Abstract
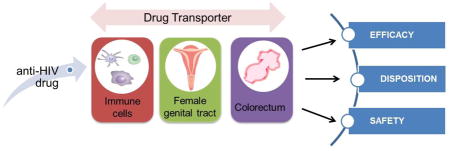
Efflux and uptake transporters of drugs are key regulators of the pharmacokinetics of many antiretroviral drugs. A growing body of literature has revealed the expression and functionality of multiple transporters in female genital tract (FGT), colorectal tissue, and immune cells. Drug transporters could play a significant role in the efficacy of preventative strategies for HIV-1 acquisition. Pre-exposure prophylaxis (PrEP) is a promising strategy, which utilizes topically (vaginally or rectally), orally or other systemically administered antiretroviral drugs to prevent the sexual transmission of HIV to receptive partners. The drug concentration in the receptive mucosal tissues and target immune cells for HIV is critical for PrEP effectiveness. Hence, there is an emerging interest in utilizing transporter information to explain tissue disposition patterns of PrEP drugs, to interpret inter-individual variability in PrEP drug pharmacokinetics and effectiveness, and to improve tissue drug exposure through modulation of the cervicovaginal, colorectal, or immune cell transporters. In this review, the existing literature on transporter expression, functionality and regulation in the transmission-related tissues and cells is summarized. In addition, the relevance of transporter function for drug delivery and strategies that could exploit transporters for increased drug concentration at target locales is discussed. The overall goal is to facilitate an understanding of drug transporters for PrEP optimization.
Keywords: Transporters, female genital tract (FGT), colorectal tissue, immune cells, HIV prevention, pre-exposure prophylaxis (PrEP)
Graphical abstract
1. Introduction
The efficacy of drug delivery to the target tissue and cell depends on several anatomical and physiological barriers such as mucous and cell membranes, protein binding, metabolizing enzymes, and drug transporters. Drug transporters are critical determinants of drug pharmacokinetics (PK), pharmacodynamics (PD), drug-drug interactions and safety. Significant progress has been made in understanding the uptake and efflux mechanisms of transporters, structural requirements of substrates, and exploiting drug transporters by inhibition and targeting to increase drug efficacy and reduce side effects. Kruijtzer et al. found that the co-administration of the breast cancer resistant protein (BCRP) and P-glycoprotein (P-gp) inhibitor, GF120918, resulted in a significant increase in the systemic exposure of oral topotecan. The apparent oral bioavailability increased from 40.0% without to 97.1% with GF120918 [1]. Studies have shown to use P-gp inhibitors to improve oral bioavailability and brain penetration of P-gp substrate drugs [2, 3]. Although preclinical studies proved efficacy of transporter inhibitors [3], limited clinical success has been achieved mostly due to their non-specific inhibition leading to increased side effects. Newer strategies such as targeted nanoparticles are being developed to restrict transporter inhibition to the target of interest. It is well established that transporters are involved in antiretroviral (ARV) drug absorption and tissue exposure [4, 5]. However, transporters relevant to sexual-transmission related tissues and cells, namely, female genital tract (FGT), colorectum, and immune cells are less studied. Because these tissues and cells HIV-1 through sexual transmission, the transporters expressed in these targets could be highly relevant for prevention of HIV-1 acquisition through prophylactic strategies.
HIV pandemic continues to be a worldwide public health problem [6]. There has been a steady increase in the number of people living with HIV worldwide [6]. In 2012 alone, 1.6 million people died of acquired immunodeficiency syndrome (AIDS) globally, and the number of people living with HIV was estimated to be 35.3 million in 2012 [6]. Although current therapies can suppress the AIDS symptoms, they are not able to eradicate the virus in HIV-positive patients [7]. As a result, more than 2 million people are newly infected every year. Therefore efforts must be made to prevent the acquisition of HIV in healthy populations.
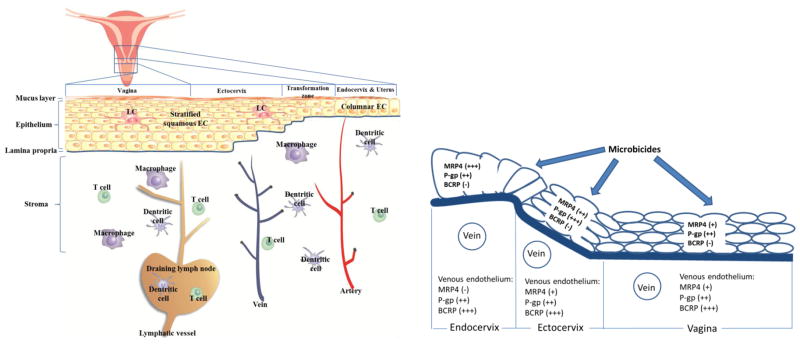
Sexual transmission is the cause of a vast majority of new HIV infections in sub-Saharan Africa, where 70% of global new infections occur. HIV sexual transmission can occur via vaginal as well as anal intercourse. Although approaches such as use of condoms, male circumcision, and reduction in the number of sex partners have been effective in reducing the acquisition rate of sexually transmitted HIV [6, 8, 9], effective implementation of these approaches is challenging. Currently, pre-exposure prophylaxis (PrEP) has been considered a self-controlled, promising strategy in the prevention of HIV sexual transmission. PrEP includes the use of ARVs such as entry inhibitors (EIs), nucleoside/nucleotide reverse transcriptase inhibitors (NRTIs), non-nucleoside reverse transcriptase inhibitors (NNRTIs), and integrase inhibitors (IIs), which target the early steps of HIV life cycle before the integration of viral DNA into host genome [10–13] to prevent HIV infection in uninfected populations. The immune cells in female genital mucosal tissues such as T cells, macrophages, dentritic cells (DCs) with positive expression of CD4 receptor on cell surface are initially infected (Figure 1) [14, 15]. Consequently, PrEP drug candidates must reach submucosal immune cells to prevent the formation and local expansion of the “founder population” of the virus at the initial stage of viral exposure. These target immune cells are distributed at different depths throughout the female genital and colorectal tracts, therefore, achieving high immune cell concentration requires rapid and deep penetration of a sufficient amount of ARV drug into the tissue. Currently, most PrEP products are at different stages of development, and they can be administered via vaginal, rectal, oral, subcutaneous, or intramuscular routes. The rationale for using topically administered products is that vaginal and rectal administration could result in better accumulation of administered drugs in the cervicovaginal tissues, colorectal tissue, and immune cells associated with these tissues, compared to the oral and systemic routes [16]. In addition, topical administration results in lower systemic drug levels compared to oral and other administration routes, and is less likely to cause systemic side effects [17, 18].
Figure 1. Anatomy and transporter expression in the female genital tract.
The FGT that are potential sites of sexual HIV transmission include uterus, endocervix, ectocervix, and vagina. A mucus layer covers the epithelia of all these tissue segments, serving as a physical barrier to vaginally administered drugs. Stratified, squamous epithelial layers line the vagina and ectocervix, and a single-layer of columnar epithelial cells lines the endocervix and uterus. The epithelial layers and stroma are separated by the collagen-rich laminar propria. The CD4+ T cells, dentritic cells and macrophages are HIV target cells, and they are distributed in epithelial layers, stroma, and draining lymph nodes. The invading HIV particles can infect these immune cells and establish local tissue infection, expansion, and progress to systemic dissemination. Blood vessels (veins, arteries) and lymphatic vessels mediate the distribution of drug between the tissues and systemic compartments (circulating blood and lymph). LCs, Langerhan’s cells, which are the dentritic cells residing in peripheral tissues. EC, epithelial cells. (The figure is based on Zhou et al. [62])
It has become a consensus in the field that cervicovaginal or colorectal tissue drug exposure is the key to the effectiveness of PrEP [19, 20]. One of the major barriers for successful prevention of HIV acquisition using PrEP is the inability to achieve high concentrations of ARVs in tissues and cells relevant to sexual-transmission of the virus. Besides physicochemical properties of drugs, anatomical, and physiological barriers, drug uptake and efflux transporters play a key role in the anti-HIV drug delivery to target tissues and cells [21]. Drug transporters are one of the major determinants of suboptimal tissue concentrations of ARVs [22]. Transporters can contribute to drug disposition, drug-drug interactions, emergence of resistant viral strains, toxicity, and inter-individual variability in ARVs efficacy [21, 23]. Transporters relevant to ARVs are expressed in different body compartments such as gastrointestinal tract, cells in systemic circulation, tissues and cells involved in sexual HIV transmission, and organs involved in drug metabolism and elimination [21, 24]. Specifically, drug transporter expression and functionality in human genital tract and colorectal compartments can significantly influence drug delivery to target tissues and cells that are involved in sexual HIV transmission. However, limited literature is available for the expression profile and functionality of transporters in specific anatomical compartments such as colorectum and vagina. This information is crucial in understanding the effect of transporters on drug delivery and ultimately safety and efficacy. An enhanced understanding of transporter-dependent tissue exposure could help delineate the causes of intra-individual and inter-individual variability in PK/PD, which are often observed with ARVs [25–27]. This new knowledge will facilitate the development of novel drug delivery strategies that enhance tissue drug exposure as well as reduce side effects. This review provides a comprehensive overview of transporters expressed in colorectal and female genital tissues and immune cells, their endogenous functionality, and their relevance to anti-HIV drug delivery, PK, and efficacy.
2. Critical barriers to achieving sufficient tissue drug concentration in pre-exposure prophylaxis (PrEP)
2.1. Barriers to achieving high ARVs concentrations in sexual-transmitted tissues and cells
It is challenging to achieve high ARV exposure in the tissues related to HIV sexual transmission, due to the physicochemical, physiological, and behavioral reasons. A number of PrEP drug candidates are either very hydrophobic (e.g. dapivirine) or quite hydrophilic (e.g. tenofovir, maraviroc). When administered topically, the absorption of these drugs can be limited due to the permeation barriers posed by the mucus layer and the epithelium (tight junctional proteins) of the cervicovaginal and colorectal tracts [28], as well as the blood and lymphatic drainage systems which serve to extract the drug from the tissue (Figure 1). This is especially true for hydrophilic drugs that have low binding affinity to tissue proteins and cannot efficiently penetrate the plasma membrane. A Phase I trial (MTN-013/IPM-026) evaluating vaginal ring products containing dapivirine (hydrophobic) and maraviroc (MVC) (hydrophilic) revealed that MVC was not absorbed well based on the blood and cervical tissue concentrations and it did not exert protective effects compared to dapivirine [29]. Another extensively studied hydrophilic microbicide candidate, tenofovir (TFV), exhibited low penetration efficiency given the millimolar level drug concentration in the vaginal fluid but micromolar level concentration in the vaginal tissue [16].
Although hydrophobic drugs can be absorbed more efficiently compared to the hydrophilic drugs, their distribution within the tissues can be potentially problematic. A study using excised human ectocervical tissue showed that film-released dapivirine mostly accumulated around the basal layers of cervicovaginal epithelium infiltrating the upper part of the stroma, while a small amount of drug reached the deep stroma [30–32]. This may be true for other hydrophobic drugs, which extensively bind to tissue proteins and consequently lead to poor penetration into deep stroma.
The low adherence often encountered with the use of once-daily products is another factor that can reduce ARV drug efficacy. Inconsistent efficacy results have been reported from different trials of 1% tenofovir gel [33–36], and the suboptimal results in CAPRISA 004, VOICE, and FEM-PrEP clinical trials have been attributed to poor patient adherence [13]. While long-acting dosage forms such as intravaginal rings are being actively pursued to resolve the adherence issue [13, 37–41], it is crucial to understand physiologic determinants of tissue drug exposure for the optimal exposure and efficacy outcomes.
As for the PrEP utilizing orally administered ARVs, the tissue distributions of some ARVs differ markedly in their ability to penetrate into mucosal tissues and fluids [22, 42–44]. It has been observed that highly protein-bound drugs have lower tissue concentration i.e. lower tissue-to-plasma ratios, because only the free drug portion not associated with plasma albumin or α1-acid glycoprotein can distribute into tissues. However, the tissue distribution cannot be solely explained by protein binding affinity of the ARVs; other mechanisms may play a role in the distribution of ARVs to cervicovaginal tissues [22, 43]. Additionally, large inter-individual variability has been observed in the FGT drug concentration, for drugs within the same class and across different classes [22]. The variability in drug exposure in FGT is generally greater than that observed in plasma [22, 43]. Therefore, a better understanding of the causes underlying the low tissue penetration and inter-individual variability will facilitate the achievement of sufficient drug exposure after oral dosing.
2.2 The necessity of better understanding critical determinants of tissue drug exposure
Currently, the effective in vivo drug concentration remains unknown for many microbicide drug candidates being evaluated [19]. The consensus on PrEP drug delivery is to achieve the maximally tolerated drug concentration in the tissues and cells relevant to HIV sexual transmission [19]. For the ARVs with poor ability to penetrate tissues, an easy way of increasing the cervicovaginal tissue drug exposure is to increase the dose. However, high topical dose of some drugs is associated with altered vaginal microbiome and/or genital tract irritation [45], and poses challenges to the manufacturability and applicability of microbicide products given limited drug loading capacity of topical products. For the oral PrEP, high doses of ARVs may cause a variety of toxicities to the liver, kidney, and cardiovascular systems [46]. The necessity and challenges of achieving high drug exposure in a safe and effective manner call for a need to better understand critical determinants of ARV exposure in the tissues and cells relevant to HIV sexual transmission. Notably, preclinical studies have demonstrated that the topically administered products could result in biologically relevant levels of DPV [47, 48], MVC [49], and TFV [50–52] in the tissues related to HIV sexual transmission. The models used in these studies include human cervical and vaginal tissue explants, rabbits, and non-human primates. The wide use of these models in microbicide testing warrants the parallel investigation of the critical determinants of tissue drug exposure in these models. This is especially important given the apparent inconsistency between preclinical and clinical testing results for some drugs (e.g. MVC). This information can lead to better design of PrEP products and significant improvement of drug delivery to target tissues and cells.
In addition, multiple physiological barriers exist and limit drug penetration into the tissues. The FGT and colorectal tissue are covered with a mucus layer that can entrap topically administered drugs and reduce their contact with epithelial cells. In FGT, the vagina and ectocervix are lined with multi-layer squamous epithelial cells (up to 40 layers) [53, 54], which serves as a permeation barrier to topical drug administration (Figure 1) [28]. The endocervix, uterus, and colorectum are lined with single-layer columnar epithelial cells (Figure 1), but the tight junction expression is more intense in these epithelial layers compared to the ectocervical and vaginal epithelia [55]. Since the target immune cells are distributed at different depths throughout the female genital and colorectal tracts, the administered drugs must penetrate deeply and accumulate in sufficient concentration in the tissue-associated immune cells.
Absorption of topically administered PrEP drug candidates can be limited due to the permeation barriers posed by the mucus layer and the epithelium (tight junctional proteins) of the cervicovaginal and colorectal tracts [28], as well as the blood and lymphatic drainage systems which serve to extract the drug from the tissue (Figure 1). This is especially true for hydrophilic drugs that have low binding affinity to tissue proteins and cannot efficiently penetrate the plasma membrane. A recent Phase I trial (MTN-013/IPM-026) evaluating vaginal ring products containing 25 mg of dapivirine (hydrophobic) and 100 mg of maraviroc (MVC) (hydrophilic) in HIV-negative women. The drug concentrations were tested in plasma, cervicovaginal fluid, and cervical tissue and ex vivo HIV challenge was performed in cervical biopsy explants to evaluate pharmacodynamics. They found that MVC was not absorbed well based on the blood and cervical tissue concentrations and did not exert a protective effect compared to dapivirine [29, 56]. Although hydrophobic drugs can be absorbed more efficiently compared to the hydrophilic drugs, their distribution within the tissues can be potentially problematic. A recent study using excised human ectocervical tissue showed that film-released dapivirine mostly accumulated around the basal layers of cervicovaginal epithelium infiltrating the upper part of the stroma, while small amount of drug reached the deep stroma [30–32]. This may be true for other hydrophobic drugs, which extensively bind to tissue proteins and consequently lead to poor penetration into deep stroma.
The tissue distributions of some orally administered ARVs differ markedly in their ability to penetrate into mucosal tissues and fluids [22, 42–44]. It has been observed that highly protein-bound drugs have lower tissue concentration, i.e. lower tissue-to-plasma ratios, because only the free drug portion not associated with plasma albumin or α1-acid glycoprotein can distribute into tissues. Additionally, large inter-individual variability has been observed in the FGT drug concentration, for drugs within the same class and across different classes [22]. The variability in drug exposure in FGT is generally greater than that observed in plasma [22, 43]. Therefore, a better understanding of the causes underlying the low tissue penetration and inter-individual variability will facilitate the achievement of sufficient drug exposure after oral dosing.
Currently, the effective in vivo drug concentration remains unknown for many microbicide drug candidates being evaluated [19]. The consensus on PrEP drug delivery is to achieve the maximally tolerated drug concentration in the tissues and cells relevant to HIV sexual transmission [19]. For the ARVs with poor ability to penetrate tissues, an easy way of increasing the cervicovaginal tissue drug exposure is to increase the dose. However, high topical dose of some drugs is associated with altered vaginal microbiome and/or genital tract irritation [45], and poses challenges to the manufacturability and applicability of microbicide products given limited drug loading capacity of topical products. For the oral PrEP, high doses of ARVs may cause a variety of toxicities to liver, kidney, and cardiovascular system [46]. The necessity and challenges of achieving high drug exposure in a safe and effective manner call for a need to better understand critical determinants of ARVs exposure in the tissues and cells relevant to HIV sexual transmission. This information can lead to better design of PrEP products and significant improvement of drug delivery to target tissues and cells.
3. Drug transporters in sexual transmission-related tissues and cells
A growing body of evidence has demonstrated that some efflux and uptake transporters are expressed in FGT, colorectal tissue, and immune cells (Table 1). Studies have demonstrated that efflux transporters of blood-derived immune cells limit the intracellular accumulation and/or efficacy of ARVs [57, 58]. Although there is little direct evidence showing the functional role of these transporters in drug PK in the tissue, clinical PK studies comparing drug exposure in different physiologic compartments have implicated the presence of active drug transport mechanisms in the FGT [44, 59]. Some transporter substrates, including MVC, lamivudine, and emtricitabine, are reported to be preferentially distributed in cervicovaginal tissues and/or fluids at higher levels than in plasma, after oral administration [44, 59]. These differential drug distribution profiles cannot be solely explained by the differences in plasma protein binding and passive permeation, as drugs with similar plasma protein binding and permeability displayed different capabilities of distributing into cervicovaginal tissues [43, 44, 59, 60].
Table 1.
