Abstract
Background
Stages of activity limitation based on activities of daily living (ADLs) and instrumental activities of daily living (IADLs) have been found to predict mortality in those age 70 years and above but have not been examined in Medicare beneficiaries age 65 years and older using routinely collected data.
Objective
To examine the association between functional stages based on activities of ADLs and IADLs with three-year mortality in Medicare beneficiaries age 65 years and older, accounting for baseline sociodemographics, heath status, smoking, subjective health, and psychological well-being.
Design
Cohort study using the Medicare Current Beneficiary Survey (MCBS) and associated health care utilization data.
Setting
Community administered survey.
Participants
We included 9698 Medicare beneficiaries 65 years of age and older who entered the MCBS in 2005–07.
Main outcome measures
Death within three years of cohort entry.
Results
The overall mortality rate was 3.6 per 100 person years, and three-year cumulative mortality was 10.3%. Unadjusted three-year mortality was monotonically associated with both ADL stage and IADL stag. Adjusted three-year mortality was associated with ADL and IADL stages, except that in some models the hazard ratio for stage III (which includes persons with atypical activity limitation patterns) was numerically lower than that for stage II.
Conclusion
We found nearly monotonic relationships between ADL and IADL stage and adjusted three-year mortality. These findings could aid in the development of population health approaches and metrics for evaluating the success of alternative economic, social, or health policies on the longevity of older adults with activity limitations.
INTRODUCTION
More than 56 million Americans (19% of the US population) had at least one disability in 2010 according to the Survey of Income and Program Participation.1 This number is expected to grow substantially as the baby boom generation ages. Approximately 25% of people 65 years of age and older have difficulty with at least one basic activity of daily living (ADL) and an additional 14% have difficulty performing at least one higher-level instrumental activity of daily living (IADL)2 as defined by the International Classification of Functioning, Disability and Health (ICF).3
This high prevalence of activity limitation along with the growing number of elderly persons in the US will present a challenge to the Medicare program. Sox has asserted that approaching each patient strictly as an individual is an obsolete organizing principal for US health care today, and that population health approaches are the best alternative for improving and maintaining the health of people in the community.4 In response to this assertion and to a 2007 Institute of Medicine report calling for the creation of comprehensive disability monitoring systems based on ICF terminology and concepts, Stineman et al developed ICF-based staging systems for ADLs and IADLs,5 which are summarized in Table 1. Disability staging systems that are based on regularly-collected survey data and predict mortality can be used to advance the goal of using population-based approaches to monitor and improve health. The five ADL and five IADL stages represent meaningful population-level measures of activity limitation that could be used by the Centers for Medicare and Medicaid Services (CMS) to monitor the prevalence of activity limitations in the Medicare population and assess the effects of efforts to promote the health, function and survival of persons with defined types and severities of activity limitation. Such monitoring can be performed using data already routinely collected as part of the Medicare Current Beneficiary Survey (MCBS).6
Table 1.
Disability Staging System based on Activities of Daily Living (ADLs) and Instrumental Activities of Daily Living (IADLs) Derived from the Medicare Current Beneficiary Survey
| Stage | ADL Domain | IADL Domain |
|---|---|---|
| Stage 0: No disability | Can eat, toilet, dress, bathe/shower, get in/out of bed or chairs, and walk without difficulty. | Can use the telephone, manage money, prepare meals, do light housework, shop for personal items, and do heavy housework. |
| Stage I: Mild disability | Eating, toileting, dressing, and bathing/showering are not difficult. May have difficulty getting in/out of bed or chairs and/or walking). | Using the telephone, managing money, preparing meals, and doing light housework are not difficult. May have difficulty shopping for personal items and/or doing heavy housework. |
| Stage II: Moderate disability | Eating and toileting are not difficult. May have difficulty dressing, bathing/showering, getting in/out of bed or chairs, and/or walking. | Using the telephone and managing money are not difficult. May have difficulty preparing meals, doing light housework, shopping for personal items, and/or doing heavy housework. |
| Stage III: Severe disability | Difficulty with eating and/or toileting but not with all ADLs. | Has difficulty using the telephone and/or managing money but not all IADLs are difficult. |
| Stage IV: Complete disability | All ADLs are difficult. | All IADLs are difficult. |
The staging systems that we examined (Table 1) are based on the ADL and IADL domains such that stage 0 represents “no”; stage I, “mild”; stage II “moderate”; stage III “severe”; and stage IV “complete” limitation within those domains. These hierarchical staging systems reflect the most common patterns of functional loss and recovery and specify clinically meaningful patterns of increasing difficulty with self-care and more complex instrumental skills. At mild stages of limitation, people are able to perform all but the typically hardest activities without difficulty, while at more advanced stages even the easiest activities (i.e., those least frequently reported as difficult) become limited. Stage III in the ADL and IADL systems was designed as a “non-fitting” stage to accommodate people with atypical patterns of disability.
ADL and IADL stages have shown expected associations with age and comorbidity7 and were found to be associated with mortality using data from 1994 National Health Interview Survey linked to data from the Second Longitudinal Study of Aging.8,9 However, to our knowledge, the association between MCBS-derived ADL and IADL stages and mortality is unknown, yet important if stages are to be used to risk stratify persons on the basis of disability in population health approaches. If these stages are independently associated with mortality they might be useful for identifying Medicare beneficiaries who might benefit from interventions to ameliorate activity limitation or for evaluating the success of policies to help the disabled elderly. We therefore sought to assess whether the MCBS-derived ADL and IADL stages predict three-year mortality after adjusting for medical comorbidity in a nationally representative sample of Medicare beneficiaries 65 years of age and older. We hypothesized that increasing ADL and IADL stages would be independently associated with increasing three-year mortality, with the possible exception of the non-fitting stage III.
