Abstract
Background
Regular follow-up after bariatric surgery is important to assess the clinical status. Various factors could influence retention (i.e., compliance with clinical follow-up). The present analysis tested the hypothesis that the distance from the center will influence clinical retention for adolescent bariatric surgery patients. Our aim was to determine whether the distance to the clinic, and other patient characteristics, would predict clinical follow-up compliance. The present study was conducted at a tertiary care, free-standing children’s hospital.
Methods
The Follow-up of Adolescent Bariatric Surgery (FABS) study is a single-center cohort study collecting demographic and clinical information. The subjects’ addresses were geocoded, and the distance to the clinic was calculated. A generalized estimating equations model was used to examine follow-up visit compliance.
Results
A total of 71 subjects underwent Roux-en-Y gastric bypass surgery (RYGB), with a mean body mass index of 59 kg/m2. The average distance to the clinic was 98 miles. Retention declined over time (6 mo, 94%; 1 yr, 89%; 2 yr, 69%; P < .01); however, distance was not associated with retention (P = .68). Age at surgery was inversely related to retention (P = .04).
Conclusion
Compliance with clinical follow-up decreased 1 and 2 years after RYGB in adolescents. The distance from the center was not associated with follow-up regimen compliance. However, increasing age was associated with decreased retention. Additional research should focus on determining the modifiable factors that influence retention.
Keywords: Bariatric surgery, Adolescent, Gastric bypass, Patient compliance, Geographic Information Systems
Obesity affects the health of millions in the United States. According to recent estimates, some 33.8% of adults and 16.9% of children/adolescents are considered obese [1,2]. Coinciding with the high prevalence of obesity and the associated health risks is the increasingly widespread adoption of weight loss surgery, especially among the youth. Estimates have pointed to a 3–5-fold increase in adolescent bariatric procedures performed during the early 2000s [3,4]. Despite their popularity, these procedures are not without risk. A recent synthesis of the adolescent bariatric data reported complication rates of 5.5–27%—estimates similar to those observed for adult populations [5]. Given the complication rates tied to weight loss procedures, the need for routine follow-up care is imperative. Indeed, inadequate follow-up visit compliance has been associated with postoperative complications [6]. Accordingly, the American Society for Metabolic and Bariatric Surgery guidelines state that bariatric programs must have a system in place to prevent, monitor, and manage complications [7]. However, few published studies have investigated the factors associated with follow-up visit compliance in the bariatric surgical population and all have focused on adult cohorts [8,9]. Therefore, we sought to explore follow-up visit compliance in an adolescent/ young adult bariatric population. This investigation focused on the relationship between compliance and basic patient characteristics, with an emphasis on the travel distance, given the broad catchment area of our clinical program. We hypothesized that a greater distance from the residence to the clinical center would be associated with poorer follow-up visit compliance.
Methods
Study population
The Follow-up of Adolescent Bariatric Surgery (FABS) study is a single-center, observational follow-up study of adolescents and young adults seeking surgical obesity treatment at a tertiary care, free-standing children’s hospital. Consecutive patients enrolled into FABS (all had undergone Roux-en-Y gastric bypass [RYGB]) from May 2001 to January 2007, whose 2-year follow-up window (i.e., 30 mo after surgery) had closed, were included in the present analysis. In addition to the basic demographic data, the anthropometric and other clinical measures were evaluated at 6 months after surgery and annually thereafter. The data were collected during routine clinic visits and/or abstracted from the clinical records. The FABS subjects received no financial incentive to return to the study site to participate in the FABS study, and the FABS research staff did not encourage or schedule follow-up study visits. Instead, the study only recorded the information obtained during clinic visits that were encouraged and scheduled by the bariatric clinical team. The institutional review board approved this research.
Geocoding
To evaluate the effect of the distance to the clinic on visit compliance, we geocoded each subject’s residence and clinical center using ArcView, version 9.2 (Environmental Systems Research Institute, Redlands, CA). We then calculated the distance between the geocoded location of each subject’s residence and the clinical center using the Great Circle method [10]. This metric determines the shortest straight-line distance between 2 points (i.e., geocoded x and y coordinates), accounting for the curvature of the earth.
