Abstract
Objective
The aim of the current study is to examine the association of environmental tobacco smoke (ETS) exposure evident by serum cotinine level, and diabetes mellitus in never smokers. Previous studies suggest that active tobacco cigarette smoking is associated with diabetes mellitus risk. However it is not clear if the low-level “background” ETS exposure is associated with diabetes among never smokers.
Methods
We present evidence from five independent replications based on the US nationally representative National Health and Nutrition Examination Surveys (NHANES) conducted 2003-12. Our exposure of interest is ETS exposure among never smokers, measured by serum cotinine levels (ng/mL), and our main outcome is diabetes mellitus assessed via self-reported physician-diagnosis, current use of insulin and/or oral hypoglycemic medications, plasma fasting glucose levels ≥126 mg/dL or glycohemoglobin levels ≥6.5%. The conceptual model encompassed age, sex, ethnic self-identification, education, poverty-income ratio, alcohol drinking, total cholesterol and body mass index.
Results
In never smokers, higher serum cotinine levels were positively associated with diabetes mellitus (the meta-analytic summary estimate is 1.2, 95% CI=1.1, 1.2). This association was not evident among never smokers with cotinine levels below 3 ng/mL.
Conclusions
These replications help sustain evidence of ETS-diabetes mellitus association, which might be explained by shared psychosocial characteristics Prospective studies with appropriate biomarkers are needed to further investigate this association.
Keywords: Environmental tobacco smoke, NHANES, Diabetes mellitus, Cotinine
1. INTRODUCTION
Several studies suggest that tobacco cigarette smoking is associated with an increased risk of developing type 2 diabetes mellitus among active smokers (Willi et al., 2007). There are only few studies investigating the relationship between environmental tobacco smoke (ETS) exposure and diabetes in never smokers (Wang et al., 2013), but this relationship might be biased if smokers do not accurately report their smoking status (Fisher et al., 2007). Cotinine, the principal metabolite of nicotine, is considered a more precise measure of exposure to cigarette smoking when compared to self-reported smoking status (Benowitz, 1996; Connor Gorber et al., 2009). Houston et al. used serum cotinine to validate smoking status in a 15-year biracial cohort of United States (US) adults and found that people with exposure to ETS; defined as participants who self-reported being never smokers and exposed to ETS, or had cotinine concentrations of 1-15 ng/mL, had an intermediate risk of developing diabetes between current smokers and never smokers without ETS exposure. However, this study only represents African-Americans and Whites recruited from four urban areas in the US and hence the results are not necessarily generalizable to other populations (Houston et al., 2006).
The number of states with comprehensive smoke-free laws in effect increased from zero on 2000, to 26 states on 2010. Between 2004 and 2007, an increasing number of states enacted different smoke-free laws that prohibit smoking in workplaces and public areas (United States Centers for Disease Control and Prevention, 2011). Accordingly exposure to ETS has steadily decreased in the US over time evident by cotinine concentrations (United States Centers for Disease Control and Prevention, 2010). The cotinine cutpoint of 15 ng/mL widely used in previous research to differentiate smokers from non-smokers was determined by Jarvis et al. more than 27 years ago when no or less strict public smoking regulations have been placed (Jarvis et al., 1987). Benowitz et al. recently suggested a lower cotinine cutpoints of 3.0 ng/mL to differentiate non-smokers from smokers, whereas levels >3 ng/mL might reflect heavier exposure to ETS or mis-reported smoking status (Benowitz et al., 2009). On the other hand, analyses of nationally representative data from 1980 to 2012 suggest a doubling of the incidence of diabetes during 1990-2008, and a plateauing between 2008 and 2012 (Geiss et al., 2014).
The aim of the current study is to investigate the association of ETS evident by serum cotinine levels and diabetes mellitus in never smokers. We derive estimates from the US nationally representative sample surveys with standardized methods; the National Health and Nutrition Examination Survey (NHANES) 2003-04, 2005-06, 2007-08, 2009-10 and 2011-12. We use a meta-analysis approach treating each data-cycle's independent sample as a separate study and deriving estimates from multiple independent replication samples (DeAndrea et al., 2013).
