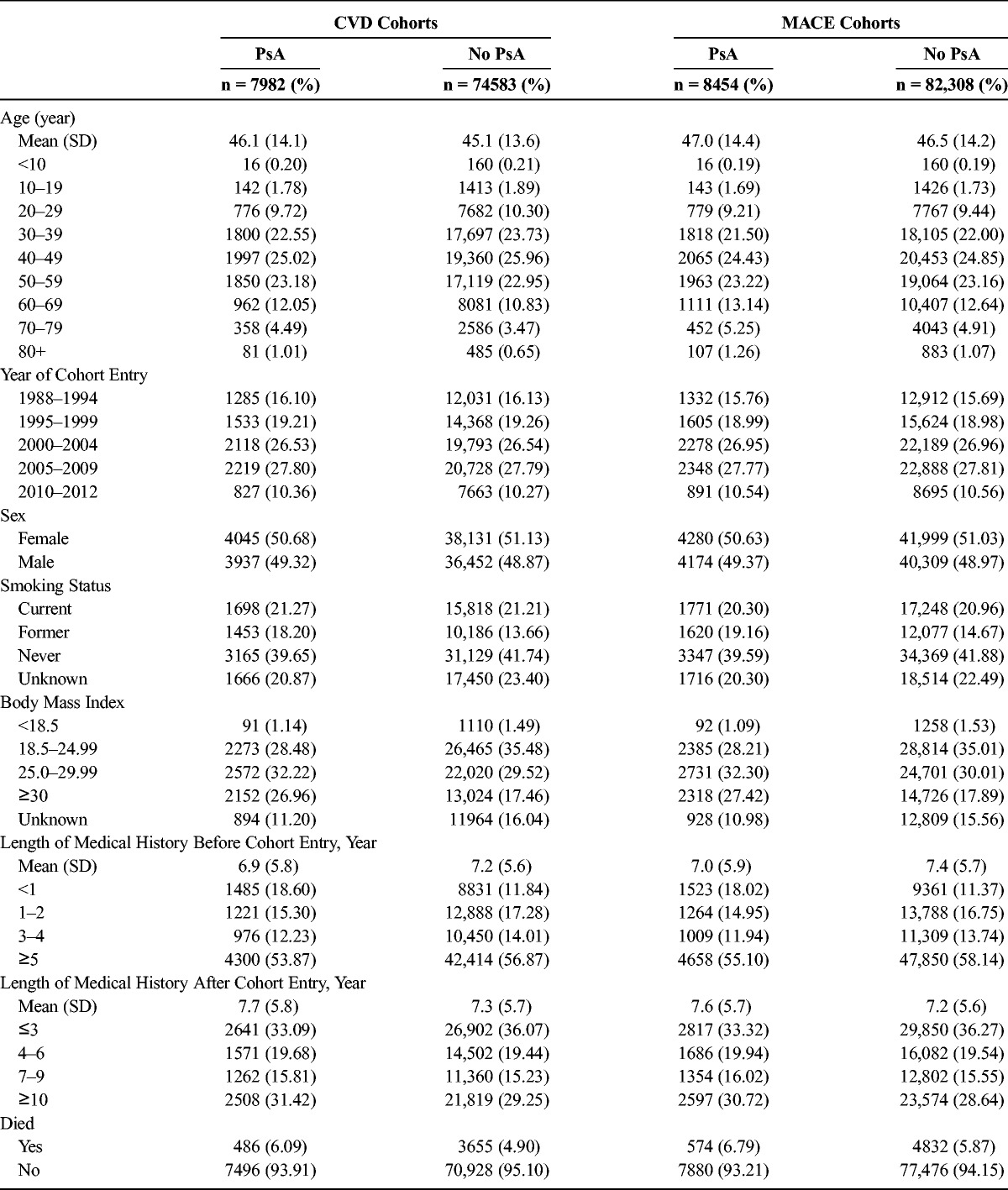
TABLE 2.
Rates of Incident CVD

FIGURE 1.
