Abstract
The main purpose of treatment of rheumatoid arthritis (RA) with disease modifying antirheumatic drugs (DMARDs) is to control activation of lymphocytes, although some patients do not respond adequately to such treatment. Among various mechanisms of multidrug resistance, P-glycoprotein (P-gp), a member of ATP-binding cassette transporters, causes drug-resistance by efflux of intracellular drugs. Certain stimuli, such as tumor necrosis factor-α, activate lymphocytes and induce P-gp expression on lymphocytes, as evident in active RA. Studies from our laboratories showed spontaneous nuclear accumulation of human Y-box-binding protein-1, a multidrug resistance 1 transcription factor, in unstimulated lymphocytes, and surface overexpression of P-gp on peripheral lymphocytes of RA patients with high disease activity. The significant correlation between P-gp expression level and RA disease activity is associated with active efflux of drugs from the lymphocyte cytoplasm and in drug-resistance. However, the use of biological agents that reduce P-gp expression as well as P-gp antagonists (e.g., cyclosporine) can successfully reduce the efflux of corticosteroids from lymphocytes in vitro, suggesting that both types of drugs can be used to overcome drug-resistance and improve clinical outcome. We conclude that lymphocytes activated by various stimuli in RA patients with highly active disease acquire P-gp-mediated multidrug resistance against corticosteroids and probably some DMARDs, which are substrates of P-gp. Inhibition/reduction of P-gp could overcome such drug resistance. Expression of P-gp on lymphocytes is a promising marker of drug resistance and a suitable therapeutic target to prevent drug resistance in patients with active RA.
Keywords: Multidrug resistance 1 gene, P-glycoprotein, Lymphocytes, Disease activity, Rheumatoid arthritis
Core tip: In patients with refractory rheumatoid arthritis (RA) and high disease activity, overexpression of P-glycoprotein (P-gp) on lymphocytes can cause resistance to anti-rheumatic drugs through efflux of intracellular drugs from these cells. Lymphocytes activated by various stimuli, including tumor necrosis factor-α in RA patients apparently acquire P-gp-mediated multidrug resistance against certain anti-rheumatic drugs, which are substrates of P-gp. The use of biological agents that reduce P-gp expression as well as P-gp antagonists can successfully reduce the efflux of drugs from lymphocytes, suggesting that they can be used to overcome drug-resistance and improve clinical outcome.
INTRODUCTION
Rheumatoid arthritis (RA) is manifested by inflammatory and chronic destruction of multiple joints with occasional systemic organ complications based on immune abnormality[1]. Poor control of RA is associated with severe painful disability and impairments at work and life. The strategic treatment to control immune-mediated synovial inflammation, joint destruction and extra-organ manifestation is by early intervention with synthetic or biological disease modifying anti-rheumatic drugs (DMARDs). Early treatment of RA with DMARDs can result in prevention of joint destruction and a better long-term outcome[2]. DMARDs commonly target lymphocytes and the cytokines produced by these cells, which play an important role in the pathogenesis of RA[3]. However, we often encounter RA patients who are refractory to these DMARDs and fail in the control of high disease activity[4]. Thus, overcoming activated lymphocytes involved in drug-resistance is an important goal of the treatment in some refractory RA patients. P-glycoprotein (P-gp) is a member of ATP-binding cassette transporters and is induced on the cell membrane by certain stimuli. P-gp transports multiple drugs from the cytoplasm to the cell exterior, resulting in the development of drug resistance. Here, we discuss the importance of P-gp on activated lymphocytes and its relevance to multidrug-resistance and the potential for treatments targeting P-gp on lymphocytes to overcome drug-resistance in refractory patients with RA.
MECHANISMS OF DRUG RESISTANCE MEDIATED BY P-GP
P-gp is encoded by the multidrug resistance-1 (MDR-1)[5-7], a member of the ATP-binding cassette transporter superfamily of genes. P-gp is recognized by structurally diverse, hydrophobic/amphiphilic substrates, ranging from 300 to 2000 Da, catches these substrates like a “vacuum cleaner” during passing through the cell membrane, and pumps them out of the cells in a manner dependent on the energy of ATP hydrolysis. Therefore, Corticosteroids, certain immunosuppressants and DMARDs, including antimalarial drugs, are extruded from lymphocytes with overexpression of P-gp, which leads to reductions in the concentrations of these drugs in cytoplasm and failure of their intracellular effects (Table 1)[8-13]. Indeed, P-gp-mediated efflux of corticosteroids from lymphocytes can result in low cytoplasmic corticosteroid concentrations and development of corticosteroid resistance in systemic lupus erythematosus[14]. Thus, excessive excretion of the drugs from P-gp-overexpressing lymphocytes can be involved in the drug-resistance often observed in patients with RA.
