Abstract
Objectives:
Childhood obesity and poor lifestyle practices are emerging as major public health challenges in the Caribbean. Given the fact that a significant part of childhood is spent at school, curriculum-based interventions aimed at improving good dietary and physical activity patterns may provide a useful vehicle for mass inculcation of long-term healthy lifestyle practices. In this study, we evaluated the long-term impact of a brief curriculum based intervention on dietary behaviour, physical activity and knowledge level of primary schoolchildren.
Methods:
The study was a randomized, controlled, school-based nutrition education and physical activity intervention. One hundred students each were then randomly assigned to the intervention (IVG) and non-intervention (NIVG) groups and followed-up for 18 months. Participants in the IVG group were exposed to a curriculum consisting of six one-hour modules followed by school-based activities geared at fostering healthy behaviours. Students in the non-intervention group did not receive any modules and were subject to the information available at school on a regular basis.
Results:
In multivariate regression equations controlling for age, gender, body mass index (BMI) and baseline values, intervention was associated with lower intake of fried foods and sodas (p < 0.05) and higher knowledge scores (p < 0.01) 18 months later but not significantly associated with improved physical activity or lower BMI.
Conclusions:
In this study, participants in the intervention group reported significantly lower intakes of fried foods and sodas and higher knowledge scores than participants in the control group some 18 months post-intervention independent of age, gender, BMI, ethnicity and the intakes at baseline.
Keywords: Childhood, dietary, intervention, school-based
Abstract
Objetivos:
La obesidad infantil y las prácticas de estilo de vida pobre se presentan cada vez más como importantes retos para la salud pública en el Caribe. Dado el hecho de que una parte significativa de la infancia transcurre en la escuela, las intervenciones basadas en el currículo dirigidas a mejorar los patrones de actividad física y dietética, pueden proporcionar una vía útil para inculcar masivamente prácticas de estilo de vida saludable a largo plazo. En este estudio, evaluamos el impacto a largo plazo de una intervención basada en un currículo breve de la conducta dietética, la actividad física, y el nivel de conocimientos de los escolares de la escuela primaria.
Métodos:
El estudio consistió en una intervención de la actividad física y educación sobre la nutrición de base escolar, controlada y randomizada. Cien estudiantes fueron individualmente asignados de forma aleatoria a grupos de intervención (GIV) y grupos de no intervención (GNIV), con un seguimiento de 18 meses. Los participantes en el grupo GIV fueron expuestos a un programa consistente en seis módulos de una hora, seguidos de actividades escolares orientadas a fomentar comportamientos saludables. Los estudiantes en el grupo de no intervención no recibieron ningún módulo y estaban sujetos a la información disponible en la escuela de forma regular.
The study was a randomized, controlled, school-based nutrition education and physical activity intervention. One hundred students each were then randomly assigned to the intervention (IVG) and non-intervention (NIVG) groups and followed up for eighteen months. Participants in the (IVG) group were exposed to a curriculum consisting of six one-hour modules followed by school-based activities geared at fostering healthy behaviours. Students in the non-intervention group did not receive any modules and were subject to the information available at school on a regular basis.
Resultados:
En las ecuaciones de regresión multivariante de edad, género, índice de masa corporal (IMC) y valores de referencia, la intervención estuvo asociada con una menor ingesta de alimentos fritos y refrescos (p < 0.05), y una mayor puntuación en cuanto a conocimientos (p < 0.01) 18 meses más tarde, pero no significativamente asociada con una mejor actividad física o un IMC más bajo.
Conclusiones:
En este estudio, los participantes en el grupo de intervención reportaron ingestas de alimentos fritos y refrescos significativamente menores, y puntuaciones de conocimiento más altas que las de los participantes en el grupo control, unos 18 meses tras la intervención, independientemente de la edad, el género, el IMC, la etnia, y las ingestas, en relación con los valores iniciales del estudio.
INTRODUCTION
The nutrition related chronic non-communicable diseases (NRNCD) such as hypertension, diabetes mellitus and coronary heart disease are major causes of illness and death in the English-speaking Caribbean (1–3). This represents a shift in the pattern of diseases among adults in the region, which a mere 50 years ago was predominantly infectious in nature (4). This epidemiological transition is further evident by the fact that NRNCD account for over fifty per cent of all visits to public health institutions by adults regionally. The causes of this epidemiological transition are multi-factorial and rooted in the developmental changes that occurred in the postcolonial era (1). Postcolonial Caribbean societies were typified by diets in which traditional unrefined plant-based foods were gradually replaced by those where the bulk of calories were derived from food high in refined sugar and fats (1). Moreover, there was a shift from the traditional labour intensive occupations associated with agrarian societies to more sedentary jobs with better remuneration. The availability of increased disposable incomes and the widespread influence of Western culture through the media and travel resulted in significant lifestyle and leisure activities that required lower levels of energy expenditure. These changes in dietary patterns and energy expenditure present challenges to a metabolic system that has evolved over several thousand years. These metabolic adaptations occurred in environments where caloric deficits rather than surpluses were the order of the day. Obesity remains one of the strongest risk factors for the development of NRNCD (5, 6). Caribbean societies in the postcolonial period present environments that are increasingly obesigenic. This may represent an important intergenerational trigger for the rapid development of the NRNCD (7, 8).
