Abstract
Background
Most studies of depression and cardiovascular risk have been conducted in white populations. We investigated this association in a community-based cohort of African Americans.
Methods and Results
We used data from the Jackson Heart Study to investigate associations of baseline depressive symptoms between 2000 and 2004 with incident stroke and coronary heart disease over 10 years. We used Kaplan-Meier estimates and Cox proportional hazards models to assess cardiovascular event risk using 3 exposure variables: any depressive symptoms (CES-D score ≥ 16); none (score < 16), minor (score 16 to less than 21) and major depression (score ≥ 21); and Center for Epidemiologic Studies Depression (CES-D) score per 1 SD increase. Models were adjusted for a stroke or CHD risk score and behavioral risk factors. Of 3309 participants with no stroke history, 738 (22.3%) had baseline depressive symptoms. A similar proportion with no prior coronary heart disease had baseline depressive symptoms (21.8%). The unadjusted 10-year risk of stroke was similar among participants with any compared with no depressive symptoms (3.7% vs 2.6%; P = .12). Unadjusted CHD rates were higher among participants with depressive symptoms (5.6 % vs. 3.6 %; p=.03), and differences persisted after adjustment for clinical and behavioral risk factors but not after adjustment for coping strategies. In adjusted models comparing major vs no depressive symptoms, patients with major depressive symptoms had a twofold greater hazard of stroke (HR, 1.95; 95% CI, 1.02–3.71; P = .04). In continuous models, a 1 SD increase in CES-D score was associated with a 30% increase in adjusted incident stroke risk (P = .04). Similar associations were observed for incident CHD in models adjusted for clinical and behavioral risk factors, but associations were not significant after adjustment for coping strategies.
Conclusions
In a community-based cohort of African Americans, major depressive symptoms were associated with greater risks of incident stroke and coronary heart disease after adjustment for clinical and behavioral risk factors.
Keywords: cardiovascular diseases, depression, outcome assessment (health care)
Although depression has long been recognized as a common consequence of acute cardiovascular outcomes, it may also be an important risk factor for first-ever stroke and coronary heart disease. Prospective studies1–5 and meta-analyses6–8 have found positive associations between depressive symptoms and incident cardiovascular disease after adjustment for other psychosocial and physiological risk factors. Yet, most studies of depression and cardiovascular outcomes have been conducted in white populations. Knowledge about depression and cardiovascular outcomes in African Americans is limited, despite higher rates of severe and disabling clinical depression and a greater degree of undertreatment than in white populations.9 A recent analysis of the Chicago Health and Aging project found associations between a composite measure of psychological distress and stroke mortality and incidence among African American adults.10 However, this study was limited to adults older than 65 years. The link between depression and incident cardiovascular disease may be especially important in younger populations.1,11
The objectives of this study were to examine associations between depressive symptoms and incident stroke and coronary heart disease in a community-based cohort of African Americans. We hypothesized that baseline depressive symptoms are positively associated with adverse cardiovascular outcomes after adjustment for sociodemographic and clinical characteristics. A secondary hypothesis was that this association is attenuated after adjustment for behavioral risk factors, antidepressant medication use, and self-reported coping strategies.
Methods
Data Sources
We used data from the Jackson Heart Study, a community-based cohort study of African Americans in Jackson, Mississippi, designed to investigate risk factors for cardiovascular disease.12 The study enrolled 5301 participants aged 21 to 94 years from 4 populations: community volunteers from the Jackson metropolitan area (30%); randomly selected residents of Jackson (17%); participants in the Jackson site of the Atherosclerosis Risk in Communities (ARIC) cohort study13 (22%); and family members of Jackson Heart Study participants (31%). All participants underwent a baseline examination between 2000 and 2004 to collect data on demographic characteristics, socioeconomic characteristics, medical history, physical examination, laboratory values, cardiac test results, behavioral factors, and medications. Deaths and nonfatal events were ascertained via annual telephone calls, review of death certificates, and abstraction of medical records for relevant International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes through 2010. The Jackson Heart Study was approved by the institutional review boards of Jackson State University, Tougaloo College, the University of Mississippi Medical Center, and the Duke University Health System. All study participants gave written informed consent.
Study Population
We included all Jackson Heart Study participants who completed at least 16 of the 20 Center for Epidemiologic Studies Depression (CES-D) scale screening questions at baseline. We excluded participants who had a history of stroke at baseline (n = 234) from analyses of incident stroke and participants with a history of coronary heart disease (n = 425) from analyses of incident coronary heart disease. For models including self-reported coping strategies, we excluded 383 participants for stroke analysis and 367 in the coronary heart disease analysis.
Exposure Definition
We defined the presence of any depressive symptoms as a binary variable based on a score of 16 or higher on the CES-D at baseline.14 The score is the sum of the 20 questions with a possible range of 0 to 60. We further classified participants into major and minor depressive symptomatology for secondary analyses using the following CES-D cut points: minor (score of 16 to less than 21) and major (score of 21 or greater). We also examined CES-D score as a continuous variable in SD units, translated as CES-D score per 1 SD increase.
Outcome Ascertainment
Strokes and coronary heart disease (ie, myocardial infarction, fatal coronary heart disease, or cardiac procedure) were ascertained via directed patient queries during annual telephone follow-up and ongoing surveillance of hospitalizations, with subsequent transmission of hospital records and death certificates to a medical record abstraction unit for review. A computer-generated diagnosis with physician adjudication was used to classify hospitalized and fatal stroke and coronary heart disease events. We included all events that occurred within 10 years of the baseline examination date based on a median of 8 years of follow-up time and a 75th percentile of 10 years.
