Abstract
Research suggests that individuals with a history of non-suicidal self-injury (NSSI) do not have difficulty generating alternatives to social problems but choose more negative solutions, suggesting a deficit in decision-making. However, studies report no significant differences in risky decision-making on a performance-based task among individuals with and without NSSI histories. A limitation of these studies is that decision-making was only assessed at baseline. As individuals with a history of NSSI typically self-injure when experiencing negative emotions, decision-making ability may become impaired specifically in the presence of these emotions. The aim of the current study was to investigate decision-making ability among individuals with and without NSSI histories both at baseline and following a distressing social exclusion task. We compared individuals with (n = 48) and without (n = 72) NSSI histories on the Iowa Gambling Task, a behavioral measure of risky decision-making, before and after exclusion or inclusion on the Cyberball task. Results indicated no significant group differences in performance regardless of condition. When participants were grouped by racial/ethnic minority status, results indicated that non-Hispanic White individuals with a history of NSSI exhibited deterioration in risky decision-making ability following social exclusion. Potential explanations for these findings and clinical implications are discussed.
Keywords: Self-harm, Self-injury, Problem-solving, Exclusion, Distress
1. Introduction
Non-suicidal self-injury (NSSI) is defined as the deliberate, self-inflicted destruction of body tissue without suicidal intent and for purposes not socially sanctioned (International Society for the Study of Self-Injury, 2007). NSSI includes behaviors such as cutting, burning, scratching, and self-hitting (Walsh, 2008) and does not include behaviors such as piercings or tattoos (ISSS, 2007). The prevalence of NSSI is high in community samples of adults (e.g., Rodham and Hawton, 2009) and college students (Paivio and McCulloch, 2004; Whitlock et al., 2006), and the behavior has many clinical correlates, including increased anxiety, depression, borderline personality disorder (BPD) characteristics, and suicide (Ross and Heath, 2002; Andover et al., 2005; Klonsky and Olino, 2008; Wilkinson et al., 2011).
Research on the functions of NSSI has provided overwhelming support for an automatic negative reinforcement function, in which NSSI is utilized as a method to reduce or eliminate negative affect (see Klonsky, 2007, for a review). Individuals may also engage in NSSI for social reinforcement, such as escaping interpersonal task demands or getting a response from others (Nock and Prinstein, 2004). Interpersonal antecedents are central to each of these functions. Between 34 and 85% of individuals with a history of self-injury reported experiencing loneliness before an episode of NSSI (Bennum and Phil, 1983; Briere and Gil, 1998; Laye-Gindhu and Schonert-Reicht, 2005). Further, Hawton and Harriss (2006) found that among the problems immediately preceding deliberate self-harm, which is a term that does not distinguish between those who self-injured with and without suicidal intent, were social isolation (35.5%), relationship with family (29.4%), relationship with partner (25.9%), bereavement/loss (16.7%), and relationship with friends (7.4%).
When faced with stressful life events, individuals with an NSSI history may be less equipped to cope with the associated unpleasant emotions in an adaptive manner, instead using NSSI as a coping mechanism (e.g., Haines et al., 1995). It has been hypothesized that individuals with a history of NSSI have difficulty solving social problems; however, Nock and Mendes (2008) examined social problem-solving among adolescents with and without NSSI histories and found no significant group differences in the average number of solutions generated in response to challenging social scenarios, both at baseline and following a distressing task. Participants did choose significantly more negative solutions across scenarios compared to individuals with no NSSI history, indicating that decision-making may be a salient area of difficulty for individuals with an NSSI history.
However, studies of decision-making ability among individuals with an NSSI history suggest otherwise. In studies using the Iowa Gambling Task (Bechara et al., 1994), a behavioral measure of risky decision-making, results showed no significant differences in performance between individuals with and without NSSI histories in adult (McCloskey et al., 2012) and adolescent (Janis and Nock, 2009) samples. Oldershaw and colleagues (2009) also found no differences on performance between individuals with and without a history of self-injury; however, they did not distinguish between self-injury with and without intent to die. A major limitation of the aforementioned studies is that decision-making ability was only assessed at baseline. As individuals with a history of NSSI typically self-injure when experiencing negative emotions, it is possible that decision-making ability becomes impaired specifically in the presence of these emotions.
The aim of the current study was to investigate decision-making ability, specifically risky decision-making, among individuals with and without NSSI histories at baseline and following a stressful social exclusion task, which was chosen given the roles of isolation and loneliness as self-reported precursors to NSSI episodes (e.g., Laye-Gindhu and Schonert-Reicht, 2005). Given the centrality of these precursors, and because individuals with an NSSI report that they are more emotionally reactive than individuals with no NSSI history (Gratz and Roemer, 2008; Heath et al., 2008; Glenn et al., 2011), we hypothesized that among individuals who were socially excluded, those with an NSSI history would report greater distress than individuals with no NSSI history. Next, based on the aforementioned research by McCloskey and colleagues (2012), we hypothesized that at baseline, there would be no significant differences in risky decision-making ability between individuals with and without histories of NSSI. Finally, as research has suggested that individuals with an NSSI choose more negative solutions across problem-solving scenarios following a distressing task (Nock and Mendes, 2008), we hypothesized that individuals with a history of NSSI who were socially excluded would perform more poorly on a risky decision-making task than individuals with an NSSI history who were socially included, and individuals with no NSSI history.
2. Methods
2.1 Participants
Participants (N = 120) were 48 young adults with at least one lifetime episode of NSSI (NSSI+ group) and 72 adults with no lifetime history of NSSI (NSSI− group). The mean age of the entire sample was 21.94 years (SD = 2.82). The sample was 64.2% female (n = 77), and 26.7% (n = 32) of the sample was Hispanic. Regarding race, 53.3% of the sample described their race as White, 22.5% as Black or African American, 10% as Asian, 7.5% as other, 4.2% as more than one race, 1.7% as unknown, and 0.8% as Native Hawaiian or other Pacific Islander. The majority of the sample (76.7%) completed some college or a two-year program. Inclusion criteria for the current study included individuals between the ages of 18 and 29 with and without NSSI histories; given that NSSI is a transdiagnostic behavior (Bentley et al., 2014), there were no exclusion criteria on the basis of psychiatric diagnosis.
2.2 Measures
The Functional Assessment of Self-Mutilation (FASM; Lloyd et al., 1997) is a self-report measure that assesses functions of NSSI, methods used, frequency, and age of onset. Internal consistency estimates for the FASM are good (Penn et al., 2003; Kaess et al., 2013), and the measure is strongly correlated with measures of suicidal ideation, past suicide attempts (Guertin et al., 2001), and recent suicide attempts (Shaffer et al., 1996). In this study, the FASM was used to assess NSSI and suicide attempt history, and the internal consistency in this study was α = 0.88.
Depression was assessed using the Beck Depression Inventory-II (BDI-II; Beck et al., 1996), a 21-item self-report measure designed to assess the severity of depressive symptoms over the past two weeks. Symptoms are rated on a four-point Likert-type scale, with higher scores representing greater depression severity. The psychometric properties of the BDI-II are well established (e.g., Beck et al., 1996), and internal consistency for the measure in this study was excellent (α = 0.93).
Emotion dysregulation was assessed using the Difficulties in Emotion Regulation Scale (DERS; Gratz and Roemer, 2004), a 36-item self-report measure. This measure was included as a clinical covariate due to its association with NSSI (e.g., Gratz et al., 2006) and our focus on individuals’ ability to engage in goal-directed activity in the presence of negative emotions. Participants indicate on a five-point Likert-type scale how often each item applies to them, with higher scores indicating greater emotion dysregulation. The DERS has been used successfully with college (e.g., Glenn and Klonsky, 2009) and adult populations (e.g., Herr et al., 2013). In the current study, internal consistency was α = 0.93.
The McLean Screening Instrument for Borderline Personality Disorder (MSI-BPD; Zanarini et al., 2003) was used to assess BPD features. BPD commonly co-occurs with NSSI (Andover et al., 2005) and is associated with impaired decision-making (LeGris et al., 2012). The MSI-BPD is a 10-item self-report measure with a total score that ranges from 0 to 10. In the current study, the self-injury criterion was removed from analyses. Internal consistency (α = 0.74) and test-retest reliability (ρ = 0.72) of the MSI-BPD are good (Zanarini et al., 2003), and internal consistency in the current study was adequate (α = 0.73).
