Abstract
Newborn screening (NBS) for sickle cell disease (SCD) has occurred in Jamaica since 1973 in two periods, the most recent being since 1995. As a result of NBS, significant lessons have been learnt about management of the disease. Additionally, significant improvements in morbidity and mortality of children affected with the disease have occurred because of the implementation of simple interventions. Unfortunately, in a country where the burden of disease is high compared to other countries, only approximately 40% of children born in Jamaica currently benefit from NBS. As such, the future of NBS for SCD in Jamaica lies in island-wide screening. There are challenges including the lack of appropriate governance and policy structures, the technology for high-volume processing and comprehensive care clinics throughout the island. On the other hand, the significant strides made in disease management, the strength and model of care of the Sickle Cell Unit, delicately balancing limited resources and increased survival cannot be disparaged. Therefore, consistent with the World Health Organization's recommendation, we are working toward achieving island-wide screening for SCD, to ensure equitable access to continued improvements in morbidity, mortality and quality of life.
Keywords: Newborn, screening, sickle cell disease
Abstract
El tamizaje neonatal (TN) para la enfermedad de células falciformes (ECF) ha ocurrido en Jamaica desde 1973 en dos períodos, siendo el más reciente el que tiene lugar desde 1995. Como resultado del TN, se han aprendido importantes lecciones sobre el manejo de la enfermedad. Además, se han producido mejoras significativas en relación con la morbilidad y la mortalidad de los niños afectados con la enfermedad, en virtud de la implementación de simples intervenciones. Desafortunadamente, en un país donde la carga de la enfermedad es alta en comparación con otros países, sólo aproximadamente el 40% de los niños nacidos en Jamaica se benefician actualmente del TN. Por lo tanto, el futuro del TN para la ECF en Jamaica se encuentra en la proyección del tamizaje a lo largo y ancho de toda la isla. Los desafíos incluyen falta de estructuras adecuadas de administración y establecimiento de políticas, tecnología para el procesamiento de alto volumen, y clínicas de atención integral en toda la isla. Por otro lado, los grandes avances realizados en el manejo de la enfermedad, la fuerza y el modelo de atención de la Unidad de Anemia Falciforme, el cuidadoso manejo de los limitados recursos, y el aumento de la supervivencia no pueden ser menospreciados. Por lo tanto, en consonancia con la recomendación de la Organización Mundial de la salud, estamos trabajando con el propósito de lograr el establecimiento de un tamizaje de la ECF en toda la isla, y lograr así un acceso equitativo a las mejoras continuas en relación con la morbilidad, la mortalidad y la calidad de vida.
INTRODUCTION
Newborn screening programmes are comprehensive systems which provide an essential public health service. Their mission is to eliminate or reduce the mortality, morbidity and disability that result from congenital disease by ensuring that all affected infants receive early diagnosis and long-term treatment in an attempt to achieve optimal health, growth and development. Disorders that can be screened for in the newborn period include: (i) haemoglobinopathies, for example sickle cell disease [SCD], (ii) endocrine diseases such as hypothyroidism and congenital adrenal hypoplasia, (iii) metabolic diseases including phenylketonuria, cystic fibrosis and galactosaemia, and (iv) hearing disorders.
Systematic newborn screening (NBS) for SCD in Jamaica was first undertaken at the Victoria Jubilee Hospital (main government maternity hospital in Jamaica) from 1973–1981 when 100 000 consecutive live, non-operative births were screened, enabling the initiation of the Jamaica Sickle Cell Cohort Study (1). Five hundred and sixty-three babies with SCD were detected: 315 SS, 201 SC, 33 Sβ+, 14 Sβ0. Three hundred and fourteen homozygous sickle cell disease (Hb SS) babies were recruited as a part of this cohort. Two normal (Hb AA) controls born of the same gender and on the same day were matched for the first 125 Hb SS babies. This cohort has provided invaluable information on the natural history of SCD as well as some of the major lessons in disease management (2).