METHODS
Study Cohort
We studied MCBS participants.6,10 The MCBS is a systematic sample of Medicare beneficiaries who are interviewed (or whose proxies are interviewed) and whose subsequent health care utilization is recorded. Each beneficiary or proxy is interviewed for a total of four years: entry year plus three years of follow-up. The resulting data consist of two linkable data sets: 1) Access to Care (which records baseline health status and the results of an interview ascertaining functional ability); and 2) Cost and Use (which includes respondents’ Medicare claims data). Each respondent is assigned a survey weight that reflects the number of Medicare beneficiaries for whom that individual stands for in the survey results.10
Our study cohort consisted of members of the 2005, 2006, and 2007 entry panels who had reached their 65th birthday by the date of panel entry (n=9700). We restricted our study to beneficiaries 65 years of age and older because we anticipated that associations between disability stages and death might differ between elderly and non-elderly Medicare beneficiaries and because of the small number of deaths in those less than 65 years of age. We excluded two beneficiaries for whom key ADL variables were missing and three beneficiaries for whom key IADL variables was missing. Thus, 9695 persons were included in the analyses. This study was approved by the University of Pennsylvania’s institutional review board.
Baseline ADL and IADL Stages
We characterized each respondent by baseline ADL and IADL stage using methods described previously.5,7 Ability to perform each ADL and IADL without versus with difficulty was ascertained at baseline based on responses to questionnaire items about six activities per domain.5,11 The ADLs were eating, toileting, dressing, bathing/showering, getting in or out of bed/chairs, and walking. The IADLs were using the telephone, managing money, preparing meals, doing light housework, shopping for personal items, and doing heavy housework.
Outcome
The outcome of interest was the occurrence and timing of death from any cause during the three-year follow-up period, as recorded in the Cost and Use files.
Covariates
We ascertained baseline covariates in four domains: sociodemographics, comorbidities, smoking, and psychological well-being and subjective health.
Sociodemographic variables included sex, race or ethnic group (non-Hispanic white, non-Hispanic black, Hispanic, or other), and age (65–74, 75–84, or ≥85 years). Education was categorized as high school graduate or higher or below high school graduate. Income was categorized as ≤$25,000 or >$25,000 per year. Social living circumstance was classified as lives alone, lives with spouse, lives with children, or other.
Baseline self-reported comorbidities were conditions or events that a doctor ever told the beneficiary had or occurred within the past year. With some of the conditions noted in Table 2, we also assessed relationships with acuity, i.e., initial diagnosis within the past year or more than a year ago. The medical conditions consisted of rheumatoid arthritis, arthritis other than rheumatoid, hypertension, myocardial infarction, angina or coronary artery diseases, congestive heart failure, heart valve problems, rhythm disturbance, stroke, cancer other than skin, osteoporosis, broken hip, asthma or chronic obstructive pulmonary disease (COPD), Parkinson’s disease, amputation, diabetes type 1, 2, or other, mental retardation, Alzheimer’s disease, mental or psychiatric conditions, depression, hardening of the arteries, and incontinence/urinary catheterization. Sensory variables were having difficulty with vision and hearing. Smoking was assessed at baseline and classified as never, past, or current. Psychological well-being variables were ascertained at baseline and consisted of difficulty concentrating (yes or no), feeling sad or blue (all of the time, most of the time, some of the time, a little of the time, or none of the time), and lost interest or pleasure in social activities (yes or no).
Table 2.