2.3 Induction of social exclusion
Social exclusion was simulated using Cyberball, a virtual ball-toss game widely used to examine exclusion and rejection (Williams and Jarvis, 2006; Williams et al., 2010). In Cyberball, participants believe they are playing an online ball-tossing game with other participants in order to practice their mental visualization skills; in fact, the “others” are controlled by the computer program. Participants were randomly assigned to either the “inclusion” condition (receiving the ball for one-third of the throws) or the “exclusion” condition (receiving the ball for the first two throws only). Cyberball has been shown to reliably induce feelings of being ostracized (e.g., Bernstein and Claypool, 2012; Gratz et al., 2013), and has received support as a negative mood induction paradigm, with individuals reporting more negative mood (Bernstein and Claypool, 2012; Kelly et al., 2012), general distress (Gratz et al., 2013), and physiological arousal (Boyes and French, 2009; Kelly et al., 2012) following exclusion compared to inclusion.
2.4 Assessment of risky decision-making ability
The Iowa Gambling Task (IGT; Bechara et al., 1994) is a computerized behavioral measure used to assess risky decision-making in a laboratory setting. Examinees are presented with four decks of cards and instructed to choose a card from any deck; each card chosen results in either the winning of a hypothetical monetary reward amount, or a win followed by a loss. Two decks are termed “disadvantageous,” or risky, incurring a larger net loss than the other two “advantageous” decks.
The IGT has been used extensively in research, and is a highly sensitive measure of impaired decision-making across many neurological and psychiatric conditions (Bechara, 2007), including BPD (Haaland and Landro, 2007), substance use (Grant et al., 2000; Bechara and Martin, 2004), and suicide attempts (Jollant et al., 2005). Convergent and concurrent validity of the IGT with other measures of executive functioning have been demonstrated (Hardy et al., 2006; Brand et al., 2007).
2.5 Procedure
Participants were recruited through a university subject pool, introductory psychology courses, and postings on community websites. Open and targeted recruitment for individuals with an NSSI history were conducted. All participants who responded to these announcements were invited to schedule an appointment in the laboratory, at which time detailed information about the study was provided (e.g., time requirements, compensation) and written informed consent was obtained. Participants who met eligibility criteria and provided informed consent continued with study procedures. Procedures were given clearance by the relevant Institutional Review Board.
First, participants provided information about demographic characteristics including age, gender, race, and ethnicity via clinical interview. NSSI and suicide attempt history were assessed using the FASM, and baseline distress level was determined using a 10-point Subjective Units of Distress Scale (SUDS). Participants were then administered the IGT. During the IGT, the research team conducted an urn randomization (Wei, 1977) stratified by gender, self-injury status, and baseline distress level to assign participants to one of two experimental conditions (Cyberball “inclusion” or “exclusion”).
Next, participants engaged in the Cyberball procedure described above, after which SUDS ratings were given a second time to assess distress immediately following the task. The IGT was then administered for a second time. We then administered a manipulation check to assess participants’ perception of exclusion on Cyberball (Oaten et al., 2008), in which participants were asked to rate on a five-point scale (ranging from 1 = not at all to 5 = very much) the following item: “I was excluded.” Finally, participants completed all self-report measures, after which they were provided with an extensive debriefing.
2.6 Data analysis
Prior to hypothesis testing, variables were examined for assumptions of normality and homogeneity. Several variables exhibited significant skew and kurtosis and variables were transformed in these cases. All analyses were also conducted using the aforementioned variables prior to transformation; patterns of significance were the same.
Missing data were observed for the following measures: baseline SUDS rating (0.8%), post-Cyberball SUDS rating (0.8%), baseline IGT net total score (2.5%), post-Cyberball IGT net total score (4.2%), BDI-II (1.7%), DERS (0.8%), and MSI-BPD (1.7%). Thus, the pattern of missing data was examined in order to justify the use of data imputation methods (cf. Schafer and Graham, 2002). Specifically, we conducted Little’s chi-square statistic for testing whether values are missing completely at random (MCAR) test (Little and Rubin, 1987), which was nonsignificant, X2(514) = 550.88, p = 0.13. This suggests that data were missing completely at random and multiple imputation was used to complete the dataset (cf. Schafer and Graham, 2002).
The first hypothesis was tested using a 2×2×2 mixed design ANOVA with Cyberball condition (inclusion, exclusion) and self-injury status (NSSI+, NSSI−) as the between-subjects variables and time (SUDS at baseline, post-Cyberball) as the within-subjects factor. The second hypothesis was tested using a t-test with NSSI status as the independent variable and baseline IGT score as the dependent variable. To test the third hypothesis, we conducted a 2×2×2 mixed design ANOVA with Cyberball condition and self-injury status as the between-subjects variables and time (mean net total score on the IGT at baseline and post-Cyberball) as the within-subjects factor. All tests were two-tailed, with alpha set at 0.017 to control for number of analyses.
3. Results
3.1 Sample characteristics
Participants in the NSSI+ group did not differ from participants in the NSSI− group by age, gender, race, or education level (Table 1). There was a trend toward significance by racial/ethnic minority status, with a smaller percentage of participants who identified their race as White and ethnicity as non-Hispanic (non-Hispanic White group) in the NSSI+ group than all other racial/ethnic minority participants (non-White group). Clinical variables were also compared to determine any significant differences between individuals with and without NSSI histories (Table 2). Individuals with an NSSI history had significantly higher scores on measures of depression, emotion dysregulation, and borderline personality traits (all ps < 0.01). Groups did not differ on baseline SUDS ratings (p = 0.42).
Table 1.
Demographic variables by group.
| NSSI+ (n = 48) |
NSSI− (n = 72) |
df | X2/t |
Cramer’s V/d |
|
|---|---|---|---|---|---|
| Age | 22.04 (2.84) | 21.88 (2.86) | 118 | −0.31 | 0.06 |
| Gender (% Female) | 70.8 | 59.7 | 1 | 1.55 | 0.11 |
| Race (%) | 6 | 6.27 | 0.23 | ||
| Asian | 10.4 | 9.7 | |||
| Native Hawaiian/Other | 2.1 | 0.0 | |||
| Pacific Islander | |||||
| Black or African American | 22.9 | 22.2 | |||
| White | 45.8 | 58.3 | |||
| More than one race | 4.2 | 4.2 | |||
| Unknown | 4.2 | 0.0 | |||
| Other | 10.4 | 5.6 | |||
| Racial/Ethnic Minority Status (%) | 1 | 3.81* | 0.18 | ||
| Non-Hispanic White | 33.3 | 51.4 | |||
| Non-White | 66.7 | 48.6 | |||
| Education Level (%) | 6 | 4.11 | 0.19 | ||
| Some high school | 6.3 | 2.8 | |||
| Completed high school | 2.1 | 4.2 | |||
| Some college or two-year program | 75.0 | 79.2 | |||
| Completed four-year college program | 6.3 | 9.7 | |||
| Some graduate school | 6.3 | 2.8 | |||
| Completed a graduate degree | 2.1 | 1.4 | |||
| Other | 2.1 | 0.0 |
Note: Unless otherwise specified, values in cells represent means, and values in parentheses represent standard deviations for variables.
p < .05
Table 2.