2. METHODS
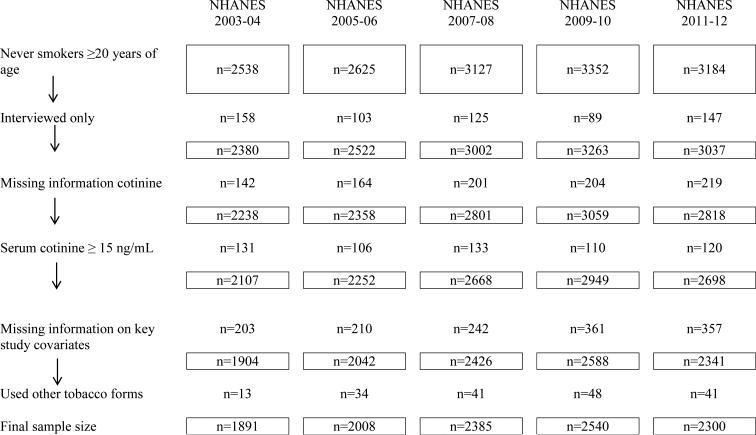
a. Study population: Never smokers ≥ 20 years of age
Each NHANES replication is designed to yield nationally representative sample survey estimates for the US non-institutionalized civilian population through multistage area probability sampling. NHANES replication estimates can be derived by combining survey cycles as follows: 2003-04, 2005-6; 2007-8; 2009-10; 2011-12. The within-cycle analysis weights take into account specific subgroups that are over-sampled in order to increase precision of NHANES estimates, as well as post-stratification adjustments (United States Centers for Disease Control and Prevention, 2010). Figure 1 presents a flow chart describing the study methodology and sample population. The NHANES study protocol has been reviewed and approved by cognizant institutional review boards for protection of human subjects in research.
Figure 1.
Flow chart describing the study methodology and sample population for each independent replication sample. Data for the United States based on the National Health and Nutrition Examination Survey, 2003–2012
b. Study outcome
The key response variable in this study is diabetes mellitus. In NHANES, diabetes mellitus is assessed based on a respondent-reported physician-diagnosis through the question “Other than during pregnancy have you ever been told by a doctor or health professional that you have diabetes or sugar diabetes?”. NHANES also has questions on current use of insulin and/or oral hypoglycemic medicines in addition to plasma fasting glucose and glycosylated hemoglobin (HbA1c) level measurement summarized in relation to American Diabetes Association guidelines for fasting glucose ≥126 mg/dL and HbA1c ≥ 6.5% (American Diabetes Association, 2010).
Fasting plasma glucose was tested in a subsample of NHANES participants who were examined in the morning session. Glycohemoglobin measures are available for the full sample. Glucose was analyzed using an enzymatic method where it is converted to glucose-6-phosphate (G-6-P) by hexokinase in the presence of adenosine triphosphate, a phosphate donor. Glucose-6-phosphate dehydrogenase then converts the G-6-P to gluconate-6-P in the presence of nicotinamide adenine dinucleotide (NADP+). As the NADP+ is reduced to NADPH during this reaction, the resulting increase in absorbance at 340 nm (secondary wavelength = 700 nm) is measured. This is an endpoint reaction that is specific for glucose.
In NHANES 2003-06, HbA1c was measured on the A1c 2.2 Plus Glycohemoglobin Analyzer (Tosoh Medics, Inc., 347 Oyster Pt. Blvd., Suite 201, So. San Francisco, Ca 94080) whereas in NHANES 2007-12, HbA1c was measured on the A1c G7 HPLC Glycohemoglobin Analyzer (Tosoh Medics, Inc., 347 Oyster Pt. Blvd., Suite 201, So. San Francisco, Ca 94080) (United States Centers for Disease Control and Prevention, 2006).
c. Study exposure
The covariate of central interest is serum cotinine levels (ng/mL) in never smokers. Serum cotinine was measured by an isotope dilution–high-performance liquid chromatography / atmospheric pressure chemical ionization tandem mass spectrometry (ID HPLC-APCI MS/MS). Cotinine concentrations were derived from the ratio of native/labeled cotinine in the sample, by comparisons to a standard curve. Detailed description of serum cotinine measurement in NHANES is available online (United States Centers for Disease Control and Prevention, 2006).
The standardized smoking questionnaire was administered in the household interview using the Computer-Assisted Personal Interviewing system (interviewer administered). On this basis, participants can be classified as never smokers; past smokers (smoked at least 100 cigarettes in lifetime and currently not smoking); and recently active smokers (smoked at least 100 cigarettes in lifetime and currently smoking). Never smokers with serum cotinine level>15 ng/mL which might reflect misclassification of smoking status were not included in the current analyses. Nicotine can be absorbed from other forms of tobacco and therefore we excluded participants who reported the use of other tobacco products such as smokeless tobacco, cigar, pipe, or hookah.
