Abstract
This study’s objective was to examine the association of self-reported bilateral knee pain (KP) and back pain (BP) with health-related quality of life (HRQoL) among older adults. In this cross-sectional study, data for 1,252 older adults (≥65 years) were included from the Osteoarthritis Initiative project. Self-reported bilateral KP and BP were used to classify participants into four groups: i) neither bilateral KP nor BP; ii) no bilateral KP with BP; iii) bilateral KP without BP; and iv) both bilateral KP and BP. Health-related quality of life was measured using the health survey short form (SF)-12. We used multiple linear regression analyses to examine the associations of bilateral KP and/or BP with the HRQoL. After controlling for covariates, bilateral KP and BP were associated with poorer HRQoL [physical composite scale (PCS): estimated average (β) = −13.1, SE = 1.15, p <0.0001; mental composite scale (MCS): β = −2.71, SE = 1.09, p = 0.013, respectively] compared to the group with neither bilateral KP nor BP. In conclusion, older adults with coexisting bilateral KP and BP had significantly poorer physical and mental HRQoL when compared to peers without these conditions.
Keywords: back pain, knee pain, older adults, quality of life
Introduction
Knee pain (KP) and back pain (BP) are major public health issues that cause functional limitations and disability in older adults [1]. Knee pain and BP prevalence increase with age, affecting more than half of people that are 65 years and older [2]. Knee pain and BP can be caused by a weakened bone structure, quadriceps weakness and changes in the structure and function of the body as a result of the aging process [3]. With the rapid growth of the older adult population, prevalence of KP and BP is expected to increase dramatically [4]. The impact of KP and BP on health-related quality of life (HRQoL) might differ according to age, which has not been evaluated previously [5].
Hirano et al. [6] demonstrated that individuals reporting knee and back pain had a significantly lower QoL. Similarly, Muraki et al. [7, 8] used a large population from the Research on Osteoarthritis Against Disability (ROAD) study to show the same negative association between knee and back pain with QoL. However, both studies examined the independent association of unilateral knee pain and back pain with QoL and did not test the effect of the simultaneous presence of the two conditions on the HRQoL. Furthermore, previous studies that compared KP’s and BP’s have disagreed on their relative importance and effect on HRQoL [7-9].
Comparing the combined influence of BP and KP to the individual influence of each one has not been studied before, which would offer further insight into the difference between regional pain versus specific pain impact. This is important to guide clinical practices and direct available resources to those most at need. The aim of the present study was to test the hypothesis that self-reported bilateral KP and BP are associated with a poorer HRQoL in older adults.
Methods
Participants and Procedure
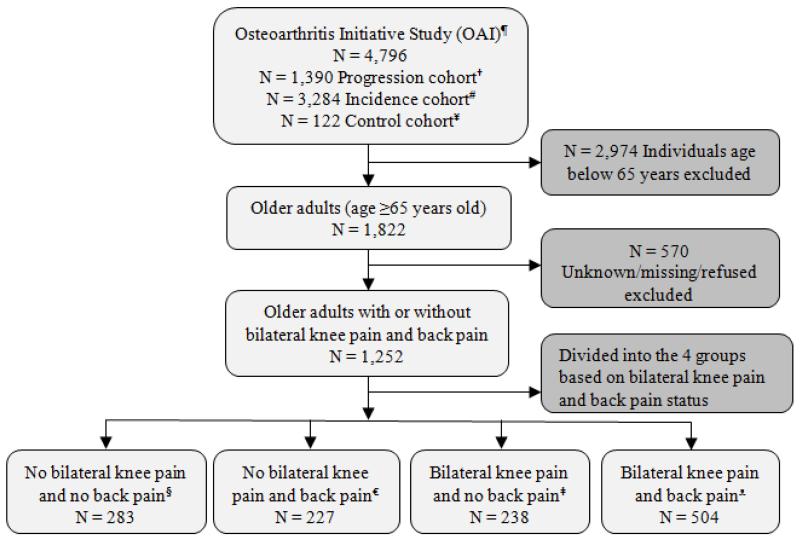
The data from the Osteoarthritis Initiative (OAI) (version 0.2.2, May 2009) were used for this study, which is available for public access at http://www.oai.ucsf.edu/. The OAI is an ongoing multicenter, longitudinal, prospective study to investigate the impact of knee osteoarthritis over time. Participants who aged ≥65 years were included and those with missing data were excluded (Figure 1).