Covariates
Because of the low number of events relative to the number of potential confounding variables, we created a single composite risk score separately for stroke and coronary heart disease covariate adjustment to avoid biased regression estimates.15,16 We calculated a 10-year stroke risk score for each participant by fitting a separate incident stroke model on the entire Jackson Heart Study cohort with no prior stroke at baseline (5067 participants, 153 stroke events) using Cox proportional hazards regression. Regression variables included age, sex, body mass index, systolic blood pressure, dialysis, prior myocardial infarction, diabetes mellitus, hypertension, atrial fibrillation, left ventricular hypertrophy, history of cardiovascular disease, smoking history, antihypertensive medication use, and antithrombotic medication use. To ascertain left ventricular hypertrophy, we used a quantitative left ventricular mass measurement from echocardiography when available (missing for 35% of participants); otherwise, we ascertained left ventricular hypertrophy based on a qualitative assessment of mild, moderate, or severe. We then used the X-beta (∑ βjXj) from this model as a continuous stroke risk score variable. A similar process was used to create a 10-year coronary heart disease risk score among participants with no prior coronary heart disease at baseline (n = 4876 participants, 192 coronary heart disease events). For the incident coronary heart disease model, we included all variables in the stroke model except for prior myocardial infarction and history of cardiovascular disease, and added variables for total cholesterol, lipid-lowering medications, and prior stroke.
Mediating Variables
Hypothesized mediators of the association between depressive symptoms and cardiovascular outcomes included socioeconomic status (education level and annual family income); alcohol use (mean number of drinks per day); physical activity (mean number of activity hours per week); antidepressant use (alpha-2 receptor antagonists [tetracyclics], monoamine oxidase inhibitors, modified cyclics, selective serotonin reuptake inhibitors, tricyclic agents, and miscellaneous antidepressants); and self-reported coping strategies (engagement and disengagement subscale scores on the Coping Strategies Inventory-Short Form [CSI-SF]).17
Statistical Analysis
A copy of the a priori statistical analysis plan is provided in the Appendix. We tested for differences in the distribution of baseline characteristics by the presence of depressive symptoms at baseline using chi-square tests for categorical variables and Kruskal-Wallis tests for continuous variables. We used Kaplan-Meier methods to calculate the cumulative incidence of first stroke or incident coronary heart disease by the presence of depressive symptoms at baseline and tested for differences between the groups using log-rank tests. We estimated covariate-adjusted associations between depressive symptoms and cardiovascular outcomes using Cox proportional hazards models with censoring at the time of death, participant loss to follow-up, or the end of study event surveillance follow-up (December 31, 2011).
We examined associations for stroke and coronary heart disease separately using 3 depressive symptom variables: any depression (yes or no); depressive symptom category (none, minor, or major); and CES-D score per 1 SD increase. For each depression variable, we ran 5 sequential models: (1) an unadjusted model in which depression was the only variable; (2) a model that included adjustment for stroke or coronary heart disease risk score and socioeconomic status; (3) a model that included adjustment for stroke or coronary heart disease risk score, socioeconomic status, and behavioral risk factors; (4) a model that included adjustment for stroke or coronary heart disease risk score, socioeconomic status, behavioral risk factors, and antidepressant medication use; and (5) a model that included the adjustment for stroke or coronary heart disease risk score, socioeconomic status, behavioral risk factors, antidepressant use, and coping strategies. In model 5, we excluded participants who had missing data for any part of the CSI-SF. In all models, we tested the proportionality assumption for the depression variable by including an interaction variable for the interaction between the depression variable and log of survival time.
Because of the high proportion of participants who did not complete the CES-D, we examined the baseline characteristics of the study population by CES-D completion. For variables with low rates of missingness (less than 5% of records), we imputed continuous variables to the overall median value, dichotomous variables to “no,” and multichotomous variables to the most frequent categorical value.18 For variables with greater than 5% missingness (ie, medications and income), we treated missing values as a separate category.19,20 We used a 2-tailed α = .05 to establish statistical significance and calculated 95% CIs. We used SAS version 9.3 for all analyses (SAS Institute, Cary, North Carolina).
Results
Of 5301 participants in the Jackson Heart Study who completed the baseline examination, we excluded participants with prior stroke (n = 234) and additionally those with incomplete CES-D information (n = 1758) for the stroke analysis. Among 3309 participants in the final study cohort, 738 (22.3%) had depressive symptoms at baseline. Table 1 shows the distribution of baseline characteristics among participants with depressive symptoms at baseline and those without. (Supplemental Table 1 shows the baseline characteristics by major, minor, and no depressive symptoms). Participants who reported depressive symptoms were younger on average and were more likely to be women than those who did not. Participants with depressive symptoms were significantly more likely to have a history of cardiovascular disease, diabetes mellitus, heart failure, prior myocardial infarction, and zero hours of weekly physical activity and to be current smokers. Median body mass index and waist circumference were higher among participants with depressive symptoms. Antidepressant use was low among participants with depressive symptoms at baseline (11.4%). Participants who did not complete the CES-D were younger on average, were more likely to be men, and had lower levels of education than those who completed the CES-D (Supplemental Table 2).
Table 1.
