Abstract
BACKGROUND
Gastrointestinal and liver diseases (GILDs) are major causes of death and disability in Middle East and North Africa (MENA). However, they have different patterns in countries with various geographical, cultural, and socio-economic status. We aimed to compare the burden of GILDs in Iran with its neighboring countries using the results of the Global Burden of Disease (GBD) Study in 2010.
METHODS
Classic metrics of GBD have been used including: age-standardized rates (ASRs) of death, years of life lost due to premature death (YLL), years of life lost due to disability (YLD), and disability adjusted life years (DALY). All countries neighboring Iran have been selected. In addition, all other countries classified in the MENA region were included. Five major groups of gastrointestinal and hepatic diseases were studied including: infections of gastrointestinal tract, gastrointestinal and pancreatobilliary cancers, acute hepatitis, cirrhosis, and other digestive diseases.
RESULTS
The overall burden of GILDs is highest in Afghanistan, Pakistan, and Egypt. Diarrheal diseases have been replaced by gastrointestinal cancers and cirrhosis in most countries in the region. However, in a number of countries including Afghanistan, Pakistan, Turkmenistan, Egypt, and Yemen, communicable GILDs are still among top causes of mortality and morbidity in addition to non-communicable GILDs and cancers. These countries are experiencing the double burden. In Iran, burden caused by cancers of stomach and esophagus are considerably higher than other countries. Diseases that are mainly diagnosed in outpatient settings have not been captured by GBD.
CONCLUSION
Improving the infrastructure of health care system including cancer registries and electronic recording of outpatient care is a necessity for better surveillance of GILDs in MENA. In contrast to expensive treatment, prevention of most GILDs is feasible and inexpensive. The health care systems in the region can be strengthened for prevention and control
Keywords: Gastrointestinal disease, Liver disease, Mortality, Disability, Burden, Middle East and North Africa
INTRODUCTION
The epidemiological transition can be observed in almost all countries worldwide.1 As neighboring countries may share geographical, political, and cultural characteristics, the pattern of transition may be somehow similar. However, heterogeneity in health indicators may also be observed due to heterogeneous socio-economic determinants and health system governance and infrastructure. It may be important for policy makers at national level to be aware of the health status in their country compared with their neighbors and other countries with similar socio-economic and cultural determinants. Policy makers can learn lessons from experiences of their neighboring countries in health care promotion.
Countries in Middle East and North Africa (MENA) share very important determinants including religion, socio-economic status, and partly ethnicity. However, significant differences in health indicators may also be observed between these countries. Gastrointestinal and liver diseases (GILDs) are among diseases that show variability in the pattern of their prevalence, incidence, mortality and the final burden they impose on societies. While some countries such as Afghanistan and Pakistan are still facing challenges regarding the control of gastrointestinal infectious diseases, other countries with better economy in the region have experienced the obvious transition from communicable to non-communicable GILDs.
In the current article, following the previous two articles regarding the burden of GILD in 2010 and its trend since 1990 in Iran, we are presenting the burden and its trend in Iran in comparison with the neighboring countries and other countries in MENA, which have been estimated in Global Burden of Disease (GBD) study 2010.2,3 We have taken the advantage of the unique metrics developed by GBD that make it possible to compare the health status of countries within the past two decades.
MATERIALS AND METHODS
The methodology of GBD study 2010 has been explained elsewhere in details.4 The concepts of death, years of life lost due to premature death (YLLs), years of life lost due to disability (YLDs), and the disability adjusted life years (DALYs) are the same as previous reports.5-9
In the estimates presented here, all countries neighboring Iran have been selected. These countries include: Pakistan, Afghanistan, Turkmenistan, Azerbaijan, Armenia, Turkey, and Iraq. In addition, all other countries classified in the MENA region were included as well. This group of countries consisted of: Algeria, Bahrain, Egypt, Jordan, Kuwait, Lebanon, Libya, Morocco, Palestine, Oman, Qatar, Saudi Arabia, Syria, Tunisia, United Arab Emirates, and Yemen. Five major groups of gastrointestinal and hepatic diseases were studied. These major groups included: infections of gastrointestinal tract, gastrointestinal and hepatobilliary cancers, acute hepatitis, cirrhosis, and other digestive diseases. The age-standardized rates (ASRs) were compared between countries in 2010. Countries were ranked in terms of total deaths and DALYs caused by overall gastrointestinal and hepatic diseases. Furthermore, trend of death and DALYs rates from 1990 to 2010 were also illustrated for all countries.
RESULTS
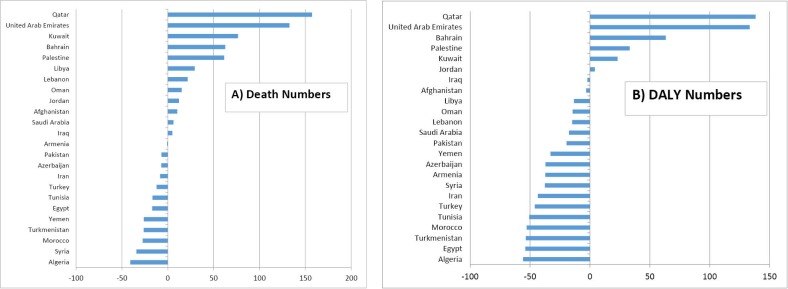
Figure 1 shows the ASRs of deaths, DALYs, YLLs, and YLDs per 100,000 for all digestive diseases in MENA region in 2010. Afghanistan, Egypt, Pakistan, Turkmenistan, and Yemen are the top five countries in terms of ASRs of deaths, DALYs, YLLs, and YLDs due to all digestive diseases in 2010. Syria, Lebanon, Kuwait, and Saudi Arabia are among the top five countries with the least ASRs of death, DALYs, and YLLs. Iraq is ranked among top five countries with least YLD rates that has replaced Kuwait. Also in 2010, Iran ranked 13th, 15th, 15th, and 12th in terms of ASR for deaths, DALYs, YLLs, and YLDs respectively caused by overall gastrointestinal diseases.
Fig 1 .
