Abstract
Background
The NHS Choices website (www.nhs.uk) provides data on the opening hours of general practices in England. If the data are accurate, they could be used to examine the benefits of extended hours.
Aim
To determine whether online data on the opening times of general practices in England are accurate regarding the number of hours in which GPs provide face-to-face consultations.
Design and setting
Cross-sectional comparison of data from NHS Choices and telephone survey data reported by general practice staff, for a nationally representative sample of 320 general practices (December 2013 to September 2014).
Method
GP face-to-face consultation times were collected by telephone for each sampled practice for each day of the week. NHS Choices data on surgery times were available online. Analysis was based on differences in the number of surgery hours (accounting for breaks) and the times of the first and last consultations of the day only between the two data sources.
Results
The NHS Choices data recorded 8.8 more hours per week than the survey data on average (40.1 versus 31.2; 95% confidence interval [CI] = 7.4 to 10.3). This was largely accounted for by differences in the recording of breaks between sessions. The data were more similar when only the first and last consultation times were considered (mean difference = 1.6 hours; 95% CI = 0.9 to 2.3).
Conclusion
NHS Choices data do not accurately measure the number of hours in which GPs provide face-to-face consultations. They better record the hours between the first and last consultations of the day.
Keywords: access to health care, consumer health information, England, family practice, general practice, primary health care
INTRODUCTION
The opening hours of general practices in England are the focus of considerable debate.1 The UK Prime Minister has pledged that everyone will be able to see a GP from 8 am to 8 pm, 7 days a week, by 2020.2 This would extend the aims of a pilot funding scheme — the Prime Minister’s Challenge Fund — first announced in October 2013.3 Another initiative is the Extended Hours Access Scheme which has paid general practices for providing consultations outside of the core hours specified in their contracts; revisions to the scheme in 2014–2015 allow practices more flexibility in how these additional consultations are provided (for example, through group working or federations).4 Despite the policy interest in extended opening hours, little research has examined the effects of such interventions. This may be partly because there are no validated sources of opening hours data for all general practices in England.
NHS Choices (www.nhs.uk) is an online source of information on health and social care nationally, including primary care services. It claims to be the ‘largest online health resource in Europe’, with 45 million website visits per month, of which 1.5 million relate to finding and comparing general practices.5,6 NHS Choices reports that more than 90% of general practices regularly update their profiles.6 Practices are able to submit data on their opening hours online, via a dedicated log-in, without any formal verification or an obligation to ensure they are kept accurate. Commissioners are supposedly made aware of any changes to practice profiles on a regular basis.6 Although primarily an information source for patients, the opening hours data also have been used by, for example, the NHS 111 non-emergency telephone service when advising patients where to seek help. They could be used also in empirical research if they are sufficiently accurate.
In 2009, the media reported inconsistencies between NHS Choices data on opening hours and data collected by telephone for 200 practices across most (111 of 152) primary care trusts.7 No data were provided, however, and the sample may not have been nationally representative. These findings came despite a nationwide review of each practice’s opening hours as recorded on NHS Choices starting in 2008.8
The present study aimed at determining whether NHS Choices supplies accurate data on the number of hours in which GPs provide face-to-face consultations, for each general practice in England.
METHOD
Study design and population
A cross-sectional comparison of data on the opening hours of general practices in England was conducted, using two sources: the NHS Choices website (www.nhs.uk) and telephone survey data reported by practice staff. The study period was December 2013 to September 2014.
How this fits in
The NHS Choices website (www.nhs.uk) provides data on the opening hours of general practices in England, listed as surgery or reception times. The accuracy of these data is unknown, but they could be used in research if sufficiently accurate. This study found that NHS Choices data on surgery hours systematically recorded a greater number of hours than did telephone survey data on GP face-to-face consultation hours. NHS Choices should review its opening hours data to improve accuracy.
The general practices included in the study were sampled from a national list of 8011 practices, each of which was present in the Health and Social Care Information Centre’s general practice population dataset for October 2013 and had at least 500 registered patients.9 An algorithm was used to sample 320 practices (4.0% of national population),10 whereby 90% of sampled practices were drawn randomly and the remainder were then automatically selected to minimise differences between the sample and population on several variables (population size, deprivation, GP supply, contract type, and rurality and region of location;Appendix 1). The sample size allowed for a Pearson’s correlation of 0.2 between weekly hours as recorded in the two datasets to be detected, with a 5% significance level and power of 95%.