Newborn screening was restarted in 1995 at the Victoria Jubilee Hospital as a collaborative effort between the Sickle Cell Unit (SCU), Kingston, Jamaica, and the Ministry of Health (MOH), Jamaica. The University Hospital of the West Indies was added in October 1997 and Spanish Town Hospital in April 1998. These three hospitals all lie within the South East Regional Health Authority of Jamaica and are responsible for approximately 40% of births island-wide (3). Jamaica has four regional health authorities.
Over the past 18 years since screening was restarted, the laboratory at the SCU has screened just over 249 000 births with approximately 21 000 and 1000 babies having a screening result suggestive of the sickle cell trait and homozygous sickle cell (Hb SS) disease, respectively. Babies with screening results suggestive of SCD (all genotypes), other haemoglobinopathies or with unclear results are traced and brought back to the SCU for confirmatory testing. Currently, all babies confirmed to have SCD are enrolled into the clinic at the SCU for follow-up. Babies with other haemoglobinopathies are referred to the other health facilities for care.
From this programme, as of the 31st December 2012, the SCU now has a new birth cohort, the Jamaica Sickle Cell Unit Birth (JamSCUB) cohort, consisting of approximately 661 children with a severe form of SCD (627 Hb SS, 34 sickle β0-thalassemia (Hb Sβ0); 342 females, 319 males). The mean age of this cohort is 9 ± 4.1 years (range 0.2–17.1 years). Twenty-two (3%) children have died; 481 (73%) are actively being followed. The remainder have defaulted from follow-up [ie not been seen in the past year] (n = 114, 17%), emigrated (n = 7, 1%) or have never come for an initial doctor's visit after confirmatory testing (n = 37, 6%).
Utilizing the JamSCUB cohort and the Jamaica Sickle Cell Cohort Study, Hanchard et al (4) have shown that there has been no decrease in the S allele frequency in Jamaica, which means that, for now, SCD will continue to be a significant health issue in Jamaica. In addition, survival estimates in the childhood period show improvement when compared with the Jamaica Sickle Cell Cohort Study (3). Overall mortality in children 10 years and under decreased from 17.6% in the Jamaica Sickle Cell Cohort Study to 1.8% in the JamSCUB cohort (3). Fewer proportions of hospital admissions and episodes of serious illness were also seen when comparing the two cohorts (3). Further, the standardized mortality ratio, which is the ratio of the mortality rate (observed number of deaths per person-year) among the JamSCUB cohort relative to the mortality rate in the general population of Jamaica (expected number of deaths per person-year) for children less than five years, was 0.47 (95% CI 0.2, 0.9).
An important element of managing SCD in the early childhood period is the prevention of pneumococcal infection with penicillin prophylaxis and vaccinations. Mortality from pneumococcal sepsis decreased by 85% with penicillin prophylaxis (5). Penicillin prophylaxis is given either via the oral route twice daily (penicillin V) or by the intramuscular route every 28 days (benzathine penicillin G). In Jamaica, penicillin prophylaxis is given from the age of four months to four years mostly by the intramuscular route with good compliance (6). In most cases, it can be discontinued only after pneumococcal polysaccharide vaccine is given at age four years.
While penicillin prophylaxis is the mainstay, pneumococcal vaccination is also important in the fight against pneumococcal infection. Pneumococcal polysaccharide vaccination has been given at the SCU for over 25 years (7). The high prevalence of administration of this vaccine, despite the fact that patients pay for the vaccine, has significantly impacted the incidence of invasive pneumococcal disease in this cohort (8). The advent of the pneumococcal conjugate vaccine which is given in the early childhood period has also had a significant impact on the incidence of invasive pneumococcal disease, especially in developed countries. Although a costly vaccine, since 2010, the Ministry of Health has been providing pneumococcal conjugate vaccine to the SCU for administration to children with SCD under the age of five years at no charge to the patient.