Figure 1.
Flow diagram of selection and classification of participants enrolled in the Osteoarthritis Initiative study
¶OAI, online database provided by coordinating center, University of California, San Francisco (http://oai.epi-ucsf.org/datarelease/)
†Subjects with symptomatic tibiofemoral knee osteoarthritis at baseline.
#Subjects with no symptomatic tibiofemoral osteoarthritis in either knee at baseline.
¥Subjects with no pain, aching, or stiffness in either knee in the past year, no radiographic finding of osteoarthritis, and no eligibility risk factors.
§No pain in both knees with no back pain.
€No pain in both knees with back pain.
‡Pain in both knees without back pain.
ᴥPain in both knees and back pain.
Measures
Self-reported bilateral KP was assessed using the following question, repeated for each body side: “Now think about the past 30 days. During the past 30 days, have you had any pain, aching or stiffness in your right/left knee?” Participants were classified as having bilateral KP if they answered “yes” to both questions. Similar questions have been used in previous longitudinal and population-based studies [10-12].
Self-reported back pain was assessed using the following question: “During the past 30 days, have you had any back pain?” A similar question has been used before in a population-based cohort study (i.e., ROAD) [8]. Based on the participants’ answers to these questions, they were grouped into four categories: neither bilateral KP nor BP; no bilateral KP with BP; bilateral KP without BP; and bilateral KP with BP.
HRQoL was assessed using the 12-item health survey short form (SF-12) [13], a generic index consisting of twelve items and two summary measures that describe a subject’s physical and mental HRQoL. The physical composite scale (PCS) and mental composite scale (MCS) scores range from 0 to 100, with higher values indicating a better HRQoL. Both the PCS and MCS have demonstrated a good discriminatory value for the assessment of HRQoL in older adults [14].
Study Design
The current study used cross-sectional data from the OAI baseline. The data were collected from four clinical sites (Baltimore, Maryland; Columbus, Ohio; Pittsburgh, Pennsylvania; and Pawtucket, Rhode Island).
Data analysis
We performed ANOVA for continuous variables and the chi-squared test for categorical variables to examine differences among the four groups. To estimate the strength of the association of bilateral KP and BP with the results of the SF-12, we performed multiple linear regression analyses with the HRQoL as the outcome variable. The assumptions of homoscedasticity, linearity and normality were tested and met. The presence of KP and/or BP was used as the exposure variable, with the participants without pain (neither KP nor BP) serving as the reference group. To address the potential for confounding in the assessment of the association of bilateral KP and BP with the SF-12 results, we composed 3 models. Model 1 examined the unadjusted relationship. Model 2 included sociodemographic variables (i.e., age, sex, race, education and income) and Model 3 included comorbidity and BMI in addition to the variables included in Model 2. All analyses were performed using the SAS, version 9.2 (SAS Institute, Cary, NC, USA) with a significance level of 0.05.
Results
The mean age of the 1,252 participants included in the study was 71.2 ± 3.9 years. Of those, 59% were women, 84% were Caucasians, and 79% had high school education or more. The participants with bilateral KP and BP presented with significantly higher BMI, were more likely to have depressive symptoms, and had lower physical and mental HRQoL than the group with neither KP nor BP (Table 1).
Table 1.
