Abstract
Introduction
Chronic pelvic pain (CPP) affects 3–4% of women worldwide. Proven treatments for CPP are limited and unsatisfactory. The meridian balance method (BM) electroacupuncture (EA) treatment (BMEA + Traditional Chinese Medicine Health Consultation (TCM HC) may be effective for CPP. Previous EA studies have demonstrated an analgesic effect. Large-scale studies on acupuncture for other chronic pain conditions suggest that patient-healthcare provider interaction might play a role in pain reduction. We propose a pilot study to explore the effectiveness of the meridian BMEA treatment in managing women with CPP to inform a future large randomised controlled trial.
Methods and analysis
A 3-armed randomised controlled pilot study is proposed with an aim to recruit 30 women with CPP in National Health Service (NHS) Lothian. Randomisation will be to BMEA treatment, TCM HC or standard care (SC). Validated pain, physical and emotional functioning questionnaires will be administered to all participants at weeks 0, 4, 8 and 12. Focus group discussions will be conducted when week 12 questionnaires are completed. The primary objective is to determine, recruitment and retention rates. The secondary objectives are to assess the effectiveness and acceptability of the proposed methods of recruitment, randomisation, interventions and assessment tools.
Ethics and dissemination
Ethical approval has been obtained from the Scotland Research Ethics Committee (REC 14/SS/1022). Data will be published in peer-reviewed journals and presented at international conferences.
Trial registration number
Keywords: electro-acupuncture, chronic pelvic pain, context effects, mixed methods research
Introduction
Over one million women in the UK suffer from chronic pelvic pain (CPP). Annual healthcare expenditures are estimated at over £150 million.1 2 CPP impacts negatively on quality of life and work productivity.3 CPP is associated with conditions such as endometriosis, painful bladder syndrome and irritable bowel syndrome. Up to 40% of women with CPP referred for diagnostic laparoscopy, have no apparent underlying cause identified for their painful symptoms.4 The management of CPP is complex and treatment is often unsatisfactory.5 We believe that acupuncture may be a helpful adjunct in the management of CPP. Our hypothesis is that the meridian BMEA treatment alleviates pain, and improves physical and emotional functioning, in women with CPP.
Meridian balance method acupuncture
For this study, we have chosen the meridian balance method (BM) acupuncture6 which is a novel approach for the management of painful conditions. With this style of acupuncture, pain relief is expected once the needle is inserted in the appropriately chosen acupuncture points.
The meridian BM acupuncture offers an interactive and systematic strategy to formulate a treatment plan through the diagnosis of the sick meridian and selection of a healthy meridian and acupuncture points. Meridian balancing has been well described in the Huang Di Nei Jing, a seminal classical Chinese medicine (CCM) text7 as well as in modern text.6 8 9 Modern traditional Chinese medicine (TCM) emerges out of the standardisation of CCM, and is one of the most popular approaches used by professional acupuncturists in the UK. In comparison, the meridian BM acupuncture is relatively unknown and rarely included in the curriculum of Chinese medicine schools. The meridian BM acupuncture has several key features: the five systems of meridian balancing (table 1), mirror and image methods.6
Table 1.
Five systems of meridian balance method
| System1 | System 2 | System 3 | System 4 | System 5 | |
|---|---|---|---|---|---|
| Sick meridian | Name Sharing | Branching Bie Jing |
Interior/exterior Biao Li |
Clock Opposite | Clock Neighbour |
| LU/hand Taiyin | SP | UB | LI | UB | LR |
| LI/hand Yangming | ST | LR | LU | KI | ST |
| ST/foot Yangming | LI | PC | SP | PC | LI |
| SP/foot Taiyin | LU | SI | ST | TH | HT |
| HT/hand Shaoyin | KI | GB | SI | GB | SP |
| SI/hand Taiyang | UB | SP | HT | LR | UB |
| UB/foot Taiyang | SI | LU | KI | LU | SI |
| KI/foot Shaoyin | HT | TH | UB | LI | PC |
| PC/hand Jueyin | LR | ST | TH | ST | KI |
| TH/hand Shaoyang | GB | KI | PC | SP | GB |
| GB/foot Shaoyang | TH | HT | LR | HT | TH |
| LR/foot Jueyin | PC | LI | GB | SI | LU |
Meridian Names: GB, gallbladder; HT, heart; KI, kidney; LI, large Intestine; LR, liver; LU, lung; PC, pericardium; SI, small intestine; SP, spleen; ST, stomach; TH, triple heater; UB, urinary bladder.
The five systems of meridian BM
The meridian BM acupuncture utilises the five systems shown in table 1. Each sick meridian (painful area) can be balanced (treated) by any one of the five systems. For example, the ‘sick meridian’, lung meridian (Lung Hand Taiyin) can be balanced by systems 1, 2, 3, 4 or 5.
Image and mirror methods
Once the healthy meridian for treating the sick meridian is identified, the image or mirror method is employed to locate more precisely the areas of the body to be treated. The acupuncturist palpates the meridian of the identified area for the best acupuncture point(s) that will relieve the pain. Thus, point selections are individualised.
