Abstract
Background
HIV infection is problematic among all drug users, not only injection drug users. Drug users are at risk for contracting HIV by engaging in risky sexual behaviors.
Objective
The present study sought to determine whether inhibitory processes moderate the relationship between problematic drug use and HIV-risk behaviors (unprotected sex and multiple sex partners).
Methods
One hundred ninety-six drug offenders enrolled in drug education programs were administered a battery of computer-based assessments. Measures included a cued go/no-go assessment of inhibitory processes, the Drug Abuse Screening Test (DAST) assessment of problematic drug use, and self-report assessment of condom use and multiple sex partners.
Results
Findings revealed that response inhibition assessed by the proportion of false alarms on the cued go/no-go moderated the relationship between problematic drug use and an important measure of HIV risk (condom nonuse) among drug offenders. However, response inhibition did not moderate the relationship between problematic drug use and another measure of HIV risk: multiple sex partners.
Conclusions
Among this sample of drug offenders, we have found a relationship between problematic drug use and condom nonuse, which is exacerbated by poor control of inhibition. These findings have implications for the development of HIV intervention components among high-risk populations.
Keywords: DAST, drug users, cued go/no-go, risky sex, HIV-risk, impulsivity, inhibition
INTRODUCTION
Inhibitory Control Processes, Drug use, and HIV-risk Behaviors
HIV rates continue to rise with over 1.1 million people infected in the United States as of 2010, approximately 18% of whom are unaware that they are HIV-positive (Centers for Disease Control and Prevention, 2012). HIV infection is high among all drug users, not only injection drug users (Des Jarlais et al., 2007). In addition to sharing needles, drug users are more likely to engage in risky sexual behaviors that are known to transmit HIV (Kalichman, Cain, Zweben, & Swain, 2003; Leigh, Ames, & Stacy, 2008; Stacy, Ames, Ullman, Zogg, & Leigh, 2006).
Several studies found drug use to be associated with risky sexual behaviors, subsequently leading to increased risk of contracting sexually transmitted diseases (STDs) and higher HIV contraction rates (Des Jarlais et al., 2007; Hwang et al., 2000; Ross, Hwang, Zack, Bull, & Williams, 2002). Kirisci et al. (2006) expanded upon these studies by investigating the severity of a drug use disorder or dependence and its relationship to risky sex. Kirisci and colleagues found severity to be positively related to engaging in risky sexual behaviors. One of the most commonly used measures of problematic drug use is the self-report Drug Abuse Screening Test (DAST; Hormes, Coffey, Drobes, & Saladin, 2011; Mdege & Lang, 2011; Webster, Dickson, Duvall, & Clark, 2010; Yudko, Lozhkina, & Fouts, 2007). The DAST has been shown to be associated with risky sexual behaviors (Kalichman & Cain, 2004; Senn, Carey, Vanable, Coury-Doniger, & Urban, 2006) leading to increased risk of contracting HIV (Ellickson, Collins, Bogart, Klein, & Taylor, 2005).
Inhibitory Control Processes
Lack of inhibitory control or impulsive tendencies involves action without planning, forethought, or conscious judgment and the inclination to engage in inappropriate or maladaptive behaviors (de Wit, 2008; Kjome et al., 2010). The loss of inhibitory control with regard to rewarding or distracting stimuli (Ersche, Turton, Pradhan, Bullmore, & Robbins, 2010) also plays a role in risky sexual behaviors, such that impulsive individuals have been found to more likely engage in sex without using a condom (Abbey, Saenz, & Buck, 2005; Donohew et al., 2000; Xiao, Palmgreen, Zimmerman, & Noar, 2010) and to have more sexual partners (Donohew et al., 2000). One study found that among adolescents using alcohol before sex, those who were more impulsive were more likely to participate in risky sex (Donohew et al., 2000). The relationship found in this study is suggestive of a potential interaction effect between alcohol (or other drug use) and impulsive tendencies, though such an interaction was not formally tested.
The other side of the same coin is response inhibition, which is the ability to control one’s actions across a range of situations. Preventing acting out impulsive tendencies requires inhibitory control, often defined as the deliberate blocking of inappropriate or unwanted actions (Mostofsky & Simmonds, 2008). The go/no-go task is one of the most frequently used measures of response inhibition and impulsivity (Roberts & Garavan, 2010; Völlm et al., 2010; Weafer, Fillmore, & Milich, 2009; see Simmonds, Pekar, & Mostofsky, 2008 for meta-analysis of neural correlates of go/no-go tasks). Cocaine-dependent individuals (as measured by the DAST) were significantly less likely to refrain from inhibiting their behavioral response to a stop-signal used in a go/no-go task than the nondrug-dependent control group (Fillmore & Rush, 2002). Fillmore and Rush (2006) found that simultaneous cocaine and alcohol users showed greater inhibition impairment and were more impulsive than those who had no history of drug abuse, as revealed on a cued go/no-go task. Research on the go/no-go task may be particularly important because it assesses performance ability, rather than relying on self-report measures of inhibitory processes or impulsive tendencies (Reynolds, Ortengren, Richards, & de Wit, 2006). Thus, the task appears to reflect a general ability that may have wide application.
