Abstract
Effective therapeutic agents are lacking for the prevention and reversal of vascular leak, a frequent pathophysiologic result of inflammatory processes such as acute respiratory distress syndrome (ARDS) and sepsis. We previously demonstrated the potent barrier-enhancing effects of related compounds sphingosine 1-phosphate (S1P), the pharmaceutical agent FTY720, and its analog (S)-FTY720 phosphonate (Tys) in models of inflammatory lung injury. In this study, we characterize additional novel FTY720 analogs for their potential to reduce vascular leak as well as utilize them as tools to better understand the mechanisms by which this class of agents modulates permeability. Transendothelial resistance (TER) and labeled dextran studies demonstrate that (R)-Methoxy-FTY720 ((R)-OMe-FTY), (R)/(S)-Fluoro-FTY720 (FTY-F), and β-Glucuronide-FTY720 (FTY-G) compounds display in vitro barrier-enhancing properties comparable or superior to FTY720 and S1P. In contrast, the (S)-Methoxy-FTY720 ((S)-OMe-FTY) analog disrupts lung endothelial cell (EC) barrier integrity in TER studies in association with actin stress fiber formation and robust intracellular calcium release, but independent of myosin light chain or ERK phosphorylation. Additional mechanistic studies with (R)-OMe-FTY, FTY-F, and FTY-G suggest that lung EC barrier enhancement is mediated through lipid raft signaling, Gi-linked receptor coupling to downstream tyrosine phosphorylation events, and S1PR1-dependent receptor ligation. These results provide important mechanistic insights into modulation of pulmonary vascular barrier function by FTY720-related compounds and highlight common signaling events that may assist the development of novel therapeutic tools in the prevention or reversal of the pulmonary vascular leak that characterizes ARDS.
Keywords: FTY720, sphingosine 1-phosphate, G protein-couple receptors, endothelial barrier regulation, acute respiratory distress syndrome
1. Introduction
Modulation of pulmonary vascular barrier function is an important clinical goal given the devastating effects of sustained vascular barrier leak on morbidity and mortality in acute inflammatory diseases, such as acute respiratory distress syndrome (ARDS) and sepsis. Within the lung, disruption of the pulmonary vascular endothelial cell (EC) monolayer results in flooding of interstitial and alveolar compartments with fluid, protein, and inflammatory cells and leads to respiratory failure (Dudek and Garcia, 2001). Specific therapies that prevent or reverse inflammation-mediated vascular barrier leak are lacking (Wheeler and Bernard, 2007). We previously demonstrated the potent barrier-enhancing properties of the endogenous phospholipid sphingosine 1-phosphate (S1P), the related pharmaceutical agent FTY720, and several novel synthetic analogs of FTY720 including (S)-FTY720-phosphonate (Tys) (Camp et al., 2009; Dudek et al., 2007; Garcia et al., 2001; Wang et al., 2014). S1P, a sphingolipid produced by multiple cell types, initiates a series of downstream effects through the ligation of the Gi-coupled S1P1 receptor (S1PR1), culminating in enhancement of the EC cortical actin ring, improved cell-cell and cell-matrix interactions, and increased barrier function in vitro (Dudek et al., 2004; Garcia et al., 2001; Shikata et al., 2003). The pharmaceutical agent FTY720, a structural analog of S1P, potently enhances lung EC barrier function via Gi-coupled receptor signaling (Dudek et al., 2007; Wang et al., 2011). Phosphonate and enephosphonate analogs of FTY720, such as Tys, demonstrate similar but not identical barrier enhancing properties to S1P and FTY720 (Camp et al., 2009). Oxazolo-oxazole derivatives of FTY720 reduce EC permeability induced by LPS or TNFα in vitro (Imeri et al., 2014). Moreover, S1P, FTY720, and Tys attenuate lipopolysaccharide (LPS)-induced lung injury in vivo (Camp et al., 2009; McVerry et al., 2004; Peng et al., 2004). Thus, S1P, FTY720, and analogs such as Tys, represent a class of agents that are potential therapeutic options for inflammatory lung disease.
However, both S1P and FTY720 exhibit certain characteristics that suggest limited therapeutic utility in acutely ill patients with ARDS. S1P has a relatively limited therapeutic window as higher concentrations (>5 μM) increase lung EC monolayer permeability in vitro (Camp et al., 2009), while intratracheal administration produces pulmonary edema in vivo through disruption of the epithelial barrier via ligation of S1PR3 (Gon et al., 2005). S1P also produces cardiac toxicity through activation of S1PR3 in the heart (Forrest et al., 2004; Hale et al., 2004a) as well as contraction of human airway smooth muscle cells (Rosenfeldt et al., 2003) and increased airway hyper-responsiveness in mice (Roviezzo et al., 2007). While FTY720 is an FDA-approved therapy for multiple sclerosis based upon its effectiveness as an immunosuppressant through down-regulation of S1PR1 signaling (Kappos et al., 2006; Pelletier and Hafler, 2012), this immunosuppressive effect may be harmful in critically ill patients with sepsis or other infectious processes. In addition, multiple recent studies have demonstrated detrimental effects on vascular permeability of higher concentrations and prolonged exposure to FTY720. High concentrations of FTY720 produce tissue edema in mice (Oo et al., 2011) as well as exacerbate ventilator-induced lung injury (Muller et al., 2011) and bleomycin-induced lung injury in mice (Shea et al., 2010; Wang et al., 2014). This barrier-disrupting effect of FTY720 likely is mediated through down-regulation of EC S1PR1 expression and subsequent increased vascular leak due to loss of the barrier-promoting pathway initiated by S1PR1 ligation (Oo et al., 2011; Wang et al., 2014). We recently reported that Tys, unlike FTY720, maintains lung S1PR1 expression during prolonged exposure and thus remains protective against lung injury in the bleomycin model (Wang et al., 2014).
Given these potential therapeutic limitations of S1P and FTY720 in patients with ARDS, we are exploring the barrier-regulatory properties of additional novel analogs of FTY720 to better understand how this class of compounds regulates permeability. The current study characterizes four novel FTY720 analogs, advances our understanding of pulmonary vascular permeability, and may potentially introduce novel therapeutic tools for prevention and reversal of vascular leak.
2. Materials and Methods
2.1 Synthesis of FTY70 analogs
Four novel analogs of FTY720 ((R)-FTY-OMe or (R)-Methoxy-FTY720; (S)-FTY-OMe or (S)-Methoxy-FTY720; FTY-F or (R)/(S)-Fluoro-FTY720 (a 7:1 mixture); and FTY-G or β-Glucuronide-FTY720) were synthesized as described in Supplemental Data (also see Figure 1 for the structures of the FTY720 analogs used in this study).
Figure 1. Structures of FTY720 and novel analogs.