The image method maps the relationship between the limb and the whole body (table 2). For example, the hand images the genitals, coccyx and sacrum, and the forearm images the lower abdomen and lower back.6
Table 2.
Image method (upper limb to head and trunk)
| Needled area | Sick area (image) |
|---|---|
| Finger | Testicles and anus |
| Hand | Genitals, coccyx, sacrum |
| Wrist | Bladder area, lumbosacral area |
| Forearm | Lower abdomen, lower back |
| Elbow | Umbilicus level, lumbar 2, waist |
| Upper arm | Upper abdomen, rib cage, chest, mid-upper back |
| Shoulder | Neck, jaw, base of skull |
| Top of shoulder | Top of head |
The mirror method ‘maps’ one limb onto another or one part of the body to another part of the body (table 3). For example, the finger mirrors the toe, and the front mirrors the back of the body and vice versa.10
Table 3.
Mirror method and reverse mirror method
| Mirror method | Reverse mirror method |
|---|---|
| Finger↔toe | Finger↔top of hip |
| Hand↔foot | Hand↔hip |
| Wrist↔ankle | Wrist↔hip joint |
| Forearm↔lower leg | Forearm↔thigh |
| Elbow↔knee | Elbow↔knee |
| Upper arm↔thigh | Upper arm↔lower leg |
| Shoulder↔hip | Shoulder↔ankle |
| Back↔front (Du↔Ren) | Front↔back (Ren↔Du) |
The image and mirror knowledge has also been described in Su Wen, another seminal CCM text that detailed the relationship between back and front, up and down, and left and right.11 This kind of mapping is known in the present day as somatotopy where a specific point of the body can be projected to a specific point in the primary somatosensory cortex of the brain.12
Electrostimulation
To maximise the specific effects of acupuncture needling, the needles may be stimulated manually (manual acupuncture; MA) or with micro electric current (electroaccupuncture, EA). Although there have been no studies to show that EA enhances the analgesic effect of the meridian BM acupuncture, it is, however, the method of choice for several reasons. Evidence from animal and human studies showed that both MA and EA produce analgesic effect.13 EA appears to be more effective than MA in some painful conditions. To obtain an analgesic effect in EA, the optimum time for the needle stimulation is 20–30 min with the frequencies set at 2 and 100 Hz.13 14 Based on these parameters, it is impractical to be manipulating the acupuncture needles manually for 20–30 min and also be consistent. With EA one can set both parameters precisely at every treatment. EA may be measured objectively and is easier to control and standardise than MA.
The context and context effects
There is mounting evidence that acupuncture treatments for chronic pain, such as low back pain,15 16 headache,17 18 shoulder and neck pain,19 are effective. However, a recent individual patient data meta-analysis on the use of acupuncture for chronic pain conditions found a small, statistically significant effect size when compared with sham acupuncture. The effect size was larger and statistically significant when compared with usual care controls.20 This would suggest that as well as the specific needling effects, other factors within the context of the acupuncture treatment play a role in reducing pain, such as the characteristics of the healthcare providers and patients, for example, their beliefs and expectations; the provider–patient interactions as well as how the treatment is administered.21 The effects that result from the complex interactions of such characteristics are known as the context effect.22 23 This effect was demonstrated in a study of pain management in patients with irritable bowel syndrome, showing that an enhanced provider–patient relationship could help alleviate pain. Patients were randomised on to a waiting list (no placebo or interaction with healthcare provider), therapeutic ritual (placebo sham acupuncture with limited interaction) or a supportive relationship (placebo sham acupuncture with enhanced relationship). The supportive relationship produced the most adequate relief of symptoms and enhanced quality of life.24
The proposed pilot study will compare the specific effects of the meridian balanced method (BM) EA needling + the context effects of a Traditional Chinese Medicine Health Consultation (+BMEA+TCM HC), with context effects of a TCM HC (patient–healthcare provider interaction) and standard care (SC). This study will enable us to tease out the different components of acupuncture treatment that contribute to its analgesic effect and to collect important information to inform a future definitive RCT.
Objectives
Primary objective
The primary objective is to determine recruitment and retention rates in National Health Service (NHS) Lothian within defined inclusion/exclusion criteria.
Secondary objectives
To determine the effectiveness and acceptability to participants of the proposed methods of recruitment, randomisation, interventions and assessment tools.
End points
Primary end points
The proportion of eligible patients randomised into the study;
The proportion of randomised patients who complete all treatment interventions and questionnaires at the final follow-up.
Secondary end points
Data on the effectiveness and acceptability of proposed methods of recruitment, randomisation, interventions and assessment tools.