2.4 Study covariates
NHANES also had measurement for a selection of covariates: age (years), sex (male/female), ethnic self-identification (non-Hispanic White/non-Hispanic Black/Hispanics/all others), educational attainment (less than high school/high school/above high school), poverty-income ratio (<1/≥1), and past-year alcohol drinking (yes/ no). The NHANES physical examination includes assessment of body mass index (BMI) based on weight in kilograms divided by height in meters squared. Total cholesterol (mg/dL) was measured enzymatically in serum. There were changes in the instruments and lab site used to measure total cholesterol in 2003-2004, 2005-2006 and 2007-2008, but the method was the same. No adjustment was necessary to account for such change (United States Centers for Disease Control and Prevention, 2006).
2.5 Statistical analysis
Exploratory data analyses were conducted to shed light on underlying distributions of the response variable and each covariate of interest. For the main analysis step, multiple logistic regressions were used to derive covariate adjusted odds ratios (OR) of diabetes mellitus among never smokers for a one-unit increase in in serum cotinine levels (ng/mL).
Whenever there are replication studies as in the case with annual surveys akin to NHANES, one option is to ignore the fact that each survey cycle serves as an independent replication and to pool data across years. This pooling approach is essential when studying rare outcomes due to the large standard errors for a rare occurrence when individual surveys are considered one by one. Nonetheless, for the suspected relationships under study, the coefficients of variation cycle-by-cycle are at least minimally satisfactory. It can make more sense to treat the annual surveys as independent replicate samples, given that participants in any given cycle are not allowed to be participants in the subsequent cycle.
Via Stata (Stata, version 13) ‘svy’ procedures for complex survey data analysis, analysis weights, and Taylor series variance estimation, the logistic regression model was fit to data from the five NHANES independent replications yielding five OR estimates and their standard errors, from which a Stata ‘metan’ meta-analytic summary estimate was derived. The meta-analysis combines results from the different studies to identify patterns among the results. The summary estimate is a weighted average of the association of serum cotinine and diabetes across the five NHANES replications. The estimate takes into account the sample size of each of the NHANES replication as well as sources of year-by-year variation in the estimates, either because there is some methods variation, or because there might be an influence on the observed relationships not otherwise captured in the analysis model specifications (as might be seen when ETS exposure shifts downwards year by year). This downward shift would not be seen if one were to pool NHANES data into a single 10-year estimate. Our final step included estimation of the association that links serum cotinine with HbA1c (%), a biomarker of glucose metabolism.
3. RESULTS
Looking across the study sample (NHANES 2003-2012, n=11124), 60% of the study participants were females. The majority of the study population was non-Hispanic Whites (67.0%). Participants with diabetes constitute 10.5% of the study population. Normal weight, overweight, and obese status were equally distributed among study participants (data not shown in table/figure).
Exposure to ETS among never smokers has decreased steadily from 2003 to 2014 (data not shown in table/figure). For example in 2003-04, 24.3% of never smokers had undetectable serum cotinine levels, compared to approximately 44.4% during 2011–12 (P<0.05).
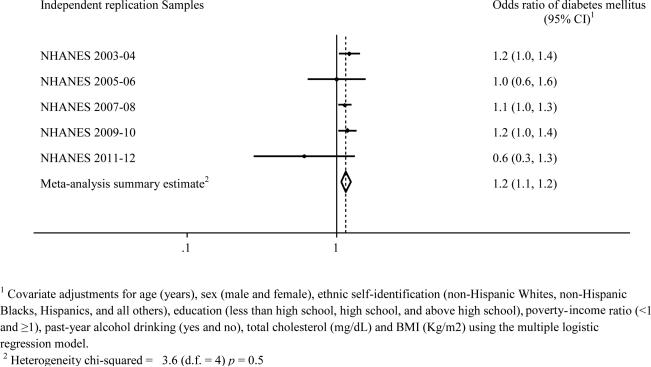
Figure 2 presents the main study estimates for each of the five independent replications as well as the meta-analysis summary estimate that draws information from all replications. With the exception of the 2011-12, higher serum cotinine levels among never smokers were positively associated with diabetes mellitus in each of the NHANES replications. The covariate-adjusted meta-analytic summary estimate is 1.2 (95% CI = 1.1, 1.2). Categorizing serum cotinine, never smokers with detectable levels of serum cotinine had higher odds of diabetes when compared to never smokers with undetectable cotinine levels (referent group). However the association is not statistically significant in the fully adjusted model (the meta-analysis summary estimate= 1.1; 95% CI= 0.9, 1.3). When we restricted our analyses to include only never smokers with serum cotinine levels < 3ng/mL, the association of serum cotinine with diabetes mellitus was not observed (meta-analytic summary estimate= 1.0; 95% CI = 0.6, 1.5; data not shown in table/figure).
