Abstract
Ultrasound imaging has been used to evaluate various shoulder pathologies, whereas, quantification of the rotator cuff muscle stiffness using shear wave elastography (SWE) has not been verified. The purpose of this study was to investigate the reliability and feasibility of SWE measurements for the quantification of supraspinatus (SSP) muscle elasticity. Thirty cadaveric shoulders (18 intact and 12 with torn rotator cuff) were used. Intra- and inter-observer reliability was evaluated on an established SWE technique for measuring the SSP muscle elasticity. To assess the effect of overlying soft tissues above the SSP muscle, SWE values were measured with the transducer placed on the skin, on the subcutaneous fat after removing the skin, on the trapezius muscle after removing the subcutaneous fat, and directly on the SSP muscle. In addition, SWE measurements on 4 shoulder positions (0°, 30°, 60°, and 90° abduction) were compared in those with/without rotator cuff tears. Intra- and inter-observer reliability of SWE measurements were excellent for all regions in SSP muscle. Also, removing the overlying soft tissue showed no significant difference on SWE values measured in the SSP muscle. The SSP muscle with 0° abduction showed large SWE values, whereas, shoulders with large-massive tear showed smaller variation throughout the adduction-abduction positions. SWE is a reliable and feasible tool for quantitatively assessing the SSP muscle elasticity. This study also presented SWE measurements on the SSP muscle under various shoulder abduction positions which might help characterize patterns in accordance to the size of rotator cuff tears.
Keywords: Shear wave elastography, Supraspinatus muscle, Muscle elasticity: Reliability, Feasibility
INTRODUCTION
Rotator cuff tendon tear is a common cause of shoulder pain and dysfunction, especially in the middle-aged and elder population (Minagawa et al., 2013, Yamamoto et al., 2010). Symptomatic patients who have failed conservative management are required to undergo surgical treatment to restore the cuff function and/or to reduce their pain. Among various surgical options available, open or arthroscopic rotator cuff repair is favorably performed for small to large size tears (Buess et al., 2005, Galatz et al., 2004, Harryman et al., 1991). Although advanced repair techniques and devices have been proposed, relatively high prevalence of re-tear after surgery is still remaining (Bartl et al., 2012, Khazzam et al., 2012, Miller et al., 2011, Zumstein et al., 2008). Among multiple factors leading to re-tear, stiffness of the cuff muscles has been a recent focus for failure. As a stiffer rotator cuff muscle requires larger tensile forces to be repaired, consequently, excessive stresses could cause the re-tear (Itoigawa et al., 2015, Liu et al., 2011, Safran et al., 2005, Steinbacher et al., 2010).
Ultrasound B-mode imaging and MRI are currently applicable tools for preoperative planning and postoperative monitoring of the rotator cuff repair (Codsi et al., 2014, Lenza et al., 2013, Roy et al., 2015). These are mainly used to assess the tear (re-tear) size, gross structures and the presence of fatty degeneration in the rotator cuff muscles (Jain et al., 2015, Lenza et al., 2013); whereas, altered material properties of the muscle or tendon cannot be assessed adequately.
Several elastography techniques have been recently investigated to quantitatively assess material properties of muscles and other soft tissues. Magnetic resonance elastography (MRE) has shown the capability to measure passive stiffness of thigh muscles (Debernard et al., 2011). However, the cost and accessibility of MRE may not only interfere with its clinical application (Brandenburg et al., 2015), but the time required for a single measurement might prevent its implementation for therapies or evaluations in which multiple measurements at different joint positions are necessary. Similarly, ultrasound elastographic techniques have also been investigated to quantify the material properties of muscles. Of these, freehand sonoelastography has been shown to quantify the strain in tissues by measuring displacement under external mechanical compression (Niitsu et al., 2011). Using this technique, previous studies have assessed the material properties of shoulder muscles (Ishikawa et al., 2015, Muraki et al., 2015). Although studies have shown good feasibility and reliability of the technique, freehand compression with a consistent load still remains a technical challenge, with amplitude and/or velocity of loading compression yet to be established (Cantisani et al., 2015). Furthermore, adjacent bony structures to shoulder muscles, including the acromion, scapular spine, and clavicle have been shown to interfere with a uniform compression of the soft tissue (Hatta et al., 2014).