Subject characteristics
The following descriptive characteristics were retrieved from the FABS database for the present analysis: age at surgery, gender, race, height, weight, insurance type (private, public), and year of surgery. The subjects were weighed and measured in light clothing and without shoes. The body weight was recorded using a digital scale (model 5002 Stand-on Scale, Scale Tronix, White Plains, NY), and the height was measured using a calibrated wall-mounted stadiometer (Ayrton Stadiometer, model S100, Ayrton, Prior Lake, MN). The body mass index (BMI) was calculated as the body weight in kilograms divided by the height in meters squared.
Outcome Measure
The typical clinical follow-up includes several assessments after surgery (2 wk, 6 wk, 3, 6, 9, 12, and 18 mo and then annually after discharge). However, the FABS study only recorded the designated milestone visits (6 and 12 mo and annually thereafter). Therefore, subject retention was defined as completion of the within-window FABS milestone clinic visits after RYGB. Such postoperative visits were defined as 6 months (range 3–9 mo), 1 year (range 9–18 mo), and 2 years (range 18–30 mo).
Statistical analysis
Descriptive statistics were generated to characterize the baseline subject attributes. The retention rates were calculated by the distance to the clinic and the follow-up visit. To assess the association between the demographic variables and the distance to the clinical center with subject retention, a generalized estimating equations model was performed. To account for within-subject correlations, an unstructured correlation structure was selected according to Akaike’s Information Criterion. Crude and adjusted odds ratios and 95% confidence intervals were generated. In addition to the distance from the clinical center, the following covariates were considered for inclusion into the model: age at surgery, gender, race, baseline BMI, insurance type, and year of surgery. All 2-way interactions were assessed. The covariates were retained in the final model when the changes in the estimates were ≥10%. P < .05 was considered statistically significant.
