Abstract
A survivorship care plan refers to a written summary of the treatment received and recommendations regarding surveillance and management of late effects. To provide evaluation of a communication skills training (CST) intervention to enhance the transition of lymphoma survivors to cancer survivorship. Nineteen oncologists specializing in lymphoma treatment were recruited and completed a survivorship CST workshop, and two standardized patient assessments (SPAs), one pretraining and one posttraining. Significant improvements in SPA scores were observed in six of the seven SPA assessment categories: use of survivorship care plan, review of disease and treatment details, long-term effects, potential late effects, specific physician recommendations, and additional health maintenance recommendations. The intervention had significant effects on physicians’ uptake of new strategies and skills, as measured through pre- and posttraining SPAs, as well as on the physicians’ self-efficacy about having these conversations.
Keywords: Lymphoma, Communication skills training, Self-efficacy, Standardized patient assessments, Survivorship care plan
INTERVENTION FOR A NEW CONSULTATION ABOUT LYMPHOMA SURVIVORSHIP
There are over 12 million cancer survivors in the USA, the number tripling over the past 30 years due to advancements in treatment and detection; within the next 10 years, this number is projected to rise past 18 million (AACR) [1, 2]. The definition of a cancer survivor varies, some applying the term from diagnosis to the end of life as a form of motivation and empowerment [3]. Cancer centers most typically use the term for those who have completed primary treatment with curative intent, identifying a population of patients who could benefit from both surveillance for recurrence, and treatment or prevention of chronic or late effects from the malignancy or its treatment [4].
Survivors experience many challenges for which they are unprepared. The Institute of Medicine (IOM) issued their seminal 2005 report on cancer survivorship “Lost in Transition,” referring to the common experience when cancer treatment is completed and patients struggle to adopt their newfound identity as a cancer survivor. Along with both concerns regarding risks of relapse and late and long-term effects of cancer and its treatment, survivors are also at risk of anxiety, depression, and problem coping [3]. When care for survivors is insufficient, these risks can be compounded and their consequences amplified. There is evidence of long-term psychological stress in adult cancer patients (for instance, survivors of leukemia or stem cell transplantation), who show higher levels of distress than the baseline population [5–7]. Somatic complaints and use of health care services are higher than controls [6–8]. Survivors of Hodgkin’s lymphoma have more anxiety, depression, and fatigue.
Lymphoma provides a suitable clinical example in which to examine how effectively we can train clinicians to discuss survivorship because the likelihood of cure from Hodgkin’s lymphoma [9] and the commonest form of Non-Hodgkin’s Lymphoma, specifically diffuse large B-cell lymphoma [10–12], is now over 90 %. Moreover, because consolidative radiation therapy is still needed in many patients, education of patients about late effects is important for their long-term wellbeing. Several studies have highlighted the many morbidities that can develop in these patients [13–16].
Survivorship care planning appears critical to ensure survivors do not “fall through the cracks” of the health care system [3, 17]. The IOM recommended providing a follow-up care plan to all cancer survivors [1], which should include a written summary of the treatment received and recommendations regarding surveillance and management of late effects, but few patients currently receive survivorship care plans (SCPs) upon transitioning to primary care [18]. In a recent study, a nationally representative sample of 1130 oncologists and 1020 primary care physicians was surveyed about survivorship care practices with survivors [19]. Results of the survey clearly indicated that a majority of oncologists (64 %) and primary care physicians (88 %) reported discussing survivorship care recommendations with survivors. However, less than half (32 %) of the oncologists discussed whom survivors should see for cancer-related and other follow-up care, and <5 % also provided a written SCP to the survivor. The results also demonstrated that oncologists who reported detailed training about late and long-term effects of cancer were more likely to provide written SCPs and discuss survivorship care planning with survivors. As well, primary care physicians who received SCPs from oncologists were nine times more likely to report survivorship discussions with survivors. Thus, training and knowledge specific to survivorship care and coordinated care between primary care physicians and oncologists were associated with increased survivorship discussions with survivors [19].
The American Society for Clinical Oncology has taken a leadership role in promoting the use of survivorship care plans [20]. As well, the Commission on Cancer (CoC) of the American College of Surgeons mandated patient-centered standards of care in 2012, including a focus on SCP that summarizes care received and provides a roadmap for future care needs [21]. The rationale is for these to summarize in writing what has happened and what patient needs exist now for long-term follow-up, late effects management, rehabilitation, adaptation, and health promotion. The goal is praiseworthy, but its translation into practice is challenging [22–24]. Successful adoption of survivorship care plans is further hampered by a lack of physician training in the use of survivorship care plans in transitioning patients [19, 23, 24].