Figure 2.
Study-specific estimates of odds ratios that quantify associations linking diabetes mellitus with serum cotinine (ng/mL) among never smokers
Data for the US based on five independent replications from the NHANES 2003-2012
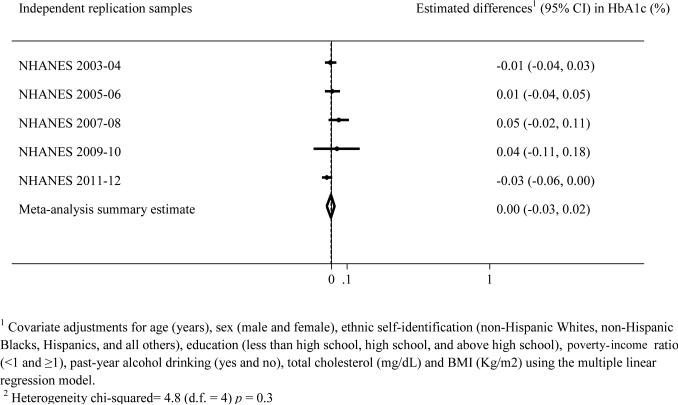
Subsequent exploratory analysis steps (Figure 3) disclosed no linear association between serum cotinine levels and glycohemoglobin among never smokers with serum cotinine levels <15 ng/mL (the meta-analysis summary estimate= 0.00; 95% CI=-0.03, 0.02) as well as among never smokers with serum cotinine <3 ng/mL (the meta-analytic summary estimate= −0.01; 95% CI =− 0.07, 0.05). Categorizing serum cotinine, never smokers with detectable levels of serum cotinine had higher HbA1c levels when compared to never smokers with undetectable serum cotinine (referent group). However the association is not statistically significant in the fully adjusted model (the meta-analytic summary estimate= 0.02; 95% CI= −0.01, 0.04; data not shown in table/figure).
Figure 3.
Serum cotinine (ng/mL) and glycohemoglobin levels (%) among never smokers
Data for the US based on five independent replications from the NHANES 2003-2012r
DISCUSSION
Studying environmental tobacco smoke exposure and diabetes mellitus in large nationally representative samples of US adults, comprising multiple independent replications, we found evidence that higher serum cotinine level is associated with diabetes mellitus among never smokers. These results help to sustain evidence on the positive ETS-diabetes association (Houston et al., 2006). There was no association between serum cotinine levels <3ng/mL and diabetes mellitus. There was no appreciable association between serum cotinine levels (ng/mL) and glycohemoglobin (%) among never smokers.
The mechanisms underlying the association of ETS exposure and diabetes mellitus in never smokers remains unknown. A possible limitation to our study is the inability to adjust for variables such as the frequency of eating in restaurants, occupational hazards and neighborhoods, which might be correlated with ETS as well as diabetes, and hence might explain why we did not detect a cotinine-HbA1c association. Pre-clinical studies have reported an apoptotic effect of nicotine on the pancreatic beta cells (Borowitz and Isom, 2008; Bruin et al., 2008). In addition, nicotine exposure was found to be pro-inflammatory (Mao et al., 2012) and associated with insulin resistance (Chiolero et al., 2008), which are fundamental aspects in the development of type 2 diabetes (Kahn et al., 2006; Calle and Fernandez, 2012).
Several of the more important study limitations merit attention. The cross-sectional nature of NHANES does not allow us to draw temporal inferences or conclusions regarding the causal role of nicotine exposure in the development of diabetes mellitus. Serum cotinine measurements may reflect recent exposure if there are great differences between the current exposure sources and the past exposure sources for each subject. However, these biases are likely to be non-differential biases, which would bias the association towards the null. In addition, based on the distributions for age of first diabetes diagnosis, we judge that the majority of diabetes cases in our samples have type 2 diabetes mellitus. Nonetheless, there is some possibility that a minority of diabetes cases are type 1.
Despite limitations such as these, the study findings are of interest because of the relatively large nationally representative samples of US adults, the standardized data collection methods, and the ability to adjust for potential confounders. We believe that our use of serum cotinine rather than relying completely on self-report will minimize the potential for the misclassification of smoking status. In addition, we emphasize that the meta-analytic summary estimates are based on multiple independent replications in an attempt to account for the decreasing trend in ETS exposure among the general population, and in extension of the initial lines of epidemiological research on this topic where multiple years were merged together.