Telephone survey and NHS Choices data
Each general practice in the sample was telephoned and the caller asked at what times patients routinely were able to see a GP on each day of a common week. The caller most often spoke with a receptionist. The caller did not have access to the NHS Choices data at the time of making the phone call or when recording responses. If a call was not answered on the first attempt, or the practice declined to provide the information, a maximum of a further two attempts were made. The caller revealed the purpose of the call or their identity to the practice staff where necessary, in which case the caller referred to the research study. Prompts were made for breaks in surgery hours during the day. The reported times were recorded in an electronic spreadsheet in a standardised format, dividing days into one or more periods of consulting (separated by breaks) where appropriate.
Data were collected on GP face-to-face consulting times only. Times during which only the reception was open, only telephone triage was operating, or only nurses were seeing patients, but no GP clinics were running, were not collected. These times were excluded for four main reasons: national policy rhetoric on extended opening hours focuses primarily on seeing a GP;2 previous research suggests that being able to see a GP specifically is associated with use of other services;11 most patients (75%) report wanting a GP face-to-face consultation on their last appointment attempt;12 and the timings and content of telephone consultation or triage periods were thought unlikely to be well defined. The analysis was repeated, however, based on timings of the first and last GP face-to-face consultations of the day only (ignoring breaks), and these hours are likely to include several other activities.
If GPs had staggered clinic times (beginning and ending at different times), the earliest start time and latest finish time were recorded, to reflect overall practice surgery hours. If a practice changed its hours on a given day in alternate weeks, an ‘averaged’ start and end time were recorded (equivalent number of hours over 2 weeks).
The ‘GP opening times’ dataset was downloaded from the NHS Choices website at regular intervals to coincide with collection of the telephone survey data.13 This dataset contains both ‘surgery opening times’ and ‘reception opening times’ as entered online for each general practice’s profile; administrators are asked to provide up to three sets of times for each day for each opening time type.6 The surgery times (rather than reception times) were analysed, which NHS Choices advised were intended to be those at which a patient can visit a GP. No definitions are provided to administrators when entering data, however, and practices may interpret these times differently. The survey data obtained for a given practice were compared with NHS Choices data collected within 2 weeks of the survey data for that practice. Reference is made to the data recorded by NHS Choices and in the telephone survey using the terms ‘surgery times’ and ‘surgery hours’ for the remainder of this article.
Statistical methods
Differences were calculated in the number of surgery hours per week within practices between the survey data and the NHS Choices data. Paired t-tests were used to test the hypothesis that the mean difference was significantly different from zero, for each day of the week and for the week overall. Scatter diagrams were plotted of the number of surgery hours provided by each general practice according to the two data sources, and the difference in the values for each practice against the average of the survey and NHS Choices data values.14 For each relationship, the Pearson’s correlation coefficient was calculated (using Fisher’s transformation to compute 95% confidence intervals [CIs]). The same methods were used in the analysis based solely on the first and last consultations of the day (ignoring breaks) as in the initial analysis deducting breaks from surgery hours. Practices with missing NHS Choices or telephone survey data were excluded. All data processing and analysis were conducted using Stata (version 13.1).
RESULTS
From the initial sample of 320 general practices, two were not listed on NHS Choices, 23 did not provide surgery times on NHS Choices, and telephone survey data were not collected for a further 27 practices. The analysis therefore included 268 practices (84% of the initial sample). Those excluded were similar to the included practices in terms of numbers of registered patients, population deprivation, GP supply, practice contract type, and the rurality and region of practice location (Appendix 2).
In the telephone survey data, the mean number of GP surgery hours per week was 31.2 (standard deviation [SD] 9.4; range 4–84). The mean number of surgery hours outside of core opening times (8 am to 6.30 pm, Monday to Friday)15 was 1.6 hours (SD 3.2). Around 6 in 10 practices (61.9%) provided GP face-to-face appointments outside of core times. Around 2 in 10 (16.8%) provided such appointments at the weekend. Among practices open outside of core times, the mean number of non-core hours was 2.6 (SD 3.8; morning 0.3 hours; evening 1.4 hours; weekend 0.9 hours). Weekday consultations commonly started at or before 9 am (90% of weekdays when practices were open; 61% at or before 8.30 am; 8 am, 18%) and typically finished at or before 7 pm (89%; 6 pm, 69%; 5 pm, 15%).