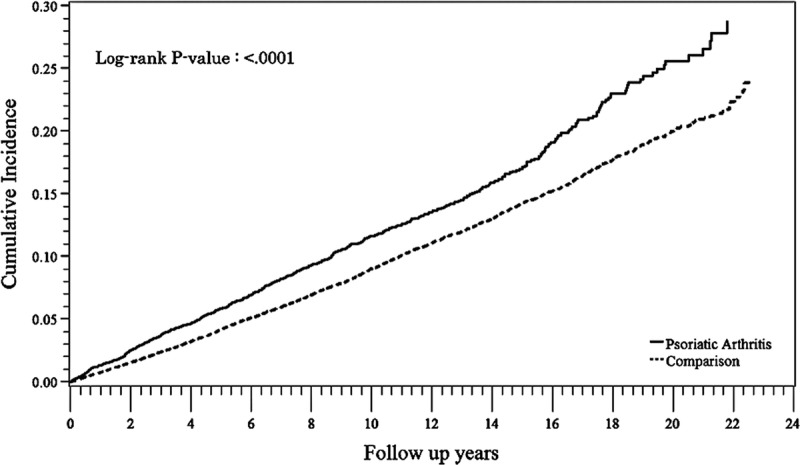
Cumulative incidence of CVD in the PsA and non-PsA cohorts.
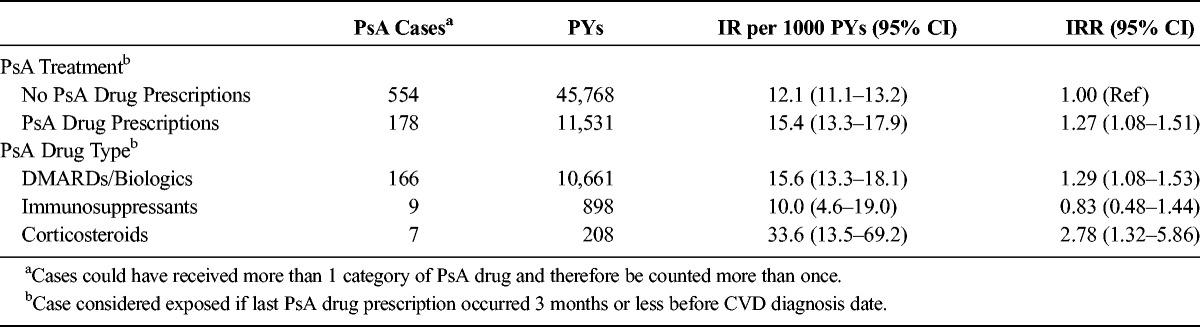
In the PsA cohort, rates of incident CVD were marginally higher in patients who received prescriptions for PsA drugs compared to those who did not (IRs, 15.4/1000 PY [95% CI, 13.3–17.9] and 12.1/1000 PY [95% CI, 11.1–13.2], respectively; IRR, 1.27 [95% CI, 1.08–1.51]; Table 3). Among those who received prescriptions for PsA drugs, IRs were highest among those treated with corticosteroids (33.6/1000 PYs; 95% CI, 13.5–69.2), followed by DMARDs/biologics (15.6/1000 PYs; 95% CI, 13.3–18.1). These differences in IRs were not significant because of the small number of patients exposed to immunosuppresants or corticosteroids. The results did not differ when we redefined the exposure window in the sensitivity analyses.
TABLE 3.
Rates of Incident CVD in Patients With PsA, Stratified by Receipt of PsA Drug Prescriptions
Major Adverse Cardiovascular Events
There were 8454 patients with PsA and 82,308 patients without PsA in the MACE cohort after exclusions. The characteristics of this cohort are presented in Table 1. The IR of incident MACE was higher in the PsA cohort compared to the non-PsA cohort (4.6/1000 PY [95% CI, 4.1–5.1] and 3.5/1000 PY [95% CI, 3.4–3.7], respectively; IRR, 1.30 [95% CI, 1.15–1.47]; Table 4). Rates were higher in the patients with PsA compared to the patients without PsA in all age groups. Rates were higher in men compared to women in both cohorts and increased with increasing age. Rates were significantly higher in the PsA cohort than in the non-PsA cohort at each time point after cohort entry (P < 0.0001; Fig. 2).
TABLE 4.
Rates of MACE

FIGURE 2.

Cumulative incidence of MACE in the PsA and non-PsA cohorts.