(A) FTY720; (B) (R)-FTY-OMe or (R)-Methoxy-FTY720; (C) (S)-FTY-OMe or (S)-Methoxy-FTY720; (D) FTY-F or (R)/(S)-Fluoro-FTY720; and (E) FTY-G or β-Glucuronide-FTY720.
2.2 Reagents
S1P was purchased from Sigma-Aldrich (St. Louis, MO), and FTY720 was generously provided by Novartis (Basel, Switzerland). SB649146 was generously provided by Glaxo Smith Kline (King of Prussia, PA). All other reagents were obtained from Sigma-Aldrich, unless otherwise noted. Immunofluorescent and Western blotting reagents were obtained as follows: rabbit anti-diphosphorylated MLC, rabbit anti-phosphorylated ERK (Cell Signaling, Beverly, MA); and mouse VE-cadherin (Santa Cruz Biotechnology, Dallas, TX). The labeled dextran vascular permeability assay kit, pertussis toxin and genistein were purchased from EMD Millipore Corporation (Billerica, MA). Fura-2/acetoxymethyl ester was obtained through Life Technologies (Grand Island, NY). JTE-013 and BML-241 were purchased from Cayman Chemicals (Ann Arbor, MI).
2.3 Cell Culture
Human pulmonary artery endothelial cells (HPAEC) were obtained from Lonza (Walkersville, MD) and were cultured as described previously (Dudek et al., 2004) in the manufacturer’s recommended endothelial growth medium-2 (EGM-2). Cells were grown at 37°C in a 5% CO2 incubator, and passages 6 to 9 were used for experiments. Media were changed one day before experimentation.
2.4 Transendothelial Monolayer Electrical Resistance
Lung EC were grown to confluence in polycarbonate wells containing evaporated gold microelectrodes, and transendothelial monolayer electrical resistance (TER) measurements were performed using an electrical cell-substrate impedance sensing system (Applied Biophysics, Troy, NY) as described previously in detail (Garcia et al., 2001). TER values from each microelectrode were pooled as discrete time points and plotted versus time as the mean ± S.E.M.
2.5 Labeled Dextran Permeability Assay
A transendothelial permeability assay was performed as previously described (Garcia et al., 1986; Wang et al., 2011) using labeled tracer flux across confluent lung EC grown on confluent polycarbonate filters (Vascular Permeability Assay Kit; Millipore Corporation). In brief, lung EC grown to confluence on transwell inserts were exposed to agonist stimulation for 1 h. After stimulation, 40 kD FITC-labeled dextran was added to the luminal compartment for 2 h, and then FITC-dextran clearance across the filter to the abluminal compartment was measured by relative fluorescence excitation at 485 nm and emission at 530 nm.
2.6 Immunofluorescence
Lung EC were grown on gelatinized coverslips before exposure to various conditions as described for individual experiments. EC were then fixed in 3.7% formaldehyde for 15 min, permeabilized with 0.25% Triton X-100 for 5 min, washed in PBS, blocked with 2% bovine serum albumin in Tris-buffered saline with Tween 20 for 1 h, and then incubated for 1 h at room temperature with the primary antibody of interest. After washing, lung EC were incubated with the appropriate secondary antibody conjugated to immunofluorescent dyes for 1 h at room temperature. After further washing with Tris-buffered saline with Tween 20, coverslips were mounted using SlowFade® Gold Antifade Reagent with DAPI (Invitrogen) and analyzed using a Nikon Eclipse TE 2000-S fluorescence microscope (60X objective lens) and MetaVue software (Universal Imaging Corp., PA).
2.7 Western Blotting
After treatment as outlined for individual experiments, lung EC were subsequently washed with cold (4° C) Ca2+/ Mg-free PBS and lysed with 0.3% SDS lysis buffer containing protease inhibitors (1 mM EDTA, 1 mM phenylmethylsulfonyl fluoride, 1 mM sodium orthovanadate, 1 mM sodium fluoride, 0.2 trypsin inhibitor unit/ml aprotinin, 10 μM leupeptin, and 5 μM pepstatin A). Sample proteins were separated with 4 to 15% SDS-PAGE gels (Bio-Rad, Hercules, CA) and transferred onto Immobilon-P polyvinylidene difluoride membranes (EMD Millipore Corporation). Membranes were then immunoblotted with primary antibodies (1: 1000, 4°C, overnight) followed by secondary antibodies conjugated to horseradish peroxidase (1:5000, room temperature, 30 min) and detected with enhanced chemiluminescence (Pierce ECL or SuperSignal West Dura; Pierce Biotechnology, Rockford, IL) on Biomax MR film (Carestream Health, Rochester, NY).
2.8 Calcium Measurements
Lung EC were grown to confluency on 9×22 mm coverslips and preloaded with 5 μM Fura-2-AM (Molecular Probes, Eugene, OR) for 15 min. Fluorescence was measured with an Aminco-Bowman Series 2 luminescence spectrometer at excitation wavelength of 340 and 380 nm and emission wavelength of 510 nm. Upon agonist challenge, intracellular calcium in nM was calculated from 340/380 ratio using calibration curves and software as previously described (Usatyuk et al., 2003). Relative intracellular calcium release compared to baseline was quantified by measuring the total area under the curve, after agonist stimulation at 100 seconds, using Photoshop densitometry readings.
3. Results
3.1 Differential Effects of FTY720 Analogs on Endothelial Barrier Function In Vitro
Four novel analogs of FTY720 were synthesized for this study: (R)-Methoxy-FTY720 or (R)-FTY-OMe; (S)-Methoxy-FTY720 or (S)-FTY-OMe; (R)/(S)-Fluoro-FTY720 (7:1 mixture) or FTY-F; β-Glucuronide-FTY720) or FTY-G (see Figure 1 and Supplemental Data). Our initial studies assessed the physiological effects of these FTY720 analogs on lung EC barrier integrity as measured by TER, a highly sensitive in vitro measure of permeability. As we have previously described (Dudek et al., 2007; Wang et al., 2011), 1 μM FTY720 induces a gradual rise in EC barrier function that peaks after 30-60 min and is sustained for several hours. At this concentration, which is optimal for FTY720-induced barrier enhancement (Dudek et al., 2007), the (R)-OMe-FTY and FTY-F analogs of FTY720 exhibit similar barrier-promoting properties as FTY720, but (S)-OMe-FTY and FTY-G have little barrier effect (Figure 2A).
Figure 2. Effects of FTY720 analogs on endothelial permeability in vitro.