Methods and analysis
Study design
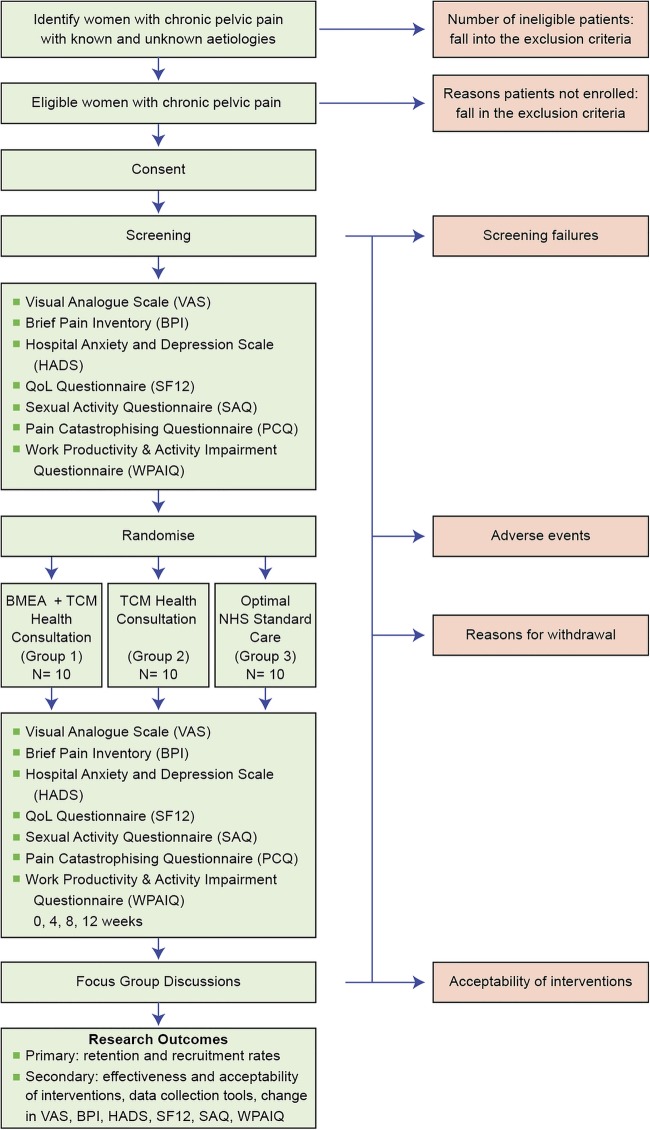
This is a single-centre, open, three-armed parallel randomised controlled pilot study comparing a meridian BMEA + TCM HC (group 1), with TCM HC (group 2) and SC (group 3; figure 1), using a mixed-methods approach.25 It includes quantitative method using validated questionnaires and qualitative method using focus groups postweek 12 questionnaire completion, as well as field notes and a reflexive diary.
Figure 1.
Flow of participants through the BMEA study.
Delivery of intervention in groups 1 and 2
The following descriptions of our study interventions adhered to guidelines in the ‘Revised Standards for Reporting Interventions in Clinical Trial of Acupuncture (STRICTA): Extending the CONSORT Statement’.26
The principal investigator (PI; OTC) will deliver all eight BMEA + TCM HC interventions for group 1 and TCM HC for group 2 within the same setting in NHS Lothian. The first intervention for both groups will last approximately 60 min. Subsequent seven interventions for both groups will last no longer than 40 min. All participants will receive twice weekly interventions for 4 weeks. Participants in group 2 will not receive the meridian BMEA. With permission from the participants, all interventions in groups 1 and 2 will be audiotaped to ensure standardisation of procedures and techniques.
All participants in groups 1, 2 and 3 will complete the questionnaires at weeks 0, 4, 8 and 12, and will be invited to the focus group discussions.
Similarly, group 1 participants will complete the questionnaries at weeks 0, 4, 8 and 12, and will be invited to the focus group discussions.
TCM HC (groups 1 and 2)
Individualised TCM HC
For groups 1 and 2 will share the same approach to the TCM HC. The initial TCM HC will be based on Chinese medicine theory that typically includes history taking: inquiring, listening and inspection of the tongue. Each participant will receive individualised advice based on the specific needs and presenting symptoms. Dietary advice based on Chinese medicine nutrition and other appropriate self-care skills, such as breathing techniques and physical activities maybe recommended and modified to accommodate the participant's changing pattern of pain, sleep, level of anxiety or other health needs. Breathing techniques involve getting the participant to focus her attention on each breath in and out. No herbal medicine therapy will be prescribed.
Individualised and systematic acupuncture point selections
Step 1: Diagnose the affected/sick meridian(s)
This first fundamental and very important step requires the acupuncturist to instruct the patient to indicate where the pain is located, so that the affected meridian(s) can be diagnosed accurately.
Step 2: Identify the balancing meridian(s) based on the five systems
Once the affected meridian(s) is/are identified, one of the following meridians can be chosen to balance the affected meridian(s):
System 1: Foot Taiyin (name sharing meridian);
System 2: Foot Taiyang (branching meridian);
System 3: Hand Yangming (interior/exterior);
System 4: Foot Taiyang (clock opposite);
System 5: Foot Jueyin (clock neighbour).