Clinical variables by group.
| NSSI+ (n = 48) |
NSSI− (n = 72) |
df | X2/t | Cramer’s V/d |
|
|---|---|---|---|---|---|
| Baseline SUDS Ratings | 2.42 (0.84) | 2.44 (2.03) | 118 | 0.06 | 0.01 |
| Baseline IGT Net Total Scores | 50.84 (9.31) | 49.15 (9.24) | 118 | −0.98 | |
| BDI-II | 14.23 (11.14) | 7.32 (7.53) | 118 | −4.17** | 0.73 |
| DERS | 90.16 (28.82) | 75.67 (22.75) | 118 | −3.04** | 0.56 |
| MSI-BPD | 4.74 (3.13) | 2.35 (2.32) | 118 | −4.95** | 0.87 |
| Suicide Attempt History (%) | 2.8 | 22.9 | 1 | 12.09** | 0.32 |
Notes: Values in cells represent means, and values in parentheses represent standard deviations for variables before transformation. SUDS = Subjective Units of Distress Scale. IGT = Iowa Gambling Task. BDI-II = Beck Depression Inventory – 2nd Edition. DERS = Difficulties in Emotion Regulation Scale. MSI-BPD = McLean Screening Instrument for Borderline Personality Disorder.
p < .01
Among individuals with a lifetime history of NSSI, 88.6% reported engaging in NSSI more than once, 54.2% reported engaging in NSSI in the past year, and the average age of onset was 13.4 years (SD = 4.40). Approximately 60% of the sample used more than one method, and the lifetime number of methods reported ranged from 1 through 8, with an average of 2.83 (SD = 2.07) methods used. The most commonly reported methods were cutting (39.6%), carving (22.9%), hitting (22.9%), and scraping (20.8%). In the current sample, the average number of lifetime episodes of NSSI was 162.35 (SD = 607.23).
3.2. Preliminary analyses
Prior to hypothesis testing, the relationship between demographic and clinical variables and dependent variables were conducted using a series of Pearson correlations. Post-Cyberball SUDS ratings were significantly correlated with scores on baseline SUDS ratings (r = 0.59, p < 0.001), BDI-II (r = 0.25, p = 0.006), DERS (r = 0.20, p = 0.03), and MSI-BPD (r = 0.21, p = 0.02). Post-Cyberball SUDS ratings were not significantly related to history of suicide attempt (r = 0.002, p = 0.98) or any demographic variables (all ps > 0.08). We controlled for significant associations in analyses involving post-Cyberball SUDS ratings as the dependent variable.1
Second, we examined the relationship between baseline IGT net total score and demographic and clinical variables. There were no statistically significant associations between any demographic variables or clinical variables and baseline IGT net total score (all ps > 0.13). Last, post-Cyberball IGT net total score was examined for potential covariates. Post-Cyberball IGT net score was significantly associated with baseline IGT net total score (r = 0.64, p < 0.001), DERS (r = −0.20, p = 0.03), and gender (r = −0.21, p = 0.02). No other clinical or demographic variables were associated with post-Cyberball IGT net total scores (all ps > 0.12). Therefore, baseline IGT net total score, DERS, and gender were included as covariates in analyses with post-Cyberball IGT net total score as the dependent variable.
Finally, a manipulation check was conducted in order to assess participants’ experience of the Cyberball task. An independent-samples t-test revealed that participants in the exclusion condition (M = 4.20, SD = 1.09) felt more strongly excluded than participants in the inclusion condition (M = 1.84, SD = 0.93), t(118) = 12.63, p < 0.001, d = 2.33. Among participants who were excluded, those in the NSSI+ group did not feel more excluded (M = 1.86, SD = 0.89) than those in the NSSI− group (M = 1.83, SD = 0.97), t(60) = −0.40, p = 0.69, d = 0.03.
3.3. Hypothesis testing
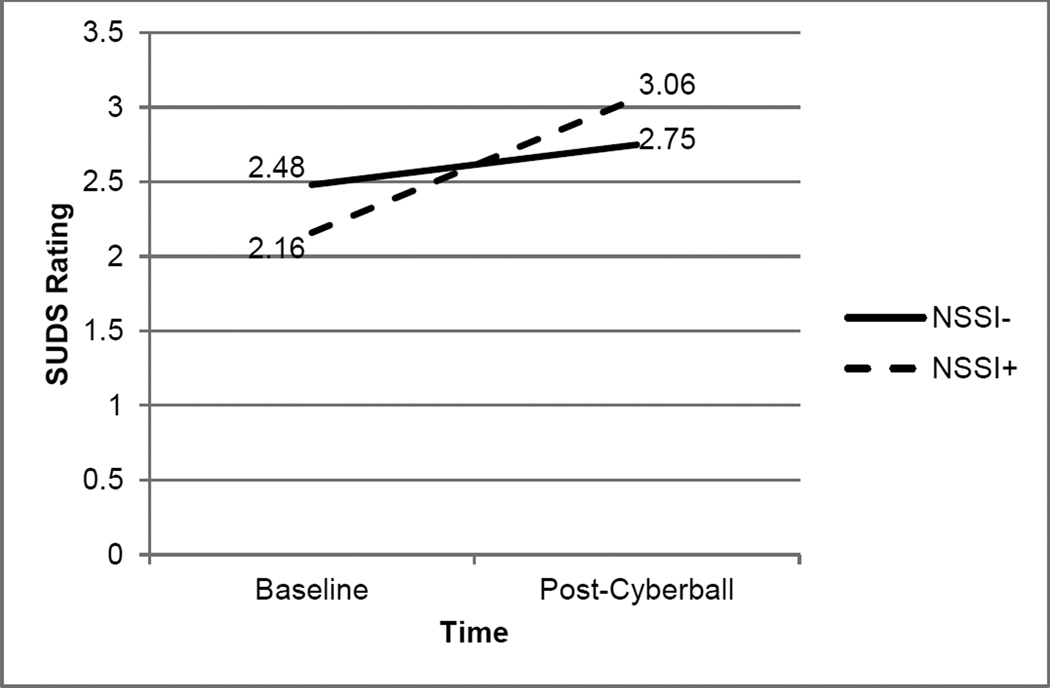
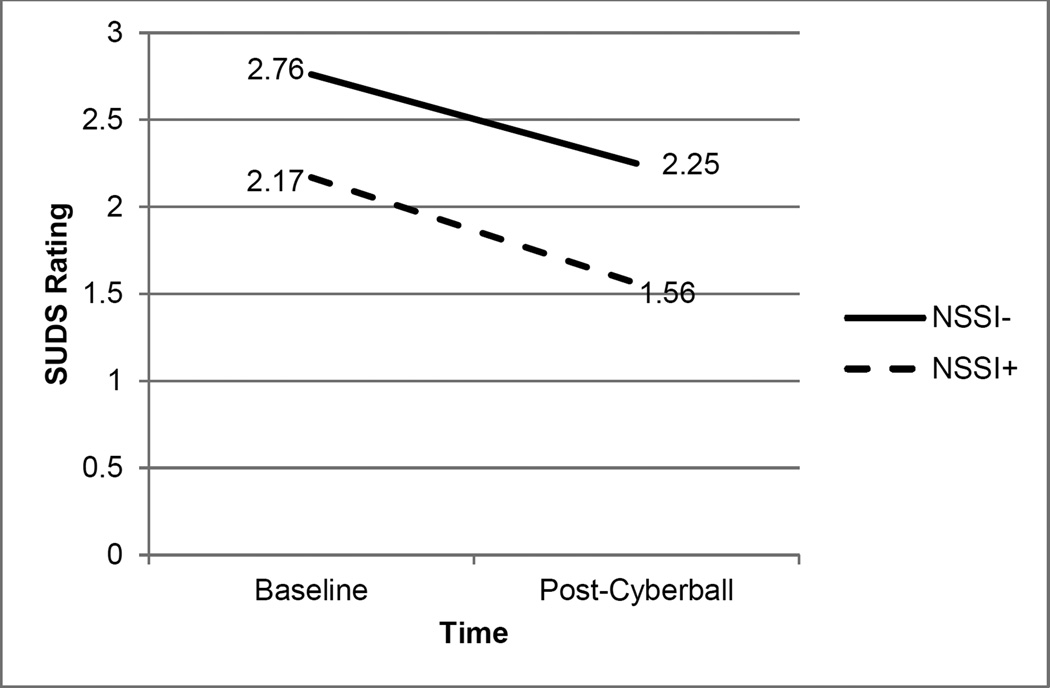
First, we hypothesized that level of distress would vary as a function of NSSI status and Cyberball condition. Analyses revealed that a three-way NSSI status × Cyberball condition × time interaction was not significant, F(1, 118) = 1.24, p = 0.27, ηp2 = 0.01. Two-way interactions were also examined. The Cyberball condition × time interaction was significant, F(1, 118) = 18.45, p = 0.001, ηp2 = 0.10; SUDS ratings increased from baseline to post-Cyberball task in the exclusion group, but decreased in the inclusion group. The NSSI status × Cyberball condition interaction, F(1,118) = 0.93, p = 0.34, ηp2 = 0.008, and the NSSI status × time interaction, F(1, 118) = 0.54, p = 0.47, ηp2 = 0.005, were not significant. There were no significant main effects on level of distress for NSSI status, F(1, 118) = 0.80, p = 0.37, ηp2 = 0.007, Cyberball condition, F(1, 118) = 1.69, p = 0.20, ηp2 = 0.02, or time, F(1, 118) = 0.01, p = 0.90, ηp2 < 0.001. Patterns of results are depicted in Fig. 1 and Fig. 2.