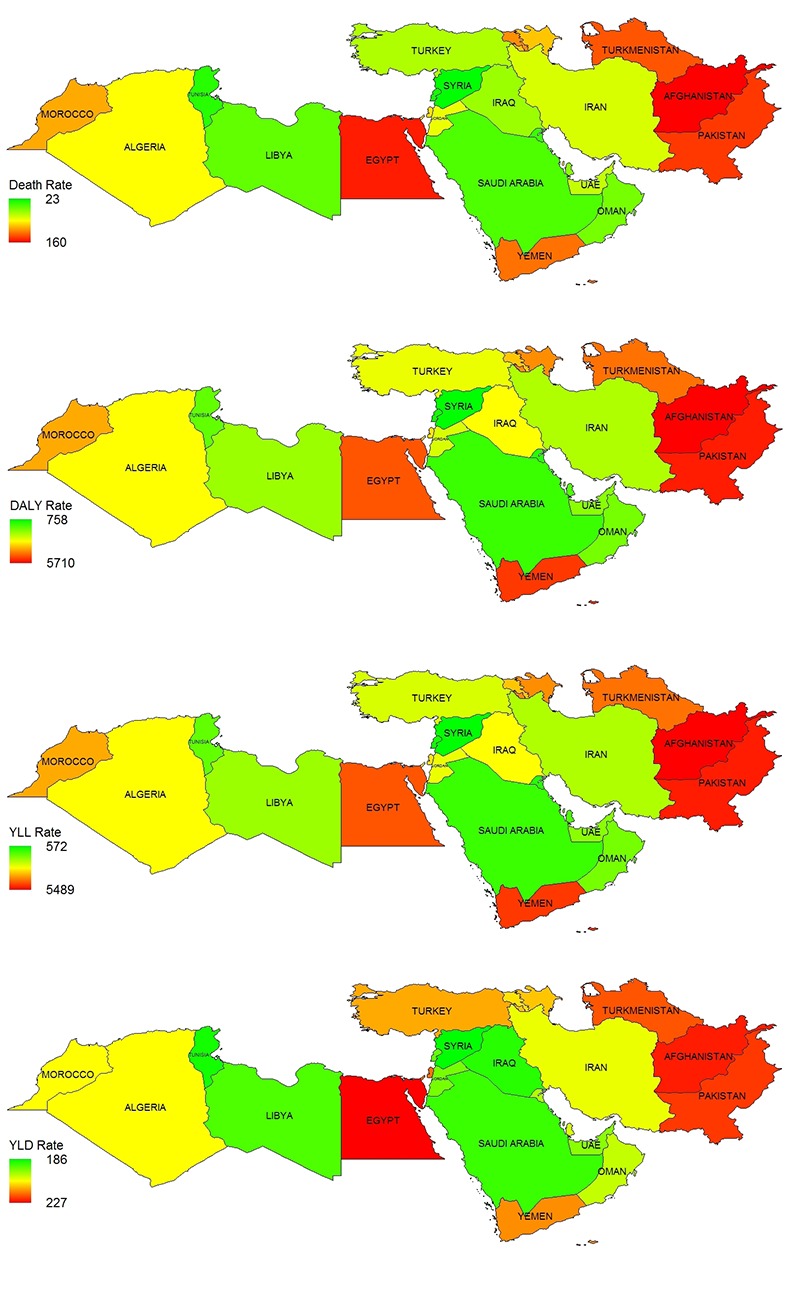
The age standardized rates (ASRs) of death, DALYs, YLLs, and YLDs for all digestive diseases per 100,000 in countries neighboring Iran and other countries in Middle East and North Africa in 2010
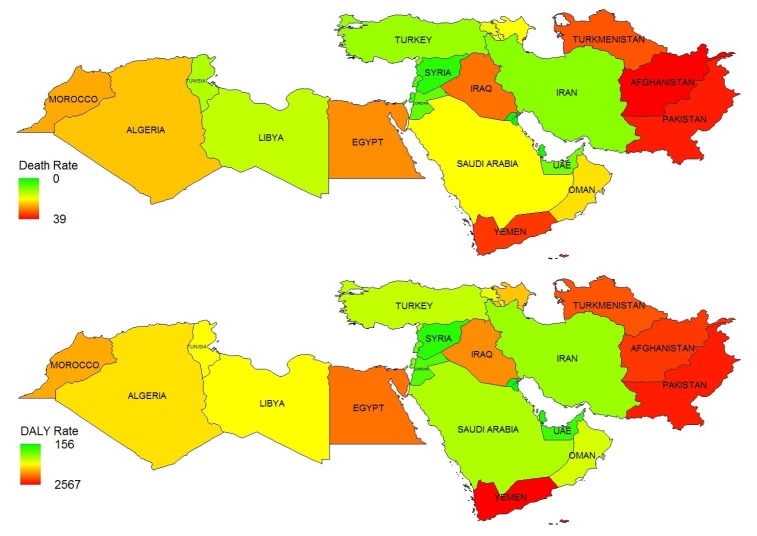
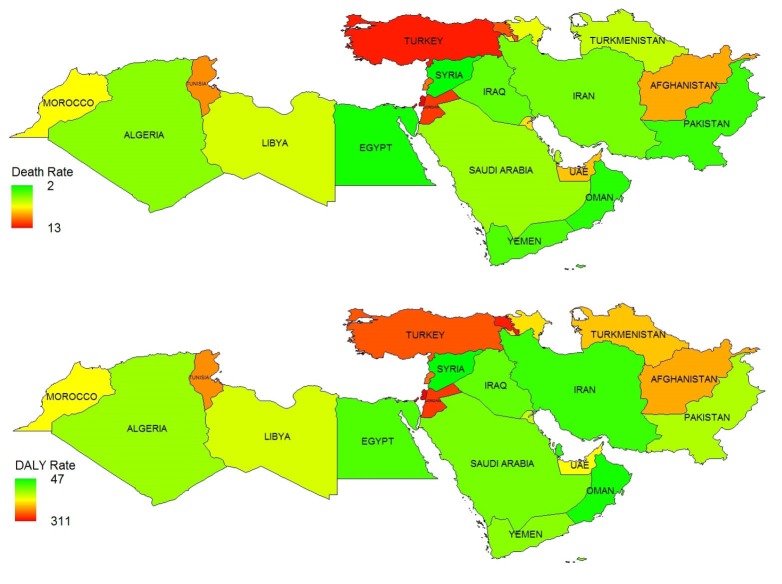
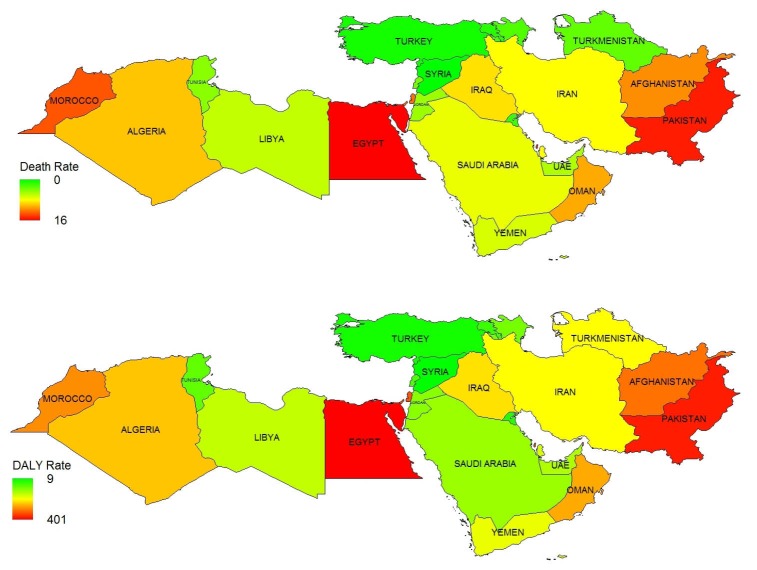
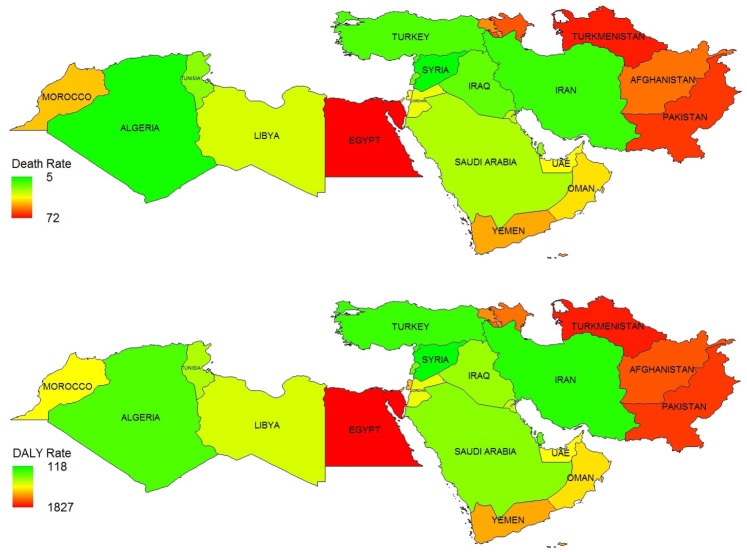
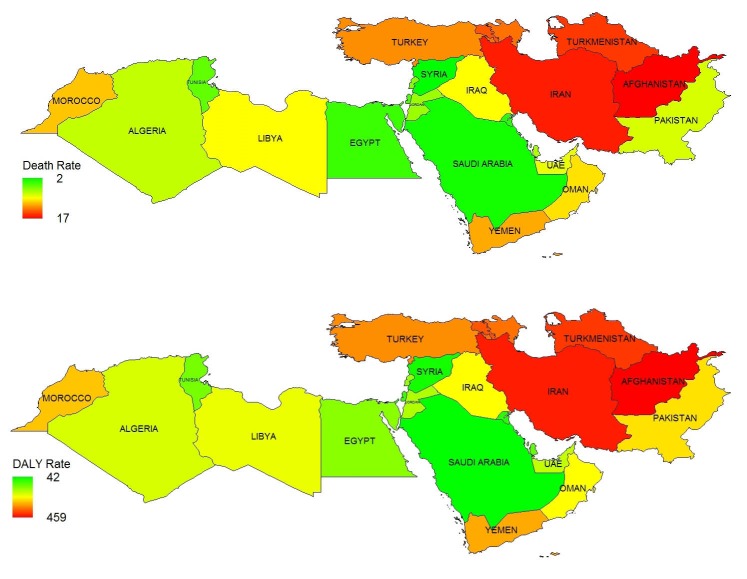
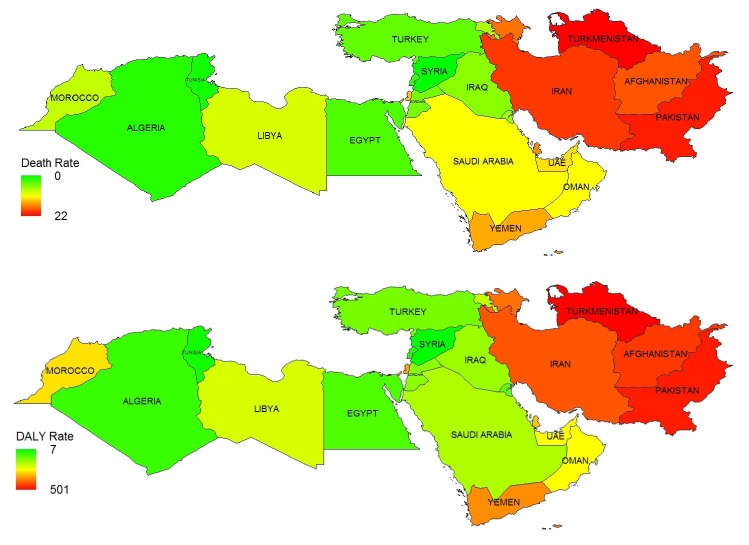
Figures 2 to 7 show the ASR for deaths and DALYs in Middle East countries for diarrheal diseases, acute hepatitis, cirrhosis, stomach cancer, esophageal cancer, and colorectal cancer. Rates for diarrheal diseases are highest in Pakistan, Afghanistan, Yemen, Turkmenistan, and Egypt and lowest in Kuwait, Qatar, and Syria. The rates of hepatitis and cirrhosis are highest in Egypt, Pakistan, and Afghanistan and lowest in Syria and Turkey. Rates for stomach cancer are highest in Afghanistan, Iran, and Turkmenistan. The highest rates for esophageal cancer are observed in Turkmenistan, Iran, Pakistan, Afghanistan, and Azerbaijan. Finally, the burden of colorectal cancer is highest in Turkey, Palestine, Armenia, Jordan, and Lebanon.
Fig 2 .
The age standardized rates of deaths and DALYs per 100,000 caused by diarrheal diseases in Middle East and North Africa DALYs: the disability adjusted life years
Fig 7 .
The age standardized rates of deaths and DALYs per 100,000 caused by colorectal cancer in Middle East and North Africa DALYs: the disability adjusted life years
Fig 3 .
The age standardized rates of deaths and DALYs per 100,000 caused by all types of acute hepatitis in Middle East and North Africa DALYs: the disability adjusted life years
Fig 4 .
The age standardized rates of deaths and DALYs per 100,000 caused by cirrhosis secondary to all risk factors in Middle East and North Africa DALYs: the disability adjusted life years
Fig 5 .
The age standardized rates of deaths and DALYs per 100,000 caused by stomach cancer in Middle East and North Africa DALYs: the disability adjusted life years
Fig 6 .
The age standardized rates of deaths and DALYs per 100,000 caused by esophageal cancer in Middle East and North Africa DALYs: the disability adjusted life years