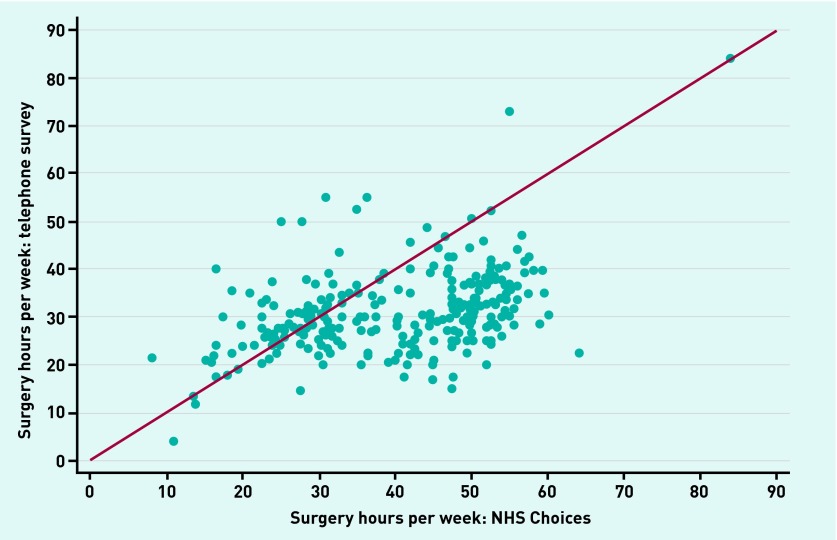
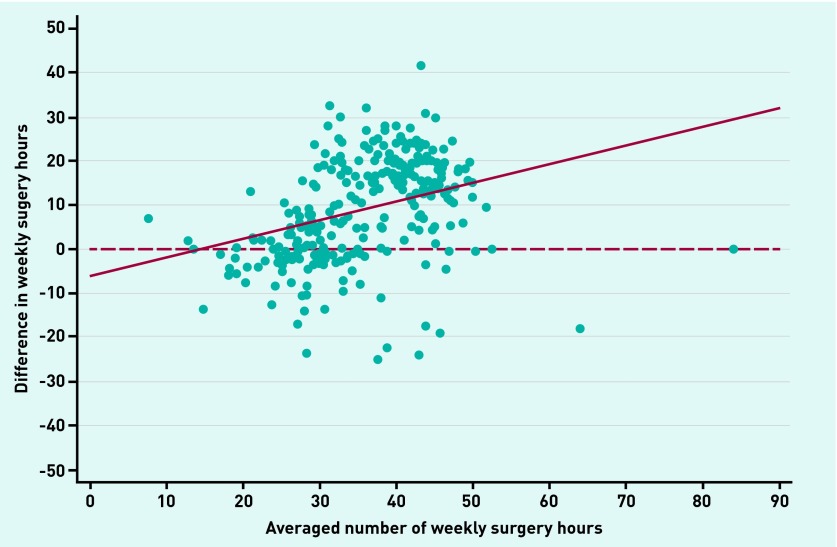
The NHS Choices data recorded 8.8 more surgery hours per week (40.1 versus 31.2; 95% CI = 7.4 to 10.3; relative difference = 1.28) than the survey data on average (Table 1). This tendency was observed across all days of the week except Sundays (P<0.001 for Monday to Friday;P<0.01 for Saturday;P = 0.66 for Sunday). The number of surgery hours calculated from the two data sources were moderately correlated (r = 0.46; 95% CI = 0.36 to 0.55) (Figure 1). The difference in this figure between the datasets was moderately correlated with the average of the values recorded in the two datasets (r = 0.34; 95% CI = 0.23 to 0.44) (Figure 2), with greater differences associated with greater average numbers of surgery hours.
Table 1.
