Abstract
We report the case of a 45-year old woman with a painless soft tissue mass on the left side of her neck. At surgery, the lesion was solid and rubbery and revealed grey-white fibrous areas. It was pathologically confirmed as an elastofibroma, a rare, benign soft tissue tumour that is most commonly encountered in patients more than 55 years of age. Elastofibroma arising from connective tissue and usually found in the subscapular region is extremely rare in the neck. The pathogenesis of elasto-fibroma is still unclear but increased mechanical stress or nutritional derangement consequent to vascular involvement and hereditary factors may predispose to this lesion. Marginal excision is the treatment of choice in symptomatic patients.
Keywords: Computed tomography, elastofibroma, magnetic resonance imaging, neck
Abstract
Reportamos el caso de una mujer de 45 años con una masa de tejido suave sin dolor en el lado izquierdo del cuello. Al realizarse la cirugía, se halló que la lesión era sólida y gomosa, y presentaba áreas fibrosas de color gris-blanco. El análisis patológico confirmó que se trataba de un elastofibroma: un tumor del tejido blando, raro y benigno, que se encuentra más comúnmente en pacientes de más de 55 años de edad. Los elastofibromas que provienen del tejido conjuntivo y que generalmente se encuentran en la región subescapular, son extremadamente raros en el cuello. La patogénesis del elastofibroma no está todavía clara, pero el aumento del estrés mecánico o los desarreglos nutricionales consecuencia de problemas vasculares y factores hereditarios, pueden predisponer a esta lesión. La extirpación marginal es el tratamiento de elección en pacientes sintomáticos.
INTRODUCTION
Elastofibroma is a rare fibrous lesion that is most commonly encountered in the elderly and arises chiefly from connective tissue between the inferomedial portion of the scapula and the chest wall. This lesion can occur bilaterally and may appear asynchronously. The occurrence of elastofibroma in other anatomic sites has been reported. We describe the first typical case of elastofibroma of the neck.
CASE REPORT
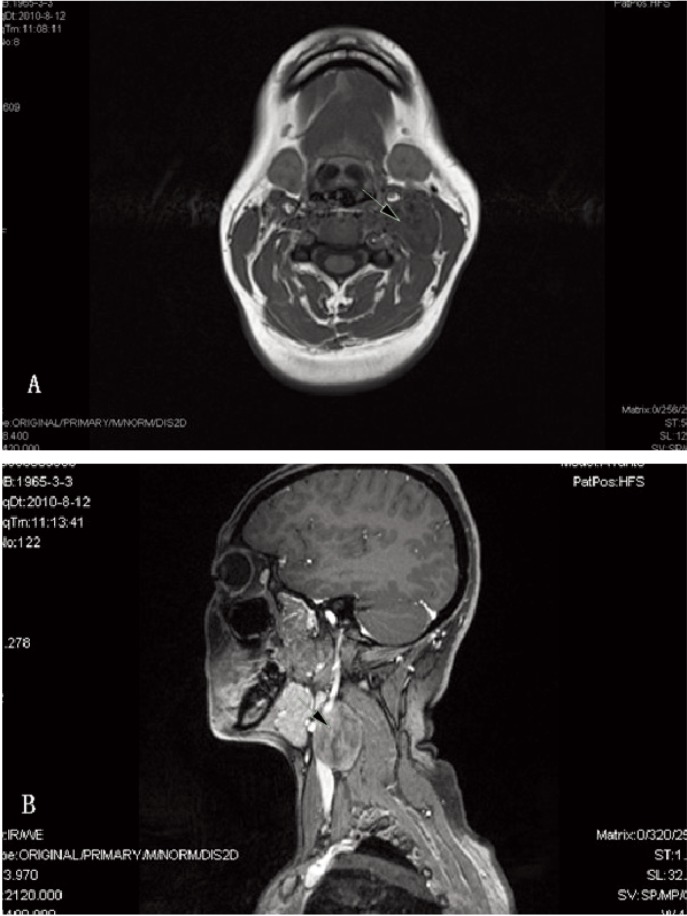
A 45-year old woman presented at our otolaryngology department with a painless soft tissue mass on the left side of her neck. The mass had grown slowly over three months, without any limitation in neck movement. The patient did not report any history of trauma. She was a housewife and her family history was unremarkable. On palpation, the mass was firm, had an even surface and was movable relative to surrounding tissues. Magnetic resonance imaging (MRI) demonstrated a mass located inside the left sternocleido-mastoid (Fig. 1). A chest radiograph and preoperative laboratory investigations were within normal limits.