Regionally, our children are adopting many of these poor lifestyle practices. Research conducted among Caribbean children suggests that obesity and several of its contributing factors are quite prevalent (1). In fact, many of the nutrition behaviours and physical activity patterns associated with NRNCD have their origin in childhood (1, 9–14). Furthermore, there is good evidence to suggest that healthy lifestyle practices adopted in childhood may be sustainable (15–17). Thus, childhood represents an important period for inculcating healthy lifestyle practices. Throughout the Caribbean, children spend a significant portion of their time within a school environment. The school environment can therefore play an important role in the formation of healthy lifetime practices (10, 18, 19). In fact, several studies have shown long-term improvement in the consumption of healthy foods following school-based intervention programmes (20–25). Inclusion of the home and community environments and physical activity components in such interventions increased the level of benefits seen (26, 27). Given these important findings and the need to have an evidence-based approach to the formulation of school health policies regionally, it is surprising to find few studies on interventions aimed at lifestyle behaviour changes among children in the region. In this study, we report the finding of a school-based intervention aimed at fostering long-term healthy dietary and physical activity habits among primary school children in Trinidad and Tobago.
SUBJECTS AND METHODS
Population
Participants were recruited from primary schools in the town of Sangre Grande, a rural community of 10 000 persons located in north-east Trinidad and whose economic activities are centred on agriculture. There are 12 primary schools in this region catering to children from neighbouring villages. Results of the mandatory primary schools' National Assessment Examinations for 2006 suggest that pupils attending schools in this region of the country obtain marks in numeracy and literacy that are among the lower percentiles nationally. We reasoned that a school-based curriculum intervention that is comprehensible to this group would meet the criteria for comprehensibility for those students whose scores are among higher percentiles. We targeted students in the sixth year of primary school who were beginning their preparation for the National Assessment Examinations. All educational materials were at a comprehension level that was one reading grade level lower than that of the targeted population.
Study design and sample
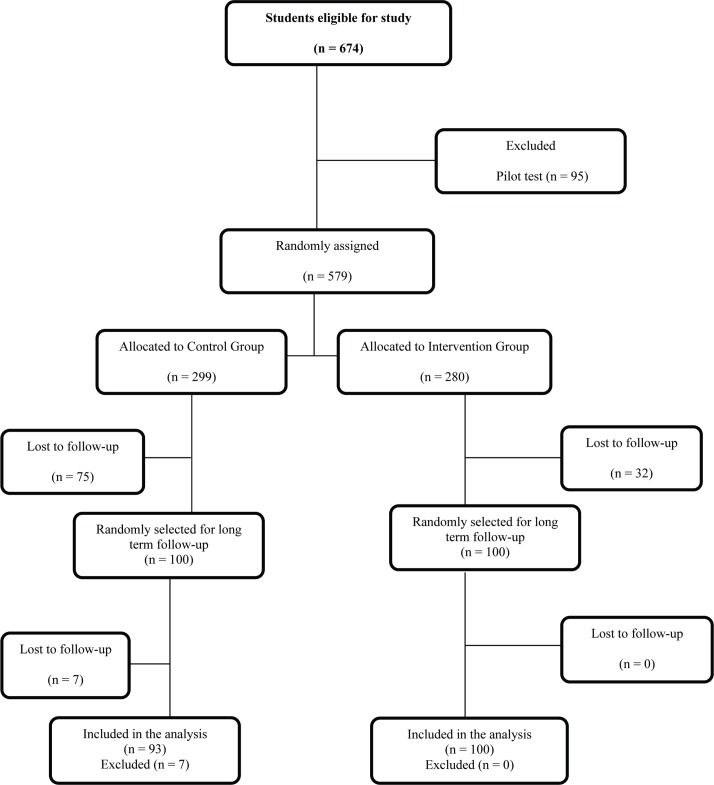
The study was a randomized controlled intervention among twelve schools in the district of Sangre Grande that met the criterion for the inclusion of having more than fifteen children in the sixth year. One school was randomly selected from this group, using the SPSS for Windows statistical software package, version 11 (SPSS Inc., Chicago, IL, USA) for pre-testing of the level of comprehension of the original questionnaire. Our analyses of the responses and questioning of the students suggested that the questionnaire items were largely comprehensible to all. Following this, we made the appropriate modifications taking into consideration the suggestions of the students. This school took no further part in the study. Of the eleven remaining schools, five were randomly assigned to the intervention group (IVG) and six to the non-intervention group (NIVG) using a table of random numbers. Four hundred and seventy-two (IVG, n = 248 and NIVG, n = 224) of the initial 579 students were evaluated three months post-intervention. We also collected qualitative data on the intervention from students, teachers and principals. The result of the short-term impact of this intervention has been reported elsewhere (28). We followed a random sample of one hundred students from each of these groups and conducted an evaluation 18 months postintervention (PI). The Ministry of Education, Trinidad and Tobago and The University of the West Indies, St Augustine, approved the study. All study participants had written parental consent and consent of their respective school principal. Figure 1 shows the distribution of participants through the study.
Fig. 1. Distribution of participants throughout the study.