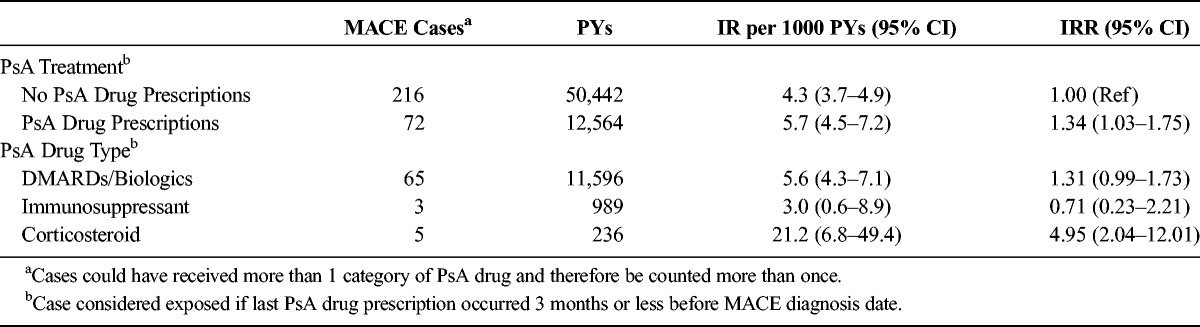
In the PsA cohort, the IR of MACE was marginally higher in patients who received prescriptions for PsA drugs compared to those who did not (IR, 5.7/1000 PYs [95% CI, 4.5–7.2] and 4.3/1000 PYs [95% CI, 3.7–4.9], respectively; IRR, 1.34 [95% CI, 1.03–1.75]; Table 5). Among those who received prescriptions for PsA drugs, IRs were highest among those treated with corticosteroids (21.2/1000 PYs, 95% CI, 6.8–49.4), followed by DMARDs/biologics (5.6/1000 PYs; 95% CI, 4.3–7.1; Table 5). These IRs were not statistically different from each other because of the small number of patients exposed to corticosteroids or immunosuppressants. The results were not materially different when we redefined the exposure window in the sensitivity analyses.
TABLE 5.
Rates of MACE in Patients With PsA, Stratified by Receipt of PsA Drug Prescriptions
DISCUSSION
Incidence rates of CVD and MACE were slightly higher in the patients with PsA compared to the patients without PsA. In the patients with PsA, IRs were higher among those who received prescriptions for systemic therapy compared to the patients with PsA who did not. Among the treated patients with PsA, rates of CVD and MACE were highest among current users of corticosteroids, compared to DMARDs/biologics and immunosuppressants, although the rates were not significantly different among any PsA treatment owing to the small number of patients exposed to corticosteroids and immunosuppressants. The higher risk in treated patients with PsA compared to non-treated patients may be explained by the severity of the PsA disease: Patients who receive treatments are likely to have more severe disease than those who do not.
There are only a few studies published to date that provide data on rates of incident CVD and MACE in patients with PsA to help put the results of this study into context. A recent analysis of patients with PsA compared to patients without PsA in The Health Improvement Network (THIN) database reported a similar incidence rate (5.7 per 1000 PYs) and found that the age- and sex-adjusted HR of MACE was 1.33 (95% CI, 1.13–1.58) among patients with PsA with no DMARD prescriptions, whereas they found no significant increased risk of MACE among patients with PsA with DMARD prescriptions.5 Because of different definitions for exposure to DMARDs and comparison group selection, it is not possible to compare our findings with theirs directly. Another recently published analysis of 1952 patients with PsA in the CPRD age 18 years or older diagnosed between July 2006 and June 2010 reported a slightly lower IR of incident CVD than presented in our study (3.7 per 1000 PYs).12 The difference in the observed IR may be due to differences in the study period (2006–2010 compared to 1988–2012), potential differences in the definition of CVD (we included arrhythmias, pulmonary hypertension, and pericardial disease, whereas they did not), or a shorter follow-up period (mean of 3 years compared to more than 7 years in our study). Additionally, this publication only reported relative risk estimates comparing PsA to patients with psoriasis; therefore, their rates are not comparable to ours. None of these studies looked at different mechanisms of heart disease, so we cannot evaluate whether PsA is associated with certain mechanisms more than others.
Our population-based study had a number of strengths. We used a very large and well-established, validated, longitudinal primary care database, the CPRD, which is known for its high accuracy and completeness of diagnoses. The mean length of follow-up was more than 7 years in both the PsA and non-PsA cohorts for each outcome of interest. By excluding patients who had less than 1 year in their history before the date of the first recorded PsA diagnosis, we reduced the risk of including patients with prevalent, rather than incident, PsA. Therefore, in contrast to previously published studies, our results reflect the risk of CVD and MACE in patients with incident PsA. This analysis contributes to an area that is not well understood in the PsA population. This study is one of a few that present population-based estimates of incident CVD and MACE in patients with PsA. Our estimates and results are similar to other studies published to date.