Table 1.
Relation of P-glycoprotein with disease modifying antirheumatic drugs and immunosuppressants
| Drug | Pharmacological substrates of P-glycoprotein | Competitive inhibitor of P-glycoprotein |
| Corticosteroids | Yes | No |
| Cyclosporine | Yes | Yes |
| Tacrolimus | Yes | Yes |
| Methotrexate | No | No |
| Leflunomide | No | No |
| Hydroxycloroquine | Yes | Yes |
| Sulfasalazine | Yes | Unknown |
| D-penicillamine | Yes | Unknown |
| Colchicine | Yes | No |
| Cyclophosphamide | No | No |
| Azathioprine | No | No |
THE REGULATION OF P-GP EXPRESSION ON LYMPHOCYTES
Endothelial cells of the blood brain barrier and various epithelial cells show congenial expression of P-gp for protection of cells from toxic substances. In contrast, P-gp expression on normal resting lymphocytes is marginal but can be induced by certain stimuli[15-17]. Overexpression of P-gp appears to be closely associated with the nuclear localization of human Y-box-binding protein-1 (YB-1) in various tumors[18]. YB-1, which is a member of the DNA/RNA-binding protein family containing a cold-shock domain, is activated in response to various genotoxic stimuli and drives the transcription of MDR-1 gene[18]. We have demonstrated that lymphocytes can be activated by various stimuli, such as cytokines and extracellular matrix to induce P-gp expression on lymphocytes, based on the following sequence of events; activation and translocation of YB-1 by IL-2, tumor necrosis factor-α (TNF-α) (Figure 1A) and fragmented hyaluronan, transcriptional activation of MDR-1 by activated YB-1, P-gp expression on the cell surface membrane of lymphocytes, expelling added dexamethasone from lymphocytes, leading to a fall in intracellular dexamethasone concentration[16,17]. Serum and synovial concentrations of IL-2 are high in patients with active RA[19,20]. TNF-α is a clinically validated pathogenic factor in inflammatory erosive arthritis in RA and is pivotal target for directed biologic intervention[3,21-23]. Fragmented hyaluronan is increased in the RA synovium and synovial fluid[24,25]. The enhanced production of fragmented hyaluronan is due to increased digestion of native hyaluronan, which is increased in inflammatory foci like synovitis by inflammatory cytokines including IL-1β and TNF-α[26] and by oxygen-derived free radicals[24,25]. Overexpression of P-gp on lymphocytes induced by these stimuli[15,16], which also play important roles in the disease activity of RA, parallels the activation of lymphocytes. P-gp expression is preferentially high on CD69-expressing lymphocytes, which is a well-defined marker of early activation of lymphocytes[16,17]. Actually, lymphocytes in highly active RA patients, i.e., pathologically active lymphocytes, show accumulation of YB-1 in the nuclei and overexpression of P-gp on the cell surface membrane (Figure 1B). Thus, lymphocyte activation by certain stimuli induces YB-1 activation followed by P-gp overexpression, resulting in acquisition of multidrug resistance mediated by P-gp (Figure 2A and B, and Table 1). Therefore, the presence of active lymphocytes that have acquired P-gp-mediated multidrug resistance are probably involved in the failure of disease control in patients with active RA.
Figure 1.