Fig. 1. (A) T1-weighted image shows a relatively well-defined, inho-mogeneous mass inside of the left sternocleidomastoid (arrow). The mass has intermediate signal intensity approximately equal to that of the surrounding muscle. (B) T2-weighted image shows signal intensity approximately the same as the muscle (arrow).
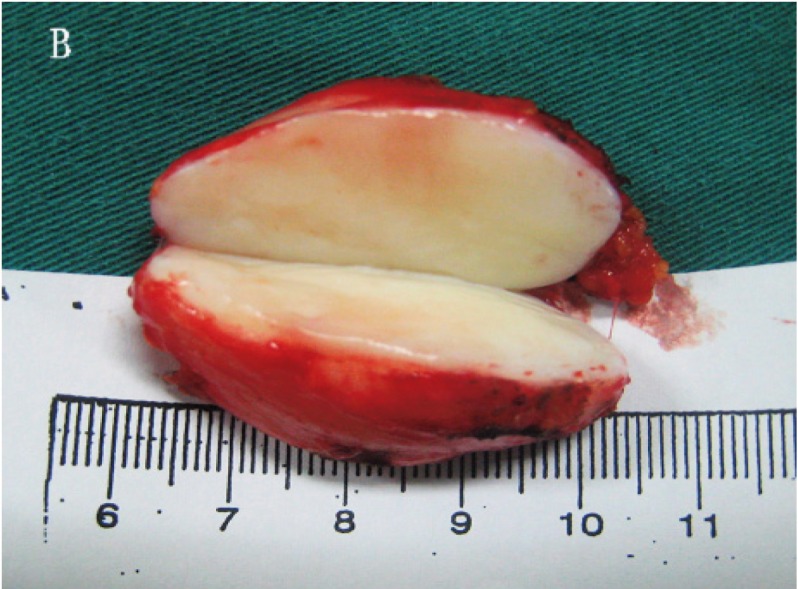
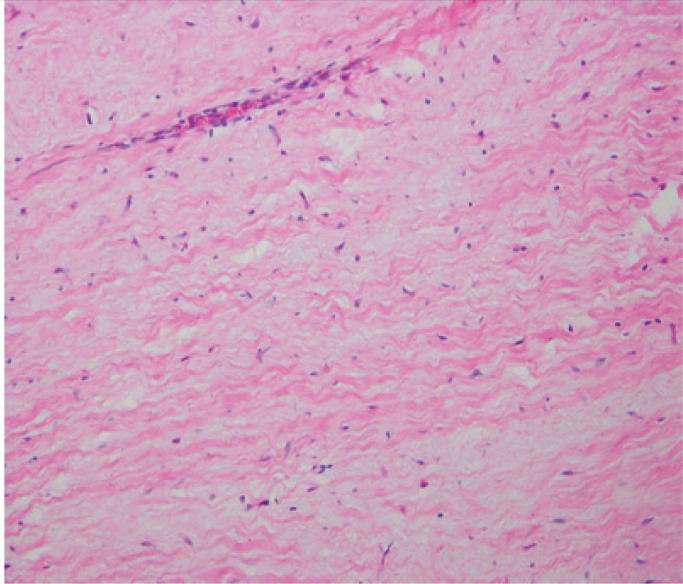
At the time of surgery under general anaesthesia, it was found that the internal jugular vein and common carotid artery were compressed. The mass was firmly adhered to the surrounding nerves but the nerves were still intact. There were many lymph nodes on the surface of the mass. On gross examination, the lesion was solid and rubbery and revealed grey-white fibrous areas (Fig. 2A). The mass measured approximately 4 cm in its largest dimension (Fig. 2B). It was completely excised. The primary suspicion at this point was neurofibroma, but the histopathologic diagnosis was elastofibroma (Fig. 3). The patient's postoperative course was satisfactory and she was discharged after two weeks. She was seen for follow-up seven months postoperatively and had neither recurrence of the elastofibroma nor any problems caused by the tumour resection.
Fig. 2. (A) Macroscopic appearance of the elastofibroma.
Fig. 2. (B) The excised elastofibroma, measuring 4 cm in diameter.
Fig. 3. The histologic appearance of the tumour shows collagen fibre bundles, abnormal elastic fibres and spindle cells suggestive of fibroblasts. The collagen fibres are interlaced with the elastic fibres (stain, haematoxylin and eosin; original magnification, × 200).