In contrast, shear wave elastography (SWE), an ultrasound technique, has been a recent focus for measuring muscle elastic modulus (Garra, 2007, Liu et al., 2011). In principle, uniform push beams are sent into the tissue, and shear waves within the muscle are generated and detected using the same ultrasound probe. The technique is fast, convenient and applicable to a variety of clinical scenarios in which other approaches would potentially be inadequate. To date, it has been used successfully for breast cancers diagnosis (Athanasiou et al., 2010, Park et al., 2014) and liver fibrosis staging (Ferraioli et al., 2014, Yoon et al., 2014). In addition, quantitative assessments of material properties of muscles have also been investigated by in vivo and in vitro studies (Akagi and Kusama, 2015, Hirata et al., 2015, Hug et al., 2013, Miyamoto et al., 2015, Itoigawa et al., 2015, Koo et al., 2014, Akagi et al., 2012). Assessment of the feasibility of supraspinatus (SSP) muscle stiffness with a potential for rotator cuff tear management has been attempted on intact cadaveric shoulders (Itoigawa et al., 2015). However, reliability or validity of the measurements has been less defined in the literature. In addition, the effect of overlying soft tissues, including the skin, subcutaneous fat, and trapezius muscle, on SWE measurements of deeper tissues has not been investigated. Since the acoustic push pulse from the ultrasound transducer propagates through multiple layers of soft tissues with different material properties before reaching the SSP muscles, it might be possible that the presence of overlying soft tissues affect the SWE values. Therefore, the effect of overlying soft tissues on SWE values of the SSP needs to be evaluated so that reliable measurements of muscle properties can be obtained and SWE can potentially be applied clinically for rotator cuff management and treatment. Moreover, we hypothesized that arm elevation would have an effect in the measured SWE values of the SSP muscle. These outcomes would be useful in the clinic for determining SWE patterns in the assessment of muscular properties related to varying shoulder positions. In particular, material properties in the SSP muscle with various conditions of rotator cuff (intact or small to massive tear) have been less documented. Thus, we also studied if muscles with rotator cuff tears presented any differences in SWE measurements, potentially providing a new tool for diagnosis of these pathologies. In summary, the purposes of the study were threefold: 1) to assess the intra- and inter-observer reliability of SWE measurements, 2) to investigate the effect of soft tissues overlying the SSP muscle, and 3) to determine the variability of SWE values based on the various shoulder abduction angles using cadaveric shoulders with and without rotator cuff tears.
MATERIAL AND METHODS
Specimen Preparation
Thirty fresh-frozen cadaveric shoulders obtained from 30 subjects were used for this study after internal approval from the bio-specimens committee at Mayo Clinic. Before the experiment, the scapula was disarticulated from the thorax, and the humerus was cut at the level of the midshaft. The scapula and a fiberglass rod inserted into the humeral medullary canal were both secured in a custom-designed experimental device made of fiberglass and Plexiglas (Altuglas International, Arkema Ltd., Philadelphia, PA; Fig. 1). Based on the International Society of Biomechanics (ISB) recommendation and relevant studies, the scapula was secured at 0° of upward/downward rotation considered as a neutral position (Schwartz et al., 2014, Wu et al., 2005). The device, designed to provide 6 degrees-of-freedom motion of the glenohumeral joint in consistent motion paths, was used to abduct the humerus parallel to the scapular plane.
Fig. 1.
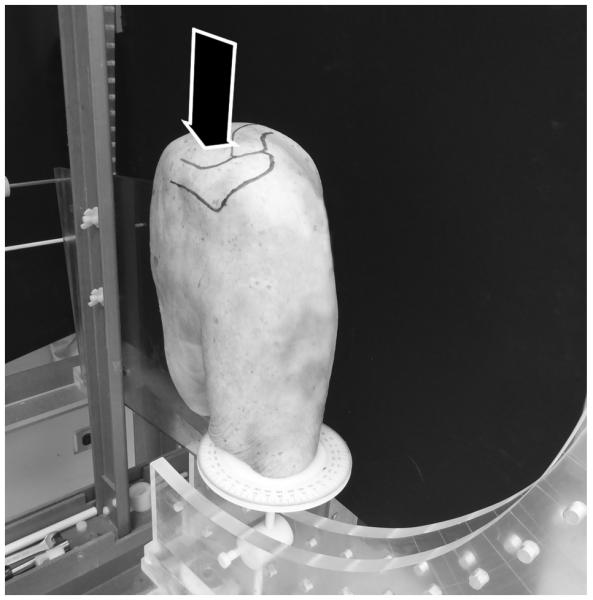
A custom-made fixture device was used to secure the scapula and a fiber glass rod inserted into the humeral medullary canal to position the humerus. Black arrow indicates the placement of the ultrasound transducer corresponding to the belly of the SSP muscle.
Experimental Procedure
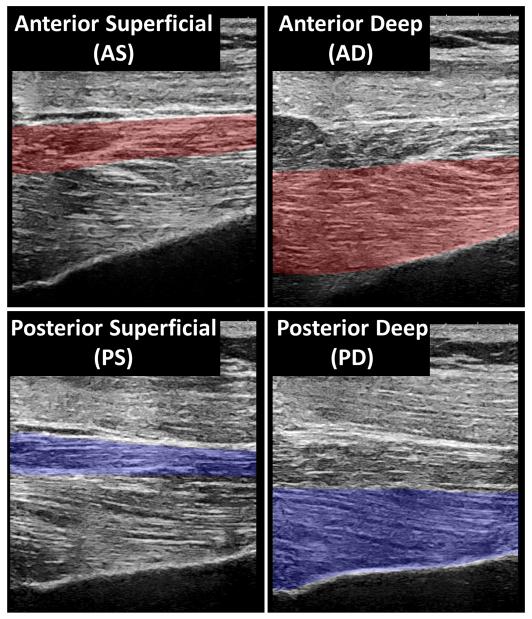
A commercial ultrasound system (Aixplorer; Supersonic Imagine, Ltd, Aix-en-provence, France) and a linear array transducer (2-10 MHz; Supersonic Imagine, Ltd) were used to perform the ultrasound examinations. Images for the SWE measurements were obtained based on an established methodology (Itoigawa et al., 2015). Briefly, four muscular regions were divided according to the muscle fiber orientation (anterior deep [AD], anterior superficial [AS], posterior deep [PD], and posterior superficial [PS]), and SWE measurements for each region were assessed independently on the plane parallel to the muscle fibers (Fig. 2). A built-in-software was used to obtain the elastic modulus (kPa) for each region. In order to consider any technical variation arising from probe positioning or probe pressure, SWE values were measured repeatedly 9 times as previously described (Hatta et al., 2014). Briefly, the ultrasound probe was positioned on the muscle of interest, data was acquired, and the probe was then lifted from the muscle before an additional measurement was performed. This process was repeated 9 times. The mean SWE values were calculated for all regions from these images to obtain the elastic modulus of the muscle region. Coefficients of variation (CV) were also calculated to assess SWE repeatability.