Distributions of daily and weekly surgery hours of general practices, by data source
| NHS Choices data | Telephone data | Mean difference | P-valuea | |||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Mean | SD | Mean | SD | |||
| Overall | 40.1 | 12.8 | 31.2 | 9.4 | 8.8b | <0.001 |
| Monday | 8.3 | 2.5 | 6.3 | 1.7 | 1.9 | <0.001 |
| Tuesday | 8.1 | 2.4 | 6.3 | 1.7 | 1.8 | <0.001 |
| Wednesday | 7.5 | 2.8 | 6.0 | 1.9 | 1.5 | <0.001 |
| Thursday | 7.6 | 2.9 | 6.0 | 2.0 | 1.6 | <0.001 |
| Friday | 7.8 | 2.4 | 6.1 | 1.7 | 1.8 | <0.001 |
| Saturday | 0.7 | 1.6 | 0.5 | 1.4 | 0.2 | <0.01 |
| Sunday | 0.1 | 1.1 | 0.1 | 1.1 | 0.02 | 0.66 |
SD = standard deviation.
The reported P-values are those from a paired t-test of the equality of means.
Standard deviation of the differences was 11.9.
Figure 1.
Agreement in the weekly number of surgery hours of general practices between NHS Choices and telephone survey data. Number of practices = 268. Pearson correlation coefficient, r= 0.46 (95% CI = 0.36 to 0.55). Line represents perfect agreement between data sources.
Figure 2.
Relationship between the averaged number of weekly surgery hours recorded in the telephone survey and NHS Choices data, and the difference between the datasets. Number of practices = 268. Difference in weekly surgery hours = number of hours in NHS Choices data – number of hours in telephone survey data. Pearson correlation coefficient, r = 0.34 (95% CI = 0.23 to 0.44). Solid line represents the predictions from a linear regression of the difference in the number of surgery hours on the averaged number of surgery hours. Dashed line represents perfect agreement between data sources.
The surgery hours in the survey data divided into a greater number of periods per day (accounting for breaks in surgery hours) than in the NHS Choices data (mean number of surgery hours periods per day: 1.5 versus 1.2; 95% CI = 0.25 to 0.31). The recording of more breaks in surgery hours in the survey data may help to explain the lower number of surgery hours recorded.
When only the start and end times of surgery hours were considered in the analysis (ignoring breaks during the day), the two datasets were more comparable. Whereas the NHS Choices data still recorded a slightly greater mean number of surgery hours (48.2 versus 46.7; P<0.001), the mean difference was smaller (1.6; 95% CI = 0.9 to 2.3) and the correlation was stronger (r = 0.65; 95% CI = 0.57 to 0.71). A weak correlation was observed between the difference in the number of surgery hours and the average over datasets (r = 0.13; 95% CI = 0.01 to 0.25).
DISCUSSION
Summary
In the telephone survey data, the mean number of GP surgery hours per week was 31.2 hours. NHS Choices data recorded 8.8 (28%) more surgery hours per week than the telephone survey data on average (40.1 versus 31.2). This difference was generally greater for general practices with longer surgery hours. When only the start and end times of surgery hours were considered, the mean difference reduced to 1.6 surgery hours (48.2 versus 46.7).
Strengths and limitations
A nationally representative sample of general practices was used to examine a policy-relevant, routinely available data source on surgery hours. This article is the first to present telephone survey data for GP face-to-face consulting hours in a large sample in England.
One limitation is that the telephone survey data were limited to GP face-to-face appointment times, thereby excluding times for telephone and nurse consultations, for example. Times for face-to-face urgent consultations with a GP also may often be included in NHS Choices data but may not have been captured in the survey data. If the NHS Choices data do include other forms of appointment in the recorded surgery hours, this could help explain the discrepancy between the two data sources. This discrepancy remained, albeit smaller, in the sensitivity analysis using the times of the first and last consultations of the day only. However, NHS Choices advised that the surgery times are intended to be those when a patient can actually visit a GP and these times were the primary interest because of their relevance to policy and future research.
Response bias could be present in the survey data, possibly because staff wanted to give a good impression of the practice, staff were busy and could not provide more detail, or staff were unsure of what information they were allowed to provide. The direction or extent of this bias is unknown, but it is perhaps unlikely to be large enough to account for all of the difference in weekly surgery hours between the two data sources. Attempts could have been made to phone each practice more than once to assess response reliability (different staff may respond differently, for example), at the expense of time taken to do so. It was felt reasonable to assume that responses would not differ greatly within the same practice, but if this is untrue agreement between the two data sources is also likely to be poor, thereby partly accounting for some of the observations.