HPAEC were plated on gold microelectrodes for TER measurements as described in Methods. At time = 0, parallel EC monolayers were stimulated with either FTY720 (black line), (R)-OMe-FTY (red), (S)-OMe-FTY (blue), FTY-F (green), or FTY-G (purple). The TER tracings represent pooled data (± S.E.M.) from 3-4 independent experiments after stimulation with 1 μM (A), 10 μM (B), or 50 μM (C) of each compound. Note that vehicle control-treated lung EC exhibited no substantive resistance changes over this time period. (D) HPAEC plated on transwell inserts were stimulated with FTY720, S1P, (R)-OMe-FTY, and FTY-F (each at 1 μM), or (S)-OMe-FTY and FTY-G (both 10 μM) for 1 h before addition of FITC-dextran. After a 2 h incubation, FITC-dextran clearance relative fluorescence was measured by excitation at 485 nm and emission at 530 nm. Data were normalized to unstimulated control. n = 3 independent transwell experiments per condition; *p<0.01 versus unstimulated control.
Additional TER studies demonstrate that (R)-OMe-FTY and FTY-F alter lung EC barrier function in a manner similar to FTY720 at all concentrations studied. For these three compounds, 10 μM induces a modest and transient increase in TER followed by prolonged barrier disruption (Figure 2B), while a higher concentration (50 μM) rapidly produces only increased permeability (Figure 2C). The (S)-OMe-FTY analog stimulates only lung EC barrier disruption at 10-50 μM and fails to increase TER at any concentration studied. In contrast, the FTY-G analog enhances lung EC barrier function at 10-50 μM (although only transiently at the higher concentration) with a significantly prolonged TER increase relative to the FTY720 parent compound (Figure 2B & 2C). These in vitro data suggest that one potential advantage of this FTY-G analog compared with FTY720 may be a broader therapeutic range in which the compound can promote endothelial barrier integrity. Also, the enantiomer (S)-OMe-FTY was barrier-disruptive at similar concentrations to the barrier-enhancing enantiomer (R)-OMe-FTY, despite being structurally very similar to each other (Figure 2B), indicating the sensitivity of this response to minor structural alterations as we have previously described for other FTY720 analogs (Camp et al., 2009).
We next determined the permeability of FITC-labeled dextran across the pulmonary EC monolayer as a complementary in vitro approach to further characterize the barrier protective effects of the four novel FTY720 analogs (Garcia et al., 1986; Wang et al., 2011). Whereas TER measurements are an assessment of EC permeability in terms of resistance to an electrical current, FITC-labeled dextran allows for characterization of changes in EC permeability to higher molecular weight molecules. Compared with control lung EC, those treated with FTY720, S1P, (R)-OMe-FTY, FTY-F, or FTY-G (Figure 2D) all demonstrate significantly decreased permeability in this assay, consistent with the TER data shown above (Figure 2A & 2B). Interestingly, 10 μM (S)-OMe-FTY also decreased labeled dextran permeability (Figure 2D), in apparent contrast with the TER data shown in Figure 2B. Close inspection of the 10 μM (S)-OMe-FTY TER tracing in Figure 2B reveals a transient early increase in resistance that may be reflected in the dextran permeability data in Figure 2D, which integrates total dextran flux across the monolayer over several hours. This apparent discrepancy may highlight the differential barrier properties characterized by these two in vitro assays.
3.2 FTY720 Analogs Induce Differential Cytoskeletal Rearrangement and Intracellular Signaling
S1P generates dramatic lung EC cytoskeletal rearrangements such as cortical actin formation and peripheral MLC phosphorylation (Garcia et al., 2001), which are not observed during FTY720-induced barrier enhancement (Dudek et al., 2007). Because (R)-OMe-FTY and FTY-F produce delayed TER elevation similar to FTY720 (Figure 2A), we next evaluated whether these compounds elicited a pattern of cytoskeletal rearrangements similar to S1P or FTY720 (Figure 3A-C). Immunofluorescent analysis reveals that S1P rapidly induces (within 5 min) translocation to the periphery of pulmonary EC of the barrier-regulatory actin-binding protein cortactin (Figure 3A) as previously described (Dudek et al., 2004). All of the novel FTY720 analogs induce less dramatic cortactin translocation similar to FTY720 within 5 min (Figure 3A) that persists for at least 30 min (data not shown) in association with the peak TER elevation observed with these compounds (Figure 2). In addition, S1P causes both peripheral MLC phosphorylation and Rac1 translocation that is not observed after FTY720 or any of its analogs tested here (Figure 3B & 3C). Interestingly, the (S)-OMe-FTY analog, which is barrier disruptive in the TER assay but barrier protective in the labeled dextran assay, induces cortactin translocation to the cell periphery, whereas thrombin, a well described and potent barrier-disrupting agent in both in vitro assays, does not (Dudek and Garcia, 2001) (Figure 3A).
Figure 3. FTY720 analogs and cytoskeletal rearrangement.

Confluent HPAEC were stimulated with vehicle control, S1P (1 μM), thrombin (1unit/ml), FTY720 (1 μM), (R)-OMe-FTY (1 μM), (S)-OMe-FTY (10 μM), FTY-F (1 μM), and FTY-G (10 μM) for 5 or 30 min as indicated. Cells were fixed using formaldehyde and stained for cortactin (A), MLC phosphorylation (B), or Rac1 (C). Yellow arrows indicate cortactin at the periphery (A), peripheral MLC-PP (B), or peripheral Rac1 (C). Images are representative of multiple experiments.
The effects of the novel FTY720 analogs on intracellular signaling events were next evaluated by examining MLC and ERK phosphorylation using Western blot analysis. Lung EC lysates demonstrate increased MLC and ERK phosphorylation at 5 min in response to S1P, whereas neither FTY720 nor any of its analogs induces significant MLC or ERK phosphorylation during this time frame (Figure 4A & 4B). Some minor increases in ERK phosphorylation are observed 30 min after (R)-OMe-FTY, FTY-F, or FTY-G, but the levels remain less than that induced by S1P (Figure 4A). Previous studies have described a brief but substantial increase in intracellular calcium (Ca2+) following S1P exposure in pulmonary EC (Garcia et al., 2001), whereas FTY720 fails to significantly increase intracellular Ca2+ (Dudek et al., 2007). In the current study HPAEC were stimulated with S1P, FTY720, FTY720 analogs, or thrombin to reveal that both thrombin and S1P produced a robust transient Ca2+ spike (Figure 5B & 5C), compared to modest but still significant responses from FTY720 and FTY-F (Figure 5D, 5G, 5I). FTY720 analog (S)-OMe-FTY displayed increased transient Ca2+ spikes that approached significance (Figure 5F & 5I) (p=0.051), suggesting that intracellular calcium may play a role in lung EC barrier regulation by (S)-OMe-FTY. (R)-OMe-FTY and FTY-G generated no appreciable calcium signal (Figure 5E, 5H, 5I).