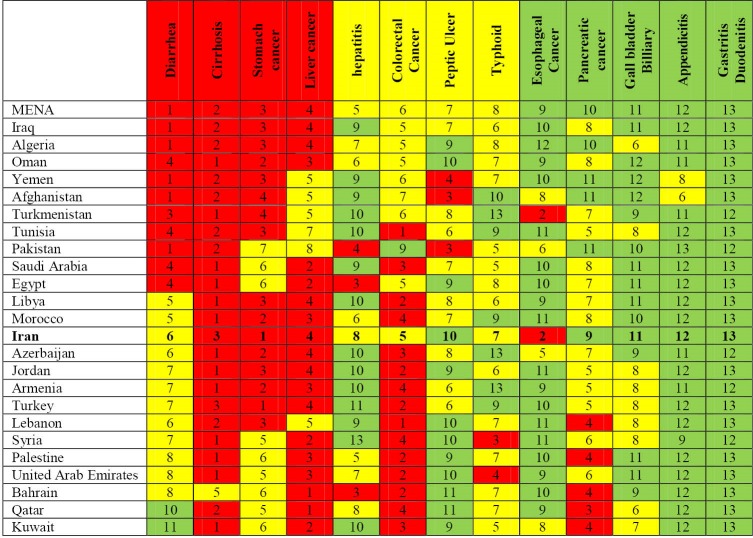
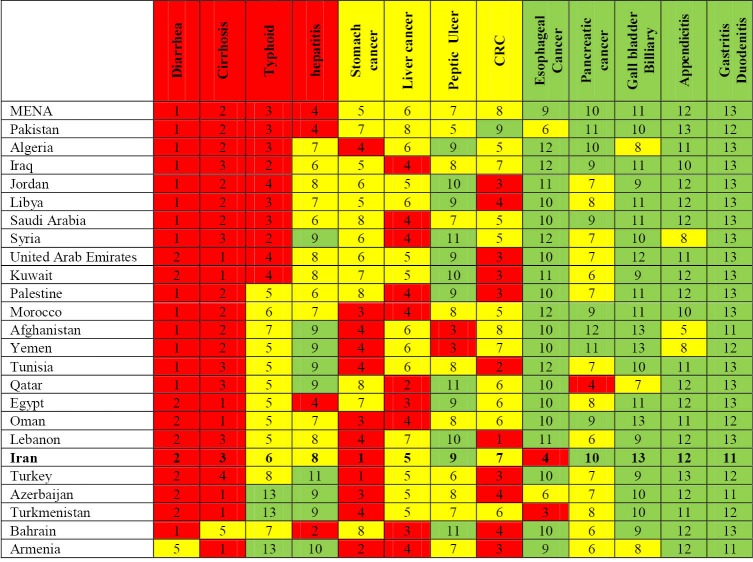
Figures 8 and 9 show the ranking of main gastrointestinal diseases in 24 countries in 2010 by ASRs of death and DALY rates per 100,000 respectively. All data are reported for both sexes. Diarrhea is the first cause for both death rates and DALY rates in the entire region. It is among the top four causes of death in 10 countries and is the first or the second cause of DALY in all countries except for Armenia. Diarrhea ranks 10th and 11th cause of death in Qatar and Kuwait, which is quite different from other countries.
Fig 8 .
Ranking of main gastrointestinal diseases by death rate in 25 countries in Middle East and neighboring Iran in 2010 MENA: Middle East and North Africa
Fig 9 .
Ranking of main gastrointestinal diseases by DALY rate in 25 countries in Middle East and neighboring Iran in 2010 MENA: Middle East and North Africa
Cirrhosis is the second cause of both death and DALY in the region. It is among the top three causes of death and DALY in all countries except for Bahrain. Typhoid and hepatitis are the 3rd and 4th causes of DALYs in the region but they are replaced by stomach cancer and liver cancer as 3rd and 4th causes of death. Stomach cancer is among the top four causes of death in 15 countries and among the top four causes of DALY in 12 countries. The respective figures for liver cancer are 19 and 11 countries. Hepatitis has high rank in Pakistan, Egypt, and Bahrain in terms of both death and DALY rates. Peptic ulcer is the 7th cause of both death and DALY in the region. Colorectal cancer is the 6th cause of death and 8th cause of DALY in the region. Esophageal cancer, pancreatic cancer, gall bladder and billiary cancer, appendicitis, and gastritis and duodenitis are the five diseases causing least deaths and DALYs in the region. The rankings of the first four causes of deaths and DALYs and the last five causes in most countries are almost compatible with the rankings in the entire region. Esophageal cancer has a specifically high rank in Iran and Turkmenistan in terms of both death and DALY. Pancreatic cancer has a specifically high death rate in Lebanon, Palestine, Bahrain, Qatar, and Kuwait.