Procedure
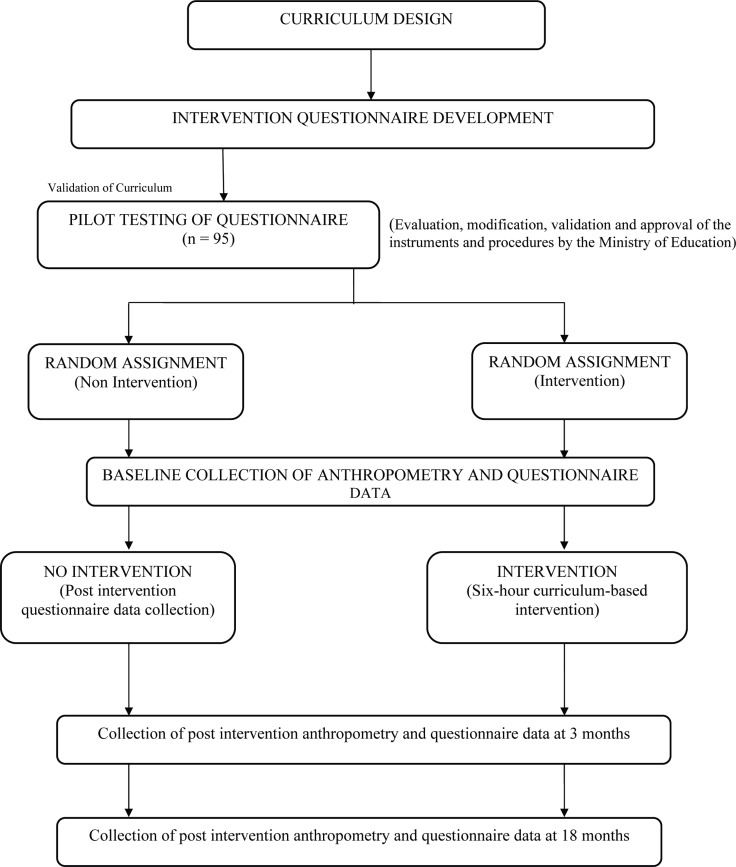
The detailed curriculum was developed, validated and approved at The University of the West Indies with input from primary-school curriculum officers of the Ministry of Education. Our methods have been published in detail elsewhere (28). To summarize, a pretested questionnaire and schoolbased curriculum was conducted on the study sample. We used a modified Block food frequency questionnaire (FFQ) to collect information on consumption patterns of participants within the past seven days prior to the interview. Similarly, we asked participants to indicate on the relevant section of the questionnaire the frequency and duration of physical activity for the seven days preceding participation in the study. We estimated the average daily serving for each food group by dividing the total servings of the food group by seven. Physical activity was classified into low-intensity activity (eg reading a book while sitting in class) and moderate- to high-intensity activity (walking, jogging, playing with friends, playing sports). The questionnaire followed the normal structure of a school day to assist the participant in recalling. The curriculum consisted of lessons on nutrition and physical activity based on Bloom's mastery learning model. The content of the curriculum engaged the students in the learning process with activities and experiences geared toward broadening their interest and mastery of learning outcomes. These activities required participants to work as teams to solve comprehension, vocabulary and mathematics questions based on nutrition-related issues. Specially trained personnel implemented the curriculum and evaluated participants' mastery of knowledge of nutrition and healthy lifestyle practices at the end of each session. We measured weight to the nearest 0.1 kg with an electronic weighing scale (model 770; Seca Corp., Hanover, MD, USA) and height to the nearest millimetre with a portable stadiometer (Seca Corp.) using standardized procedures (29). We used the averages of two readings each for weight and height in subsequent analyses. These we used to calculate body mass index (BMI) – weight in kilograms divided by the square of height in metres (kg/m2). The Centers for Disease Control and Prevention (CDC) age and gender-specific cut-off values were used to categorize BMI into risk of overweight (85th percentile ≤ BMI > 95th percentile) and overweight [BMI ≥ 95th percentile] (30). All measurements were taken with students clad in their school uniform with shoes removed and pockets emptied of their contents. In addition, participants completed the Children's Eating Attitude Test-26 (ChEAT26). This is a 26-item measure that yields a single index of disordered eating attitudes and could provide a measure of participants' feelings and perceptions toward eating (eg 'I do not eat when I am hungry'). Participants were required to rate how each question applied to them by selecting 'always', 'very often', 'often', 'sometimes', 'rarely' or 'never'. We then scored these as recommended (31). Trained personnel were available to assist students where there might have been difficulties in understanding issues on the questionnaire. We re-administered the questionnaire in all participating schools three months and 18 months PI (Fig. 2). Weekly meetings were held with all persons involved in the implementation of the intervention to solve any problems that may have arisen and to ensure quality of measurements and continued standardization of instructions. We collected baseline data for all participating schools during the month of October 2006 and conducted the intervention in the IVG schools over a one-month period.
Fig. 2. Summary of overall study design and implementation.
Statistical analysis
The SPSS for Windows statistical software package, version 11.1 (SPSS Inc., 2001) was used to analyse the data. To assess changes in the outcome variables between the study from baseline and 18 months PI, we used the t-test to determine group differences for normally distributed variables and the Mann-Whitney test for variables that were not normally distributed. We used the Chi-squared test to ascertain whether the intervention was associated with outcomes for categorical variables. We then conducted multivariate linear and logistic regression analyses to assess the effect of the intervention. For each analysis, we entered the change in the variable from baseline to PI as the dependent variable and age, BMI, gender, baseline value of the variable and time spent in moderate-to-vigorous physical activity as independent variables.
RESULTS
One hundred and ninety-three (100 in the IVG and 93 in the NIVG) out of 200 participants were evaluated at 18 months PI. Table 1 shows the characteristics of participants. There were no age or gender differences between participants in the two groups. Participants in both groups were of similar weight, height and BMI. The proportion of participants at risk of overweight and overweight were similar between the groups. Approximately 23% of participants had BMI ≥ 85th percentile of the CDC age-and gender-specific reference. Male participants were significantly taller and heavier than their female counterparts. Table 2 shows knowledge, dietary intakes and attitudes at baseline and 18 months PI by group status. There were no significant differences in the proportion of persons reporting fruit and vegetable consumption levels ≥ 2 servings/day between the IVG and the NIVG 18 months PI. Compared to the persons in the IVG, there was a reduction in the proportion of persons in the NIVG consuming ≥ 2 servings of vegetable per day (p < 0.01). Persons in the IVG had on average significantly higher mean absolute changes in their knowledge scores than participants in the NIVG up to 18 months post baseline. Notwithstanding, both groups experienced significant changes in the knowledge score 18 months PI. Participants in both groups had significantly lower ChEAT 26 scores 18 months PI compared to baseline.