In conclusion, we have epidemiological evidence from five independently drawn replication samples from US community-dwelling adults on the association of ETS exposure evident by serum cotinine and diabetes mellitus among never smokers. The lack of a cotinine glycohemoglobin association might suggest that modest association might be explained by shared unmeasured psychosocial characteristics. However, ETS exposure and higher serum cotinine levels can be detrimental to health, especially in patients with diabetes mellitus. Heart diseases and stroke are major causes of death and disability among people with type 2 diabetes (American Diabetes Association, 2010). Never smokers with detectable cotinine levels had a higher susceptibility to cardiovascular disease (CVD) (Venn and Britton, 2007). Due to limited evidence, we cannot speculate if the co-occurrence of diabetes and ETS can affect the progression of CVD. Hence, prospective studies with adequate measurements are needed to further investigate this reported association.
FUNDING SOURCES AND ACKNOWLEDGMENTS
This work is completed during OA's second year of postdoctoral epidemiology fellowship, supported by the National Institute on Drug Abuse (T32DA021129). The authors would like to thank Dr. James C. Anthony for his valuable suggestions.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- United States Centers for Disease Control and Prevention Vital signs: nonsmokers' exposure to secondhand smoke --- United States, 1999-2008. MMWR Morb Mortal Wkly Rep. 2010 Sep;59(35):1141–6. ISSN 1545-861X. Available at: < http://www.ncbi.nlm.nih.gov/pubmed/20829748 >. [PubMed] [Google Scholar]
- United States Centers for Disease Control and Prevention State smoke-free laws for worksites, restaurants, and bars--United States, 2000-2010. MMWR Morb Mortal Wkly Rep. 2011 Apr;60(15):472–5. ISSN 1545-861X. Available at: < http://www.ncbi.nlm.nih.gov/pubmed/21508923 >. [PubMed] [Google Scholar]
- American Diabetes Association Standards of Medical Care in Diabetes—2010. Diabetes Care. 2010;33(Supplement 1):S11–S61. doi: 10.2337/dc10-S011. Available at: < http://care.diabetesjournals.org/content/33/Supplement_1/S11.short >. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benowitz NL. Cotinine as a Biomarker of Environmental Tobacco Smoke Exposure. Epidemiologic Reviews. 1996;18(2):188–204. doi: 10.1093/oxfordjournals.epirev.a017925. Available at: < http://epirev.oxfordjournals.org/content/18/2/188.short >. [DOI] [PubMed] [Google Scholar]
- Benowitz NL, et al. Optimal Serum Cotinine Levels for Distinguishing Cigarette Smokers and Nonsmokers Within Different Racial/Ethnic Groups in the United States Between 1999 and 2004. American Journal of Epidemiology. 2009;169(2):236–248. doi: 10.1093/aje/kwn301. Available at: < http://aje.oxfordjournals.org/content/169/2/236.abstract >. [DOI] [PubMed] [Google Scholar]
- Borowitz JL, Isom GE. Nicotine and Type 2 Diabetes. Toxicological Sciences. 2008;103(2):225–227. doi: 10.1093/toxsci/kfn050. Available at: < http://toxsci.oxfordjournals.org/content/103/2/225.short >. [DOI] [PubMed] [Google Scholar]
- Bruin JE, et al. Increased Pancreatic Beta-Cell Apoptosis following Fetal and Neonatal Exposure to Nicotine Is Mediated via the Mitochondria. Toxicological Sciences. 2008;103(2):362–370. doi: 10.1093/toxsci/kfn012. Available at: < http://toxsci.oxfordjournals.org/content/103/2/362.abstract >. [DOI] [PubMed] [Google Scholar]
- Calle MC, Fernandez ML. Inflammation and type 2 diabetes. Diabetes Metab. 2012 Jun;38(3):183–91. doi: 10.1016/j.diabet.2011.11.006. ISSN 1262-3636. Available at: < http://dx.doi.org/10.1016/j.diabet.2011.11.006 >. [DOI] [PubMed] [Google Scholar]
- Chiolero A, et al. Consequences of smoking for body weight, body fat distribution, and insulin resistance. The American Journal of Clinical Nutrition. 2008;87(4):801–809. doi: 10.1093/ajcn/87.4.801. Available at: < http://ajcn.nutrition.org/content/87/4/801.abstract >. [DOI] [PubMed] [Google Scholar]