Expression and localization of transporters in human tissues and cells relevant to HIV sexual transmission.
| Compartments | Tissue/cell type | mRNA/protein expression | Cellular localization | Ref. |
|---|---|---|---|---|
| Female genital tract | Uterus | (+): P-gp, BCRP, MRP1, MRP4, MRP5, MRP7, OCT3, CNT1, ENT1,2 OATP3A1 | Glandular cells of endometrium (P-gp, MRP4, CNT1, ENT1,2); endometrial capillaries (P-gp) | [76, 81, 83, 88–90] |
| Endocervix | (+): P-gp, BCRP, MRP2, MRP4 (−):OAT1,3, OATP1B1 |
Glandular epithelium and submucosal immune cells (P- gp, MRP2); vascular endothelium of stroma (BCRP) | [80, 90–92] | |
| Ectocervix | (+): P-gp, BCRP, MRP1, MRP4, MRP5, MRP7, OAT2, OCT1,2,3, ENT1,2 (−): MRP2, MRP6, OAT1,3, OATP1B1 |
Squamous epithelium and stromal tissue (P-gp); vascular endothelium of stroma (BCRP) | [24, 89, 90, 92, 93] | |
| Vagina | (+): P-gp, BCRP, MRP1, MRP2, MRP3, MRP4, MRP5, MRP7, OAT2, OCT1,2,3, ENT1,2 (−):MRP3, 6, OAT1, 3, OATP1B1 |
Squamous epithelium and submucosal immune cells (P- gp and MRP); deeper layers of epithelial cells and vascular endothelial cells (MRP3,4). | [24, 77, 80, 91, 94] | |
|
| ||||
| Colorectal tissues | Colon | (+): P-gp, BCRP, MRP1, MRP2, MRP3, MRP4, MRP5, MRP7 (−): MRP2, OAT1, 2, 3, |
Columnar epithelium (P-gp, BCRP, MRP3,4,5, OATP2B1,4A1,4C1); secretory epithelial cells (goblet cells) (MRP3,4, OATP1C1,2B1,4C1) | [76, 89, 93, 95–109] |
| Colorectum | (+): P-gp, MRP2, MRP4 (−):OAT1,3, OATP1B1 |
Columnar epithelium and submucosal immune cells (P- gp and MRP2) | [91, 94, 106] | |
|
| ||||
| Immune cells | Within cervicovaginal and colorectal tissues | (+): P-gp, MRP2, MRP4 (−): OAT1, 3, OATP1B1 |
A subset of submucosal lymphocytes and monocytes in cervicovaginal and colorectal tissues (P-gp and MRP2) | [94, 95] |
|
| ||||
| Blood-derived | PBMCs (+): P-gp, BCRP, MRP1,2,3,4,6,7, OCT1, OAT2, ENT1,2, OATP2B1, 3A1 | [89, 110– 127] | ||
| Lymphocytes or CD4+ T cells (+): P-gp, BCRP, MRP1,2, OATP1A2, OATP3A1 | [58, 89, 91, 94, 122, 128–146] | |||
| Macrophages (+): P-gp, MRP1,4,5,7 CNT1,2,3, ENT1,2, OCT1,3, OCTN1,2 | [122, 147–149] | |||
| Dentritic cells (+): P-gp, CNT1,2,3, ENT1,2, OCT1,3, OCTN1,2 | [122, 150] | |||
These studies demonstrate that efflux transporters expressed in FGT could play a functional role on drug absorption. Additionally, the low expression of uptake transporters in FGT concomitant with their expression in tissues/cells involved in drug removal from vaginal lumen suggests that effective drug delivery strategies should exploit efflux transporters to increase the tissue drug concentrations for PrEP-based HIV prevention. Factors relating to transporter expression changes with menstruation, and the anatomical location within the genital tract should be noted. The effect of hormones and hormonal receptor signaling on transporter expression could guide the design of combination drug delivery strategies.
Thompson et al. summarized published literature of 58 drugs and developed a mathematical model to predict a compound’s cervicovaginal tissue penetration ratio (TPR) based on physicochemical properties and protein binding. The analysis showed that the TPR of orally administered drugs was significantly associated with its probability of being the substrate of efflux transporters, multidrug resistance-associated proteins (MRP1 and MRP4) [61]. This analysis highlighted the possibility of in vivo functional role of these transporters, in the blood-to-tissue distribution of ARVs in lower FGT. Several efflux and uptake transporters are also expressed in human FGT, colorectal tissues, and immune cells (Table 1). In this section, a brief overview of drug efflux and uptake transporters as well as their role relevant to ARVs is discussed.
3.1. Expression and function of drug transporters in sexual transmission-related tissues and cells
Drug transporters are transmembrane proteins that control the movement of substrates in and out of the cells. They are localized on plasma membrane or the membrane of intracellular organelles such as mitochondria [63]. Numerous studies have established the role of transporters in controlling drug accumulation, and in maintaining the homeostasis of endogenous substances in multiple tissues/organs including brain, liver and kidney [58, 63–71], and in various types of cells including epithelial cells [62, 72], endothelial cells [73], and immune cells [57] [74]. ATP-binding cassette (ABC) and solute carrier (SLC) superfamilies are transporters that are most relevant to efflux and uptake of ARVs respectively. The subfamilies of ABC and SLC transporters are reviewed elsewhere [75].
3.1.1. Transporters in FGT (uterus, endocervix, ectocervix, vagina)
Transporters such as P-glycoprotein (P-gp), breast cancer resistance protein (BCRP), multi-drug resistance proteins (MRPs) from ABC superfamily, and organic anion and organic cation transporters (OATs and OCTs), equillibrative transporters (ENTs), and organic anion-transporting polypeptides (OATPs) from SLC superfamily (Table 1) have been experimentally demonstrated to transport ARVs and are most frequently studied transporters in ARV PK. As listed in Table 1, P-gp, BCRP, MRP4 are consistently expressed along the entire FGT. BCRP appeared to be the most highly expressed transporter among ABC transporters in FGT. The uterine BCRP mRNA level was found to be the highest among all types of female reproductive tract tissues [76]. The BCRP mRNA level in endocervix, ectocervix, and vagina was comparable to or higher than that in liver [24], 92]. Several other MRP isoforms are also expressed at different segments of FGT (Table 1). There are contradictory reports regarding the expression of MRP3. This is mainly due to the difference in detection methods and criterion of “positive expression.” For example, Zhou et al. reported MRP3 mRNA level undetectable in human ectocervix and vagina, as the RT-PCR products for this transporter did not show visible bands in the agarose gel after electrophoresis [24]. However, Gunawardana et al. detected MRP3 protein in sporadic basal epithelial layers of human vagina using immunofluorescence staining, thus considering MRP3 as positively expressed [77]. Our group has also recently studied the mRNA expression and protein localization of three efflux transporters, P-gp, MRP4, and BCRP, in the lower genital tract of premenopausal women and pigtailed macaques [62]. The IHC staining showed that P-gp and MRP4 were localized in multiple cell types including epithelial cells and vascular endothelial cells in the female lower genital tract while BCRP was predominantly localized in the vascular endothelial cells. Compared to human tissues, the macaque cervicovaginal tissues displayed comparable expression and localization patterns of the three transporters, although subtle differences were observed between the two species. Transporter expression was also studied in cervicovaginal cell lines such as End1/E6E7, Ect1/E6E7, and VK2/E6E7 [78].
Compared to the ABC transporters, SLC transporters have been generally less studied in the FGT. The most relevant SLC transporters OAT1, OAT3 and OATP1B1 were found to be not expressed in endocervix, ectocervix, and vagina [24], which are major sites of PrEP drug action. The type of cells that harbour transporter proteins varies among different segments of FGT (Table 1).
Transporter functionality has been explored in few studies. Schinkel et al. found that Mdr1a/1b double knockout resulted in 2.2-fold increase in digoxin accumulation in mouse uterus, after intravenous administration [79]. Using a rabbit model, Grammen et al. demonstrated that the systemic uptake of P-gp substrate talinolol after vaginal administration could be significantly increased with the co-administration (vaginal route) of the P-gp inhibitor verapamil [80]. These studies indicate that ARV drug delivery to FGT and systemic circulation can be increased with the concomitant use of transporter inhibitors.
The regulation of transporter expression and localization in FGT has also been reported. In premenopausal women, the cellular localization, staining intensity, and percentage of P-gp in uterine tissue varied with the phase of the menstrual cycle. The staining intensity increased from early proliferative to late proliferative endometrial stages while it diminished from early secretory to late secretory phase.[81] P-gp expression parallels that of nuclear progesterone receptor expression in the normal human endometrial cycle and early gestational endometrium. In addition, P-gp expression corresponds to rising plasma and tissue levels of progesterone as well as to morphologic changes in the endometrial glandular epithelium associated with the marked development of the secretory apparatus [81]. In addition to P-gp, the MRP4 protein expression was found to undergo cyclic change during the estrous cycle in intact bovine endometrial tissues [82]. In the uteri from peritoneal endometriosis patients, Gori et al. reported that MRP4 was expressed in eutopic and ectopic endometrium, where it was overexpressed in peritoneal lesions and localized in the cytoplasm of glandular epithelial cells. Attenuation of MRP4 mRNA and protein levels in endometriotic epithelial cells by Lipoxin A4 was found to be mediated through estrogen receptor α, as examined using receptor antagonists and small interfering RNA [83]. The regulation of P-gp and Mrp4 expression at mRNA and protein levels by menstrual cycle has also been reported in a mouse model. The cyclic change of transporter expression during the menstrual cycle is presumably a result of the cyclic change of the reproductive hormones (estrogens and progesterone). Hormones have been shown to affect transporter expression and functionality through a variety of mechanisms, and the transcriptional regulation through hormone-responding nuclear receptors is most well studied [84]. In addition to endogenous hormones, synthetic hormonal contraceptives such as Depo-Provera also have the potential to modulate transporter expression, due to their ability to bind nuclear receptors [85]. However, the effect of hormonal contraceptives on transporter expression in cervicovaginal tissues, colorectal tissue, and immune cells has not been reported. This information is important given that hormonal contraceptives are widely used in participants of PrEP clinical trials [86]. For example, in the CAPRISA 004 trial which provided critical evidence of the effectiveness of tenofovir vaginal gel, 80% of participants were on the progestin contraceptives [87]. The effect of the commonly used contraceptives warrant further investigation for better delineation of the mechanisms underlying suboptimal exposure and efficacy of ARVs in PrEP trials.
3.1.2 Transporters in colorectal tissues (Colon, colorectum)
As shown in Table 2, P-gp, BCRP, MRPs1–7 are positively expressed in human colorectal tissues at moderate to high levels, compared to other genes expressed in colorectum [58, 89, 95, 100, 103, 106, 108], or compared to the expression level of the same transporter in liver [76]. The detection methods include qRT-PCR, Western blot, and IHC staining. De Rosa et al. compared the expression levels of multiple ABC transporters in the sigmoid colon of HIV-uninfected man [58]. In this evaluation, the ranking of transporter mRNA level was: MRP2>MRP4>MRP1> P-gp > BCRP, and the ranking of transporter protein level was: MRP1 > MRP4 = BCRP > MRP2 > P-gp [58]. However, Zimmermann et al. reported that the rank order of the transporter mRNA level was: MRP3 ≫ MDR1 > MRP4 almost equal to MRP5 > MRP1 ≫ MRP2[108]. One possible cause for this difference is the source of tissue samples. De Rosa et al. used tissues from young men with a median age of 39, while Zimmermann et al. used the tissues from both men and women with the average age of 62[58, 108]. Colorectal tissue P-gp, BCRP, MRP2, MRP3, MRP4 were localized on the plasma membrane of multiple cell types, including specialized epithelial cells with secretory/excretory functions, and endothelial cells of capillary blood vessels [93, 94, 99, 104, 151]. Furthermore, MRP4 was localized in endoplasmic-Golgi complex and basolateral location in goblet cells [104], MRP3 and MRP5 were localized on the basolateral membrane of glandular epithelial cells [104, 152]. The regional distribution of transporters along the intestinal tract has also been studied. Blokzijl et al. reported that P-gp mRNA level in colon was 5-fold lower than the level in terminal ileum [95]. Prime-Chapman et al. examined the mRNA expression of MRP1–6 in human colon and rectum. All the 6 MRPs were detected in the colon, but MRP2 and MRP6 were not detectable in the rectum [106]. The differential expression of the same transporter between colorectum and female genital tract was also reported by Nicol et al. In this study P-gp and MRP2 were expressed at lower levels compared to vagina, while the colorectal MRP4 level was higher than the vaginal level [94]. As to the SLC transporters, OAT2, CNT1, ENT1 were found to be highly expressed [89], while OAT1, OAT3, OCT2, OCT3 and OATP1B1 were negligible in human colorectum [94, 103].
Table 2.
Summary of the drug transporters that efflux or uptake ARVs.
| Antiretroviral drug class | Antiretroviral drugs | BCS Class | ABC transporters | SLC transporters |
|---|---|---|---|---|
| Entry inhibitors (EIs) | Maraviroc† | 3 | P-gp | OATP1B1 |
|
| ||||
| Nucleoside/nucleotide reverse transcriptase inhibitor (NRTIs) | Lamivudine | 3 | BCRP | OCT1, OCT2, CNT1 |
| Emtricitabine† | 3 | MRP1 | ||
| Tenofovir DF† | 3 | P-gp | ||
| Tenofovir† | 3 | MRP4, MRP7 | OAT1, OAT3 | |
| Abacavir | 1 | P-gp, BCRP, MRP4 | ||
| Zidovudine | 1 | BCRP, MRP4 | OAT1, OAT2, OAT3, CNT1, CNT3, ENT2 | |
| Didanosine | 3 | BCRP | CNT2, CNT3, ENT1, ENT2 | |
| Stavudine | 1 | BCRP, MRP5 | CNT1 | |
|
| ||||
| Non-nucleoside reverse transcriptase inhibitors (NNRTIs) | Efavirenz | 2 | ||
| Nevirapine | 2 | MRP7 | ||
| Delavirdine | 1 | |||
| Etravirine | 4 | |||
|
| ||||
| Protease inhibitors (PIs) | Atazanavir | 2 | P-gp, MRP1, MRP2 | |
| Ritonavir | 2 | P-gp, MRP1, MRP2 | ||
| Fosamprenavir | 2 | |||
| Amprenavir | 2 | P-gp | ||
| Lopinavir | 2 | P-gp, MRP1, MRP2 | OATP1A2, OATP1B1 | |
| Saquinavir | 2 | P-gp, MRP1, MRP2 | OATP1A2, OATP1B1 | |
| Darunavir | 2 | P-gp | OATP1A2, OATP1B1 | |
| Indinavir | 2 | P-gp, MRP1, MRP2 | ||
| Tipranavir | 2 | P-gp | ||
| Nelfinavir | 2 | P-gp | ||
|
| ||||
| Integrase inhibitors (IIs) | Raltegravir† | 2 | P-gp, BCRP* | |
The drug-transporter interactions listed in this table are adapted from a review by Kis et al [58].
Obtained from reference [173].
A number of these drugs are already undergoing clinical testing (denoted by †) toward the development of PrEP products, including MVC, emtricitabine, TFV, TDF, and raltegravir. The currently available transporter inhibitors of ARVs were reviewed previously by O. Kis et al [58].
The functionalities of colorectal P-gp and BCRP have been studied using human tissues and preclinical models. Collett et al. studied the permeability of the P-gp substrate UK-338,003 through mouse ileum and colon. The colonic permeability of UK-338,003 was at least 40 times lower than that of ileum, with large asymmetry (basolateral-to-apical permeability was much larger than the apical-to-basolateral permeability). The application of P-gp inhibitor markedly increased the colonic permeability of UK-338,003 to the level comparable to that of ileum. Low apical-to-basolateral permeability of UK-338,003 was also observed in the ex vivo human distal intestine, however the increase in UK-338,003 permeability after the co-administration of P-gp inhibitor was significantly lower than the increase in mouse colon [98]. This result has potential implications for drug delivery, specifically the route of administration and targeting specific parts of gastrointestinal tract to achieve effective drug permeability in the presence of P-gp inhibitors. Enokizono et al. used 4-methylum-belliferone (4MU) as substrate to examine BCRP functionality on the everted mouse colon sacs. A marked reduction in the mucosal secretion clearance of the 4MU sulfate was observed in the colon of BCRP knockout mice compared to that of the wild-type mice [101].
The studies examining the regulation of colorectal transporters have focused on several ABC transporters. The effect of gender on human colonic transporter expression remains unknown, but there is no difference in colonic P-gp mRNA level between male and female mice [153]. The impact of inflammation on transporter expression is different for different transporters. Ulcerative colitis (UC), Crohn’s disease (CD), collagenous colitis and diverticulitis cause tissue inflammation and strongly decreased P-gp mRNA and protein expression in colonic epithelial cells and submucosal mononuclear cells. The inflammation also down-regulates BCRP expression [100]. The down-regulation of P-gp is independent of PXR protein level [95], while the decrease in BCRP level was negatively correlated with the interleukin (IL)-6 mRNA level [100]. On the contrary, UC and CD significantly increased MRP1 mRNA expression [95]. HIV infection significantly down-regulated P-gp and MRP2 protein levels in male recto-sigmoid colon, while ARV treatment up-regulated P-gp and MRP2 protein levels [109]. The HIV infection and treatment did not have obvious effect on the expression of MRP1, MRP4 and BCRP [109]. In contrast to ABC transporters, the regulation of SLC transporters by infection or ARV treatment is not well understood. Kleberg et al. reported that neoplasia up-regulated OATP2B1 and OATP4A1 mRNA levels in human colorectum [104].
In addition to the anatomical differences that influence drug absorption, distribution, and elimination between FGT and colorectal tissues, these studies indicate that the transporter expression is also significantly different. The presence of uptake transporters in colorectum could provide a differential tissue exposure, PK, and efficacy when compared to FGT. Therefore, drug delivery strategies targeting FGT and colorectal tissues need to take into account these differences and exploit respective transporter expression and functionalities for effective drug delivery. The influence of pathophysiology such as inflammation on mucosal permeability and transporter expression are additional factors that can effect drug accumulation and elimination in colorectal tissues and cells.
3.1.3. Transporters in HIV target immune cells
Due to the scarcity of human cervicovaginal and colorectal tissues, and the difficulty of purifying immune cells from these tissues, there is a lack of characterization of the transporter expression and activity of the tissue-associated submucosal immune cells. However, there have been abundant reports on peripheral blood mononuclear cells (PBMCs), PBMC-derived immune cell subsets, and immortalized immune cell lines. Numerous studies have revealed the expression profile, functionality, and regulating factors of a number of ABC and SLC transporters in PBMCs, blood-derived lymphocytes or CD4+ T cells, blood monocyte-derived macrophages (MDM), and blood-derived DCs. Table 1 lists transporters expressed in immune cells from peripheral blood, and cervicovaginal and colorectal tissues. Large inter-individual differences in P-gp level have been observed in primary lymphocytes isolated from healthy volunteers [128].
ABC transporters in human blood-derived immune cells have been demonstrated to efflux ARVs and other drugs. The expression and functionality of several transporters were investigated in immune cells using transporter inhibitors. In healthy PBMCs, Janneh et al. reported the inhibitors of P-gp, MRP1 and MRP2 significantly increased the intracellular accumulation of saquinavir in healthy PBMCs [114]. Janneh et al. demonstrated that the MRP inhibitors tariquidar, MK571, frusemide and dipyridamole, as well as protease inhibitors (PIs) ritonavir, amprenavir and atazanavir significantly increased the intracellular concentration of lopinavir [131]. In lymphocytes, Gupta et al. revealed positive efflux activity of P-gp in healthy CD4+ T cells [130]. Clemente et al. revealed that the non-steroidal anti-inflammatory drugs (NSAIDs) blocked MRP4 efflux, increased the intracellular concentration and anti-viral efficacy of several nucleoside reverse transcriptase inhibitors (NRTIs) including zidovudine (AZT) in peripheral blood lymphocytes (PBLs) [112]. Liptrott et al. revealed the nevirapine concentration in the healthy CD4+ blood cells can be increased by small interfering RNA knockdown of MRP7 [143]. Lee et al. detected MRP1 efflux activity in the CD4+ T cells isolated from healthy subjects [154]. The lymphocyte transporter has also been studied in mouse. Elliott et al. revealed the positive expression and activity of P-gp (Mdr1a/1b), Mrp1, and Bcrp in mouse blood lymphocytes [137]. Schinkel et al. examined P-gp function in mice, and found that the lymph node accumulation of intravenously administered digoxin was significantly increased in Mdr1a/1b double knockout mice, compared to the wild type mice [155]. In human MDMs, the P-gp inhibitor PSC833 and the MRP1 inhibitor probenecid increased the intracellular accumulation of AZT in HIV-infected MDM, and increased the efficacy of AZT and indinavir [148]. Liptrott et al. reported the functionality of MRP7 in effluxing nevirapine from MDMs, using small interfering RNA that specifically knocked down MRP7 [143]. Due to the observed efflux activity of immune cell transporters, the genetic polymorphisms of P-gp, MRP1, MRP4, MRP5 transporters have been shown to correlate with varying intracellular concentration and/or efficacy of substrate drugs including PIs and NRTIs, in PBMCs and blood CD4+ T cells [112, 116, 127, 144].