In Iran, diarrhea is the 6th cause of death. The first cause of death is stomach cancer, followed by esophageal cancer, cirrhosis, liver cancer, and colorectal cancer. Stomach cancer is the first cause of DALY in Iran as well followed by diarrhea, cirrhosis, and esophageal cancer.
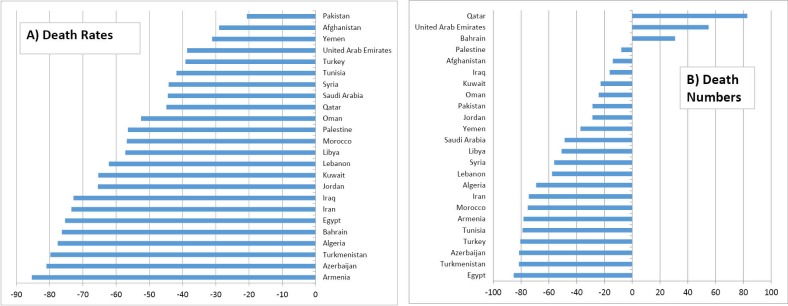
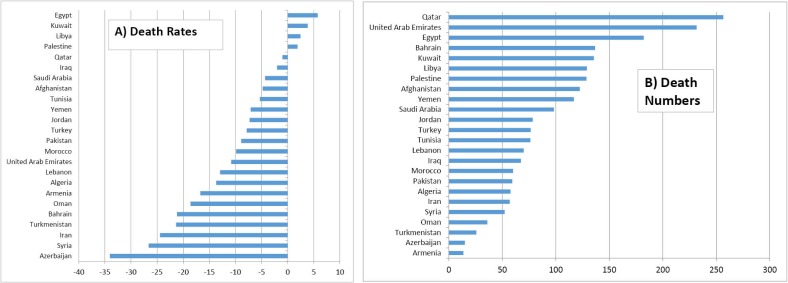
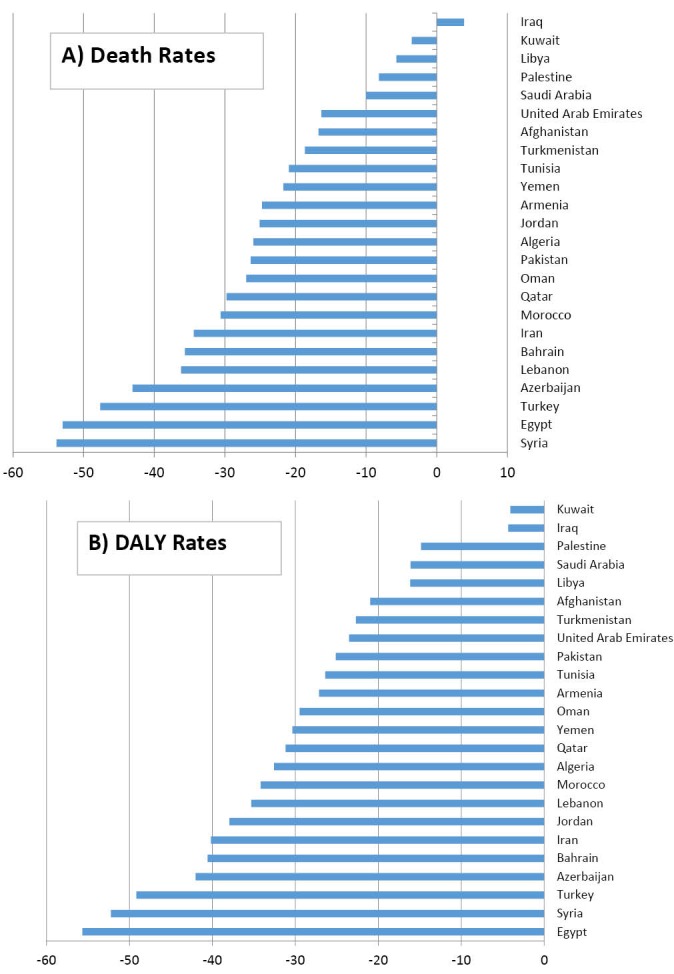
Figures 10 and 11 show the trend of ASRs and number of deaths and DALYs in all ages in 24 countries from 1990 to 2010 for all gastrointestinal and hepatobilliary causes. Figure 12 shows the trend of ASRs and numbers of deaths caused by diarrhea from 1990 to 2010 and figure 13 shows similar estimates for the entire gastrointestinal and pancreatobilliary cancers.
Fig 10 .
Trend of the rate of deaths and DALYs for all gastrointestinal diseases in 24 countries from 1990 to 2010
Fig 11 .
Trend of the number of deaths and DALYs for all gastrointestinal diseases in 24 countries from 1990 to 2010
Fig 12 .
Trends in number and rates of deaths due to diarrhea in 24 countries from 1990 to 2010
Fig 13 .
Trends in number and rates of deaths due to GI and pancreatobilliary cancers in 24 countries from 1990 to 2010
DISSCUTION
The results of GBD study in MENA show that GILDs impose considerable burden on countries in this region. While the ASRs of deaths and DALYs have decreased in almost all countries in the region, the number of deaths and DALYs due to total GILDs shows rises in some countries such as Qatar, United Arab Emirates, Bahrain, Kuwait, and Palestine. These findings show that the increase in numbers may be due to ageing of the population in spite of decreasing ASRs.
The rates and numbers of deaths due to diarrhea have decreased in most countries. For gastrointestinal and hepatobilliary cancers, although the rates of death decreased, the numbers of deaths have increased in all countries. In several countries such as Iran, Turkey, Syria, Kuwait, Lebanon, and Qatar, diarrheal diseases and acute hepatitis have been replaced by gastrointestinal and hepatobilliary malignancies. However, while malignancies impose increasing burden in some countries including Afghanistan, Pakistan, Turkmenistan, Egypt, and Yemen, the burden due to diarrheal diseases and hepatitis is still significant and these countries are suffering from double burden of both communicable and non-communicable GILDs.
Existing evidence shows that diarrheal diseases are still quite common in Afghanistan,10,11 Pakistan,12,13 Yemen14 and Egypt.15 The estimates are specifically made for deaths due to diarrheal diseases among children under 5 years old.13,16-19, There is compelling evidence on effectiveness of improving hygiene including hand washing and sanitation facilities that significantly reduce the incidence and recurrence of diarrheal diseases.20-23 Mothers’ education has a substantial role in the home management of diarrhea in children,24,25 and their health seeking behavior for childhood illnesses.26 Service packages specifically devised for management of diarrhea are demonstrated to be effective in Pakistan, Egypt, and Yemen.14,23,27
There is evidence on high prevalence of hepatitis C (>3.5%) and hepatitis B in MENA region.28,29 However reports about the Maghreb region in Middle East including Algeria, Tunisia, Libya, and Morocco show that the prevalence of hepatitis B and C is low and comparable to developed countries.30 The prevalence of hepatitis C in Maghreb is also low and comparable to developed countries. In contrast, there is abundant evidence on high prevalence of acute hepatitis of all kinds in Egypt and their subsequent progression to cirrhosis and hepatocellular carcinoma. Hepatitis B and C virus infections are major public health concerns in Egypt.31,32 The prevalence of hepatitis C virus in Egypt is the highest in the world. About 14.7% of the population in Egypt are antibody positive and hepatitis C has become a massive epidemic in national level.33,34 Transmission mainly occurs through sexual contact and intravenous drug use.35 Evidence shows that Afghanistan is also facing a high prevalence of hepatitis B and C infection.36,37 Intravenous drug use, unsafe sex, unsafe blood transfusion, and vertical transmission are the main routes of transmission.38-44 Hepatitis B and C infections are prevalent in Pakistan as well and are higher than its neighboring countries such as India and Nepal.45,46 Unlike hepatitis B, as there is no vaccine available to prevent hepatitis C, the primary prevention should be focused on safe blood transfusion, safe sex, and safe injection of drugs.28,47
Chronic hepatitis B and C are the main causes of liver cirrhosis and progression to hepatocellular carcinoma. The results of GBD 2010 show that cirrhosis is among the top four causes of death in all countries in MENA except for Bahrain. The death rate caused by cirrhosis in Egypt is by far the highest in the world, followed by Pakistan, Afghanistan, Yemen, and Morocco.48 Pakistan is specifically experiencing an epidemic of cirrhosis.49 It is estimated that globally, 30% of cirrhosis is attributable to HBV and another 27% is attributable to HCV.50 It is also estimated that mortality due to liver cirrhosis imposes substantial burden worldwide each year, causing more than one million deaths in 2010.48 Its treatment is expensive and unavailable in most parts of the world. Additionally, treatment of cirrhosis does not significantly increase the survival in decompensated forms.51 However, preventive measures such as safe blood transfusion, hygienic health facilities, vaccination for HBV, screening, and general education are inexpensive and cost-effective.47,52-55 Preventive measures are highly recommended at national levels especially in low-income countries to tackle this growing public health concern.