Step 3: Acupuncture point(s) selection for treatment
Once the balancing meridian has been selected, step 3 involves locating the therapeutic points along the balancing meridian by using the mirror or the image method. The acupuncturist will palpate for the most tender and tight point(s) (ashii points) along the balancing meridian. The ashii point(s) is/are the therapeutic point(s) if on pressing the point(s), the patient reports that the pain has been reduced. Thus, point selections are based on the steps outlined and not on TCM pattern diagnosis.
Step 4: Connecting the battery operated AS SUPER 4 digital stimulator to the acupuncture needles
The negatively charged, black lead (to stimulate) will be connected to the acupuncture needle inserted in the point that gave the most pain relief, while the positively charged lead (red) will be connected to another needle inserted in the same area. We will use the ‘AS SUPER 4’ electro-stimulator (Manufacturer: Schwa-medico, Germany) with four outputs. The electro-stimulator emits a square wave of low frequency (2 Hz) for 3 s alternating with high frequency (100 Hz). Programme 2 will be selected and the duration of treatment will be no shorter than 20 min and no longer than 30 min. These parameters are based on the work of Han et al.27 The intensity of the electrical stimulation will be adjusted based on the participant's feedback, to produce a strong sensation without pain or discomfort.
Depth of needle insertion
The depth of the needle insertion will be adapted to the thickness of the muscles and subcutaneous fatty tissue. For example, for the gluteal muscle, typically a 0.30 mm×75 mm (3 inches) long the needle will be inserted to a depth of between 1.0 and 2 inches. For the forearm, typically a 0.18 mm×30 mm (1.20 inches) will be inserted to a depth of about 0.25–0.75 inch. The number of needles inserted will be individualised. We will use Dong Bang (Korea) and Aculine needles (China).
Group 3—SC
Participants will follow their SC as given by their clinician. SC is defined here as care and treatment that patients would normally receive at The Pelvic Pain Service, NHS Lothian: oral analgesics, neuromodulators such as anticonvulsants and antidepressants, hormonal approaches, counselling/behavioural therapy or surgical interventions when indicated. The Pelvic Pain Service consists of consultant gynaecologist, anaesthetist specialising in pain, a psychologist and a specialist nurse. The participants will not receive the meridian BMEA treatment or the TCM HC.
Participants
Thirty (30) women (aged greater than or equal to 18 years) with a history of CPP will be recruited.
Sample size
We believe that a sample size of 30 patients is appropriate for a pilot study and will allow estimation of percentage rates of recruitment and retention to within a SE of at most 10%.
Inclusion criteria
CPP longer than 6 months duration;
Average numerical pain score of at least 4 out of 10 in the previous week;
Able and willing to comply with intervention;
Women aged 18 and above.
Exclusion criteria
Pregnancy;
Malignancy;
Severe bleeding disorders (eg, type 2, 3 Von Willebrand disease);
Regular anticoagulant administration;
Severe needle phobia;
A history of seizures;
A pace maker in situ;
Moderate to severe psychiatric illness (currently under the care of a psychiatrist);
Treatment with EA and meridian BM within the past 6 months.
Randomisation procedure
We will use an envelope randomisation system created by our statistician. There will be 30 sealed envelopes: 10 meridian BMEA + TCM HC (group 1), 10 TCM HC (group 2) and 10 SC (group 3). The envelopes are randomly assigned a number from 1 to 30. At the start of the study, the first participant who passes the screening will receive envelope number 1; and the second will receive the envelope number 2 and so on. The envelope will be opened in front of the participant by a member of the research team who screens the participant. If randomised into either groups 1 or 2, the participant will receive the appropriate treatment on the same day. If randomised into group 3, the participant will be instructed to continue the NHS SC. There will be no stratification.
Intervention
Eligible women will be randomised into meridian BMEA + TCM HC (group 1), TCM HC (group 2) or SC (group 3). Participants in group 1 will receive eight interventions: twice a week×4 weeks. Participants in group 2 will receive eight TCM HC: twice a week×4 weeks. Participants in group 3 will receive optimal SC (table 4). With permission from the participants, all interventions in groups 1 and 2 will be audiotaped to ensure standardisation of procedures and techniques.
Table 4.
Study intervention schedule
| Group 1 | Group 2 | Group 3 | ||
|---|---|---|---|---|
| Baseline week 0 | BMEA +TCM HC | TCM HC alone | SC | |
| Week 1 | Twice weekly | Twice weekly | SC | |
| Week 2 | Twice weekly | Twice weekly | SC | |
| Week 3 | Twice weekly | Twice weekly | SC | |
| Week 4 | Twice weekly | Twice weekly | SC | |
| Total | 4 Weeks | 8 Interventions | 8 Interventions | SC |
BMEA, balance method electroacupuncture; SC, standard care; TCM HC, Traditional Chinese Medicine Health Consultation.