The effects of disease, drug treatment, and activation status on immune cell transporter expression and activity have been evaluated. The effect of HIV infection depended on the model and cell type selected for examination. In human PBMCs, HIV infection up-regulated mRNA levels of P-gp and MRP1, 4, 5 [127]. In H9 (T cell line) and U937 (monocytic cell line) cells, HIV infection increased the expression of P-gp and increased the efflux of P-gp substrates AZT and daunorubicin [138]. In MDMs, HIV infection increased the mRNA levels of MRP1, 4, 5 [147]. However, Lucia et al. reported that viral load did not affect P-gp expression in the PBMCs of treatment-naive and –experienced patients [118]. In cynomolgus macaques, simian/human immunodeficiency virus (SHIV) infection decreased P-gp mRNA level in PBMCs and lymph node mononuclear cells [115]. Besides HIV infection, myasthenia gravis decreased P-gp efflux function of PBMCs [125], and increased intracellular cholesterol levels markedly up-regulated P-gp activity in PBMCs [126]. The effect of cytokine and ARV/anticancer drug treatment on immune cell transporters appeared to be drug-specific. IL-2 and interferon (IFN)-γ significantly increased the mRNA and protein expression of P-gp, MRP1 and MRP2, and reduced accumulation of digoxin and saquinavir, in the PBMCs of healthy volunteers [117]. In MDMs, IFN-γ increased P-gp mRNA abundance, induced polarized redistribution of P-gp protein in pseudopodia, and increased the efflux activity of P-gp [149]. The anticancer treatment of Kaposi sarcoma using the liposomal formulation of anthracycline doxorubicin up-regulated P-gp in the PBMCs of treatment-naive and -experienced patients [118]. AZT increased the MRP4 expression level in HIV infected T lymphocytes [112]. Despite these up-regulating effects, Lucia et al. reported that highly active antiretroviral therapy (HAART) did not affect P-gp expression in the PBMCs of treatment-naive and -experienced HIV-infected patients [118]. Agrati et al. reported that ARV treatment did not affect P-gp expression in PBMCs of HIV-infected patients [110]. Bossi et al. found that the PI treatment had no effect on the P-gp expression and activity, and was not linked to the treatment outcome [136]. Chinn et al. observed no significant effect of saquinavir and atazanavir treatments on P-gp expression and activity of lymphocytes isolated from healthy subjects [128]. In addition, Lucia et al. found that treatment with PIs, including ritonavir, saquinavir, nelfinavir and indinavir, reduced the efflux of rhodamine 123 in blood lymphocytes from healthy and HIV infected patients [119]. Lee et al. reported that PIs exerted differential effects [154]. In this study, MRP1 expression and efflux activity in healthy CD4+ T cells were reduced after the treatment of darunavir/ritonavir, but not after efavirenz treatment alone. In SHIV infected cynomolgus macaques, HAART (AZT, lamivudine, and indinavir) accentuated the infection-induced decrease of P-gp mRNA level, in macaque PBMCs and lymph node mononuclear cells [115]. The chemical-induced activation was shown to increase the expression and/or activity of P-gp and ENTs in primary lymphocytes [122, 130].
These studies demonstrate that drug transporters in immune cells are functional and they can influence the ARV drug uptake. Furthermore, the effect of concomitant presence of diseases and activating stimuli on transporter expression and functionality suggests possible implications for ARV drug delivery. Although few reports studied immune cells in female genital tissues and colorectum, preliminary evidence indicate expression of efflux transporters (Table 1) [94, 95]. It is necessary that new drug delivery methods are developed and utilized in targeting specific immune cells relevant to HIV transmission. Targeting ARVs to specific immune cells such as CD4+ T cells, macrophages, and DCs in blood and lymphatic system has proven efficacious previously [156–159]. These targeting methods could be further improved if transporter-relevant factors are considered.
3.2. Summary
The positive expression of multiple transporters in the tissues and cells relevant to HIV transmission indicates that these transporters may play a role in drug absorption and disposition and PrEP effectiveness. Especially, some important transporters (P-gp, BCRP, MRPs) have been demonstrated to localize in multiple cell types (epithelial cells, secretory glandular cells, vascular endothelial cells) in these tissues, indicating these transporters may affect multiple processes of drug handling in the tissues and cells. The uptake transporters were generally less studied compared to efflux transporters. OCTs, CNTs, ENTs, and OATPs can be detected in some tissues, however the expression profiles of OAT1 and OAT3, which are the major uptake transporters for TFV, were found to have minimal expression in the cervicovaginal tissues and their expression and activity remain unknown in the tissues and immune cells. The positively expressed transporters may be able to affect the drug PK in all the three compartments in HIV transmission (mucosal fluid, tissue, and blood).
The observation that transporters (e.g. P-gp) can be regulated by exogenous hormones, disease status, and concomitantly used drugs highlights the possibility that the transporter functionality may be variable under different pathophysiological conditions. It has been reported that many factors influence transporter expression and activity (varying level of sex hormones, age, gender, methods of lymphocyte activation, etc.) [57]. Finally, transporter information will help explain and predict the transporter-mediated drug-drug interaction, and inter-individual variability in ARV PK and PD. An important source of variability is pathophysiological factors including age, gender, and disease status, and the effects of these factors on ARV drug disposition and efficacy are mediated partially by transporters.
Contradictory reports have been observed for transporter expression and activity, especially in immune cells. There is large heterogeneity between different subsets of immune cells, and even within same subset (e.g. CD4+ T cells) [57]. In addition to the differences in experimental approaches, the potential inherent heterogeneity in immune cells being tested may also contribute to the observed conflicting results for transporter expression and activity in immune cells. However, MRP1 was consistently reported to be highly expressed in human lymphocytes [144, 160], indicating that this transporter may play a consistently significant role in the PK of ARVs in the immune cells. Taken together, there is a clear need for a more insightful understanding of the transporters in tissues and cells relevant to HIV sexual transmission.
4. Drug transporters in the pharmacokinetics of ARVs
4.1. ABC transporters in the pharmacokinetics of ARVs
In humans, the ABC transporter superfamily is further categorized into 7 families, from ABCA to ABCG [161, 162]. In this review, emphasis is given to ABCB1 (P-gp) from the ABCB subfamily, ABCC1 to 7 (MRP 1 to 7) from the ABCC subfamily, and ABCG2 (BCRP) from the ABCG subfamily, since they comprise the major efflux pumps for ARVs.
ABC transporters affect the intracellular accumulation of all classes of ARVs, such as MVC (EI), saquinavir (PI), TFV (NRTI), efavirenz (NNRTI), and raltegravir (II). Apart from being the substrates, xenobiotic and endogenous substances could also inhibit transporter activity by competitively binding to domains critical for transporter activity. For example, the PIs (e.g. ritonavir) are potent P-gp inhibitors, which exert their inhibitory effect through competitive binding to the extracellular domain of P-gp [58, 63]. Besides marketed drugs, some generally-regarded-as-safe (GRAS) excipients have been shown to potently inhibit ABC transporters, by temporarily depleting intracellular ATP availability and/or reversibly modifying plasma membrane fluidity [63, 163].
In tissues with high expression and/or critical localization of transporters, differential tissue distribution patterns of the substrates vs. non-substrates have been observed. In addition, genetic polymorphisms of a number of transporters are associated with inter-individual variability in ARV drug PK [164, 165]. Up-regulation or down-regulation of transporter expression/activity could alter ARV drug PK profile and efficacy [22, 166]. Co-administration of efflux transporter inhibitors, including ARVs and pharmaceutical excipients, has been shown to be an effective approach to enhance drug exposure in tissues with high levels of transporter expression [167]. Since many drugs can modulate transporter expression and activity, a significant portion of drug-drug interactions is mediated by transporters; more detailed information on this topic can be found in published reviews [21, 63, 64]. A compilation of efflux and uptake transporters and different classes of ARVs that are shown to be inhibitors or substrates of these transporters is listed in Table 2.
4.1.1. ABCB1 (P-gp)
Many ARVs are substrates of P-gp [58]. All PIs are high-affinity substrates of P-gp [5, 168–173]. In addition, the EI, MVC, the NRTIs such as tenofovir disoproxil fumarate (TDF) and abacavir, and some IIs such as raltegravir, can be transported by P-gp. At cellular level, P-gp is localized in epithelial cells, vascular endothelial cells, as well as the immune cells. Therefore, this transporter could affect drug transport across physiologic barriers that are constructed by epithelial cells (e.g. small intestinal enterocytes) and endothelial cells (blood-brain barrier), and in the immune cells. Due to the wide tissue distribution and broad substrate specificity, P-gp has been recognized as the major efflux pump responsible for cellular resistance to antiviral and anticancer drugs. Among ARVs, some PIs and NNRTIs can inhibit P-gp [174–179]. The plasma area under the curve (AUC) after oral administration of MVC (P-gp substrate) was 3 times higher in P-gp knockout mice compared to the wild type mice [180]. In humans, the concomitant use of P-gp inhibitors atazanavir, ritonavir, saquinavir and ketoconazole have been shown to significantly increase the Cmax and AUC of orally administered MVC up to 5 fold [181]. These studies highlight that P-gp plays an important role in the PK/PD of substrate ARV drugs.
4.1.2. ABCCs (MRPs)
MRPs belong to the C family of ABC superfamily, and transport a diverse array of ARVs [58]. The MRP members most relevant to ARVs are MRP1, 2, 4 and 5. MRP1 and MRP2 are shown to transport several PIs, including ritonavir, lopinavir, atazanavir, saquinavir, and indinavir [114, 182–185]. MRP1, 2, and 4 also mediate the efflux of many NRTIs. For example, MRP1 mediates emtricitabine efflux from lymphocytes. MRP2, 4, and 5 transport TFV [186–189]. Administration of TFV to Mrp4 knockout mice resulted in more than 2-fold higher TFV concentration in the kidney after intravenous administration [188]. In humans, genetic ABCC4 3463G variants lead to TFV-DP concentrations in PBMCs, which was significantly higher than that of wild type [116]. MRP5 has been shown to transport stavudine in vitro [187]. NNRTIs and NRTIs including delavirdine, efavirenz, and emtricitabine inhibit several MRPs at clinically relevant concentrations, as revealed in cell culture experiments [190]. In addition, NSAIDs such as indomethacin and ibuprofen are reported to be potent inhibitors of MRP4 [112, 191–193], and have been demonstrated to enhance the antiviral efficacy of NRTIs in HIV-1-infected T-lymphocytes [112].
4.1.3. ABCG2 (BCRP)
BCRP belongs to the G family of the ABC superfamily, and transports a number of ARVs from different classes [58]. As demonstrated in lymphocytes and BCRP-overexpressed cell cultures, this transporter confers resistance to many NRTIs, including abacavir, AZT, lamivudine, didanosine, and stavudine [194–197]. In Bcrp-knockout mice, the brain accumulation of abacavir was significantly increased [194]. BCRP genetic polymorphisms exerted an impact on its activity in vitro, however no in vivo correlation was observed between BCRP polymorphisms and the concentrations of AZT- and lamivudine-triphosphates [165]. Although PIs and NNRTIs are not BCRP substrates; [97] they have been demonstrated to be potent inhibitors of BCRP. In vitro assays demonstrated that PIs and NNRTIs such as ritonavir, saquinavir, nelfinavir, lopinavir, delavirdine, efavirenz, atazanavir, and amprenavir showed BCRP inhibition with IC50 values in micromolar range [97, 98] It should be noted that the in vivo free plasma concentration of PIs and NNRTIs are usually in nanomolar or micromolar range, thus the in vivo effect of these drugs on BCRP-mediated transport needs further investigation [98]. The BCRP-inhibiting drugs may at least play a role in the absorption process of co-administered drugs that are BCRP substrates, such as a number of NRTIs mentioned above [98].
4.2. SLC transporters in the pharmacokinetics of ARVs
SLC transporters are widely distributed in tissues and cells including liver, kidney, intestine, and immune system cells. This review focuses on the SLC subfamilies most relevant to ARVs, which are OATs, OCTs, CNTs, ENTs, and OATPs.
4.2.1. SLC22A family members (OATs and OCTs)
OATs and OCTs belong to the SLC22 family. They transport the ionized drugs across plasma membranes. In the PK of ARVs, the most extensively studied OATs are OAT1 (SLC22A6) and OAT3 (SLC22A8), which can transport TFV. On the basolateral membrane of renal proximal tubular epithelial cells, these two OATs facilitate the uptake of TFV from blood circulation into the renal epithelial cells, which could be subsequently effluxed by MRP4 into urine. The genetic polymorphisms of renal SLC22A6 are associated with TFV-induced kidney toxicity. OCT1 and OCT2 have been shown to transport several NRTIs including lamivudine and zalcitabine [198]. Among ARVs, some PIs including indinavir, nelfinavir, ritonavir, and saquinavir, can inhibit OCT1 and OCT2 activities in vitro [199].
4.2.2. SLC28 and SLC29 family members (CNTs and ENTs)
CNTs and ENTs belong to the SLC28 and SLC29 families, respectively. They are known to transport nucleoside analogues, including NRTIs. Based on their relative affinities to cellular nucleotides, CNTs are considered as high affinity transporters while ENTs are considered as low affinity transporters [200]. They are ubiquitously distributed in various types of tissues and cells. Among ARVs, AZT and lamivudine are transported by CNT1 [151, 201], and didanosine can be transported by CNT2 [202]. AZT and didanosine can be transported by ENT3, but the affinity of this transporter is low [203]. The NRTIs are well-known substrates of ENTs. For example, didanosine can be transported by ENT1 and ENT2, AZT can be transported by ENT2 [204], and stavudine and zalcitabine can be transported by ENT3 [21].
4.2.3. SLCO family members (OATPs)
The OATPs belong to the SLCO family. OATP1A2 and 1B1 are mostly studied OATPs in ARV drug PK. OATP1A2 and OATP1B1 transport PIs and EIs including darunavir, lopinavir, saquinavir and MVC in vitro [205–207]. An OATP1B1 polymorphism, 521T>C, was significantly associated with higher plasma levels of lopinavir and MVC in patients [206, 207]. In addition to being transported by OATPs, some PIs are potent inhibitors of OATP1B1 [208, 209].
4.3. Summary
The mentioned studies demonstrate that several subclasses of uptake and efflux transporters could affect the PK of ARVs. Furthermore, inhibition studies suggest that these transporters could be major determinants of ARVs absorption. Despite the scarcity of human studies on transporter function in FGT and colorectal tissues, it is apparent that multiple transporters, especially the ARV-relevant efflux transporters, are positively expressed in these tissues, and some are shown to affect the ARV PK and efficacy in these tissue sites. The cumulative effects of tissue and systemic transporter function dictate the drug levels in tissues and cells relevant to the sexual-transmission of HIV. Because specific ARVs have been shown to be inhibitors or inducers of transporter expression, the drug delivery methods should consider potential drug-drug interactions and the opportunities to utilize them as boosting agents. By understanding the factors that could influence drug disposition such as ARV-transporter interaction, expression of major transporters in compartments relevant to the route of delivery, and the influence of drug combinations, effective drug delivery strategies can be designed.
5. Drug delivery strategies to increase PrEP efficacy
The goal of drug delivery for PrEP-based HIV prevention is to increase drug accumulation in target tissues and cells. Studies demonstrate that drug transporters expressed in female genital tissues, colorectum, and immune cells could affect the systemic and tissue levels of ARVs. Therefore, transporter-dependent and transporter-independent drug delivery methods are needed to curb the negative impact of drug transporters. Several factors need to be considered for efficient drug delivery such as physiochemical aspects of ARVs, effect of combination drugs and excipients on transporter function, routes of administration, differential expression of transporters in cells and tissues involved in sexual HIV transmission, and influence of physiological and pathophysiological factors. The effect of drug transporters on tissue/cell uptake of drugs could be minimized by strategies that utilize inhibition, saturation, or circumvention of transporters.
Uptake and efflux transporters relevant to HIV drugs are ubiquitously expressed in the body [21, 166]. Therefore, the frequency and extent of drug exposure to transporters is dependent on the route of delivery. Anti-HIV drugs delivered through the oral route can be subjected to transporters in the gastrointestinal tract, immune cells in systemic circulation, and metabolism/elimination organs such as the liver and kidneys. For example, the availability of ARVs in the central nervous system is limited by P-gp expressed in the gastrointestinal tract as well as blood-brain-barrier (BBB) [5]. Local delivery approaches to vaginal and colorectal tissues using gels, tablets, films, vaginal rings, enemas, and suppositories could overcome some of these barriers. Intravaginal and rectal delivery can surpass first pass metabolism thus reducing drug-transporter interaction in the liver. However, patient adherence and inability to deliver uniform doses are potential challenges with insertion-based administration. In addition, genetic polymorphisms of transporters are shown to affect drug PK and contribute to inter-individual variability. Development of novel transporter-independent drug delivery strategies that can maintain sustained intracellular drug concentration should be considered.
5.1. Physiochemical properties of antiretroviral drugs
Drug delivery to target tissues and cells can be governed by the physiochemical properties of ARVs, namely, solubility, permeability, and protein binding. The tissue exposure of administered drugs can be greatly affected by these properties [22]. For a given ARV drug, being an in vitro substrate of a transporter does not necessarily mean that the transporter will play a significant role in the drug’s tissue absorption and disposition in vivo. The functional role of transporters is affected by the drug’s permeability and solubility [21, 210]. The Biopharmaceutics Classification System (BCS) categorizes different drugs into 4 classes according to drug permeability and solubility: Class 1, high permeability, high solubility; Class 2, high permeability, low solubility; Class 3, low permeability, high solubility; Class 4, low permeability, low solubility [210, 211]. The BCS classification, and the interaction with efflux transporters and uptake transporters are summarized for FDA-approved ARVs in Table 2.
Class 1 drugs, due to their relatively high permeability, can enter the tissue without the aid of uptake transporters [21, 210]. Three NRTIs, AZT, abacavir, and stavudine, belong to Class 1 (Table 2). These drugs can easily saturate the efflux transporters because they can quickly enter cells and accumulate high intracellular concentration. Therefore, the Class 1 drugs, including abacavir, AZT, stavudine and delavirdine, are not likely to be influenced by efflux and uptake transporters even if they are substrates (Table 2) [210].
Class 2 drugs are not likely to be affected by uptake transporters due to high permeability, but they are prone to be influenced by efflux transporters because their low solubility renders them unlikely to saturate efflux transporters [21, 210]. The efflux transporters are able to pump the drug back into the lumen (topical administration) or blood stream (oral administration), and the drug can re-enter the tissue and be repeatedly exposed to intracellular metabolizing enzymes. Therefore, a feature of Class 2 drugs is that they are more likely to be subjected to transporter-enzyme interplay [210]. As shown in Table 2, all the PIs, some NNRTIs such as nevirapine, and the IIs raltegravir belong to Class 2. Therefore, these drugs will be affected by efflux transporters.
Drugs from Class 3 and Class 4 require uptake transporters to accumulate in tissues due to their low permeability [21, 210]. The effect of uptake transporters is especially evident for Class 3 drugs which have relatively higher solubility [21]. These two classes also have the potential to be influenced by efflux transporters, since they are unlikely to achieve high intracellular concentrations that could saturate efflux transporters [21, 210]. As shown in Table 2, five NRTIs including lamivudine, emtricitabine, TDF, TFV, and didanosine belong to Class 3. The EI MVC also belongs to Class 3. Currently only one ARV drug etravirine (NNRTI) belongs to Class 4. These drugs may be influenced by both efflux and uptake transporters.