Figure 4. Effects of FTY720 analogs on MLC and ERK phosphorylation.

Confluent HPAEC were stimulated with thrombin (1 unit/ml), S1P (1 μM), FTY720 (1 μM), or FTY720 analogs at 1 μM ((R)-OMe-FTY; FTY-F) or 10 μM ((S)-OMe-FTY; FTY-G), for 5 or 30 min, then lysed for Western blotting with (A) phospho-ERK and total VE-Cadherin or (B) phospho-MLC and total VE-Cadherin antibodies as indicated. Experiments were independently performed in triplicate with representative blots shown.
Figure 5. Effects of FTY720 analogs on intracellular calcium release.

Cultured HPAEC were stimulated with (B) thrombin (1unit/ml), (C) S1P (1 μM), (D) FTY720 (1 μM), (E) (R)-OMe-FTY (1 μM), (F) (S)-OMe-FTY (10 μM), (G) FTY-F (1 μM), or (H) FTY-G (10 μM), and intracellular calcium levels were measured (over 900 seconds) as change in [Ca2+] relative to (A) static HPAEC baseline readings, as determined by Fura-2 as described in Methods (nM, calculated from 340/380 ratio using calibration curves and software as previously described (Usatyuk et al., 2003)). (I) Bar graphs depicting relative intracellular calcium release compared to baseline were then quantified by measuring the total area under the curve after agonist stimulation at 100 seconds, using Photoshop densitometry readings. n = 4 independent experiments per condition with representative graphs shown (A-H); *p<0.01 or #p<0.05 versus static control.
3.3 Lung EC Signaling Events Associated with Barrier Enhancement by FTY720 Analogs
The next series of experiments were designed to mechanistically explore the manner in which these FTY720 analogs produce barrier enhancement. Similar to S1P and FTY720 (Dudek et al., 2007), TER elevation induced by the barrier-enhancing FTY720 analogs (R)-OMe-FTY, FTY-F, and FTY-G is significantly inhibited by pre-incubation with either pertussis toxin (PTX) or genistein, a nonspecific tyrosine kinase inhibitor (Figure 6A), indicating essential involvement of Gi-coupled signaling and tyrosine phosphorylation events in these responses. We also have reported previously that signaling pathways initiated in membrane lipid rafts are essential to S1P- and FTY720- induced barrier enhancement (Dudek et al., 2007; Singleton et al., 2005). Consistent with the involvement of lipid rafts in barrier enhancement by these novel FTY720 analogs, the lipid raft-disrupting agent, methyl-β-cyclodextrin (MβCD), significantly attenuates their ability to increase TER (Figure 6A).
Figure 6. Effect of Inhibitors on Barrier Regulation.
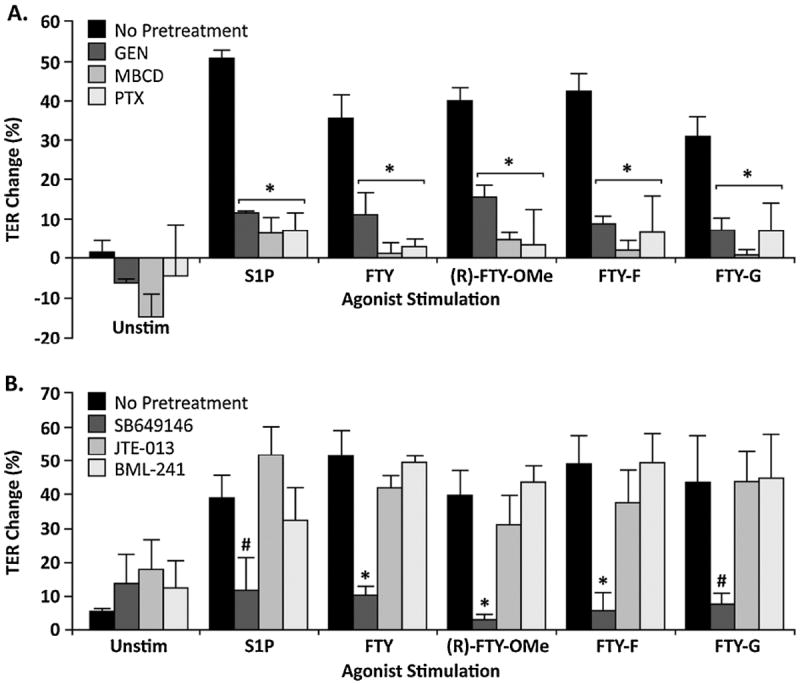
(A) Inhibitory effects of genistein, MβCD, and pertussis toxin on FTY720 analog-induced barrier enhancement. HPAEC were plated on gold microelectrodes for TER measurements as described in Methods. At time = 0, parallel lung EC monolayers were pre-treated with 100 μM genistein (GEN) for 30 min, 2 mM methyl-β-cyclodextrin (MβCD) for 1 hr in serum free media, or 100 ng/ml pertussis toxin (PTX) for 3 hr. Bar graphs depict pooled TER data from HPAEC pre-treated with GEN (dark gray), MβCD (medium gray), or PTX (light gray), then stimulated with S1P (1 μM), FTY720 (1 μM), (R)-OMe-FTY (1 μM), FTY-F (1 μM), and FTY-G (10 μM) as indicated. (B) FTY720 analog-induced barrier enhancement requires S1PR1 activation. HPAEC were plated on gold microelectrodes for TER measurements as described in Methods. Bar graphs depict pooled TER data from HPAEC pre-treated for 1 hr with 10 μM SB649146 (dark gray), JTE-013 (medium gray), or BML-241 (light gray), then stimulated with S1P (1 μM), FTY720 (1 μM), (R)-OMe-FTY (1 μM), FTY-F (1 μM), and FTY-G (10 μM) as indicated. The data are expressed as maximal percentage TER change (±S.E.M.) obtained within 60 min. Positive values indicate barrier enhancement. Negative values indicate barrier disruption. n = 3-4 independent experiments per condition; *p<0.01 or #p<0.05 versus no pre-treatment.
The S1P receptors are critical mediators of barrier regulation by S1P and other related compounds (Rosen et al., 2009; Wang and Dudek, 2009). We next explored the role of these S1P receptors in barrier regulation by the novel FTY720 analogs. Pretreatment with either JTE-013, a selective S1PR2 receptor antagonist (Osada et al., 2002), or BML-241, a selective S1PR3 receptor antagonist (Koide et al., 2002), did not significantly block TER elevation induced by the barrier-enhancing FTY720 analogs (R)-OMe-FTY, FTY-F, and FTY-G (Figure 6B). However, pretreatment with SB649146, an inverse agonist of the S1PR1 receptor (Waters et al., 2006), significantly inhibited TER elevation induced by the barrier-enhancing FTY720 analogs (R)-OMe-FTY, FTY-F, and FTY-G (Figure 6B), similar to S1P and FTY720. Overall, these in vitro data support a barrier-enhancing pathway induced by FTY720 analogs (R)-OMe-FTY, FTY-F, and FTY-G that includes lipid raft signaling, Gi-linked receptor coupling to downstream tyrosine phosphorylation events, and S1PR1-dependent receptor ligation (Figure 6).