No records were made of each practice’s surgery hours at several points in time to assess longitudinal changes in both NHS Choices and survey data. If there is little measurement error in the changes in surgery hours through time (irrespective of the cross-sectional error), the NHS Choices data may be suitable for use in certain panel data analyses. This is perhaps unlikely to be the case, however, given the large cross-sectional error reported.
Comparison with existing literature
Previously, the median number of surgery hours per week recorded in NHS Choices data have been reported for the national practice population (40 hours; 8973 practices),16 which is consistent with the sample estimate here. Similar data had been analysed for a sample of 639 practices from 13 primary care trusts before this,17 but these data were not compared with telephone survey data.
Most general practices are contracted to provide essential services within core hours, equivalent to 52.5 hours per week, under the general medical services contract.15 These services must be in place ‘throughout the core hours in case of emergency’.15 When only the start time of the first consultation and end time of the last consultation each day were analysed, the mean weekly surgery hours in the NHS Choices data was 48.2. It is plausible therefore that emergency consultations often occur outside (either before or after) the surgery hours listed on NHS Choices, and reported in the telephone survey.
In the 2012 cross-section of the GP Worklife Survey (n = 1112), GPs reported an average of 41.7 hours of work per week and 26.0 hours of direct patient care per week.18 These figures are comparable with the surgery hours, including breaks, recorded on NHS Choices (40.1 hours) and in the survey data (31.2 hours), respectively. This suggests that NHS Choices data may more closely record routine working hours rather than consulting hours, although it is noted that GPs often work in excess of 40 hours a week. The difference between the direct patient care hours reported in the GP Worklife Survey and the surgery hours in the survey data (26.0 versus 31.2 hours) could be explained by clinical sessions not always running in parallel.
Satisfaction with general practice opening hours is generally high: in the 2013–14 General Practice Patient Survey (n = 903 357), 79.9% of responders felt their practice was open at convenient times.1 Of those who did not, after 6.30 pm and on Saturdays were the most desired additional opening times (71% and 74% of responders, respectively).1
Implications for research and practice
The precise detail of the government’s pledge to ensure everyone in England will be able to see a GP from 8 am to 8 pm, 7 days a week, by 2020 remains unclear. If the long-term goal is for each practice to offer GP consultations between these times (84 hours per week), this represents an exceptional change to general practice when compared with the survey data (for example, currently no weekend GP face-to-face appointments in 83.2% of practices).16
However, such a change is unrealistic in the short term and practices are more likely to offer extended opening hours working in groups, as commonly done in the pilot schemes of the Challenge Fund.19 The government should note, however, that changes in opening hours do not represent a holistic approach to improving access to primary care.
NHS Choices should review its general practice opening hours data. A survey of NHS Choices users suggests that these data are the most valued when choosing a new practice.20 This study makes three recommendations in particular. First, each set of opening times should have a standardised definition that can be seen by patients online and can inform general practices what times to include when entering data. Second, separate times should be entered for each of the following where appropriate: GP face-to-face appointments; GP telephone appointments; nurse appointments; and reception opening. Arguably, it would be more difficult to specifically list emergency appointments, which may be equivalent to book-on-day, walk-in, or ‘extra’ slots in some cases, or may even be seen out of consulting times, if a genuine clinical emergency. The consulting hours of individual GPs or the number of clinics running within each session would provide additional valuable information for patients. Third, data submitted online should be formally verified, possibly using a ‘mystery shopper’ approach21 or by contacting practices as was done in this study. Also, this may help ensure that the data remain up-to-date. NHS Choices does not currently supply data that accurately measure the number of hours in which GPs provide face-to-face consultations. It is unclear who is ultimately accountable for this; NHS Choices states in its terms and conditions that it does not accept liability for content provided by third parties.22
The government has announced that NHS Choices is intended to become the single point of access for all digital healthcare transactions in England, including registration with a general practice and the new online booking of general practice appointments.23 It is fundamental that the data required to support these new functionalities, including on opening hours, are accurate.