Communication skills training (CST) programs have demonstrated effectiveness in improving physician communication skills both generally and in specific contexts (e.g., Breaking Bad News; see [25]). Our research team has successfully built a comprehensive communication skills training program at the Memorial Sloan Kettering Cancer Center (MSKCC) [26–28]. Thus, we chose to use similar educational methods to develop and implement a new survivorship CST module, in order to help oncologists effectively use a survivorship care plan in their interactions with patients. This CST module provides a structured method to review and prioritize with the patient a personalized care plan for their future. We hypothesized that new skill acquisition of using the care plan properly will be achieved through demonstrated best practices in CST, including modeling of exemplary behaviors and facilitator-led small group role play practice with continuous feedback leading to a dynamically iterative process of behavior change.
COMMUNICATION SKILLS TRAINING ABOUT LYMPHOMA SURVIVORSHIP
Our research team’s overall goal is to understand the impact of a patient-centered survivorship consultation, using a survivorship care plan. To begin with, we needed to develop a training intervention to prepare physicians for this type of consultation with their patients. For the project reported on in this paper, we used our previously well-developed model for CST interventions that explicitly defines the important components that we teach [29]. In doing so, we conceive of patient–provider consultations as having communication goals. For the module that was tested in this intervention, entitled “Transitioning a lymphoma patient to survivorship” the communication goal is “To facilitate the patient’s adaptation to their new role as a cancer survivor after they have completed their primary anti-cancer treatment through i) review of their diagnosis, treatment, and prognosis to promote integration of knowledge; ii) creation of a continuing care plan covering anti-cancer monitoring, cancer screening and health promotion, potential late or long-term effects from treatment, and any lifestyle implications for their future; and iii) promotion of their sense of efficacy and confidence in their future.” The communication goal gives us a framework from which to build up a common sense understanding of cancer survivorship. We then distinguish between communication strategies (defined as a priori plans that direct communication behaviors toward the successful realization of the goal), skills (defined as discrete verbal utterances by which a physician can further the clinical dialogue), and tasks (defined as sets of verbal or nonverbal behaviors or dialogues which create an environment for effective communication) as the means to achieve this communication goal. The strategies, skills, and tasks were organized into a modular blueprint (Table 1). This blueprint is intended to act as conceptual map for the consultation, not as a script or checklist that should be followed exactly. The purpose of our conceptual model is to promote individualized, patient-centered approaches to communication.
Table 1.
Modular blueprint for communication skills training intervention for lymphoma survivorship
| Strategy | Tasks | Skills |
|---|---|---|
| 1. Establish the consultation framework as being about the identification of the completion of primary anti-cancer treatment and the need to transition into survivorship | Set up as a discrete appointment | Declare your agenda items |
| Create a focus on survivorship and what is meant by “transition” into survivorship | Invite patient agenda items | |
| Negotiate agenda | ||
| 2. Review patient’s knowledge about his/her diagnosis and treatment | Create a written summary of the following: | Check patient understanding |
| Cancer diagnosis | Categorize | |
| Key test results | Summarize | |
| Staging and prognosis | Invite patient questions | |
| Treatment given | ||
| Names and doses of agents | ||
| Relevant toxicities, if occurred | ||
| 3. Check patient’s coping and concerns | Discuss “uncertainty” if raised | Ask open questions |
| Discuss strategies to cope with “fear of recurrence” if present | Encourage expression of feelings | |
| Empathically acknowledge, normalize or validate feelings | ||
| Promote hope with an emphasis on constructive framing of the prognosis | Praise patient efforts | |
| Identify future care plan as a source of support | Clarify and restate if needed | |
| 4. Provide an overview of the goals of future care, schedule of follow-up visits, scanning frequency and monitoring plan | Create a written future care plan summary with the following: | Preview information |
| Schedule of future visit frequencies | Categorize | |
| Elements of shared multidisciplinary follow-up care | Summarize | |
| Cancer monitoring schedule | Check understanding | |
| Symptoms to report | ||
| 5. Ascertain patient’s understanding of long-term effects and interest in knowledge about late effects and discuss as appropriate | Identify likely long-term effects of treatments | Check patient preference information |
| Identify potential late effects | Preview information | |