Semple, Zians, Grant, and Patterson (2006) conducted a study investigating self-reported impulsivity as a moderator of effects of methamphetamine use on unprotected sex among HIV-positive men who have sex with men (MSM). Among participants with higher levels of impulsivity, the relationship between methamphetamine use intensity and unprotected sex was strongest (Semple et al., 2006). However, methamphetamine was the only type of drug investigated. Thus, it is important to determine if this finding holds across drug use problems in general.
The research, just summarized, suggests that there are a variety of concepts and measures in the domain of inhibitory control and impulsivity that relate to risky sexual behavior and drug use. Investigators have also uncovered synergistic (interactive) effects between other neurocognitive functions and spontaneous sex associations in drug users promoting risky sexual behaviors (see Ames, Grenard, & Stacy, 2012; Grenard, Ames, & Stacy, 2013) as well as inhibition/impulsivity and drug use. However, it is not yet clear whether performance measures of general inhibitory control, revealed on the go/no-go task, interact with drug problems in predicting risky sex. Investigating this possibility will expand our understanding of the generality of inhibitory effects on risky behavior.
Hypotheses
This study examined inhibitory control ability and its effect on the relationship between problematic drug use and risky sex. Specifically, we hypothesized that increased problems with drug use would be related to increased condom nonuse and this relationship would be moderated (exacerbated) by lack of inhibitory control. In addition, we hypothesized that a positive relationship between problematic drug use and sex with multiple partners would be moderated (exacerbated) by lack of inhibitory control.
METHODS
Participants
Adults enrolled in drug diversion/education programs in Southern California between 2009 and 2010 were recruited for this study. These programs provide services for convicted drug offenders in lieu of jail time. Four hundred ninety clients agreed to participate in the assessment. Eligibility criteria included having attended court-mandated outpatient drug treatment, being a minimum of 18 years, and demonstrating linguistic competence in English. During the computer-based assessment, participants were randomly assigned to complete either a cued go/no-go task or another task not within the scope of the present article. The sample for this study included 196 drug diversion clients with a mean age of 31.18 (SD = 11.40), 66.84% were male, 55.10% self-described as Hispanic, and 85.57% reported high English acculturation where 63.18% communicated only in English and 23.20% communicated in English more than any other language (see Table 1).
TABLE 1.
Descriptive statistics (n = 196)
| Item | M | SD |
|---|---|---|
| Age in years | 31.26 | 11.60 |
| Sex, n (%) | ||
| Male | 131 (66.84%) | |
| Female | 63 (32.14%) | |
| Missing | 2 (1.2%) | |
| Ethnicity, n (%) | ||
| Hispanic | 108 (55.10%) | |
| Non-Hispanic | 82 (41.84%) | |
| Missing | 6 (3.06%) | |
| Acculturation, weighted%a | 85.57% | |
| English only | 63.18% | |
| English more than another language | 23.20% | |
| Go/No-Go | .06 | .08 |
| DAST | 4.83 | 2.90 |
| Condom nonuse | 14.96 | 8.20 |
| Multiple sex partners | 12.78 | 9.72 |
Four acculturation questions were compiled and the weighted percentages for all questions is presented.
Procedures
Administrators from drug diversion/education programs in the metropolitan Los Angeles area approved the study in advance, allowing data collectors to administer the computer-based assessments to clients in a room at the programs’ facilities. Laptop computers were set up before clients arrived. Once all of the clients were seated, data collectors distributed an informed consent form, and it was dictated aloud. Clients were assured that their assessments were completely anonymous, and that a Certificate of Confidentiality from the National Institutes of Health was issued for the study so that the researchers would not be forced to disclose the data to law enforcement or other government agencies. Verbal consent was obtained from participants prior to beginning the self-administered computer-based assessments. The assessments took between 60 and 90 minutes to complete and participants were compensated $15 for their time and effort in completing the assessments. The University’s Institutional Review Board approved all procedures.
Measures
Cued Go/No-Go
The cued go/no-go task used in this study was based on the work of Fillmore, Marczinski, and Bowman (2005) and consisted of two types of stimuli trials: during “go” trials, participants were instructed to react as rapidly as possible to stimuli presented on the computer screen (e.g. press the “/” key in response to a green rectangle stimulus) and withhold a response to “no-go” trials (e.g. inhibit a response to a blue rectangle stimulus), without making mistakes (see Fillmore et al., 2005; Simmonds et al., 2008; Weafer et al., 2009). The go/no-go task taps into basic inhibitory processes or the ability to suppress a prepotent response. All subjects completed 200 trials, 80% of which were “go” trials and 20% were “no-go” trials. The outcome measure used for the present analyses was the proportion of false alarms or the failure to withhold a key-press response for a no-go stimulus (for review see Marczinski & Fillmore, 2003; Weafer et al., 2009).