Baseline Characteristics of Enrollees of the 2005, 2006, and 2007 Entry Panels of the Medicare Beneficiary Survey who had Reached their 65th Birthday by Activity of Daily Living (ADL) and Instrumental Activity of Daily Living (IADL) Stage
| Variable | All (N=9695) |
ADL Stage | IADL Stage | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 (N=6713) |
I (N=1609) |
II (N=758) |
III (N=512) |
IV (N=103) |
p | 0 (N=6076) |
I (N=1676) |
II (N=713) |
III (N=1014) |
IV N=(216) |
p | |||
| Sociodemographic | ||||||||||||||
| Sex | Female | 55.8 | 53.7 | 58.8 | 63.2 | 67.0 | 63.6 | <.001 | 50.3 | 73.7 | 71.7 | 51.3 | 64.3 | <.001 |
| Race | Non-Hispanic White | 81.7 | 83.1 | 80.1 | 77.5 | 75.1 | 58.6 | <.001 | 83.1 | 82.0 | 76.5 | 78.3 | 64.4 | <.001 |
| Non-Hispanic Black | 7.5 | 6.8 | 8.5 | 10.4 | 10.8 | 11.4 | 7.0 | 7.8 | 9.1 | 7.9 | 17.0 | |||
| Hispanic | 7.3 | 6.7 | 8.3 | 8.8 | 9.6 | 21.6 | 6.7 | 6.7 | 10.0 | 10.0 | 15.2 | |||
| Other | 3.4 | 3.4 | 3.1 | 3.3 | 4.5 | * | 3.2 | 3.5 | 4.5 | 3.8 | * | |||
| Age | 65–74 | 56.9 | 62.3 | 45.5 | 39.6 | 37.4 | 32.9 | <.001 | 63.3 | 50.0 | 45.0 | 36.4 | 21.3 | <.001 |
| 75–84 | 33.4 | 31.0 | 39.6 | 39.8 | 39.8 | 40.7 | 30.7 | 36.5 | 40.3 | 41.2 | 41.2 | |||
| ≥85 | 9.8 | 6.7 | 14.9 | 20.6 | 22.8 | 26.4 | 6.0 | 13.5 | 14.6 | 22.4 | 37.5 | |||
| Education | Below high school graduate | 24.9 | 21.2 | 31.8 | 35.8 | 41.1 | 49.1 | <.001 | 20.1 | 28.0 | 36.8 | 40.8 | 51.9 | <.001 |
| Income | ≤$25,000 | 50.7 | 56.4 | 39.0 | 32.5 | 31.0 | 21.6 | <.001 | 57.9 | 40.6 | 33.1 | 35.0 | 18.6 | <.001 |
| Social living circumstance | Alone | 29.4 | 28.5 | 31.7 | 32.8 | 32.1 | 25.2 | <.001 | 27.8 | 35.9 | 32.8 | 29.2 | 20.8 | <.001 |
| Spouse | 55.9 | 59.6 | 49.3 | 42.8 | 41.0 | 39.6 | 60.9 | 46.6 | 45.0 | 48.1 | 33.7 | |||
| Children | 9.3 | 7.1 | 12.8 | 16.8 | 18.3 | 27.3 | 6.6 | 11.7 | 14.6 | 16.9 | 34.0 | |||
| Other | 5.3 | 4.7 | 6.2 | 7.6 | 8.5 | * | 4.7 | 5.8 | 7.7 | 5.8 | 11.4 | |||
| Health status conditions | ||||||||||||||
| Rheumatoid arthritis | 7.9 | 5.6 | 12.7 | 16.3 | 14.4 | 10.4 | <.001 | 5.4 | 11.5 | 15.3 | 12.9 | 12.7 | <.001 | |
| Arthritis other than rheumatoid | >1 year | 12.2 | 12.2 | 13.2 | 9.9 | 11.2 | 10.6 | <.001 | 11.9 | 13.4 | 11.9 | 12.3 | 9.9 | <.001 |
| ≤1 year | 34.4 | 28.3 | 50.8 | 49.1 | 53.7 | 43.4 | 27.5 | 51.2 | 55.1 | 39.1 | 39.7 | |||
| Hypertension | >1 year | 11.5 | 11.7 | 11.8 | 9.3 | 10.1 | * | <.001 | 11.9 | 10.5 | 10.7 | 10.9 | 8.6 | <.001 |
| ≤1 year | 49.2 | 44.9 | 60.4 | 60.8 | 60.5 | 66.2 | 43.8 | 60.1 | 62.5 | 58.3 | 58.1 | |||
| Myocardial infarction | >1 year | 10.5 | 8.6 | 16.1 | 14.2 | 15.4 | 15.3 | <.001 | 8.6 | 12.7 | 13.9 | 16.9 | 18.4 | <.001 |
| ≤1 year | 1.9 | 1.3 | 3.4 | 3.3 | 3.9 | * | 1.3 | 2.3 | 6.3 | 2.6 | * | |||
| Angina or coronary artery diseases | >1 year | 5.7 | 5.2 | 7.6 | 7.6 | 6.1 | * | <.001 | 5.0 | 7.4 | 7.1 | 6.4 | 9.4 | <.001 |
| ≤1 year | 3.6 | 2.5 | 6.4 | 6.7 | 6.2 | * | 2.5 | 4.7 | 7.3 | 6.3 | 7.5 | |||
| Congestive heart failure | >1 year | 3.5 | 2.4 | 6.3 | 5.9 | 7.4 | * | <.001 | 2.2 | 5.9 | 6.1 | 5.8 | 11.4 | <.001 |
| ≤1 year | 2.5 | 1.2 | 4.8 | 8.3 | 7.1 | * | 1.0 | 4.2 | 8.2 | 5.3 | 7.6 | |||
| Heart valve problems | >1 year | 4.3 | 3.8 | 5.7 | 5.9 | 5.7 | * | <.001 | 3.7 | 6.0 | 4.9 | 5.6 | * | <.001 |
| ≤1 year | 3.2 | 2.6 | 5.0 | 4.4 | 5.3 | * | 2.1 | 5.6 | 5.6 | 5.3 | * | |||
| Rhythm disturbance | >1 year | 8.0 | 7.4 | 9.1 | 8.5 | 13.6 | * | <.001 | 7.3 | 8.8 | 11.5 | 9.2 | 10.9 | <.001 |
| ≤ 1year | 8.4 | 6.4 | 12.9 | 14.9 | 14.8 | 12.0 | 5.8 | 13.2 | 15.4 | 12.6 | 13.8 | |||
| Stroke | >1 year | 8.0 | 5.2 | 12.7 | 18.6 | 17.9 | 26.2 | <.001 | 5.0 | 9.8 | 15.7 | 16.7 | 33.2 | <.001 |
| ≤1 year | 1.8 | 1.1 | 2.8 | 4.5 | 5.3 | 11.2 | 1.0 | 2.4 | 4.4 | 4.0 | 9.6 | |||
| Cancer other than skin | >1 year | 12.0 | 11.6 | 12.8 | 12.5 | 15.8 | * | <.001 | 11.0 | 15.0 | 12.1 | 14.1 | 11.6 | <.001 |
| ≤1 year | 5.0 | 4.3 | 6.1 | 6.9 | 8.9 | * | 4.4 | 5.6 | 7.9 | 6.2 | * | |||
| Osteoporosis | 16.8 | 14.2 | 22.1 | 25.9 | 25.9 | 22.0 | <.001 | 12.4 | 26.1 | 29.9 | 21.1 | 23.7 | <.001 | |
| Broken hip | >1 year | 2.6 | 1.4 | 4.6 | 6.3 | 8.1 | * | <.001 | 1.4 | 4.0 | 5.2 | 5.5 | 11.0 | <.001 |
| ≤1 year | 0.6 | 0.2 | 0.8 | 2.8 | 1.9 | * | 0.2 | 0.6 | 1.8 | 1.6 | * | |||