More recently, the Manchester Project (9, 10), funded by the National Health Fund, Jamaica, and the Alcoa Project began NBS for SCD in the southern region of Jamaica: Mandeville Regional Hospital in August 2008, Percy Junor and Hargreaves Memorial hospitals in January 2009 and May Pen and Black River hospitals in January 2010. Each year, the project now screens between 8000 and 9000 babies with the detection of approximately 50 babies with SCD. These babies are followed in sickle cell clinics, managed by paediatricians, at the Mandeville Regional Hospital in Manchester.
Testing for sickle cell disease
Since 1973, haemoglobin (Hb) electrophoresis has been the method for diagnosing SCD at the SCU laboratory (11). Haemoglobin electrophoresis is a simple, inexpensive but labour intensive process. It is not good for high volume processing. It is based on the principle that haemoglobin separates at varying pH. The common haemoglobins detected are F, A, S, A2 and C.
At the SCU, blood spots on filter paper, collected from cord blood at or shortly after delivery are initially screened on agar gel (pH 6.4). Confirmatory testing, using mainly heel-prick samples when babies are recalled, is done using cellulose acetate membrane (pH 8.4).
Newer techniques such as high pressure liquid chromatography (HPLC), iso-electric focussing and capillary electrophoresis can also be used for diagnosis. High pressure liquid chromatography is an automated and quantitative process. It is more costly, but less labour intensive than Hb electrophoresis and useful for high volume processing. It is highly sensitive and is capable of differentiating among many abnormal haemoglobins in a single test. The Manchester Project utilizes HPLC for diagnoses of SCD.
WHAT LIES AHEAD
Evidence clearly highlights the benefits of NBS, enrolment into a comprehensive care programme and implementation of simple interventions such as penicillin prophylaxis (3, 5, 12). Such services are essential in countries like Jamaica where the burden of disease is high compared to other countries. As such, the future of NBS for SCD in Jamaica lies with islandwide screening. The implications of this, however, highlight some of the challenges faced, for in addition to mere testing, NBS implies that comprehensive care systems are in place to provide health maintenance for babies diagnosed to have SCD.
Governance
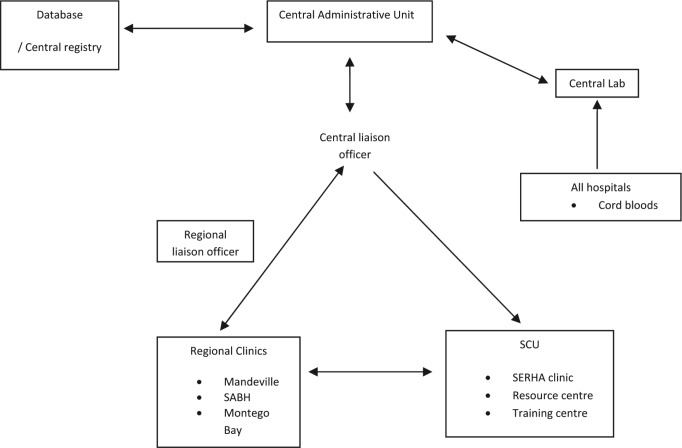
A resolution adopted by the General Assembly of the United Nations in 2008 (13) stated that "sickle cell anaemia is one of the world's foremost genetic diseases, that it has severe physical, psychological and social consequences for those affected and their families, and that in its homozygote form it is one of the most lethal genetic disease" and as such designated sickle cell anaemia as a public health problem. In keeping with this resolution, increasing its recognition as a health priority, SCD has recently been included in the noncommunicable disease policy of the Ministry of Health, Jamaica. Increasing survival means that persons with SCD are living longer and additional complications of the disease, such as renal disease, will now become manifest. The necessary policies need to be put in place to allow for islandwide NBS and to allow patients with SCD, as with other chronic diseases, to benefit from health programmes such as the National Health Fund. In addition, establishment and support of an appropriate administrative unit to provide governance, with appropriate policy guidelines for a sickle cell programme targeting issues such as increasing public awareness of the disease, and disease surveillance and management in keeping with the model (Figure) is critical.