Acupuncturist information
The PI (OTC) completed 2196 h of acupuncture training and obtained a Masters of Science Degree in Acupuncture at an accredited school in New York City, USA. She is trained in four styles of acupuncture: TCM, Kiiko Matsumoto Japanese style, Five Element and the meridian balanced method. She studied EA as part of her acupuncture training and at the British Medical Acupuncture Society (BMAS). She has over 10 years of experience using Five Element acupuncture to address psychoemotional issues and the meridian balanced method acupuncture for pain management in hospital settings such as the New York University Cancer Institute and Royal Infirmary of Edinburgh, UK. She is a Professional Registered Nurse, a National Board Certified Acupuncturist and Chinese medicine herbalist in New York State, USA. She is also Professional Registered Nurse in the UK.
Data collection
Screening
Eligible women will be consented and screened by a member of the research team. They will be randomised when they have passed screening. All data will be recorded on a case record form and transferred to a secure database.
Assessment tools
Before randomisation, a questionnaire (baseline week 0) will be given to all participants. This will include the following validated tools:
Visual analogue scale;
Brief Pain Inventory (BPI);
Hospital Anxiety and Depression Scale (HADS);
Quality Of Life: SF-12;
Sexual Activity Questionnaire (SAQ);
Pain Catastrophising Questionnaire (PCQ);
Work Productivity and Activity Impairment Questionnaire (WPAIQ).
The set of questionnaires at baseline (week 0) will include participants’ demographic and relevant clinical information. The same questionnaire will be posted to all participants at weeks 4, 8 and 12 with an addressed envelope enclosed.
Focus groups
Three focus group discussions will be conducted after questionnaires in week 12 are completed. All participants from the groups 1, 2 and 3 will be sent a letter of invitation to the focus group discussions. To ensure a high turnout, a week before the designated date of the respective focus group discussions, a member of the research team will contact each participant to encourage them to attend. In order not to bias the group discussions, the PI (OTC) who provides the interventions will not be conducting the focus groups. A separate member of the research team will conduct the three focus group discussions lasting approximately 60 min each. A content guide will be used in each group to focus the discussions,28 which will provide additional data relevant to the study. The topic guide will focus on questions that will explore the participants’ perceived benefits or otherwise of the BMEA treatment (group 1), TCM HC (group2) and NHS SC (group 3). The focus groups will provide in-depth exploration of how and if the perceived benefits affect the quality of their lives, such as sleep quality, energy levels and sexual activities. The discussions will be audiotaped, transcribed and thematically analysed.
Field notes and a reflexive diary
The PI will keep field notes and a reflexive diary during the course of the study. After each intervention, the PI will write notes related to her own observation of salient events, discussions, remarks or behaviours that provide more information about the participant and her experience of pain, as well as the possible impact or otherwise of the intervention. For example, the PI might notice changes in facial colour or expression when a participant describes how the CPP impacted her life; or a participant who started a treatment intervention apparently agitated but who is looking calmer at the close of the session. Such data can add scope and depth as well as illuminate the different aspects of the interventions and the patient–healthcare provider interactions that might not be captured otherwise. In her reflexive diary, the PI will make a note of her thoughts, feelings and insights of such observations. This reflexive practice involves the PI to be introspective, conscious of her role, reactions and assumptions she brings to the intervention and the research process.29
Adverse events
When administered by an appropriately trained and qualified acupuncturist, EA is safe and serious adverse events (SAEs) are not anticipated. However, any SAEs that occur during the study will be reported in the participant's medical record and followed up until resolution of the event. We will also report it to the ACCORD Research Governance (http://www.accord.ed.ac.uk) and Quality Assurance Office based at the University of Edinburgh within 24 h. After randomisation, participants in groups 1 and 2 will be instructed to contact a member of the clinical research team if they have an event that necessitates hospitalisation, or results in significant disability or incapacity. In addition, they will be asked about the occurrence of adverse effects at every of the eight visits during the study. Open-ended and non-leading verbal questioning of the participant will be used to enquire about adverse events, or if they have been admitted to hospital. If there is any doubt as to whether a clinical observation is an AE, the event will be recorded.
End of study
The end of study is defined as the last participant's last visit.
Proposed analyses
Determine recruitment and retention rates
The recruitment rate will be calculated from the number of eligible patients in the participant log. An acceptable recruitment rate is about 50%. We aim to retain 90% of those recruited to the study. If retention rates are low, we will explore the reasons why at the poststudy focus group discussions. Information obtained in the discussions will be used to improve compliance in any future study.
CIs will be calculated for the estimates of rates of recruitment, retention and unanswered questions. The study is not powered to allow comparisons between the randomised groups, and outcomes in each group will just be summarised rather than being compared by formal statistical tests.
Data from the focus groups will be analysed thematically. Thematic analysis aims to highlight and record patterns or themes within a set of data. Such themes capture a certain phenomenon and could be related to the specific research questions or shed light on a specific salient event. Thematic analysis is commonly used in analysis in qualitative research.
Effectiveness and acceptability of proposed methods of recruitment, randomisation, BMEA treatments, TCM HC and assessment tools
Effectiveness will be measured by reductions in pain and associated symptoms such as sleep disturbances, anxiety or depression that are covered in the questionnaires. Additional information on effectiveness, not covered in the questionnaires, will be captured in the focus groups. The appropriateness of assessment tools used can be assessed through examination of data completion and patterns of missing data. The focus groups will be complementary to understanding if the tools chosen are appropriate and will also provide information on acceptability of recruitment, randomisation and the treatments themselves.