There were a few potential limitations to consider. First, it is possible that we included some people who did not actually have PsA. However, we assessed the number of PsA diagnoses, codes for PsA symptoms, and treatments for PsA to validate the diagnosis and found that approximately 98% of potential patients with PsA identified had at least one of these supporting codes. Thus, we are confident that most of people in the PsA cohort did have the disease. Second, it is possible that we miscalculated person-time of exposure, since some patients with PsA may have stopped taking systemic PsA therapies sooner or later than we assumed based on the prescription data. To assess this, we conducted sensitivity analyses, where we extended and shortened the exposure time window. There were no material differences in the results regardless of the exposure window used. In the UK, biologics are often prescribed by consultants (specialists) and thus are rarely captured in the GP record; thus, it is possible that we misclassified some exposed person-time as nonexposed. The incomplete capture of exposure to biologics also limits our ability to separate independent effects of biologics from DMARDs.
In summary, incidence rates of CVD and MACE were slightly higher in patients with newly diagnosed PsA compared to patients without PsA. In patients with PsA, IRs were higher among those who received prescriptions for systemic therapy compared to patients with PsA who did not; however, this could reflect the effect of the severity of PsA rather than an effect of the systemic therapies. This study, which followed patients with newly diagnosed PsA, had a shorter duration of disease experience as compared to other studies but has found similar results to studies of patients with long-term PsA, providing further evidence of an association between PsA and CVD and MACE.
Footnotes
Conflicts of Interest and Source of Funding: This study was sponsored by Celgene Corporation. Li, Hagberg, and Jick received funding from Celgene Corporation to conduct the study. Peng, Shah, and Paris are all employees of and own stock/have stock options in Celgene Corporation.
REFERENCES
- 1. Tobin AM, Veale DJ, Fitzgerald O, et al. Cardiovascular disease and risk factors in patients with psoriasis and psoriatic arthritis. J Rheumatol. 2010; 37: 1386– 1394. [DOI] [PubMed] [Google Scholar]
- 2. Jamnitski A, Symmons D, Peters MJ, et al. Cardiovascular comorbidities in patients with psoriatic arthritis: a systematic review. Ann Rheum Dis. 2013; 72: 211– 216. [DOI] [PubMed] [Google Scholar]
- 3. Han C, Robinson DW, Jr, Hackett MV, et al. Cardiovascular disease and risk factors in patients with rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis. J Rheumatol. 2006; 33: 2167– 2172. [PubMed] [Google Scholar]
- 4. Gladman DD, Ang M, Su L, et al. Cardiovascular morbidity in psoriatic arthritis. Ann Rheum Dis. 2009; 68: 1131– 1135. [DOI] [PubMed] [Google Scholar]
- 5. Ogdie A, Yu Y, Haynes K, et al. Risk of major cardiovascular events in patients with psoriatic arthritis, psoriasis and rheumatoid arthritis: a population-based cohort study. Ann Rheum Dis. 2015; 74: 326– 332. doi: 10.1136/annrheumdis-2014-205675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ernste FC, Sánchez-Menéndez M, Wilton KM, et al. Cardiovascular risk profile at the onset of psoriatic arthritis: a population-based, cohort study. Arthritis Care Res (Hoboken). 2015; 67: 1015– 1021. doi: 10.1002/acr.22536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gulati AM, Semb AG, Rollefstad S, et al. On the HUNT for cardiovascular risk factors and disease in patients with psoriatic arthritis: population-based data from the Nord-Trøndelag Health Study. Ann Rheum Dis. 2015. pii: annrheumdis-2014-206824. doi: 10.1136/annrheumdis-2014-206824. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 8. Lawson DH, Sherman V, Hollowell J. The General Practice Research Database. Scientific and Ethical Advisory Group. QJM. 1998; 91: 445– 452. [DOI] [PubMed] [Google Scholar]
- 9. Jick H, Jick SS, Derby LE. Validation of information recorded on general practitioner based computerized data resource in the United Kingdom. BMJ. 1991; 302: 766– 768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jick H, Terris BZ, Derby LE, et al. Further validation of information recorded on a general practitioner based computerized data resource in the United Kingdom. Pharmacoepidemiol Drug Saf. 1992; 1: 347– 349. [Google Scholar]
- 11. Jick SS, Kaye JA, Vasilakis-Scaramozza C, et al. Validity of the general practice research database. Pharmacotherapy. 2003; 23: 686– 689. [DOI] [PubMed] [Google Scholar]
- 12. Edson-Heredia E, Zhu B, Lefevre C, et al. Prevalence and incidence rates of cardiovascular, autoimmune, and other diseases in patients with psoriatic or psoriatic arthritis: a retrospective study using Clinical Practice Research Datalink. J Eur Acad Dermatol Venereol. 2015; 29: 955– 963. doi: 10.1111/jdv.12742. [DOI] [PubMed] [Google Scholar]