Fig. 2.
Quadrisected regions of the supraspinatus (SSP) muscle for shear wave elastography (SWE). The SSP muscles were divided into 4 regions: anterior deep (AD), anterior superficial (AS), posterior deep (PD), and posterior superficial (PS) based on the muscular fiber orientation. The SWE measurements were performed for each region.
Overlying Soft Tissue Assessment
Before addressing the effect of soft tissues overlying the SSP muscle, 12 cadavers were used to assess intra- and inter-observer reliability. Using the fixture device, cadavers were placed with the shoulder positions of 0° abduction and 0° rotation. Three investigators (T.H., K.U., and S.O.) measured SWE values independently. One investigator (T.H.) repeated the measurements twice at 1 hour interval to assess intra-observer reproducibility. Subsequently, these 12 cadavers were used to test the effect of soft tissue on SWE values. First, the skin was removed and SWE for the SSP muscle was examined by a trans-subcutaneous fat approach. Next, after removing the subcutaneous fat tissue overlying the trapezius muscle, SWE was examined by a trans-trapezius muscle approach. Finally, the SSP muscle was exposed by stripping off the overlying trapezius muscle. After placing the transducer on top of the SSP muscle via adequate ultrasound coupling gel, SWE values were obtained by a direct approach.
Abduction Angle Assessment
Thirty cadaveric shoulders were used to measure SWE values of the supraspinatus muscle subjected to various passive muscular stiffness based on the shoulder abduction/adduction. Specimens were placed with the arm at 0°, 30°, 60°, and 90° abduction. The arm was kept with 0° rotation during all measurements. SWE values were measured, 9 times as previously described, for each shoulder position. Furthermore, SWE values between intact and cuff tear specimens were compared to address the effect of cuff conditions on elasticity measurements (SWE values). For this analysis, cuff tear specimens were divided into two sub-groups; small-medium tear and large-massive tear group, and compared to the intact shoulders.
Rotator Cuff Tear Assessment
The size of the tears in those with rotator cuff tear was measured macroscopically after all overlying tissues were removed with a digital caliper, and then classified according to the classification by Post et al (Post et al., 1983). In brief, measured in its longest diameter, each tear was defined as a small (less than 1 cm), medium (less than 3 cm), large (less than 5 cm), or massive tear (more than 5 cm).
Statistical Analyses
Intra- and inter-observer reliability was examined using intraclass correlation coefficient (ICC; ICC(1,1) and ICC(2,1), respectively). Continuous variables of SWE data were tested for normality and equal variance before following statistical analyses. Because the data did not present a normal distribution, non-parametric tests were performed. Friedman with Dunn’s post hoc tests was used to evaluate the difference in SWE values for the overlaying soft tissues approach (percutaneous, trans-subcutaneous fat, trans-trapezius muscle, and direct approach), and abduction angles (0°, 30°, 60°, and 90° abduction). SWE values for different cuff conditions (intact, small-medium, and large-massive) were compared using Kruskal-Wallis with Dunn’s post hoc tests. Statistical analyses were performed using the software SPSS (version 18.0, SPSS, Chicago, IL) and GraphPad Prism (version 6.0, GraphPad Prism, San Diego, CA). The level of significance was set at a P value of 0.05.
RESULTS
Of the 30 total shoulders, 18 shoulders (mean age, 76 years [50-92 years]; 5 males and 13 females) had an intact rotator cuff (no tears), and 12 shoulders (mean age, 82 years [72-90 years]; 4 males and 8 females) had a rotator cuff tear. There were 5 shoulders with small tear, 2 shoulders with medium tear, 4 shoulders with large tear, and 1 shoulder with massive tear.
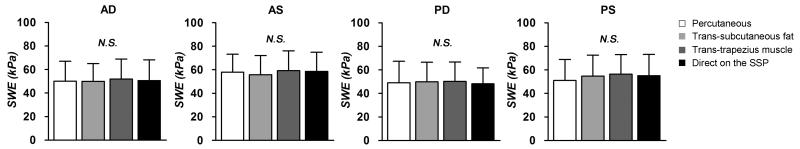
The elastic moduli of the SSP muscle were successfully obtained for all conditions and experimental approaches. Mean (standard deviation) of coefficients of variation (CV) of elastic modulus among overall measurements was 4.93 (3.05) %, indicating good repeatability among 9 SWE images. Intra-observer reproducibility and the inter-observer reliability was satisfactory for all regions of the SSP muscle (ICC(1,1) of 0.945 – 0.970, ICC(2,1) of 0.882 – 0.948, respectively) (Table 1). SWE values of the SSP muscle showed no significant difference with the sequential removal of the overlying soft tissues (P = .475 to .593; Fig. 3).