Table 1. Characteristics of participants by group.
| Variables | IVG Mean (SD) = 100 | NIVG Mean (SD) n = 93 | p-value |
|---|---|---|---|
| Current age (years) | 11.7 (0.9) | 11.7 (1.4) | 0.83 |
| Weight (kg) | 45.3 (12.5) | 45.4 (10.6) | 0.94 |
| Height (cm) | 156.2 (8.4) | 154.5 (10.4) | 0.23 |
| BMI (kg/m2) | 18.5 (4.3) | 19.1 (4.3) | 0.35 |
| % | % | ||
| Weight category | |||
| 85th percentile < BMI | 76.1 | 77.6 | |
| 85th percentile ≤ BMI < 95th percentile | 13.5 | 11.2 | |
| BMI ≥ 95th percentile | 10.4 | 11.2 | |
| χ2 | 0.45 | ||
| Gender | |||
| Male | 42.4 | 41.8 | |
| Female | 57.6 | 58.2 | |
| χ2 | 1.0 | ||
IVG = intervention group, NIVG = non-intervention group, BMI = body mass index
Table 2. Knowledge, dietary intakes and attitudes at baseline (B) and 18 months post-intervention (PI) by group status.
| Variable | IVG | NIVG | p-value | |
|---|---|---|---|---|
| B | Fruit intake ≥ 2 servings/day (%) | 49.0 | 61.2 | 0.008 |
| PI | Fruit intake ≥ 2 servings/day (%) | 43.4 | 52.7 | 0.2 |
| Change | -5.6 | -8.5 | ||
| p-value | 0.3 | 0.2 | ||
| B | Fruit eaten in past 24 hours (%) | 90.6 | 88.4 | 0.4 |
| PI | Fruit eaten in past 24 hours (%) | 81.8 | 87.8 | 0.2 |
| Change | -8.8 | -0.6 | ||
| p-value | 0.02 | 0.9 | ||
| B | Vegetable intake ≥ 2 servings/day (%) | 33.9 | 47.0 | 0.004 |
| PI | Vegetable intake ≥ 2 servings/day (%) | 27.3 | 15.6 | 0.05 |
| Change | -6.6 | -31.4 | ||
| p-value | 0.2 | < 0.0001 | ||
| B | Vegetables eaten in past 24 hours (%) | 60.3 | 74.1 | 0.001 |
| PI | Vegetables eaten in past 24 hours (%) | 73.3 | 70.7 | 0.5 |
| Change | +13 | -3.4 | ||
| p-value | 0.02 | 0.7 | ||
| B | Percentage knowledge score, mean (SD) | 46.0 (19.4) | 41.3 (23.1) | 0.02 |
| PI | Percentage knowledge score, mean (SD) | 69.7 (46.1) | 52.7 (50.2) | 0.02 |
| Change | +23.7 | +11.4 | ||
| p-value | < 0.0001 | 0.006 | ||
| B | ChEAT26 score, mean (SD) | 12.1 (9.5) | 13.8 (9.7) | 0.06 |
| PI | ChEAT26 score, mean (SD) | 6.7 (5.3) | 8.5 (5.9) | 0.03 |
| Change | -5.4 | -5.3 | ||
| p-value | 0.0001 | < 0.0001 | ||
| B | Soda intake 8 oz servings/week, mean (SD) | 4.6 (3.9) | 3.4 (3.6) | 0.0006 |
| PI | Soda intake 8 oz servings/week, mean (SD) | 3.5 (3.6) | 7.7 (6.5) | < 0.0001 |
| Change | -1.1 | +4.3 | ||
| p-value | 0.02 | < 0.0001 | ||
| B | Soda intake in past 24 hours (%) | 67.4 | 53.2 | 0.002 |
| PI | Soda intake in past 24 hours (%) | 26.3 | 40.4 | 0.002 |
| Change | -41 | -12.8 | ||
| p-value | 0.0001 | 0.04 | ||
| B | Fried food servings/day, mean (SD) | 3.0 (3.1) | 2.4 (2.5) | 0.1 |
| PI | Fried food servings/day, mean (SD) | 0.89 (1.4) | 1.8 (2.2) | 0.0007 |
| Change | -2.11 | -0.6 | ||
| p-value | < 0.0001 | 0.05 | ||
| B | Fried food eaten in past 24 hours (%) | 85.0 | 74.4 | 0.004 |
| PI | Fried food eaten in past 24 hours (%) | 70.0 | 72.0 | 0.8 |
| Change | -15 | -2.4 | ||
| p-value | 0.001 | 0.7 | ||
| B | HFSS foods 502 KJ/day (120 kcal/day), mean (SD) | 4.6 (4.4) | 4.5 (5.2) | -0.8 |
| PI | HFSS foods 502 KJ/day (120 kcal/day), mean (SD) | 3.8 (3.5) | 4.2 (3.8) | 0.5 |
| Change | 0.8 | -0.3 | ||
| p-value | 0.1 | 0.6 | ||
| B | HFSS foods eaten in past 24 hour (%) | 85 | 74 | 0.003 |
| PI | HFSS foods eaten in past 24 hour (%) | 46 | 80 | 0.0001 |
| Change | -28 | +6 | ||
| p-value | 0.0001 | 0.3 |
IVG = intervention group, NIVG = non-intervention group, ChEAT26 = Children's Eating Attitude Test-26, HFSS = high in fat, sugar and salt2: Knowledge, dietary intakes and attitudes at baseline (B) and 18 months post-intervention (PI) by group status
Participants in the NIVG reported significantly higher mean intakes of sodas compared to participants in the NIVG at 18 months PI. Overall, there was a significant reduction in soda consumption among participants in the IVG, which was sustainable throughout the intervention. There was a significant decline in the proportion of persons in both groups reporting soda consumption in the 24 hours preceding the interview. Average reported daily servings of fried foods were significantly lower in the IVG than the NIVG. In addition, there was a significant decline in reported fried food intakes in the IVG at the PI assessment compared to baseline. Finally, there was a significant increase (+18.2%; p < 0.05) in the proportion of persons reporting participation in moderate-to-high intensity activity at school at least three times per week in the IVG only (Table 3).