| Consider genetic or familial risk | Summarize | |
| Add any monitoring steps to written care plan | Check understanding | |
| 6. Ascertain interest in health promotion behaviors, lifestyle concerns, and discuss as appropriate | Identify value in screening for other cancers | Endorse question asking |
| Name and discuss any key steps in health promotion: exercise, nutrition and weight, smoking cessation, alcohol moderation, sun protection, chemoprevention approaches | Check patient preference information | |
| Add any key health promotion behaviors to written care plan | Preview information | |
| Review as appropriate: relational and sexual functioning, fertility concerns, family impact, work issues, financial impact, insurance concerns, fear of recurrence, future coping and support, community resources—groups, programs, primary care clinician | Summarize | |
| Add any key plans to written care plan | Review next steps | |
| Check understanding | ||
| Encourage expression of feelings and empathize | ||
| 7. Review overall understanding about the constructed survivorship care plan | Give patient a copy of the cancer treatment summary and care plan | Check patient understanding |
| Offer letter about summary and written care plan to primary care physician and other shared care clinicians or nurses | Correct misunderstandings | |
| Provide future appointments | Endorse question asking | |
| Express a willingness to help |
We developed structured patient assessments (SPAs) and conducted a pilot CST workshop to train nine fellows working with the lymphoma service at MSKCC. In pretraining SPAs, these participants’ mean activity rating score was 19.44 (SD = 3.09) (range, 14–23 out of 36 tasks); in posttraining SPAs, mean score = 28.22 (SD = 5.17) (range, 19–35); using paired t tests, p < 0.01 (effect size, Cohen’s d = 2.06). Effect sizes for key activities include “offer to write to GP” d = 3.4, “discusses care plan” d = 2.6, “cancer screening” d = 1.2, “health promotion” d = 1.1, “long-term effects” d = 0.8, “late effects” d = 0.7, and “plan for future visits” d = 0.7. Significant skill increases were seen in checking understanding, declaring agendas, seeking out patients’ agenda, and previewing information. This pilot work established reasonable preliminary evidence for the value of our CST module.
In this paper, we report on the development and evaluation of this CST workshop to train physicians in the provision of a new consultation that is focused on a patient-centered approach to cancer survivorship. Our CST module provides a structured method to review and prioritize this personalized care plan for their future. Demonstration of the efficacy of this CST intervention will advance survivorship care. We hypothesized that new skill acquisition will be achieved through a variety of techniques and resources, including modular approaches to categorization, use of naturalistic sequences, modeling of exemplary behaviors, and practice with continuous feedback leading to a dynamically iterative process of behavior change. Here, we present the evaluation of a CST Module to Enhance Transition to Cancer Survivorship.
METHODS
Design
The CST intervention we report here was nested within a larger ongoing study involving a cluster-randomized, clinical trial design. Participating sites were stratified by size and randomized to either experimental or control groups. The CST survivorship intervention was delivered to physicians at two sites, Memorial Sloan Kettering Cancer Center (New York, NY, USA), and Moffitt Cancer Center (Tampa, FL, USA), while clinicians at Maimonides Medical Center (Brooklyn, NY, USA) and MD Anderson Cancer Center (Houston, TX, USA) were trained in an attention-time control consultation that focused on general rehabilitation, with exercise and dietary instruction. In this paper, we only report on the training delivered to the experimental group—the physicians discussing lymphoma survivorship at MSKCC and Moffitt.
Participants and procedure
Nineteen (N = 19) oncologists specializing in treatment of lymphoma were recruited from their departments and, after providing informed consent, completed a survivorship training based upon the described CST model of workshop. The training was a workshop of 5-h duration, with two SPAs (one pre, one post) and 2.5 h of structured teaching and role play. The format included a didactic presentation about survivorship, review of the evidence that describes the need for a survivorship consultation, covering themes for survivors in general and then lymphoma survivors in particular (such as dealing with fear of recurrence, frequency of scans, health promotion, and screening issues; 30 min), an exemplary video (15 min) featuring a senior MSKCC lymphoma physician modeling the strategies in the survivorship module (see Table 1), role play work about transitioning patients to lymphoma survivorship (3 h), and concluding with a reflective discussion about the benefits and barriers in implementation through creating a dedicated consultation focusing on survivorship (15 min). To evaluate the effectiveness of the training, we asked the oncologists to participate in 15-min pre- and posttraining SPAs and to complete a course evaluation form.