Ethics and dissemination
Data will be presented at international conferences and published in peer-reviewed journals. We will make the information obtained from the study available to the public through national bodies and charities. Participants will be informed of the result of the trial via the Pelvic Pain Clinic, NHS Lothian.
Discussion
We believe that a definitive evaluation of the effectiveness of the meridian BMEA treatment in the management of CPP requires a multicentre randomised controlled trial (RCT). We anticipate potential difficulties in a large RCT in acupuncture for chronic pain, and therefore we have designed this pilot study to evaluate its feasibility.
Both MA30 and EA31 32 are safe when performed by appropriately trained acupuncturists. However, because of some theoretical safety concerns, we have erred on the side of caution to exclude, for example, patients who have a history of seizures or have an implanted pace maker.
According to Chinese medicine theory, pain results from blocked meridians leading to an imbalance in the system. On the surface of the body is a network of 12 meridians (6 yin and 6 yang) that connect acupuncture points together.33 Theoretically, these meridians act as a conduit between the surface of the body and the internal organs. The meridian BM acupuncture treats pain by balancing these meridians, for example, using a ‘healthy’ yin meridian to balance a ‘blocked’ yang meridians.9 However, there are considerable skepticisms and controversies surrounding these theories and the existence as physical entities of acupuncture points and the meridian system. Despite efforts to understand these systems, there are continued disagreements as to what they constitute.13 34 Indeed, the PI (OTC) argues that it is more useful to view these systems as a conceptual framework that guides the clinical practice of acupuncture, rather than to argue if they exist. Tangentially related to this view is work undertaken by Langevin et al35 whereby it is hypothesised that acupuncture points and meridians have correspondence to the connective tissue and not as illustrated in Chinese medicine text.
A survey of the literature indicates that this is the first study to investigate the effectiveness of the meridian BMEA treatment for CPP in women using a mixed-methods approach. The mixed-methods approach utilises validated questionnaires and focus group discussions, field notes and a reflexive diary. Undertaking a mixed-methods approach is one of the strengths of the study because we are examining the feasibility of studying a complex intervention, which involves a number of phenomena, which include: TCM health consult, EA and the context effect. Alongside an understanding of participants’ perceived benefits or otherwise of the interventions, this methodology will also help us to understand the role of the researcher in the study intervention. The focus group discussions will capture participants’ subjective experiences of the study intervention.
It is generally considered that the gold standard in effectiveness of RCTs is the use of a placebo control for the study intervention. However, our pilot study does not employ a placebo (sham acupuncture treatment) for several reasons. A considerable body of evidence from large-scale effectiveness studies has demonstrated that sham acupuncture treatments as controls are problematic. For some chronic pain conditions, the observed effects of acupuncture treatments are larger in usual care controls when compared with sham controls. This might suggest that sham acupuncture treatments have physiological effects, and are thus not inert. Past sham controlled studies have employed techniques such as shallow needling, and needling with a retractable needle or toothpick.15 36 Such techniques create a sensation not dissimilar to light touch which has some data to show that it has physiological effects.37 It is also conceivable and probable that shallow needling and needling with a retractable needle elicit similar physiological effects as deep needling. These sham acupuncture techniques are therefore inappropriate. We feel that until better sham techniques are available, it is prudent to design a study that does not employ a placebo control.
Context effects such as expectancy38 treatment rituals39 or patient–provider interactions24 40 have been shown to have an impact on the experience of pain. These may have confounded past studies and might explain the small effect sizes when sham acupuncture treatments were compared with true acupuncture treatments. Attempting to separate the context effects of acupuncture treatment from the specific effects of acupuncture needling presents a major challenge in this area of research. In response, we have designed a three arm RCT to address these challenges. The first arm includes acupuncture needling, electro-stimulation (specific effects of needling) and the patient–healthcare provider interactions (context effects) via a TCM consult (TCM HC). Group 2, (participants receive only TCM HC) controls for the patient–healthcare provider interactions (context effect). Participants in group 3 (SC) will receive the standard NHS care for CPP. Having these two control groups is likely to yield the true effect size of the specific effect of EA needling and the non-specific (context effect) of the patient–healthcare provider interactions. We acknowledge that this pilot study is investigating only one aspect of the several context effects of acupuncture treatment. However, we believe that understanding the clinical outcome of the patient–healthcare provider relationship will create a critical mass of literature to influence the education of future generations of healthcare professionals. The UK SIGN 136 guideline for the management of chronic pain acknowledged that while preliminary data showed that the nature of such a relationship could influence clinical outcome, there are not enough high-quality studies to recommend widespread training.41 (Management of chronic pain. Edinburgh: SIGN; December 2013. Available from URL: http://www.sign.ac.uk; accessed March 2015.)