Table 1.
Reliability of the shear wave elastography (SWE)
| Intra-observer | Inter-observer | |
|---|---|---|
| AD | 0.948 [0.838 - 0.985] | 0.928 [0.825 - 0.976] |
| AS | 0.970 [0.902 - 0.991] | 0.882 [0.729 - 0.961] |
| PD | 0.959 [0.870 - 0.988] | 0.928 [0.827 - 0.977] |
| PS | 0.945 [0.828 - 0.984] | 0.948 [0.871 - 0.983] |
Values represent intraclass correlation coefficient (ICC) [95% confidence interval].
ICC(1,1) and ICC(2,1) were used for intra- and inter-observer reliability.
Fig. 3.
The SWE values for the SSP muscles obtained with the 4 measurement approaches: percutaneous approach, trans-subcutaneous fat tissue approach, trans-trapezius muscle approach, and direct SSP approach. N.S.; not significant.
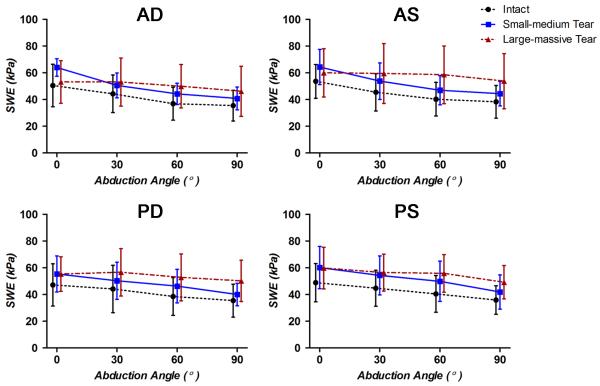
SWE values in the intact and small-medium groups were higher in all four regions (AD, AS, PD and PS) with the arm at 0° abduction compared to other angles (Table 2). In the intact shoulder group (N = 18), SWE values decreased with increased shoulder abduction, with significant differences in 0°-30° at AS (P = .012), 30°-60° at AD (P = .002) and PS (P = .027), and at all four regions for 0°-60° (P < .001), 0°-90° (P < .001) and 30°-90° (P < .001 to = .018). The small-medium tear groups (N = 7) showed a similar trend. SWE values were significantly decreased in abducted shoulders when comparing 0°-60° at AD and AS (P = .043), 30°-90° at AS, PD and PS (P = .011), and 0°-90° at all 4 regions (P < .001 to = .003). On the other hand, the large-massive tear group (N = 5) showed no significant differences of the SWE values throughout the adduction-abduction.
Table 2.
SWE values (mean ± SD) associated with shoulder abduction
| 0° | 30° | 60° | 90° | P values | |||||
|---|---|---|---|---|---|---|---|---|---|
| 0°-30° | 0°- 60° | 0°- 90° | 30°- 60° | 30°- 90° | |||||
| Intact (N = 18) | |||||||||
| AD | 50.5 ± 15.8 | 44.2 ± 14.1 | 36.9 ± 12.3 | 35.4 ± 11.4 | < .001 | < .001 | .002 | .003 | |
| AS | 53.6 ± 12.7 | 45.4 ± 14.0 | 40.3 ± 12.6 | 38.3 ± 12.3 | .012 | < .001 | < .001 | .012 | |
| PD | 47.1 ± 15.8 | 44.2 ± 17.7 | 38.6 ± 14.1 | 35.4 ± 12.3 | < .001 | < .001 | .018 | ||
| PS | 48.9 ± 14.4 | 44.7 ± 13.5 | 40.5 ± 13.7 | 35.9 ± 10.7 | < .001 | < .001 | .027 | < .001 | |
| Small-medium Tear (N = 7) | |||||||||
| AD | 63.9 ± 6.5 | 50.6 ± 9.3 | 44.2 ± 7.9 | 40.8 ± 8.5 | .043 | .003 | |||
| AS | 64.3 ± 13.2 | 53.8 ± 13.6 | 47.0 ± 10.9 | 44.4 ± 9.1 | .043 | < .001 | .011 | ||
| PD | 55.4 ± 13.4 | 50.3 ± 13.9 | 46.3 ± 12.5 | 40.6 ± 8.4 | < .001 | .011 | |||
| PS | 60.2 ± 15.8 | 54.3 ± 14.5 | 49.9 ± 15.1 | 41.9 ± 12.8 | < .001 | .011 | |||
| Large-massive Tear (N = 5) | |||||||||
| AD | 53.1 ± 15.9 | 53.0 ± 18.0 | 50.0 ± 16.2 | 46.1 ± 18.7 | |||||
| AS | 59.9 ± 18.1 | 59.5 ± 22.3 | 58.5 ± 21.5 | 53.8 ± 20.6 | |||||
| PD | 55.3 ± 12.9 | 56.6 ± 17.7 | 52.8 ± 17.5 | 50.2 ± 15.4 | |||||
| PS | 59.8 ± 15.6 | 56.4 ± 13.8 | 55.8 ± 14.0 | 49.2 ± 12.5 | |||||
Comparison among shoulder abductions was analyzed using Friedman test.