Appendix 1. Representativeness of general practices in study sample
| Variable | Sample (n= 320) | National population (n= 8011) | Difference |
|---|---|---|---|
| Continuous variables (means presented) | |||
| Number of registered patients | 7000.8 | 7075.6 | −74.7 |
| Number of GP FTEs | 4.4 | 4.4 | −0.1 |
| Number of GP FTEs per 1000 patients | 0.6 | 0.6 | 0.0 |
| IMD score | 23.8 | 23.8 | −0.1 |
| Categorical variables (percentages presented) | |||
| General Medical Services contract | 55.6 | 55.4 | 0.2 |
| Urban location | 84.4 | 84.5 | −0.2 |
| Region of England | |||
| North | 30.3 | 30.2 | 0.1 |
| Midlands and East | 29.4 | 29.4 | 0.0 |
| London | 18.1 | 18.1 | 0.0 |
| South | 22.2 | 22.3 | −0.1 |
Data for each variable were obtained from the Health and Social Care Information Centre (hscic.gov.uk; indicators. ic.nhs.uk). FTE = full-time equivalent. IMD = Index of Multiple Deprivation.
Appendix 2. Comparison of included and excluded practices from initial sample
| Variable | Included (n= 268) | Excluded (n= 52) | Difference | P-valuea |
|---|---|---|---|---|
| Continuous variables (means presented) | ||||
| Number of registered patients | 7062.0 | 6685.8 | 376.2 | 0.55 |
| Number of GP FTEs | 4.5 | 3.7 | 0.9 | 0.07 |
| Number of GP FTEs per 1000 patients | 0.6 | 0.6 | 0.1 | 0.14 |
| IMD score | 23.2 | 26.7 | −3.5 | 0.07 |
| Categorical variables (percentages presented) | ||||
| General Medical Services contract | 55.2 | 57.7 | −2.5 | 0.74 |
| Urban location | 84.0 | 86.5 | −2.6 | 0.64 |
| Region of England | 0.26 | |||
| North | 30.6 | 28.9 | 1.8 | |
| Midlands and East | 27.2 | 40.4 | −13.1 | |
| London | 19.0 | 13.5 | 5.6 | |
| South | 23.1 | 17.3 | 5.8 |
Data for each variable were obtained from the Health and Social Care Information Centre (hscic.gov.uk; indicators. ic.nhs.uk).
P-values are from a t-test for equality of means (continuous variables) or a χ2 test (discrete variables). FTE = full-time equivalent. IMD = Index of Multiple Deprivation.
Funding
This report is independent research funded by the National Institute for Health Research (NIHR) (Doctoral Research Fellowship, Mr Thomas Cowling, DRF-2013-06-142). The views expressed in this publication are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health. The Department of Primary Care and Public Health at Imperial College London is grateful for support from the Northwest London NIHR Collaboration for Leadership in Applied Health Research and Care (CLAHRC), the Imperial NIHR Biomedical Research Centre (BRC), and the Imperial Centre for Patient Safety and Service Quality (CPSSQ). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Ethical approval
Not applicable.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article:bjgp.org/letters
REFERENCES
- 1.Cowling TE, Harris MJ, Majeed A. Evidence and rhetoric about access to UK primary care. BMJ. 2015;350:h1513. doi: 10.1136/bmj.h1513. [DOI] [PubMed] [Google Scholar]
- 2.Iacobucci G. Cameron reiterates promise of seven day access to GPs. BMJ. 2014;349:g5960. doi: 10.1136/bmj.g5960. [DOI] [PubMed] [Google Scholar]
- 3.Department of Health Seven day, 8am–8pm, GP access for hard working people. 2013. https://www.gov.uk/government/news/seven-day-8am-8pm-gp-access-for-hard-working-people?utm_source=rss&utm_medium=rss&utm_campaign=press-release-seven-day-8am-8pm-gp-access-for-hard-working-people (accessed 16 Oct 2015).