Fig. 1.
Effects of Cyberball condition, NSSI status, and social exclusion on SUDS ratings
Note: SUDS = Subjective Units of Distress Scale. NSSI− = Individuals with no lifetime non-suicidal self-injury (NSSI) history. NSSI+ = Individuals with a lifetime NSSI history.
Fig. 2.
Effects of Cyberball condition, NSSI status, and social inclusion on SUDS ratings
Notes: SUDS = Subjective Units of Distress Scale. NSSI− = Individuals with no lifetime non-suicidal self-injury (NSSI) history. NSSI+ = Individuals with a lifetime NSSI history.
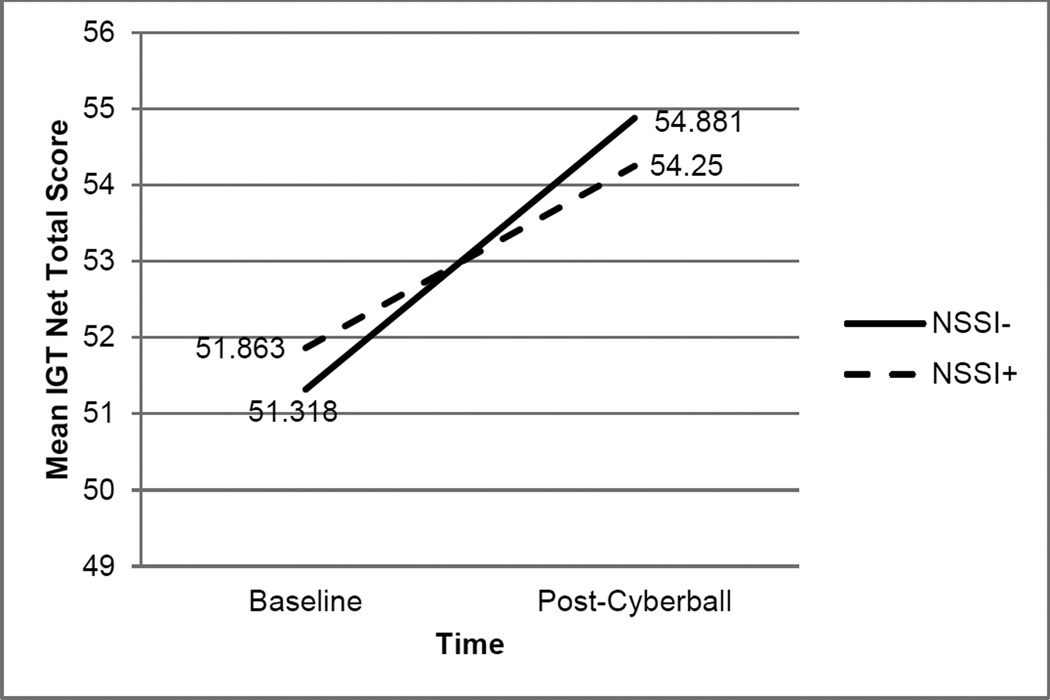
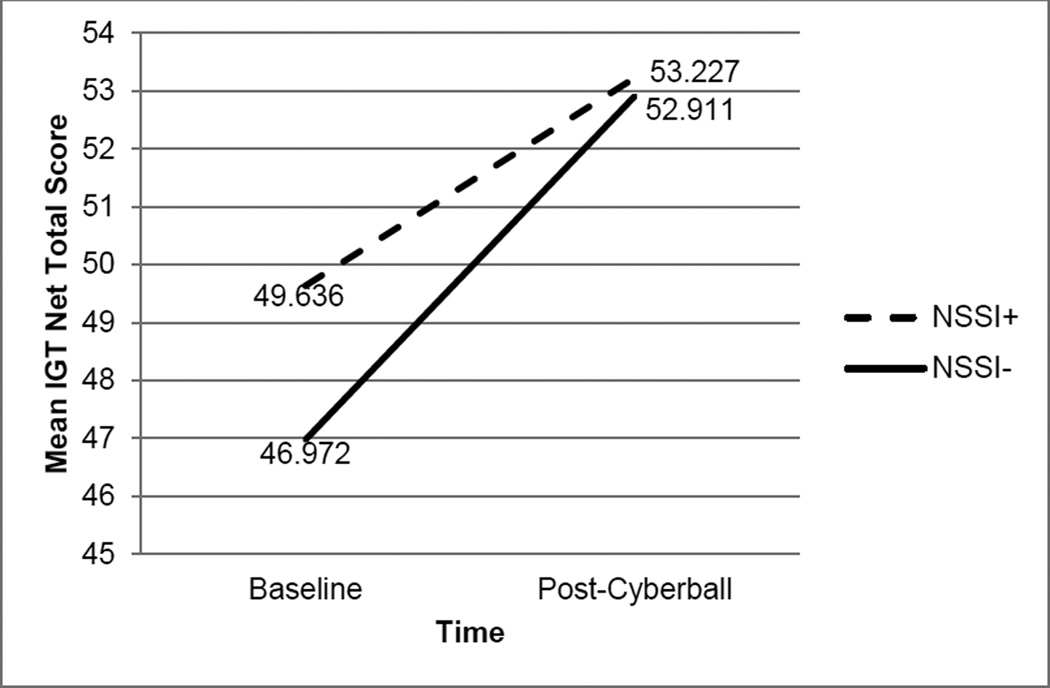
The next set of hypotheses focused on decision-making ability. There were no significant differences in baseline IGT net total scores between individuals with and without NSSI histories, t(118) = −0.98, p = 0.33, d = 0.18. We also hypothesized that changes in decision-making ability would vary as a function of NSSI history and social inclusion or exclusion. Analyses revealed that a three-way NSSI status × Cyberball condition × time interaction was not significant, F(1, 118) = 0.11, p = 0.75, ηp2 = 0.001. The NSSI status × Cyberball condition interaction, F(1,118) = 0.18, p = 0.68, ηp2 = .002, NSSI status × time interaction, F(1, 118) = 0.96, p = 0.33, ηp2 = 0.008, and Cyberball condition × time interaction, F(1, 118) = 0.99, p = 0.32, ηp2 = 0.008, were also not significant. Analyses revealed a significant main effect of time (baseline, post-Cyberball task), F(1, 118) = 18.58, p < 0.001, ηp2 = 0.14, with IGT net total scores increasing from baseline to post-Cyberball. There were no significant main effects for NSSI status, F(1, 118) = 0.16, p = 0.69, ηp2 = 0.001, or Cyberball condition, F(1, 118) = 1.70, p = 0.20, ηp2 = 0.01. Patterns of results are depicted in Fig. 3 and Fig. 4.
Fig. 3.
Effects of Cyberball condition, NSSI status, and social exclusion on IGT net total score
Notes: IGT = Iowa Gambling Task. NSSI− = Individuals with no lifetime non-suicidal self-injury (NSSI) history. NSSI+ = Individuals with a lifetime NSSI history.
Fig. 4.
Effects of Cyberball condition, NSSI status, and social inclusion on IGT net total score
Notes: IGT = Iowa Gambling Task. NSSI− = Individuals with no lifetime non-suicidal self-injury (NSSI) history. NSSI+ = Individuals with a lifetime NSSI history.
3.4. Post hoc exploratory analysis
Descriptive statistics revealed that individuals who identified as non-White (47.8%; n = 32) engaged in NSSI at higher rates than individuals who identified as non-Hispanic White (30.2%; n = 16), X2(1, N = 120) = 3.81, p = 0.05, phi = 0.18. Therefore, post-hoc exploratory analyses examining decision-making ability across racial/ethnic minority groups were conducted. Analyses revealed that non-White individuals were significantly older than non-Hispanic White individuals; groups did not differ with regard to other demographic and clinical characteristics (Table 3). Individuals’ experience of distress and exclusion on the Cyberball task was also examined (Table 3). Those in the non-White group reported feeling more excluded regardless of whether they were included or excluded on the Cyberball task, but there were no significant group differences on post-Cyberball SUDS ratings.