4. Discussion
In this study, we demonstrate the potent effects of several novel FTY720 analogs on in vitro pulmonary vascular barrier function and signal activation. Modulation of the pulmonary vascular barrier has direct therapeutic relevance for acute inflammatory diseases such as ARDS, a condition with high morbidity afflicting an estimated 200,000 people annually and causing 75,000 deaths in the United States (Rubenfeld et al., 2005). To date, there are no effective interventions that target the underlying pulmonary vascular leak that characterizes this syndrome (Wheeler and Bernard, 2007). We have identified S1P as a potent pulmonary vascular barrier-enhancing agent both in vitro and in vivo (Garcia et al., 2001; McVerry et al., 2004; Peng et al., 2004). However, because of its potential to produce negative effects, including cardiac toxicity, pulmonary edema at higher doses, and airway hyperresponsiveness (Camp et al., 2009; Forrest et al., 2004; Gon et al., 2005; Hale et al., 2004a; Roviezzo et al., 2007), the compound S1P is not an optimal therapeutic candidate. We and others also have demonstrated the potent barrier-enhancing properties of the related pharmacologic agent, FTY720, both in vitro and in vivo (Dudek et al., 2007; Peng et al., 2004; Sanchez et al., 2003). Unfortunately, FTY720 has the potential to produce negative effects such as bradycardia, immunosuppression, and increased vascular leak at higher doses (Brown et al., 2007; Camp et al., 2009; Forrest et al., 2004; Kappos et al., 2006; Pelletier and Hafler, 2012) that are likely to limit its utility in critically ill patients with ARDS. In addition, multiple recent animal studies have demonstrated detrimental effects on vascular permeability of higher concentrations and prolonged exposure to FTY720, which produce tissue edema in mice (Oo et al., 2011) and worsen ventilator-induced lung injury (Muller et al., 2011) and bleomycin-induced lung injury (Shea et al., 2010; Wang et al., 2014).
Multiple groups have synthesized various derivatives of FTY720 primarily for characterizing them in terms of S1P receptor affinity and the ability to induce lymphopenia (Clemens et al., 2005; Forrest et al., 2004; Foss et al., 2005; Hale et al., 2004b; Hanessian et al., 2007; Imeri et al., 2014; Mandala et al., 2002; Zhu et al., 2007), to evaluate the pro-apoptotic effects of sphingosine and FTY720 (Don et al., 2007), or as possible antiangiogenic agents (Nakayama et al., 2008). However, our group has focused on their value as potential barrier regulatory agents (Camp et al., 2009; Wang et al., 2014), in the hopes of designing a more optimal therapeutic agent. To further our mechanistic understanding of how these compounds regulate EC barrier function, in the current study we have generated four additional analogs of FTY720 (Figure 1). The differential effects on lung EC barrier function by these novel FTY720 analogs illustrate the value of this approach. The (R)-Methoxy-FTY720 ((R)-OMe-FTY) and (R)/(S)-Fluoro-FTY720 (FTY-F) compounds display in vitro barrier enhancing properties comparable or superior to FTY720 and S1P (Figure 2A & 2D). Moreover, the barrier-enhancing β-Glucuronide-FTY720 analog (FTY-G) may be a more optimal therapeutic agent than S1P or FTY720 for treating ARDS-associated pulmonary edema because it exhibits a broader therapeutic index with increased potency in vitro (Figure 2B) (Camp et al., 2009). Similar to FTY720, (R)-OMe-FTY, FTY-F, and FTY-G do not require ERK phosphorylation, MLC phosphorylation, or Rac1 translocation to regulate EC barrier function, although there is subtle translocation of cortactin to the cell periphery with the novel FTY720 analogs (Figure 3A-C & Figure 4A-B). Measurements of [Ca2+]i indicate that only FTY-F induces significant intracellular calcium release above baseline, but it remains modest compared to the robust transient Ca2+ spikes from S1P (Figure 5I). Similar to both S1P and FTY720, mechanistic studies suggest that EC barrier enhancement by (R)-OMe-FTY, FTY-F, and FTY-G is mediated through lipid raft signaling, Gi-linked receptor coupling to downstream tyrosine phosphorylation events, and S1PR1-dependent receptor ligation (Figure 6).
However, even though S1PR1 likely is involved in barrier enhancement elicited by (R)-OMe-FTY, FTY-F, and FTY-G, these agents differ from S1P in the downstream signaling events that result from S1PR1 activation as they induce neither robust intracellular calcium release nor MLC/ERK phosphorylation. In addition, these analogs may have differential effects on S1PR1 degradation, as we recently reported for the (S)-phosphonate analog of FTY720 (Wang et al., 2014), which is an important mechanism for regulating S1PR signaling and will be explored in future studies. However, it is important to note that a limitation in our S1P receptor data. In the current study we utilized pharmacologic inhibitors, such as SB649146, to assess the roles of S1P receptors in these pathways, and all pharmacologic inhibitors have the potential for off-target effects. Additional studies to specifically downregulate S1P receptor expression (e.g., with siRNA) would provide further confirmation.
Our results also demonstrate that subtle structural changes are sufficient to significantly alter the barrier regulatory properties of these compounds. Despite being structurally similar to the parent FTY720 compound and an enantiomer of the (R)-OMe-FTY compound, the (S)-Methoxy-FTY720 ((S)-OMe-FTY) compound is barrier-disruptive in the TER assay (Figure 2B) but appears barrier-protective in the labeled dextran assay (Figure 2D). Moreover, (S)-OMe-FTY exhibits characteristics associated with both lung EC barrier disruption and enhancement. It causes some increased actin stress fiber formation similar to thrombin (data not shown), but does not appear to involve MLC phosphorylation, as observed after thrombin (Dudek and Garcia, 2001). In contrast, (S)-OMe-FTY induces peripheral cortactin translocation as observed during barrier enhancement by S1P (Dudek et al., 2004). It is interesting to speculate that some of the differential effects of (S)-OMe-FTY compared to (R)-OMe-FTY may be related to the observation that the latter compound ((R)-OMe-FTY) inhibits the S1P-generating enzyme sphingosine kinase 2, while the former compound ((S)-OMe-FTY) does not (Lim et al., 2011). Further study of these interesting (R)- and (S)-OMe-FTY compounds hopefully will provide additional insights into lung EC barrier regulation by this class of agents.