Table 3. Physical activity pattern at baseline (B) and 18 months post-intervention (PI) by group status.
| Variable | IVG | NIVG | p-value | |
|---|---|---|---|---|
| B | Moderate to high-intensity physical activity > 1 hour/week (%) | 51.2 | 76.8 | 0.001 |
| PI | Moderate to high-intensity physical activity > 1 hour/week (%) | 69.4 | 84.4 | 0.01 |
| Change | +18.2 | +7.6 | ||
| p-value | 0.002 | 0.1 | ||
| B | Vigorous activity in past 24 hours (%) | 51.3 | 53.2 | 0.7 |
| PI | Vigorous activity in past 24 hours (%) | 78.0 | 63.2 | 0.02 |
| Change | +26.7 | +11.9 | ||
| p-value | 0.0001 | 0.1 | ||
| B | Frequency of low-level activity/week, mean (SD) | 3.0 (3.1) | 2.4 (2.5) | 0.9 |
| PI | Frequency of low-level activity/week, mean (SD) | 2.5 (2.6) | 2.4 (2.6) | 0.9 |
| Change | -0.5 | 0 | ||
| p-value | 0.9 | NS | ||
| B | Low-level activity in past 24 hours (%) | 85.0 | 74.4 | 0.004 |
| PI | Low-level activity in past 24 hours (%) | 61.8 | 58.2 | 0.6 |
| Change | -23.2 | -16.2 | ||
| p-value | 0.0001 | 0.004 | ||
| B | Television viewing > 2 hours/day (%) | 44.9 | 36.0 | 0.05 |
| PI | Television viewing > 2 hours/day (%) | 61.4 | 65.0 | 0.6 |
| Change | +16.5 | +29.0 | ||
| p-value | 0.005 | < 0.0001 |
Tables 4a and 4b show the results of multivariate analyses. In multivariate regression equations controlling for age, gender, BMI, baseline value, time spent in moderate-to-high physical activity, intervention was significantly associated with lower levels of intakes of fried foods, sodas, snack foods high in fats, sugar and salt (HFSS), and higher knowledge scores. Intervention was not significantly associated with fruit and vegetable intakes, physical activity and ChEAT scores after controlling for age, gender, BMI and the relevant baseline values. Further adjusting for ethnicity did not change these findings. Time spent in moderate-to-vigorous physical activity was positively significantly associated with consumption of fruit and HFSS.
Table 4a. Regression analyses for post-intervention dietary intakes and intervention status controlling for the effects of age, body mass index (BMI), gender, physical activity and baseline.
| Soda | Fried foods | Post-intervention Snack foods high in fats, sugar, and salt | Vegetable | Fruit | |
|---|---|---|---|---|---|
| Constant | 7.40 | 6.90 | 12.6 | -4.00 | 2.00 |
| Status | -3.00* | -7.90* | -0.25 | -0.19 | 0.61 |
| Gender | -1.40 | -1.60 | -3.20* | -0.30 | -1.00 |
| Age | -0.25 | 0.80 | -0.11 | 0.21 | 0.01 |
| Current BMI | -0.01 | -0.05 | -0.43** | 0.13** | 0.07 |
| Time spent in moderate-to-vigorous physical activity | 0.02 | -0.08 | 0.04* | 0.007 | 0.03** |
| Baseline | 0.37** | 0.02 | 0.06** | 0.03** | -0.005 |
| Adjusted R2 (%) | 11.1 | 3.8 | 15.0 | 21.4 | 3.8 |
Table 4b. Regression analyses for post-intervention nutrition knowledge and dietary related behaviours and intervention status controlling for the effects of age, body mass index (BMI), gender and baseline.
| Post-intervention | |||||
|---|---|---|---|---|---|
| Moderate-to-high intensity physical activity | Low intensity physical activity | TV viewing | Knowledge | Childhood Eating Attitude Test 26 (ChEAT 26) | |
| Constant | 53.20 | 0.80 | 0.50 | 28.8 | 4.2 |
| Status | -11.60 | 0.17 | 0.08 | 1.70* | -0.90 |
| Gender | 9.30 | -0.06 | -0.09 | -1.10 | -1.50 |
| Age | 0.02 | 0.07 | -0.004 | -0.90** | 0.40 |
| BMI | 0.70 | 0.01 | 0.09** | 0.009 | 0.05 |
| Baseline | 2.60 | 0.17* | 0.06 | 0.20** | 0.07 |
| Adjusted R2 (%) | 0.8 | 0.8 | 21.6 | 13.0 | 0.6 |
DISCUSSION
We evaluated the effectiveness of a school-based intervention on improving long-term knowledge, attitude and behaviour of primary school children toward better dietary and activity habits. The results suggest that this intervention resulted in significantly lower reported intakes of sodas and fried foods and higher knowledge scores after controlling for age, gender, BMI and baseline intakes of these foods in the long-term. The intervention had no impact on long-term fruit and vegetable intakes after controlling for age, gender, BMI and baseline intakes of these foods. This is similar to the findings of other studies and suggests that such interventions may lead to sustainable changes in the consumption of individual food groups (23, 32–37). It also underscores the need to understand the environmental enablers and barriers to healthy food consumption patterns and maintenance of healthy body composition ranges (15, 38, 39).