- 4.NHS Employers . General medical services contract 2014/15: guidance and audit requirements. Leeds: NHS Employers; 2014. http://www.nhsemployers.org/∼/media/Employers/Documents/Primary%20care%20contracts/GMS/GMS%20guidance%202010-present/2014-15/201415%20GMS%20Guidance.pdf (accessed 16 Oct 2015). [Google Scholar]
- 5.NHS England . Annual report and accounts 2014–15. Leeds: NHS England; 2015. http://www.england.nhs.uk/wp-content/uploads/2015/07/nhse-annual-report-2014-15.pdf (accessed 16 Oct 2015). [Google Scholar]
- 6.NHS Choices GP practice profiles. 2014 http://www.nhs.uk/aboutNHSChoices/professionals/healthandcareprofessionals/your-pages/Pages/GPpracticeprofiles.aspx (accessed 16 Oct 2015). [Google Scholar]
- 7.Nowottny S. NHS ‘guidebook to GPs’ website riddled with errors. Pulse. 2009. Mar 10, http://www.pulsetoday.co.uk/nhs-guidebook-to-gps-website-riddled-with-errors/10999968.article#.VVNvcSh0wdU (accessed 16 Oct 2015).
- 8.Ashby G. GP data on NHS Choices. 2008 http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_091160.pdf (accessed 16 Oct 2015). [Google Scholar]
- 9.Health and Social Care Information Centre Numbers of patients registered at a GP practice — October 2013. 2013. http://www.hscic.gov.uk/searchcatalogue?productid=12549&topics=0%2fPrimary+care+services&sort=Relevance&size=10&page=1#top (accessed 16 Oct 2015).
- 10.Kontopantelis E. A greedy algorithm for representative sampling: repsample in Stata. J Stat Software. 2013;55:1–19. [Google Scholar]
- 11.Cowling TE, Cecil EV, Soljak MA, et al. Access to primary care and visits to emergency departments in England: a cross-sectional, population-based study. PLoS One. 2013;8(6):e66699. doi: 10.1371/journal.pone.0066699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ipsos MORI GP Patient Survey — surveys and reports. 2015 https://gp-patient.co.uk/surveys-and-reports (accessed 16 Oct 2015). [Google Scholar]
- 13.NHS Choices Freedom of information. 2015 http://www.nhs.uk/aboutNHSChoices/contactus/Pages/freedom-of-information.aspx (accessed 16 Oct 2015). [Google Scholar]
- 14.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–310. [PubMed] [Google Scholar]
- 15.Department of Health . Standard general medical services contract. London: DH; 2013. https://www.gov.uk/government/publications/standard-general-medical-services-contract (accessed 16 Oct 2015). [Google Scholar]
- 16.Cowling TE, Harris MJ, Soljak MA, et al. Opening hours of general practices in England. BMJ. 2013;347:f7570. doi: 10.1136/bmj.f7570. [DOI] [PubMed] [Google Scholar]
- 17.Morgan CL, Beerstecher HJ. Satisfaction, demand, and opening hours in primary care: an observational study. Br J Gen Pract. 2011 doi: 10.3399/bjgp11X588475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hann M, McDonald J, Checkland K, et al. Seventh National GP Worklife Survey. Manchester: University of Manchester; 2013. http://www.population-health.manchester.ac.uk/healtheconomics/research/reports/FinalReportofthe7thNationalGPWorklifeSurvey.pdf (accessed 16 Oct 2015). [Google Scholar]
- 19.NHS England Prime Minister’s Challenge Fund. 2014. http://www.england.nhs.uk/ourwork/qual-clin-lead/calltoaction/pm-ext-access/#wave2 (accessed 16 Oct 2015).
- 20.NHS Choices Choosing a GP & NHS Choices data. 2012. http://www.slideshare.net/NHSChoices/choosing-a-gp-and-nhs-choices-data (accessed 16 Oct 2015).
- 21.Campbell JL, Carter M, Davey A, et al. Accessing primary care: a simulated patient study. Br J Gen Pract. 2013 doi: 10.3399/bjgp13X664216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.NHS Choices Terms and conditions. 2015. http://www.nhs.uk/aboutNHSChoices/aboutnhschoices/termsandconditions/Pages/termsandconditions.aspx (accessed 16 Oct 2015).
- 23.Department of Health . Personalised health and care 2020: a framework for action. London: DH; 2014. https://www.gov.uk/government/publications/personalised-health-and-care-2020 (accessed 16 Oct 2015). [Google Scholar]