Characteristics of all study participants, stratified by self-reported bilateral knee pain and back pain (N = 1,252)
| Characteristics, n% | ALL Sample N = 1,252 |
No bilateral knee pain and no back pain N = 283 (23%) |
No bilateral knee pain and back pain N = 227 (18%) |
Bilateral knee pain and no back pain N = 238 (19%) |
Bilateral knee and back pain 504 (40%) |
P value |
|---|---|---|---|---|---|---|
| Sex | 0.16 | |||||
| Men | 511 (41) | 128 (45) | 95 (42) | 100 (42) | 188 (37) | |
| Women | 741 (59) | 155 (55) | 132 (58) | 138 (58) | 316 (63) | |
| Race | <0.0001 | |||||
| White/Caucasians | 1,057 (84) | 258 (91) | 204 (90) | 190 (80) | 405 (80) | |
| Others (Blacks/Asians/non- whites) |
195 (16) | 25 (9) | 23 (10) | 48 (20) | 99 (20) | |
| Education | 0.60 | |||||
| <High school | 266 (21) | 59 (21) | 42 (18) | 56 (24) | 109 (22) | |
| ≥High school | 986 (79) | 224 (79) | 185 (82) | 182 (76) | 395 (78) | |
| Income per year in US dollars($) | 0.067 | |||||
| <$50,000 | 620 (50) | 124 (44) | 107 (47) | 129 (54) | 260 (52) | |
| >$50,000 | 632 (50) | 159 (56) | 120 (53) | 109 (46) | 244 (48) | |
| Co-morbidity | 0.08 | |||||
| ≥1 | 389 (31) | 82 (29) | 61 (27) | 69 (29) | 327 (65) | |
| 0 | 863 (69) | 201 (71) | 166 (73) | 169 (71) | 177 (35) | |
| Depressive symptoms (CESD) | 0.010 | |||||
| Yes | 78 (6) | 8 (3) | 12 (5) | 23 (10) | 35 (7) | |
| No | 1,174 (94) | 275 (97) | 215 (95) | 215 (90) | 469 (93) | |
|
| ||||||
| Characteristics, mean ± SD | ||||||
|
| ||||||
| Age in years | 71.3 ± 3.9 | 71.6 ± 4.0 | 71.8 ± 4.0 | 71.3 ± 3.7 | 70.8 ± 4.0 | 0.0025 |
| BMI (kg/m2) | 28.0 ± 4.1 | 27.4 ± 3.9 | 27.5 ± 4.0 | 28.3 ± 4.2 | 28.8 ± 4.6 | <0.0001 |
|
| ||||||
| Self-reported quality of life, mean ± SD | ||||||
|
| ||||||
| SF-12, PCS | 48.5 ± 7.9 | 53.0 ± 6.0 | 49.6 ± 7.3 | 46.1 ± 8.9 | 45.4 ± 9.4 | <0.0001 |
| SF-12, MCS | 55.3 ± 6.8 | 56.2 ± 5.6 | 55.3 ± 6.4 | 55.3 ± 7.5 | 54.6 ± 7.9 | 0.028 |
Abbreviations: BMI, body mass index; PCS, physical composite scale; MCS, mental composite scale; SD, standard deviation; CESD, Center for Epidemiological Studies Depression Scale; SF-12, Medical health survey short form-12.
The multiple linear regression analyses for the association of bilateral KP and BP with the SF-12 results are presented in Tables 2 and 3 for PCS and MCS, respectively. For the three groups with pain, a significant negative relationship with PCS was found in the unadjusted and adjusted analyses, but only the group with both bilateral KP and BP had a significant negative association with the MCS under all models. Under the unadjusted analyses (Model 1), participants with “BP only” showed the weakest negative association (better HRQoL) [PCS (β = −6.8); MCS (β = −1.92)], whereas participants in the group with both bilateral KP and BP showed the strongest negative association (worst HRQoL) [PCS (β = −15.3); MCS (β = −3.19)], compared with the group with neither KP nor BP. Similarly, after controlling for comorbidity and BMI) along with the other covariate variables in, the participants with BP demonstrated the weakest negative association (better HRQoL) [PCS (β = −6.7); MCS (β = −1.39)], while the participants with both conditions demonstrated the strongest negative association (worst HRQoL) [PCS (β = −13.1); MCS (β = −2.71)]. The covariates that showed significant association with PCS were age, race, income, and comorbidity, while only income was associated with MCS. In the model containing all covariates, the R2 for PCS increased from 0.16 to 0.28 and that for MCS increased from 0.01 to 0.04 under all models.