Participants in this study spend approximately 35 hours each week at school. In addition, many of them are recipients of breakfast and lunch as part of the National School Feeding Programme administered by the National Schools Dietary Services Limited. Thus, the school environment provides us with the opportunity to understand the barriers and enablers to healthy dietary behaviours. It also provides us with the opportunity to alter the environment in a manner that would result in healthier eating behaviours (10, 40, 41). Such interventions may consider menu alteration and healthy choices. Such interventions also need to take into consideration the context in which foods are consumed in the home and community if they are going to sustain the appropriate behaviour changes into adulthood (10).
Our intervention was quite successful in improving the knowledge and awareness on issues related to nutrition and physical activity in the long term. This is consistent with the findings of other studies. Furthermore, it suggests that the approach used in this study may be applicable to the entire primary school population as the participating schools in this region had scores among the lower percentiles on the National School Assessment Examinations (42–44). The limited contact hours with participants suggests that even short exposure in a well-designed and culturally relevant school-based intervention can result in significant increases in knowledge and awareness among children in a cost-effective manner (45). The PI evaluation of the curriculum with teachers and principals of all the intervention schools suggests that the intervention was successful and non-disruptive to the day-to-day school and curriculum processes and required little additional resources. Moreover, the majority of the students were able to achieve mastery of the modules (28).
The results of this study suggest that the intervention had no significant long-term effect on the level of physical activity when age, BMI, gender and baseline level of physical activity are taken into consideration. This is consistent with the findings of other studies that suggest an overall failure of school- and curriculum-based intervention aimed at sustainable increases in physical activity in childhood (46). Clearly, there is an urgent need to evaluate different types of interventions in our population in order to identify those that are effective in increasing participation in physical activity among our children.
The major strength of this study lies in its design. As an intervention study, it provides strong evidence for a causal relation between the intervention and outcomes. In addition, collection of qualitative data from students and staff members of the schools provides useful insights into the possibility of success of such intervention in the school system. Notwithstanding, the study has a few limitations. First, the study was conducted in one area of the country that may not be representative of the general population. Secondly, dietary intakes and physical activity were reported and therefore subject to recall biases. Finally, the study focusses primarily on the school environment without investigation of the home and community context of nutrition behaviours and therefore limits its ability to provide a more complete picture of eating behaviours among participants. Consequently, the results should be interpreted with caution.
CONCLUSION
The intervention was associated with lower reported levels of intakes of fried foods and soda after controlling for age, gender, BMI and the appropriate baseline value in the long term. It also resulted in greater knowledge and awareness on issues related to nutrition and physical activity. Overall, our results suggest that intervention of this kind may be implemented successfully in the school system in Trinidad and Tobago.
ACKNOWLEDGEMENTS
We are grateful to the Ministry of Education, Trinidad and Tobago, for approval of the investigation and granting access to the participating schools. To the principal and teachers, we express a heartfelt thank you for their accommodation and participation in the study. We thank the National Schools Dietary Services Limited, Trinidad and Tobago, for providing serving size portions of foods commonly eaten by participants. Finally, we thank the student and parents for agreeing to participate in this intervention.
REFERENCES
- 1.Sinha DP. Changing patterns of food, nutrition and health in the Caribbean. Nut Research. 1995;15:899–938. [Google Scholar]
- 2.Pan American Health Organization Publication; Caribbean Community Secretariat (CARICOM) Report of the Caribbean commission on health and development. Jamaica: Ian Randle Publishers; 2006. [Google Scholar]
- 3.Barceló A, Gregg EW, Pastor-Valero M, Robles SC. Waist circumference, BMI and the prevalence of self-reported diabetes among the elderly of the United States and six cities of Latin America and the Caribbean. Diabetes Res Clin Pract. 2007;78:418–427. doi: 10.1016/j.diabres.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 4.Luke A, Cooper RS, Prewitt TE, Adeyemo AA, Forrester TE. Nutritional consequences of the African diaspora. Annu Rev Nutr. 2001;21:47–71. doi: 10.1146/annurev.nutr.21.1.47. [DOI] [PubMed] [Google Scholar]