Table 3.
Demographic and clinical variables by race/ethnicity.
| Non-White (n = 67) |
Non-Hispanic White (n = 53) |
df | X2/t/F |
phi/d/ ηp2 |
|
|---|---|---|---|---|---|
| Age | 22.69 (3.01) | 21.00 (2.32) | 118 | 3.37** | 0.63 |
| Gender (% Female) | 67.2 | 60.4 | 1 | 0.59 | 0.07 |
| Education Level (%) | 5 | 9.97 | 0.29 | ||
| Some high school | 7.5 | 0.0 | |||
| Completed high school | 7.5 | 1.9 | |||
| Some college or two-year program | 68.7 | 86.8 | |||
| Completed four-year college program | 10.4 | 5.7 | |||
| Some graduate school | 3.0 | 5.7 | |||
| Completed a graduate degree | 3.0 | 0.0 | |||
| Baseline SUDS Ratings | 2.25 (1.88) | 2.66 (2.03) | 118 | −1.15 | 0.21 |
| Post-Cyberball SUDS Ratings | |||||
| Exclusion Group | 2.80 (2.44) | 3.07 (2.09) | 1, 60 | 0.33 | 0.01 |
| Inclusion Group | 1.84 (1.61) | 2.08 (1.92) | 1, 56 | 0.40 | 0.01 |
| Baseline IGT Net Total Scores | 48.39 (8.47) | 51.63 (9.98) | 118 | −1.92 | 0.35 |
| BDI-II | 11.14 (10.42) | 8.76 (8.66) | 118 | 1.28 | 0.25 |
| DERS | 80.47 (26.63) | 82.73 (25.90) | 118 | −0.57 | 0.09 |
| MSI-BPD | 3.42 (2.72) | 3.17 (3.16) | 118 | 0.43 | 0.08 |
| Suicide Attempt History (%) | 13.4% | 7.5% | 1 | 1.06 | 0.09 |
| Experience of Exclusion | |||||
| Exclusion Group | 4.46 (0.78) | 3.89 (1.24) | 60 | 2.19* | 0.55 |
| Inclusion Group | 2.90 (0.96) | 1.54 (0.81) | 56 | 2.34* | 1.53 |
Notes: Unless otherwise specified, values in cells represent means, and values in parentheses represent standard deviations for variables. SUDS = Subjective Units of Distress Scale. IGT = Iowa Gambling Task. BDI-II = Beck Depression Inventory – 2nd Edition. DERS = Difficulties in Emotion Regulation Scale. MSI-BPD = McLean Screening Instrument for Borderline Personality Disorder.
p < .05,
p < .01
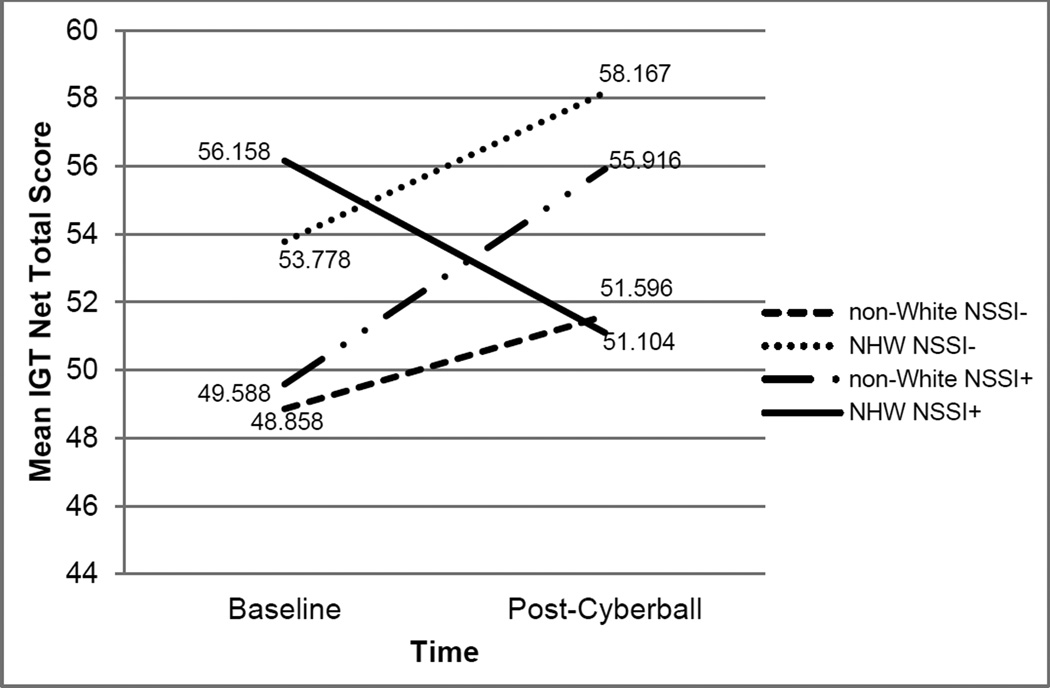
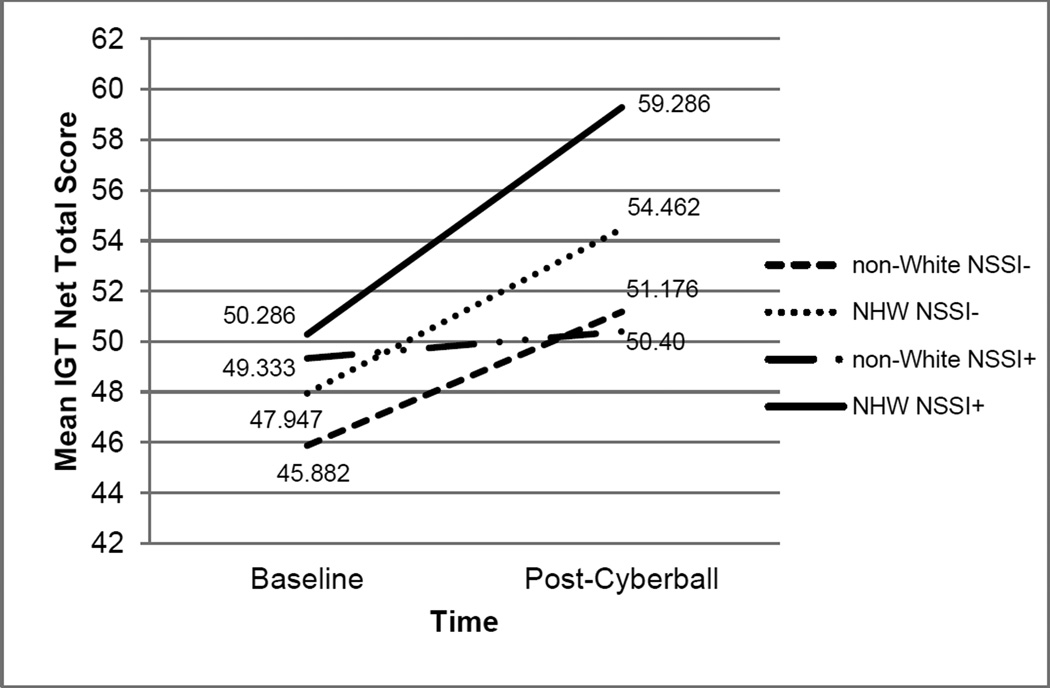
We then examined whether decision-making ability varied by racial/ethnic minority group using a 4×2×2 mixed design ANOVA with Cyberball condition (inclusion, exclusion) and racial/ethnic minority/NSSI status (non-Hispanic White with and without an NSSI history, non-White with and without an NSSI history) as the between-subjects variables and time (baseline, post-Cyberball task) as the within-subjects factor. A three-way racial/ethnic minority/NSSI status × Cyberball condition × time interaction was significant, F(1, 118) = 3.86, p = 0.01, ηp2 = 0.09; in the exclusion condition, the non-Hispanic White group performed more poorly from baseline to post-Cyberball, while all other groups’ performance improved. In addition, two-way interactions were examined. Analyses revealed that the racial/ethnic minority/NSSI status × Cyberball condition interaction, F(1, 118) = 0.37, p = 0.77, ηp2 = 0.007, the racial/ethnic minority/NSSI Status × time interaction, F(1, 118) = 0.56, p = 0.64, ηp2 = 0.02, and the Cyberball condition × time interaction, F(1, 118) = 3.50, p = 0.06, ηp2 = 0.03, were not significant. Finally, analyses revealed a significant main effect of time (baseline, post-Cyberball task), F(1, 118) = 17.72, p < 0.001, ηp2 = 0.14, with IGT net total scores increasing from baseline to post-Cyberball task. There were no significant main effects of racial/ethnic minority/NSSI status, F(1, 118) = 0.56, p = 0.64, ηp2 = 0.02, or Cyberball condition, F(1, 118) = 1.17, p = 0.28, ηp2 = 0.01. Patterns of results are depicted in Fig. 5 and Fig. 6.