Baseline Characteristics of the Study Population
| Characteristic | Depressive Symptoms |
P Value |
|
|---|---|---|---|
| No (n = 2571) |
Yes (n = 738) |
||
| Age, median (IQR), y | 54.3 (44.9–63.7) | 52.2 (42.9–63.0) | .003 |
| Women, No. (%) | 1627 (63.3) | 536 (72.6) | < .001 |
| Medical history, No. (%) | |||
| Atrial fibrillation | 4 (0.2) | 2 (0.3) | .52 |
| Cardiovascular disease | 127 (4.9) | 68 (9.2) | < .001 |
| Diabetes mellitus | 497 (19.3) | 170 (23.0) | .03 |
| Dialysis | 8 (0.3) | 5 (0.7) | .16 |
| Heart failure | 151 (5.9) | 78 (10.6) | < .001 |
| Hypertension | 1491 (58.0) | 451 (61.1) | .13 |
| Left ventricular hypertrophy | 178 (6.9) | 57 (7.7) | .46 |
| Myocardial infarction | 85 (3.3) | 51 (6.9) | < .001 |
| Physical examination, median (IQR) | |||
| Body mass index, kg/m2 | 30.5 (27.0–35.1) | 31.1 (27.1–36.5) | .02 |
| Systolic blood pressure, mm Hg | 124.0 (114.0–135.0) | 125.0 (114.0–136.0) | .30 |
| Waist circumference, cm | 98.0 (89.0–108.0) | 101.0 (89.0–111.0) | .01 |
| Socioeconomic characteristics, No. (%) | |||
| Education | < .001 | ||
| Less than high school | 284 (11.0) | 145 (19.6) | |
| High school graduate | 1014 (39.4) | 385 (52.2) | |
| College degree | 699 (27.2) | 139 (18.8) | |
| Graduate or professional degree | 574 (22.3) | 69 (9.3) | |
| Annual family income | < .001 | ||
| < $20,000 | 474 (18.4) | 258 (35.0) | |
| $20,000–$50,000 | 807 (31.4) | 233 (31.6) | |
| $50,000–$75,000 | 482 (18.7) | 88 (11.9) | |
| > $75,000 | 467 (18.2) | 48 (6.5) | |
| Missing | 341 (13.3) | 111 (15.0) | |
| Medications, No. (%) | |||
| Anticoagulant agent | 15 (0.6) | 8 (1.1) | .15 |
| Antidepressant agent | 106 (4.1) | 84 (11.4) | < .001 |
| Antihyperlipidemic agent | 295 (11.5) | 76 (10.3) | .37 |
| Antihypertensive agent | 733 (28.5) | 243 (32.9) | .02 |
| Antiplatelet agent | 22 (0.9) | 5 (0.7) | .64 |
| Antithrombotic agent (anticoagulant, antiplatelet, or cyclooxygenase-2 inhibitor) | 182 (7.1) | 85 (11.5) | < .001 |
| Cyclooxygenase-2 inhibitor | 147 (5.7) | 73 (9.9) | < .001 |
| Missing | 181 (7.0) | 64 (8.7) | .14 |
| Behavioral factors | |||
| Drinks per day in the prior year, median (IQR) | 0.2 (0.7) | 0.2 (0.9) | .96 |
| Hours of physical activity per week, No. (%) | < .001 | ||
| None | 1088 (42.3) | 383 (51.9) | |
| < 1 hour | 268 (10.4) | 83 (11.2) | |
| 1 to < 2 hours | 480 (18.7) | 115 (15.6) | |
| 2 to < 3 hours | 214 (8.3) | 64 (8.7) | |
| 3 to < 4 hours | 182 (7.1) | 33 (4.5) | |
| ≥ 4 hours | 339 (13.2) | 60 (8.1) | |
| Smoking history, No. (%) | < .001 | ||
| Never smoked | 1837 (71.5) | 471 (63.8) | |
| Former smoker | 486 (18.9) | 128 (17.3) | |
| Current smoker | 248 (9.6) | 139 (18.8) | |
| CSI-SF scores, median (IQR) | |||
| Disengagement score | 22.0 (20.0–25.0) | 25.0 (22.0–28.0) | < .001 |
| Engagement score | 29.0 (26.0–32.0) | 26.0 (23.0–29.0) | < .001 |
| Stroke risk scores, median (IQR) | |||
| Framingham stroke risk score | 5.0 (2.0–9.0) | 6.0 (3.0–10.0) | .007 |
| Internally derived stroke risk score | 4.9 (4.0, 5.7) | 4.9 (3.9, 5.9) | .30 |
Abbreviations: CSI-SF, Coping Skills Inventory-Short Form; IQR, interquartile range.
Of 5301 participants in the Jackson Heart Study who completed the baseline examination, we excluded participants with prior coronary heart disease (n = 425) and additionally those with incomplete CES-D information (n = 1698) from the incident coronary heart disease analysis. Among 3178 participants in the final study cohort, 692 (21.8%) had depressive symptoms at baseline. The distribution of baseline characteristics by depressive symptoms in the incident coronary heart disease cohort was similar to that of the incident stroke cohort (Supplemental Table 3 shows the baseline characteristics of the incident coronary heart disease cohort by depressive symptoms, and Supplemental Table 4 shows the baseline characteristics of the incident coronary heart disease cohort by major, minor, and no depressive symptoms).