Figure. Organization of newborn screening programme.
SABH – St Ann's Bay Hospital, SCU – Sickle Cell Unit, SERHA – South East Regional Health Authority
Testing
With an annual birth cohort of 40 000–45 000 babies/year, testing for SCD using Hb electrophoresis is not practical. A key element to the development of island-wide screening is acquiring the technology which will allow for high-volume processing. A collaborative effort between the Governments of Brazil and Jamaica will in the near future see Jamaica receiving technical assistance in the form of an HPLC machine, as well as training of technicians and other health professionals. In the interim, an alternate, more economical complementary method – capillary electrophoresis, may need to be employed.
Comprehensive care clinics
Although sickle cell trait occurs in one in every 10 persons in Jamaica, another 5% have other genes which put them at risk of having a child with SCD. And with one in every 170 persons having a form of SCD in Jamaica, studies have shown that without newborn screening, only approximately 25% of patients not diagnosed at birth will be diagnosed by symptoms by age two years, despite the fact that approximately 61% of patients are symptomatic by that age (14). Symptoms such as mild pains are too often ignored by parents or misdiagnosed by healthcare professionals. Additionally, a clinic-based study in Jamaica showed that approximately 65% of children with Hb SS disease not diagnosed at birth will not benefit from important early-life interventions and remain at risk for high morbidity and mortality in the early childhood period (15).
Too often, SCD is seen as a disease managed by "the experts". Unlike most countries, where patients with SCD are managed by haematologists, the SCU is primarily staffed by family practitioners, paediatricians and internists who provide high level, appropriate care. Patients are often referred to the SCU for health maintenance, a distance from home. This causes undue stress and additional expenses for patients and caregivers. Establishment of sickle cell clinics within existing paediatric or internal medicine clinics at major hospitals in the regional health authorities will be critical to the process of island-wide screening and management. Decentralization of care will provide health maintenance for patients much closer to home.
To assist local healthcare professionals in the health maintenance of persons with SCD and to ensure standardization of care informed by best care practice, taking into account resource limitations, local guidelines – "Sickle Cell Disease: The Clinical Care Guidelines of the Sickle Cell Unit" – have been developed (16). These guidelines are a practical guide to effective and comprehensive care of patients with SCD. They provide step-by-step guidance from diagnoses and counselling through to management of complications in both outpatient and inpatient facilities. The SCU will provide a consultative service to assist with complicated patients at regional clinics or in hospitals.
CONCLUSION
Although a developing country, Jamaica has made significant strides in the management of patients with sickle cell disease, resulting in increased survival of persons living with the disease. Our model of care, wherein management of persons living with SCD is not under the purview of haematologists but of paediatricians, internists and family practitioners, is an effective one that can be utilized by other resource-limited countries where haematologists are rare. Our strength as a unit delicately balancing limited resources and improved survival cannot be disparaged. We will continue efforts toward the goal of island-wide newborn screening for SCD in order to ensure continued improvements in morbidity, mortality and quality of life. Furthermore, our progress will provide guidance for other resource constrained economies, allowing for South-South collaborations to improve the care of persons living with SCD regionally and internationally.