Drug Abuse Screening Test (DAST-10)
The DAST (Skinner, 1982) measures problems related to drug abuse and dependence. The DAST-10 consists of 10 items from the original DAST measure that quantify level of problems with drugs. Participants respond “yes” or “no” to a range of items; for example, “Are you unable to stop using drugs when you want to?” Higher scores are indicative of increased problems with drug use within the past year (scores range from 0 to 10). Previous studies have found the DAST-10 to have high internal validity (alphas across studies = .86 to .94), strong criterion validity (r = .31 to .39), and strong construct validity (r = .40; Yudko et al., 2007). The internal consistency was very good in the current study (alpha = .80).
Condom Use
A total of 14 items assessed condom use behaviors. Three items measured frequency of condom use with regular partners, casual partners, and exchange partners with responses on a five-point Likert scale ranging from “every time” to “never” (alpha = .73; Darke Hall, Heather, Ward, & Wodak, 1991; DiFranceisco, McAuliffe, & Sikkema, 1998). The next three-item scale measured how often participants used condoms during vaginal, anal, and oral sex on a five-point Likert scale ranging from “used a condom all the time” to “never used a condom” (Donenberg, Emerson, Bryant, Wilson, & Weber-Shifrin, 2001). The last scale consisting of eight items asking about condom use within the past 4 months across different situations such as “with someone you have never had sex with before” and “with someone you know had other sexual partners.” Responses were measured on a five-point Likert scale and ranged from “always” to “never” (Donenberg et al., 2001). Scores from all three scales were compiled into one single 14-item scale of condom use, with higher scores indicating not using condoms. The internal consistency across the 14 items was excellent (alpha = .89).
Multiple Sex Partners
A five-item measure was used (Reilly & Woo, 2001; Richardson et al., 2004) in which participants reported the frequency of their sex partners within the past 4 months by answering the following questions: (1) “How many sexual partners have you had?” (2) “How many new sexual partners have you had?” (3) “How many casual sexual partners have you had?” (4) “How many people have you had sex with on the same day you first met them?,” and (5) “How many one-night stands have you had?.” Participants answered on a scale from 0 to 6 or more and responses were compiled for a total score ranging from 0 to 30. The internal consistency was excellent (alpha = .88).
Acculturation
A four-item language-based proxy was used to measure acculturation (Marin, Sabogal, Marin, Otero-Sabogal, & Perez-Stable, 1987). The questions asked about use of the English language in general, at home, with friends, and selected media. For acculturation, the items were reverse coded and scored on a five-point Likert scale ranging from “only English” to “only another language (not English).” Higher scores indicate more use of English. The internal consistency was excellent (alpha = .88).
Data Analysis
Analytic procedures consisted of general linear regression models using SAS® software Version 9.3 (SAS Institute Inc., 2011) to evaluate main and interaction effects. All models evaluated included the following covariates: gender, ethnicity, acculturation, and age. Continuous variables were centered on their means before the regression models were analyzed. Consistent with recommendations for continuous variable interactions (Cohen, Cohen, West, & Aiken, 2003), the interaction term in the analysis consisted of the product of the centered mean scores on the DAST and the centered mean proportion of failed inhibitory responses (false alarms on the go/no-go task). The dependent variables, condom nonuse, and multiple sex partners were regressed on main effects predictors first and then the interaction term. Missing data were handled using multiple imputation (n = 40) under the normal model to avoid variance lost (Graham, 2009).
RESULTS
Participant Characteristics
See Table 1 for participant characteristics. The mean DAST score for participants was 4.83 (SD = 2.89) and the mean proportion of failed inhibited responses or false alarms to the cued go/no-go task was .06 (SD = .08).
Interaction Models
Residuals were normally distributed for the interaction effect on condom nonuse. The interaction term was significant in the regression model for condom nonuse (B = 9.63, p = .004). Residuals were not normally distributed on number of sex partners. Because of the assumption violation, robust regression employing least trimmed squares estimation (Cohen et al., 2003) was used for the interaction effect on number of sex partners. In this model, the interaction term was nonsignificant for number of sex partners (B = .61, p = .76). Both model parameters are described below and are shown in Table 2.1
TABLE 2.