To summarize, efflux transporters mainly affect drugs from Classes 2, 3, and 4, especially Class 2 drugs. Uptake transporters mainly affect drugs from Classes 3 and 4, especially Class 3 drugs [21, 210]. In addition to solubility and permeability, protein binding is also a governing factor for tissue exposure of drugs [22]. It has been demonstrated that highly protein-bound ARVs show reduced mucosal tissue levels, i.e. in colorectal and cervicovaginal tissues. Of note, protein binding can differ between blood plasma and cervicovaginal fluid. For topical PrEP, protein binding within FGT may impact drug distribution in cervicovaginal tissues, immune cells, and local lymph nodes. Significant protein binding could reduce tissue drug levels because only the free drug form can permeate through the mucosal layers. Therefore, the prediction of the in vivo functional role of transporters in tissue drug exposure will need to incorporate the information of drug solubility, permeability, and protein binding of ARVs, even if the drugs are proven to be transporter substrates in vitro. In addition to BCS classification, the Biopharmaceutics Drug Disposition Classification System that incorporates transporter information should be utilized [210]. This information can guide formulating effective drug delivery systems that impact solubility, permeability, and protein binding, and achieve high target concentrations of ARVs.
5.2. Formulation
It is well known that formulation ingredients impact transporter functionality. For example, pharmaceutical excipients such as cremophor, pluronic P85, Vitamin E TPGS, and polysorbate 80 are potent P-gp inhibitors [163]. Similarly, excipients such as pluronic P85, polyethylene glycol 300, and cyclodextrins are reported to inhibit MRPs [163]. Cremophor EL has shown a dose-dependent increase in oral absorption of saquinavir, which is a substrate for P-gp [212]. Thiolated chitosan, which is used as a mucoadhesive and a permeation enhancing polymer, has been shown to inhibit P-gp [213]. Such multifunctional polymers could increase intracellular drug concentration through efflux transporter inhibition, permeation enhancement, and longer retention via mucoadhesion. Therefore, currently used oral and vaginal formulations for HIV can be modified to include these excipients to modulate the transporter function and increase the efficiency of drug delivery to the target cells. However, it is important to note that formulation excipients such as surfactants could potentially increase the membrane fluidity [214, 215], which could ultimately increase the probability of viral entry to the target cells. This aspect is particularly important for products designed for local application in the vaginal and rectal cavities.
Additionally, drug combinations containing transporter inhibitors can be sought to increase intracellular concentrations of drug of interest. Co-administration of multiple ARVs and drugs belonging to other classes has shown effect on transporter function and drug PK [58, 216]. HAART combines several ARVs to achieve significant reduction in viral activity [217]. For topical PrEP-based prevention of HIV acquisition, combination drugs have been utilized such as TFV and emtricitabine [218] for vaginal gels, TFV and dapivirine for vaginal gel [219], ring [220], and film [221], dapivirine and MVC [222] for vaginal rings, and TFV and nevirapine [223] for vaginal rings. In addition to the additive and synergistic roles of combination drugs, their effects on transporter functionality can guide the choice of drug combinations. For example, ARVs such as atazanavir, ritonavir, and saquinavir inhibit P-gp and increase oral absorption of MVC [181]. Due to the positive expression of P-gp in tissues and cells relevant to sexual-transmission of HIV, local delivery approaches can also benefit from these drug combinations. In addition to ARVs, NSAIDs have also shown P-gp inhibitory activity [112]. The combination of hormonal contraceptives and ARVs is sought to increase the use of ARV as prophylactic strategy in women [224]. Because sex hormones have been shown to modulate transporters [225], these combinations can also be guided by their effect on transporter function. Alternatively, recent studies indicate that ARVs alter the PK of hormonal contraceptives by either increasing or decreasing AUC [226, 227]. In addition to ARV effects on metabolizing enzymes, this effect could be partly influenced by transporter functions. It should be noted that some ARVs are associated with increased expression of efflux transporters or inhibition of uptake transporters, which should be considered for combination drug approach. The potential effects of these combinations on homeostatic roles of drug transporters need to be evaluated. Since the drugs can be substrates, inhibitors, or inducers of transporter function [228, 229], the complexity of this interplay needs validation in ex vivo and in vitro studies.
Sustained release formulations are being actively pursued as a means to improve patient product use compliance. Such strategies could also modulate transporter function by maintaining effective concentrations for longer periods, in addition to increasing patient adherence. Formulation methods that can increase drug absorption through solubility and permeability enhancement such as prodrugs, use of surfactants and permeation enhancers could also increase target concentration of ARVs. For vaginal and colorectal delivery, the use of mucoadhesives can increase the dosage form residence time and drug delivery efficacy. These methods can be effectively combined with transporter-function modifying excipients or drugs to achieve and sustain effective drug concentration at the target locales.
5.3. Nanomedicine and targeting approaches
Nanomedicine offers several opportunities to increase and sustain target concentrations of ARVs. Several reviews have been published in this area [230–232]. Compared to drug in solution, drug loaded in nanoparticles can markedly increase the target drug accumulation and sustain drug levels for a longer period of time [233]. Several studies demonstrated the use of nanoparticles to increase oral absorption by inhibition or circumvention of P-gp transporters [234, 235]. Beloqui et al. reported nanostructured lipid carriers to increase oral absorption of saquinavir by modifying physiochemical properties such as size, which effectively circumvented efflux by intestinal P-gp [234]. Nanoparticles functionalized with a cell penetrating peptide (TAT) have been utilized to evade P-gp transporters and increase permeability across cell membranes after intravenous administration [236]. This approach can be highly useful to deliver ARVs that are limited by permeability. Similar strategies could be employed to evade drug efflux from tissues and cells involved in sexual transmission of HIV. For vaginal drug delivery, nanoparticles have been shown to increase epithelial penetration and mucoadhesion [237, 238].
Immune cells in blood, lymph node, and lymphoid tissues act as reservoirs for HIV and are known to express efflux transporters, which reduce target drug accumulation. Nanoparticles could be utilized to target specific immune cells to increase cellular uptake and circumvent transporters. Several in vitro studies have been reported that utilized nanoparticles as potential vaginal delivery agents to immune cells. Yang et al. investigated antibody-functionalized saquanivir loaded nanoparticles to increase uptake in CD4+ T cells [239]. Specific peptides have also been reported for active targeting of CD4+ T cells [240]. Puligujja et al. reported ritonavir-boosted atazanavir nanocrystals conjugated with folic acid to target monocyte-macrophages [158]. These nanoparticles showed enhanced accumulation in macrophage-rich areas of lymph nodes and lymphoid tissues after intravenous administration. Nanoparticles containing anti-HIV drug combinations were also reported, which showed marked increase in accumulation in mononuclear cells in peripheral blood and lymph nodes [159].
In addition to nanoparticles, efforts were made to utilize prodrugs for targeting uptake transporters or inhibiting efflux transporters. In order to increase the uptake through BBB, Namanja et al. reported a dimeric prodrug of abacavir, which is a known susbtrate of P-gp. This prodrug inhibited P-gp, while preserving the anti-HIV efficacy in vitro [241]. A dipeptide prodrug of lopinavir was also utilized to circumvent P-gp and MRP2 [242]. Specific transporters are involved in uptake of ARVs. Prodrugs targeting uptake transporters have been successfully implemented to increase oral absorption of drugs such as acyclovir using L-valyl ester of acyclovir (valcylovir) [243]. The prodrug approach could be potentially utilized for ARVs used in oral and topical PrEP. However, prodrugs targeting uptake transporters might be less successful for vaginal drug delivery systems, because current studies indicate that these transporters are sparingly expressed in FGT.
6. Future directions
There is a lack of systematic characterization of transporter expression and localization in the transmission-relevant human tissues and cells, in the context of PrEP. Transporter expression and functionality studies should consider influencing factors such as varying blood hormone level (menstrual cycle stages and menopause), exogenously administered hormones, contraceptives, concomitantly administered drugs, pre-existing local tissue inflammation (e.g. vaginosis), which are frequently encountered by PrEP participants. These factors have been demonstrated to impact transporter expression in metabolic organs, but almost no studies investigated their effect on cervicovaginal and colorectal transporters. The FGT is a highly dynamic tissue due to drastic change in hormone levels during the menstrual cycle. This in turn, results in cyclic change in epithelial thickness, tight junction expression and passive permeability, and may also impact the expression/localization/activity of a variety of transporters, such as P-gp. Therefore, experimental design should reduce sources of variability. For example, female animals in the same group could be synchronized to a fixed stage of their menstrual (estrous) cycle using exogenously administered hormones. The effect of gender on colorectal and immune cell transporter expression is also an important consideration. This effect, if present, may result in differential PK behavior between men and women for the same drug in the same tissue compartment (e.g. colorectum).
The role of transporters, relevant to sexual transmission of HIV, in PrEP PK remains largely unknown. Although some transporters are positively expressed, it is unclear whether they significantly impact drug PK in the critical sites of HIV transmission (lumen, tissue, lymph nodes). In addition to the blood-derived immune cells, the effect of submucosal and lymphoid immune cells on drug PK needs further investigation. The transporter function in female genital and colorectal tissues has been occasionally studied, mostly as a barrier to topically administered drugs intended for systemic absorption. However, it is more important to know whether the transporters could affect drug distribution and retention within the tissues. Moreover, most of the reported transporter functionality studies were conducted in animal models, which have well-known limitations when used in microbicide testing, in terms of interspecies differences in reproductive tract anatomy, transporter expression level, as well as substrate and inhibitor spectra of transporters. All these interspecies differences warrant future human investigations to elucidate the function of cervicovaginal and colorectal transporters in the context of PrEP.
The role of drug transporters in the physiology of transmission-relevant tissues and cells remains elusive. The efflux and uptake transporters expressed in FGT, colorectal tissue, and immune cells also transport endogenous substances (endobiotics) such as sex hormones (e.g. 17-β-estradiol) [244] and hormone derivatives [245], and immune mediators [246] [247], which are critical in maintaining the physical and immunological barriers of mucosal tissues. The effect of co-administration of efflux transporter inhibitors and ARVs on tissue/cell homeostatic functions needs to be evaluated. In addition, some transporters have been suggested to directly affect HIV binding to the target cell [142], or participate in immune response such as DC migration [248]. Therefore, the net effect of transporter inhibition on the effectiveness of PrEP drugs remains unclear, and needs to be tested in efficacy models.
Utilizing the existing literature and future studies, there is a need to design drug delivery strategies that modulate transporter function and increase target drug concentrations in select tissues and cells. Although transporter inhibition has been utilized to increase bioavailability and CNS availability of ARVs in preclinical and clinical studies [249, 250], it has not been applied for PrEP-based HIV prevention.
There is also lack of studies targeting uptake and efflux transporters to increase drug accumulation in FGT and colorectal tissues. Novel drug delivery approaches utilizing nanoparticles, targeting ligands, and mucoadhesive polymers that affect transporter expression and function need to be developed. Overall, the outcomes from transporter research should be diligently utilized to design next generation drug delivery strategies for prevention of HIV acquisition.
7. Concluding remarks
A number of efflux and uptake transporters are positively expressed in the FGT, colorectal tissues, and immune cells that are susceptible to HIV sexual transmission. Given their high expression levels, and their localization in multiple cell types, it is tempting to speculate that transporters affect the tissue exposure and efficacy of ARVs used in PrEP. In addition, the modulation of transporters by chemical inhibitors, many of which are ARVs or pharmaceutical excipients, may exert beneficial effects on the PK and PD of PrEP drug candidates. However, more studies are warranted to confirm this speculation, and furthermore to identify the factors that could influence transporter expression/activity in the transmission-related tissues and cells. The existing knowledge summarized in this article, combined with the proposed future research, will likely facilitate successful delivery of PrEP drug candidates. Many anti-infective and anti-cancer drugs are also transporter substrates and/or modulators [63, 251]. The transporter information in cervicovaginal/colorectal tissues and immune cells will also shed light on the delivery and targeting of these drugs. Ultimately, an improved understanding of transporters in these tissues and cells will benefit large number of women and men that have various health issues.
Acknowledgments
This work was supported by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health under Award Number AI082639. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kruijtzer C, Beijnen J, Rosing H, ten Bokkel Huinink W, Schot M, Jewell R, Paul E, Schellens J. Increased oral bioavailability of topotecan in combination with the breast cancer resistance protein and P-glycoprotein inhibitor GF120918. Journal of Clinical Oncology. 2002;20:2943–2950. doi: 10.1200/JCO.2002.12.116. [DOI] [PubMed] [Google Scholar]
- 2.Malingré MM, Richel DJ, Beijnen JH, Rosing H, Koopman FJ, Huinink WWTB, Schot ME, Schellens JH. Coadministration of cyclosporine strongly enhances the oral bioavailability of docetaxel. Journal of Clinical Oncology. 2001;19:1160–1166. doi: 10.1200/JCO.2001.19.4.1160. [DOI] [PubMed] [Google Scholar]
- 3.Amin ML. P-glycoprotein Inhibition for Optimal Drug Delivery. Drug Target Insights. 2013;7:27–34. doi: 10.4137/DTI.S12519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Robillard KR, Chan GN, Zhang G, la Porte C, Cameron W, Bendayan R. Role of P-glycoprotein in the distribution of the HIV protease inhibitor atazanavir in the brain and male genital tract. Antimicrob Agents Chemother. 2014;58:1713–1722. doi: 10.1128/AAC.02031-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim RB, Fromm MF, Wandel C, Leake B, Wood AJ, Roden DM, Wilkinson GR. The drug transporter P-glycoprotein limits oral absorption and brain entry of HIV-1 protease inhibitors. J Clin Invest. 1998;101:289–294. doi: 10.1172/JCI1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.UNAIDS. UNAIDS Report on the Global AIDS Epidemic. 2013. [Google Scholar]
- 7.Palmer S, Josefsson L, Coffin JM. HIV reservoirs and the possibility of a cure for HIV infection. J Intern Med. 2011;270:550–560. doi: 10.1111/j.1365-2796.2011.02457.x. [DOI] [PubMed] [Google Scholar]
- 8.Baeten JM. New biomedical strategies for HIV-1 prevention in women. Curr Infect Dis Rep. 2008;10:490–498. doi: 10.1007/s11908-008-0080-1. [DOI] [PubMed] [Google Scholar]
- 9.Weiss HA, Halperin D, Bailey RC, Hayes RJ, Schmid G, Hankins CA. Male circumcision for HIV prevention: from evidence to action? Aids. 2008;22:567–574. doi: 10.1097/QAD.0b013e3282f3f406. [DOI] [PubMed] [Google Scholar]
- 10.Cottrell ML, Kashuba AD. Topical microbicides and HIV prevention in the female genital tract. J Clin Pharmacol. 2014;54:603–615. doi: 10.1002/jcph.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hladik F, Doncel GF. Preventing mucosal HIV transmission with topical microbicides: challenges and opportunities. Antiviral Res. 2010;88(Suppl 1):S3–9. doi: 10.1016/j.antiviral.2010.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McGowan I, Dezzutti C. Rectal Microbicide Development. Curr Top Microbiol Immunol. 2013 doi: 10.1007/82_2013_325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Romano J, Kashuba A, Becker S, Cummins J, Turpin J, Veronese F On Behalf Of The Antiretroviral Pharmacology In Hiv Prevention Think Tank Participants. Pharmacokinetics and Pharmacodynamics in HIV Prevention: Current Status and Future Directions: A Summary of the DAIDS and BMGF Sponsored Think Tank on Pharmacokinetics (PK)/Pharmacodynamics (PD) in HIV Prevention. AIDS Res Hum Retroviruses. 2013 doi: 10.1089/aid.2013.0122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haase AT. Early events in sexual transmission of HIV and SIV and opportunities for interventions. Annu Rev Med. 2011;62:127–139. doi: 10.1146/annurev-med-080709-124959. [DOI] [PubMed] [Google Scholar]