Results
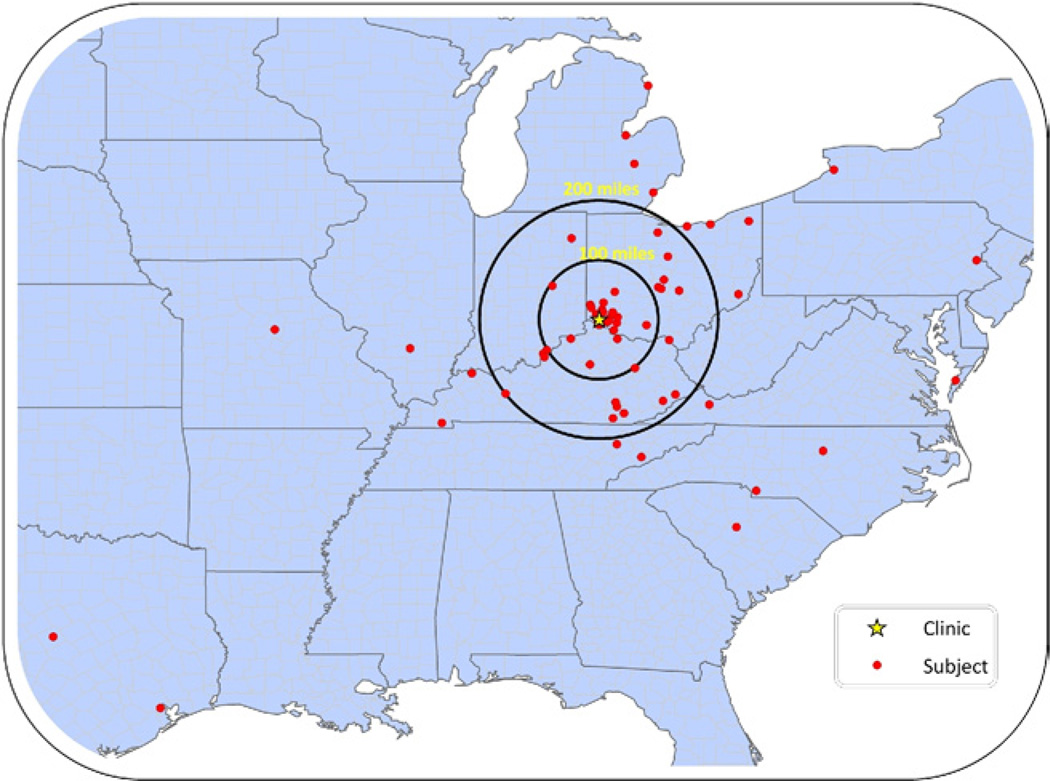
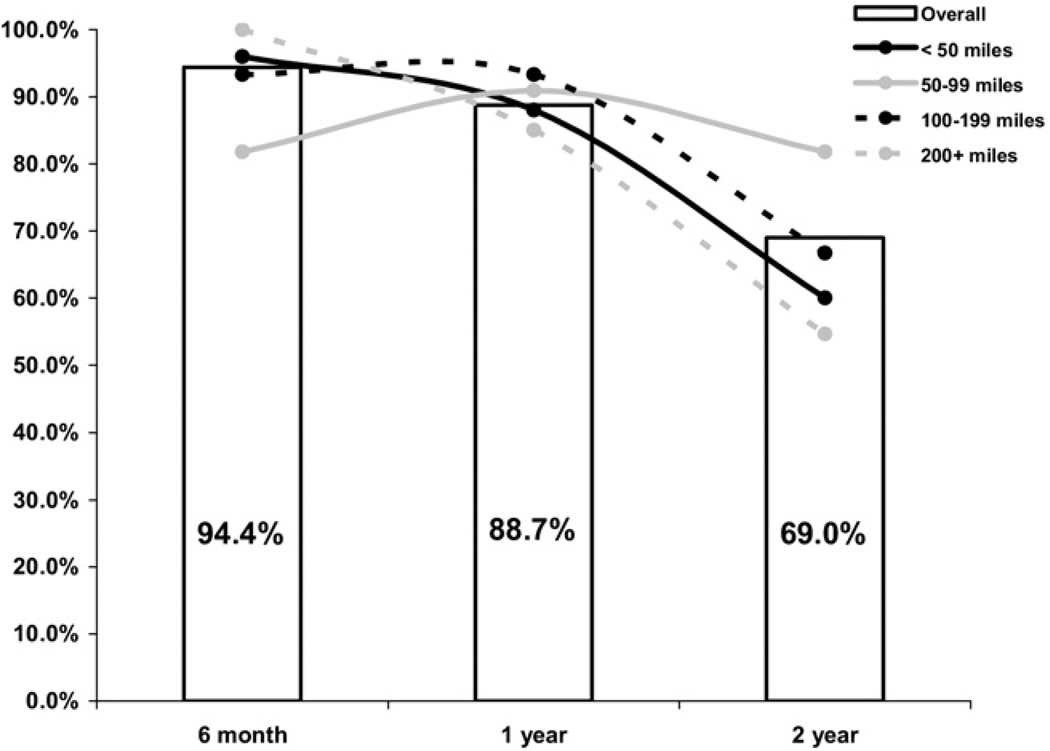
A total of 71 subjects met the inclusion criteria and were included in the present analysis. The baseline characteristics of the cohort are listed in Table 1. At baseline, the subjects had a mean BMI of 59.2 kg/m2, with nearly 70% of the cohort female and 87% self-identified as white. The mean age at surgery was 17.3 years. Most (59.6%) were covered by private health insurance, and none was self-pay. The subjects resided in 13 states, averaging 158 miles (median 98 miles, (range 2–913) from the clinic. More than one third (35.2%) lived <50 miles from the clinical center, and more than one quarter resided ≥200 miles away (Fig. 1). Overall, subject retention declined over time (P < .001), decreasing from 94.4% at 6 months to 88.7% at 1 year postoperatively and 69.0% 2 years after surgery. A crude assessment of the retention rates indicated negligible differences by distance to the clinic and follow-up visit (Fig. 2). The crude and adjusted odds ratios for follow-up visit completion are listed in Table 2. Adjusted analyses from the final model indicated the distance to the clinic was not associated with retention (P = .680), nor did this relationship vary by follow-up visit (distance × visit interaction, P = .672). However, patient age at surgery was inversely related to retention (P = .044). For each additional year of age at surgery, the odds of retention decreased by approximately 35% (odds ratio .64, 95% confidence interval .44 –.92). This surgical age–retention dynamic did not vary by follow-up visit (age × visit interaction, P = .306). The baseline BMI, gender, race, insurance type, and year of surgery did not significantly affect retention.
Table 1.