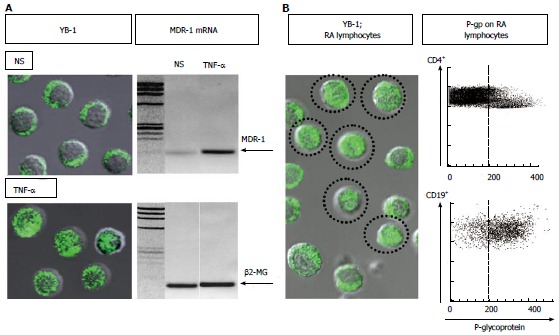
Up-regulation of nuclear translocation of Y-box-binding protein-1, transcription of multidrug resistance 1 in lymphocytes, and P-glycoprotein expression on lymphocytes. A: Left: Immunostaining and confocal microscopy analysis of Y-box-binding protein-1 (YB-1) in 1 × 105 of peripheral blood mononuclear cells (PBMCs). YB-1 was expressed in the cytoplasm of all non-stimulated PBMCs (NS). In contrast, nuclear translocation of YB-1 was induced in 30% or more of PBMCs incubated with 10 ng/mL of tumor necrosis factor-α (TNF-α). Immunostaining for YB-1 using a specific antibody (Ab) against YB-1[19] with FITC-conjugated anti-rabbit IgG Ab (BD Biosciences Pharmingen). Confocal analysis of YB-1 using a LSM 5 Pascal invert Laser Scan Microscope (Carl Zeiss Microscope Systems, Germany). Magnification, × 600; Right: Multidrug resistance-1 (MDR-1) mRNA expression was examined by RT-PCR using total RNA extracted from PBMCs incubated with 10 ng/mL of TNF-α or no stimulation (NS). The primer sequences were as follows: human β2-microglobulin forward 5’-ACCCCCACTGAAAAAGATGA-3’, reverse 5’-ATCTTCAAACCTCCATGATG-3’; human MDR-1 forward 5’-CCCATCATTGCAATAGCAGG-3’, reverse 5’-GTTCAAACTTCTGCTCCTGA-3’. Amplified products were electrophoresed with Marker 4 (Nippon Gene, Tokyo) on 3% agarose gels; B: Spontaneous nuclear translocation of YB-1 and P-glycoprotein (P-gp) expression on lymphocytes from a typical patient with active rheumatoid arthritis (RA). Left: Immunostaining and confocal microscopy analysis of YB-1 in 1 × 105 of PBMCs. YB-1 was expressed in the nuclei of a proportion of unstimulated PBMCs (encircled cells). Magnification, × 600; Right: P-gp expression on CD4+ and CD19+ peripheral blood lymphocytes. The dotted line represents the gate set to discriminate negative from positive stained cells as determined by control FITC-conjugated anti-mouse IgG Ab. The specific antibodies for staining and flow cytometric analysis were as follows: staining for P-gp using MRK16 (a specific monoclonal Ab against P-gp; Kyowa Medex, Tokyo) with FITC-conjugated goat anti-mouse IgG Ab (BD Biosciences Pharmingen), cy-chrome-conjugated CD4 monoclonal Ab, cy-chrome-conjugated CD19 monoclonal Ab (BD Biosciences Pharmingen).
Figure 2.
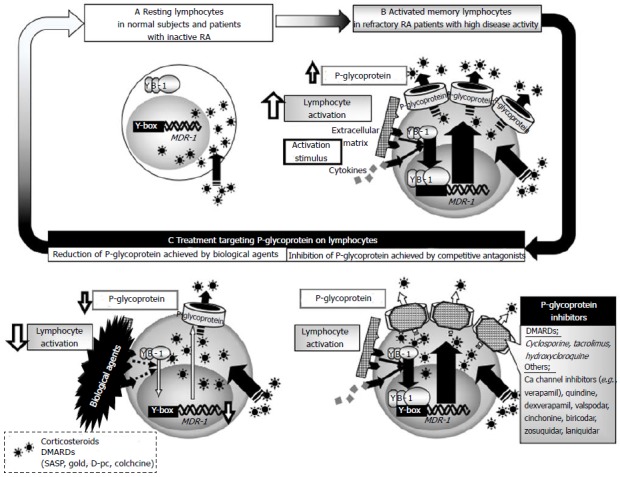
Schematic diagram of the relevance of P-glycoprotein to drug resistance in rheumatoid arthritis. A: Y-box-binding protein-1 is located in the cytoplasm of lymphocytes and P-glycoprotein (P-gp) is only marginally expressed on normal lymphocytes of normal subjects and patients with inactive RA; B: In patients with highly active rheumatoid arthritis (RA), various stimuli induce P-gp expression on lymphocytes, which leads to active efflux of drugs from lymphocytes, resulting in drug-unresponsiveness and failure to control disease activity; C: Reduction of P-gp achieved by intensive immunosuppressive therapy and inhibition of P-gp by competitive antagonists, such as cyclosporine, could overcome P-gp-related drug-resistance in patients with highly active RA. DMARDs: Disease modifying antirheumatic drugs; MDR-1: Multidrug resistance 1.