REFERENCES
- 1.Serjeant GR, Serjeant BE, Forbes M, Hayes RJ, Higgs DR, Lehmann H. Haemoglobin gene frequencies in the Jamaican population: a study in 100,000 newborns. Br J Haematol. 1986;64:253–262. doi: 10.1111/j.1365-2141.1986.tb04117.x. [DOI] [PubMed] [Google Scholar]
- 2.Serjeant GR, Serjeant BE. Management of sickle cell disease; lessons from the Jamaican Cohort Study. Blood Rev. 1993;7:137–145. doi: 10.1016/0268-960x(93)90001-k. [DOI] [PubMed] [Google Scholar]
- 3.King L, Fraser R, Forbes M, Grindley M, Ali S, Reid M. Newborn sickle cell disease screening: the Jamaican experience (1995–2006) J Med Screen. 2007;14:117–122. doi: 10.1258/096914107782066185. [DOI] [PubMed] [Google Scholar]
- 4.Hanchard NA, Hambleton I, Harding RM, McKenzie CA. The frequency of the sickle allele in Jamaica has not declined over the last 22 years. Br J Haematol. 2005;130:939–942. doi: 10.1111/j.1365-2141.2005.05704.x. [DOI] [PubMed] [Google Scholar]
- 5.Gaston MH, Verter JI, Woods G, Pegelow C, Kelleher J, Presbury G, et al. Prophylaxis with oral penicillin in children with sickle cell anemia. A randomized trial. New Eng J Med. 1986;314:1593–1599. doi: 10.1056/NEJM198606193142501. [DOI] [PubMed] [Google Scholar]
- 6.King L, Ali S, Knight-Madden J, MooSang M, Reid M. Compliance with intramuscular penicillin prophylaxis in children with sickle cell disease in Jamaica. West Indian Med J. 2011;60:177–180. [PubMed] [Google Scholar]
- 7.Knight-Madden J, Serjeant GR. Invasive pneumococcal disease in homozygous sickle cell disease: Jamaican experience 1973–1997. J Pediatr. 2001;138:65–70. doi: 10.1067/mpd.2001.109709. [DOI] [PubMed] [Google Scholar]
- 8.Hardie R, King L, Fraser R, Reid M. Prevalence of pneumococcal polysaccharide vaccine administration and incidence of invasive pneumococcal disease in children in Jamaica aged over 4 years with sickle cell disease diagnosed by newborn screening. Ann Trop Paediatr. 2009;29:197–202. doi: 10.1179/027249309X12467994693851. [DOI] [PubMed] [Google Scholar]
- 9.Serjeant G. Can we prevent sickle cell disease? The Manchester Project. The Gleaner. 2011 Jan 16; In Focus. [Google Scholar]
- 10.Wilson N. The Manchester Project – screening for sickle cell, one baby at a time. Jamaica Observer. 2013 Feb 11; News. [Google Scholar]
- 11.Serjeant BE, Forbes M, Williams LL, Serjeant GR. Screening cord bloods for detection of sickle cell disease in Jamaica. Clin Chem. 1974;20:666–669. [PubMed] [Google Scholar]
- 12.Emond AM, Collis R, Darvill D, Higgs DR, Maude GH, Serjeant GR. Acute splenic sequestration in homozygous sickle cell disease: natural history and management. J Pediatr. 1985;107:201–206. doi: 10.1016/s0022-3476(85)80125-6. [DOI] [PubMed] [Google Scholar]
- 13.UN General Assembly . Recognition of sickle cell anaemia as a public health problem. A/RES/63/237. Washington, DC: United Nations; 2008. [Google Scholar]
- 14.Singhal A, David S, Serjeant G. Perinatal problems of islands in relation to the prevention of handicaps: Editions. In: Berchel CP, De Caunes F, editors. Delayed diagnosis of sickle cell disease in Jamaica. Guadeloupe: INSERM; 1992. pp. 268–275. [Google Scholar]
- 15.Hambleton IR, Wierenga KJ. Identifying homozygous sickle cell disease when neonatal screening is not available: a clinic-based observational study. J Med Screen. 2004;11:175–179. doi: 10.1258/0969141042467331. [DOI] [PubMed] [Google Scholar]
- 16.Asnani M, Bhatt K, Bortolusso Ali S, Cumming V, King L, Knight-Madden J, et al. In: Sickle cell disease: the clinical care guidelines of the Sickle Cell Unit. Bortolusso Ali S, editor. Kingston: Tropical Metabolism Research Institute, The University of the West Indies; 2008. [Google Scholar]