| Emphysema/asthma/chronic obstructive pulmonary disease | 13.4 | 10.4 | 21.3 | 21.2 | 23.7 | 16.8 | <.001 | 9.8 | 19.8 | 26.0 | 19.2 | 16.4 | <.001 | |
| Parkinson’s disease | 1.1 | 0.5 | 1.6 | 3.0 | 4.6 | * | <.001 | 0.4 | 1.3 | 2.4 | 2.9 | 9.2 | <.001 | |
| Amputation | 0.6 | 0.3 | 0.9 | 2.2 | 1.9 | * | <.001 | 0.4 | 0.8 | * | 1.1 | * | <.001 | |
| Diabetes | Type 1 | 2.5 | 1.5 | 4.4 | 5.9 | 5.0 | * | <.001 | 1.5 | 3.3 | 6.5 | 4.4 | 7.6 | <.001 |
| Type 2 | 16.0 | 13.5 | 21.1 | 26.0 | 24.2 | 21.7 | 13.5 | 20.6 | 24.7 | 19.5 | 21.3 | |||
| Other type | 4.9 | 4.5 | 5.9 | 4.4 | 7.4 | * | 4.7 | 4.8 | 5.4 | 6.4 | 6.8 | |||
| Mental retardation | 0.3 | 0.2 | * | * | * | * | <.001 | * | * | * | 1.1 | * | <.001 | |
| Mental or psychiatric conditions | >1 year | 0.5 | 0.5 | * | * | * | * | <0.01 | 0.3 | 0.8 | * | * | * | <.001 |
| ≤1 year | 1.0 | 0.7 | 1.4 | 2.0 | * | * | 0.6 | 0.8 | * | 3.0 | * | |||
| Alzheimer’s disease | 2.4 | 1.3 | 2.3 | 7.1 | 9.3 | 25.2 | <.001 | 0.7 | 0.8 | 2.2 | 11.1 | 39.9 | <.001 | |
| Depression | >1 year | 7.2 | 6.1 | 9.4 | 12.2 | 9.0 | * | <.001 | 5.6 | 9.6 | 11.8 | 10.7 | 11.7 | <.001 |
| ≤1 year | 8.6 | 5.6 | 13.6 | 17.9 | 22.9 | 24.7 | 4.5 | 13.9 | 20.9 | 17.2 | 25.6 | |||
| Hardening of the arteries | 7.1 | 5.8 | 9.5 | 10.3 | 13.4 | 12.2 | <.001 | 5.3 | 9.5 | 10.7 | 12.2 | 12.4 | <.001 | |
| Incontinence | Yes | 27.9 | 21.8 | 37.3 | 50.1 | 53.5 | 66.8 | <.001 | 20.3 | 41.9 | 46.7 | 38.7 | 61.8 | <.001 |
| Dialysis/catheterization | 0.6 | 0.2 | * | * | 4.2 | 10.9 | * | 1.3 | * | 1.4 | 6.7 | |||
| Vision | Has difficulty | 5.9 | 3.4 | 9.5 | 15.0 | 15.8 | 29.7 | <.001 | 2.5 | 8.2 | 13.5 | 16.3 | 32.9 | <.001 |
| Hearing | Has difficulty | 6.2 | 4.6 | 7.9 | 13.4 | 13.8 | 18.4 | <.001 | 3.0 | 5.6 | 8.5 | 26.0 | 25.6 | <.001 |
| Paralysis | >1 year | 1.3 | 0.8 | 2.2 | 2.9 | 3.3 | * | <.001 | 0.7 | 2.0 | 3.0 | 2.2 | * | <.001 |
| ≤1 year | 1.0 | 0.2 | 1.2 | 3.7 | 5.8 | 19.5 | 0.2 | 0.7 | 3.4 | 3.4 | 10.7 | |||
| Smoking Status | Not a smoker | 44.1 | 44.4 | 41.4 | 43.2 | 47.0 | 54.0 | 0.043 | 43.3 | 46.1 | 46.1 | 43.0 | 53.2 | 0.046 |
| Ever a smoker | 44.0 | 43.7 | 45.2 | 46.2 | 44.0 | 34.4 | 44.3 | 43.2 | 41.7 | 46.4 | 39.6 | |||
| Current smoker | 11.9 | 11.8 | 13.4 | 10.6 | 9.0 | 11.7 | 12.4 | 10.7 | 12.3 | 10.6 | 7.2 | |||
| Subjective health and psychological well-being | ||||||||||||||
| Difficulty concentrating | 11.0 | 6.4 | 16.6 | 29.2 | 32.1 | 57.5 | <.001 | 5.1 | 12.6 | 23.1 | 32.5 | 70.5 | <.001 | |
| Feeling sad or blue | All of the time | 1.0 | 0.6 | 1.2 | 3.3 | 2.9 | * | <.001 | 0.6 | 1.2 | 2.9 | 1.8 | 6.2 | <.001 |
| Most of the time | 3.9 | 2.9 | 4.9 | 7.2 | 9.1 | 21.4 | 2.5 | 4.7 | 6.9 | 8.1 | 17.5 | |||
| Some of the time | 17.0 | 13.4 | 24.3 | 28.8 | 31.6 | 23.4 | 12.3 | 23.3 | 31.0 | 28.5 | 28.7 | |||
| A little of the time | 35.5 | 34.9 | 38.9 | 36.7 | 33.1 | 29.6 | 34.5 | 41.6 | 35.6 | 33.7 | 24.4 | |||
| None of the time | 42.6 | 48.3 | 30.8 | 24.0 | 23.4 | 15.7 | 50.2 | 29.2 | 23.6 | 27.8 | 23.3 | |||
| Lost interest or pleasure in social activities | 10.4 | 6.5 | 15.9 | 23.8 | 27.9 | 43.1 | <.001 | 5.5 | 15.7 | 25.2 | 21.8 | 35.5 | <.001 | |
| Global health perceptions | Excellent | 19.3 | 24.3 | 6.1 | 6.0 | 5.4 | * | <.001 | 25.7 | 6.4 | 3.7 | 9.1 | 5.4 | <.001 |
| Very good | 29.3 | 33.7 | 19.3 | 16.2 | 14.8 | * | 34.7 | 21.0 | 12.7 | 19.6 | 9.2 | |||
| Good | 31.0 | 29.8 | 37.4 | 31.2 | 30.7 | 18.0 | 29.6 | 38.2 | 27.5 | 31.4 | 25.9 | |||
| Fair | 15.1 | 10.4 | 26.0 | 31.2 | 27.7 | 34.5 | 8.5 | 26.7 | 34.6 | 26.6 | 29.2 | |||
| Poor | 5.4 | 1.8 | 11.2 | 15.3 | 21.4 | 39.3 | 1.5 | 7.6 | 21.4 | 13.2 | 30.3 | |||
| Comparative general health status to a year ago | Much better | 4.9 | 5.2 | 4.1 | 4.8 | 3.4 | * | <.001 | 5.1 | 5.1 | 4.6 | 4.0 | * | <.001 |
| Somewhat better | 10.4 | 10.0 | 12.0 | 13.0 | 7.8 | * | 9.7 | 12.4 | 12.0 | 10.7 | 8.5 | |||
| About the same | 66.0 | 72.6 | 52.6 | 44.0 | 44.8 | 34.9 | 74.3 | 54.8 | 38.4 | 51.0 | 37.4 | |||
| Somewhat worse | 16.3 | 11.5 | 27.1 | 30.4 | 33.4 | 36.7 | 10.4 | 24.4 | 35.8 | 27.5 | 34.8 | |||
| Much worse | 2.4 | 0.8 | 4.2 | 7.8 | 10.7 | 19.6 | 0.5 | 3.3 | 9.3 | 6.8 | 16.9 | |||