Fig. 5.
Effects of Cyberball condition, racial/ethnic minority/NSSI status, and social exclusion on IGT net total score
Notes: IGT = Iowa Gambling Task. NSSI− = Individuals with no lifetime non-suicidal self-injury (NSSI) history. NSSI+ = Individuals with a lifetime NSSI history. NHW = non-Hispanic White.
Fig. 6.
Effects of Cyberball condition, racial/ethnic minority/NSSI status, and social inclusion on IGT net total score
Notes: IGT = Iowa Gambling Task. NSSI− = Individuals with no lifetime non-suicidal self-injury (NSSI) history. NSSI+ = Individuals with a lifetime NSSI history. NHW = non-Hispanic White.
4. Discussion
4.1 Social exclusion and distress
One aim of this study was to examine social exclusion as an antecedent to distress in NSSI. Results indicated that following social exclusion, but not inclusion, individuals with and without an NSSI history reported increased distress, suggesting that the Cyberball task did differentially impact distress levels following social inclusion and exclusion. However, these changes did not differ as a function of NSSI history; individuals with an NSSI history experienced similar levels of distress than individuals without NSSI following social exclusion. This finding was surprising given research indicating that individuals with an NSSI history describe themselves as more emotionally reactive on self-report measures than individuals with no NSSI history (Gratz and Roemer, 2008; Heath et al., 2008; Glenn et al., 2011). It is possible that SUDS ratings are not specific enough to capture the emotional distress experienced by these individuals.
4.2 Social exclusion and risky decision-making ability
The second set of hypotheses focused on risky decision-making ability. Our findings were consistent with previous research examining decision-making ability among individuals with an NSSI history (Janis and Nock, 2009; McCloskey et al., 2012), suggesting that individuals with and without an NSSI history perform similarly on the IGT. However, as discussed previously, the aforementioned studies only examined decision-making at baseline, and it is possible that individuals with an NSSI history exhibit deficits in decision-making in some contexts (e.g., when distressed) but not in others. Results of the current study did not support this hypothesis, as changes in risky decision-making before and after social inclusion and exclusion did not vary based on NSSI history.
These results were unexpected given the strong theoretical rationale for this hypothesis, but there are several potential explanations. It is possible that the social exclusion paradigm did not produce a level of distress intense enough to adequately simulate the environmental conditions that individuals experience prior to an episode of NSSI. In addition, all groups, independent of inclusion/exclusion status or NSSI history, performed more strongly on the second administration of the IGT due to learning effects. Thus, learning effects may have obscured the relationship between social exclusion and risky decision-making ability among those with an NSSI history. It is possible that a more highly powered study would reveal a significant relationship. On the other hand, it is possible that risky decision-making ability is truly not impaired in individuals with an NSSI history, or that it is only impaired with regard to the decision to select NSSI as a solution to a problem and not across situations more generally.
4.3 Racial/ethnic minority group
Previous research on race and ethnicity in NSSI has yielded mixed results. Some studies have found that Hispanic and Black individuals are as likely as White individuals to engage in NSSI (e.g., Whitlock et al., 2006; Croyle, 2007), while others suggest that Black and Hispanic individuals are less likely than White individuals to engage in NSSI (e.g., Gratz & Roemer, 2008; Whitlock et al., 2008), and still another found that Asian and White individuals self-injure at higher rates than Hispanic and Black individuals (Chesin et al., 2013). Our study was the first to report that individuals who identify as non-White were more likely to engage in NSSI than individuals who identify as non-Hispanic White. However, it is important to note that both NSSI-targeted and open recruitment were conducted as part of the current study, so prevalence rates may not reflect true rates of NSSI among these groups in the community.
In order to better understand the roles of race and ethnicity in NSSI, post-hoc analyses were conducted to explore the association among social exclusion, decision-making, and NSSI in these groups. Among individuals who were socially included, all groups – non-Hispanic White and non-White individuals with and without NSSI histories – showed improvement from baseline to post-Cyberball on the IGT. Interestingly, among individuals who were socially excluded, all groups showed improvement from baseline to post-Cyberball on the IGT with the exception of non-Hispanic White individuals with an NSSI history, who performed significantly worse following social exclusion compared to baseline. This finding suggests that this group in particular may be prone to poor decision-making following a social stressor.
Interestingly, non-White participants who were excluded reported that they felt more excluded on the Cyberball task than non-Hispanic White participants who were excluded, but they did not report increased distress. Research suggests that people who are stigmatized, including members of racial and ethnic minority groups, are more likely to experience social exclusion (Goodwin et al., 2010). Therefore, the experience of being ostracized on a computer-based task may not have been emotionally salient for this group and did not hinder performance on the decision-making task. A separate body of literature has suggested that individuals who experience aversive self-awareness, or the experience of negative and self-relevant emotions and cognitions in response to negative events, are more susceptible to NSSI (Armey and Crowther, 2008). It is possible that aversive self-awareness in response to the Cyberball exclusion task was most salient for the non-Hispanic White group with an NSSI history, and this cognitive bias may have impeded decision-making. These data are preliminary, and these potential explanations were not examined directly in this study. Given the small sample size in the non-Hispanic White group, further research in this area is necessary to replicate these results.
4.4 Limitations
There are several limitations of note in the current study. Due to feasibility concerns, we did not exclude for disorders or conditions that may have impacted performance on the IGT, such as substance use (Grant et al., 2000; Bechara and Martin, 2004) or impulsive aggressive disorders (Best et al., 2002). Therefore, it is possible that comorbid diagnoses may have been differentially represented among individuals with and without histories of NSSI. Next, although the IGT is a measure of risky decision-making, it is also a measure of learning. When designing the current study, it was assumed that learning effects would have been distributed evenly across conditions. However, our results suggest that individuals with an NSSI history may have learned the contingencies on the IGT more slowly than individuals with no NSSI history, although this difference was not significant.
The use of SUDS ratings as the primary outcome measure for distress may have lacked the sensitivity necessary to accurately interpret the results of the current study. Distress is a broad conceptualization of negative affect that may not have adequately accounted for different aspects of negative emotions, some of which may have been more salient in the context of social exclusion than others (e.g., loneliness). In addition, there was no direct assessment of the extent to which participants believed the Cyberball cover task, which may have impacted the level of distress they experienced during the task. Another limitation of the current study is that we recruited both college students and community participants, and although we did control for education level, it is possible that these groups would show different response patterns on the outcome variables. Further, individuals completed self-report measures at the end of the study procedures, and it is possible that engaging in the Cyberball task may have influenced their responses, despite low self-reported distress in the overall sample. Finally, this study was limited by its small sample size, and it is possible that group differences would emerge as power increases.
4.5 Future directions
The current study is the first to examine decision-making ability among individuals with an NSSI history both at baseline and following an experimental manipulation of social context. The results of the current study did not yield significant differences with regard to decision-making ability among individuals with and without an NSSI history; however, this is an important area for further investigation given the limitations of the current study and the necessity of identifying underlying mechanisms of NSSI that are malleable and amenable to intervention.