Hepatocellular carcinoma is another complication of chronic hepatitis. It is estimated that 78% of all cases are attributable to either chronic HBV or HCV infections.50 In another report, 55% of global hepatocellular carcinoma is attributed to chronic HBV infection.56 This figure is 89% in endemic regions.56 Pakistan is specifically experiencing a significant rise in hepatocellular carcinoma secondary to HBV and HCV infections.57
Although it may seem that the burden of hepatitis B and C infections may be higher in long-term, the burden of acute hepatitis A and E should not be forgotten either.58-62 Vertical transmission of hepatitis E is not uncommon in Egypt, Afghanistan, and Pakistan.63
Results of GBD 2010 show that 28% of all deaths and 16% of all DALYs due to GILDs are caused by gastrointestinal and hepatobilliary cancers in MENA. Stomach cancer ranks 3rd as a cause of death and 5th as a cause of DALY in the region. It is among top four causes of death in 15 countries and among top four causes of DALY in 12 countries. The rates of stomach cancer are highest in Afghanistan, Iran, and Turkmenistan. Cancer of stomach is followed by liver cancer, colorectal cancer, esophageal cancer, pancreatic cancer, and gall bladder and hepatobilliary cancer in the entire region. Liver cancer is among the top four causes of death in 18 countries and among the top four causes of DALY in 10 countries. Colorectal cancer has the highest rate of death and DALY in Turkey, Tunisia, Lebanon, and Jordan. The lowest rates are seen in Pakistan. Esophageal cancer is among the top four causes of death and DALY only in Turkmenistan and Iran. The results are compatible with global cancer data (GLOBOCAN) in 2012 in which stomach cancer, liver cancer, colorectal cancer, and esophageal cancer accounted for 8.4%, 8.1%, 7.8%, and 4.6% of all incidental cases respectively in less developed countries.64 Globally, all gastrointestinal and hepatobilliary cancers accounted for almost 30% of all incidental cases and 37% of all cancer deaths in 2012 based on GLOBOCAN results.64 Generally speaking, the rates of deaths and DALYs caused by gastrointestinal and hepatobilliary cancers in North African countries are lower than Middle Eastern countries.64-68 In contrast, specifically in countries located in the Caspian Littoral, esophageal and gastric cancers are higher due to genetic and certain life style exposures.69-71 Evidence shows that while esophageal cancer in this area is declining,72 there is a general rise in stomach cancer.73 A large prospective cohort study, the Golestan Cohort Study (GCS) in Golestan province, north east of Iran, has been conducted on over 50,000 Iranians, mostly of Turkmen ethnicity, to investigate the epidemiology and determinants of upper gastrointestinal malignancies in the Caspian Littoral. This study is the largest cohort study in Middle East.74,75 The results of this study have shown that low consumption of fruit and vegetable, very hot tea drinking, life style and other aspects of diet, opium and tobacco use, and poor oral health, along with low socio-economic status are the most likely etiologies of high esophageal cancer rate reported in this region.76-79
Cancer registries are the best existing sources for estimating the prevalence and incidence of major cancers. However, cancer registries in general have two defects: incompleteness and misclassification. Since the first results of national cancer registries were released in 1975, stomach cancer, cancer of the colon and rectum, and esophageal cancer have retained their ranks in the hierarchy of cancers, but there is a steep rise in the prevalence of liver cancer 80-83 in MENA and specifically in Egypt.84,85 Yet, in effect, the cancers of stomach, colon and rectum, and esophagus are underestimated while the liver cancer is overestimated as metastatic cancers of other sites may be misclassified as liver cancer. Expansion and accuracy of population-based cancer registries is a necessity especially in developing countries for more precise estimations of the burden of cancers.86
The unique metrics developed and the novel statistical methods used in GBD have made it possible to make estimations for times and places where data is sparse or is of low quality. GBD has used novel methods to overcome these challenges among which, the scarcity and low quality of hospital data and data in outpatient settings are very bold. There is compelling evidence on increasing trend of GILDs that are regularly diagnosed in outpatient setting and have not been captured by GBD. These include but are not restricted to gastroesophageal reflux disease (GERD),87 inflammatory bowel diseases (IBD),88,89 irritable bowel syndrome (IBS),90,91 non-alcoholic fatty liver disease (NAFLD), and non-alcoholic steatohepatitis (NASH).92
DALYs reported in GBD 2010 show regional heterogeneity in the causes of premature death and disability, which highlights the importance of regular epidemiological assessments for every country in the MENA. To further improve precision of the estimated DALYs, qualitative studies should be done in every region to determine how people define quality of life. Collecting high quality evidence is a necessity for policy makers in developing countries in order to effectively allocate the limited resources for prevention and control.
CONFLICT OF INTERESTS
None.
ACKNOWLEDGEMENTS
This study was supported by grants from Iranian Association of Gastroenterology and Hepatology.
Please cite this paper as:
Sepanlou GS, Malekzadeh F, Delavari F, Naghavi M, Forouzanfar MH, Moradi-Lakeh M, Malekzadeh R, Poustchi H, Pourshams A. Burden of Gastrointestinal and Liver Diseases in Middle East and North Africa: Results of Global Burden of Diseases Study from 1990 to 2010. Middle East J Dig Dis 2015;7:201-215.
References
- 1. Global Status Report on Noncommunicable Diseases. 2011, World Health Organization: Geneva.