CLINICAL VALIDATION OF THE RELATIONSHIP BETWEEN P-GP-EXPRESSING RA LYMPHOCYTES AND DRUG RESISTANCE
The expression level of P-gp is significantly high on most peripheral CD4+ T cells and CD19+ B cells in RA patients, but marginal in normal subjects. Evidence indicates that P-gp expression level on lymphocytes characteristically correlates significantly with RA disease activity, estimated by the disease activity score (DAS) 28-3[27], and that its levels on CD4+ T cells and CD19+ B cells are markedly increased in patients with inadequate response to one DMARD treatment with corticosteroids or to at least two DMARDs for at least 2 years, compared with responders and normal volunteers (Figure 3).
Figure 3.
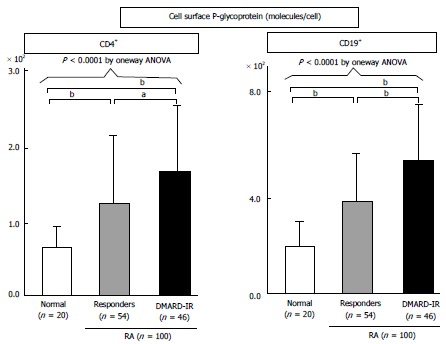
Expression of P-glycoprotein on lymphocytes from patients with refractory rheumatoid arthritis, as determined by flow cytometry. P-glycoprotein (P-gp) expression on CD4+ or CD19+ peripheral blood lymphocytes from 20 normal volunteers (open bar) and 100 RA patients [responders, hatched bars; with inadequate response to DMARDs (DMARD-IR), closed bars]. The specific antibodies for staining and flow cytometric analysis were as follows: staining for P-gp using MRK16 [a specific monocloncal antibody (Ab) against P-gp; Kyowa Medex, Tokyo] with FITC-conjugated goat anti-mouse IgG Ab (BD Biosciences Pharmingen), cy-chrome-conjugated CD4 monoclonal Ab, cy-chrome-conjugated CD19 monoclonal Ab (BD Biosciences Pharmingen). Data represent the number of molecules expressed per cell, calculated using standard QIFIKIT beads. Values are mean ± SD of independent experiments. One-way ANOVA were used to compare data between groups. aP < 0.05, bP < 0.01, by multiple comparison. DMARD: Disease modifying antirheumatic drug; RA: Rheumatoid arthritis.
To elucidate the relationship between P-gp expression and P-gp-mediated efflux of intracellular drugs in vitro, intracellular and extracellular concentrations of dexamethasone, a representative substrate of P-gp (Table 1), were determined by the C/M ratio, an index of intracellular concentration of dexamethasone (C) and extracellular concentration of dexamethasone in the conditioned medium (M). Using this method, we analyzed in vitro peripheral blood lymphocytes from RA patients with highly active disease (DAS 28-3 > 5.1). Significantly low intracellular dexamethasone levels were found in P-gp-overexpressing lymphocytes, compared with those from RA patients with mild to moderate active disease (DAS 28-3 < 5.1) and normal volunteers. The above findings indicate that overexpression of P-gp on activated lymphocytes leads to active efflux of certain intracellular drugs, substrates of P-gp, from the cells, and results in the development of drug resistance and failure of the disease control in highly active RA (Figure 2B). Taken together, it is possible that treatment that targets P-gp on lymphocytes could overcome drug-resistance in refractory patients with RA. Treatment modalities that target P-gp are classified into those that reduce P-gp expression and others that inhibit P-gp function.