There were no significant differences among the groups for rotator cuff conditions (intact, small-medium, and large-massive tear groups) throughout adducted-abducted positions. However, with the arm in abduction, the mean SWE values showed a higher trend in the large-massive tear group compared to those in the intact and small-medium tear shoulder groups (P = .090 to .196 at 60°, and P = .083 to .156 at 90° abduction; Fig. 4).
Fig. 4.
The alteration of the SWE values in association with shoulder abduction.
DISCUSSION
The reliability and validity of elastographic measurements have been investigated in several studies (Park et al., 2014, Yoon et al., 2014). Regarding the muscular tissues, in particular, the crural and the brachial muscles have been shown to have good measurement reliably with satisfactory ICCs (Brandenburg et al., 2015, Koo et al., 2013, Koo et al., 2014, Taniguchi et al., 2015). These muscles are known to have relatively consistent muscle fiber orientation. Therefore, SWE measurements might provide reliable material property measurements by aligning the transducer imaging plane with the muscle fiber orientation (Miyamoto et al., 2015, Eby et al., 2015, Taniguchi et al., 2015). On the other hand, the SSP muscle has more complicated fiber architectures (Itoigawa et al., 2015, Kim et al., 2010). Previous investigators have examined the segmented assessment for SSP muscle properties divided into several regions based on the muscle fiber orientation. In particular, Itoigawa et al (Itoigawa et al., 2015) proposed a quadrisection of the muscle for SWE assessment. Accordingly, our study analyzed these 4 regions and showed satisfactory values of ICCs for each region supporting this methodology as a reliable approach for SSP muscles.
A previous study by Hatta et al (Hatta et al., 2014) reported a minimal effect of overlying tissues using other elastographic technique (freehand sonoelastography). To our knowledge, this is the first study to assess the effect of overlying soft tissues of the SWE technique. In the clinical setting, the extent of soft tissues on top of the SSP muscle may vary among subjects, such as the thickness of subcutaneous fat tissue and/or trapezius muscle. This study demonstrated that the presence of these soft tissues did not affect the SWE values. Although our results were obtained from cadaveric specimens, these findings indicate that elasticity measurements could be obtained without a significant influence of such overlying soft tissues.
This study also described the effect of the estimated elastic modulus of the SSP muscle via SWE based on shoulder abduction angles. Most of the shoulders demonstrated high SWE values with the arm in adducted position. Especially in intact shoulders, SWE values gradually decreased with increased shoulder abduction. These results indicate an increased passive stiffness due to the elongated SSP muscles. It is notable that shoulders with small to middle size tear also presented similar patterns with shoulder abduction, although with limited significances compared to intact shoulders. On the other hand, shoulders with large to massive rotator cuff tears showed almost no change in SWE values with respect to the abduction angles. Consequently, although not significant, the SSP muscle in large-massive rotator cuff tears showed higher SWE values with abducted shoulders in comparison with those without tears. This characteristic pattern in larger tears might be caused by the relaxation of the muscle and the absence of passive tension during abduction (Akagi et al., 2012, Dresner et al., 2001). As the tension of the SSP muscle with large or massive tear is independent of the humeral positions because of a discontinuity with the humerus, chronically the muscle might become a stiffer structure due to a loss of the stretched conditions.
The strength of the ultrasound technique in the clinical setting is the dynamic visualization of the shoulder with various arm positions. A combination of ultrasound techniques, such as B-mode and SWE, may provide dynamic assessment of rotator cuff tears detecting not only anatomical pathologies but also biomechanical degradation. The results presented in this study show representative data of SWE values and patterns under adduction-abduction in shoulders with various sizes of cuff tear as well as standard patterns in intact shoulders.
There are several limitations in this study. First, the SWE data for the SSP muscle were obtained from cadaveric shoulders. This study addressed the reliability and validity of SWE values evaluating passive SSP muscle elasticity on cadaveric specimens. In addition, cadaveric assessment on the effect of overlying soft tissues showed these to have a minimal effect on SWE values of the SSP. It is important to note that fresh-frozen cadaveric muscles have shown altered mechanical properties in response to mechanical loadings (Gottsauner-Wolf et al., 1995, Van Ee et al., 2000). Therefore, further studies using in vivo subjects should be carried out to complement these cadaveric findings, especially in comparing SWE outcomes between intact and torn rotator cuff tendons as well as muscle measurements over time. Furthermore, even in in vivo passive assessment, there might be low-level muscular activation, which could potentially result in altered SWE values compared to the results obtained in this study. Further assessment of the SSP muscle with both actively and passively abducted shoulders could also address the effect of such muscular activities on the variance of the SWE values. Second, we divided 30 shoulders into three groups based on cuff conditions (intact, small-middle, and large-massive). Although a specific SWE pattern during shoulder abduction was observed among all groups, a difference in group sample number, especially in the cuff tear groups, might have affected our final outcome. Both tear groups presented fewer shoulders compared to the intact group due to the difficulty in obtaining pathological shoulders. Further studies including more specimens with various sizes of tear would define SWE patterns related to an increased tear size.