| Amount of time health limits contact with friends and family during the past month | None of the time | 71.6 | 83.1 | 50.0 | 33.7 | 25.4 | * | <.001 | 85.9 | 52.5 | 25.4 | 44.6 | 14.8 | <.001 |
| Some of the time | 17.2 | 12.9 | 29.2 | 29.0 | 30.1 | 16.9 | 11.0 | 31.0 | 30.9 | 28.0 | 18.5 | |||
| Most of the time | 7.1 | 3.0 | 14.2 | 22.0 | 24.0 | 25.5 | 2.3 | 12.7 | 25.9 | 15.5 | 22.2 | |||
| All of the time | 4.1 | 1.0 | 6.6 | 15.3 | 20.5 | 51.3 | 0.8 | 3.8 | 17.8 | 11.8 | 44.5 | |||
| Outcome | ||||||||||||||
| Three-year mortality | 10.3 | 6.2 | 14.8 | 26.6 | 29.6 | 48.6 | <.001 | 5.7 | 12.2 | 23.1 | 23.5 | 51.8 | <.001 | |
Cannot display percentage since cell size is less than 11 because of policies of the Centers for Medicare and Medicaid Services.
Perceived overall health was recorded as excellent, very good, good, fair, or poor. Comparative general health status relative to a year ago was recorded as much better, somewhat better, about the same, somewhat worse, or much worse. Amount of time that health limited contact with friends and family during the past month was recorded as none, some, most, or all of the time.
Analysis
All analyses incorporated the complex design of MCBS such as stratification, clustering, and weights.12 Baseline covariates were first examined among persons at different baseline ADL and IADL stages. Hazard ratios and 95% confidence intervals (CIs) for the associations between baseline ADL and IADL stage and three-year mortality were then estimated using proportional hazard models. A multivariable model for each domain (ADL or IADL stages) was fit as follows. 1) Unadjusted associations between three-year mortality and each variable were assessed. 2) An intermediate model was fit that included pre-specified variables (age, gender, race, education, social living circumstances, hypertension, myocardial infarction, angina or coronary artery diseases, congestive heart failure, heart valve problems, rhythm disturbance, stroke, cancer other than skin, osteoporosis, broken hip, emphysema or asthma, Parkinson’s disease, obviously paralyzed, diabetes type 1, 2, or other, mental retardation, Alzheimer’s, mental or psychiatric conditions, depression, or hardening of the arteries, smoking, psychological status and mood, global health perceptions, comparative health to a year ago, and social consequences of health) as well as any variable associated with three-year mortality using a threshold of p<0.2 in the unadjusted models. 3) Covariates were then removed through backward selection one by one starting from the one with the largest p-value, until all p-values were <0.05.
The validity of the proportional hazards assumption was tested by examining an interaction term between each variable in the final model and follow-up time, classified as <1.5 years or ≥1.5 years post baseline (1.5 years was chosen since it is the midpoint of three years). We included time interactions for each variable in any domain-specific model that had a p-value <0.05 before a final backward selection procedure was conducted to obtain the final models with main effects and interactions. Finally, to explore effects of potential collinearity between disability stage and perceived health status, we fit an additional Cox proportional hazard model excluding perceived health status variables. We used SAS version 9.4 (SAS Institute, Inc., Cary, NC) for descriptive analyses to compare the distribution of covariates according to ADL and IADL stage. We used the survey procedures of STATA/MP 13.1 (Stata Corp, Inc., College Station, TX) for regressions to take into account the complex survey design.
RESULTS
Table 2 presents baseline characteristics of Medicare beneficiaries 65 years of age and older by ADL and IADL stage. As expected, the prevalences of many disabling conditions (i.e., rheumatoid arthritis, Parkinson disease, Alzheimer disease, depression) were associated with ADL and IADL stage, although not monotonically in all cases. Also as expected, the prevalence of excellent and very good perceived health status tended to be lower in those with higher disability stages, although not monotonically in all cases.