- 2.Malekzadeh F, Sepanlou SG, Poustchi H, Naghavi M, Forouzanfar M, Shahraz S. et al. Burden of Gastrointestinal and Liver Diseases in Iran: Estimates Based on the Global Burden of Disease, Injuries, and Risk Factors Study, 2010. Middle East J Dig Dis. 2015;7:138–54. [PMC free article] [PubMed] [Google Scholar]
- 3.Sepanlou SG, Malekezadeh F, Naghavi M, Forouzanfar M, Shahraz S, Moradi-Lakeh M. et al. Trend of Gastrointestinal and Liver Diseases in Iran: Results of the Global Burden of Disease Study, 2010. Middle East J Dig Dis. 2015;7:121–37. [PMC free article] [PubMed] [Google Scholar]
- 4.Murray CJ, Ezzati M, Flaxman AD, Lim S, Lozano R, Michaud C. et al. GBD 2010: design, definitions, and metrics. Lancet. 2012;380:2063–6. doi: 10.1016/S0140-6736(12)61899-6. [DOI] [PubMed] [Google Scholar]
- 5.Wang H, Dwyer-Lindgren L, Lofgren KT, Rajaratnam JK, Marcus JR, Levin-Rector A. et al. Age-specific and sex-specific mortality in 187 countries, 1970-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2071–94. doi: 10.1016/S0140-6736(12)61719-X. [DOI] [PubMed] [Google Scholar]
- 6.Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M. et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2163–96. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Salomon JA, Vos T, Hogan DR, Gagnon M, Naghavi M, Mokdad A. et al. Common values in assessing health outcomes from disease and injury: disability weights measurement study for the Global Burden of Disease Study 2010. Lancet. 2012;380:2129–43. doi: 10.1016/S0140-6736(12)61680-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C. et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2197–223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 9.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V. et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Assefa F, Jabarkhil MZ, Salama P, Spiegel P. Malnutrition and mortality in Kohistan District, Afghanistan, April 2001. JAMA. 2001;286:2723–8. doi: 10.1001/jama.286.21.2723. [DOI] [PubMed] [Google Scholar]
- 11.Choudhry VP, Fazal I, Aram G, Choudhry M, Arya LS, Torpeki MS. Pattern of preventable diseases in Afghanistan: suggestions to reduce the morbidity and mortality at IGICH. Indian Pediatr. 1989;26:654–9. [PubMed] [Google Scholar]
- 12.Rabbani F, Mukhi A, Perveen S, Gul X, Iqbal S, Qazi S. et al. Improving community case management of diarrhoea and pneumonia in district Badin, Pakistan through a cluster randomised study inverted question markthe NIGRAAN trial protocol. Implement Sci. 2014;9:186. doi: 10.1186/s13012-014-0186-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rahman AE, Moinuddin M, Molla M, Worku A, Hurt L, Kirkwood B. et al. Childhood diarrhoeal deaths in seven low- and middle-income countries. Bull World Health Organ. 2014;92:664–71. doi: 10.2471/BLT.13.134809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Al-Hamzi HH, Al-Zubairi LM, Raja’a YA, Al-Dabagh AY, Al-Bayatti NM. Quality of management for acute respiratory tract infections and diarrhoeal diseases in rural Yemen. East Mediterr Health J. 2009;15:1119–25. [PubMed] [Google Scholar]
- 15.Ahmed SF, Shaheen HI, Abdel-Messih IA, Mostafa M, Putnam SD, Kamal KA. et al. The epidemiological and clinical characteristics of diarrhea associated with enteropathogenic, enteroaggregative and diffuse-adherent Escherichia coli in Egyptian children. J Trop Pediatr. 2014;60:397–400. doi: 10.1093/tropej/fmu034. [DOI] [PubMed] [Google Scholar]
- 16.Prasad AN Disease profile of children in Kabul: the unmet need for health care. J Epidemiol Community Health. 2006;60:20–3. doi: 10.1136/jech.2005.040147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Al-Badani A, Al-Areqi L, Majily A, Al-Sallami S, Al-Madhagi A, Amood Al-Kamarany M. Rotavirus Diarrhea among Children in Taiz, Yemen: Prevalence-Risk Factors and Detection of Genotypes. Int J Pediatr. 2014;2014:928529. doi: 10.1155/2014/928529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hershey CL, Doocy S, Anderson J, Haskew C, Spiegel P, Moss WJ. Incidence and risk factors for Malaria, pneumonia and diarrhea in children under 5 in UNHCR refugee camps: A retrospective study. Confl Health. 2011;5:24. doi: 10.1186/1752-1505-5-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ei-Deeb MT, Hamid DH. Growth assessment in Egyptian infants and children with chronic diarrhea. J Egypt Soc Parasitol. 2012;42:605–17. doi: 10.12816/0006344. [DOI] [PubMed] [Google Scholar]
- 20.Aluisio AR, Maroof Z, Chandramohan D, Bruce J, Masher MI, Manaseki-Holland S. et al. Risk factors associated with recurrent diarrheal illnesses among children in Kabul, Afghanistan: a prospective cohort study. PLoS One. 2015;10:e0116342. doi: 10.1371/journal.pone.0116342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Opryszko MC, Majeed SW, Hansen PM, Myers JA, Baba D, Thompson RE. et al. Water and hygiene interventions to reduce diarrhoea in rural Afghanistan: a randomized controlled study. J Water Health. 2010;8:687–702. doi: 10.2166/wh.2010.121. [DOI] [PubMed] [Google Scholar]
- 22.Hassan KE, Mansour A, Shaheen H, Amine M, Riddle MS, Young SY. et al. The impact of household hygiene on the risk of bacterial diarrhea among Egyptian children in rural areas, 2004-2007. J Infect Dev Ctries. 2014;8:1541–51. doi: 10.3855/jidc.4539. [DOI] [PubMed] [Google Scholar]
- 23.Mansour AM, Mohammady HE, Shabrawi ME, Shabaan SY, Zekri MA, Nassar M. et al. Modifiable diarrhoea risk factors in Egyptian children aged <5 years. Epidemiol Infect. 2013;141:2547–59. doi: 10.1017/S0950268813000319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mashal T, Takano T, Nakamura K, Kizuki M, Hemat S, Watanabe M. et al. Factors associated with the health and nutritional status of children under 5 years of age in Afghanistan: family behaviour related to women and past experience of war-related hardships. BMC Public Health. 2008;8:301. doi: 10.1186/1471-2458-8-301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Azim SM, Rahaman MM. Home management of childhood diarrhoea in rural Afghanistan: a study in Urgun, Paktika Province. J Diarrhoeal Dis Res. 1993;11:161–4. [PubMed] [Google Scholar]
- 26.Webair HH, Bin-Gouth AS. Factors affecting health seeking behavior for common childhood illnesses in Yemen. Patient Prefer Adherence. 2013;7:1129–38. doi: 10.2147/PPA.S51124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Habib MA, Soofi S, Sadiq K, Samejo T, Hussain M, Mirani M. et al. A study to evaluate the acceptability, feasibility and impact of packaged interventions (“Diarrhea Pack”) for prevention and treatment of childhood diarrhea in rural Pakistan. BMC Public Health. 2013;13:922. doi: 10.1186/1471-2458-13-922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mohd Hanafiah K, Groeger J, Flaxman AD, Wiersma ST. Global epidemiology of hepatitis C virus infection: new estimates of age-specific antibody to HCV seroprevalence. Hepatology. 2013;57:1333–42. doi: 10.1002/hep.26141. [DOI] [PubMed] [Google Scholar]
- 29.Specialist Panel on Chronic Hepatitis B in the Middle East. A review of chronic hepatitis B epidemiology and management issues in selected countries in the Middle East. J Viral Hepat. 2012;19:9–22. doi: 10.1111/j.1365-2893.2011.01511.x. [DOI] [PubMed] [Google Scholar]