Regression models
| Variable | B | 95% CI | t | P | Cumulative R2 |
|---|---|---|---|---|---|
| Condom nonuse model | |||||
| Intercept | 13.664 | 11.18–16.15 | 10.78 | <.001 | |
| Sex (1 = female, 0 = male) | −.954 | −3.31–1.340 | −.79 | .427 | |
| Ethnicity (1 = Hispanic, 0 = other) | 2.214 | −.29–4.72 | 1.73 | .083 | |
| Language acculturation | .138 | −.24–.51 | .72 | .472 | |
| Age | .097 | −.01–.20 | 1.82 | .069 | .0241 |
| DAST | .978 | .57–1.38 | 4.72 | <.001 | .1072 |
| Go/No-Go | −16.071 | −32.34–.19 | −1.94 | .053 | .1074 |
| DAST X Go/No-Go | 9.626 | 3.07–16.19 | 2.88 | <.001 | .1431 |
| Multiple sex partners model (Robust LTS estimation) | |||||
| Intercept | 9.291 | 6.063–12.519 | 5.64 | <.001 | |
| Sex (1 = female, 0 = male) | 3.980 | .877–7.084 | 2.51 | .012 | |
| Ethnicity (1 = Hispanic, 0 = other) | −1.074 | −2.208–4.356 | .64 | .521 | |
| Language acculturation | .690 | .207–1.172 | 2.80 | .005 | |
| Age | −.064 | −.202–.074 | −0.91 | .363 | .0922 |
| DAST | .279 | −.252–.811 | 1.03 | .303 | .0992 |
| Go/No-Go | 7.026 | −14.352–28.404 | .64 | .520 | .1015 |
| DAST X Go/No-Go | −.052 | −8.547–8.651 | .01 | .991 | .1053 |
Note. Continuous predictor variables were centered on their means to obtain the (nonstandardized) parameter estimates (B); LTS = Least Trimmed Squares. Supplemental analyses evaluated gender by DAST scores, gender by go/no-go false alarms, and a three-way interaction analysis evaluated gender by DAST score by go/no-go false alarms. Results of these analyses were similar to the two-way interaction models and no interactions by gender were significant.
Covariates and Main Effects
Gender, ethnicity, acculturation, and age were not significant predictors of condom nonuse (all ps > .05). Response inhibition as measured by the cued go/no-go trended toward significance in the prediction of condom nonuse (B = −16.07, p = .0528). Both the DAST (B = .98, p < .0001) and the interaction term (B = 9.63, p = .004) were significant predictors of condom nonuse. The overall model accounted for 14.31% of the variance and the interaction term accounted for 3.57% of the variance in condom nonuse. The relationship between the DAST (x-axis) and condom nonuse (y-axis) moderated by response inhibition is shown in Figure 1. The slopes increase with increasing response disinhibition scores showing the relationship to be stronger between substance abuse and condom nonuse among those participants with more false alarms or greater inhibition errors than among those with more inhibitory control.
FIGURE 1.
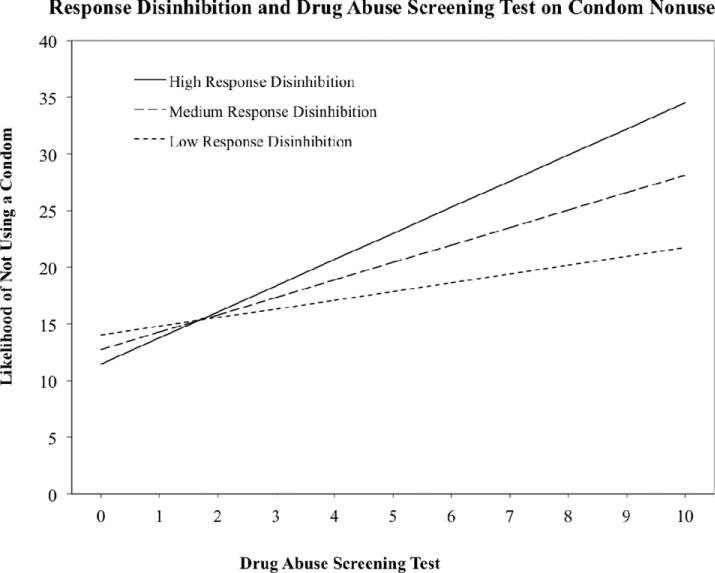
Plot of the interactions between cued go/no-go and DAST in the prediction of the likelihood of not using a condom. The cued go/no-go is plotted at the mean (medium response disinhibition), the mean plus 1 SD (high response disinhibition), and the mean minus 1 SD (low response disinhibition).
Gender, ethnicity, acculturation, DAST, response inhibition as measured by the cued go/no-go, and the interaction term were not significant predictors of multiple sex partners. The only significant predictors were gender and language acculturation (both ps < .05). The overall model accounted for 10.53% of the variance.
DISCUSSION
This study evaluated the relationship between problematic drug use and risky sexual behaviors as moderated by inhibitory control or impulsive tendencies. As hypothesized, the relationship between problematic drug use and condom nonuse was stronger among those drug offenders with less inhibitory control. Both first order and interaction terms were significant (see Figure 1). The model evaluated here explained 14.31% of the variance for condom nonuse. Although the variance explained by the interaction term was small, this is not unusual in moderated relationships in field studies (Grenard et al., 2008; McClelland & Judd, 1993). Field studies often provide nonoptimal distributions influencing the residual variance leading to lower power. In addition, key predictor variables (e.g. DAST and go/no-go) are already entered in the model to evaluate first-order effects, thus influencing the effect size (McClelland & Judd, 1993). The interaction effect found in this study is consistent with one study in which impulsivity was found to moderate the relationship between methamphetamine use and unprotected sex among HIV-positive MSM (Semple et al., 2006). Contrary to our hypothesis, impulsive tendencies did not moderate the relationship between drug abuse problems and multiple sex partners.