Standardized patient assessments
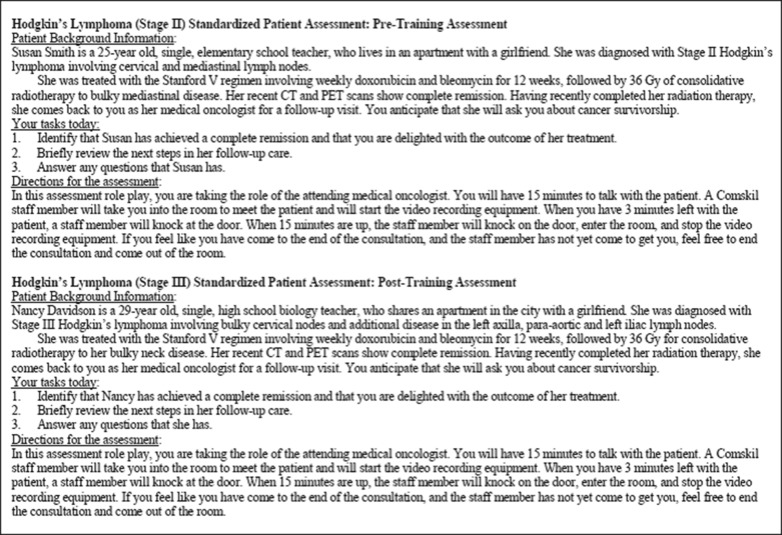
Fifteen-minute SPAs were recorded pre- and posttraining (on the training day; see Fig. 1 for the pre- and posttraining SPA scenarios). The SPA was an interaction of the physician with a standardized patient (actor). The SPAs were video recorded. Blinded coding was completed by two of the co-authors (SB and KM) with a coding manual developed for Transition to Survivorship module. The SPA has been shown to be a reliable assessment with discriminant validity [30].
Fig 1.
Pre- and posttraining standardized patient assessments
The SPA coding manual was developed through the pilot (DK and CB) and covered seven key activities undertaken within the consultation focused on survivorship (the SPA coding manual is available from the first author). The coding manuals provide a glossary of behaviors to standardize recognition between coders. Interrater reliability was established at r = 0.99 for this module.
The seven categories assessed in the Transition to Survivorship Coding Schema included (1) use of survivorship care plan, (2) disease and treatment details, (3) long-term effects discussion, (4) potential late effects discussion, (5) specific physician recommendations, (6) additional health maintenance recommendations, and (7) possible social issues discussion. These are summed to generate a score for total adherence to survivorship care plan. The physicians received a score for each individual item that they completed within each category. For instance, disease and treatment details included seven individual activities (e.g., reviews type of lymphoma, reviews chemotherapy drugs). Physicians received a score of “1” if they completed each activity, and the overall category score was a summed score of individual activities. Given that the categories of “specific physician recommendations” and “additional health maintenance recommendations” differed for male and female patients (e.g., the recommendation of Pap smear is applicable only to female patients), we calculated a percentage score for the two categories.
We also used the Comskil coding schema [26, 29] to examine change in general use of communication skills from before to after training. This coding schema charts the use of core communication skills (such as agenda setting, check understanding, acknowledge, and validate) that are foundational in our other CST programs.
Course evaluations
At the end of the module, participants were given an evaluation form that contained eight statements about the workshop. All course evaluation measures were rated using a 5-point Likert scale with anchors at 1 (strongly disagree) and 5 (strongly agree). A retrospective pre–postmethodology [31] was used in the first two statements: (1) “Before this module, I felt confident discussing the transition to survivorship with my patients” and (2) “Now that I have attended this module, I feel confident in my ability to discuss the transition to survivorship with my patients.” The rest of the items focused on posttraining attitudes regarding the skills learned and how they could be applied during routine clinical practice and for better patient care.
RESULTS
Effect of training on SPAs
Paired sample t test results clearly indicate significant improvements (i.e., posttraining scores > pretraining scores) in six of the seven levels of SPA assessment categories: use of survivorship care plan, t(18) = −18.00, p < 0.001; review of disease and treatment details, t(18) = −8.81, p < 0.001; long-term effects discussion, t(18) = −9.35, p < 0.001; potential late effects discussion, t(18) = −4.86, p < 0.001; specific physician recommendations, t(18) = −5.38, p < 0.001; and additional health maintenance recommendations, t(18) = −3.13, p < 0.01 (see Table 2).
Table 2.