BIOLOGICAL AGENTS CAN OVERCOME P-GP-MEDIATED DRUG RESISTANCE IN PATIENTS WITH REFRACTORY RHEUMATOID ARTHRITIS
TNF-α is a central player in the inflammatory process of RA, as it exacerbates erosive synovitis and enhances disease activity, and is thus an excellent molecular target for directed biologic intervention[3,21-23]. Infliximab and etanercept, two highly effective antagonists of TNF-α, have revolutionized treatment strategies for RA. In one study, infliximab improved clinical disease activity in intractable RA through significant reduction of P-gp expression levels on CD4+ T cells and CD19+ B cells, which were otherwise uncontrolled by treatment with MTX[27]. In another study published by our group, etanercept significantly reduced CD69 and P-gp expression on CD4+ T cells and CD19+ B cells in each of 11 patients with intractable RA, including two who experienced secondary loss of infliximab efficacy and eight who did not use MTX[17]. The above two studies demonstrated that treatment with TNF-α antagonists can improve RA disease activity within two weeks[17,27], and allow tapering or withdrawal of steroid therapy[17]. These effects were associated with recovery of intracellular dexamethasone levels in lymphocytes accompanied by falls in P-gp levels in these cells[17,27]. The results imply that intensive treatment with TNF-α antagonists reduces P-gp expression and results in rescue of DMARD and steroid concentrations in the cytoplasm of lymphocytes.
TNF antagonists act extracellularly and inhibit lymphocyte activation without being affected by P-gp[17]. Inhibition of lymphocyte activation by TNF-α antagonists probably suppresses YB-1-driven transcriptional activation of MDR-1 and P-gp expression on lymphocytes, and excretion of multiple drugs from the cytoplasm to the extracellular compartment. Therefore, inhibition of lymphocyte activation by TNF-α antagonists can probably thwart P-gp-mediated treatment resistance in refractory patients with RA (Figure 2C).
Translated clinically, when treatment with DMARDs and corticosteroids fails to control high disease activity in RA patients, administration of DMARDs or immunosuppressants that escape from P-gp-orchestrated excretion (Table 1), is a better treatment option. Furthermore, treatment with biological agents including TNF-α antagonists, should be initiated.
P-GP COMPETITORS REGULATE P-GP-MEDIATED DRUG RESISTANCE IN PATIENTS WITH REFRACTORY RHEUMATOID ARTHRITIS
The immunosuppressants cyclosporine and tacrolimus act as calcineurin inhibitors and inhibit cytokine production promoted by NF-AT, as well as act as P-gp-competitive inhibitors. Recent therapeutic intervention studies have investigated the efficacy of P-gp competitors, such as cyclosporine and its derivatives, in overcoming P-gp-mediated treatment resistance[28,29]. We have demonstrated that two P-gp competitive immunosuppressants, cyclosporine and tacrolimus, inhibited dexamethasone excretion from IL-2-activated lymphocytes, and that this action was concentration-dependent. In addition, treatment with these competitors resulted in recovery of intracellular dexamethasone concentrations in IL-2-activated lymphocytes by doses lower than trough levels measured clinically when these agents are used as calcineurin inhibitors[15]. Actually, the addition of low doses of tacrolimus and cyclosporine to lymphocytes harvested from highly active RA patients, resulted in recovery of intra-lymphocytes dexamethasone concentrations (Figure 4).
Figure 4.
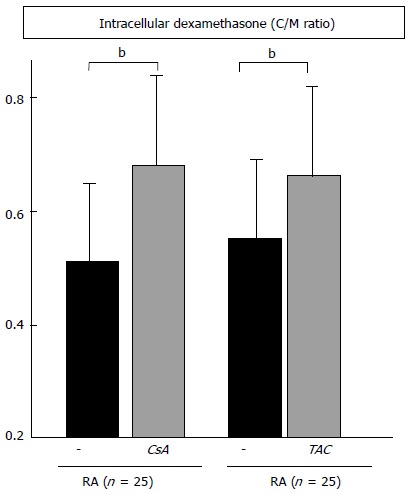
Inhibition of P-glycoprotein-related dexamethasone efflux by cyclosporine and tacrolimus. The C/M ratio in peripheral blood mononuclear cells of 25 rheumatoid arthritis (RA) patients was measured in the absence or presence of 100 ng/mL of cyclosporine (CsA), or 10 ng/mL of tacrolimus (TAC). Data are mean ± SD. bP < 0.01, by the paired t test.