There are several implications of these findings. Although drug users with higher levels of drug abuse are at risk for failure to use condoms, this risk from drug abuse is elevated even further for those with poorer inhibitory control. Response inhibition was not a significant predictor by itself, though it showed a trend toward significance. Its relevance only appeared in its interaction effect with drug problems. In other words, drug problems and poorer response inhibition acted in concert to enhance each other’s effects. On the basis of the analytic strategy and pattern of findings, it is reasonable to consider either response inhibition or drug problems as a moderator of the first-order effect of the other variable in the interaction: drug problems and inhibitory control appear to operate synergistically.
Future research needs to replicate these findings due to the lack of studies conducted in this area, and prospective studies are particularly needed to see if these relationships replicate longitudinally. However, the present study was a reasonable first step in exploring the interactions between inhibitory control ability and drug abuse. Clearly, intervention in this population should take both problematic drug use and disinhibition into account. Those most at risk for engaging in unprotected sex have more problematic drug use and are highly impulsive. Future research might consider addressing problematic drug use and impulsivity to potentially improve the prevention of HIV transmission among drug users. Timely intervention on problematic drug use is particularly important because of its exacerbating effect on impulsive tendencies. One should consider screening drug users for impulsivity, and interventions may need to be specifically tailored for highly impulsive individuals. By definition, impulsive individuals often do not use forethought or consider consequences; therefore interventions emphasizing those elements may not be successful for these individuals. Instead, interventionists should identify safe activities that can be incorporated into sexual situations that are novel and exciting to the individual, and ones which could become habitual enough to avoid reliance on forethought or deliberation. Tailoring interventions to personality traits such as impulsivity has been successful in reducing drug and alcohol use in other populations (Conrod, Castellanos-Ryan, & Mackie, 2011; Conrod, Castellanos-Ryan, & Strang, 2010; O’Leary-Barrett, Mackie, Castellanos-Ryan, Al-Khudhairy, & Conrod, 2010).
There are several limitations to this study. Due to the sensitive nature of drug use and sexual behavior, there is the possibility that some participants underestimated the number of sexual partners they have had or overestimated condom use. Even though the interaction of impulsivity and drug use problems on condom nonuse was significant, the effect could have been attenuated if these inaccuracies occurred. Attenuation is the most likely bias of inaccuracies because of concomitant decreased variation in responses. Furthermore, this study was cross-sectional and our inferences are suggestive rather than causal. Therefore, caution is necessary when drawing conclusions from cross-sectional data. While the literature supports these inferences, a carefully controlled longitudinal study should be conducted to confirm our findings.
Although the current study focused on a central hypothesis, other pathways from drug use to unsafe sexual behavior are possible. These include, but are not limited to, transactional sex (Jenness et al., 2011) and impairment under the influence of alcohol or various types of drugs (Leigh, 2002; Leigh et al., 2008). Further, it is likely that condom nonuse can frequently be a deliberate choice due to having a long-term main partner rather than an effect of impulsivity. Future studies might investigate the relationship between other possible pathways, the role of monogamous-relationship status, and additional effects of the role of impulsivity on unsafe sexual behavior.
CONCLUSIONS
In conclusion, we have documented a relationship between problematic drug use and condom nonuse, which is exacerbated by poor control of inhibition. These findings are the first to identify this relationship among drug users and are important for the development of HIV interventions among this high-risk population.
Biographies

Liesl A. Nydegger received her M.P.H. in 2011 and is a doctoral student at Claremont Graduate University in the School of Community and Global Health. Her current research interests include HIV prevention among vulnerable populations including adolescent and adult substance users, abuse survivors, rural South African adolescents, and other international populations. In addition, her work has focused on the development of web-based interventions and intimate partner violence prevention. She has published several peer-reviewed articles related to this research and has led several intervention and epidemiologic projects on HIV risk.

Dr. Susan L. Ames received her Ph.D. in Preventive Medicine from the Keck School of Medicine at the University of Southern California. She has conducted a variety of studies that focus on associative (habit-based) memory processes and dual process models of appetitive behaviors among adolescents and other at-risk populations. She has been influential in linking basic neurocognitive findings to cognitive assessment in addiction and contributed to methodological developments in neurocognitive assessment, including increasing understanding of neural processes underlying automatic implicit associations and control mechanisms in substance use and eating-related behaviors in adolescents and emerging adults.