- 15.Haase AT. Targeting early infection to prevent HIV-1 mucosal transmission. Nature. 2010;464:217–223. doi: 10.1038/nature08757. [DOI] [PubMed] [Google Scholar]
- 16.Hendrix CW, Chen BA, Guddera V, Hoesley C, Justman J, Nakabiito C, Salata R, Soto-Torres L, Patterson K, Minnis AM, Gandham S, Gomez K, Richardson BA, Bumpus NN. MTN-001: Randomized Pharmacokinetic Cross-Over Study Comparing Tenofovir Vaginal Gel and Oral Tablets in Vaginal Tissue and Other Compartments. Plos One. 2013;8 doi: 10.1371/journal.pone.0055013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rohan LC, Devlin B, Yang H. Microbicide Dosage Forms. In: Nuttall J, editor. Microbicides for Prevention of HIV Infection. Springer; Berlin Heidelberg: 2014. pp. 27–54. [DOI] [PubMed] [Google Scholar]
- 18.Vermani K, Garg S. The scope and potential of vaginal drug delivery. Pharmaceutical science & technology today. 2000;3:359–364. doi: 10.1016/s1461-5347(00)00296-0. [DOI] [PubMed] [Google Scholar]
- 19.Karim SS, Kashuba AD, Werner L, Karim QA. Drug concentrations after topical and oral antiretroviral pre-exposure prophylaxis: implications for HIV prevention in women. Lancet. 2011;378:279–281. doi: 10.1016/S0140-6736(11)60878-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Richardson-Harman N, Mauck C, McGowan I, Anton P. Dose-response relationship between tissue concentrations of UC781 and explant infectibility with HIV type 1 in the RMP-01 rectal safety study. AIDS Res Hum Retroviruses. 2012;28:1422–1433. doi: 10.1089/aid.2012.0073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Minuesa G, Huber-Ruano I, Pastor-Anglada M, Koepsell H, Clotet B, Martinez-Picado J. Drug uptake transporters in antiretroviral therapy. Pharmacol Ther. 2011;132:268–279. doi: 10.1016/j.pharmthera.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 22.Thompson CG, Cohen MS, Kashuba AD. Antiretroviral pharmacology in mucosal tissues. J Acquir Immune Defic Syndr. 2013;63(Suppl 2):S240–247. doi: 10.1097/QAI.0b013e3182986ff8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Michaud V, Bar-Magen T, Turgeon J, Flockhart D, Desta Z, Wainberg MA. The Dual Role of Pharmacogenetics in HIV Treatment: Mutations and Polymorphisms Regulating Antiretroviral Drug Resistance and Disposition. Pharmacological Reviews. 2012;64:803–833. doi: 10.1124/pr.111.005553. [DOI] [PubMed] [Google Scholar]
- 24.Zhou T, Hu M, Cost M, Poloyac S, Rohan L. Expression of Transporters and Metabolizing Enzymes in the Female Lower Genital Tract: Implications for Microbicide Research. AIDS Res Hum Retroviruses. 2013 doi: 10.1089/aid.2013.0032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ter Heine R, Mulder JW, Van Gorp E, Wagenaar JF, Beijnen JH, Huitema AD. Intracellular and plasma steady-state pharmacokinetics of raltegravir, darunavir, etravirine and ritonavir in heavily pre-treated HIV-infected patients. British journal of clinical pharmacology. 2010;69:475–483. doi: 10.1111/j.1365-2125.2010.03634.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Siccardi M, Almond L, Schipani A, Csajka C, Marzolini C, Wyen C, Brockmeyer N, Boffito M, Owen A, Back D. Pharmacokinetic and pharmacodynamic analysis of efavirenz dose reduction using an in vitro–in vivo extrapolation model. Clinical Pharmacology & Therapeutics. 2012;92:494–502. doi: 10.1038/clpt.2012.61. [DOI] [PubMed] [Google Scholar]
- 27.Hendrix CW, Mayer K, Patterson K. DOSE-PROPORTIONALITY AND INTRA-INDIVIDUAL VARIABILITY OF INTRACELLULAR TENOFOVIR DIPHOSPHATE AND EMTRICITABINE TRIPHOSPHATE IN HEALTHY VOLUNTEERS. 2010 [Google Scholar]
- 28.Rohan LC, Sassi AB. Vaginal drug delivery systems for HIV prevention. AAPS J. 2009;11:78–87. doi: 10.1208/s12248-009-9082-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen PLBA, Hoesley C, Hendrix C, van der Straten A, Husnik M, et al. Safety and pharmacokinetics/pharmacodynamics of dapivirine and maraviroc vaginal rings [abstract no. 41]. 21st Conference on Retroviruses and Opportunistic Infections; Boston. 2014. [Google Scholar]
- 30.CONRAD. A Phase I Trial to Assess the Safety of Tenofovir Gel and Film Formulations: FAME 04 [Google Scholar]
- 31.MTN. First Trial of Combination ARV Vaginal Ring for HIV Prevention Finds Ring Safe but One ARV Carrying the Weight. Microbicide Trials Network; [Google Scholar]
- 32.Cole AM, Patton DL, Rohan LC, Cole AL, Cosgrove-Sweeney Y, Rogers NA, Ratner D, Sassi AB, Lackman-Smith C, Tarwater P, Ramratnam B, Ruchala P, Lehrer RI, Waring AJ, Gupta P. The formulated microbicide RC-101 was safe and antivirally active following intravaginal application in pigtailed macaques. PLoS One. 2010;5:e15111. doi: 10.1371/journal.pone.0015111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Van Damme L, Corneli A, Ahmed K, Agot K, Lombaard J, Kapiga S, Malahleha M, Owino F, Manongi R, Onyango J, Temu L, Monedi MC, Mak’Oketch P, Makanda M, Reblin I, Makatu SE, Saylor L, Kiernan H, Kirkendale S, Wong C, Grant R, Kashuba A, Nanda K, Mandala J, Fransen K, Deese J, Crucitti T, Mastro TD, Taylor D F.E.-P.S. Group. Preexposure prophylaxis for HIV infection among African women. N Engl J Med. 2012;367:411–422. doi: 10.1056/NEJMoa1202614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Trivedi RA, Mallawarachi C, UK-I JM, Graves MJ, Horsley J, Goddard MJ, Brown A, Wang L, Kirkpatrick PJ, Brown J, Gillard JH. Identifying inflamed carotid plaques using in vivo USPIO-enhanced MR imaging to label plaque macrophages. Arterioscler Thromb Vasc Biol. 2006;26:1601–1606. doi: 10.1161/01.ATV.0000222920.59760.df. [DOI] [PubMed] [Google Scholar]
- 35.Abdool Karim Q, Abdool Karim SS, Frohlich JA, Grobler AC, Baxter C, Mansoor LE, Kharsany AB, Sibeko S, Mlisana KP, Omar Z, Gengiah TN, Maarschalk S, Arulappan N, Mlotshwa M, Morris L, Taylor D C.T. Group. Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women. Science. 2010;329:1168–1174. doi: 10.1126/science.1193748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Collares-Buzato CB, Jepson MA, Simmons NL, Hirst BH. Increased tyrosine phosphorylation causes redistribution of adherens junction and tight junction proteins and perturbs paracellular barrier function in MDCK epithelia. European Journal of Cell Biology. 1998;76:85–92. doi: 10.1016/S0171-9335(98)80020-4. [DOI] [PubMed] [Google Scholar]
- 37.van der Straten A, Montgomery ET, Cheng H, Wegner L, Masenga G, von Mollendorf C, Bekker L, Ganesh S, Young K, Romano J, Nel A, Woodsong C. High acceptability of a vaginal ring intended as a microbicide delivery method for HIV prevention in African women. AIDS Behav. 2012;16:1775–1786. doi: 10.1007/s10461-012-0215-0. [DOI] [PubMed] [Google Scholar]
- 38.Smith DJ, Wakasiaka S, Hoang TD, Bwayo JJ, Del Rio C, Priddy FH. An evaluation of intravaginal rings as a potential HIV prevention device in urban Kenya: behaviors and attitudes that might influence uptake within a high-risk population. J Womens Health (Larchmt) 2008;17:1025–1034. doi: 10.1089/jwh.2007.0529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Thurman AR, Clark MR, Hurlburt JA, Doncel GF. Intravaginal rings as delivery systems for microbicides and multipurpose prevention technologies. Int J Womens Health. 2013;5:695–708. doi: 10.2147/IJWH.S34030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Derby N, Zydowsky T, Robbiani M. In search of the optimal delivery method for anti-HIV microbicides: are intravaginal rings the way forward? Expert Rev Anti Infect Ther. 2013;11:5–8. doi: 10.1586/eri.12.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.MTN. Microbicides: A Promising Strategy. Microbicide Trials Network; [Google Scholar]
- 42.Trezza CR, Kashuba AD. Pharmacokinetics of antiretrovirals in genital secretions and anatomic sites of HIV transmission: implications for HIV prevention. Clin Pharmacokinet. 2014;53:611–624. doi: 10.1007/s40262-014-0148-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nicol MR, Kashuba AD. Pharmacologic opportunities for HIV prevention. Clin Pharmacol Ther. 2010;88:598–609. doi: 10.1038/clpt.2010.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dumond JB, Yeh RF, Patterson KB, Corbett AH, Jung BH, Rezk NL, Bridges AS, Stewart PW, Cohen MS, Kashuba AD. Antiretroviral drug exposure in the female genital tract: implications for oral pre- and post-exposure prophylaxis. Aids. 2007;21:1899–1907. doi: 10.1097/QAD.0b013e328270385a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ravel J, Gajer P, Fu L, Mauck CK, Koenig SS, Sakamoto J, Motsinger-Reif AA, Doncel GF, Zeichner SL. Twice-daily application of HIV microbicides alter the vaginal microbiota. MBio. 2012;3 doi: 10.1128/mBio.00370-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Calmy A, Hirschel B, Cooper DA, Carr A. A new era of antiretroviral drug toxicity. Antivir Ther. 2009;14:165–179. doi: 10.1177/135965350901400203. [DOI] [PubMed] [Google Scholar]
- 47.Akil A, Parniak MA, Dezzutti CS, Moncla BJ, Cost MR, Li M, Rohan LC. Development and characterization of a vaginal film containing dapivirine, a non-nucleoside reverse transcriptase inhibitor (NNRTI), for prevention of HIV-1 sexual transmission. Drug delivery and translational research. 2011;1:209–222. doi: 10.1007/s13346-011-0022-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nuttall JP, Thake DC, Lewis MG, Ferkany JW, Romano JW, Mitchnick MA. Concentrations of dapivirine in the rhesus macaque and rabbit following once daily intravaginal administration of a gel formulation of [14C] dapivirine for 7 days. Antimicrobial agents and chemotherapy. 2008;52:909–914. doi: 10.1128/AAC.00330-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Malcolm RK, Veazey RS, Geer L, Lowry D, Fetherston SM, Murphy DJ, Boyd P, Major I, Shattock RJ, Klasse PJ. Sustained release of the CCR5 inhibitors CMPD167 and maraviroc from vaginal rings in rhesus macaques. Antimicrobial agents and chemotherapy. 2012;56:2251–2258. doi: 10.1128/AAC.05810-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Clark MR, Friend DR. Pharmacokinetics and topical vaginal effects of two tenofovir gels in rabbits. AIDS research and human retroviruses. 2012;28:1458–1466. doi: 10.1089/AID.2011.0328. [DOI] [PubMed] [Google Scholar]
- 51.Nuttall J, Kashuba A, Wang R, White N, Allen P, Roberts J, Romano J. Pharmacokinetics of tenofovir following intravaginal and intrarectal administration of tenofovir gel to rhesus macaques. Antimicrobial agents and chemotherapy. 2012;56:103–109. doi: 10.1128/AAC.00597-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pereira LE, Clark MR, Friend DR, Garber DA, McNicholl JM, Hendry RM, Doncel GF, Smith JM. Pharmacokinetic and safety analyses of tenofovir and tenofovir-emtricitabine vaginal tablets in pigtailed macaques. Antimicrobial agents and chemotherapy. 2014;58:2665–2674. doi: 10.1128/AAC.02336-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hafez E, Kenemans P. Atlas of Human Reproduction: By Scanning Electron Microscopy. Springer Science & Business Media; 2012. [Google Scholar]
- 54.Krstic RV. Human microscopic anatomy: an atlas for students of medicine and biology. Springer Science & Business Media; 2013. [Google Scholar]
- 55.Blaskewicz CD, Pudney J, Anderson DJ. Structure and function of intercellular junctions in human cervical and vaginal mucosal epithelia. Biol Reprod. 2011;85:97–104. doi: 10.1095/biolreprod.110.090423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chen BA, Panther L, Marzinke MA, Hendrix CW, Hoesley CJ, van der Straten A, Husnik MJ, Soto-Torres L, Nel A, Johnson S, Richardson-Harman N, Rabe LK, Dezzutti CS. Phase 1 Safety, Pharmacokinetics, and Pharmacodynamics of Dapivirine and Maraviroc Vaginal Rings: a Double-Blind Randomized Trial. J Acquir Immune Defic Syndr. 2015 doi: 10.1097/QAI.0000000000000702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Giraud C, Manceau S, Treluyer JM. ABC transporters in human lymphocytes: expression, activity and role, modulating factors and consequences for antiretroviral therapies. Expert Opin Drug Metab Toxicol. 2010;6:571–589. doi: 10.1517/17425251003601953. [DOI] [PubMed] [Google Scholar]
- 58.Kis O, Robillard K, Chan GNY, Bendayan R. The complexities of antiretroviral drug-drug interactions: role of ABC and SLC transporters. Trends in pharmacological sciences. 2010;31:22–35. doi: 10.1016/j.tips.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 59.Dumond JB, Patterson KB, Pecha AL, Werner RE, Andrews E, Damle B, Tressler R, Worsley J, Kashuba AD. Maraviroc concentrates in the cervicovaginal fluid and vaginal tissue of HIV-negative women. J Acquir Immune Defic Syndr. 2009;51:546–553. doi: 10.1097/QAI.0b013e3181ae69c5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Clavel C, Peytavin G, Tubiana R, Soulie C, Crenn-Hebert C, Heard I, Bissuel F, Ichou H, Ferreira C, Katlama C, Marcelin AG, Mandelbrot L. Raltegravir concentrations in the genital tract of HIV-1-infected women treated with a raltegravir-containing regimen (DIVA 01 study) Antimicrob Agents Chemother. 2011;55:3018–3021. doi: 10.1128/AAC.01460-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Thompson CG, Sedykh A, Nicol MR, Muratov E, Fourches D, Tropsha A, Kashuba AD. Cheminformatics Analysis to Identify Predictors of Antiviral Drug Penetration into the Female Genital Tract. AIDS Res Hum Retroviruses. 2014 doi: 10.1089/aid.2013.0254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zhou T, Hu M, Pearlman A, Patton D, Rohan L. Expression and localization of p-glycoprotein, multidrug resistance protein 4, and breast cancer resistance protein in the female lower genital tract of human and pigtailed macaque. AIDS Res Hum Retroviruses. 2014;30:1106–1116. doi: 10.1089/aid.2013.0281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.International Transporter C. Giacomini KM, Huang SM, Tweedie DJ, Benet LZ, Brouwer KL, Chu X, Dahlin A, Evers R, Fischer V, Hillgren KM, Hoffmaster KA, Ishikawa T, Keppler D, Kim RB, Lee CA, Niemi M, Polli JW, Sugiyama Y, Swaan PW, Ware JA, Wright SH, Yee SW, Zamek-Gliszczynski MJ, Zhang L. Membrane transporters in drug development. Nat Rev Drug Discov. 2010;9:215–236. doi: 10.1038/nrd3028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ho RH, Kim RB. Transporters and drug therapy: implications for drug disposition and disease. Clin Pharmacol Ther. 2005;78:260–277. doi: 10.1016/j.clpt.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 65.Leonard GD, Fojo T, Bates SE. The role of ABC transporters in clinical practice. Oncologist. 2003;8:411–424. doi: 10.1634/theoncologist.8-5-411. [DOI] [PubMed] [Google Scholar]
- 66.Luker GD, Fracasso PM, Dobkin J, Piwnica-Worms D. Modulation of the multidrug resistance P-glycoprotein: detection with technetium-99m-sestamibi in vivo. J Nucl Med. 1997;38:369–372. [PubMed] [Google Scholar]
- 67.Sasongko L, Link JM, Muzi M, Mankoff DA, Yang X, Collier AC, Shoner SC, Unadkat JD. Imaging P-glycoprotein transport activity at the human blood-brain barrier with positron emission tomography. Clin Pharmacol Ther. 2005;77:503–514. doi: 10.1016/j.clpt.2005.01.022. [DOI] [PubMed] [Google Scholar]
- 68.Kartenbeck J, Leuschner U, Mayer R, Keppler D. Absence of the canalicular isoform of the MRP gene-encoded conjugate export pump from the hepatocytes in Dubin-Johnson syndrome. Hepatology. 1996;23:1061–1066. doi: 10.1053/jhep.1996.v23.pm0008621134. [DOI] [PubMed] [Google Scholar]
- 69.Strautnieks SS, Bull LN, Knisely AS, Kocoshis SA, Dahl N, Arnell H, Sokal E, Dahan K, Childs S, Ling V, Tanner MS, Kagalwalla AF, Nemeth A, Pawlowska J, Baker A, Mieli-Vergani G, Freimer NB, Gardiner RM, Thompson RJ. A gene encoding a liver-specific ABC transporter is mutated in progressive familial intrahepatic cholestasis. Nat Genet. 1998;20:233–238. doi: 10.1038/3034. [DOI] [PubMed] [Google Scholar]
- 70.Kubitz R, Droge C, Stindt J, Weissenberger K, Haussinger D. The bile salt export pump (BSEP) in health and disease. Clin Res Hepatol Gastroenterol. 2012;36:536–553. doi: 10.1016/j.clinre.2012.06.006. [DOI] [PubMed] [Google Scholar]
- 71.Fromm MF. Importance of P-glycoprotein for drug disposition in humans. Eur J Clin Invest. 2003;33(Suppl 2):6–9. doi: 10.1046/j.1365-2362.33.s2.4.x. [DOI] [PubMed] [Google Scholar]
- 72.Endter S, Francombe D, Ehrhardt C, Gumbleton M. RT-PCR analysis of ABC, SLC and SLCO drug transporters in human lung epithelial cell models. Journal of Pharmacy and Pharmacology. 2009;61:583–591. doi: 10.1211/jpp/61.05.0006. [DOI] [PubMed] [Google Scholar]
- 73.Warren MS, Zerangue N, Woodford K, Roberts LM, Tate EH, Feng B, Li C, Feuerstein TJ, Gibbs J, Smith B. Comparative gene expression profiles of ABC transporters in brain microvessel endothelial cells and brain in five species including human. Pharmacological research. 2009;59:404–413. doi: 10.1016/j.phrs.2009.02.007. [DOI] [PubMed] [Google Scholar]
- 74.Chaudhary PM, Mechetner EB, Roninson I. Expression and activity of the multidrug resistance P-glycoprotein in human peripheral blood lymphocytes [see comments] Blood. 1992;80:2735–2739. [PubMed] [Google Scholar]
- 75.Nigam SK. What do drug transporters really do? Nature Reviews Drug Discovery. 2015;14:29–44. doi: 10.1038/nrd4461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Langmann T, Mauerer R, Zahn A, Moehle C, Probst M, Stremmel W, Schmitz G. Real-time reverse transcription-PCR expression profiling of the complete human ATP-binding cassette transporter superfamily in various tissues. Clin Chem. 2003;49:230–238. doi: 10.1373/49.2.230. [DOI] [PubMed] [Google Scholar]