In our clinical trial, we experienced refractory patients with high disease activity who were treated with low-dose cyclosporine or tacrolimus and showed significant improvement of clinical features within two weeks, which was not accompanied by falls in P-gp expression levels on lymphocytes[30]. One representative case was a 56-year-old woman with P-gp-overexpressing lymphocytes. Despite treatment with MTX, sulphasalazine, and D-penicillamine (D-pc), the RA disease activity flared several times and the joints destruction rapidly progressed during a period of two years. Low-dose cyclosporine therapy (serum cyclosporine concentration < 100 ng/mL), added to MTX with D-pc, markedly improved RA disease activity and normalized CRP and MMP-3 within two months. This outcome suggests that cyclosporine and tacrolimus, administered at low doses and over a relatively short period of time than necessary for NFAT inhibition, competitively inhibit elimination of intracellular drugs through P-gp on lymphocytes without simultaneously reducing P-gp expression, and can thus be used to overcome drug resistance and result in improvement of clinical features. We propose that competitors of P-gp, including cyclosporine, tacrolimus and hydroxycloroquine (Table 1), are potentially effective therapies for RA patients with high disease activity who are refractory to treatments with conventional DMARDs (Figure 2C).
CONCLUSION
Pharmacotherapy is the main form of treatment of RA; therefore, drug resistance induced by activated lymphocytes is a potentially serious challenge in the clinical management of RA. P-gp overexpression on activated pathogenic lymphocytes leads to the development of P-gp-mediated multidrug resistance. Therefore, treatments that target P-gp and preferentially reduce P-gp-mediated drug-resistance, can overcome drug-resistance. Taken together, we propose that the level of P-gp expressed on peripheral lymphocytes measured in RA patients is a useful marker for P-gp-mediated drug resistance and might help in the selection of more effective treatment, including treatment that reduce P-gp expression (such as biological agents) and inhibit P-gp function (such as P-gp competitors).
ACKNOWLEDGMENTS
The authors thank Ms. Adachi T for the excellent technical assistance.
Footnotes
Supported by In part by research Grants-In-Aid for Scientific Research by the Ministry of Health, Labor and Welfare of Japan; the Ministry of Education, Culture, Sports, Science and Technology of Japan; University of Occupational and Environmental Health, Japan.
Conflict-of-interest statement: Tanaka Y has received consulting fees, lecture fees, and/or honoraria from Abbvie, Chugai, Astellas, Takeda, Santen, Mitsubishi-Tanabe, Pfizer, Janssen, Eisai, Daiichi-Sankyo, UCB, GlaxoSmithKline, and Bristol-Myers, and has also received research grants from Mitsubishi-Tanabe, Chugai, MSD, Astellas, and Novartis; Dr. Tsujimura S declares no conflict of interest.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: September 13, 2014
First decision: September 28, 2014
Article in press: August 31, 2015
P- Reviewer: La Montagna G, Song J, Sakkas L S- Editor: Gong XM L- Editor: A E- Editor: Wu HL
References
- 1.Smolen JS, Aletaha D. The assessment of disease activity in rheumatoid arthritis. Clin Exp Rheumatol. 2010;28:S18–S27. [PubMed] [Google Scholar]
- 2.Smolen JS, Landewé R, Breedveld FC, Buch M, Burmester G, Dougados M, Emery P, Gaujoux-Viala C, Gossec L, Nam J, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2013 update. Ann Rheum Dis. 2014;73:492–509. doi: 10.1136/annrheumdis-2013-204573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Choy EH, Panayi GS. Cytokine pathways and joint inflammation in rheumatoid arthritis. N Engl J Med. 2001;344:907–916. doi: 10.1056/NEJM200103223441207. [DOI] [PubMed] [Google Scholar]