Future research might examine the role of different metrics of NSSI severity in risky decision-making ability, such as recency and frequency of NSSI episodes, as well as consider utilizing more varied tasks to examine decision-making in this population. Although the IGT is a measure of risky decision-making, it is also associated with learning. Other behavioral measures of risky decision-making, such as the Balloon Analog Risk Task (Lejuez et al., 2002) or measures of delay discounting, might yield purer results. Similarly, it is possible that individuals who engage in NSSI do not make risky decisions in general, but more specifically with regard to self-injury. Future research may investigate this construct by tailoring externally valid measures of problem-solving and decision-making, such as the Social Problem-Solving Skills Test (Nock, 2006), to include NSSI-specific scenarios.
Finally, this study was the first to report that individuals who identify as non-White were more likely to engage in NSSI than individuals who identify as non-Hispanic White. Further research is needed to replicate this finding, which has important implications for research, treatment, and overall public health. First, future research on NSSI should be sure to include demographic questions about ethnicity – in addition to race – as part of their analyses. Further, researchers can look to the extensive body of literature on ethnicity-specific stressors in order to investigate particular aspects of the experience of these individuals that might contribute to increased engagement in NSSI.
4.6 Conclusion
The current study supported previous research indicating that individuals with an NSSI history perform similarly to individuals with no NSSI history on a behavioral measure of risky decision-making. However, data also showed that following a distressing social exclusion task, individuals with an NSSI history do not perform poorly compared to individuals with no NSSI history. It is possible that there truly is no relationship between risky decision-making ability and NSSI history as a function of distress. However, exploratory analyses suggest that non-Hispanic White individuals with an NSSI history do perform more poorly on the IGT following social exclusion than non-White individuals; therefore, a relationship between risky decision-making ability and NSSI may exist in specific subgroups of individuals. Future research in this area is needed to better understand how individuals make the decision to engage in NSSI despite the availability of other problem-solving solutions.
Highlights.
History of NSSI did not predict baseline decision-making ability.
Social exclusion did not impact decision-making ability across groups.
Groups did not differ on distress ratings following social exclusion.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Given group differences on clinical variables (BDI-II, MSI-BPD, DERS), hypothesis testing was also conducted without clinical covariates. The same pattern of results emerged.
References
- Andover MS, Pepper CM, Ryabchenko KA, Orrico EG, Gibb BE. Self-mutilation and symptoms of depression, anxiety, and borderline personality disorder. Suicide and Life Threatening Behaviors. 2005;35:581–591. doi: 10.1521/suli.2005.35.5.581. [DOI] [PubMed] [Google Scholar]
- Armey MF, Crowther JH. A comparison of linear versus non-linear models of aversive self-awareness, dissociation, and non-suicidal self-injury among young adults. Journal of Consulting and Clinical Psychology. 2008;76:9–14. doi: 10.1037/0022-006X.76.1.9. doi: http://dx.doi.org.revproxy.brown.edu/10.1037/0022-006X.76.1.9. [DOI] [PubMed] [Google Scholar]
- Bechara A. Iowa gambling task professional manual. Lutz: Psychological Assessment Resources; 2007. [Google Scholar]
- Bechara A, Damasio AR, Damasio H, Anderson SW. Insensitivity to future consequences following damage to human prefrontal cortex. Cognition. 1994;50:7–15. doi: 10.1016/0010-0277(94)90018-3. [DOI] [PubMed] [Google Scholar]
- Bechara A, Martin EM. Impaired decision making related to working memory deficits in individuals with substance addictions. Neuropsychology. 2004;18:152–162. doi: 10.1037/0894-4105.18.1.152. doi: dx.doi.org/10.1037/0894-4105.18.1.152. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. BDI-II manual. San Antonio: Harcourt Brace & Company; 1996. [Google Scholar]
- Bennum I, Phil M. Depression and hostility in self-mutilation. Suicide and Life-Threatening Behavior. 1983;13:71–84. doi: 10.1111/j.1943-278x.1983.tb00006.x. [DOI] [PubMed] [Google Scholar]
- Bentley KH, Nock MK, Barlow DH. The four-function model of nonsuicidal self-injury: Key directions for future research. Clinical Psychological Science. 2014;2:638–656. [Google Scholar]
- Bernstein MJ, Claypool HM. Not all social exclusions are created equal: Emotional distress following social exclusion is moderated by exclusion paradigm. Social Influence. 2012;7:113–130. [Google Scholar]
- Best M, Williams JM, Coccaro EF. Evidence for a dysfunctional prefrontal circuit in patients with an impulsive aggressive disorder. Proceedings of the National Academy of Sciences. 2002;99:8448–8453. doi: 10.1073/pnas.112604099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyes ME, French DJ. Having a Cyberball: Using a ball-throwing game as an experimental social stressor to examine the relationship between neuroticism and coping. Personality and Individual Differences. 2009;47:396–401. [Google Scholar]
- Brand M, Recknor EC, Grabenhorst F, Bechara A. Decisions under ambiguity and decisions under risk: correlations with executive functions and comparisons of two different gambling tasks with implicit and explicit rules. Journal of Clinical and Experimental Neuropsychology. 2007;29:86–99. doi: 10.1080/13803390500507196. [DOI] [PubMed] [Google Scholar]
- Briere J, Gil E. Self-mutilation in clinical and general population samples: Prevalence, correlates, and functions. American Journal of Orthopsychiatry. 1998;68:609–620. doi: 10.1037/h0080369. [DOI] [PubMed] [Google Scholar]
- Favazza AR. The coming of age of self-mutilation. Journal of Nervous and Mental Disease. 1998;186:259–268. doi: 10.1097/00005053-199805000-00001. [DOI] [PubMed] [Google Scholar]
- Glenn CR, Blumenthal TD, Klonsky ED, Hajcak G. Emotional reactivity in nonsuicidal self-injury: Divergence between self-report and startle measures. International Journal of Psychophysiology. 2011;80:166–170. doi: 10.1016/j.ijpsycho.2011.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glenn CR, Klonsky ED. Emotion dysregulation as a core feature of borderline personality disorder. Journal of Personality Disorders. 2009;23:20–28. doi: 10.1521/pedi.2009.23.1.20. [DOI] [PubMed] [Google Scholar]
- Goodwin SA, Williams KD, Carter-Sowell AR. The psychological sting of stigma: The costs of attributing ostracism to racism. Journal of Experimental Social Psychology. 2010;46:612–618. [Google Scholar]
- Grant S, Contoreggi C, London ED. Drug abusers show impaired performance in a laboratory test of decision making. Neuropsychologia. 2000;38:1180–1187. doi: 10.1016/s0028-3932(99)00158-x. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Dixon-Gordon KL, Breetz A, Tull M. A laboratory-based examination of responses to social rejection in borderline personality disorder: The mediating role of emotion dysregulation. Journal of Personality Disorders. 2013;27:157–171. doi: 10.1521/pedi.2013.27.2.157. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment. 2004;26:41–54. [Google Scholar]
- Gratz KL, Roemer L. The relationship between emotion dysregulation and deliberate self-harm among female undergraduate students at an urban commuter university. Cognitive Behaviour Therapy. 2008;37:14–25. doi: 10.1080/16506070701819524. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Rosenthal MZ, Tull MT, Lejuez CW, Gunderson JG. An experimental investigation of emotion dysregulation in borderline personality disorder. Journal of Abnormal Psychology. 2006;115:850–855. doi: 10.1037/0021-843X.115.4.850. [DOI] [PubMed] [Google Scholar]
- Guertin T, Lloyd-Richardson E, Spirito A, Donaldson D, Boergers J. Self-mutilation in adolescents who attempt suicide by overdose. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:1062–1069. doi: 10.1097/00004583-200109000-00015. [DOI] [PubMed] [Google Scholar]