Subject characteristics
| Characteristic | Value |
|---|---|
| Age at surgery (yr) | |
| Mean ± SD | 17.3 ± 1.99 |
| Range | 13–23 |
| Age group (yr) | |
| 13–15 | 26.7% (19) |
| 16–17 | 42.3% (30) |
| ≥18 | 31.0% (22) |
| Gender | |
| Male | 31.0% (22) |
| Female | 69.0% (49) |
| Race | |
| White | 87.3% (62) |
| Black | 12.7% (9) |
| Distance from clinic (miles) | |
| Mean ± SD | 157.9 ± 181.36 |
| Range | 2–913 |
| Distance group (miles) | |
| <50 | 35.2% (25) |
| 50–99 | 15.5% (11) |
| 100–199 | 21.1% (15) |
| ≥200 | 28.2% (20) |
| Baseline BMI (kg/m2) | |
| Mean ± SD | 59.2 ± 11.46 |
| Range | 41–95 |
| BMI group (kg/m2) | |
| <50 | 18.3% (13) |
| 50–59 | 42.3% (30) |
| ≥60 | 39.4% (28) |
| Insurance | |
| Private | 58.6% (41) |
| Public | 41.4% (29) |
| Year of surgery | |
| 2001–2002 | 9.9% (7) |
| 2003 | 25.4% (18) |
| 2004 | 29.6% (21) |
| 2005 | 21.1% (15) |
| 2006–2007 | 14.0% (10) |
SD = standard deviation; BMI = body mass index.
Data in parentheses are numbers.
Fig. 1.
Location of subject’s residence and clinical center.
Fig. 2.
Retention by follow-up visit and distance to clinic.
Table 2.
Association between distance to clinic and other characteristics with follow-up visit compliance
| Crude model | Full model* | Final model | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | OR | 95% CI | P value | |
| Follow-up visit | <.001 | <.001 | <.001 | ||||||
| 6 mo (referent) | |||||||||
| 1 yr | .55 | .22–1.32 | .51 | .21–1.29 | .51 | .21–1.26 | |||
| 2 yr | .13 | .05–.37 | .11 | .04–.31 | .11 | .04–.30 | |||
| Age at surgery | .76 | .60–.97 | .075 | .65 | .45–.93 | .046 | .64 | .44–.92 | .044 |
| Gender | .359 | .287 | |||||||
| Male | 1.68 | .56–5.05 | 2.04 | .52–7.93 | |||||
| Female (referent) | |||||||||
| Race | .892 | .615 | |||||||
| White (referent) | |||||||||
| Black | 1.09 | .32–3.77 | .54 | .08–3.52 | |||||
| Distance from clinic (miles) | .872 | .587 | .680 | ||||||
| <50 (referent) | |||||||||
| 50–99 | 1.17 | .26–5.32 | .86 | .13–5.56 | .72 | .12–4.53 | |||
| 100–199 | .91 | .29–2.86 | .46 | .12–1.78 | .51 | .14–1.83 | |||
| ≥200 | 1.42 | .51–3.97 | .46 | .11–1.87 | .55 | .16–1.93 | |||
| Baseline BMI | 1.01 | .97–1.05 | .776 | 1.00 | .96–1.05 | .875 | |||
| Insurance | .979 | .795 | |||||||
| Private (referent) | |||||||||
| Public | 1.01 | .43–2.40 | .86 | .27–2.68 | |||||
| Year of surgery | .438 | .582 | .451 | ||||||
| 2001–2003 | .85 | .25–2.91 | 1.54 | .35–6.83 | 1.92 | .42–8.78 | |||
| 2004 | 1.93 | .56–6.66 | 2.69 | .51–14.14 | 3.25 | .65–16.28 | |||
| 2005 | .96 | .25–3.66 | .97 | .26–3.70 | 1.20 | .30–4.89 | |||
| 2006–2007 (referent) | |||||||||
OR = odds ratio; CI = confidence interval; BMI = body mass index.
Full model included all variables listed in Table 2.
Discussion
The present investigation represents the first assessment of factors influencing follow-up visit compliance in a predominantly adolescent bariatric surgical cohort. We found that compliance with designated follow-up visits declined significantly over time—a result that was not entirely unexpected, given the compliance of adolescents with clinical follow-up recommendations from other pediatric chronic diseases [11,12]. Our surgical weight loss program draws patients from great distances, leading us to investigate the effect of travel distance on compliance with the follow-up visits. We hypothesized that a greater travel distance from the patient’s residence to our center would result in poorer follow-up compliance. However, our results indicated such distances had no significant effect on the completion of visits ≤2 years after surgery. These findings are consistent with those from Zeller et al. [13], who reported that distance was not associated with attrition from a pediatric weight management program. In contrast, our findings diverged from adult bariatric results. Lara et al. [8] evaluated the effect of travel distance on follow-up compliance in adults after RYGB. At 1 year after surgery, they found that adults <50 miles from clinic had a nearly threefold greater odds of visit compliance compared with those >50 miles away [8].