- 77.Gunawardana M, Mullen M, Moss JA, Pyles RB, Nusbaum RJ, Patel J, Vincent KL, Wang C, Guo C, Yuan YC, Warden CD, Baum MM. Global Expression of Molecular Transporters in the Human Vaginal Tract: Implications for HIV Chemoprophylaxis. PLoS One. 2013;8 doi: 10.1371/journal.pone.0077340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Smith KA, Mukhopadhya I, Berry S, Hold GL, Hijazi K. Expression of Drug Transporters in Cervicovaginal Cell Lines and Modulatory Effect of Candidate Anti-retroviral Microbicides. AIDS Res Hum Retroviruses. 2014;30:A201–A201. [Google Scholar]
- 79.Schinkel AH, Mayer U, Wagenaar E, Mol CAAM, van Deemter L, Smit JJM, van der Valk MA, Voordouw AC, Spits H, van Tellingen O, Zijlmans JMJM, Fibbe WE, Borst P. Normal viability and altered pharmacokinetics in mice lacking mdr1-type (drug-transporting) P-glycoproteins (vol 94, pg 4028, 1997) Proc Natl Acad Sci U S A. 2003;100:8036–8036. doi: 10.1073/pnas.94.8.4028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Grammen C, Baes M, Haenen S, Verguts J, Augustyns K, Zydowsky T, La Colla P, Augustijns P, Brouwers J. Vaginal Expression of Efflux Transporters and the Potential Impact on the Disposition of Microbicides in Vitro and in Rabbits. Mol Pharm. 2014 doi: 10.1021/mp5005004. [DOI] [PubMed] [Google Scholar]
- 81.Axiotis CA, Guarch R, Merino MJ, Laporte N, Neumann RD. P-glycoprotein expression is increased in human secretory and gestational endometrium. Lab Invest. 1991;65:577–581. [PubMed] [Google Scholar]
- 82.Lacroix-Pepin N, Danyod G, Krishnaswamy N, Mondal S, Rong PM, Chapdelaine P, Fortier MA. The Multidrug Resistance-Associated Protein 4 (MRP4) Appears as a Functional Carrier of Prostaglandins Regulated by Oxytocin in the Bovine Endometrium. Endocrinology. 2011;152:4993–5004. doi: 10.1210/en.2011-1406. [DOI] [PubMed] [Google Scholar]
- 83.Gori I, Rodriguez Y, Pellegrini C, Achtari C, Hornung D, Chardonnens E, Wunder D, Fiche M, Canny GO. Augmented epithelial multidrug resistance-associated protein 4 expression in peritoneal endometriosis: regulation by lipoxin A4. Fertil Steril. 2013;99:1965–1973 e1962. doi: 10.1016/j.fertnstert.2013.01.146. [DOI] [PubMed] [Google Scholar]
- 84.Staudinger JL, Woody S, Sun M, Cui W. Nuclear-receptor-mediated regulation of drug- and bile-acid-transporter proteins in gut and liver. Drug metabolism reviews. 2013;45:48–59. doi: 10.3109/03602532.2012.748793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Schindler AE, Campagnoli C, Druckmann R, Huber J, Pasqualini JR, Schweppe KW, Thijssen JH. Classification and pharmacology of progestins. Maturitas. 2008;61:171–180. doi: 10.1016/j.maturitas.2008.11.013. [DOI] [PubMed] [Google Scholar]
- 86.Thurman AR, Anderson S, Doncel GF. Effects of hormonal contraception on antiretroviral drug metabolism, pharmacokinetics and pharmacodynamics. Am J Reprod Immunol. 2014;71:523–530. doi: 10.1111/aji.12210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Abdool Karim Q, Abdool Karim SS, Frohlich JA, Grobler AC, Baxter C, Mansoor LE, Kharsany AB, Sibeko S, Mlisana KP, Omar Z, Gengiah TN, Maarschalk S, Arulappan N, Mlotshwa M, Morris L, Taylor D. Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women. Science. 2010;329:1168–1174. doi: 10.1126/science.1193748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Axiotis CA, Monteagudo C, Merino MJ, LaPorte N, Neumann RD. Immunohistochemical detection of P-glycoprotein in endometrial adenocarcinoma. Am J Pathol. 1991;138:799–806. [PMC free article] [PubMed] [Google Scholar]
- 89.Bleasby K, Castle JC, Roberts CJ, Cheng C, Bailey WJ, Sina JF, Kulkarni AV, Hafey MJ, Evers R, Johnson JM, Ulrich RG, Slatter JG. Expression profiles of 50 xenobiotic transporter genes in humans and pre-clinical species: A resource for investigations into drug disposition. Xenobiotica. 2006;36:963–988. doi: 10.1080/00498250600861751. [DOI] [PubMed] [Google Scholar]
- 90.Finstad CL, Saigo PE, Rubin SC, Federici MG, Provencher DM, Hoskins WJ, Lewis JL, Jr, Lloyd KO. Immunohistochemical localization of P-glycoprotein in adult human ovary and female genital tract of patients with benign gynecological conditions. J Histochem Cytochem. 1990;38:1677–1681. doi: 10.1177/38.11.1976674. [DOI] [PubMed] [Google Scholar]
- 91.Nicol M, Fedoriw Y, Mathews M, Micheli J, Kroetz D, Kashuba A. Gene and protein expression of drug transporters in vaginal, cervical, and rectal tissues: implications for drug disposition in HIV prevention. XX Conference on Retroviruses and Opportunistic Infections; Atlanta, GA. 2013. [Google Scholar]
- 92.Schneider J, Efferth T, Mattern J, Rodriguez-Escudero FJ, Volm M. Immunohistochemical detection of the multi-drug-resistance marker P-glycoprotein in uterine cervical carcinomas and normal cervical tissue. Am J Obstet Gynecol. 1992;166:825–829. doi: 10.1016/0002-9378(92)91341-7. [DOI] [PubMed] [Google Scholar]
- 93.Maliepaard M, Scheffer GL, Faneyte IF, van Gastelen MA, Pijnenborg AC, Schinkel AH, van De Vijver MJ, Scheper RJ, Schellens JH. Subcellular localization and distribution of the breast cancer resistance protein transporter in normal human tissues. Cancer Res. 2001;61:3458–3464. [PubMed] [Google Scholar]
- 94.Nicol MR, Fedoriw Y, Mathews M, Prince HM, Patterson KB, Geller E, Mollan K, Mathews S, Kroetz DL, Kashuba AD. Expression of six drug transporters in vaginal, cervical, and colorectal tissues: Implications for drug disposition in HIV prevention. J Clin Pharmacol. 2013 doi: 10.1002/jcph.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Blokzijl H, Vander Borght S, Bok LIH, Libbrecht L, Geuken M, Van den Heuvel FAJ, Dijkstra G, Roskams TAD, Moshage H, Jansen PLM, Faber KN. Decreased P-glycoprotein (P-gp/MDR1) expression in inflamed human intestinal epithelium is independent of PXR protein levels. Inflamm Bowel Dis. 2007;13:710–720. doi: 10.1002/ibd.20088. [DOI] [PubMed] [Google Scholar]
- 96.Bogush EA, Ravcheeva AB, Konukhova AV, Bogush TA, Komov DV, Baryshnikov A, Kalganov ID, Zhuchenko AP. Functional activity of ABC transporters (markers of multidrug resistance) in human colon adenocarcinoma and normal colonic mucosa. Antibiot Khimioter. 2002;47:3–8. [PubMed] [Google Scholar]
- 97.Calcagno AM, Ludwig JA, Fostel JM, Gottesman MM, Ambudkar SV. Comparison of drug transporter levels in normal colon, colon cancer, and Caco-2 cells: Impact on drug disposition and discovery. Mol Pharm. 2006;3:87–93. doi: 10.1021/mp050090k. [DOI] [PubMed] [Google Scholar]
- 98.Collett A, Stephens RH, Harwood MD, Humphrey M, Dallman L, Bennett J, Davis J, Carlson GL, Warhurst G. Investigation of regional mechanisms responsible for poor oral absorption in humans of a modified release preparation of the alpha-adrenoreceptor antagonist, 4-amino-6,7-dimethoxy-2(5-methanesulfonamido-1,2,3,4 tetrahydroisoquinol-2-yl)-5(2-pyridyl)quinazoline (UK-338,003): The rational use of ex vivo intestine to predict in vivo absorption. Drug Metabolism and Disposition. 2008;36:87–94. doi: 10.1124/dmd.107.016865. [DOI] [PubMed] [Google Scholar]
- 99.Cordoncardo C, Obrien JP, Boccia J, Casals D, Bertino JR, Melamed MR. Expression of the Multidrug Resistance Gene-Product (P-Glycoprotein) in Human Normal and Tumor-Tissues. Journal of Histochemistry & Cytochemistry. 1990;38:1277–1287. doi: 10.1177/38.9.1974900. [DOI] [PubMed] [Google Scholar]
- 100.Englund G, Jacobson A, Rorsmon F, Artursson P, Kindmark A, Ronnblom A. Efflux transporters in ulcerative colitis: Decreased expression of BCRP (ABCG2) and Pgp (ABCB1) Inflamm Bowel Dis. 2007;13:291–297. doi: 10.1002/ibd.20030. [DOI] [PubMed] [Google Scholar]
- 101.Enokizono J, Kusuhara H, Sugiyama Y. Regional expression and activity of breast cancer resistance protein (Bcrp/Abcg2) in mouse intestine: overlapping distribution with sulfotransferases. Drug Metabolism and Disposition. 2007;35:922–928. doi: 10.1124/dmd.106.011239. [DOI] [PubMed] [Google Scholar]
- 102.Fojo AT, Ueda K, Slamon DJ, Poplack DG, Gottesman MM, Pastan I. Expression of a Multidrug-Resistance Gene in Human-Tumors and Tissues. Proc Natl Acad Sci U S A. 1987;84:265–269. doi: 10.1073/pnas.84.1.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Hilgendorf C, Ahlin G, Seithel A, Artursson P, Ungell AL, Karlsson J. Expression of thirty-six drug transporter genes in human intestine, liver, kidney, and organotypic cell lines. Drug Metabolism and Disposition. 2007;35:1333–1340. doi: 10.1124/dmd.107.014902. [DOI] [PubMed] [Google Scholar]
- 104.Kleberg K, Jensen GM, Christensen DP, Lundh M, Grunnet LG, Knuhtsen S, Poulsen SS, Hansen MB, Bindslev N. Transporter function and cyclic AMP turnover in normal colonic mucosa from patients with and without colorectal neoplasia. Bmc Gastroenterology. 2012;12 doi: 10.1186/1471-230X-12-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.De Rosa THMF, Kim CJ, Kandel G, Kovacs C, Kaul R, Bendayan R. Expression of Membrane Drug Transporters in Rectosigmoid Colon from HIV Infected Men: Potential Role in Microbicide permeability. Microbicides 2010 Conference; Pittsburgh, PA, USA. 2010. [Google Scholar]
- 106.Prime-Chapman HM, Fearn RA, Cooper AE, Moore V, Hirst BH. Differential multidrug resistance-associated protein 1 through 6 isoform expression and function in human intestinal epithelial Caco-2 cells. Journal of Pharmacology and Experimental Therapeutics. 2004;311:476–484. doi: 10.1124/jpet.104.068775. [DOI] [PubMed] [Google Scholar]
- 107.Seithel A, Karlsson J, Hilgendorf C, Bjorquist A, Ungell AL. Variability in mRNA expression of ABC- and SLC-transporters in human intestinal cells: comparison between human segments and Caco-2 cells. Eur J Pharm Sci. 2006;28:291–299. doi: 10.1016/j.ejps.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 108.Zimmermann C, Gutmann H, Hruz P, Gutzwiller JP, Beglinger C, Drewe J. Mapping of multidrug resistance gene 1 and multidrug resistance-associated protein isoform 1 to 5 mRNA expression along the human intestinal tract. Drug Metabolism and Disposition. 2005;33:219–224. doi: 10.1124/dmd.104.001354. [DOI] [PubMed] [Google Scholar]
- 109.De Rosa MF, Robillard KR, Kim CJ, Hoque MT, Kandel G, Kovacs C, Kaul R, Bendayan R. Expression of membrane drug efflux transporters in the sigmoid colon of HIV-infected and uninfected men. J Clin Pharmacol. 2013;53:934–945. doi: 10.1002/jcph.132. [DOI] [PubMed] [Google Scholar]
- 110.Agrati C, Poccia F, Topino S, Narciso P, Selva C, Pucillo LP, D’Offizi G, Antonelli G, Bellomi F, Turriziani O, Bambacioni F. P-glycoprotein expression by peripheral blood mononuclear cells from human immunodeficiency virus-infected patients is independent from response to highly active antiretroviral therapy. Clin Diagn Lab Immunol. 2003;10:191–192. doi: 10.1128/CDLI.10.1.191-192.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ansermot N, Rebsamen M, Chabert J, Fathi M, Gex-Fabry M, Daali Y, Besson M, Rossier M, Rudaz S, Hochstrasser D, Dayer P, Desmeules J. Influence of ABCB1 gene polymorphisms and P-glycoprotein activity on cyclosporine pharmacokinetics in peripheral blood mononuclear cells in healthy volunteers. Drug Metab Lett. 2008;2:76–82. doi: 10.2174/187231208784040951. [DOI] [PubMed] [Google Scholar]
- 112.Clemente MI, Alvarez S, Serramia MJ, Turriziani O, Genebat M, Leal M, Fresno M, Munoz-Fernandez MA. Non-steroidal anti-inflammatory drugs increase the antiretroviral activity of nucleoside reverse transcriptase inhibitors in HIV type-1-infected T-lymphocytes: role of multidrug resistance protein 4. Antivir Ther. 2009;14:1101–1111. doi: 10.3851/IMP1468. [DOI] [PubMed] [Google Scholar]
- 113.Gollapud S, Gupta S. Anti-P-glycoprotein antibody-induced apoptosis of activated peripheral blood lymphocytes: a possible role of P-glycoprotein in lymphocyte survival. J Clin Immunol. 2001;21:420–430. doi: 10.1023/a:1013177710941. [DOI] [PubMed] [Google Scholar]
- 114.Janneh O, Owen A, Chandler B, Hartkoorn RC, Hart CA, Bray PG, Ward SA, Back DJ, Khoo SH. Modulation of the intracellular accumulation of saquinavir in peripheral blood mononuclear cells by inhibitors of MRP1, MRP2, P-gp and BCRP. Aids. 2005;19:2097–2102. doi: 10.1097/01.aids.0000194793.36175.40. [DOI] [PubMed] [Google Scholar]
- 115.Jorajuria S, Clayette P, Dereuddre-Bosquet N, Benlhassan-Chahour K, Thiebot H, Vaslin B, Le Grand R, Dormont D. The expression of P-glycoprotein and cellular kinases is modulated at the transcriptional level by infection and highly active antiretroviral therapy in a primate model of AIDS. AIDS Res Hum Retroviruses. 2003;19:307–311. doi: 10.1089/088922203764969500. [DOI] [PubMed] [Google Scholar]
- 116.Kiser JJ, Aquilante CL, Anderson PL, King TM, Carten ML, Fletcher CV. Clinical and genetic determinants of intracellular tenofovir diphosphate concentrations in HIV-infected patients. J Acquir Immune Defic Syndr. 2008;47:298–303. doi: 10.1097/qai.0b013e31815e7478. [DOI] [PubMed] [Google Scholar]
- 117.Liptrott NJ, Penny M, Bray PG, Sathish J, Khoo SH, Back DJ, Owen A. The impact of cytokines on the expression of drug transporters, cytochrome P450 enzymes and chemokine receptors in human PBMC. Br J Pharmacol. 2009;156:497–508. doi: 10.1111/j.1476-5381.2008.00050.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Lucia MB, Rutella S, Leone G, Larocca LM, Vella S, Cauda R. In vitro and in vivo modulation of MDR1/P-glycoprotein in HIV-infected patients administered highly active antiretroviral therapy and liposomal doxorubicin. J Acquir Immune Defic Syndr. 2002;30:369–378. doi: 10.1097/00042560-200208010-00001. [DOI] [PubMed] [Google Scholar]
- 119.Lucia MB, Rutella S, Leone G, Vella S, Cauda R. HIV-protease inhibitors contribute to P-glycoprotein efflux function defect in peripheral blood lymphocytes from HIV-positive patients receiving HAART. J Acquir Immune Defic Syndr. 2001;27:321–330. doi: 10.1097/00126334-200108010-00001. [DOI] [PubMed] [Google Scholar]
- 120.Malorni W, Lucia MB, Rainaldi G, Cauda R, Cianfriglia M, Donelli G, Ortona L. Intracellular expression of P-170 glycoprotein in peripheral blood mononuclear cell subsets from healthy donors and HIV-infected patients. Haematologica. 1998;83:13–20. [PubMed] [Google Scholar]
- 121.Meaden ER, Hoggard PG, Khoo SH, Back DJ. Determination of P-gp and MRP1 expression and function in peripheral blood mononuclear cells in vivo. J Immunol Methods. 2002;262:159–165. doi: 10.1016/s0022-1759(02)00020-0. [DOI] [PubMed] [Google Scholar]
- 122.Minuesa G, Purcet S, Erkizia I, Molina-Arcas M, Bofill M, Izquierdo-Useros N, Casado FJ, Clotet B, Pastor-Anglada M, Martinez-Picado J. Expression and functionality of anti-human immunodeficiency virus and anticancer drug uptake transporters in immune cells. Journal of Pharmacology and Experimental Therapeutics. 2008;324:558–567. doi: 10.1124/jpet.107.131482. [DOI] [PubMed] [Google Scholar]
- 123.Park SW, Lomri N, Simeoni LA, Fruehauf JP, Mechetner E. Analysis of P-glycoprotein-mediated membrane transport in human peripheral blood lymphocytes using the UIC2 shift assay. Cytometry A. 2003;53:67–78. doi: 10.1002/cyto.a.10039. [DOI] [PubMed] [Google Scholar]
- 124.Storch CH, Nikendei C, Schild S, Haefeli WE, Weiss J, Herzog W. Expression and activity of P-glycoprotein (MDR1/ABCB1) in peripheral blood mononuclear cells from patients with anorexia nervosa compared with healthy controls. Int J Eat Disord. 2008;41:432–438. doi: 10.1002/eat.20519. [DOI] [PubMed] [Google Scholar]
- 125.Tanaka S, Hirano T, Saito T, Wakata N, Oka K. P-glycoprotein function in peripheral blood mononuclear cells of myasthenia gravis patients treated with tacrolimus. Biol Pharm Bull. 2007;30:291–296. doi: 10.1248/bpb.30.291. [DOI] [PubMed] [Google Scholar]
- 126.Troost J, Albermann N, Emil Haefeli W, Weiss J. Cholesterol modulates P-glycoprotein activity in human peripheral blood mononuclear cells. Biochem Biophys Res Commun. 2004;316:705–711. doi: 10.1016/j.bbrc.2004.02.102. [DOI] [PubMed] [Google Scholar]
- 127.Turriziani O, Gianotti N, Falasca F, Boni A, Vestri AR, Zoccoli A, Lazzarin A, Antonelli G. Expression levels of MDR1, MRP1, MRP4, and MRP5 in peripheral blood mononuclear cells from HIV infected patients failing antiretroviral therapy. J Med Virol. 2008;80:766–771. doi: 10.1002/jmv.21152. [DOI] [PubMed] [Google Scholar]
- 128.Chinn LW, Gow JM, Tse MM, Becker SL, Kroetz DL. Interindividual variability in the effect of atazanavir and saquinavir on the expression of lymphocyte P-glycoprotein. Journal of Antimicrobial Chemotherapy. 2007;60:61–67. doi: 10.1093/jac/dkm135. [DOI] [PubMed] [Google Scholar]
- 129.Gupta S, Gollapudi S. P-glycoprotein (MDR 1 gene product) in cells of the immune system: its possible physiologic role and alteration in aging and human immunodeficiency virus-1 (HIV-1) infection. J Clin Immunol. 1993;13:289–301. doi: 10.1007/BF00920237. [DOI] [PubMed] [Google Scholar]
- 130.Gupta S, Kim CH, Tsuruo T, Gollapudi S. Preferential expression and activity of multidrug resistance gene 1 product (P-glycoprotein), a functionally active efflux pump, in human CD8+ T cells: a role in cytotoxic effector function. J Clin Immunol. 1992;12:451–458. doi: 10.1007/BF00918857. [DOI] [PubMed] [Google Scholar]
- 131.Janneh O, Jones E, Chandler B, Owen A, Khoo SH. Inhibition of P-glycoprotein and multidrug resistance-associated proteins modulates the intracellular concentration of lopinavir in cultured CD4 T cells and primary human lymphocytes. Journal of Antimicrobial Chemotherapy. 2007;60:987–993. doi: 10.1093/jac/dkm353. [DOI] [PubMed] [Google Scholar]
- 132.Jones K, Bray PG, Khoo SH, Davey RA, Meaden ER, Ward SA, Back DJ. P-glycoprotein and transporter MRP1 reduce HIV protease inhibitor uptake in CD4 cells: potential for accelerated viral drug resistance? Aids. 2001;15:1353–1358. doi: 10.1097/00002030-200107270-00004. [DOI] [PubMed] [Google Scholar]