- 30.Fadlalla FA, Mohamoud YA, Mumtaz GR, Abu-Raddad LJ. The epidemiology of hepatitis C virus in the maghreb region: systematic review and meta-analyses. PLoS One. 2015;10:e0121873. doi: 10.1371/journal.pone.0121873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bruggmann P, Berg T, Ovrehus AL, Moreno C, Brandao Mello CE, Roudot-Thoraval F. et al. Historical epidemiology of hepatitis C virus (HCV) in selected countries. J Viral Hepat. 2014;21 Suppl 1:5–33. doi: 10.1111/jvh.12247. [DOI] [PubMed] [Google Scholar]
- 32.Edris A, Nour MO, Zedan OO, Mansour AE, Ghandour AA, Omran T. Seroprevalence and risk factors for hepatitis B and C virus infection in Damietta Governorate, Egypt. East Mediterr Health J. 2014;20:605–13. [PubMed] [Google Scholar]
- 33.Mohamoud YA, Mumtaz GR, Riome S, Miller D, Abu-Raddad LJ. The epidemiology of hepatitis C virus in Egypt: a systematic review and data synthesis. BMC Infect Dis. 2013;13:288. doi: 10.1186/1471-2334-13-288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Waked I, Doss W, El-Sayed MH, Estes C, Razavi H, Shiha G. et al. The current and future disease burden of chronic hepatitis C virus infection in Egypt. Arab J Gastroenterol. 2014;15:45–52. doi: 10.1016/j.ajg.2014.04.003. [DOI] [PubMed] [Google Scholar]
- 35.Mohsen A, Bernier A, LeFouler L, Delarocque-Astagneau E, El-Daly M, El-Kafrawy S. et al. Hepatitis C virus acquisition among Egyptians: analysis of a 10-year surveillance of acute hepatitis C. Trop Med Int Health. 2015;20:89–97. doi: 10.1111/tmi.12410. [DOI] [PubMed] [Google Scholar]
- 36.Attaullah S, Rehman S, Khan S, Ali I, Ali S, Khan SN. Prevalence of hepatitis B virus genotypes in HBsAg positive individuals of Afghanistan. Virol J. 2011;8:281. doi: 10.1186/1743-422X-8-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Khan S, Attaullah S. Share of Afghanistan populace in hepatitis B and hepatitis C infection’s pool: is it worthwhile? Virol J. 2011;8:216. doi: 10.1186/1743-422X-8-216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sanders-Buell E, Rutvisuttinunt W, Todd CS, Nasir A, Bradfield A, Lei E. et al. Hepatitis C genotype distribution and homology among geographically disparate injecting drug users in Afghanistan. J Med Virol. 2013;85:1170–9. doi: 10.1002/jmv.23575. [DOI] [PubMed] [Google Scholar]
- 39.Mansoor GF, Rahmani AM, Kakar MA, Hashimy P, Abrahimi P, Scott PT. et al. Blood supply safety in Afghanistan: a national assessment of high-volume facilities. Transfusion. 2013;53:2061–8. doi: 10.1111/trf.12005. [DOI] [PubMed] [Google Scholar]
- 40.Mansoor GF, Rahmani AM, Kakar MA, Hashimy P, Abrahimi P, Scott PT. et al. A national mapping assessment of blood collection and transfusion service facilities in Afghanistan. Transfusion. 2013;53:69–75. doi: 10.1111/j.1537-2995.2012.03674.x. [DOI] [PubMed] [Google Scholar]
- 41.Nasir A, Todd CS, Stanekzai MR, Bautista CT, Botros BA, Scott PT. et al. Implications of hepatitis C viremia vs antibody alone on transmission among male injecting drug users in three Afghan cities. Int J Infect Dis. 2011;15:e201–5. doi: 10.1016/j.ijid.2010.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nasir A, Todd CS, Stanekzai MR, Bautista CT, Botros BA, Scott PT. et al. Prevalence of HIV, hepatitis B and hepatitis C and associated risk behaviours amongst injecting drug users in three Afghan cities. Int J Drug Policy. 2011;22:145–52. doi: 10.1016/j.drugpo.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Todd CS, Nasir A, Stanekzai MR, Bautista CT, Botros BA, Scott PT. et al. HIV, hepatitis B, and hepatitis C prevalence and associated risk behaviors among female sex workers in three Afghan cities. AIDS. 2010;24 Suppl 2:S69–75. doi: 10.1097/01.aids.0000386736.25296.8d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Todd CS, Ahmadzai M, Atiqzai F, Miller S, Smith JM, Ghazanfar SA. et al. Seroprevalence and correlates of HIV, syphilis, and hepatitis B and C virus among intrapartum patients in Kabul, Afghanistan. BMC Infect Dis. 2008;8:119. doi: 10.1186/1471-2334-8-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Umar M, Bushra HT, Ahmad M, Data A, Khurram M, Usman S. et al. Hepatitis C in Pakistan: a review of available data. Hepat Mon. 2010;10:205–14. [PMC free article] [PubMed] [Google Scholar]
- 46.Ali M, Idrees M, Ali L, Hussain A, Ur Rehman I, Saleem S. et al. Hepatitis B virus in Pakistan: a systematic review of prevalence, risk factors, awareness status and genotypes. Virol J. 2011;8:102. doi: 10.1186/1743-422X-8-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shepard CW, Finelli L, Alter MJ. Global epidemiology of hepatitis C virus infection. Lancet Infect Dis. 2005;5:558–67. doi: 10.1016/S1473-3099(05)70216-4. [DOI] [PubMed] [Google Scholar]
- 48.Mokdad AA, Lopez AD, Shahraz S, Lozano R, Mokdad AH, Stanaway J. et al. Liver cirrhosis mortality in 187 countries between 1980 and 2010: a systematic analysis. BMC Med. 2014;12:145. doi: 10.1186/s12916-014-0145-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ahmad K. Pakistan:a cirrhotic state? Lancet. 2004;364:1843–4. doi: 10.1016/S0140-6736(04)17458-8. [DOI] [PubMed] [Google Scholar]
- 50.Perz JF, Armstrong GL, Farrington LA, Hutin YJ, Bell BP. The contributions of hepatitis B virus and hepatitis C virus infections to cirrhosis and primary liver cancer worldwide. J Hepatol. 2006;45:529–38. doi: 10.1016/j.jhep.2006.05.013. [DOI] [PubMed] [Google Scholar]
- 51.Gluud C. Mortality from cirrhosis: lack of progress over the last 35 years. Gut. 2005;54:1523–6. doi: 10.1136/gut.2005.072876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Huang LM, Lu CY, Chen DS. Hepatitis B virus infection, its sequelae, and prevention by vaccination. Curr Opin Immunol. 2011;23:237–43. doi: 10.1016/j.coi.2010.12.013. [DOI] [PubMed] [Google Scholar]
- 53.Schillie SF, Murphy TV. Seroprotection after recombinant hepatitis B vaccination among newborn infants: a review. Vaccine. 2013;31:2506–16. doi: 10.1016/j.vaccine.2012.12.012. [DOI] [PubMed] [Google Scholar]
- 54.Bosetti C, Levi F, Lucchini F, Zatonski WA, Negri E, La Vecchia C. Worldwide mortality from cirrhosis: an update to 2002. J Hepatol. 2007;46:827–39. doi: 10.1016/j.jhep.2007.01.025. [DOI] [PubMed] [Google Scholar]
- 55.Kim DD, Hutton DW, Raouf AA, Salama M, Hablas A, Seifeldin IA. et al. Cost-effectiveness model for hepatitis C screening and treatment: Implications for Egypt and other countries with high prevalence. Glob Public Health. 2015;10:296–317. doi: 10.1080/17441692.2014.984742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kew MC. Epidemiology of chronic hepatitis B virus infection, hepatocellular carcinoma, and hepatitis B virus-induced hepatocellular carcinoma. Pathol Biol (Paris) 2010;58:273–7. doi: 10.1016/j.patbio.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 57.Butt AS, Hamid S, Wadalawala AA, Ghufran M, Javed AA, Farooq O. et al. Hepatocellular carcinoma in Native South Asian Pakistani population; trends, clinico-pathological characteristics & differences in viral marker negative & viral-hepatocellular carcinoma. BMC Res Notes. 2013;6:137. doi: 10.1186/1756-0500-6-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Asghar RJ. Hepatitis A and E: not to be forgotten. East Mediterr Health J. 2014;20:212–3. [PubMed] [Google Scholar]
- 59.Carmoi T, Safiullah S, Nicand E. Risk of enterically transmitted hepatitis A, hepatitis E, and Plasmodium falciparum malaria in Afghanistan. Clin Infect Dis. 2009;48:1800. doi: 10.1086/599231. [DOI] [PubMed] [Google Scholar]