Our results pointed to a significant inverse relationship between age at surgery and compliance, a finding also noted in pediatric solid organ transplantation recipients [12]. In our population, follow-up declined for each age group (age 13–15 yr, 100%, 95%, and 84%; age 16 –17 yr, 97%, 90%, and 70%; and age ≥18 yr, 86%, 82%, and 55% at 6, 12, and 24 mo, respectively). Furthermore, the results from our model indicated that each added year of age at surgery translated into a 35% decreased odds of follow-up visit completion through 2 years postoperatively. In contrast, analyses of adult bariatric populations have either found no association with age or increasing odds of compliance with age [8,9]. A few possibilities exist that could explain the inverse relationship in adolescents. First, as adolescents age out of parental health insurance coverage, clinical visits become a financial burden, thereby introducing a prominent barrier to care. Similarly, as these subjects gain independence with increased age, they could be less likely to remain in compliance than when under the supervision and direction of their parents or guardians.
Our results also differed from other measures associated with compliance in bariatric adult cohorts. Wheeler et al. [9] reported that an increasing BMI at baseline resulted in a decreased odds of compliance through 90 days postoperatively; however, we did not observe such an association (P = .875). Jelalian et al. [14] found that parental BMI predicted attrition in an adolescent weight control program. However, we did not collect parental BMI values from our cohort. Lara et al. [8] reported that males were significantly more compliant than were females at 12 months; however, our results did not point to any gender differences. Although inadequate power is a possible explanation for the lack of effect of demographic variables in our study, it is also not unreasonable to speculate that adults and adolescents actually differ in this regard. Studies with larger sample sizes, such as the Teen-Longitudinal Assessment of Bariatric Surgery [15], are needed to confirm our findings.
The strengths of the present investigation primarily relate to the data source used. Consecutive adolescent patients undergoing RYGB were included in our analysis, minimizing the potential effect of selection bias. The moderately large sample size (n = 71) was also a strength of our study, given that many adolescent bariatric outcome studies published to date have had smaller sample sizes. However, the present study had several limitations. First, our investigation used data that were, in part, retrospectively collected from clinical records. However, among the variables used in the present analysis, no values were missing. Also, only the baseline visit distance to the clinic was used. This method could have been limiting in the event a subject had moved during the 2 years after surgery. This is particularly relevant for adolescents who might move away for college, work, and so forth. In this population, more than one-quarter (27%) were <18 years old at 2 years after surgery, reducing the likelihood of relocation by some level.
Additional research is clearly needed in this area to better define the problem and solutions. For instance, unlike noncompliance in pediatric transplantation programs in which allograft loss represents a very clear and measurable adverse outcome of noncompliance, adolescent bariatric programs have not yet been able to gauge the effect of noncompliance on important outcome measures. It will be important to begin assessing whether compliance with clinical follow-up in adolescent bariatric patients affects weight loss efficacy, long-term weight regain, adherence to vitamin intake, or the incidence of nutritional deficiencies as measured by blood tests. The challenge is measuring these key outcome variables in patients who are not able or willing to return to the clinic for follow-up. In this regard, 1 tactic that could be used for future research is to contract with research partners who are trained to conduct study visits at the participant’s home, a research practice used in epidemiologic studies [16]. Thus, one could measure the effect of compliance with in-person visits on outcomes, such as iron deficiency anemia, late weight regain, and quality of life. In the upcoming FABS funding cycle, this exact topic will be addressed.
Conclusion
The results from the present study suggest that age but perhaps not distance from the clinic influences compliance with the follow-up visits after surgery. This information could be useful as progress is made toward developing more individually tailored care paradigms in adolescent bariatric surgery. Comprehensive retention plans should include a variety of methods to maintain contact with and ensure appropriate medical and nutritional monitoring. It is likely that future care guidelines will incorporate new research findings regarding which postoperative health behaviors are most needed to ensure the best weight loss and medical outcomes. Knowledge of these behaviors and a willingness to share responsibility for long-term postoperative care with providers in the patient’s medical home will enable us to help patients succeed as they emerge into adulthood.