- Haaland VO, Landro NI. Decision making as measured with the Iowa Gambling Task in patients with borderline personality disorder. Journal of the International Neuropsychological Society. 2007;13:699–703. doi: 10.1017/S1355617707070890. [DOI] [PubMed] [Google Scholar]
- Haines J, Williams CL, Brain KL. The psychopathology of incarcerated self-mutilators. The Canadian Journal of Psychiatry. 1995;40:514–522. doi: 10.1177/070674379504000903. [DOI] [PubMed] [Google Scholar]
- Hardy DJ, Hinkin CH, Levine AJ, Castellon SA, Lam MN. Risky decision-making assessed with the gambling task in adults with HIV. Neuropsychology. 2006;20:355–360. doi: 10.1037/0894-4105.20.3.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawton K, Harriss L. Deliberate self-harm in people aged 60 years and over: Characteristics and outcome of a 20-year cohort. International Journal of Geriatric Psychiatry. 2006;21:572–581. doi: 10.1002/gps.1526. [DOI] [PubMed] [Google Scholar]
- Heath NL, Toste JR, Nedecheva T, Charlebois A. An examination of nonsuicidal self-injury among college students. Journal of Mental Health Counseling. 2008;30:137–156. [Google Scholar]
- Herr NR, Rosenthal MZ, Geiger PJ, Erikson K. Difficulties with emotion regulation mediate the relationship between borderline personality disorder symptom severity and interpersonal problems. Personality and Mental Health. 2012;7:191–202. doi: 10.1002/pmh.1204. [DOI] [PubMed] [Google Scholar]
- Janis EB, Nock MK. Are self-injurers impulsive?: Results from two laboratory studies. Psychiatry Research. 2009;169:261–267. doi: 10.1016/j.psychres.2008.06.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jollant F, Bellivier F, Leboyer M, Astruc B, Torres S, Verdier R, Castelnau D, Malafosse A, Courtet P. Impaired decision-making in suicide attempters. American Journal of Psychiatry. 2005;162:304–310. doi: 10.1176/appi.ajp.162.2.304. [DOI] [PubMed] [Google Scholar]
- Kaess M, Parzer P, Mattern M, Plener P, Bifulco A, Resch F, Brunner R. Adverse childhood experiences and their impact on severity, frequency, and the individual function of nonsuicidal self-injury in youth. Psychiatry Research. 2013;206:265–272. doi: 10.1016/j.psychres.2012.10.012. [DOI] [PubMed] [Google Scholar]
- Kelly M, McDonald S, Rushby J. All alone with sweaty palms-Physiological arousal and ostracism. International Journal of Psychophysiology. 2012;83:309–314. doi: 10.1016/j.ijpsycho.2011.11.008. [DOI] [PubMed] [Google Scholar]
- Klonsky ED. The functions of deliberate self-injury: A review of the evidence. Clinical Psychology Review. 2007;27:226–239. doi: 10.1016/j.cpr.2006.08.002. [DOI] [PubMed] [Google Scholar]
- Klonsky ED, Olino TM. Identifying clinically distinct subgroups of self-injurers among young adults: A latent class analysis. Journal of Consulting and Clinical Psychology. 2008;76:22–27. doi: 10.1037/0022-006X.76.1.22. [DOI] [PubMed] [Google Scholar]
- Laye-Gindhu A, Schonert-Reichl KA. Nonsuicidal self-harm among community adolescents: Understanding the “whats” and “whys” of self-harm. Journal of Youth and Adolescence. 2005;34:447–457. [Google Scholar]
- LeGris J, Links PS, van Reekum R, Tannock R, Toplak M. Executive function and suicidal risk in women with Borderline Personality Disorder. Psychiatry Research. 2012;196:101–108. doi: 10.1016/j.psychres.2011.10.008. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Aklin WM, Jones HA, Richards JB, Strong DR, Kahler CW, Read JP. The balloon analogue risk task (BART) differentiates smokers and nonsmokers. Experimental and Clinical Psychopharmacology. 2003;11:26–33. doi: 10.1037//1064-1297.11.1.26. [DOI] [PubMed] [Google Scholar]
- Little RJA, Rubin DB. Statistical analysis with missing data. New York: Wiley; 1987. [Google Scholar]
- Lloyd EE, Kelley ML, Hope T. Poster session at the annual meeting of the Society for Behavioral Medicine. New Orleans, LA: 1997. Self-mutilation in a community sample of adolescents: Descriptive characteristics and provisional prevalence rates. [Google Scholar]
- McCloskey MS, Look AE, Chen EY, Pajoumand G, Berman ME. Nonsuicidal self-injury: Relationship to behavioral and self-rating measures of impulsivity and self-aggression. Suicide and Life-Threatening Behavior. 2012;42:197–209. doi: 10.1111/j.1943-278X.2012.00082.x. [DOI] [PubMed] [Google Scholar]
- Nock MK. Social Problem Solving Skills Test: Administration and coding manual. Cambridge, MA: Unpublished manuscript, Harvard University; 2006. [Google Scholar]
- Nock MK, Mendes WB. Physiological arousal, distress tolerance, and social problem-solving deficits among adolescent self-injurers. Journal of Consulting and Clinical Psychology. 2008;76:28–38. doi: 10.1037/0022-006X.76.1.28. [DOI] [PubMed] [Google Scholar]
- Oaten M, Williams KD, Jones A, Zadro L. The effects of ostracism on self-regulation in the socially anxious. Journal of Social and Clinical Psychology. 2008;45:465–481. [Google Scholar]
- Oldershaw A, Grima E, Jollant F, Richards C, Simic M, Taylor L, Schmidt U. Decision making and problem solving in adolescents who deliberately self-harm. Psychological Medicine. 2009;39:95–104. doi: 10.1017/S0033291708003693. [DOI] [PubMed] [Google Scholar]
- Paivio SC, McCulloch CR. Alexithymia as a mediator between childhood trauma and self-injurious behaviors. Child Abuse and Neglect. 2004;28:339–354. doi: 10.1016/j.chiabu.2003.11.018. [DOI] [PubMed] [Google Scholar]
- Penn JV, Esposito CL, Schaeffer LE, Fritz GK, Spirito A. Suicide attempts and self-mutilative behavior in a juvenile correctional facility. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:762–769. doi: 10.1097/01.CHI.0000046869.56865.46. [DOI] [PubMed] [Google Scholar]
- Rodham K, Hawton K. Epidemiology and phenomenology of nonsuicidal self-injury. In: Nock MK, editor. Understanding Nonsuicidal Self-Injury: Origins, Assessment, and Treatment. Washington D.C.: American Psychological Association; 2009. pp. 37–62. doi: http://dx.doi.org.revproxy.brown.edu/10.1037/11875-003. [Google Scholar]
- Ross S, Heath N. A study of the frequency of self-mutilation in a community sample of adolescents. Journal of Youth and Adolescence. 2002;31:67–77. [Google Scholar]
- Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychological Methods. 2002;7:147. [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Dulcan MK, Davies M. The NIMH Diagnostic Interview Schedule for Children Version 2.3 (DISC-2.3): Description, acceptability, prevalence rates, and performance in the MECA study. Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35:865–877. doi: 10.1097/00004583-199607000-00012. [DOI] [PubMed] [Google Scholar]
- Walsh B. Treating self-injury: A practical guide. New York: The Guilford Press; 2008. [Google Scholar]
- Wei LJ. A class of designs for sequential clinical trials. Journal of the American Statistical Association. 1977;72:382–386. [Google Scholar]
- Whitlock J, Eckenrode J, Silverman D. Self-injurious behaviors in a college population. Pediatrics. 2006;117:1939–1948. doi: 10.1542/peds.2005-2543. [DOI] [PubMed] [Google Scholar]
- Wilkinson P, Kelvin R, Roberts C, Dubicka B, Goodyer I. Clinical and psychosocial predictors of suicide attempts and nonsuicidal self-injury in the Adolescent Depression Antidepressants and Psychotherapy Trial (ADAPT) American Journal of Psychiatry. 2011;168:495–501. doi: 10.1176/appi.ajp.2010.10050718. [DOI] [PubMed] [Google Scholar]
- Williams KD, Cheung CKT, Choi W. Cyberostracism: Effects of being ignored over the Internet. Journal of Personality and Social Psychology. 2000;79:748–762. doi: 10.1037//0022-3514.79.5.748. [DOI] [PubMed] [Google Scholar]
- Williams KD, Jarvis B. Cyberball: A program for use in research on interpersonal ostracism and acceptance. Behavior Research Methods. 2006;38:174–180. doi: 10.3758/bf03192765. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Vujanovic AA, Parachini EA, Boulanger JL, Frankenburg FR, Hennen J. A screening measure for BPD: The McLean screening instrument for borderline personality disorder (MSI-BPD) Journal of Personality Disorders. 2003;17:568–573. doi: 10.1521/pedi.17.6.568.25355. [DOI] [PubMed] [Google Scholar]