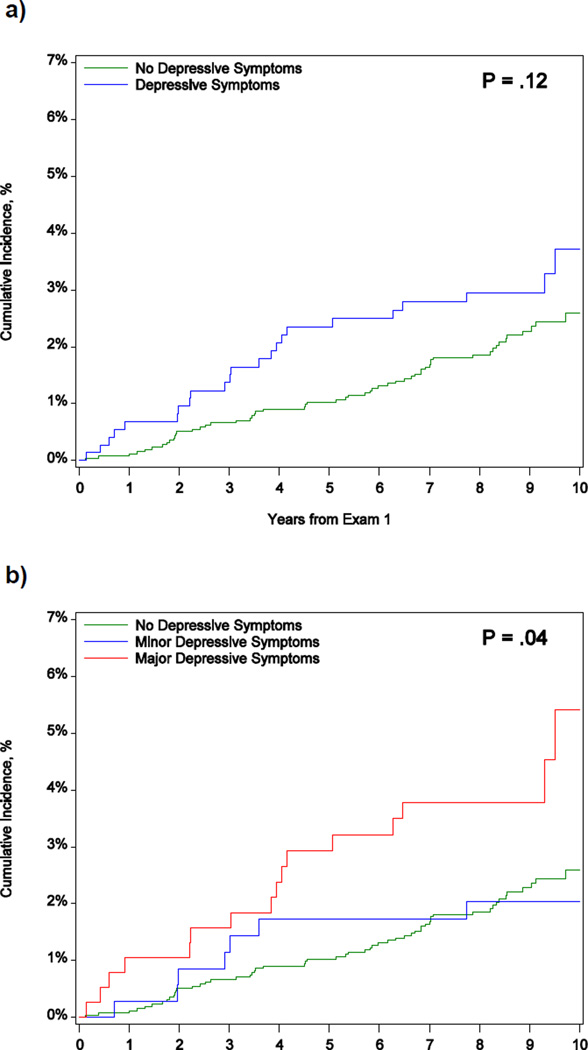
As shown in Figure 1, participants with depressive symptoms had higher cumulative incidence of stroke than those without. The unadjusted 10-year cumulative incidence of stroke was 3.7% (n=23 stroke events; 95% CI, 2.4%–5.8%; censoring rates: death [63 (8.5%)], loss to JHS surveillance [83 (11.2%)], less than 10 years follow-up [437 (59.2%)]) for participants with depressive symptoms and 2.6% (n=56 stroke events; 95% CI, 2.0%–3.4%; censoring rates: death [170 (6.6%)], loss to JHS surveillance [255 (9.9%)] and less than 10 years follow-up [1619 (63.0%)]) for those with no depressive symptoms (P = .12; Figure 1, panel a). When we stratified participants by minor and major depressive symptoms (Figure 1, panel b), the highest 10-year cumulative incidence rates of stroke were observed for participants with major depressive symptoms (5.4%; 95% CI, 3.1%–9.4%), followed by those with no depressive symptoms (2.6%; 95% CI, 2.0%–3.4%), and those with minor depressive symptoms (2.0%; 95% CI, 1.0%–4.3%; P = .04).
Figure 1.
Kaplan-Meier Curves for Incident Stroke Among Patients With and Without Depressive Symptoms at Baseline (Panel A) and With No, Minor, or Major Depressive Symptoms at Baseline (Panel B)
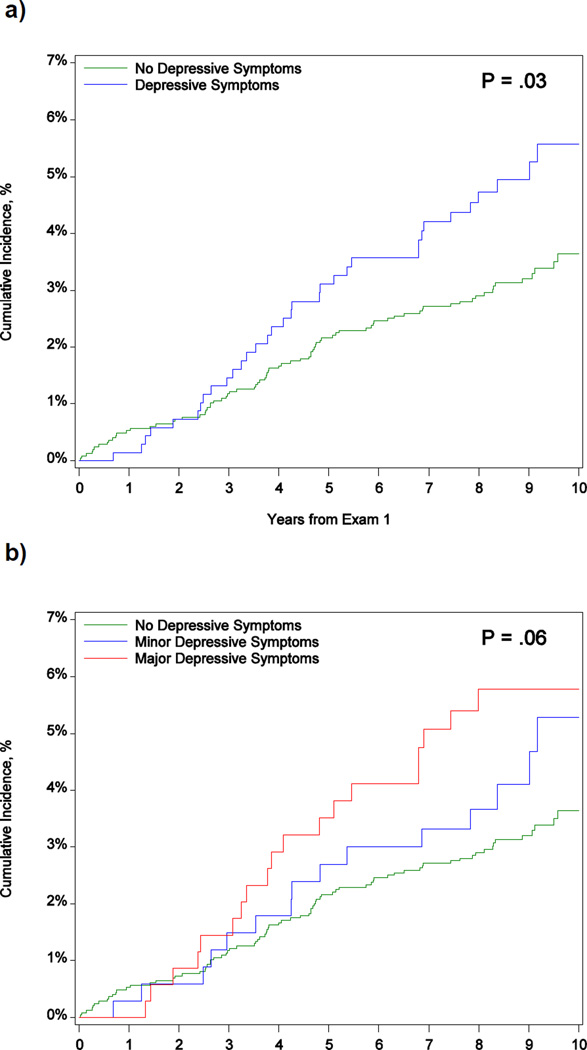
The unadjusted 10-year cumulative incidence of CHD was 5.6% (n=34 CHD events; 95% CI, 4.0%–7.8 %; censoring rates: death [52 (7.5%)], loss to JHS surveillance [79 (11.4%)] and less than 10 years follow-up [400 (57.8%)]) for participants with depressive symptoms and 3.6 % (n=79 stroke events; 95% CI, 2.9 %- 4.6 %; censoring rates: death [143 (5.8%)], loss to JHS surveillance [244 (9.8%)] and less than 10 years follow-up [1576 (63.4%)]) for those with no depressive symptoms (P = .03) (Figure 2, panel a). When we stratified participants by minor and major depressive symptoms, the highest 10-year cumulative incidence rates of CHD were observed for participants with major depressive symptoms (5.8 %; 95% CI, 3.7 %– 9.0 %), followed by those with minor depressive symptoms (5.3 %; 95% CI, 3.2 %- 8.8 %), and those with no depressive symptoms (3.6 %; 95% CI, 2.9 %– 4.6 %; P = .06; Figure 2, panel B).
Figure 2.
Kaplan-Meier Curves for Incident Coronary Heart Disease Among Patients With and Without Depressive Symptoms at Baseline (Panel A) and With No, Minor, or Major Depressive Symptoms at Baseline (Panel B)
Table 2 shows hazard ratios (HRs) for the unadjusted and adjusted associations between the presence of depressive symptoms and incident stroke and coronary heart disease. Presence of any depressive symptoms was not significantly associated with stroke in unadjusted or adjusted models, but was associated with a 58% increase in the hazard of incident coronary heart disease in unadjusted models. In models classifying depressive symptoms as major, minor, or none, major depressive symptoms were associated with a 2-fold increase in the hazard of stroke compared with no depressive symptoms (Table 3). This association persisted after adjustment for stroke risk, socioeconomic status, behavioral risk factors, antidepressant use, and coping strategies. Similar associations were observed in incident coronary heart disease models, with a 76% increase in incident coronary heart disease among patients with major vs no depressive symptoms. This increase in risk persisted after adjustment for the incident coronary heart disease risk score, socioeconomic status, behavioral risk factors, and antidepressant use, but was no longer significant after adjustment for coping strategies.