CONCLUSION
We investigated the reliability and feasibility of shear wave elastography (SWE) for quantitatively assessing supraspinatus (SSP) muscle elasticity using cadaveric shoulders. Our results suggested that this technique may be reliably used without significant influences by the overlying soft tissues. Furthermore, this study showed SWE measurements on the SSP muscle under various shoulder abduction positions. Although this was a cadaveric study, the SWE patterns obtained under different shoulder positions provided valuable insight into its possible application for characterizing patterns based on the size of rotator cuff tears under shoulder abduction-adduction positions. Future studies should investigate SWE patterns in patients with rotator cuff tears and various shoulder positions.
Acknowledgement
Research reported in this publication was supported by the National Institute of Arthritis And Musculoskeletal And Skin Diseases of the National Institutes of Health under Award Number R21 AR065550 and T32 AR56950. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of interest statement
The authors confirm that there is no potential conflict of interest, including employment, consultancies, stock ownership, honoraria and paid expert testimony and patent applications, influencing this work.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Akagi R, Chino K, Dohi M, Takahashi H. Relationships between muscle size and hardness of the medial gastrocnemius at different ankle joint angles in young men. Acta radiologica. 2012;53:307–11. doi: 10.1258/ar.2011.110481. [DOI] [PubMed] [Google Scholar]
- Akagi R, Kusama S. Comparison Between Neck and Shoulder Stiffness Determined by Shear Wave Ultrasound Elastography and a Muscle Hardness Meter. Ultrasound in medicine & biology. 2015;41:2266–71. doi: 10.1016/j.ultrasmedbio.2015.04.001. [DOI] [PubMed] [Google Scholar]
- Athanasiou A, Tardivon A, Tanter M, Sigal-Zafrani B, Bercoff J, Deffieux T, Gennisson JL, Fink M, Neuenschwander S. Breast lesions: quantitative elastography with supersonic shear imaging--preliminary results. Radiology. 2010;256:297–303. doi: 10.1148/radiol.10090385. [DOI] [PubMed] [Google Scholar]
- Bartl C, Kouloumentas P, Holzapfel K, Eichhorn S, Wortler K, Imhoff A, Salzmann GM. Long-term outcome and structural integrity following open repair of massive rotator cuff tears. International journal of shoulder surgery. 2012;6:1–8. doi: 10.4103/0973-6042.94304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandenburg JE, Eby SF, Song P, Zhao H, Landry BW, Kingsley-Berg S, Bamlet WR, Chen S, Sieck GC, An KN. Feasibility and reliability of quantifying passive muscle stiffness in young children by using shear wave ultrasound elastography. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2015;34:663–70. doi: 10.7863/ultra.34.4.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buess E, Steuber KU, Waibl B. Open versus arthroscopic rotator cuff repair: a comparative view of 96 cases. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2005;21:597–604. doi: 10.1016/j.arthro.2005.01.002. [DOI] [PubMed] [Google Scholar]
- Cantisani V, Maceroni P, D'Andrea V, Patrizi G, Di Segni M, De Vito C, Grazhdani H, Isidori AM, Giannetta E, Redler A, Frattaroli F, Giacomelli L, Di Rocco G, Catalano C, D'Ambrosio F. Strain ratio ultrasound elastography increases the accuracy of colour-Doppler ultrasound in the evaluation of Thy-3 nodules. A bi-centre university experience. European radiology. 2015 doi: 10.1007/s00330-015-3956-0. [DOI] [PubMed] [Google Scholar]
- Codsi MJ, Rodeo SA, Scalise JJ, Moorehead TM, Ma CB. Assessment of rotator cuff repair integrity using ultrasound and magnetic resonance imaging in a multicenter study. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons … [et al.] 2014;23:1468–72. doi: 10.1016/j.jse.2014.01.045. [DOI] [PubMed] [Google Scholar]
- Debernard L, Robert L, Charleux F, Bensamoun SF. Analysis of thigh muscle stiffness from childhood to adulthood using magnetic resonance elastography (MRE) technique. Clinical biomechanics. 2011;26:836–40. doi: 10.1016/j.clinbiomech.2011.04.004. [DOI] [PubMed] [Google Scholar]
- Dresner MA, Rose GH, Rossman PJ, Muthupillai R, Manduca A, Ehman RL. Magnetic resonance elastography of skeletal muscle. Journal of magnetic resonance imaging : JMRI. 2001;13:269–76. doi: 10.1002/1522-2586(200102)13:2<269::aid-jmri1039>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Eby SF, Cloud BA, Brandenburg JE, Giambini H, Song P, Chen S, LeBrasseur NK, An KN. Shear wave elastography of passive skeletal muscle stiffness: influences of sex and age throughout adulthood. Clinical biomechanics. 2015;30:22–7. doi: 10.1016/j.clinbiomech.2014.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferraioli G, Parekh P, Levitov AB, Filice C. Shear wave elastography for evaluation of liver fibrosis. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2014;33:197–203. doi: 10.7863/ultra.33.2.197. [DOI] [PubMed] [Google Scholar]
- Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. The Journal of bone and joint surgery. American volume. 2004;86-A:219–24. doi: 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- Garra BS. Imaging and estimation of tissue elasticity by ultrasound. Ultrasound quarterly. 2007;23:255–68. doi: 10.1097/ruq.0b013e31815b7ed6. [DOI] [PubMed] [Google Scholar]
- Gottsauner-Wolf F, Grabowski JJ, Chao EY, An KN. Effects of freeze/thaw conditioning on the tensile properties and failure mode of bone-muscle-bone units: a biomechanical and histological study in dogs. Journal of orthopaedic research : official publication of the Orthopaedic Research Society. 1995;13:90–5. doi: 10.1002/jor.1100130114. [DOI] [PubMed] [Google Scholar]
- Harryman DT, 2nd, Mack LA, Wang KY, Jackins SE, Richardson ML, Matsen FA., 3rd Repairs of the rotator cuff. Correlation of functional results with integrity of the cuff. The Journal of bone and joint surgery. American volume. 1991;73:982–9. [PubMed] [Google Scholar]
- Hatta T, Yamamoto N, Sano H, Itoi E. In vivo measurement of rotator cuff tendon strain with ultrasound elastography: an investigation using a porcine model. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2014;33:1641–6. doi: 10.7863/ultra.33.9.1641. [DOI] [PubMed] [Google Scholar]
- Hirata K, Kanehisa H, Miyamoto-Mikami E, Miyamoto N. Evidence for intermuscle difference in slack angle in human triceps surae. Journal of biomechanics. 2015;48:1210–3. doi: 10.1016/j.jbiomech.2015.01.039. [DOI] [PubMed] [Google Scholar]
- Hug F, Lacourpaille L, Maisetti O, Nordez A. Slack length of gastrocnemius medialis and Achilles tendon occurs at different ankle angles. Journal of biomechanics. 2013;46:2534–8. doi: 10.1016/j.jbiomech.2013.07.015. [DOI] [PubMed] [Google Scholar]
- Ishikawa H, Muraki T, Sekiguchi Y, Ishijima T, Morise S, Yamamoto N, Itoi E, Izumi S. Noninvasive assessment of the activity of the shoulder girdle muscles using ultrasound real-time tissue elastography. Journal of electromyography and kinesiology : official journal of the International Society of Electrophysiological Kinesiology. 2015;25:723–30. doi: 10.1016/j.jelekin.2015.07.010. [DOI] [PubMed] [Google Scholar]
- Itoigawa Y, Sperling JW, Steinmann SP, Chen Q, Song P, Chen S, Itoi E, Hatta T, An KN. Feasibility assessment of shear wave elastography to rotator cuff muscle. Clinical anatomy. 2015;28:213–8. doi: 10.1002/ca.22498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain NB, Collins J, Newman JS, Katz JN, Losina E, Higgins LD. Reliability of Magnetic Resonance Imaging Assessment of Rotator Cuff: The ROW Study. PM & R : the journal of injury, function, and rehabilitation. 2015;7:245–254. e3. doi: 10.1016/j.pmrj.2014.08.949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khazzam M, Kuhn JE, Mulligan E, Abboud JA, Baumgarten KM, Brophy RH, Jones GL, Miller B, Smith M, Wright RW. Magnetic resonance imaging identification of rotator cuff retears after repair: interobserver and intraobserver agreement. The American journal of sports medicine. 2012;40:1722–7. doi: 10.1177/0363546512449424. [DOI] [PubMed] [Google Scholar]
- Kim S, Bleakney R, Boynton E, Ravichandiran K, Rindlisbacher T, McKee N, Agur A. Investigation of the static and dynamic musculotendinous architecture of supraspinatus. Clinical anatomy. 2010;23:48–55. doi: 10.1002/ca.20896. [DOI] [PubMed] [Google Scholar]
- Koo TK, Guo JY, Cohen JH, Parker KJ. Relationship between shear elastic modulus and passive muscle force: an ex-vivo study. Journal of biomechanics. 2013;46:2053–9. doi: 10.1016/j.jbiomech.2013.05.016. [DOI] [PubMed] [Google Scholar]
- Koo TK, Guo JY, Cohen JH, Parker KJ. Quantifying the passive stretching response of human tibialis anterior muscle using shear wave elastography. Clinical biomechanics. 2014;29:33–9. doi: 10.1016/j.clinbiomech.2013.11.009. [DOI] [PubMed] [Google Scholar]
- Lenza M, Buchbinder R, Takwoingi Y, Johnston RV, Hanchard NC, Faloppa F. Magnetic resonance imaging, magnetic resonance arthrography and ultrasonography for assessing rotator cuff tears in people with shoulder pain for whom surgery is being considered. The Cochrane database of systematic reviews. 2013;9 doi: 10.1002/14651858.CD009020.pub2. CD009020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X, Manzano G, Kim HT, Feeley BT. A rat model of massive rotator cuff tears. Journal of orthopaedic research : official publication of the Orthopaedic Research Society. 2011;29:588–95. doi: 10.1002/jor.21266. [DOI] [PubMed] [Google Scholar]