Table 2.
Multiple linear regression analysis on physical composite scale (PSC), stratified by self-reported bilateral knee pain and back pain (N = 780)
| Predictor variable | Model #1 N = 780 β |
SE | β | Model #2 N = 780 SE |
β | Model #3 N = 780 SE |
|---|---|---|---|---|---|---|
| Intercept | 45.4* | 0.37 | 63.0* | 5.25 | 70.7* | 5.78 |
|
| ||||||
| Four groups based on bilateral knee pain and back pain | ||||||
|
| ||||||
| 1. No bilateral knee and no back pain | Reference | Reference | Reference | |||
| 2. No bilateral knee pain and back pain | −6.8* | 1.19 | −6.7* | 1.17 | −6.7* | 1.15 |
| 3. Bilateral knee pain and no back pain | −13.8* | 1.32 | −13.3* | 1.32 | −12.8* | 1.30 |
| 4. Bilateral knee and back pain | −15.3* | 1.25 | −14.5* | 1.23 | −13.2* | 1.19 |
| R 2 | 0.16 | 0.21 | 0.28 | |||
Abbreviations: β, estimate; SE, standard error.
Model 1: unadjusted.
Model 2 included age, sex, race, education, and income.
Model 3 included Model 2 plus comorbidity and BMI.
p <.0001.
Table 3.
Multiple linear regression analysis on mental composite scale (MSC), stratified by self-reported bilateral knee pain and back pain (N = 780)
| Predictor variable | Model #1 N = 780 β |
SE | β | Model #2 N = 780 SE |
β | Model #3 N = 780 SE |
|---|---|---|---|---|---|---|
| Intercept | 54.6* | 0.32 | 56.3* | 4.60 | 51.8* | 5.29 |
|
| ||||||
| Four groups based on bilateral knee pain and back pain | ||||||
|
| ||||||
| 1. No bilateral knee and no back pain | Reference | Reference | Reference | |||
| 2. No bilateral knee pain and back pain | −1.92 | 1.07 | −1.80 | 1.07 | −1.91 | 1.06 |
| 3. Bilateral knee pain and no back pain | −1.76 | 1.17 | −0.99 | 1.17 | −1.20 | 1.17 |
| 4. Bilateral knee and back pain | −3.19** | 1.07 | −2.63** | 1.08 | −2.71** | 1.09 |
| R 2 | 0.011 | 0.037 | 0.041 | |||
Abbreviations: β, estimate; SE, standard error.
Model 1: unadjusted.
Model 2 included age, sex, race, education, and income.
Model 3 included Model 2 plus comorbidity and BMI.
p <.0001
p <.05.
Discussion
The aim of the current study was to examine the association of self-reported bilateral KP and BP with HRQoL among older adults (ages ≥65 years). In support of our hypothesis, we found that self-reported bilateral KP and BP were significantly associated with poorer physical and mental HRQoL after accounting for all covariates.
We used the generic SF-12 questionnaire to capture the physical and mental aspects of the HRQoL of the study participants [15]. Both conditions (bilateral KP and BP) were associated with a reduced HRQoL compared with the control group who had neither KP nor BP. Among the participants with pain, the physical HRQoL scores were worst for those with both bilateral KP and BP followed by bilateral KP only and then by BP only. The PCS score for the participants with bilateral KP was significantly lower than that for BP alone. These results are in agreement with a recent Korean study [9] and differ from those of the ROAD study, which reported that the negative association of back pain with HRQoL was greater than that for knee pain in almost all of the quality of life domains in Japanese men and women [7, 8]. Cultural differences in addition to different age groups have been suggested as reasons for such discrepancy [9].