- 133.Janneh O, Bray PG, Jones E, Wyen C, Chiba P, Back DJ, Khoo SH. Concentration-dependent effects and intracellular accumulation of HIV protease inhibitors in cultured CD4 T cells and primary human lymphocytes. Journal of Antimicrobial Chemotherapy. 2010;65:906–916. doi: 10.1093/jac/dkq082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Ford J, Khoo SH, Back DJ. The intracellular pharmacology of antiretroviral protease inhibitors. Journal of Antimicrobial Chemotherapy. 2004;54:982–990. doi: 10.1093/jac/dkh487. [DOI] [PubMed] [Google Scholar]
- 135.Bleiber G, May M, Suarez C, Martinez R, Marzolini C, Egger M, Telenti A, Swiss HIVCS. MDR1 genetic polymorphism does not modify either cell permissiveness to HIV-1 or disease progression before treatment. J Infect Dis. 2004;189:583–586. doi: 10.1086/380134. [DOI] [PubMed] [Google Scholar]
- 136.Bossi P, Legrand O, Faussat AM, Legrand M, Bricaire F, Marie JP, Agut H, Diquet B, Katlama C, Huraux JM, Calvez V. P-glycoprotein in blood CD4 cells of HIV-1-infected patients treated with protease inhibitors. HIV Med. 2003;4:67–71. doi: 10.1046/j.1468-1293.2003.00134.x. [DOI] [PubMed] [Google Scholar]
- 137.Elliott JI, Raguz S, Higgins CF. Multidrug transporter activity in lymphocytes. Br J Pharmacol. 2004;143:899–907. doi: 10.1038/sj.bjp.0705940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Gollapudi S, Gupta S. Human immunodeficiency virus I-induced expression of P-glycoprotein. Biochem Biophys Res Commun. 1990;171:1002–1007. doi: 10.1016/0006-291x(90)90783-j. [DOI] [PubMed] [Google Scholar]
- 139.Haraguchi S, Ho SK, Morrow M, Goodenow MM, Sleasman JW. Developmental regulation of P-glycoprotein activity within thymocytes results in increased anti-HIV protease inhibitor activity. J Leukoc Biol. 2011;90:653–660. doi: 10.1189/jlb.0111-009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Hulgan T, Donahue JP, Hawkins C, Unutmaz D, D’Aquila RT, Raffanti S, Nicotera F, Rebeiro P, Erdem H, Rueff M, Haas DW. Implications of T-cell P-glycoprotein activity during HIV-1 infection and its therapy. J Acquir Immune Defic Syndr. 2003;34:119–126. doi: 10.1097/00126334-200310010-00001. [DOI] [PubMed] [Google Scholar]
- 141.Kyle-Cezar F, Echevarria-Lima J, Rumjanek VM. Independent regulation of ABCB1 and ABCC activities in thymocytes and bone marrow mononuclear cells during aging. Scand J Immunol. 2007;66:238–248. doi: 10.1111/j.1365-3083.2007.01965.x. [DOI] [PubMed] [Google Scholar]
- 142.Lee CG, Ramachandra M, Jeang KT, Martin MA, Pastan I, Gottesman MM. Effect of ABC transporters on HIV-1 infection: inhibition of virus production by the MDR1 transporter. FASEB J. 2000;14:516–522. doi: 10.1096/fasebj.14.3.516. [DOI] [PubMed] [Google Scholar]
- 143.Liptrott NJ, Pushpakom S, Wyen C, Fatkenheuer G, Hoffmann C, Mauss S, Knechten H, Brockmeyer NH, Hopper-Borge E, Siccardi M, Back DJ, Khoo SH, Pirmohamed M, Owen A H.A. German Competence Network for. Association of ABCC10 polymorphisms with nevirapine plasma concentrations in the German Competence Network for HIV/AIDS. Pharmacogenet Genomics. 2012;22:10–19. doi: 10.1097/FPC.0b013e32834dd82e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Meaden ER, Hoggard PG, Newton P, Tjia JF, Aldam D, Cornforth D, Lloyd J, Williams I, Back DJ, Khoo SH. P-glycoprotein and MRP1 expression and reduced ritonavir and saquinavir accumulation in HIV-infected individuals. J Antimicrob Chemother. 2002;50:583–588. doi: 10.1093/jac/dkf161. [DOI] [PubMed] [Google Scholar]
- 145.Sankatsing SU, Cornelissen M, Kloosterboer N, Crommentuyn KM, Bosch TM, Mul FP, Jurriaans S, Huitema AD, Beijnen JH, Lange JM, Prins JM, Schuitemaker H. Antiviral activity of HIV type 1 protease inhibitors nelfinavir and indinavir in vivo is not influenced by P-glycoprotein activity on CD4+ T cells. AIDS Res Hum Retroviruses. 2007;23:19–27. doi: 10.1089/aid.2006.0027. [DOI] [PubMed] [Google Scholar]
- 146.Speck RR, Yu XF, Hildreth J, Flexner C. Differential effects of p-glycoprotein and multidrug resistance protein-1 on productive human immunodeficiency virus infection. J Infect Dis. 2002;186:332–340. doi: 10.1086/341464. [DOI] [PubMed] [Google Scholar]
- 147.Jorajuria S, Dereuddre-Bosquet N, Naissant-Storck K, Dormont D, Clayette P. Differential expression levels of MRP1, MRP4, and MRP5 in response to human immunodeficiency virus infection in human macrophages. Antimicrob Agents Chemother. 2004;48:1889–1891. doi: 10.1128/AAC.48.5.1889-1891.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Jorajuria S, Dereuddre-Bosquet N, Becher F, Martin S, Porcheray F, Garrigues A, Mabondzo A, Benech H, Grassi J, Orlowski S, Dormont D, Clayette P. ATP binding cassette multidrug transporters limit the anti-HIV activity of zidovudine and indinavir in infected human macrophages. Antivir Ther. 2004;9:519–528. [PubMed] [Google Scholar]
- 149.Puddu P, Fais S, Luciani F, Gherardi G, Dupuis ML, Romagnoli G, Ramoni C, Cianfriglia M, Gessani S. Interferon-gamma up-regulates expression and activity of P-glycoprotein in human peripheral blood monocyte-derived macrophages. Lab Invest. 1999;79:1299–1309. [PubMed] [Google Scholar]
- 150.Randolph GJ, Beaulieu S, Pope M, Sugawara I, Hoffman L, Steinman RM, Muller WA. A physiologic function for p-glycoprotein (MDR-1) during the migration of dendritic cells from skin via afferent lymphatic vessels. Proc Natl Acad Sci U S A. 1998;95:6924–6929. doi: 10.1073/pnas.95.12.6924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Cano-Soldado P, Lorrayoz IM, Molina-Arcas M, Casado FJ, Martinez-Picado J, Lostao MP, Pastor-Anglada M. Interaction of nucleoside inhibitors of HIV-1 reverse transcriptase with the concentrative nucleoside transporter-1 (SLC28A1) Antivir Ther. 2004;9:993–1002. [PubMed] [Google Scholar]
- 152.Rost D, Mahner S, Sugiyama Y, Stremmel W. Expression and localization of the multidrug resistance-associated protein 3 in rat small and large intestine. American Journal of Physiology-Gastrointestinal and Liver Physiology. 2002;282:G720–G726. doi: 10.1152/ajpgi.00318.2001. [DOI] [PubMed] [Google Scholar]
- 153.Cui YJ, Cheng X, Weaver YM, Klaassen CD. Tissue distribution, gender-divergent expression, ontogeny, and chemical induction of multidrug resistance transporter genes (Mdr1a, Mdr1b, Mdr2) in mice. Drug Metabolism and Disposition. 2009;37:203–210. doi: 10.1124/dmd.108.023721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Lee LS, Soon GH, Shen P, Yong EL, Flexner C, Pham P. Darunavir/ritonavir and efavirenz exert differential effects on MRP1 transporter expression and function in healthy volunteers. Antivir Ther. 2010;15:275–279. doi: 10.3851/IMP1505. [DOI] [PubMed] [Google Scholar]
- 155.Schinkel AH, Mayer U, Wagenaar E, Mol CA, van Deemter L, Smit JJ, van der Valk MA, Voordouw AC, Spits H, van Tellingen O, Zijlmans JM, Fibbe WE, Borst P. Normal viability and altered pharmacokinetics in mice lacking mdr1-type (drug-transporting) P-glycoproteins. Proc Natl Acad Sci U S A. 1997;94:4028–4033. doi: 10.1073/pnas.94.8.4028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Gunaseelan S, Gunaseelan K, Deshmukh M, Zhang X, Sinko PJ. Surface modifications of nanocarriers for effective intracellular delivery of anti-HIV drugs. Advanced Drug Delivery Reviews. 2010;62:518–531. doi: 10.1016/j.addr.2009.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Puligujja P, McMillan J, Kendrick L, Li T, Balkundi S, Smith N, Veerubhotla RS, Edagwa BJ, Kabanov AV, Bronich T, Gendelman HE, Liu X-M. Macrophage folate receptor-targeted antiretroviral therapy facilitates drug entry, retention, antiretroviral activities and biodistribution for reduction of human immunodeficiency virus infections. Nanomedicine: Nanotechnology, Biology and Medicine. 2013;9:1263–1273. doi: 10.1016/j.nano.2013.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Puligujja P, Balkundi SS, Kendrick LM, Baldridge HM, Hilaire JR, Bade AN, Dash PK, Zhang G, Poluektova LY, Gorantla S, Liu X-M, Ying T, Feng Y, Wang Y, Dimitrov DS, McMillan JM, Gendelman HE. Pharmacodynamics of long-acting folic acid-receptor targeted ritonavir-boosted atazanavir nanoformulations. Biomaterials. 2015;41:141–150. doi: 10.1016/j.biomaterials.2014.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Freeling JP, Koehn J, Shu C, Sun J, Ho RJY. Anti-HIV Drug-Combination Nanoparticles Enhance Plasma Drug Exposure Duration as Well as Triple-Drug Combination Levels in Cells Within Lymph Nodes and Blood in Primates. AIDS Res Hum Retroviruses. 2015;31:107–114. doi: 10.1089/aid.2014.0210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Albermann N, Schmitz-Winnenthal FH, Z’graggen K, Volk C, Hoffmann MM, Haefeli WE, Weiss J. Expression of the drug transporters MDR1/ABCB1, MRP1/ABCC1, MRP2/ABCC2, BCRP/ABCG2, and PXR in peripheral blood mononuclear cells and their relationship with the expression in intestine and liver. Biochemical pharmacology. 2005;70:949–958. doi: 10.1016/j.bcp.2005.06.018. [DOI] [PubMed] [Google Scholar]
- 161.Choudhuri S, Klaassen CD. Structure, function, expression, genomic organization, and single nucleotide polymorphisms of human ABCB1 (MDR1), ABCC (MRP), and ABCG2 (BCRP) efflux transporters. Int J Toxicol. 2006;25:231–259. doi: 10.1080/10915810600746023. [DOI] [PubMed] [Google Scholar]
- 162.Klein I, Sarkadi B, Varadi A. An inventory of the human ABC proteins. Biochim Biophys Acta. 1999;1461:237–262. doi: 10.1016/s0005-2736(99)00161-3. [DOI] [PubMed] [Google Scholar]
- 163.Goole J, Lindley DJ, Roth W, Carl SM, Amighi K, Kauffmann JM, Knipp GT. The effects of excipients on transporter mediated absorption. Int J Pharm. 2010;393:17–31. doi: 10.1016/j.ijpharm.2010.04.019. [DOI] [PubMed] [Google Scholar]
- 164.Ma Q, Brazeau D, Zingman BS, Reichman RC, Fischl MA, Gripshover BM, Venuto CS, Slish JC, DiFrancesco R, Forrest A. Multidrug resistance 1 polymorphisms and trough concentrations of atazanavir and lopinavir in patients with HIV. 2007 doi: 10.2217/14622416.8.3.227. [DOI] [PubMed]
- 165.Anderson PL, Lamba J, Aquilante CL, Schuetz E, Fletcher CV. Pharmacogenetic characteristics of indinavir, zidovudine, and lamivudine therapy in HIV-infected adults: a pilot study. J Acquir Immune Defic Syndr. 2006;42:441–449. doi: 10.1097/01.qai.0000225013.53568.69. [DOI] [PubMed] [Google Scholar]
- 166.Griffin L, Annaert P, Brouwer KL. Influence of drug transport proteins on the pharmacokinetics and drug interactions of HIV protease inhibitors. Journal of pharmaceutical sciences. 2011;100:3636–3654. doi: 10.1002/jps.22655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Busti AJ, Bain AM, Hall RG, Bedimo RG, Leff RD, Meek C, Mehvar R. Effects of atazanavir/ritonavir or fosamprenavir/ritonavir on the pharmacokinetics of rosuvastatin. Journal of cardiovascular pharmacology. 2008;51:605–610. doi: 10.1097/FJC.0b013e31817b5b5a. [DOI] [PubMed] [Google Scholar]
- 168.Lee CG, Gottesman MM, Cardarelli CO, Ramachandra M, Jeang KT, Ambudkar SV, Pastan I, Dey S. HIV-1 protease inhibitors are substrates for the MDR1 multidrug transporter. Biochemistry. 1998;37:3594–3601. doi: 10.1021/bi972709x. [DOI] [PubMed] [Google Scholar]
- 169.Ronaldson PT, Lee G, Dallas S, Bendayan R. Involvement of P-glycoprotein in the transport of saquinavir and indinavir in rat brain microvessel endothelial and microglia cell lines. Pharm Res. 2004;21:811–818. doi: 10.1023/b:pham.0000026433.27773.47. [DOI] [PubMed] [Google Scholar]
- 170.Jones K, Hoggard PG, Sales SD, Khoo S, Davey R, Back DJ. Differences in the intracellular accumulation of HIV protease inhibitors in vitro and the effect of active transport. Aids. 2001;15:675–681. doi: 10.1097/00002030-200104130-00002. [DOI] [PubMed] [Google Scholar]
- 171.Zastre JA, Chan GN, Ronaldson PT, Ramaswamy M, Couraud PO, Romero IA, Weksler B, Bendayan M, Bendayan R. Up-regulation of P-glycoprotein by HIV protease inhibitors in a human brain microvessel endothelial cell line. J Neurosci Res. 2009;87:1023–1036. doi: 10.1002/jnr.21898. [DOI] [PubMed] [Google Scholar]
- 172.Fujimoto H, Higuchi M, Watanabe H, Koh Y, Ghosh AK, Mitsuya H, Tanoue N, Hamada A, Saito H. P-glycoprotein mediates efflux transport of darunavir in human intestinal Caco-2 and ABCB1 gene-transfected renal LLC-PK1 cell lines. Biol Pharm Bull. 2009;32:1588–1593. doi: 10.1248/bpb.32.1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Hoque MT, Kis O, De Rosa MF, Bendayan R. Raltegravir Permeability across Blood-Tissue Barriers and the Potential Role of Drug Efflux Transporters. Antimicrob Agents Chemother. 2015;59:2572–2582. doi: 10.1128/AAC.04594-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Perloff ES, Duan SX, Skolnik PR, Greenblatt DJ, von Moltke LL. Atazanavir: effects on P-glycoprotein transport and CYP3A metabolism in vitro. Drug Metabolism and Disposition. 2005;33:764–770. doi: 10.1124/dmd.104.002931. [DOI] [PubMed] [Google Scholar]
- 175.Seminari E, Castagna A, Lazzarin A. Etravirine for the treatment of HIV infection. Expert Rev Anti Infect Ther. 2008;6:427–433. doi: 10.1586/14787210.6.4.427. [DOI] [PubMed] [Google Scholar]
- 176.Weiss J, Weis N, Ketabi-Kiyanvash N, Storch CH, Haefeli WE. Comparison of the induction of P-glycoprotein activity by nucleotide, nucleoside, and non-nucleoside reverse transcriptase inhibitors. Eur J Pharmacol. 2008;579:104–109. doi: 10.1016/j.ejphar.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 177.Perloff MD, von Moltke LL, Greenblatt DJ. Fexofenadine transport in Caco-2 cells: inhibition with verapamil and ritonavir. J Clin Pharmacol. 2002;42:1269–1274. doi: 10.1177/009127002762491370. [DOI] [PubMed] [Google Scholar]
- 178.Storch CH, Theile D, Lindenmaier H, Haefeli WE, Weiss J. Comparison of the inhibitory activity of anti-HIV drugs on P-glycoprotein. Biochemical Pharmacology. 2007;73:1573–1581. doi: 10.1016/j.bcp.2007.01.027. [DOI] [PubMed] [Google Scholar]
- 179.Vishnuvardhan D, Moltke LL, Richert C, Greenblatt DJ. Lopinavir: acute exposure inhibits P-glycoprotein; extended exposure induces P-glycoprotein. Aids. 2003;17:1092–1094. doi: 10.1097/01.aids.0000060380.78202.b5. [DOI] [PubMed] [Google Scholar]
- 180.Walker DK, Abel S, Comby P, Muirhead GJ, Nedderman AN, Smith DA. Species differences in the disposition of the CCR5 antagonist, UK-427,857, a new potential treatment for HIV. Drug Metabolism and Disposition. 2005;33:587–595. doi: 10.1124/dmd.104.002626. [DOI] [PubMed] [Google Scholar]
- 181.Abel S, Back DJ, Vourvahis M. Maraviroc: pharmacokinetics and drug interactions. Antivir Ther. 2009;14:607–618. [PubMed] [Google Scholar]
- 182.van der Sandt ICJ, Vos CMP, Nabulsi L, Blom-Roosemalen MCM, Voorwinden HH, de Boer AG, Breimer DD. Assessment of active transport of HIV protease inhibitors in various cell lines and the in vitro blood-brain barrier. Aids. 2001;15:483–491. doi: 10.1097/00002030-200103090-00007. [DOI] [PubMed] [Google Scholar]
- 183.Janneh O, Jones E, Chandler B, Owen A, Khoo SH. Inhibition of P-glycoprotein and multidrug resistance-associated proteins modulates the intracellular concentration of lopinavir in cultured CD4 T cells and primary human lymphocytes. The Journal of antimicrobial chemotherapy. 2007;60:987–993. doi: 10.1093/jac/dkm353. [DOI] [PubMed] [Google Scholar]
- 184.Huisman MT, Smit JW, Crommentuyn KM, Zelcer N, Wiltshire HR, Beijnen JH, Schinkel AH. Multidrug resistance protein 2 (MRP2) transports HIV protease inhibitors, and transport can be enhanced by other drugs. Aids. 2002;16:2295–2301. doi: 10.1097/00002030-200211220-00009. [DOI] [PubMed] [Google Scholar]
- 185.Dallas S, Ronaldson PT, Bendayan M, Bendayan R. Multidrug resistance protein 1-mediated transport of saquinavir by microglia. Neuroreport. 2004;15:1183–1186. doi: 10.1097/00001756-200405190-00020. [DOI] [PubMed] [Google Scholar]
- 186.Mallants R, Van Oosterwyck K, Van Vaeck L, Mols R, De Clercq E, Augustijns P. Multidrug resistance-associated protein 2 (MRP2) affects hepatobiliary elimination but not the intestinal disposition of tenofovir disoproxil fumarate and its metabolites. Xenobiotica. 2005;35:1055–1066. doi: 10.1080/00498250500354493. [DOI] [PubMed] [Google Scholar]
- 187.Reid G, Wielinga P, Zelcer N, De Haas M, Van Deemter L, Wijnholds J, Balzarini J, Borst P. Characterization of the transport of nucleoside analog drugs by the human multidrug resistance proteins MRP4 and MRP5. Mol Pharmacol. 2003;63:1094–1103. doi: 10.1124/mol.63.5.1094. [DOI] [PubMed] [Google Scholar]
- 188.Imaoka T, Kusuhara H, Adachi M, Schuetz JD, Takeuchi K, Sugiyama Y. Functional involvement of multidrug resistance-associated protein 4 (MRP4/ABCC4) in the renal elimination of the antiviral drugs adefovir and tenofovir. Mol Pharmacol. 2007;71:619–627. doi: 10.1124/mol.106.028233. [DOI] [PubMed] [Google Scholar]
- 189.Ray AS, Cihlar T, Robinson KL, Tong L, Vela JE, Fuller MD, Wieman LM, Eisenberg EJ, Rhodes GR. Mechanism of active renal tubular efflux of tenofovir. Antimicrob Agents Chemother. 2006;50:3297–3304. doi: 10.1128/AAC.00251-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Weiss J, Theile D, Ketabi-Kiyanvash N, Lindenmaier H, Haefeli WE. Inhibition of MRP1/ABCC1, MRP2/ABCC2, and MRP3/ABCC3 by nucleoside, nucleotide, and non-nucleoside reverse transcriptase inhibitors. Drug Metabolism and Disposition. 2007;35:340–344. doi: 10.1124/dmd.106.012765. [DOI] [PubMed] [Google Scholar]
- 191.Reid G, Wielinga P, Zelcer N, van der Heijden I, Kuil A, de Haas M, Wijnholds J, Borst P. The human multidrug resistance protein MRP4 functions as a prostaglandin efflux transporter and is inhibited by nonsteroidal antiinflammatory drugs. Proc Natl Acad Sci U S A. 2003;100:9244–9249. doi: 10.1073/pnas.1033060100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.El-Sheikh AA, van den Heuvel JJ, Koenderink JB, Russel FG. Interaction of nonsteroidal anti-inflammatory drugs with multidrug resistance protein (MRP) 2/ABCC2- and MRP4/ABCC4-mediated methotrexate transport. Journal of Pharmacology and Experimental Therapeutics. 2007;320:229–235. doi: 10.1124/jpet.106.110379. [DOI] [PubMed] [Google Scholar]