- Miller BS, Downie BK, Kohen RB, Kijek T, Lesniak B, Jacobson JA, Hughes RE, Carpenter JE. When do rotator cuff repairs fail? Serial ultrasound examination after arthroscopic repair of large and massive rotator cuff tears. The American journal of sports medicine. 2011;39:2064–70. doi: 10.1177/0363546511413372. [DOI] [PubMed] [Google Scholar]
- Minagawa H, Yamamoto N, Abe H, Fukuda M, Seki N, Kikuchi K, Kijima H, Itoi E. Prevalence of symptomatic and asymptomatic rotator cuff tears in the general population: From mass-screening in one village. Journal of orthopaedics. 2013;10:8–12. doi: 10.1016/j.jor.2013.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyamoto N, Hirata K, Kanehisa H, Yoshitake Y. Validity of measurement of shear modulus by ultrasound shear wave elastography in human pennate muscle. PloS one. 2015;10:e0124311. doi: 10.1371/journal.pone.0124311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muraki T, Ishikawa H, Morise S, Yamamoto N, Sano H, Itoi E, Izumi S. Ultrasound elastography-based assessment of the elasticity of the supraspinatus muscle and tendon during muscle contraction. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons … [et al.] 2015;24:120–6. doi: 10.1016/j.jse.2014.04.012. [DOI] [PubMed] [Google Scholar]
- Niitsu M, Michizaki A, Endo A, Takei H, Yanagisawa O. Muscle hardness measurement by using ultrasound elastography: a feasibility study. Acta radiologica. 2011;52:99–105. doi: 10.1258/ar.2010.100190. [DOI] [PubMed] [Google Scholar]
- Park HY, Han KH, Yoon JH, Moon HJ, Kim MJ, Kim EK. Intra-observer reproducibility and diagnostic performance of breast shear-wave elastography in Asian women. Ultrasound in medicine & biology. 2014;40:1058–64. doi: 10.1016/j.ultrasmedbio.2013.12.021. [DOI] [PubMed] [Google Scholar]
- Post M, Silver R, Singh M. Rotator cuff tear. Diagnosis and treatment. Clinical orthopaedics and related research. 1983:78–91. [PubMed] [Google Scholar]
- Roy JS, Braen C, Leblond J, Desmeules F, Dionne CE, MacDermid JC, Bureau NJ, Fremont P. Diagnostic accuracy of ultrasonography, MRI and MR arthrography in the characterisation of rotator cuff disorders: a meta-analysis. British journal of sports medicine. 2015 doi: 10.1136/bjsports-2014-094148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safran O, Derwin KA, Powell K, Iannotti JP. Changes in rotator cuff muscle volume, fat content, and passive mechanics after chronic detachment in a canine model. The Journal of bone and joint surgery. American volume. 2005;87:2662–70. doi: 10.2106/JBJS.D.02421. [DOI] [PubMed] [Google Scholar]
- Schwartz C, Croisier JL, Rigaux E, Denoel V, Bruls O, Forthomme B. Dominance effect on scapula 3-dimensional posture and kinematics in healthy male and female populations. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons … [et al.] 2014;23:873–81. doi: 10.1016/j.jse.2013.08.020. [DOI] [PubMed] [Google Scholar]
- Steinbacher P, Tauber M, Kogler S, Stoiber W, Resch H, Sanger AM. Effects of rotator cuff ruptures on the cellular and intracellular composition of the human supraspinatus muscle. Tissue & cell. 2010;42:37–41. doi: 10.1016/j.tice.2009.07.001. [DOI] [PubMed] [Google Scholar]
- Taniguchi K, Shinohara M, Nozaki S, Katayose M. Acute decrease in the stiffness of resting muscle belly due to static stretching. Scandinavian journal of medicine & science in sports. 2015;25:32–40. doi: 10.1111/sms.12146. [DOI] [PubMed] [Google Scholar]
- Van Ee CA, Chasse AL, Myers BS. Quantifying skeletal muscle properties in cadaveric test specimens: effects of mechanical loading, postmortem time, and freezer storage. Journal of biomechanical engineering. 2000;122:9–14. doi: 10.1115/1.429621. [DOI] [PubMed] [Google Scholar]
- Wu G, van der Helm FC, Veeger HE, Makhsous M, Van Roy P, Anglin C, Nagels J, Karduna AR, McQuade K, Wang X, Werner FW, Buchholz B. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion--Part II: shoulder, elbow, wrist and hand. Journal of biomechanics. 2005;38:981–992. doi: 10.1016/j.jbiomech.2004.05.042. [DOI] [PubMed] [Google Scholar]
- Yamamoto A, Takagishi K, Osawa T, Yanagawa T, Nakajima D, Shitara H, Kobayashi T. Prevalence and risk factors of a rotator cuff tear in the general population. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons … [et al.] 2010;19:116–20. doi: 10.1016/j.jse.2009.04.006. [DOI] [PubMed] [Google Scholar]
- Yoon JH, Lee JM, Han JK, Choi BI. Shear wave elastography for liver stiffness measurement in clinical sonographic examinations: evaluation of intraobserver reproducibility, technical failure, and unreliable stiffness measurements. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2014;33:437–47. doi: 10.7863/ultra.33.3.437. [DOI] [PubMed] [Google Scholar]
- Zumstein MA, Jost B, Hempel J, Hodler J, Gerber C. The clinical and structural long-term results of open repair of massive tears of the rotator cuff. The Journal of bone and joint surgery. American volume. 2008;90:2423–31. doi: 10.2106/JBJS.G.00677. [DOI] [PubMed] [Google Scholar]