According to our data, the participants with both conditions showed significantly poorer MCS scores than participants who had neither KP nor BP, even after the adjustment for all covariates. No association with the MCS was observed for the bilateral KP group or the BP group. The difference in MCS scores among our subjects suggests that the widespread pain in joints and back impacted areas beyond physical function. The results from the Epidemiology of Functional Disorders (EPIFUND) study found poorer mental health and a greater risk for anxiety and depression in participants with both joint and back pain than in participants with neither joint nor back pain [16]. They reported that poor psychosocial status has repeatedly been identified as a risk marker for the widespread pain in the joints and back.
Consistent with our findings, Cho et al. [17] and McBeth et al. [18] showed that the health status of participants with widespread pain in joints and the back was worse than that of participants without pain after adjustment for covariates, but the difference was only significant for physical functioning and the PCS scores of the SF-12. Hoogeboom et al. in cross-sectional [19] and longitudinal [20] studies showed that participants with joint pain had significantly worse SF-36 physical functioning scores and physical PCS than participants without joint pain.
We found that HRQoL was significantly associated with some demographic characteristics (i.e., age, race, and income) as well as comorbidity. These associations were in the expected direction and similar to other previous study [21]. Older age, non-white race, lower income, and the presence of comorbidity were associated with a poorer physical HRQoL. With regard to the association with mental HRQoL, although all associations were in the expected direction, only the negative association between lower income and MCS was statistically significant.
A better understanding of the relationship of bilateral KP and BP with physical and mental HRQoL is necessary to develop effective prevention and intervention programs to reduce the potential permanent disability and direct available resources to those most at risk [22]. In fact, HRQoL could be better targeted if patients are categorized into groups with similar characteristics and prognosis. For example, if future studies confirm that older adults with both KP and BP show reduced physical and mental functions than others, then additional attention and resources should be devoted to developing specific educational and training programs to aid this subpopulation and their caregivers in managing their health conditions and to improve their HRQoL [23]. Furthermore, if researchers consider these differences, they would be better equipped to evaluate patients’ outcomes and tailor interventions for the benefit of the patients as well as the society. The finding that widespread pain has significant impact beyond physical function is important for caregivers and therapists who treat these patients. They need to be aware of this possible impact to treat patients accordingly or to refer them to other healthcare professionals to receive the required care. Compared with other chronic diseases, knee pain and BP showed a stronger negative impact on HRQoL [9]. The existence of these two conditions together could have devastating effect on HRQoL at the long term unless early management strategies are in place.
Our study has a few limitations. First, because the data used was cross-sectional, the negative associations of bilateral KP and/or BP with HRQoL should be interpreted cautiously and not be viewed as causal relationships [8]. Second, the self-reported nature of the key variables, i.e., bilateral KP and BP, might resulted in imprecise answers and, therefore, there is a small chance patients were misclassified, which might limit the ability to generalize the current findings [24]. Third, we excluded participants aged ≤64 years, which may limit the validity of the study for younger subjects [7]. Finally, wide groups were used here to categorize race variable (white vs. non-white), so some specific racial groups might have been masked.
Conclusions
Older adults with self-reported bilateral KP and BP demonstrated a poorer HRQoL, compared with those who did not have neither KP nor BP. Self-reported bilateral KP and BP were significantly associated with decreased scores for the physical and mental components of the SF-12 after adjusting for potential covariates. Future longitudinal research is necessary to examine how HRQoL changes over time and its relation to other clinical outcomes.
Acknowledgement
The authors extend their appreciation to the Research Centre, College of Applied Medical Sciences and the Deanship of Scientific Research at King Saud University for funding this research.