- 193.Morioka N, Kumagai K, Morita K, Kitayama S, Dohi T. Nonsteroidal anti-inflammatory drugs potentiate 1-methyl-4-phenylpyridinium (MPP+)-induced cell death by promoting the intracellular accumulation of MPP+ in PC12 cells. Journal of Pharmacology and Experimental Therapeutics. 2004;310:800–807. doi: 10.1124/jpet.104.065300. [DOI] [PubMed] [Google Scholar]
- 194.Giri N, Shaik N, Pan G, Terasaki T, Mukai C, Kitagaki S, Miyakoshi N, Elmquist WF. Investigation of the role of breast cancer resistance protein (Bcrp/Abcg2) on pharmacokinetics and central nervous system penetration of abacavir and zidovudine in the mouse. Drug Metabolism and Disposition. 2008;36:1476–1484. doi: 10.1124/dmd.108.020974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Wang X, Furukawa T, Nitanda T, Okamoto M, Sugimoto Y, Akiyama S, Baba M. Breast cancer resistance protein (BCRP/ABCG2) induces cellular resistance to HIV-1 nucleoside reverse transcriptase inhibitors. Mol Pharmacol. 2003;63:65–72. doi: 10.1124/mol.63.1.65. [DOI] [PubMed] [Google Scholar]
- 196.Wang X, Nitanda T, Shi M, Okamoto M, Furukawa T, Sugimoto Y, Akiyama S, Baba M. Induction of cellular resistance to nucleoside reverse transcriptase inhibitors by the wild-type breast cancer resistance protein. Biochemical Pharmacology. 2004;68:1363–1370. doi: 10.1016/j.bcp.2004.05.052. [DOI] [PubMed] [Google Scholar]
- 197.Pan G, Giri N, Elmquist WF. Abcg2/Bcrp1 mediates the polarized transport of antiretroviral nucleosides abacavir and zidovudine. Drug Metabolism and Disposition. 2007;35:1165–1173. doi: 10.1124/dmd.106.014274. [DOI] [PubMed] [Google Scholar]
- 198.Jung N, Lehmann C, Rubbert A, Knispel M, Hartmann P, van Lunzen J, Stellbrink HJ, Faetkenheuer G, Taubert D. Relevance of the organic cation transporters 1 and 2 for antiretroviral drug therapy in human immunodeficiency virus infection. Drug Metabolism and Disposition. 2008;36:1616–1623. doi: 10.1124/dmd.108.020826. [DOI] [PubMed] [Google Scholar]
- 199.Zhang L, Gorset W, Washington CB, Blaschke TF, Kroetz DL, Giacomini KM. Interactions of HIV protease inhibitors with a human organic cation transporter in a mammalian expression system. Drug Metabolism and Disposition. 2000;28:329–334. [PubMed] [Google Scholar]
- 200.Kong W, Engel K, Wang J. Mammalian nucleoside transporters. Curr Drug Metab. 2004;5:63–84. doi: 10.2174/1389200043489162. [DOI] [PubMed] [Google Scholar]
- 201.Lostao MP, Mata JF, Larrayoz IM, Inzillo SM, Casado FJ, Pastor-Anglada M. Electrogenic uptake of nucleosides and nucleoside-derived drugs by the human nucleoside transporter 1 (hCNT1) expressed in Xenopus laevis oocytes. FEBS Lett. 2000;481:137–140. doi: 10.1016/s0014-5793(00)01983-9. [DOI] [PubMed] [Google Scholar]
- 202.Ritzel MW, Yao SY, Ng AM, Mackey JR, Cass CE, Young JD. Molecular cloning, functional expression and chromosomal localization of a cDNA encoding a human Na+/nucleoside cotransporter (hCNT2) selective for purine nucleosides and uridine. Mol Membr Biol. 1998;15:203–211. doi: 10.3109/09687689709044322. [DOI] [PubMed] [Google Scholar]
- 203.Ritzel MW, Ng AM, Yao SY, Graham K, Loewen SK, Smith KM, Ritzel RG, Mowles DA, Carpenter P, Chen XZ, Karpinski E, Hyde RJ, Baldwin SA, Cass CE, Young JD. Molecular identification and characterization of novel human and mouse concentrative Na+-nucleoside cotransporter proteins (hCNT3 and mCNT3) broadly selective for purine and pyrimidine nucleosides (system cib) J Biol Chem. 2001;276:2914–2927. doi: 10.1074/jbc.M007746200. [DOI] [PubMed] [Google Scholar]
- 204.Yao SY, Ng AM, Sundaram M, Cass CE, Baldwin SA, Young JD. Transport of antiviral 3′-deoxy-nucleoside drugs by recombinant human and rat equilibrative, nitrobenzylthioinosine (NBMPR)-insensitive (ENT2) nucleoside transporter proteins produced in Xenopus oocytes. Mol Membr Biol. 2001;18:161–167. doi: 10.1080/09687680110048318. [DOI] [PubMed] [Google Scholar]
- 205.Su Y, Zhang X, Sinko PJ. Human organic anion-transporting polypeptide OATP-A (SLC21A3) acts in concert with P-glycoprotein and multidrug resistance protein 2 in the vectorial transport of Saquinavir in Hep G2 cells. Mol Pharm. 2004;1:49–56. doi: 10.1021/mp0340136. [DOI] [PubMed] [Google Scholar]
- 206.Hartkoorn RC, San Kwan W, Shallcross V, Chaikan A, Liptrott N, Egan D, Sora ES, James CE, Gibbons S, Bray PG, Back DJ, Khoo SH, Owen A. HIV protease inhibitors are substrates for OATP1A2, OATP1B1 and OATP1B3 and lopinavir plasma concentrations are influenced by SLCO1B1 polymorphisms. Pharmacogenet Genomics. 2010;20:112–120. doi: 10.1097/FPC.0b013e328335b02d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Siccardi M, D’Avolio A, Nozza S, Simiele M, Baietto L, Stefani FR, Moss D, Kwan WS, Castagna A, Lazzarin A, Calcagno A, Bonora S, Back D, Di Perri G, Owen A. Maraviroc is a substrate for OATP1B1 in vitro and maraviroc plasma concentrations are influenced by SLCO1B1 521 T > C polymorphism. Pharmacogenet Genomics. 2010;20:759–765. doi: 10.1097/FPC.0b013e3283402efb. [DOI] [PubMed] [Google Scholar]
- 208.Annaert P, Ye ZW, Stieger B, Augustijns P. Interaction of HIV protease inhibitors with OATP1B1, 1B3, and 2B1. Xenobiotica. 2010;40:163–176. doi: 10.3109/00498250903509375. [DOI] [PubMed] [Google Scholar]
- 209.Campbell SD, de Morais SM, Xu JHJ. Inhibition of human organic anion transporting polypeptide OATP 1B1 as a mechanism of drug-induced hyperbilirubinemia. Chemico-Biological Interactions. 2004;150:179–187. doi: 10.1016/j.cbi.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 210.Shugarts S, Benet LZ. The role of transporters in the pharmacokinetics of orally administered drugs. Pharm Res. 2009;26:2039–2054. doi: 10.1007/s11095-009-9924-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Amidon GL, Lennernas H, Shah VP, Crison JR. A theoretical basis for a biopharmaceutic drug classification: the correlation of in vitro drug product dissolution and in vivo bioavailability. Pharm Res. 1995;12:413–420. doi: 10.1023/a:1016212804288. [DOI] [PubMed] [Google Scholar]
- 212.Martin-Facklam M, Burhenne J, Ding R, Fricker R, Mikus G, Walter-Sack I, Haefeli WE. Dose-dependent increase of saquinavir bioavailability by the pharmaceutic aid cremophor EL. British journal of clinical pharmacology. 2002;53:576–581. doi: 10.1046/j.1365-2125.2002.01595.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Werle M, Hoffer M. Glutathione and thiolated chitosan inhibit multidrug resistance P-glycoprotein activity in excised small intestine. Journal of Controlled Release. 2006;111:41–46. doi: 10.1016/j.jconrel.2005.11.011. [DOI] [PubMed] [Google Scholar]
- 214.Rege BD, Kao JP, Polli JE. Effects of nonionic surfactants on membrane transporters in Caco-2 cell monolayers. European journal of pharmaceutical sciences. 2002;16:237–246. doi: 10.1016/s0928-0987(02)00055-6. [DOI] [PubMed] [Google Scholar]
- 215.Hugger ED, Novak BL, Burton PS, Audus KL, Borchardt RT. A comparison of commonly used polyethoxylated pharmaceutical excipients on their ability to inhibit P-glycoprotein activity in vitro. Journal of pharmaceutical sciences. 2002;91:1991–2002. doi: 10.1002/jps.10176. [DOI] [PubMed] [Google Scholar]
- 216.Tseng A, Foisy M. Important Drug-Drug Interactions in HIV-Infected Persons on Antiretroviral Therapy: An Update on New Interactions Between HIV and Non-HIV Drugs. Current Infectious Disease Reports. 2012;14:67–82. doi: 10.1007/s11908-011-0229-1. [DOI] [PubMed] [Google Scholar]
- 217.Sosnik A, Chiappetta DA, Carcaboso AM. Drug delivery systems in HIV pharmacotherapy: What has been done and the challenges standing ahead. Journal of Controlled Release. 2009;138:2–15. doi: 10.1016/j.jconrel.2009.05.007. [DOI] [PubMed] [Google Scholar]
- 218.Parikh UM, Dobard C, Sharma S, Cong ME, Jia HW, Martin A, Pau CP, Hanson DL, Guenthner P, Smith J, Kersh E, Garcia-Lerma JG, Novembre FJ, Otten R, Folks T, Heneine W. Complete Protection from Repeated Vaginal Simian-Human Immunodeficiency Virus Exposures in Macaques by a Topical Gel Containing Tenofovir Alone or with Emtricitabine. J Virol. 2009;83:10358–10365. doi: 10.1128/JVI.01073-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Schader SM, Colby-Germinario SP, Schachter JR, Xu HT, Wainberg MA. Synergy against drug-resistant HIV-1 with the microbicide antiretrovirals, dapivirine and tenofovir, in combination. Aids. 2011;25:1585–1594. doi: 10.1097/QAD.0b013e3283491f89. [DOI] [PubMed] [Google Scholar]
- 220.Johnson TJ, Gupta KM, Fabian J, Albright TH, Kiser PF. Segmented polyurethane intravaginal rings for the sustained combined delivery of antiretroviral agents dapivirine and tenofovir (vol 39, pg 203, 2010) European Journal of Pharmaceutical Sciences. 2010;41:736–736. doi: 10.1016/j.ejps.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 221.Akil A, Devlin B, Cost M, Rohan LC. Increased Dapivirine Tissue Accumulation through Vaginal Film Codelivery of Dapivirine and Tenofovir. Molecular Pharmaceutics. 2014;11:1533–1541. doi: 10.1021/mp4007024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Fetherston SM, Boyd P, McCoy CF, McBride MC, Edwards KL, Ampofo S, Malcolm RK. A silicone elastomer vaginal ring for HIV prevention containing two microbicides with different mechanisms of action. European Journal of Pharmaceutical Sciences. 2013;48:406–415. doi: 10.1016/j.ejps.2012.12.002. [DOI] [PubMed] [Google Scholar]
- 223.Dang NTT, Sivakumaran H, Harrich D, Shaw PN, Davis-Poynter N, Coombes AGA. Synergistic activity of tenofovir and nevirapine combinations released from polycaprolactone matrices for potential enhanced prevention of HIV infection through the vaginal route. European Journal of Pharmaceutics and Biopharmaceutics. 2014;88:406–414. doi: 10.1016/j.ejpb.2014.05.018. [DOI] [PubMed] [Google Scholar]
- 224.Thurman AR, Anderson S, Doncel GF. Effects of Hormonal Contraception on Antiretroviral Drug Metabolism, Pharmacokinetics and Pharmacodynamics. American Journal of Reproductive Immunology. 2014;71:523–530. doi: 10.1111/aji.12210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Fröhlich M, Albermann N, Sauer A, Walter-Sack I, Haefeli WE, Weiss J. In vitro and ex vivo evidence for modulation of P-glycoprotein activity by progestins. Biochemical Pharmacology. 2004;68:2409–2416. doi: 10.1016/j.bcp.2004.08.026. [DOI] [PubMed] [Google Scholar]
- 226.Atrio J, Stanczyk FZ, Neely M, Cherala G, Kovacs A, Mishell DR., Jr Effect of protease inhibitors on steady-state pharmacokinetics of oral norethindrone contraception in HIV-infected women. Journal of acquired immune deficiency syndromes (1999) 2014;65:72. doi: 10.1097/QAI.0b013e3182a9b3f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Vieira CS, Bahamondes MV, de Souza RM, Brito MB, Prandini TRR, Amaral E, Bahamondes L, Duarte G, Quintana SM, Scaranari C. Effect of antiretroviral therapy including lopinavir/ritonavir or efavirenz on etonogestrel-releasing implant pharmacokinetics in HIV-positive women. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2014;66:378–385. doi: 10.1097/QAI.0000000000000189. [DOI] [PubMed] [Google Scholar]
- 228.Weiss J, Haefeli WE. Potential of the novel antiretroviral drug rilpivirine to modulate the expression and function of drug transporters and drug-metabolising enzymes in vitro. International Journal of Antimicrobial Agents. 2013;41:484–487. doi: 10.1016/j.ijantimicag.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 229.Cattaneo D, Gervasoni C, Cozzi V, Baldelli S, Fucile S, Meraviglia P, Landonio S, Boreggio G, Rizzardini G, Clementi E. Co-administration of raltegravir reduces daily darunavir exposure in HIV-1 infected patients. Pharmacological Research. 2012;65:198–203. doi: 10.1016/j.phrs.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 230.Mahajan S, Law Aalinkeel, Reynolds Nair, Sykes Yong, Roy Prasad, Schwartz S. Anti-HIV-1 nanotherapeutics: promises and challenges for the future. International Journal of Nanomedicine. 2012:5301. doi: 10.2147/IJN.S25871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Mamo T, Moseman EA, Kolishetti N, Salvador-Morales C, Shi J, Kuritzkes DR, Langer R, Andrian Uv, Farokhzad OC. Emerging nanotechnology approaches for HIV/AIDS treatment and prevention. Nanomedicine. 2010;5:269–285. doi: 10.2217/nnm.10.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.das Neves J, Amiji M, Sarmento B. Mucoadhesive nanosystems for vaginal microbicide development: friend or foe? Wiley Interdisciplinary Reviews: Nanomedicine and Nanobiotechnology. 2011;3:389–399. doi: 10.1002/wnan.144. [DOI] [PubMed] [Google Scholar]
- 233.Shibata A, McMullen E, Pham A, Belshan M, Sanford B, Zhou Y, Goede M, Date AA, Destache CJ. Polymeric Nanoparticles Containing Combination Antiretroviral Drugs for HIV Type 1 Treatment. AIDS Res Hum Retroviruses. 2013;29:746–754. doi: 10.1089/aid.2012.0301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Beloqui A, Solins Mn, Gascn AR, del Pozo-Rodrguez A, des Rieux A, Prat V. Mechanism of transport of saquinavir-loaded nanostructured lipid carriers across the intestinal barrier. Journal of Controlled Release. 2013;166:115–123. doi: 10.1016/j.jconrel.2012.12.021. [DOI] [PubMed] [Google Scholar]
- 235.Patel K, Patil A, Mehta M, Gota V, Vavia P. Oral delivery of paclitaxel nanocrystal (PNC) with a dual Pgp-CYP3A4 inhibitor: preparation, characterization and antitumor activity. International journal of pharmaceutics. 2014;472:214–223. doi: 10.1016/j.ijpharm.2014.06.031. [DOI] [PubMed] [Google Scholar]
- 236.Rao KS, Reddy MK, Horning JL, Labhasetwar V. TAT-conjugated nanoparticles for the CNS delivery of anti-HIV drugs. Biomaterials. 2008;29:4429–4438. doi: 10.1016/j.biomaterials.2008.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Ham AS, Cost MR, Sassi AB, Dezzutti CS, Rohan LC. Targeted delivery of PSC-RANTES for HIV-1 prevention using biodegradable nanoparticles. Pharm Res. 2009;26:502–511. doi: 10.1007/s11095-008-9765-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.das Neves J, Nunes R, Machado A, Sarmento B. Polymer-based nanocarriers for vaginal drug delivery. Advanced Drug Delivery Reviews. 2014 doi: 10.1016/j.addr.2014.12.004. [DOI] [PubMed] [Google Scholar]
- 239.Yang S, Chen Y, Gu K, Dash A, Sayre CL, Davies NM, Ho E. Novel intravaginal nanomedicine for the targeted delivery of saquinavir to CD4+ immune cells. International Journal of Nanomedicine. 2013:2847. doi: 10.2147/IJN.S46958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Endsley AN, Ho RJY. Design and Characterization of Novel Peptide-Coated Lipid Nanoparticles for Targeting Anti-HIV Drug to CD4 Expressing Cells. The AAPS Journal. 2012;14:225–235. doi: 10.1208/s12248-012-9329-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Namanja HA, Emmert D, Davis DA, Campos C, Miller DS, Hrycyna CA, Chmielewski J. Toward Eradicating HIV Reservoirs in the Brain: Inhibiting P-Glycoprotein at the Blood–Brain Barrier with Prodrug Abacavir Dimers. Journal of the American Chemical Society. 2012;134:2976–2980. doi: 10.1021/ja206867t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Patel M, Sheng Y, Mandava NK, Pal D, Mitra AK. Dipeptide prodrug approach to evade efflux pumps and CYP3A4 metabolism of lopinavir. International journal of pharmaceutics. 2014;476:99–107. doi: 10.1016/j.ijpharm.2014.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Zhang Y, Gao Y, Wen X, Ma H. Current prodrug strategies for improving oral absorption of nucleoside analogues. Asian Journal of Pharmaceutical Sciences. 2014;9:65–74. [Google Scholar]
- 244.Chen Z-S, Robey RW, Belinsky MG, Shchaveleva I, Ren X-Q, Sugimoto Y, Ross DD, Bates SE, Kruh GD. Transport of methotrexate, methotrexate polyglutamates, and 17β-estradiol 17-(β-d-glucuronide) by ABCG2: effects of acquired mutations at R482 on methotrexate transport. Cancer research. 2003;63:4048–4054. [PubMed] [Google Scholar]
- 245.Friesema EC, Jansen J, Milici C, Visser TJ. Thyroid hormone transporters. Vitamins & Hormones. 2005;70:137–167. doi: 10.1016/S0083-6729(05)70005-4. [DOI] [PubMed] [Google Scholar]
- 246.Le Vee M, Lecureur V, Stieger B, Fardel O. Regulation of drug transporter expression in human hepatocytes exposed to the proinflammatory cytokines tumor necrosis factor-α or interleukin-6. Drug Metabolism and Disposition. 2009;37:685–693. doi: 10.1124/dmd.108.023630. [DOI] [PubMed] [Google Scholar]
- 247.Evseenko DA, Paxton JW, Keelan JA. Independent regulation of apical and basolateral drug transporter expression and function in placental trophoblasts by cytokines, steroids, and growth factors. Drug Metabolism and Disposition. 2007;35:595–601. doi: 10.1124/dmd.106.011478. [DOI] [PubMed] [Google Scholar]
- 248.van de Ven R, de Jong MC, Reurs AW, Schoonderwoerd AJ, Jansen G, Hooijberg JH, Scheffer GL, de Gruijl TD, Scheper RJ. Dendritic cells require multidrug resistance protein 1 (ABCC1) transporter activity for differentiation. The Journal of Immunology. 2006;176:5191–5198. doi: 10.4049/jimmunol.176.9.5191. [DOI] [PubMed] [Google Scholar]
- 249.Noor MA, Flint OP, Maa JF, Parker RA. Effects of atazanavir/ritonavir and lopinavir/ritonavir on glucose uptake and insulin sensitivity: demonstrable differences in vitro and clinically. AIDS. 2006;20:1813–1821. doi: 10.1097/01.aids.0000244200.11006.55. [DOI] [PubMed] [Google Scholar]
- 250.Kis O, Robillard K, Chan GN, Bendayan R. The complexities of antiretroviral drug-drug interactions: role of ABC and SLC transporters. Trends in pharmacological sciences. 2010;31:22–35. doi: 10.1016/j.tips.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 251.Yan Q. Membrane transporters and drug development: relevance to pharmacogenomics, nutrigenomics, epigenetics, and systems biology. Methods Mol Biol. 2010;637:1–21. doi: 10.1007/978-1-60761-700-6_1. [DOI] [PubMed] [Google Scholar]