- 5.Chakravarthy MV, Booth FW. Eating, exercise, and "thrifty" genotypes: connecting the dots toward an evolutionary understanding of modern chronic diseases. J Appl Physiol. 2004;96:3–10. doi: 10.1152/japplphysiol.00757.2003. [DOI] [PubMed] [Google Scholar]
- 6.Heber D. An integrative view of obesity. Am J Clin Nutr. 2010;91(Suppl):280S–283S. doi: 10.3945/ajcn.2009.28473B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Veena SR, Kumaran K, Swarnagowri MN, Jayakumar MN, Leary SD, Stein CE, et al. Intergenerational effects on size at birth in South India. Paediatr Perinat Epidemiol. 2004;18:361–370. doi: 10.1111/j.1365-3016.2004.00579.x. [DOI] [PubMed] [Google Scholar]
- 8.McEnry M, Palloni A. Early life exposures and the occurrence and timing of heart disease among the older adult Puerto Rican population. Demography. 2010;47:23–43. doi: 10.1353/dem.0.0093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gaskin PS, Walker SP. Obesity in a cohort of black Jamaican children as estimated by BMI and other indices of adiposity. Eur J Clin Nutr. 2003;57:420–426. doi: 10.1038/sj.ejcn.1601564. [DOI] [PubMed] [Google Scholar]
- 10.Flynn MA, McNeil DA, Maloff B, Mutasingwa D, Wu M, Ford C, et al. Reducing obesity and related chronic disease risk in children and youth: a synthesis of evidence with 'best practice' recommendations. Obes Rev. 2006;7(Suppl 1):7–66. doi: 10.1111/j.1467-789X.2006.00242.x. [DOI] [PubMed] [Google Scholar]
- 11.Lioret S, Volatier JL, Lafay L, Touvier M, Maire B. Is food portion size a risk factor of childhood overweight? Eur J Clin Nutr. 2009;63:382–391. doi: 10.1038/sj.ejcn.1602958. [DOI] [PubMed] [Google Scholar]
- 12.Nichols SD, Cadogan F. BMI-based obesity cutoffs and excess adiposity in a Caribbean adolescent population of African origin. Eur J Clin Nutr. 2009;63:253–258. doi: 10.1038/sj.ejcn.1602913. [DOI] [PubMed] [Google Scholar]
- 13.Donin AS, Nightingale CM, Owen CG, Rudnicka AR, McNamara MC, Prynne CJ, et al. Ethnic differences in blood lipids and dietary intake between UK children of black African, black Caribbean, South Asian, and white European origin: the Child Heart and Health Study in England (CHASE) Am J Clin Nutr. 2010;92:776–783. doi: 10.3945/ajcn.2010.29533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Owen CG, Nightingale CM, Rudnicka AR, Sattar N, Cook DG, Ekelund U, et al. Physical activity, obesity and cardiometabolic risk factors in 9-to 10-year-old UK children of white European, South Asian and black African-Caribbean origin: the Child Heart And Health Study in England (CHASE) Diabetologia. 2010;53:1620–1630. doi: 10.1007/s00125-010-1781-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Epstein LH, Valoski A, Wing RR, McCurley J. Ten years follow-up of behavioural family-based treatment for obese children. JAMA. 1990;264:2519–2523. [PubMed] [Google Scholar]
- 16.Ashcroft J, Semmler C, Carnell S, van Jaarsveld CH, Wardle J. Continuity and stability of eating behaviour traits in children. Eur J Clin Nutr. 2008;62:985–990. doi: 10.1038/sj.ejcn.1602855. [DOI] [PubMed] [Google Scholar]
- 17.Seidell JC, Verschuren WM, van Leer EM, Kromhout D. Overweight, underweight, and mortality. A perspective study of 48 287 men and women. Arch Intern Med. 1996;156:958–963. doi: 10.1001/archinte.156.9.958. [DOI] [PubMed] [Google Scholar]
- 18.Telama R, Yang X, Viikari J, Välimäki II, Wanne O, Raitakari O. Physical activity from childhood to adulthood: a 21-year tracking study. Am J Prev Med. 2005;28:267–273. doi: 10.1016/j.amepre.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 19.Sharma M. International school-based interventions for preventing obesity in children. Obes Rev. 2008;8:155–167. doi: 10.1111/j.1467-789X.2006.00268.x. [DOI] [PubMed] [Google Scholar]
- 20.Kolbe LJ. Increasing the impact of school health promotion programs: emerging research perspectives. Health Educ. 1986;17:47–52. [PubMed] [Google Scholar]
- 21.French SA. Public health strategies for dietary change: schools and workplaces. J Nutr. 2005;135:910–912. doi: 10.1093/jn/135.4.910. [DOI] [PubMed] [Google Scholar]
- 22.Flodmark C-E, Marcus C, Brittton M. Interventions to prevent obesity in children and adolescents: a systematic literature review. Int J Obes. 2006;30:579–589. doi: 10.1038/sj.ijo.0803290. [DOI] [PubMed] [Google Scholar]
- 23.Spiegel S, Foulk D. Reducing overweight through a multidisciplinary school-based intervention. Obesity (Silver Spring) 2006;14:88–96. doi: 10.1038/oby.2006.11. [DOI] [PubMed] [Google Scholar]
- 24.Campbell KJ, Crawford DA, Salmon J, Carver A, Garnett SP, Baur LA. Associations between the home food environment and obesity-promoting eating behaviors in adolescence. Obesity (Silver Spring) 2007;15:719–730. doi: 10.1038/oby.2007.553. [DOI] [PubMed] [Google Scholar]
- 25.Contento IR, Koch PA, Lee H, Calabrese-Barton A. Adolescents demonstrate improvement in obesity risk behaviors after completion of choice, control & change, a curriculum addressing personal agency and autonomous motivation. J Am Diet Assoc. 2010;110:1830–1839. doi: 10.1016/j.jada.2010.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Patrick K, Norman GJ, Calfas KJ, Sallis JF, Zabinski MF, Rupp J, et al. Diet, physical activity, and sedentary behaviors as risk factors for overweight in adolescence. Arch Pediatr Adolesc Med. 2004;158:385–390. doi: 10.1001/archpedi.158.4.385. [DOI] [PubMed] [Google Scholar]