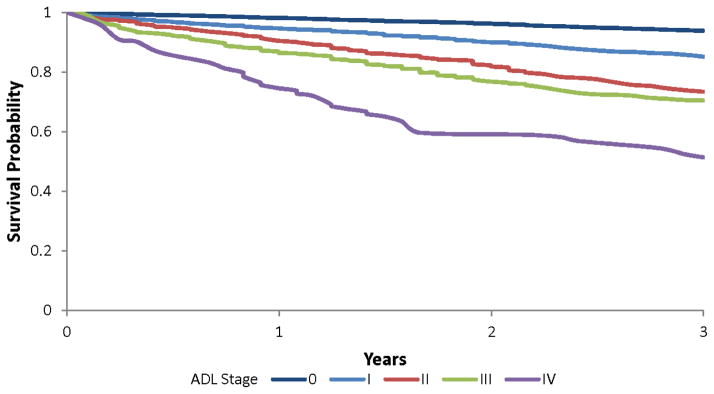
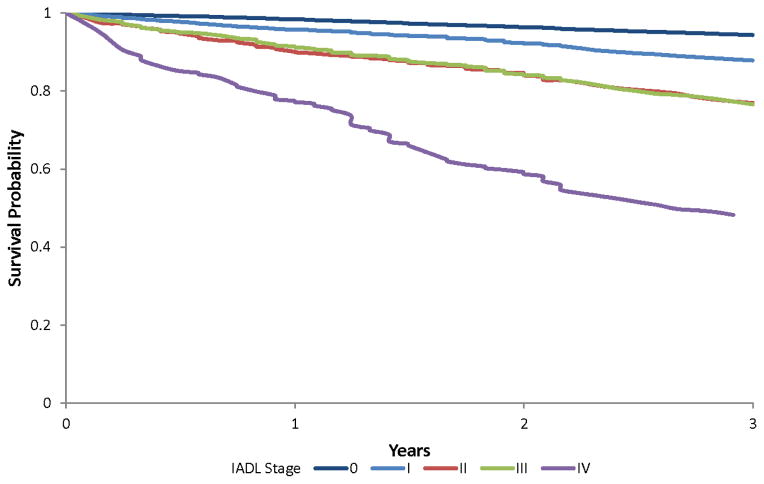
The overall mortality rate was 3.6 per 100 person years, and the cumulative incidence of mortality over three years was 10.3%. Both increasing ADL stage and increasing IADL stage were monotonically associated with unadjusted three-year cumulative mortality, although the differences between stage II and III were small in both the ADL and IADL staging systems (Table 2). This is also reflected in the similarity of the survival curves (Figure 1a and b) for stages II and III, especially in the IADL staging system. Except for these similarities in the curves for stages II and III, there was early and strong separation of survival curves by ADL and IADL stage.
Figure 1.
Figure 1a. Survival of Medicare Beneficiaries 65 Years of Age and Older by Activity of Daily Living (ADL) Stage Measured at Baseline
Figure 1b. Survival of Medicare Beneficiaries 65 Years of Age and Older by Instrumental Activity of Daily Living (IADL) Stage Measured at Baseline
The interaction between ADL stage and follow-up time was not statistically significant in the model including health perception (p=0.42) or in the model excluding it (p=0.33), indicating that the assumption of proportional hazards by ADL stage was not violated. The same was true for IADL stage in the model including health perception (p=0.85) and excluding it (p=0.69). However, hazard ratios for several covariates varied by follow-up duration. Therefore, the results presented in Table 3 allow hazard ratios for these covariates to vary by follow-up duration. Table 3 presents adjusted hazard ratios (with 95% CIs) for all-cause three-year mortality for each ADL and IADL stage, both adjusting for and not adjusting for perceived health status. Consistent with the unadjusted survival curves, higher ADL and IADL stages were associated with higher adjusted hazard ratios for death, except that in the IADL models the hazard ratio for stage III was numerically lower than that for stage II.
Table 3.
Adjusted Hazard Ratio (95% Confidence Interval) for All-cause Three-year Mortality for Activity of Daily Living (ADL) and Instrumental Activity of Daily Living (IADL) Stage
| ADL Stage | IADL Stage | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0 (n=6713) | I (n=1609) | II (n=758) | III (n=512) | IV (n=103) | 0 (n=6076) | I (n=1676) | II (n=713) | III (n=1014) | IV (n=216) | |
| Fully adjusted* | 1.0 (ref) | 1.3 (1.1–1.6) | 2.1 (1.7–2.5) | 2.1 (1.7–2.5) | 3.2 (2.2–4.6) | 1.0 (ref) | 1.3 (1.1–1.6) | 1.7 (1.4–2.1) | 1.7 (1.4–2.0) | 2.4 (1.8–3.2) |
| Health perception omitted† | 1.0 (ref) | 1.6 (1.3–1.9) | 2.5 (2.1–3.0) | 2.6 (2.1–3.2) | 4.7 (3.3–6.7) | 1.0 (ref) | 1.6 (1.3–1.9) | 2.6 (2.1–3.2) | 2.3 (1.9–2.7) | 4.2 (3.2–5.5) |
Ref denotes reference category
The ADL model included terms for sex, race, age (categorized as shown in Table 2), income (≥$25,000 versus <$25,000), social living circumstance, smoking status (never, past, or current), angina or coronary artery diseases, Alzheimer’s disease, amputation, congestive heart failure, arthritis other than rheumatoid, cancer, broken hip, depression, diabetes, incontinence, global health perceptions (excellent, very good, good, fair, or poor), comparative general health status to a year ago, amount of time health limits contact with friends and family during the past month, and interactions between age of “75–84”, “other type” of diabetes and time to death >1.5 years. The IADL model additionally included terms for education (less than high school versus high school and above) and interaction between health limits contact with friends and family during the past month “All of the time” and follow-up time >1.5 years.
The ADL model included all variables listed above for the ADL model except for global health perception, comparative general health status to a year ago, amount of time health limits contact with friends and family during the past month. The IADL model included all variables listed above except for global health perception, comparative general health status to a year ago, amount of time health limits contact with friends and family during the past month, and the interaction between health limits contact with friends and family during the past month “all of the time” and follow-up time >1.5 years. The latter were removed since they describe concepts similar to activity limitation.