- Connor Gorber S, et al. The accuracy of self-reported smoking: a systematic review of the relationship between self-reported and cotinine-assessed smoking status. Nicotine Tob Res. 2009 Jan;11(1):12–24. doi: 10.1093/ntr/ntn010. ISSN 1462-2203 (Print)1462-2203. Available at: < http://dx.doi.org/10.1093/ntr/ntn010 >. [DOI] [PubMed] [Google Scholar]
- DeAndrea DC, Troost JP, Anthony JC. Toward primary prevention of extra-medical OxyContin® use among young people. Preventive Medicine. 2013;57(3):244–246. doi: 10.1016/j.ypmed.2013.05.004. 9// ISSN 0091-7435. Available at: < http://www.sciencedirect.com/science/article/pii/S0091743513001497 >. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher MA, et al. Sociodemographic characteristics and diabetes predict invalid self-reported non-smoking in a population-based study of U.S. adults. BMC Public Health. 2007;7:33. doi: 10.1186/1471-2458-7-33. ISSN 1471-2458. Available at: < http://www.ncbi.nlm.nih.gov/pubmed/17352826 >. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geiss LS, et al. Prevalence and incidence trends for diagnosed diabetes among adults aged 20 to 79 years, United States, 1980-2012. JAMA. 2014 Sep;312(12):1218–26. doi: 10.1001/jama.2014.11494. ISSN 1538-3598. Available at: < http://www.ncbi.nlm.nih.gov/pubmed/25247518 >. [DOI] [PubMed] [Google Scholar]
- Houston TK, et al. Active and passive smoking and development of glucose intolerance among young adults in a prospective cohort: CARDIA study. BMJ. 2006 May;332(7549):1064–9. doi: 10.1136/bmj.38779.584028.55. ISSN 1756-1833. Available at: < http://www.ncbi.nlm.nih.gov/pubmed/16603565 >. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarvis MJ, et al. Comparison of tests used to distinguish smokers from nonsmokers. Am J Public Health. 1987 Nov;77(11):1435–8. doi: 10.2105/ajph.77.11.1435. ISSN 0090-0036. Available at: < http://www.ncbi.nlm.nih.gov/pubmed/3661797 >. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature. 2006 Dec 14;444(7121):840–6. doi: 10.1038/nature05482. ISSN 0028-0836. Available at: < http://dx.doi.org/10.1038/nature05482 >. [DOI] [PubMed] [Google Scholar]
- Mao J, et al. Nicotine induces the expression of C-reactive protein via MAPK-dependent signal pathway in U937 macrophages. Mol Cells. 2012 Nov;34(5):457–61. doi: 10.1007/s10059-012-0205-0. ISSN 0219-1032. Available at: < http://www.ncbi.nlm.nih.gov/pubmed/23149874 >. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Centers for Disease Control and Prevention . National Center for Health Statistics (NCHS), National Health and Nutrition Examination Survey Laboratory Protocol. Department of Health and Human Services, Centers for Disease Control and Prevention; Hyattsville, MD: U.S.: 2006. Avaialble at: < http://www.cdc.gov/nchs/nhanes/nhanes_citation.htm >. [Google Scholar]
- United States Centers for Disease Control and Prevention . National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Data. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2010. [11/1]. Avaialble at: < http://wwwn.cdc.gov/nchs/nhanes/search/nhanes09_10.aspx >. [Google Scholar]
- Venn A, Britton J. Exposure to secondhand smoke and biomarkers of cardiovascular disease risk in never-smoking adults. Circulation. 2007 Feb;115(8):990–5. doi: 10.1161/CIRCULATIONAHA.106.648469. ISSN 1524-4539. Available at: < http://www.ncbi.nlm.nih.gov/pubmed/17296856 >. [DOI] [PubMed] [Google Scholar]
- Wang Y, et al. Passive Smoking and Risk of Type 2 Diabetes: A Meta-Analysis of Prospective Cohort Studies. PLoS ONE. 2013;8(7):e69915. doi: 10.1371/journal.pone.0069915. Available at: < http://dx.doi.org/10.1371/journal.pone.0069915 >. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willi C, et al. Active smoking and the risk of type 2 diabetes: A systematic review and meta-analysis. JAMA. 2007;298(22):2654–2664. doi: 10.1001/jama.298.22.2654. ISSN 0098-7484. Available at: < http://dx.doi.org/10.1001/jama.298.22.2654 >. [DOI] [PubMed] [Google Scholar]