- 27.Taylor RW, Mcauley KA, Williams SM, Barbezat W, Nielsen G, Mann JI. Reducing weight gain in children through enhancing physical activity and nutrition: the APPLE project. Int J Pediatr Obes. 2006;1:146–152. doi: 10.1080/17477160600881247. [DOI] [PubMed] [Google Scholar]
- 28.Francis M, Nichols SDS, Dalrymple M. The effects of a school-based intervention programme on dietary intakes and physical activity among primary school children in Trinidad and Tobago. Public Health Nutr. 2010;13:738–747. doi: 10.1017/S1368980010000182. [DOI] [PubMed] [Google Scholar]
- 29.Lohman T, Roche A, Martorell R, editors. Anthropometric standardization reference manual. Champaign, Illinois: Human Kinetics Book; 1988. [Google Scholar]
- 30.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, et al. CDC growth charts: United States. Adv Data. 2000;314:1–27. [PubMed] [Google Scholar]
- 31.Maloney MJ, McGuire JB, Daniels SR. Reliability testing of a children's version of the Eating Attitude Test. J Am Acad Child Adolesc Psychiatry. 1988;27:541–543. doi: 10.1097/00004583-198809000-00004. [DOI] [PubMed] [Google Scholar]
- 32.Schor EL. American Academy of Pediatrics Task Force on the Family Family pediatrics: report of the Task Force on the Family. Pediatrics. 2003;111:1541–1571. [PubMed] [Google Scholar]
- 33.Anderson AS, Porteous LE, Foster E, Higgins C, Stead M, Hetherington M, et al. The impact of a school-based nutrition education intervention on dietary intake and cognitive and attitudinal variables relating to fruits and vegetables. Public Health Nutr. 2005;8:650–656. doi: 10.1079/phn2004721. [DOI] [PubMed] [Google Scholar]
- 34.Aranceta Bartrina J, Pérez-Rodrigo C. Resources for a healthy diet: school meals. Br J Nutr. 2006;96(Suppl 1):S78–S81. doi: 10.1079/bjn20061705. [DOI] [PubMed] [Google Scholar]
- 35.Nelson M, Lowes K, Hwang V. members of the Nutrition Group, School Meals Review Panel, Department for Education and Skills The contribution of school meals to food consumption and nutrient intakes of young people aged 4–18 years in England. Public Health Nutr. 2007;10:652–662. doi: 10.1017/S1368980007382529. [DOI] [PubMed] [Google Scholar]
- 36.Neumark-Sztainer DR, Friend SE, Flattum CF, Hannan PJ, Story MT, Bauer KW, et al. New moves – preventing weight-related problems in adolescent girls a group – randomized study. Am J Prev Med. 2010;39:421–432. doi: 10.1016/j.amepre.2010.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.O'Toole TP, Anderson S, Miller C, Guthrie J. Nutrition services and foods and beverages available at school: results from the School Health Policies and Programs Study 2006. J Sch Health. 2007;77:500–521. doi: 10.1111/j.1746-1561.2007.00232.x. [DOI] [PubMed] [Google Scholar]
- 38.Davison KK, Lawson CT. Do attributes in the physical environment influence children's physical activity? Areview of the literature. [[cited 2013 Dec 20]];Int J Behav Nutr Phys Act. 2006 3:19–19. doi: 10.1186/1479-5868-3-19. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1557665/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rodenburg G, Oenema A, Kremers SP, van de Mheen D. Clustering of diet- and activity-related parenting practices: cross-sectional findings of the INPACT study. [[cited 2013 Dec 20]];Int J Behav Nutr Phys Act. 2013 10:36–36. doi: 10.1186/1479-5868-10-36. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3618009/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McVey G, Tweed S, Blackmore E. Healthy schools-healthy kids: a controlled evaluation of a comprehensive universal eating disorder prevention program. Body Image. 2007;4:115–136. doi: 10.1016/j.bodyim.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 41.Raich RM, Portell M, Peláez-Fernández MA. Evaluation of a schoolbased programme of universal eating disorders prevention: is it more effective in girls at risk? Eur Eat Disord Rev. 2010;18:49–57. doi: 10.1002/erv.968. [DOI] [PubMed] [Google Scholar]
- 42.Harrabi I, Maatoug J, Gaha M, Kebaili R, Gaha R, Ghannem H. Schoolbased intervention to promote healthy lifestyles in Sousse, Tunisia. Indian J Community Med. 2010;35:94–99. doi: 10.4103/0970-0218.62581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shah P, Misra A, Gupta N, Hazra DK, Gupta R, Petal Seth. Improvement in nutrition-related knowledge and behaviour of urban Asian Indian school children: findings from the 'Medical education for children/Adolescents for Realistic prevention of obesity and diabetes and for healthy ageing' (MARG) intervention study. Br J Nutr. 2010;104:427–436. doi: 10.1017/S0007114510000681. [DOI] [PubMed] [Google Scholar]
- 44.Singhal N, Misra A, Shah P, Gulati S. Effects of controlled school-based multi-component model of nutrition and lifestyle interventions on behavior modification, anthropometry and metabolic risk profile of urban Asian Indian adolescents in North India. Eur J Clin Nutr. 2010;64:364–373. doi: 10.1038/ejcn.2009.150. [DOI] [PubMed] [Google Scholar]
- 45.Mihas C, Mariolis A, Manios Y, Naska A, Arapaki A, Mariolis-Sapsakos T, et al. Evaluation of a nutrition intervention in adolescents of an urban area in Greece: short- and long-term effects of the VYRONAS study. Public Health Nutr. 2010;13:712–719. doi: 10.1017/S1368980009991625. [DOI] [PubMed] [Google Scholar]
- 46.Dobbins M, De Corby K, Robeson P, Husson H, Tirilis D. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6-18. Cochrane Database Syst Rev. 2009;21 doi: 10.1002/14651858.CD007651. CD007651. [DOI] [PubMed] [Google Scholar]