DISCUSSION
Summary of Key Findings
The goal of this study was to assess the potential utility of ADL and IADL stages for population health applications by testing the hypothesis that disability stages5 are independent predictors of three-year mortality in Medicare beneficiaries 65 years of age and older. We observed strong and early separation of unadjusted survival curves by disability stage, except that survival curves for IADL stages II and III overlapped. In models assessing the independent associations of three-year mortality with ADL disability stage, we found nearly monotonic relationships. IADL stage was also independently associated with increased three-year mortality, with hazard ratios that were similar in magnitude to those of the ADL stages. Because stage III includes people whose disability patterns are outside the typical hierarchy, the observed non-fit of that stage was expected. Our results are consistent with those of prior studies that also found functional limitations to be associated with higher mortality.8,13–21
Significance of Findings
The findings of an association between MCBS-based ADL and IADL stages with three-year mortality are important because unlike earlier work with stages,7 this study used survey data that are collected on an ongoing basis, which permits the annual measurement of disability prevalence based on routinely collected data. Specifically, these staging systems will enable the ongoing analyses of samples representative of all non-institutionalized Medicare beneficiaries 65 years of age and older, which includes about 93% of all community-dwelling US residents in this age group.22
Stage profiles derived from such metrics can be used to identify groups of beneficiaries who are similar with respect to both the severity and the nature of the activity limitation experienced. For example, the IADL I cohort is by definition able to do all IADLs without difficulty except heavy housework, while the IADL IV cohort has difficulty in all IADLs.
There are a number of key clinical and policy implications of our findings. Particularly noteworthy are the findings that the hazard ratios for IADL limitations were of similar magnitude to those for ADL limitations. This implies that either ADL or IADL stages can be used to stratify populations by risk of mortality. Second, the relationship between disability stage and mortality was evident even after extensive adjustments for age, comorbidity and perceived health status variables. While these associations may be due to unmeasured or residual confounding rather than being causal, it remains possible that at least some of the individuals experiencing activity limitation may have had functional deficits that were remediable or even reversible, or may have faced access barriers that could be reduced or eliminated. Nevertheless, the strength of associations between disability stage and death might inform policy makers and health plan administrators who wish to identify subsets of the Medicare population who are at the greatest risk of death and who might benefit the most from interventions that ameliorate activity limitation. Further, such associations could facilitate the development of metrics for evaluating the success of economic, social, or health policies to help the disabled elderly. These metrics could support population surveillance applications such as those applied in Chart Books published periodically by the US Department of Health and Human Services,23 or as baseline or target measures for Healthy People objectives. Third, because self-reported ADL and IADL questions are easily collected from patients or family members, stage assessment might prove valuable as a clinical tool. Fourth, our findings of strong associations with mortality support the establishment of multivariable risk indices for mortality drawing on information from thousands of Medicare beneficiaries. Finally, early pilot work supports development of clinical tools for falls risk assessment, as well as for establishing the likelihood of nursing home placement and functional deterioration.24–27
Strengths and Limitations
A major strength of this study is its use of a representative sample of non-institutionalized Medicare beneficiaries, which makes its results broadly generalizable to the community-dwelling US population 65 years of age and older. Other strengths of the study include the large size and breadth of the data, the routine collection of MCBS data, and the richness of the data available for adjustment. A potential limitation is that despite our best efforts to identify independent effects of disability itself, we cannot be certain that the observed associations with disability stage are due wholly to persons’ activity limitations rather than to unmeasured medical conditions and other factors that contribute to those limitations. It may be that disability acts as a proxy for poor health. Further, our results are not generalizable to persons residing in long-term care facilities or to those younger than 65 years of age. There is also the potential for response bias and imperfect recall by participants. Although inclusion of proxies reduced selection bias it may also have increased measurement error.28
Conclusion
We found that ADL and IADL stages are highly associated with three-year mortality. As healthcare organizations move increasingly toward seeking population health rather than focusing solely on health of the individual, these stages could prove valuable to rehabilitation and other health professionals. Future research should examine associations between MCBS-derived ADL and IADL stages and other adverse outcomes. The utility of adding disability stages to predictive indices to identify high-risk patients in clinical settings also deserves evaluation. Finally, it will be important to develop and evaluate disability prevention and management strategies to reduce the burden of activity limitation. Stage-specific strategies might include patient-, family-, and community-level programs implemented in medical homes, accountable care organizations, and programs of all-inclusive care for elders (PACE) targeted to increase ADL and IADL functioning and to reduce mortality.
Acknowledgments
Neither the National Institutes of Health nor the Centers for Medicare and Medicaid Services (CMS) (which provided the data) played a role in the design or conduct of the study, in the analysis, or interpretation of the data, or in the preparation, review, or approval of the manuscript.
Funding source: This research was supported by the National Institutes of Health (R01AG040105, R01HD074756, R01AG025152, and R01DK102694).
Footnotes
There are no conflicts of interest of any of the authors.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.United states census bureau. [Accessed August 13, 2014];survey of income and program participation. https://www.census.gov/people/disability/publications/disab10/table_1.pdf.
- 2.Federal interagency forum on aging related statistics. [Accessed October 9, 2014];older americans (key indicators of well-being) http://www.agingstats.gov/agingstatsdotnet/Main_Site/Data/2010_Documents/docs/Health_Status.pdf.
- 3.World Health Organization. International Classification of Functioning, Disability and Health: ICF. Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- 4.Sox HC. Resolving the tension between population health and individual health care. JAMA. 2013;310(18):1933–1934. doi: 10.1001/jama.2013.281998. [DOI] [PubMed] [Google Scholar]
- 5.Stineman MG, Streim JE, Pan Q, Kurichi JE, Schussler-Fiorenza Rose SM, Xie D. Activity limitation stages empirically derived for activities of daily living (ADL) and instrumental ADL in the U.S. adult community-dwelling medicare population. PM R. 2014;6(11):976–987. doi: 10.1016/j.pmrj.2014.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.US department of health & human services. medicare current beneficiary survey (MCBS) 2010 http://www.cms.hhs.gov/MCBS/2014.