DISCUSSION
Elastofibroma is a benign soft tissue tumour mostly of the subscapular region (1), which was first reported by Jarvi and Saxen as “elastofibroma dorsi” in 1961 (2). The reported cases of elastofibroma are mostly in patients more than 55 years of age, and occur more commonly in women than in men (3). Elastofibromas are quite rarely found in locations other than subscapular, such as the infraolecranon, the deltoid muscle and the oculi (3–5). Although one case involving the neck had been previously reported (6), the imaging features and location are atypical. But we describe the first typical case of elastofibroma of the neck.
The pathogenesis of elastofibroma is not completely understood. Increased mechanical stress or nutritional derangement consequent to vascular involvement and hereditary factors may predispose to this lesion (3, 7). For example, elastofibroma occurs in the subscapular region because of friction between the chest wall and the scapula. In the index patient, who had never in her life done heavy work, there were no precipitating factors or activities to explain its occurrence in the neck.
Ultrasonography, computed tomography (CT) and MRI can all be used for radiologic diagnosis of elastofibroma. Ultrasonography shows an echogenic soft tissue mass with focal internal hypoechoic areas. Magnetic resonance imaging is the investigative method of choice because of the ability to evaluate signal intensity and the possibility of selectively suppressing the signal from fatty tissue. On T1-weighted and T2-weighted sequences, fibrous tissue produces low-intensity signals identical to that produced by muscular tissue. Computed tomography shows the same changes, but is less sensitive for visualizing the strands of fatty tissue. Most of the reported CT and MRI findings for elastofibroma describe a low-intensity signal comparable to that of muscle and well-defined margins (8). Our case is different from the previously reported case, in both its location and its imaging characteristics (6). Our patient's lesion is unusual in that it did not demonstrate any contiguity with the supraclavicular region and the MRI showed a well-defined lesion correlating closely with the gross surgical specimen of a well-encapsulated mass.
The differential diagnosis includes aggressive fibro-matosis, neurofibroma, cicatricial fibroma, sarcoma, lipoma and malignant fibrous histiocytoma. Marginal excision is the treatment of choice in symptomatic patients, while follow-up is a good solution for asymptomatic patients (9). Marginal excision has been suggested because it carries a low risk of recurrence (8). There are no known cases of malignant degeneration, and only one case of local recurrence has been reported in the literature (3).
In summary, our report of a patient with elastofibroma is aimed at improving the understanding of the diagnosis and treatment of this rare tumour in the neck.
REFERENCES
- 1.Vastamaki M. Elastofibroma scapulae. Clin Orthop. 2001;392:404–408. [PubMed] [Google Scholar]
- 2.Jarvi OH, Saxen AE. Elastofibroma dorsi. Acta Pathol Microbiol Scand. 1961;144(Suppl 51):83–84. [PubMed] [Google Scholar]
- 3.Nagamine N, Nohara Y, Ito E. Elastofibroma in Okinawa: a clinico-pathologic study of 170 cases. Cancer. 1982;50:1794–1805. doi: 10.1002/1097-0142(19821101)50:9<1794::aid-cncr2820500925>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 4.Mirra JM, Straub LR, Jarvi OH. Elastofibroma of the deltoid. A case report. Cancer. 1974;33:234–238. doi: 10.1002/1097-0142(197401)33:1<234::aid-cncr2820330135>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 5.Hsu JK, Cavanagh HD, Green WR. An unusual case of elastofibroma oculi. Cornea. 1997;16:112–119. [PubMed] [Google Scholar]
- 6.Maldjian C, Adam RJ, Maldjian JA, Rudelli R, Bonakdarpour A. Elastofibroma of the neck. Skeletal Radiol. 2000;29:109–111. doi: 10.1007/s002560050021. [DOI] [PubMed] [Google Scholar]
- 7.Jarvi OH, Saxen AE, Hopsu-Havu VK, Wartiovaara JJ, Vaissalo VT. Elastofibroma: a degenerative pseudotumor. Cancer. 1969;23:42–63. doi: 10.1002/1097-0142(196901)23:1<42::aid-cncr2820230105>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 8.Oueslati S, Douira-Khomsi W, Bouaziz MC, Zaouia K. Elastofibroma dorsi: a report on 6 cases. Acta Orthop Belg. 2006;72:237–242. [PubMed] [Google Scholar]
- 9.Muratori F, Esposito M, Rosa F, Liuzza F, Magarelli N, Rossi B, et al. Elastofibroma dorsi: 8 case reports and a literature review. J Orthop Traumatol. 2008;9:33–37. doi: 10.1007/s10195-008-0102-7. [DOI] [PMC free article] [PubMed] [Google Scholar]