5. Conclusions
In summary, modulation of pulmonary vascular barrier function remains an important clinical goal for devastating acute inflammatory diseases such as ARDS and sepsis. The current study utilizes several novel FTY720 analogs to further our understanding of EC barrier regulation. These results add to the growing literature supporting a potential therapeutic role for this class of compounds in reversing the pulmonary vascular leak that characterizes ARDS. Given the high mortality of this syndrome and lack of specific therapies (Wheeler and Bernard, 2007), additional preclinical studies of these novel FTY720 analogs are warranted to better characterize this therapeutic potential.
Supplementary Material
Highlights.
Novel therapeutics are needed to treat vascular leak in ARDS
This study characterizes effects of 4 novel FTY720 analogs on vascular permeability
These analogs employ S1P-related signaling pathways to alter permeability
Three novel analogs are barrier-enhancing comparable or superior to FTY720/S1P
These mechanistic insights may assist in novel ARDS therapeutic development
Acknowledgments
This work was supported by the National Institutes of Health grants P01 HL 58064 (JGNG), and P01 HL 98050 (VN). This article is dedicated to the memory of Dr. Robert Bittman. Dr. Bittman was a dear friend and exceptional lipid biochemist without whose insight, enthusiasm, and friendship this research would have never been completed. The conception, design, and synthesis of the novel compounds described in this study were performed entirely under his direction and would not have been possible without his vast experience and outstanding scientific acumen.
Abbreviations
- ARDSA
cute respiratory distress syndrome
- EC
endothelial cell
- HPAEC
human pulmonary artery endothelial cells
- MβCD
methyl-β-cyclodextrin
- MLC
myosin light chain
- PTX
pertussis toxin
- S1P
sphingosine 1-phosphate
- S1P1R
S1P1 receptor
- S1P2R
S1P2 receptor
- S1P3R
S1P3 receptor
- TER
transendothelial electrical resistance
- ERK
extracellular signal-regulated kinase
- FTY720
2-amino-2-(2-[4-octylphenyl]ethyl)-1, 3-propanediol
- FITC
fluorescein isothiocyanate
- PBS
phosphate-buffered saline
- (R)-FTY-OMe
(R)-Methoxy-FTY720
- (S)-FTY-OMe
(S)-Methoxy-FTY720
- FTY-F
(R)/(S)-Fluoro-FTY720
- FTY-G
β-Glucuronide-FTY720
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Billman JH, Parker EE. Amino Acids. IV. Amino Acids Related to Serine. J Am Chem Soc. 1945;67:1069–1070. [Google Scholar]
- Brown BA, Kantesaria PP, McDevitt LM. Fingolimod: a novel immunosuppressant for multiple sclerosis. The Annals of pharmacotherapy. 2007;41:1660–1668. doi: 10.1345/aph.1G424. [DOI] [PubMed] [Google Scholar]
- Camp SM, Bittman R, Chiang ET, Moreno-Vinasco L, Mirzapoiazova T, Sammani S, Lu X, Sun C, Harbeck M, Roe M, Natarajan V, Garcia JG, Dudek SM. Synthetic analogs of FTY720 [2-amino-2-(2-[4-octylphenyl]ethyl)-1,3-propanediol] differentially regulate pulmonary vascular permeability in vivo and in vitro. The Journal of pharmacology and experimental therapeutics. 2009;331:54–64. doi: 10.1124/jpet.109.153544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clemens JJ, Davis MD, Lynch KR, Macdonald TL. Synthesis of 4(5)-phenylimidazole-based analogues of sphingosine-1-phosphate and FTY720: discovery of potent S1P1 receptor agonists. Bioorganic & medicinal chemistry letters. 2005;15:3568–3572. doi: 10.1016/j.bmcl.2005.05.097. [DOI] [PubMed] [Google Scholar]
- Don AS, Martinez-Lamenca C, Webb WR, Proia RL, Roberts E, Rosen H. Essential requirement for sphingosine kinase 2 in a sphingolipid apoptosis pathway activated by FTY720 analogues. The Journal of biological chemistry. 2007;282:15833–15842. doi: 10.1074/jbc.M609124200. [DOI] [PubMed] [Google Scholar]
- Dudek SM, Camp SM, Chiang ET, Singleton PA, Usatyuk PV, Zhao Y, Natarajan V, Garcia JG. Pulmonary endothelial cell barrier enhancement by FTY720 does not require the S1P1 receptor. Cellular signalling. 2007;19:1754–1764. doi: 10.1016/j.cellsig.2007.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dudek SM, Garcia JG. Cytoskeletal regulation of pulmonary vascular permeability. J Appl Physiol. 2001;91:1487–1500. doi: 10.1152/jappl.2001.91.4.1487. [DOI] [PubMed] [Google Scholar]
- Dudek SM, Jacobson JR, Chiang ET, Birukov KG, Wang P, Zhan X, Garcia JG. Pulmonary endothelial cell barrier enhancement by sphingosine 1-phosphate: roles for cortactin and myosin light chain kinase. The Journal of biological chemistry. 2004;279:24692–24700. doi: 10.1074/jbc.M313969200. [DOI] [PubMed] [Google Scholar]
- Duimstra JA, Femia FJ, Meade TJ. A Gadolinium Chelate for Detection of β-Glucuronidase: A Self-Immolative Approach. J Am Chem Soc. 2005;127:12847–12855. doi: 10.1021/ja042162r. [DOI] [PubMed] [Google Scholar]
- Forrest M, Sun SY, Hajdu R, Bergstrom J, Card D, Doherty G, Hale J, Keohane C, Meyers C, Milligan J, Mills S, Nomura N, Rosen H, Rosenbach M, Shei GJ, Singer II, Tian M, West S, White V, Xie J, Proia RL, Mandala S. Immune cell regulation and cardiovascular effects of sphingosine 1-phosphate receptor agonists in rodents are mediated via distinct receptor subtypes. The Journal of pharmacology and experimental therapeutics. 2004;309:758–768. doi: 10.1124/jpet.103.062828. [DOI] [PubMed] [Google Scholar]
- Foss FW, Jr, Clemens JJ, Davis MD, Snyder AH, Zigler MA, Lynch KR, Macdonald TL. Synthesis, stability, and implications of phosphothioate agonists of sphingosine-1-phosphate receptors. Bioorganic & medicinal chemistry letters. 2005;15:4470–4474. doi: 10.1016/j.bmcl.2005.07.057. [DOI] [PubMed] [Google Scholar]