- 7.Stineman MG, Henry-Sanchez JT, Kurichi JE, et al. Staging activity limitation and participation restriction in elderly community-dwelling persons according to difficulties in self-care and domestic life functioning. Am J Phys Med Rehabil. 2012;91(2):126–140. doi: 10.1097/PHM.0b013e318241200d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang Z, Xie D, Kurichi JE, Streim J, Zhang G, Stineman MG. Mortality predictive indexes for the community-dwelling elderly US population. J Gen Intern Med. 2012;27(8):901–910. doi: 10.1007/s11606-012-2027-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stineman MG, Xie D, Pan Q, et al. All-cause 1-, 5-, and 10-year mortality in elderly people according to activities of daily living stage. J Am Geriatr Soc. 2012;60(3):485–492. doi: 10.1111/j.1532-5415.2011.03867.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kautter J, Khatutsky G, Pope GC, Chromy JR, Adler GS. Impact of nonresponse on medicare current beneficiary survey estimates. Health Care Financ Rev. 2006;27(4):71–93. [PMC free article] [PubMed] [Google Scholar]
- 11.Stineman MG, Xie D, Pan Q, Kurichi JE, Saliba D, Streim J. Activity of daily living staging, chronic health conditions, and perceived lack of home accessibility features for elderly people living in the community. J Am Geriatr Soc. 2011;59(3):454–462. doi: 10.1111/j.1532-5415.2010.03287.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lo AGA. Variance estimation and the componets of variance for the medicare current beneficiary survey sample. American Statistical Association Section on Survey Research Methods. 2005:3333–3341. [Google Scholar]
- 13.Lubitz J, Cai L, Kramarow E, Lentzner H. Health, life expectancy, and health care spending among the elderly. N Engl J Med. 2003;349(11):1048–1055. doi: 10.1056/NEJMsa020614. [DOI] [PubMed] [Google Scholar]
- 14.Covinsky KE, Eng C, Lui LY, Sands LP, Yaffe K. The last 2 years of life: Functional trajectories of frail older people. J Am Geriatr Soc. 2003;51(4):492–498. doi: 10.1046/j.1532-5415.2003.51157.x. jgs51157 [pii] [DOI] [PubMed] [Google Scholar]
- 15.Inouye SK, Peduzzi PN, Robison JT, Hughes JS, Horwitz RI, Concato J. Importance of functional measures in predicting mortality among older hospitalized patients. JAMA. 1998;279(15):1187–1193. doi: 10.1001/jama.279.15.1187. joc71756 [pii] [DOI] [PubMed] [Google Scholar]
- 16.Walter LC, Brand RJ, Counsell SR, et al. Development and validation of a prognostic index for 1-year mortality in older adults after hospitalization. JAMA. 2001;285(23):2987–2994. doi: 10.1001/jama.285.23.2987. joc01917 [pii] [DOI] [PubMed] [Google Scholar]
- 17.Covinsky KE, Justice AC, Rosenthal GE, Palmer RM, Landefeld CS. Measuring prognosis and case mix in hospitalized elders. the importance of functional status. J Gen Intern Med. 1997;12(4):203–208. doi: 10.1046/j.1525-1497.1997.012004203.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carey EC, Walter LC, Lindquist K, Covinsky KE. Development and validation of a functional morbidity index to predict mortality in community-dwelling elders. J Gen Intern Med. 2004;19(10):1027–1033. doi: 10.1111/j.1525-1497.2004.40016.x. JGI40016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cesari M, Onder G, Zamboni V, et al. Physical function and self-rated health status as predictors of mortality: Results from longitudinal analysis in the ilSIRENTE study. BMC Geriatr. 2008;8:34–2318. doi: 10.1186/1471-2318-8-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Keller BK, Potter JF. Predictors of mortality in outpatient geriatric evaluation and management clinic patients. J Gerontol. 1994;49(6):M246–51. doi: 10.1093/geronj/49.6.m246. [DOI] [PubMed] [Google Scholar]
- 21.Mayo NE, Nadeau L, Levesque L, Miller S, Poissant L, Tamblyn R. Does the addition of functional status indicators to case-mix adjustment indices improve prediction of hospitalization, institutionalization, and death in the elderly? Med Care. 2005;43(12):1194–1202. doi: 10.1097/01.mlr.0000185749.04875.cb. 00005650-200512000-00006 [pii] [DOI] [PubMed] [Google Scholar]
- 22.Administration on aging administration for community living. [Accessed October 3, 2014];A profile of older americans. 2012 http://www.aoa.gov/Aging_Statistics/Profile/2012/docs/2012profile.pdf.
- 23.Prevention CfDCa. [Accessed October 15, 2014];health, united states, 2013 - chartbook. 2013 http://www.cdc.gov/nchs/hus/chartbook.htm.
- 24.Henry-Sanchez JT, Kurichi JE, Xie D, Pan Q, Stineman MG. Do elderly people at more severe activity of daily living limitation stages fall more? Am J Phys Med Rehabil. 2012;91(7):601–610. doi: 10.1097/PHM.0b013e31825596af. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brown J, Kurichi JE, Xie D, Pan Q, Stineman MG. Instrumental activities of daily living staging as a possible clinical tool for falls risk assessment in physical medicine and rehabilitation. PM R. 2014;6(4):316–23. doi: 10.1016/j.pmrj.2013.10.007. quiz 323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stineman MG, Zhang G, Kurichi JE, et al. Prognosis for functional deterioration and functional improvement in late life among community-dwelling persons. PM R. 2013;5(5):360–371. doi: 10.1016/j.pmrj.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 27.Stineman MG, Xie D, Streim JE, et al. Home accessibility, living circumstances, stage of activity limitation, and nursing home use. Arch Phys Med Rehabil. 2012;93(9):1609–1616. doi: 10.1016/j.apmr.2012.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stineman MG, Ross RN, Maislin G. Functional status measures for integrating medical and social care. Int J Integr Care. 2005;5:e07P. doi: 10.5334/ijic.141. [DOI] [PMC free article] [PubMed] [Google Scholar]