Table 2.
Association Between Any Depressive Symptoms and Incident Stroke and CHD
| Incident Stroke | ||
| Model |
Hazard Ratio (95% CI) |
P Value |
| Model 1. Unadjusted | 1.47 (0.90–2.38) | .12 |
| Model 2. Adjusted for stroke risk score and socioeconomic status | 1.30 (0.79–2.14) | .30 |
| Model 3. Model 2 plus behavioral risk factors | 1.30 (0.79–2.14) | .30 |
| Model 4. Model 3 plus antidepressant use | 1.33 (0.81–2.20) | .26 |
| Model 5. Model 4 plus coping strategies | 1.28 (0.74–2.23) | .37 |
| Incident CHD | ||
| Model |
Hazard Ratio (95% CI) |
P Value |
| Model 1. Unadjusted | 1.58 (1.05–2.36) | .03 |
| Model 2. Adjusted for CHD risk score and SES | 1.54 (1.02–2.34) | .04 |
| Model 3. Model 2 + behavioral risk factors | 1.54 (1.01–2.33) | .04 |
| Model 4. Model 3 + antidepressant use | 1.55 (1.02–2.35) | .04 |
| Model 5. Model 4 + coping strategies | 1.41 (0.90–2.21) | .14 |
Table 3.
Association Between Minor and Major Symptoms and Incident Stroke and Coronary Heart Disease
| Incident Stroke | ||||
| Model | Depressive Symptoms | |||
|
Minor vs None, HR (95% CI) |
P Value |
Major vs None, HR (95% CI) |
P Value |
|
| Model 1. Unadjusted | 0.91 (0.42–2.00) | .82 | 2.00 (1.15–3.48) | .01 |
| Model 2. Adjusted for stroke risk score and socioeconomic status | 0.80 (0.36–1.75) | .57 | 1.82 (1.02–3.22) | .04 |
| Model 3. Model 2 plus behavioral risk factors | 0.78 (0.35–1.72) | .54 | 1.86 (1.05–3.30) | .03 |
| Model 4. Model 3 plus antidepressant use | 0.79 (0.36–1.74) | .56 | 1.93 (1.09–3.42) | .03 |
| Model 5. Model 4 plus coping strategies | 0.75 (0.32–1.78) | .52 | 1.95 (1.02–3.71) | .04 |
| Incident CHD | ||||
| Model |
Minor vs None HR (95% CI) |
p- value |
Major vs None HR (95% CI) |
p- value |
| Model 1. Unadjusted | 1.39 (0.80–2.42) | .24 | 1.76 (1.07–2.90) | .03 |
| Model 2. Adjusted for CHD risk score and SES | 1.27 (0.72–2.22) | .41 | 1.87 (1.12–3.13) | .02 |
| Model 3. Model 2 + behavioral risk factors | 1.26 (0.72–2.20) | .42 | 1.87 (1.12–3.13) | .02 |
| Model 4. Model 3 + antidepressant use | 1.26 (0.72–2.20) | .43 | 1.90 (1.13–3.20) | .01 |
| Model 5. Model 4 + coping strategies | 1.19 (0.66–2.15) | .55 | 1.67 (0.95–2.93) | .07 |
Abbreviation: HR, hazard ratio.
We further examined the association between continuous CES-D score per 1 SD increase and stroke risk. The unadjusted risk of incident stroke increased by 26% per 1 SD increase in CES-D (Table 4). After adjustment, each SD increase in CES-D score was associated with a statistically significant 30% increase in the risk of incident stroke (HR per 1 SD increase, 1.30; 95% CI, 1.02–1.66; P = .04). We also observed positive associations for continuous CES-D and incident coronary heart disease, with a 19% increase in coronary heart disease risk for each 1 SD increase in CES-D score. This association also persisted after adjustment for incident coronary heart disease risk score, socioeconomic status, behavioral risk factors, and antidepressant use, but was attenuated and no longer significant after adjustment for coping strategies.
Table 4.
Association Between CES-D Score and Incident Stroke and CHDa
| Incident Stroke | ||
| Model |
Hazard Ratio (95% CI) |
P Value |
| Model 1. Unadjusted | 1.26 (1.04–1.53) | .02 |
| Model 2. Adjusted for stroke risk score and socioeconomic status | 1.239 (0.998–1.538) | .052 |
| Model 3. Model 2 plus behavioral risk factors | 1.241 (1.001–1.537) | .048 |
| Model 4. Model 3 plus antidepressant use | 1.27 (1.02–1.57) | .03 |
| Model 5. Model 4 plus coping strategies | 1.30 (1.02–1.66) | .04 |
| Incident CHD | ||
| Model |
Hazard Ratio (95% CI) |
p- value |
| Model 1. Unadjusted | 1.187 (1.002–1.407) | .047 |
| Model 2. Adjusted for CHD risk score and SES | 1.22 (1.02–1.48) | .03 |
| Model 3. Model 2 + behavioral risk factors | 1.22 (1.02–1.47) | .03 |
| Model 4. Model 3 + antidepressant use | 1.23 (1.02–1.49) | .03 |
| Model 5. Model 4 + coping strategies | 1.17 (0.95–1.45) | .13 |
Abbreviation: CES-D, Center for Epidemiologic Studies Depression.