In assessing the outcome of the interventions, we have chosen validated assessment tools rather than using TCM outcome measures. This is because there are no standardised or validated TCM outcome measures. Arguably, better known validated questionnaires might be more meaningful within a biomedical setting than TCM outcome measures.
In conclusion, our pilot study protocol will enable us to determine the retention and recruitment rate as well as the patients’ experience of the study intervention. It will help us gain better insight into the impact of meridian BMEA needling and the patient–practitioner relationship on CPP in women.
Footnotes
Contributors: OTC; HODC, AWH and MF were involved in research, contribution of original material, editing and approval of final manuscript. RE and EH were involved in editing and approval of final manuscript.
Funding: This work is partly supported by the Barbour Watson Trust, Edinburgh Palliative and Supportive Care Research Fund and MRC Centre for Reproductive Health.
Competing interests: None declared.
Ethics approval: South East Scotland Research Ethics Committee 02 (REC 14/SS/1022).
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Daniels J, Khan KS. Chronic pelvic pain in women. BMJ 2010;341:c4834 10.1136/bmj.c4834 [DOI] [PubMed] [Google Scholar]
- 2.Latthe P, Latthe M, Say L et al. . WHO systematic review of prevalence of chronic pelvic pain: a neglected reproductive health morbidity. BMC Public Health 2006;6:177 10.1186/1471-2458-6-177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Daniels J, Gray R, Hills RK et al. . Laparoscopic uterosacral nerve ablation for alleviating chronic pelvic pain: a randomized controlled trial. JAMA 2009;302:955–61. 10.1001/jama.2009.1268 [DOI] [PubMed] [Google Scholar]
- 4.Howard FM. The role of laparoscopy as a diagnostic tool in chronic pelvic pain. Baillieres Best Pract Res Clin Obstet Gynaecol 2000;14:467–94. 10.1053/beog.1999.0086 [DOI] [PubMed] [Google Scholar]
- 5.Cheong Y, Stones WR. Chronic pelvic pain: aetiology and therapy. Best Pract Res Clin Obstet Gynaecol 2006;20:695–711. 10.1016/j.bpobgyn.2006.04.004 [DOI] [PubMed] [Google Scholar]
- 6.Tan R. Dr. Tan's strategy of twelve magical points. San Diego, CA: Richard Tan Publishing; 2003. [Google Scholar]
- 7.Unschuld P. Huang Di Nei Jing Su Wen: nature, knowledge, imagery in an ancient Chinese medical text. California, USA: University of California Press, 2003. [Google Scholar]
- 8.McCann H, Ross H. Practical Atlas of Tung's Acupuncture. 2nd edn Germany: Verlag Muller & Steinicke Munchen, 2013. [Google Scholar]
- 9.Twicken D. I Ching acupuncture: the balance method. Philadelphia, USA: Singing Dragon, 2012. [Google Scholar]
- 10.Tan R. Acupuncture 1, 2, 3 For Back Pain 2008 2009 Richard Tan Publishing.
- 11.Dun AC. The Yellow Emperor's Inner Classic, Spiritual Pivot (Huang Di Nei Jing Su Wen Jiao Zhu Yu Yi). Tianjin, China: Tianjin Science and Technology Press, 1989. [Google Scholar]
- 12.Dhond RP, Kettner N, Napadow V. Neuroimaging acupuncture effects in the human brain. J Altern Complement Med 2007;13:603–16. 10.1089/acm.2007.7040 [DOI] [PubMed] [Google Scholar]
- 13.Ulett GH, Han SP, Han JS. Electroacupuncture: mechanisms and clinical application. Biol Psychiatry 1998;44:129–38. 10.1016/S0006-3223(97)00394-6 [DOI] [PubMed] [Google Scholar]
- 14.Thomas M, Lundberg T. Importance of modes of acupuncture in the treatment of chronic nociceptive low back pain. Acta Anaesthesiol Scand 1994;38:63–9. 10.1111/j.1399-6576.1994.tb03839.x [DOI] [PubMed] [Google Scholar]
- 15.Haake M, Müller HH, Schade-Brittinger C et al. . German acupuncture trials (gerac) for chronic low back pain: randomized, multicenter, blinded, parallel-group trial with 3 groups. Arch Intern Med 2007;167:1892–8. 10.1001/archinte.167.17.1892 [DOI] [PubMed] [Google Scholar]
- 16.Brinkhaus B, Witt CM, Jena S et al. . Acupuncture in patients with chronic low back pain: a randomized controlled trial. Arch Intern Med 2006;166:450–7. 10.1001/archinte.166.4.450 [DOI] [PubMed] [Google Scholar]
- 17.Melchart D, Streng A, Hoppe A et al. . The acupuncture randomised trial (ART) for tension-type headache—details of the treatment. Acupunct Med 2005;23:157–65. 10.1136/aim.23.4.157 [DOI] [PubMed] [Google Scholar]