Footnotes
Conflict of interest statement
The authors declare that they have no conflicts of interest
References
- 1.Symmons DP. Knee pain in older adults: the latest musculoskeletal “epidemic”. Ann Rheum Dis. 2001;60:89–90. doi: 10.1136/ard.60.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hartvigsen J, Christensen K, Frederiksen H. Back pain remains a common symptom in old age. a population-based study of 4486 Danish twins aged 70-102. Eur Spine J. 2003;12:528–534. doi: 10.1007/s00586-003-0542-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Molton IR, Terrill AL. Overview of persistent pain in older adults. Am Psychol. 2014;69:197–207. doi: 10.1037/a0035794. [DOI] [PubMed] [Google Scholar]
- 4.Muraki S, Oka H, Akune T, Mabuchi A, En-yo Y, Yoshida M, Saika A, Suzuki T, Yoshida H, Ishibashi H, Yamamoto S, Nakamura K, Kawaguchi H, Yoshimura N. Prevalence of radiographic knee osteoarthritis and its association with knee pain in the elderly of Japanese population-based cohorts: the ROAD study. Osteoarthritis Cartilage. 2009;17:1137–1143. doi: 10.1016/j.joca.2009.04.005. [DOI] [PubMed] [Google Scholar]
- 5.Mannion AF, Elfering A, Staerkle R, Junge A, Grob D, Semmer NK, Jacobshagen N, Dvorak J, Boos N. Outcome assessment in low back pain: how low can you go? Eur Spine J. 2005;14:1014–1026. doi: 10.1007/s00586-005-0911-9. [DOI] [PubMed] [Google Scholar]
- 6.Hirano K, Imagama S, Hasegawa Y, Ito Z, Muramoto A, Ishiguro N. Impact of low back pain, knee pain, and timed up-and-go test on quality of life in community-living people. J Orthop Sci. 2014;19:164–171. doi: 10.1007/s00776-013-0476-0. [DOI] [PubMed] [Google Scholar]
- 7.Muraki S, Akune T, Oka H, En-Yo Y, Yoshida M, Saika A, Suzuki T, Yoshida H, Ishibashi H, Tokimura F, Yamamoto S, Nakamura K, Kawaguchi H, Yoshimura N. Health-related quality of life in subjects with low back pain and knee pain in a population-based cohort study of Japanese men: the Research on Osteoarthritis Against Disability study. Spine (Phila Pa 1976) 2011;36:1312–1319. doi: 10.1097/BRS.0b013e3181fa60d1. [DOI] [PubMed] [Google Scholar]
- 8.Muraki S, Akune T, Oka H, En-Yo Y, Yoshida M, Saika A, Suzuki T, Yoshida H, Ishibashi H, Tokimura F, Yamamoto S, Nakamura K, Kawaguchi H, Yoshimura N. Impact of knee and low back pain on health-related quality of life in Japanese women: the Research on Osteoarthritis Against Disability (ROAD) Mod Rheumatol. 2010;20:444–451. doi: 10.1007/s10165-010-0307-5. [DOI] [PubMed] [Google Scholar]
- 9.Kim W, Jin YS, Lee CS, Bin SI, Lee SY, Choi KH. Influence of Knee Pain and Low Back Pain on the Quality of Life in Adults Over Age Fifty. PM&R. 2015 doi: 10.1016/j.pmrj.2015.03.002. [DOI] [PubMed] [Google Scholar]
- 10.Creamer P, Lethbridge-Cejku M, Costa P, Tobin JD, Herbst JH, Hochberg MC. The relationship of anxiety and depression with self-reported knee pain in the community: data from the Baltimore Longitudinal Study of Aging. Arthritis Care Res. 1999;12:3–7. doi: 10.1002/1529-0131(199902)12:1<3::aid-art2>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 11.Blake VA, Allegrante JP, Robbins L, Mancuso CA, Peterson MG, Esdaile JM, Paget SA, Charlson ME. Racial differences in social network experience and perceptions of benefit of arthritis treatments among New York City Medicare beneficiaries with self-reported hip and knee pain. Arthritis Rheum. 2002;47:366–371. doi: 10.1002/art.10538. [DOI] [PubMed] [Google Scholar]