Discussion
We investigated associations between depressive symptoms and incident cardiovascular outcomes in a community-based cohort of African Americans. Depressive symptoms were present in nearly one-quarter of cohort participants. Participants who reported depressive symptoms had greater comorbidity burden and more cardiovascular risk factors, were more likely to be current smokers, reported less physical activity, and had lower socioeconomic status. Unadjusted rates of incident stroke and coronary heart disease were higher among participants with depressive symptoms than those without. After adjustment for baseline risk, relevant confounders, and hypothesized mediators, major depressive symptoms were associated with a twofold increase in incident stroke risk. In adjusted analyses of continuous CES-D, each 1 SD increase in the score was associated with a 30% increase in the hazard of incident stroke. We observed similar patterns for incident coronary heart disease, but these associations were attenuated after adjustment for coping strategies.
Depression is increasingly recognized as an important risk factor for adverse cardiovascular events. Investigators from the Framingham Heart Study reported a fourfold increase in risk of stroke or transient ischemic attack among cohort participants 65 years or younger with depressive symptoms (CES-D ≥ 16).1 However, results from other studies have been less conclusive,21,22 and the majority of work to date has been conducted in white populations. Evidence from the Chicago Health and Aging Project suggests that unadjusted stroke incidence rates were higher among older African Americans (mean age, 77 years; n = 2649) reporting psychological distress (a composite measure of depressive symptoms, perceived stress, neuroticism, and life dissatisfaction) than those who reported no distress.10 Similar to our findings, this association was attenuated after adjustment for stroke risk factors. Positive associations were found among 2557 African Americans who reported depressive symptoms in the Health and Retirement Study.23 However, neither study included younger adults, a population that may be especially vulnerable to adverse cardiovascular effects of clinical depression.1 In addition, these studies relied on administrative claims and self-report for event ascertainment. Although the association between depressive symptoms and incident coronary heart disease has been more fully explored, few studies have examined these associations in black patients, and existing studies have produced mixed results.4,24,25 Our study builds upon previous work in a well-characterized cohort with a large sample of African Americans and detailed information on cardiovascular risk factors and physician-adjudicated events.
Our finding of increased event risk in patients with major but not minor depressive symptoms is consistent with previous work on psychological correlates of adverse health outcomes.26–28 In a cohort study of the association between CES-D score and cardiac mortality, Penninx et al29 reported a nearly two-fold increase in excess mortality associated with major depressive symptoms compared with minor depressive symptoms. It is possible that “minor depressive symptoms” represents a more sensitive but less specific classification of the exposure of interest. It may also be that reports of minor depression are more reflective of daily mood fluctuations rather than long-term dysthymia, and therefore are less predictive of long-term cardiovascular risk. Future analyses are needed to further elucidate the excess cardiovascular risk associated with minor depressive symptoms in African Americans. In addition, in contrast to results from incident stroke models, we found that the association between depressive symptoms and coronary heart disease risk was no longer significant after adjustment for coping strategies. It is possible that coping strategies are particularly important for mitigating the increased coronary heart disease risk associated with depressive symptoms, but not for the increased risk of stroke. While outside the scope of the present analysis, this hypothesis warrants additional study.
The need for greater understanding of associations between depressive symptoms and cardiovascular outcomes in African Americans is particularly salient in light of reported racial disparities in disease severity, timely diagnosis, and use of pharmacotherapy. Although evidence suggests that African Americans are more likely to visit a primary care physician for mental health-related concerns,30 they may also be less likely to have depression detected in primary care settings.31 African Americans report higher rates of disabling depression compared with white persons, and African Americans are also less likely to be prescribed evidence-based pharmacotherapy.9 In one study of antidepressant use among Medicaid recipients, African American patients were significantly less likely than white patients to receive selective serotonin reuptake inhibitors at the time of the initial depression diagnosis than were white patients.32 However, these treatment differences may be at least partly a result of patient preferences. Previous research suggests that African American patients are less likely than white patients to find antidepressant medication acceptable33 and less likely to believe that depression is biologically based.34 Consistent with previous findings, we found that only 11.4% of participants with depressive symptoms were treated with antidepressants at baseline. In addition, the relatively high rate of Jackson Heart Study participants who did not complete the CES-D scale may represent reluctance to disclose mental health information because of cultural stigma associated with depression.35
There are several limitations to our study. First, we did not have information on changes in depressive symptomatology over time. Second, we used the CES-D, a validated screening tool, to identify depressive symptomatology, consistent with what has been used in previous studies of depression and cardiovascular disease. However, because we did not have information on clinically diagnosed depression, some misclassification of depression status is possible. Third, we did not have information on traumatic brain injury or disability; however, we did include a detailed set of clinical comorbid conditions in adjustment models and an indicator for weekly physical activity level. We also did not have baseline CES-D information on 1889 participants in the Jackson Heart Study. The full distribution of baseline characteristics by CES-D completion is provided in Supplemental Table 2. Finally, the Jackson Heart Study cohort represents a population with relatively high socioeconomic status, with nearly half of cohort members reporting a college education or higher. Therefore, the results may not be generalizable to populations of lower socioeconomic status.
Our study has several unique strengths. First, the Jackson Heart Study is the largest US-based cohort with contemporary data on cardiovascular risk factors among African Americans, a population with a greater burden of severe depression than white populations. Second, we were able to examine multiple measures of depressive symptoms using a validated scale. Third, we had detailed information on a wide range of clinical confounders and socioeconomic indicators not typically available in administrative or retrospective registry data sets. Finally, all cardiovascular events in the Jackson Heart Study were adjudicated by clinical reviewers, reducing the potential for event misclassification.
In conclusion, we found a positive association between major depressive symptoms and risk of incident stroke and incident coronary heart disease, which persisted after multivariable adjustment for clinical and behavioral risk factors. Future work characterizing the burden of depression over time and risk of adverse cardiovascular events in African Americans is warranted.
Supplementary Material
What is Known
Prior studies have found that depression is predictive of adverse cardiovascular events.
Compared with white populations, African Americans have higher rates of severe depression, but there is limited data on the prognostic significance of depression in African American cohorts.