Dr. Alan W. Stacy’s research translates compelling but rarely applied basic research in cognitive neuroscience and memory systems for use in preventive medicine and allied areas. He was one of the first to apply basic research on memory systems and implicit (automatic) cognition to appetitive habits relevant to addiction, HIV risk behavior, and diet. He has published major reviews of this literature (e.g., Annual Review of Clinical Psychology, Stacy & Wiers, 2010; Current Directions in Psychological Science, Wiers & Stacy, 2006) that help explain why some people engage in nonoptimal, risky appetitive behavior even when they have sufficient knowledge of the risks.

Dr. Jerry L. Grenard received his Ph.D. in Preventive Medicine from the Keck School of Medicine at the University of Southern California. Although recently retired, his research examined dual cognitive processes that influence behavior related to chronic diseases such as substance use, HIV, and diabetes.
Footnotes
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
Supplemental analyses evaluated gender by DAST scores, gender by go/no-go false alarms, and a three-way interaction analysis evaluated gender by DAST score by go/no-go false alarms. Results of these analyses were similar to the two-way interaction models and no interactions by gender were significant.
References
- Abbey A, Saenz C, Buck PO. Cumulative effects of acute alcohol consumption, individual differences and situational perceptions on sexual decision making. Journal of Studies on Alcohol & Drugs. 2005;66:82–90. doi: 10.15288/jsa.2005.66.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ames SL, Grenard JL, Stacy AW. Dual process interaction model of HIV-risk behaviors among drug offenders. AIDS and Behavior. 2013;17(3):914–925. doi: 10.1007/s10461-012-0140-2. Retrieved from http://link.springer.com/article/10.1007%2Fs10461-012-0140-2#. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 U.S. dependent areas—2010. HIV Surveillance Supplemental Report. 2012;17(3, Part A) Retrieved from http://www.cdc.gov/hiv/surveillance/resources/reports/2010suppvol17no3/pdf/hssrvol17no3.pdf#page=22. [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3rd. Mahwah, New Jersey: Lawrence Erlbaum Associates; 2003. Interactions among continuous variables. [Google Scholar]
- Conrod PJ, Castellanos-Ryan N, Mackie C. Longterm effects of a personality-targeted intervention to reduce alcohol use in adolescents. Journal of Consulting and Clinical Psychology. 2011;79:296–306. doi: 10.1037/a0022997. [DOI] [PubMed] [Google Scholar]
- Conrod PJ, Castellanos-Ryan N, Strang J. Brief, personality-targeted coping skills interventions and survival as a non-drug user over a 2-year period during adolescence. Archives of General Psychiatry. 2010;67:85–93. doi: 10.1001/archgenpsychiatry.2009.173. [DOI] [PubMed] [Google Scholar]
- Darke S, Hall W, Heather N, Ward J, Wodak A. The reliability and validity of a scale to measure HIV risk-taking behaviour among intravenous drug users. AIDS. 1991;5:181–185. doi: 10.1097/00002030-199102000-00008. [DOI] [PubMed] [Google Scholar]
- Des Jarlais DC, Arasteh K, Perlis T, Hagan H, Abdul-Quader A, Heckathorne DD, Friedman SR. Convergence of HIV seroprevalence among injecting and non-injecting drug users in New York City. AIDS. 2007;21:231–235. doi: 10.1097/QAD.0b013e3280114a15. [DOI] [PubMed] [Google Scholar]
- de Wit H. Impulsivity as a determinant and consequence of drug use: A review of underlying processes. Addiction Biology. 2008;14:22–31. doi: 10.1111/j.1369-1600.2008.00129.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiFranceisco W, McAuliffe TL, Sikkema KJ. Influences of survey instrument format and social desirability on the reliability of self-reported high risk sexual behavior. AIDS and Behavior. 1998;2:329–337. [Google Scholar]
- Donenberg GR, Emerson E, Bryant FB, Wilson H, Weber-Shifrin E. Understanding AIDS-risk behavior among adolescents in psychiatric care: Links to psychopathology and peer relationships. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:642–653. doi: 10.1097/00004583-200106000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donohew L, Zimmerman R, Cupp PS, Novak S, Colon S, Abell R. Sensation seeking, impulsive decision-making, and risky sex: Implications for risk-taking and design of interventions. Personality and Individual Differences. 2000;28:1079–1091. [Google Scholar]
- Ellickson PL, Collins RL, Bogart LM, Klein DJ, Taylor SL. Scope of HIV risk and co-occurring psychosocial health problems among young adults: Violence, victimization, and substance use. Journal of Adolescent Health. 2005;36:401–409. doi: 10.1016/j.jadohealth.2004.06.008. [DOI] [PubMed] [Google Scholar]