- 12.Bindawas SM, Vennu V, Al Snih S. Differences in health-related quality of life among subjects with frequent bilateral or unilateral knee pain: data from the Osteoarthritis Initiative study. J Orthop Sports Phys Ther. 2015;45:128–136. doi: 10.2519/jospt.2015.5123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Andresen EM, Meyers AR. Health-related quality of life outcomes measures. Arch Phys Med Rehabil. 2000;81:S30–45. doi: 10.1053/apmr.2000.20621. [DOI] [PubMed] [Google Scholar]
- 14.Younsi M, Chakroun M. Measuring health-related quality of life: psychometric evaluation of the Tunisian version of the SF-12 health survey. Qual Life Res. 2014 doi: 10.1007/s11136-014-0641-8. [DOI] [PubMed] [Google Scholar]
- 15.Der-Martirosian C, Kritz-Silverstein D, Barrett-Connor E. Five-year stability in associations of health-related quality of life measures in community-dwelling older adults: the Rancho Bernardo Study. Qual Life Res. 2010;19:1333–1341. doi: 10.1007/s11136-010-9700-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nicholl BI, Macfarlane GJ, Davies KA, Morriss R, Dickens C, McBeth J. Premorbid psychosocial factors are associated with poor health-related quality of life in subjects with new onset of chronic widespread pain - results from the EPIFUND study. Pain. 2009;141:119–126. doi: 10.1016/j.pain.2008.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cho NH, Kim I, Lim SH, Kim HA. Prevalence of widespread pain and its influence on quality of life: population study in Korea. J Korean Med Sci. 2012;27:16–21. doi: 10.3346/jkms.2012.27.1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McBeth J, Lacey RJ, Wilkie R. Predictors of new-onset widespread pain in older adults: results from a population-based prospective cohort study in the UK. Arthritis Rheumatol. 2014;66:757–767. doi: 10.1002/art.38284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hoogeboom TJ, den Broeder AA, Swierstra BA, de Bie RA, van den Ende CH. Joint-pain comorbidity, health status, and medication use in hip and knee osteoarthritis: a cross-sectional study. Arthritis Care Res (Hoboken) 2012;64:54–58. doi: 10.1002/acr.20647. [DOI] [PubMed] [Google Scholar]
- 20.Hoogeboom TJ, den Broeder AA, de Bie RA, van den Ende CH. Longitudinal impact of joint pain comorbidity on quality of life and activity levels in knee osteoarthritis: data from the Osteoarthritis Initiative. Rheumatology (Oxford) 2013;52:543–546. doi: 10.1093/rheumatology/kes314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mili F, Helmick CG, Moriarty DG. Health related quality of life among adults reporting arthritis: analysis of data from the Behavioral Risk Factor Surveillance System, US, 1996-99. J Rheumatol. 2003;30:160–166. [PubMed] [Google Scholar]
- 22. [Accessed March 30 2015];Health people 2020: Arthritis, Osteoporosis, and Chronic Back Conditions. 2014 Healthypeople.gov. https://www.healthypeople.gov/2020/topics-objectives/topic/Arthritis-Osteoporosis-and-Chronic-Back-Conditions#Ref-09.
- 23.Koh HK. A 2020 vision for healthy people. N Engl J Med. 2010;362:1653–1656. doi: 10.1056/NEJMp1001601. [DOI] [PubMed] [Google Scholar]
- 24.Miles TP, Flegal K, Harris T. Musculoskeletal disorders: time trends, comorbid conditions, self-assessed health status, and associated activity limitations. Vital Health Stat. 1993;3:275–288. [PubMed] [Google Scholar]