Acknowledgments
Support for the Follow-up of Adolescent Bariatric Surgery study provided by Ethicon Endo-Surgery (to T. H. Inge, primary investigator; IIS grant 15161).
Footnotes
Disclosures
The authors have no commercial associations that might be a conflict of interest in relation to this article.
References
- 1.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303:242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 3.Tsai WS, Inge TH, Burd RS. Bariatric surgery in adolescents: recent national trends in use and in-hospital outcome. Arch Pediatr Adolesc Med. 2007;161:217–221. doi: 10.1001/archpedi.161.3.217. [DOI] [PubMed] [Google Scholar]
- 4.Schilling PL, Davis MM, Albanese CT, Dutta S, Morton J. National trends in adolescent bariatric surgical procedures and implications for surgical centers of excellence. J Am Coll Surg. 2008;206:1–12. doi: 10.1016/j.jamcollsurg.2007.07.028. [DOI] [PubMed] [Google Scholar]
- 5.Pratt JS, Lenders CM, Dionne EA, et al. Best practice updates for pediatric/adolescent weight loss surgery. Obesity (Silver Spring) 2009;17:901–910. doi: 10.1038/oby.2008.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Poole NA, Al Atar A, Kuhanendran D, et al. Compliance with surgical after-care following bariatric surgery for morbid obesity: a retrospective study. Obes Surg. 2005;15:261–265. doi: 10.1381/0960892053268499. [DOI] [PubMed] [Google Scholar]
- 7.Guidelines for Granting Privileges in Bariatric Surgery. [Accessed August 8, 2010];American Society for Metabolic and Bariatric Surgery. 2005 Available from: http://www.asbs.org/Newsite07/resources/asbs_granting_privileges.htm. [Google Scholar]
- 8.Lara MD, Baker MT, Larson CJ, Mathiason MA, Lambert PJ, Kothari SN. Travel distance age, sex as factors in follow-up visit compliance in the post-gastric bypass population. Surg Obes Relat Dis. 2005;1:17–21. doi: 10.1016/j.soard.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 9.Wheeler E, Prettyman A, Lenhard MJ, Tran K. Adherence to outpatient program postoperative appointments after bariatric surgery. Surg Obes Relat Dis. 2008;4:515–520. doi: 10.1016/j.soard.2008.01.013. [DOI] [PubMed] [Google Scholar]
- 10.Linking SAS analytics, U.S. Gazetteer data, and ArcView geocoding software for Medicare fraud screening. [Accessed August 18, 2010];2006 Available from: http://www.nesug.org/proceedings/nesug06/dm/da20.pdf. [Google Scholar]
- 11.Dietz E, Ga C, Chung SE, et al. Adherence to scheduled appointments among HIV-infected female youth in five U.S. cities. J Adolesc Health. 2010;46:278–283. doi: 10.1016/j.jadohealth.2009.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dew MA, Dabbs AD, Myaskovsky L, et al. Meta-analysis of medical regimen adherence outcomes in pediatric solid organ transplantation. Transplantation. 2009;88:736–746. doi: 10.1097/TP.0b013e3181b2a0e0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zeller M, Kirk S, Claytor R, et al. Predictors of attrition from a pediatric weight management program. J Pediatr. 2004;144:466–470. doi: 10.1016/j.jpeds.2003.12.031. [DOI] [PubMed] [Google Scholar]
- 14.Jelalian E, Hart CN, Mehlenbeck RS, et al. Predictors of attrition and weight loss in an adolescent weight control program. Obesity (Silver Spring) 2008;16:1318–1323. doi: 10.1038/oby.2008.51. [DOI] [PubMed] [Google Scholar]
- 15.Inge TH, Zeller M, Harmon C, et al. Teen-Longitudinal Assessment of Bariatric Surgery: methodological features of the first prospective multicenter study of adolescent bariatric surgery. J Pediatr Surg. 2007;42:1969–1971. doi: 10.1016/j.jpedsurg.2007.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Howard VJ, Cushman M, Pulley L, et al. The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology. 2005;25:135–143. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]