- Ersche KD, Turton AJ, Pradhan S, Bullmore ET, Robbins TW. Drug addiction endophenotypes: Impulsive versus sensation-seeking personality traits. Biological Psychiatry. 2010;68:770–773. doi: 10.1016/j.biopsych.2010.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fillmore MT, Marczinski CA, Bowman AM. Acute tolerance to alcohol effects on inhibitory and activational mechanisms of behavioral control. Journal of Studies on Alcohol. 2005;66:663–672. doi: 10.15288/jsa.2005.66.663. [DOI] [PubMed] [Google Scholar]
- Fillmore MT, Rush CR. Impaired inhibitory control of behavior in chronic cocaine users. Drug and Alcohol Dependence. 2002;66:265–273. doi: 10.1016/s0376-8716(01)00206-x. [DOI] [PubMed] [Google Scholar]
- Fillmore MT, Rush CR. Polydrug abusers display impaired discrimination-reversal learning in a model of behavioral control. Journal of Psychopharmacology. 2006;20:24–32. doi: 10.1177/0269881105057000. [DOI] [PubMed] [Google Scholar]
- Graham JW. Missing data analysis: Making it work in the real world. Annual Review of Psychology. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- Grenard JL, Ames SL, Stacy AW. Deliberative and spontaneous cognitive processes associated with HIV risk behavior. Journal of Behavioral Medicine. 2013;36(1):95–107. doi: 10.1007/s10865-012-9404-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grenard JL, Ames SL, Wiers RW, Thush C, Sussman S, Stacy AW. Working memory capacity moderates the predictive effects of drug-related associations on substance use. Psychology of Addictive Behaviors. 2008;22:426–432. doi: 10.1037/0893-164X.22.3.426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hormes JM, Coffey SF, Drobes DJ, Saladin ME. The Obsessive Compulsive Cocaine Use Scale: Development and initial validation of a self-rated instrument for the quantification of thoughts about cocaine use. Drug and Alcohol Dependence. 2011;120:250–254. doi: 10.1016/j.drugalcdep.2011.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang LY, Ross MW, Zack C, Bull L, Rickman K, Holleman M. Prevalence of sexually transmitted infections and associated risk factors among populations of drug abusers. Clinical Infectious Diseases. 2000;31:920–926. doi: 10.1086/318131. [DOI] [PubMed] [Google Scholar]
- Jenness SM, Kobrak P, Wendel T, Neaigus A, Murrill CS, Hagan H. Patterns of exchange sex and HIV infection in high-risk heterosexual men and women. Journal of Urban Health. 2011;88(2):329–341. doi: 10.1007/s11524-010-9534-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Cain D. The relationship between indicators of sexual compulsivity and high risk sexual practices among men and women receiving services from a sexually transmitted infection clinic. Journal of Sex Research. 2004;41:235–241. doi: 10.1080/00224490409552231. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Cain D, Zweben A, Swain G. Sensation seeking, alcohol use and sexual risk behaviors among men receiving services at a clinic for sexually transmitted infections. Journal of Studies on Alcohol. 2003;64:564–569. doi: 10.15288/jsa.2003.64.564. [DOI] [PubMed] [Google Scholar]
- Kirisci L, Tarter RE, Vanyukov M, Martin C, Mezzich A, Brown S. Application of item response theory to quantify substance use disorder severity. Addictive Behaviors. 2006;31:1035–1049. doi: 10.1016/j.addbeh.2006.03.033. [DOI] [PubMed] [Google Scholar]
- Kjome KL, Lane SD, Schmitz JM, Green C, Ma L, Prasla I, Moeller FG. Relationship between impulsivity and decision making in cocaine dependence. Psychiatry Research. 2010;178:299–304. doi: 10.1016/j.psychres.2009.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leigh BC. Alcohol and condom use: A meta-analysis of event-level studies. Sexually Transmitted Diseases. 2002;29(8):476–482. doi: 10.1097/00007435-200208000-00008. [DOI] [PubMed] [Google Scholar]
- Leigh BC, Ames SL, Stacy AW. Alcohol, drugs, and condom use among drug offenders: An event-based analysis. Drug and Alcohol Dependence. 2008;93:38–42. doi: 10.1016/j.drugalcdep.2007.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marczinski CA, Fillmore MT. Dissociative antagonistic effects of caffeine on alcohol-induced impairment of behavioral control. Experimental and Clinical Psychopharmacology. 2003;11:228–236. doi: 10.1037/1064-1297.11.3.228. [DOI] [PubMed] [Google Scholar]
- Marin G, Sabogal F, Marin BV, Otero-Sabogal R, Perez-Stable EJ. Development of a short acculturation scale for Hispanics. Hispanic Journal of Behavioral Sciences: Special Acculturation Research. 1987;9:183–205. [Google Scholar]