- 60.Sridhar S, Lau SK, Woo PC. Hepatitis E: A disease of reemerging importance. J Formos Med Assoc. 2015;114:681–90. doi: 10.1016/j.jfma.2015.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Itani T, Jacobsen KH, Nguyen T, Wiktor SZ. A new method for imputing country-level estimates of hepatitis A virus endemicity levels in the Eastern Mediterranean region. Vaccine. 2014;32:6067–74. doi: 10.1016/j.vaccine.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 62.Melhem NM, Talhouk R, Rachidi H, Ramia S. Hepatitis A virus in the Middle East and North Africa region: a new challenge. J Viral Hepat. 2014;21:605–15. doi: 10.1111/jvh.12282. [DOI] [PubMed] [Google Scholar]
- 63.El Sayed Zaki M, El Aal AA, Badawy A, El-Deeb DR, El-Kheir NY. Clinicolaboratory study of mother-to-neonate transmission of hepatitis E virus in Egypt. Am J Clin Pathol. 2013;140:721–6. doi: 10.1309/AJCPT55TDMJNPLLV. [DOI] [PubMed] [Google Scholar]
- 64.Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M. et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–86. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 65.Bray F, Ren JS, Masuyer E, Ferlay J. Global estimates of cancer prevalence for 27 sites in the adult population in 2008. Int J Cancer. 2013;132:1133–45. doi: 10.1002/ijc.27711. [DOI] [PubMed] [Google Scholar]
- 66.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 67.Salim EI, Moore MA, Al-Lawati JA, Al-Sayyad J, Bazawir A, Bener A. et al. Cancer epidemiology and control in the arab world - past, present and future. Asian Pac J Cancer Prev. 2009;10:3–16. [PubMed] [Google Scholar]
- 68.Salim EI, Moore MA, Bener A, Habib OS, Seif-Eldin IA, Sobue T. Cancer epidemiology in South-West Asia - past, present and future. Asian Pac J Cancer Prev. 2010;11 Suppl 2:33–48. [PubMed] [Google Scholar]
- 69.Kmet J, Mahboubi E. Esophageal cancer in the Caspian littoral of Iran: initial studies. Science. 1972;175:846–53. doi: 10.1126/science.175.4024.846. [DOI] [PubMed] [Google Scholar]
- 70.Mahboubi E, Kmet J, Cook PJ, Day NE, Ghadirian P, Salmasizadeh S. Oesophageal cancer studies in the Caspian Littoral of Iran: the Caspian cancer registry. Br J Cancer. 1973;28:197–214. doi: 10.1038/bjc.1973.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Akbari MR, Malekzadeh R, Nasrollahzadeh D, Amanian D, Sun P, Islami F. et al. Familial risks of esophageal cancer among the Turkmen population of the Caspian littoral of Iran. Int J Cancer. 2006;119:1047–51. doi: 10.1002/ijc.21906. [DOI] [PubMed] [Google Scholar]
- 72.Semnani S, Sadjadi A, Fahimi S, Nouraie M, Naeimi M, Kabir J. et al. Declining incidence of esophageal cancer in the Turkmen Plain, eastern part of the Caspian Littoral of Iran: a retrospective cancer surveillance. Cancer Detect Prev. 2006;30:14–9. doi: 10.1016/j.cdp.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 73.Babaei M, Pourfarzi F, Yazdanbod A, Chiniforush MM, Derakhshan MH, Mousavi SM. et al. Gastric cancer in Ardabil, Iran--a review and update on cancer registry data. Asian Pac J Cancer Prev. 2010;11:595–9. [PubMed] [Google Scholar]
- 74.Sepanlou SG, Etemadi A, Kamangar F, Sepehr A, Pourshams A, Poustchi H. et al. The gastro-esophageal malignancies in Northern Iran research project: impact on the health research and health care systems in Iran. Arch Iran Med. 2013;16:46–53. [PMC free article] [PubMed] [Google Scholar]
- 75.Pourshams A, Khademi H, Malekshah AF, Islami F, Nouraei M, Sadjadi AR. et al. Cohort Profile: The Golestan Cohort Study--a prospective study of oesophageal cancer in northern Iran. Int J Epidemiol. 2010;39:52–9. doi: 10.1093/ije/dyp161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Islami F, Kamangar F, Aghcheli K, Fahimi S, Semnani S, Taghavi N. et al. Epidemiologic features of upper gastrointestinal tract cancers in Northeastern Iran. Br J Cancer. 2004;90:1402–6. doi: 10.1038/sj.bjc.6601737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Islami F, Pourshams A, Nasrollahzadeh D, Kamangar F, Fahimi S, Shakeri R. et al. Tea drinking habits and oesophageal cancer in a high risk area in northern Iran: population based case-control study. BMJ. 2009;338:b929. doi: 10.1136/bmj.b929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Pourfarzi F, Whelan A, Kaldor J, Malekzadeh R. The role of diet and other environmental factors in the causation of gastric cancer in Iran--a population based study. Int J Cancer. 2009;125:1953–60. doi: 10.1002/ijc.24499. [DOI] [PubMed] [Google Scholar]
- 79.Islami F, Kamangar F, Nasrollahzadeh D, Aghcheli K, Sotoudeh M, Abedi-Ardekani B. et al. Socio-economic status and oesophageal cancer: results from a population-based case-control study in a high-risk area. Int J Epidemiol. 2009;38:978–88. doi: 10.1093/ije/dyp195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Parkin DM, Laara E, Muir CS. Estimates of the worldwide frequency of sixteen major cancers in 1980. Int J Cancer. 1988;41:184–97. doi: 10.1002/ijc.2910410205. [DOI] [PubMed] [Google Scholar]
- 81.Parkin DM, Stjernsward J, Muir CS. Estimates of the worldwide frequency of twelve major cancers. Bull World Health Organ. 1984;62:163–82. [PMC free article] [PubMed] [Google Scholar]
- 82.Parkin DM, Bray FI, Devesa SS. Cancer burden in the year 2000 The global picture. Eur J Cancer. 2001;37 Suppl 8:S4–66. doi: 10.1016/s0959-8049(01)00267-2. [DOI] [PubMed] [Google Scholar]
- 83.Parkin DM. Global cancer statistics in the year 2000. Lancet Oncol. 2001;2:533–43. doi: 10.1016/S1470-2045(01)00486-7. [DOI] [PubMed] [Google Scholar]
- 84.Abdel-Hamid M, El-Daly M, Molnegren V, El-Kafrawy S, Abdel-Latif S, Esmat G. et al. Genetic diversity in hepatitis C virus in Egypt and possible association with hepatocellular carcinoma. J Gen Virol. 2007;88:1526–31. doi: 10.1099/vir.0.82626-0. [DOI] [PubMed] [Google Scholar]
- 85.Abdel-Wahab M, El-Ghawalby N, Mostafa M, Sultan A, El-Sadany M, Fathy O. et al. Epidemiology of hepatocellular carcinoma in lower Egypt, Mansoura Gastroenterology Center. Hepatogastroenterology. 2007;54:157–62. [PubMed] [Google Scholar]
- 86.Parkin DM. The evolution of the population-based cancer registry. Nat Rev Cancer. 2006;6:603–12. doi: 10.1038/nrc1948. [DOI] [PubMed] [Google Scholar]
- 87.El-Serag HB, Sweet S, Winchester CC, Dent J. Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2014;63:871–80. doi: 10.1136/gutjnl-2012-304269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Nasseri-Moghaddam S. Inflammatory bowel disease. Middle East J Dig Dis. 2012;4:77–89. [PMC free article] [PubMed] [Google Scholar]
- 89.Farrukh A, Mayberry JF. Epidemiology of inflammatory bowel disease in the Middle East--an opportune time. Arab J Gastroenterol. 2014;15:163–5. doi: 10.1016/j.ajg.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 90.Chey WD, Kurlander J, Eswaran S. Irritable bowel syndrome: a clinical review. JAMA. 2015;313:949–58. doi: 10.1001/jama.2015.0954. [DOI] [PubMed] [Google Scholar]
- 91.Nellesen D, Yee K, Chawla A, Lewis BE, Carson RT. A systematic review of the economic and humanistic burden of illness in irritable bowel syndrome and chronic constipation. J Manag Care Pharm. 2013;19:755–64. doi: 10.18553/jmcp.2013.19.9.755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.LaBrecque DR, Abbas Z, Anania F, Ferenci P, Khan AG, Goh KL. et al. World Gastroenterology Organisation global guidelines: Nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. J Clin Gastroenterol. 2014;48:467–73. doi: 10.1097/MCG.0000000000000116. [DOI] [PubMed] [Google Scholar]