What the Study Adds
Depression was common in this African American population, affecting nearly one-quarter of cohort participants.
Participants with depressive symptoms had more comorbidities, lower physical activity and lower socioeconomic status.
Even after adjusting for clinical and behavioral risk factors, major depressive symptoms were associated with a nearly two-fold increase in incidence of stroke and coronary heart disease.
Acknowledgments
We thank the staff and participants of the Jackson Heart Study for their important contributions to this work. Damon M. Seils, MA, Duke University, assisted with manuscript preparation.
Sources of Funding The Jackson Heart Study is supported by contracts HHSN268201300046C, HHSN268201300047C, HHSN268201300048C, HHSN268201300049C, and HHSN268201300050C from the National Heart, Lung, and Blood Institute and the National Institute on Minority Health and Health Disparities. Research reported in this manuscript was supported by grant R01HL117305 from the National Heart, Lung, And Blood Institute.
Footnotes
Disclaimer: The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute, the National Institute on Minority Health and Health Disparities, or the National Institutes of Health.
Disclosures: None.
References
- 1.Salaycik KJ, Kelly-Hayes M, Beiser A, Nguyen AH, Brady SM, Kase CS, Wolf PA. Depressive symptoms and risk of stroke: the Framingham Study. Stroke. 2007;38:16–21. doi: 10.1161/01.STR.0000251695.39877.ca. [DOI] [PubMed] [Google Scholar]
- 2.O’Donnell MJ, Xavier D, Liu L, Zhang H, Chin SL, Rao-Melacini P, Rangarajan S, Islam S, Pais P, McQueen MJ, Mondo C, Damasceno A, Lopez-Jaramillo P, Hankey GJ, Dans AL, Yusoff K, Truelsen T, Diener HC, Sacco RL, Ryglewicz D, Czlonkowska A, Weimar C, Wang X, Yusuf S INTERSTROKE investigators. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet. 2010;376:112–123. doi: 10.1016/S0140-6736(10)60834-3. [DOI] [PubMed] [Google Scholar]
- 3.Jonas BS, Mussolino ME. Symptoms of depression as a prospective risk factor for stroke. Psychosom Med. 2000;62:463–471. doi: 10.1097/00006842-200007000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Ford DE, Mead LA, Chang PP, Cooper-Patrick L, Wang NY, Klag MJ. Depression is a risk factor for coronary artery disease in men: the precursors study. Arch Intern Med. 1998;158:1422–1426. doi: 10.1001/archinte.158.13.1422. [DOI] [PubMed] [Google Scholar]
- 5.Sims M, Redmond N, Khodneva Y, Durant RW, Halanych J, Safford MM. Depressive symptoms are associated with incident coronary heart disease or revascularization among blacks but not among whites in the Reasons for Geographical and Racial Differences in Stroke study. Ann Epidemiol. 2015;25:426–432. doi: 10.1016/j.annepidem.2015.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dong JY, Zhang YH, Tong J, Qin LQ. Depression and risk of stroke: a meta-analysis of prospective studies. Stroke. 2012;43:32–37. doi: 10.1161/STROKEAHA.111.630871. [DOI] [PubMed] [Google Scholar]
- 7.Pan A, Sun Q, Okereke OI, Rexrode KM, Hu FB. Depression and risk of stroke morbidity and mortality: a meta-analysis and systematic review. JAMA. 2011;306:1241–1249. doi: 10.1001/jama.2011.1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rugulies R. Depression as a predictor for coronary heart disease. a review and meta-analysis. Am J Prev Med. 2002;23:51–61. doi: 10.1016/s0749-3797(02)00439-7. [DOI] [PubMed] [Google Scholar]
- 9.Williams DR, Gonzalez HM, Neighbors H, Nesse R, Abelson JM, Sweetman J, Jackson JS. Prevalence and distribution of major depressive disorder in African Americans, Caribbean Blacks, and non-Hispanic whites: results from the National Survey of American Life. Arch Gen Psychiatry. 2007;64:305–315. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- 10.Henderson KM, Clark CJ, Lewis TT, Aggarwal NT, Beck T, Guo H, Lunos S, Brearley A, Mendes de Leon CF, Evans DA, Everson-Rose SA. Psychosocial distress and stroke risk in older adults. Stroke. 2013;44:367–372. doi: 10.1161/STROKEAHA.112.679159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shah AJ, Ghasemzadeh N, Zaragoza-Macias E, Patel R, Eapen DJ, Neeland IJ, Pimple PM, Zafari AM, Quyyumi AA, Vaccarino V. Sex and age differences in the association of depression with obstructive coronary artery disease and adverse cardiovascular events. J Am Heart Assoc. 2014;3:e000741. doi: 10.1161/JAHA.113.000741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Taylor HA, Jr, Wilson JG, Jones DW, Sarpong DF, Srinivasan A, Garrison RJ, Nelson C, Wyatt SB. Toward resolution of cardiovascular health disparities in African Americans: design and methods of the Jackson Heart Study. Ethn Dis. 2005;15:S6-4-17. [PubMed] [Google Scholar]
- 13.The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. The ARIC Investigators. Am J Epidemiol. 1989;129:687–702. [PubMed] [Google Scholar]
- 14.Radloff L. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 15.Arbogast PG, Kaltenbach L, Ding H, Ray WA. Adjustment for multiple cardiovascular risk factors using a summary risk score. Epidemiology. 2008;19:30–37. doi: 10.1097/EDE.0b013e31815be000. [DOI] [PubMed] [Google Scholar]
- 16.Arbogast PG, Ray WA. Performance of disease risk scores, propensity scores, and traditional multivariable outcome regression in the presence of multiple confounders. Am J Epidemiol. 2011;174:613–620. doi: 10.1093/aje/kwr143. [DOI] [PubMed] [Google Scholar]