- McClelland GH, Judd CM. Statistical difficulties of detecting interactions and moderator effects. Psychological Bulletin. 1993;114:376–390. doi: 10.1037/0033-2909.114.2.376. [DOI] [PubMed] [Google Scholar]
- Mdege ND, Lang J. Screening instruments for detecting illicit drug use/abuse that could be useful in general hospital wards: A systematic review. Addictive Behaviors. 2011;36:1111–1119. doi: 10.1016/j.addbeh.2011.07.007. [DOI] [PubMed] [Google Scholar]
- Mostofsky SH, Simmonds DJ. Response inhibition and response selection: Two sides of the same coin. Journal of Cognitive Neuroscience. 2008;20:751–761. doi: 10.1162/jocn.2008.20500. [DOI] [PubMed] [Google Scholar]
- O’Leary-Barrett M, Mackie CJ, Castellanos-Ryan N, Al-Khudhairy N, Conrod PJ. Personality-targeted interventions delay uptake of drinking and decrease risk of alcohol-related problems when delivered by teachers. Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49:954–963. doi: 10.1016/j.jaac.2010.04.011. [DOI] [PubMed] [Google Scholar]
- Reilly T, Woo G. Predictors of high-risk sexual behavior among people living with HIV/AIDS. AIDS and Behavior. 2001;5:205–217. [Google Scholar]
- Reynolds B, Ortengren A, Richards JB, de Wit H. Dimensions of impulsive behavior: Personality and behavioral measures. Personality and Individual Differences. 2006;40:305–315. [Google Scholar]
- Richardson JL, Milam J, McCutchan A, Stoyanoff S, Bolan R, Weiss J, Marks G. Effect of brief safer-sex counseling by medical providers to HIV-1 seropositive patients: A multi-clinic assessment. AIDS. 2004;18:1179–1186. doi: 10.1097/00002030-200405210-00011. [DOI] [PubMed] [Google Scholar]
- Roberts GMP, Garavan H. Evidence of increased activation underlying cognitive control in ecstasy and cannabis users. NeuroImage. 2010;52:429–435. doi: 10.1016/j.neuroimage.2010.04.192. [DOI] [PubMed] [Google Scholar]
- Ross MW, Hwang LY, Zack C, Bull L, Williams ML. Sexual risk behaviors and STIs in drug abuse treatment populations whose drug of choice is crack cocaine. International Journal of STD and AIDS. 2002;13:769–774. doi: 10.1258/095646202320753736. [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc. SAS O® 9.3. Cary, NC: SAS Institute Inc; 2011. [Google Scholar]
- Semple SJ, Zians J, Grant I, Patterson TL. Methamphetamine use, impulsivity, and sexual risk behavior among HIV-positive men who have sex with men. Journal of Addictive Diseases. 2006;25:105–114. doi: 10.1300/J069v25n04_10. [DOI] [PubMed] [Google Scholar]
- Senn TE, Carey MP, Vanable PA, Coury-Doniger P, Urban MA. Childhood sexual abuse and sexual risk behavior among men and women attending a sexually transmitted disease clinic. Journal of Consulting and Clinical Psychology. 2006;74(4):720–731. doi: 10.1037/0022-006X.74.4.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmonds DJ, Pekar JJ, Mostofsky SH. Meta-analysis of go/no-go tasks demonstrating that fMRI activation associated with response inhibition is task-dependent. Neuropsychologia. 2008;46:224–232. doi: 10.1016/j.neuropsychologia.2007.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner HA. The Drug Abuse Screening Test. Addictive Behaviors. 1982;7:363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- Stacy AW, Ames SL, Ullman JB, Zogg JB, Leigh BC. Spontaneous cognition and HIV risk behavior. Psychology of Addictive Behaviors. 2006;20:196–206. doi: 10.1037/0893-164X.20.2.196. [DOI] [PubMed] [Google Scholar]
- Völlm B, Richardson P, McKie S, Reniers R, Elliot R, Deakin B. Neuronal correlates and serotonergic modulation of behavioural inhibition and reward in healthy and antisocial individuals. Journal of Psychiatric Research. 2010;44:123–131. doi: 10.1016/j.jpsychires.2009.07.005. [DOI] [PubMed] [Google Scholar]
- Weafer J, Fillmore MT, Milich R. Increased sensitivity to the disinhibiting effects of alcohol in adults with ADHD. Experimental and Clinical Psychopharmacology. 2009;17:113–121. doi: 10.1037/a0015418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster JM, Dickson MF, Duvall JL, Clark DB. Rural and urban differences in Kentucky DUI offenders. Journal of Addiction Medicine. 2010;4:186–190. doi: 10.1097/ADM.0b013e3181c6cb24. [DOI] [PubMed] [Google Scholar]
- Xiao Z, Palmgreen P, Zimmerman R, Noar S. Adapting and applying a multiple domain model of condom use to Chinese college students. AIDS Care. 2010;22:332–338. doi: 10.1080/09540120903193609. [DOI] [PubMed] [Google Scholar]
- Yudko E, Lozhkina O, Fouts A. A comprehensive review of the psychometric properties of the Drug Abuse Screening Test. Journal of Substance Abuse Treatment. 2007;32:189–198. doi: 10.1016/j.jsat.2006.08.002. [DOI] [PubMed] [Google Scholar]