- Garcia JG, Liu F, Verin AD, Birukova A, Dechert MA, Gerthoffer WT, Bamberg JR, English D. Sphingosine 1-phosphate promotes endothelial cell barrier integrity by Edg-dependent cytoskeletal rearrangement. The Journal of clinical investigation. 2001;108:689–701. doi: 10.1172/JCI12450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia JG, Siflinger-Birnboim A, Bizios R, Del Vecchio PJ, Fenton JW, 2nd, Malik AB. Thrombin-induced increase in albumin permeability across the endothelium. Journal of cellular physiology. 1986;128:96–104. doi: 10.1002/jcp.1041280115. [DOI] [PubMed] [Google Scholar]
- Gon Y, Wood MR, Kiosses WB, Jo E, Sanna MG, Chun J, Rosen H. S1P3 receptor-induced reorganization of epithelial tight junctions compromises lung barrier integrity and is potentiated by TNF. Proceedings of the National Academy of Sciences of the United States of America. 2005;102:9270–9275. doi: 10.1073/pnas.0501997102. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Hale JJ, Doherty G, Toth L, Mills SG, Hajdu R, Keohane CA, Rosenbach M, Milligan J, Shei GJ, Chrebet G, Bergstrom J, Card D, Forrest M, Sun SY, West S, Xie H, Nomura N, Rosen H, Mandala S. Selecting against S1P3 enhances the acute cardiovascular tolerability of 3-(N-benzyl)aminopropylphosphonic acid S1P receptor agonists. Bioorganic & medicinal chemistry letters. 2004a;14:3501–3505. doi: 10.1016/j.bmcl.2004.04.070. [DOI] [PubMed] [Google Scholar]
- Hale JJ, Neway W, Mills SG, Hajdu R, Ann Keohane C, Rosenbach M, Milligan J, Shei GJ, Chrebet G, Bergstrom J, Card D, Koo GC, Koprak SL, Jackson JJ, Rosen H, Mandala S. Potent S1P receptor agonists replicate the pharmacologic actions of the novel immune modulator FTY720. Bioorganic & medicinal chemistry letters. 2004b;14:3351–3355. doi: 10.1016/j.bmcl.2004.02.106. [DOI] [PubMed] [Google Scholar]
- Hanessian S, Charron G, Billich A, Guerini D. Constrained azacyclic analogues of the immunomodulatory agent FTY720 as molecular probes for sphingosine 1-phosphate receptors. Bioorganic & medicinal chemistry letters. 2007;17:491–494. doi: 10.1016/j.bmcl.2006.10.014. [DOI] [PubMed] [Google Scholar]
- He L, Byun H-S, Smit J, Wilschut J, Bittman R. Enantioselective Synthesis of a Novel Trans Double Bond Ceramide Analogue via Catalytic Asymmetric Dihydroxylation of an Enyne: The Role of the Trans Double Bond of Ceramide in the Fusion of Semliki Forest Virus with Target Membranes. J Am Chem Soc. 1999;121:3897–3903. [Google Scholar]
- Imeri F, Fallegger D, Zivkovic A, Schwalm S, Enzmann G, Blankenbach K, Meyer zu Heringdorf D, Homann T, Kleuser B, Pfeilschifter J, Engelhardt B, Stark H, Huwiler A. Novel oxazolo-oxazole derivatives of FTY720 reduce endothelial cell permeability, immune cell chemotaxis and symptoms of experimental autoimmune encephalomyelitis in mice. Neuropharmacology. 2014;85:314–327. doi: 10.1016/j.neuropharm.2014.05.012. [DOI] [PubMed] [Google Scholar]
- Kappos L, Antel J, Comi G, Montalban X, O’Connor P, Polman CH, Haas T, Korn AA, Karlsson G, Radue EW. Oral fingolimod (FTY720) for relapsing multiple sclerosis. The New England journal of medicine. 2006;355:1124–1140. doi: 10.1056/NEJMoa052643. [DOI] [PubMed] [Google Scholar]
- Koide Y, Hasegawa T, Takahashi A, Endo A, Mochizuki N, Nakagawa M, Nishida A. Development of novel EDG3 antagonists using a 3D database search and their structure-activity relationships. Journal of medicinal chemistry. 2002;45:4629–4638. doi: 10.1021/jm020080c. [DOI] [PubMed] [Google Scholar]
- Lim KG, Sun C, Bittman R, Pyne NJ, Pyne S. (R)-FTY720 methyl ether is a specific sphingosine kinase 2 inhibitor: Effect on sphingosine kinase 2 expression in HEK 293 cells and actin rearrangement and survival of MCF-7 breast cancer cells. Cellular signalling. 2011;23:1590–1595. doi: 10.1016/j.cellsig.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu X, Sun C, Valentine WJ, Shuyu E, Liu J, Tigyi G, Bittman R. Chiral vinylphosphonate and phosphonate analogues of the immunosuppressive agent FTY720. J Org Chem. 2009;74:3192–3195. doi: 10.1021/jo900023u. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandala S, Hajdu R, Bergstrom J, Quackenbush E, Xie J, Milligan J, Thornton R, Shei GJ, Card D, Keohane C, Rosenbach M, Hale J, Lynch CL, Rupprecht K, Parsons W, Rosen H. Alteration of lymphocyte trafficking by sphingosine-1-phosphate receptor agonists. Science (New York, N Y) 2002;296:346–349. doi: 10.1126/science.1070238. [DOI] [PubMed] [Google Scholar]
- McVerry BJ, Peng X, Hassoun PM, Sammani S, Simon BA, Garcia JG. Sphingosine 1-phosphate reduces vascular leak in murine and canine models of acute lung injury. American journal of respiratory and critical care medicine. 2004;170:987–993. doi: 10.1164/rccm.200405-684OC. [DOI] [PubMed] [Google Scholar]
- Muller HC, Hocke AC, Hellwig K, Gutbier B, Peters H, Schonrock SM, Tschernig T, Schmiedl A, Hippenstiel S, N’Guessan PD, Rosseau S, Suttorp N, Witzenrath M. The Sphingosine-1 Phosphate receptor agonist FTY720 dose dependently affected endothelial integrity in vitro and aggravated ventilator-induced lung injury in mice. Pulmonary pharmacology & therapeutics. 2011;24:377–385. doi: 10.1016/j.pupt.2011.01.017. [DOI] [PubMed] [Google Scholar]
- Nakayama S, Uto Y, Tanimoto K, Okuno Y, Sasaki Y, Nagasawa H, Nakata E, Arai K, Momose K, Fujita T, Hashimoto T, Okamoto Y, Asakawa Y, Goto S, Hori H. TX-2152: a conformationally rigid and electron-rich diyne analogue of FTY720 with in vivo antiangiogenic activity. Bioorganic & medicinal chemistry. 2008;16:7705–7714. doi: 10.1016/j.bmc.2008.07.003. [DOI] [PubMed] [Google Scholar]