- 17.Addison CC, Campbell-Jenkins BW, Sarpong DF, Kibler J, Singh M, Dubbert P, Wilson G, Payne T, Taylor H. Psychometric evaluation of a Coping Strategies Inventory Short-Form (CSI-SF) in the Jackson Heart Study cohort. Int J Environ Res Public Health. 2007;4:289–295. doi: 10.3390/ijerph200704040004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harrell FE., Jr . Multivariable modeling strategies. In: Harrell FE Jr, editor. Regression Modeling Strategies: With Applications to Linear Models, Logistic Regression, and Survival Analysis. New York, NY: Springer-Verlag; 2001. pp. 53–85. [Google Scholar]
- 19.Keenan PS, Normand SL, Lin Z, Drye EE, Bhat KR, Ross JS, Schuur JD, Stauffer BD, Bernheim SM, Epstein AJ, Wang Y, Herrin J, Chen J, Federer JJ, Mattera JA, Wang Y, Krumholz HM. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circ Cardiovasc Qual Outcomes. 2008;1:29–37. doi: 10.1161/CIRCOUTCOMES.108.802686. [DOI] [PubMed] [Google Scholar]
- 20.Krumholz HM, Wang Y, Mattera JA, Han LF, Ingber MJ, Roman S, Normand SL. An administrative claims model suitable for profiling hospital performance based on 30-day mortality rates among patients with heart failure. Circulation. 2006;113:1693–1701. doi: 10.1161/CIRCULATIONAHA.105.611194. [DOI] [PubMed] [Google Scholar]
- 21.Jackson CA, Mishra GD. Depression and risk of stroke in midaged women: a prospective longitudinal study. Stroke. 2013;44:1555–1560. doi: 10.1161/STROKEAHA.113.001147. [DOI] [PubMed] [Google Scholar]
- 22.Wassertheil-Smoller S, Applegate WB, Berge K, Chang CJ, Davis BR, Grimm R, Jr, Kostis J, Pressel S, Schron E. Change in depression as a precursor of cardiovascular events. SHEP Cooperative Research Group (Systoloc Hypertension in the Elderly) Arch Intern Med. 1996;156:553–561. [PubMed] [Google Scholar]
- 23.Glymour MM, Yen JJ, Kosheleva A, Moon JR, Capistrant BD, Patton KK. Elevated depressive symptoms and incident stroke in Hispanic, African-American, and white older Americans. J Behav Med. 2012;35:211–220. doi: 10.1007/s10865-011-9356-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lewis TT, Guo H, Lunos S, Mendes de Leon CF, Skarupski KA, Evans DA, Everson-Rose SA. Depressive symptoms and cardiovascular mortality in older black and white adults: evidence for a differential association by race. Circ Cardiovasc Qual Outcomes. 2011;4:293–299. doi: 10.1161/CIRCOUTCOMES.110.957548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Capistrant BD, Gilsanz P, Moon JR, Kosheleva A, Patton KK, Glymour MM. Does the association between depressive symptoms and cardiovascular mortality risk vary by race? Evidence from the Health and Retirement Study. Ethn Dis. 2013;23:155–160. [PMC free article] [PubMed] [Google Scholar]
- 26.Koenig HG, George LK. Depression and physical disability outcomes in depressed medically ill hospitalized older adults. Am J Geriatr Psychiatry. 1998;6:230–247. [PubMed] [Google Scholar]
- 27.Vogt T, Pope C, Mullooly J, Hollis J. Mental health status as a predictor of morbidity and mortality: a 15-year follow-up of members of a health maintenance organization. Am J Public Health. 1994;84:227–231. doi: 10.2105/ajph.84.2.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goldston K, Baillie AJ. Depression and coronary heart disease: a review of the epidemiological evidence, explanatory mechanisms and management approaches. Clin Psychol Rev. 2008;28:288–306. doi: 10.1016/j.cpr.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 29.Penninx BW, Guralnik JM, Mendes de Leon CF, Pahor M, Visser M, Corti MC, Wallace RB. Cardiovascular events and mortality in newly and chronically depressed persons >70 years of age. Am J Cardiol. 1998;81:988–994. doi: 10.1016/s0002-9149(98)00077-0. [DOI] [PubMed] [Google Scholar]
- 30.Snowden LR, Pingitore D. Frequency and scope of mental health service delivery to African Americans in primary care. Ment Health Serv Res. 2002;4:123–130. doi: 10.1023/a:1019709728333. [DOI] [PubMed] [Google Scholar]
- 31.Borowsky SJ, Rubenstein LV, Meredith LS, Camp P, Jackson-Triche M, Wells KB. Who is at risk of nondetection of mental health problems in primary care? J Gen Intern Med. 2000;15:381–388. doi: 10.1046/j.1525-1497.2000.12088.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Melfi CA, Croghan TW, Hanna MP, Robinson RL. Racial variation in antidepressant treatment in a Medicaid population. J Clin Psychiatry. 2000;61:16–21. doi: 10.4088/jcp.v61n0105. [DOI] [PubMed] [Google Scholar]
- 33.Cooper LA, Gonzales JJ, Gallo JJ, Rost KM, Meredith LS, Rubenstein LV, Wang NY, Ford DE. The acceptability of treatment for depression among African-American, Hispanic, and white primary care patients. Med Care. 2003;41:479–489. doi: 10.1097/01.MLR.0000053228.58042.E4. [DOI] [PubMed] [Google Scholar]
- 34.Givens JL, Houston TK, Van Voorhees BW, Ford DE, Cooper LA. Ethnicity and preferences for depression treatment. Gen Hosp Psychiatry. 2007;29:182–191. doi: 10.1016/j.genhosppsych.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 35.Menke R, Flynn H. Relationships between stigma, depression, and treatment in white and African American primary care patients. J Nerv Ment Dis. 2009;197:407–411. doi: 10.1097/NMD.0b013e3181a6162e. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.