- 4.Jorgensen C, Maillefert JF. Multidrug resistances genes in rheumatology. Is their role immunological or pharmacological? Joint Bone Spine. 2000;67:8–10. [PubMed] [Google Scholar]
- 5.Kuwano M, Uchiumi T, Hayakawa H, Ono M, Wada M, Izumi H, Kohno K. The basic and clinical implications of ABC transporters, Y-box-binding protein-1 (YB-1) and angiogenesis-related factors in human malignancies. Cancer Sci. 2003;94:9–14. doi: 10.1111/j.1349-7006.2003.tb01344.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leonard GD, Polgar O, Bates SE. ABC transporters and inhibitors: new targets, new agents. Curr Opin Investig Drugs. 2002;3:1652–1659. [PubMed] [Google Scholar]
- 7.McKeegan KS, Borges-Walmsley MI, Walmsley AR. The structure and function of drug pumps: an update. Trends Microbiol. 2003;11:21–29. doi: 10.1016/s0966-842x(02)00010-0. [DOI] [PubMed] [Google Scholar]
- 8.Jansen G, Scheper RJ, Dijkmans BA. Multidrug resistance proteins in rheumatoid arthritis, role in disease-modifying antirheumatic drug efficacy and inflammatory processes: an overview. Scand J Rheumatol. 2003;32:325–336. doi: 10.1080/03009740310004333. [DOI] [PubMed] [Google Scholar]
- 9.Ueda K. ABC proteins protect the human body and maintain optimal health. Biosci Biotechnol Biochem. 2011;75:401–409. doi: 10.1271/bbb.100816. [DOI] [PubMed] [Google Scholar]
- 10.Llorente L, Richaud-Patin Y, Díaz-Borjón A, Alvarado de la Barrera C, Jakez-Ocampo J, de la Fuente H, Gonzalez-Amaro R, Diaz-Jouanen E. Multidrug resistance-1 (MDR-1) in rheumatic autoimmune disorders. Part I: Increased P-glycoprotein activity in lymphocytes from rheumatoid arthritis patients might influence disease outcome. Joint Bone Spine. 2000;67:30–39. [PubMed] [Google Scholar]
- 11.List AF, Kopecky KJ, Willman CL, Head DR, Slovak ML, Douer D, Dakhil SR, Appelbaum FR. Cyclosporine inhibition of P-glycoprotein in chronic myeloid leukemia blast phase. Blood. 2002;100:1910–1912. [PubMed] [Google Scholar]
- 12.Pariante CM. The role of multi-drug resistance p-glycoprotein in glucocorticoid function: studies in animals and relevance in humans. Eur J Pharmacol. 2008;583:263–271. doi: 10.1016/j.ejphar.2007.11.067. [DOI] [PubMed] [Google Scholar]
- 13.van der Heijden JW, Oerlemans R, Tak PP, Assaraf YG, Kraan MC, Scheffer GL, van der Laken CJ, Lems WF, Scheper RJ, Dijkmans BA, et al. Involvement of breast cancer resistance protein expression on rheumatoid arthritis synovial tissue macrophages in resistance to methotrexate and leflunomide. Arthritis Rheum. 2009;60:669–677. doi: 10.1002/art.24354. [DOI] [PubMed] [Google Scholar]
- 14.Tsujimura S, Saito K, Nakayamada S, Nakano K, Tanaka Y. Clinical relevance of the expression of P-glycoprotein on peripheral blood lymphocytes to steroid resistance in patients with systemic lupus erythematosus. Arthritis Rheum. 2005;52:1676–1683. doi: 10.1002/art.21032. [DOI] [PubMed] [Google Scholar]
- 15.Tsujimura S, Saito K, Nakayamada S, Nakano K, Tsukada J, Kohno K, Tanaka Y. Transcriptional regulation of multidrug resistance-1 gene by interleukin-2 in lymphocytes. Genes Cells. 2004;9:1265–1273. doi: 10.1111/j.1365-2443.2004.00803.x. [DOI] [PubMed] [Google Scholar]
- 16.Tsujimura S, Saito K, Kohno K, Tanaka Y. Fragmented hyaluronan induces transcriptional up-regulation of the multidrug resistance-1 gene in CD4+ T cells. J Biol Chem. 2006;281:38089–38097. doi: 10.1074/jbc.M601030200. [DOI] [PubMed] [Google Scholar]
- 17.Tsujimura S, Saito K, Nakayamada S, Tanaka Y. Etanercept overcomes P-glycoprotein-induced drug resistance in lymphocytes of patients with intractable rheumatoid arthritis. Mod Rheumatol. 2010;20:139–146. doi: 10.1007/s10165-009-0247-0. [DOI] [PubMed] [Google Scholar]