- Oo ML, Chang SH, Thangada S, Wu MT, Rezaul K, Blaho V, Hwang SI, Han DK, Hla T. Engagement of S1P-degradative mechanisms leads to vascular leak in mice. The Journal of clinical investigation. 2011;121:2290–2300. doi: 10.1172/JCI45403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osada M, Yatomi Y, Ohmori T, Ikeda H, Ozaki Y. Enhancement of sphingosine 1-phosphate-induced migration of vascular endothelial cells and smooth muscle cells by an EDG-5 antagonist. Biochemical and biophysical research communications. 2002;299:483–487. doi: 10.1016/s0006-291x(02)02671-2. [DOI] [PubMed] [Google Scholar]
- Pelletier D, Hafler DA. Fingolimod for multiple sclerosis. The New England journal of medicine. 2012;366:339–347. doi: 10.1056/NEJMct1101691. [DOI] [PubMed] [Google Scholar]
- Peng X, Hassoun PM, Sammani S, McVerry BJ, Burne MJ, Rabb H, Pearse D, Tuder RM, Garcia JG. Protective effects of sphingosine 1-phosphate in murine endotoxin-induced inflammatory lung injury. American journal of respiratory and critical care medicine. 2004;169:1245–1251. doi: 10.1164/rccm.200309-1258OC. [DOI] [PubMed] [Google Scholar]
- Rosen H, Gonzalez-Cabrera PJ, Sanna MG, Brown S. Sphingosine 1-phosphate receptor signaling. Annual review of biochemistry. 2009;78:743–768. doi: 10.1146/annurev.biochem.78.072407.103733. [DOI] [PubMed] [Google Scholar]
- Rosenfeldt HM, Amrani Y, Watterson KR, Murthy KS, Panettieri RA, Jr, Spiegel S. Sphingosine-1-phosphate stimulates contraction of human airway smooth muscle cells. Faseb J. 2003;17:1789–1799. doi: 10.1096/fj.02-0836com. [DOI] [PubMed] [Google Scholar]
- Roviezzo F, Di Lorenzo A, Bucci M, Brancaleone V, Vellecco V, De Nardo M, Orlotti D, De Palma R, Rossi F, D’Agostino B, Cirino G. Sphingosine-1-phosphate/sphingosine kinase pathway is involved in mouse airway hyperresponsiveness. American journal of respiratory cell and molecular biology. 2007;36:757–762. doi: 10.1165/rcmb.2006-0383OC. [DOI] [PubMed] [Google Scholar]
- Rubenfeld GD, Caldwell E, Peabody E, Weaver J, Martin DP, Neff M, Stern EJ, Hudson LD. Incidence and outcomes of acute lung injury. The New England journal of medicine. 2005;353:1685–1693. doi: 10.1056/NEJMoa050333. [DOI] [PubMed] [Google Scholar]
- Sanchez T, Estrada-Hernandez T, Paik JH, Wu MT, Venkataraman K, Brinkmann V, Claffey K, Hla T. Phosphorylation and action of the immunomodulator FTY720 inhibits vascular endothelial cell growth factor-induced vascular permeability. The Journal of biological chemistry. 2003;278:47281–47290. doi: 10.1074/jbc.M306896200. [DOI] [PubMed] [Google Scholar]
- Schumacher DP, Clark JE, Murphy BL, Fischer PA. An efficient synthesis of florfenicol. J Org Chem. 1990;55:5291–5294. [Google Scholar]
- Shea BS, Brooks SF, Fontaine BA, Chun J, Luster AD, Tager AM. Prolonged exposure to sphingosine 1-phosphate receptor-1 agonists exacerbates vascular leak, fibrosis, and mortality after lung injury. American journal of respiratory cell and molecular biology. 2010;43:662–673. doi: 10.1165/rcmb.2009-0345OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shikata Y, Birukov KG, Garcia JG. S1P induces FA remodeling in human pulmonary endothelial cells: role of Rac, GIT1, FAK, and paxillin. J Appl Physiol. 2003;94:1193–1203. doi: 10.1152/japplphysiol.00690.2002. [DOI] [PubMed] [Google Scholar]
- Singleton PA, Dudek SM, Chiang ET, Garcia JG. Regulation of sphingosine 1-phosphate-induced endothelial cytoskeletal rearrangement and barrier enhancement by S1P1 receptor, PI3 kinase, Tiam1/Rac1, and alpha-actinin. Faseb J. 2005;19:1646–1656. doi: 10.1096/fj.05-3928com. [DOI] [PubMed] [Google Scholar]
- Usatyuk PV, Fomin VP, Shi S, Garcia JG, Schaphorst K, Natarajan V. Role of Ca2+ in diperoxovanadate-induced cytoskeletal remodeling and endothelial cell barrier function. American journal of physiology. 2003;285:L1006–1017. doi: 10.1152/ajplung.00408.2002. [DOI] [PubMed] [Google Scholar]
- Wang L, Chiang ET, Simmons JT, Garcia JG, Dudek SM. FTY720-induced human pulmonary endothelial barrier enhancement is mediated by c-Abl. Eur Respir J. 2011;38:78–88. doi: 10.1183/09031936.00047810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L, Dudek SM. Regulation of vascular permeability by sphingosine 1-phosphate. Microvascular research. 2009;77:39–45. doi: 10.1016/j.mvr.2008.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L, Sammani S, Moreno-Vinasco L, Letsiou E, Wang T, Camp SM, Bittman R, Garcia JG, Dudek SM. FTY720 (s)-phosphonate preserves sphingosine 1-phosphate receptor 1 expression and exhibits superior barrier protection to FTY720 in acute lung injury. Critical care medicine. 2014;42:e189–199. doi: 10.1097/CCM.0000000000000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters CM, Long J, Gorshkova I, Fujiwara Y, Connell M, Belmonte KE, Tigyi G, Natarajan V, Pyne S, Pyne NJ. Cell migration activated by platelet-derived growth factor receptor is blocked by an inverse agonist of the sphingosine 1-phosphate receptor-1. Faseb J. 2006;20:509–511. doi: 10.1096/fj.05-4810fje. [DOI] [PubMed] [Google Scholar]
- Wheeler AP, Bernard GR. Acute lung injury and the acute respiratory distress syndrome: a clinical review. Lancet. 2007;369:1553–1564. doi: 10.1016/S0140-6736(07)60604-7. [DOI] [PubMed] [Google Scholar]
- Zhu R, Snyder AH, Kharel Y, Schaffter L, Sun Q, Kennedy PC, Lynch KR, Macdonald TL. Asymmetric synthesis of conformationally constrained fingolimod analogues--discovery of an orally active sphingosine 1-phosphate receptor type-1 agonist and receptor type-3 antagonist. Journal of medicinal chemistry. 2007;50:6428–6435. doi: 10.1021/jm7010172. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