- 18.Endres H, Bowing G, Diener HC et al. . Acupuncture for tension-type headache: a multicentre, sham-controlled, patient-and observer-blinded, randomised trial. J Headache Pain 2007;8:306–14. 10.1007/s10194-007-0416-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Witt C, Jena S, Brinkhaus B et al. . Acupuncture for patients with chronic neck pain. Pain 2006;125:98–106. 10.1016/j.pain.2006.05.013 [DOI] [PubMed] [Google Scholar]
- 20.Vickers AJ, Cronin AM, Maschino AC et al. . Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med 2012;172:1444–53. 10.1001/archinternmed.2012.3654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Benedetti F. How the doctor's words affect the patient's brain. Eval Health Prof 2002;25:369–86. 10.1177/0163278702238051 [DOI] [PubMed] [Google Scholar]
- 22.Price DD, Finniss DG, Benedetti F. A comprehensive review of the placebo effect: recent advances and current thought. Annu Rev Psychol 2008;59:565–90. 10.1146/annurev.psych.59.113006.095941 [DOI] [PubMed] [Google Scholar]
- 23.Miller FG, Kaptchuk TJ. The power of context: reconceptualizing the placebo effect. J R Soc Med 2008;101:222–5. 10.1258/jrsm.2008.070466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kaptchuk T, Kelley JM, Conboy L et al. . Components of placebo effect: randomised controlled trial in patients with irritable bowel syndrome. BMJ 2008;336:999–1003. 10.1136/bmj.39524.439618.25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Creswell J, Clark VLP. Designing and conducting mixed methods research. 2nd edn Sage, 2011:2–5. [Google Scholar]
- 26.MacPherson H, Altman DG, Hammerschlag R et al. . Revised standards for reporting interventions in clinical trials of acupuncture (STRICTA): extending the CONSORT statement. J Evid Based Med 2010;3:140–55. 10.1111/j.1756-5391.2010.01086.x [DOI] [PubMed] [Google Scholar]
- 27.Han JS, Terenius L. Neurochemical basis of acupuncture analgesia. Annu Rev Pharmacol Toxicol 1982;22:193–220. 10.1146/annurev.pa.22.040182.001205 [DOI] [PubMed] [Google Scholar]
- 28.Morgan DL. Focus groups as qualitative research. 2nd edn London: Sage Publications, 1997:47–8. [Google Scholar]
- 29.Finlay L. “Outing” the researcher: the provenance, process, and practice of reflexivity. Qual Health Res 2002;12:531–45. 10.1177/104973202129120052 [DOI] [PubMed] [Google Scholar]
- 30.MacPherson H, Thomas K, Walters S et al. . The York acupuncture safety study: prospective survey of 34 000 treatments by traditional acupuncturists. BMJ 2001;323:486–7. 10.1136/bmj.323.7311.486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cummings M. Safety aspects of electroacupuncture. Acupunct Med 2011;29:83–5. 10.1136/acupmed-2011-010035 [DOI] [PubMed] [Google Scholar]
- 32.Thompson JW, Cummings M. Investigating the safety of electroacupuncture with a Picoscope. Acupunct Med 2008;26:133–9. 10.1136/aim.26.3.133 [DOI] [PubMed] [Google Scholar]
- 33.Deadman P, Al-Khafaji M, Baker K. A manual of acupuncture. England, UK: Journal of Chinese Medicine Publications, 2001:13–16. [Google Scholar]
- 34.Pandolfi M. The autumn of acupuncture. Eur J Intern Med 2012;23:31–3. 10.1016/j.ejim.2011.07.017 [DOI] [PubMed] [Google Scholar]
- 35.Langevin HM, Churchill DL, Wu JR et al. . Evidence of connective tissue involvement in acupuncture. FASEB J 2002;16:872–4. 10.1096/fj.01-0925fje [DOI] [PubMed] [Google Scholar]
- 36.Langevin H, Wayne PM, MacPherson H et al. . Paradoxes in acupuncture research: strategies for moving forward. Evid Based Complement Altern Med 2011;2011:180805 10.1155/2011/180805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lund I, Lundeberg T. Are minimal, superficial or sham acupuncture procedures acceptable as inert placebo controls? Acupunct Med 2006;24:13–15. 10.1136/aim.24.1.13 [DOI] [PubMed] [Google Scholar]
- 38.Kong J, Kaptchuk TJ, Polich G et al. . Expectancy and treatment interactions: a dissociation between acupuncture analgesia and expectancy evoked placebo analgesia. Neuroimage 2009;45: 940–9. 10.1016/j.neuroimage.2008.12.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kaptchuk TJ. The placebo effect in alternative medicine: can the performance of a healing ritual have clinical significance? Ann Intern Med 2002;136:817–25. 10.7326/0003-4819-136-11-200206040-00011 [DOI] [PubMed] [Google Scholar]
- 40.Paterson C, Dieppe P. Characteristic and incidental (placebo) effects in complex interventions such as acupuncture. BMJ 2005;330:1202–5. 10.1136/bmj.330.7501.1202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Management of Chronic Pain, UK Scottish Intercollegiate Guideline Network (SIGN) Guideline #136.