- 18.Kuwano M, Oda Y, Izumi H, Yang SJ, Uchiumi T, Iwamoto Y, Toi M, Fujii T, Yamana H, Kinoshita H, et al. The role of nuclear Y-box binding protein 1 as a global marker in drug resistance. Mol Cancer Ther. 2004;3:1485–1492. [PubMed] [Google Scholar]
- 19.Kuroda T, Tanabe N, Sakatsume M, Nozawa S, Mitsuka T, Ishikawa H, Tohyama CT, Nakazono K, Murasawa A, Nakano M, et al. Interleukin-2 levels are elevated in the bone marrow serum of patients with mutilans-type rheumatoid arthritis. Clin Rheumatol. 2002;21:23–27. doi: 10.1007/s100670200006. [DOI] [PubMed] [Google Scholar]
- 20.Camilleri JP, Amos N, Williams BD, Emery P, Williams LA, Jessop JD. Serum soluble interleukin 2 receptor levels and radiological progression in early rheumatoid arthritis. J Rheumatol. 2001;28:2576–2578. [PubMed] [Google Scholar]
- 21.Smolen JS, Aletaha D, Redlich K. The pathogenesis of rheumatoid arthritis: new insights from old clinical data? Nat Rev Rheumatol. 2012;8:235–243. doi: 10.1038/nrrheum.2012.23. [DOI] [PubMed] [Google Scholar]
- 22.Matsuno H, Yudoh K, Katayama R, Nakazawa F, Uzuki M, Sawai T, Yonezawa T, Saeki Y, Panayi GS, Pitzalis C, et al. The role of TNF-alpha in the pathogenesis of inflammation and joint destruction in rheumatoid arthritis (RA): a study using a human RA/SCID mouse chimera. Rheumatology (Oxford) 2002;41:329–337. doi: 10.1093/rheumatology/41.3.329. [DOI] [PubMed] [Google Scholar]
- 23.Tanaka Y. Intensive treatment and treatment holiday of TNF-inhibitors in rheumatoid arthritis. Curr Opin Rheumatol. 2012;24:319–326. doi: 10.1097/BOR.0b013e3283524e4c. [DOI] [PubMed] [Google Scholar]
- 24.Balazs EA, Watson D, Duff IF, Roseman S. Hyaluronic acid in synovial fluid. I. Molecular parameters of hyaluronic acid in normal and arthritis human fluids. Arthritis Rheum. 1967;10:357–376. doi: 10.1002/art.1780100407. [DOI] [PubMed] [Google Scholar]
- 25.Dahl LB, Dahl IM, Engström-Laurent A, Granath K. Concentration and molecular weight of sodium hyaluronate in synovial fluid from patients with rheumatoid arthritis and other arthropathies. Ann Rheum Dis. 1985;44:817–822. doi: 10.1136/ard.44.12.817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wells AF, Klareskog L, Lindblad S, Laurent TC. Correlation between increased hyaluronan localized in arthritic synovium and the presence of proliferating cells. A role for macrophage-derived factors. Arthritis Rheum. 1992;35:391–396. doi: 10.1002/art.1780350405. [DOI] [PubMed] [Google Scholar]
- 27.Tsujimura S, Saito K, Nawata M, Nakayamada S, Tanaka Y. Overcoming drug resistance induced by P-glycoprotein on lymphocytes in patients with refractory rheumatoid arthritis. Ann Rheum Dis. 2008;67:380–388. doi: 10.1136/ard.2007.070821. [DOI] [PubMed] [Google Scholar]
- 28.O’Brien MM, Lacayo NJ, Lum BL, Kshirsagar S, Buck S, Ravindranath Y, Bernstein M, Weinstein H, Chang MN, Arceci RJ, et al. Phase I study of valspodar (PSC-833) with mitoxantrone and etoposide in refractory and relapsed pediatric acute leukemia: a report from the Children’s Oncology Group. Pediatr Blood Cancer. 2010;54:694–702. doi: 10.1002/pbc.22366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Morjani H, Madoulet C. Immunosuppressors as multidrug resistance reversal agents. Methods Mol Biol. 2010;596:433–446. doi: 10.1007/978-1-60761-416-6_19. [DOI] [PubMed] [Google Scholar]
- 30.Suzuki K, Saito K, Tsujimura S, Nakayamada S, Yamaoka K, Sawamukai N, Iwata S, Nawata M, Nakano K, Tanaka Y. Tacrolimus, a calcineurin inhibitor, overcomes treatment unresponsiveness mediated by P-glycoprotein on lymphocytes in refractory rheumatoid arthritis. J Rheumatol. 2010;37:512–520. doi: 10.3899/jrheum.090048. [DOI] [PubMed] [Google Scholar]