Pre- and poststandardized patient assessment results for physicians participating in communication skills training intervention for lymphoma survivorship (N = 19)
| Pre | Post | t (18) | Cohen’s d | |
|---|---|---|---|---|
| M (SD) | M (SD) | |||
| 1. Use of survivorship care plan (out of 1) | 0.00 (0.00) | 0.95 (0.23) | −18.00*** | 5.87 |
| 2. Disease and treatment details (out of 7) | 2.84 (1.21) | 6.37 (1.34) | −8.81*** | 2.76 |
| 3. Long-term effects discussion (out of 7) | 1.16 (1.07) | 5.11 (2.01) | −9.35*** | 2.47 |
| 4. Potential late effects discussion (out of 6) | 2.32 (1.46) | 4.26 (1.15) | −4.86*** | 1.48 |
| 5. Specific physician recommendations (out of 10 for female, out of 8 for male) | 0.24 (0.18) | 0.61 (0.26) | −5.38*** | 2.70 |
| 6. Additional health maintenance recommendations (out of 4 for female, out of 2 for male) | 0.21 (0.31) | 0.57 (0.37) | −3.13** | 1.03 |
| 7. Possible social issues discussion (out of 4) | 1.13 (0.97) | 1.38 (1.49) | −1.05 | – |
| Total adherence to survivorship care plan (out of 39 for female, out of 35 for male) | 0.27 (0.10) | 0.68 (0.15) | −10.11*** | 3.23 |
Given that the categories of “specific physician recommendations” and “additional health maintenance recommendations” differed for male and female patients (e.g., the recommendation of Pap smear is applicable only to female patients), we calculated a percentage score for the two categories. The final category, i.e., “Total adherence to survivorship care plan” also presents a percentage score
**p < 0.01, ***p < 0.001
In addition, we undertook Comskil coding [26, 29] and saw significant gains in the use of core communication skills, specifically agenda setting [(pre-SPA: mean = 0.16; SD = 0.38; post-SPA: mean = 0.68; SD = 0.48), t = −3.75, p < 0.001, d = 1.21] and physician’s checking of patients’ understanding of their illness [(pre-SPA: mean = 0.53, SD = 1.22; post-SPA: mean = 1.21, SD = 1.03), t = −2.17, p < 0.05, d = 0.60].
Results for course evaluations
The oncologists’ confidence in discussing the transition to survivorship with patients increased significantly when compared before and after they attended the survivorship training, t(15) = −2.76, p < 0.05. Mean agreement to the pretraining self-efficacy item was 4.03 (SD = 1.03) and to the posttraining self-efficacy item was 4.69 (SD = 0.48).
Additionally, we combined physician ratings of “agree” or “strongly agree” to be an indicator of satisfaction with the lymphoma survivorship training and its effectiveness. Table 3 displays the percentages of participating physicians who reported satisfaction with the six posttraining items. Overall, participants agreed or strongly agreed to all items 87.5–100 % of the time.
Table 3.
Participant ratings of communication skills training intervention for lymphoma survivorship (N = 16)
| Items from course evaluations | “Agree” or “strongly agree” (%) |
|---|---|
| 1. I feel confident that I will use the skills I learned in this module | 100 |
| 2. The skills I learned in this module will allow me to provide better patient care | 87.50 |
| 3. The module prompted me to critically evaluate my own communication skills | 93.75 |
| 4. The experience of video feedback was helpful to the development of my skills | 87.50 |
| 5. The skills I learned were reinforced through the feedback I received in the small group | 100 |
| 6. The small group facilitators were effective | 100 |
DISCUSSION
We developed and tested a CST intervention for oncologists about discussing the transition to survivorship using a survivorship care plan for lymphoma patients. The intervention had significant effects on the physicians’ uptake of new tasks and skills, as measured through pre- and posttraining SPAs, as well as on the physicians’ self-efficacy about having these conversations.
Of note, we saw relatively large effect sizes comparing the post- to pre-SPA scores across the categories assessed. The pre-SPAs were a baseline, showing us what the oncologists’ regular practices were. The largest change was observed in the Use of Survivorship Care Plan. This was expected, as routine use of survivorship care plans was not the norm at either center prior to study enrollment. The other six categories better represented how the oncologists may have been discussing survivorship themes before attending the CST intervention. For instance, for the discussion of Disease and Treatment Details, some participating oncologists were already doing this well prior to the training intervention.
The one category in which we did not see significant improvement was discussion of social issues. In general, approximately one social issue was discussed at the pre-SPA and one at the post-SPA. One possible reason for the lack of a significant finding here could be that the participants did not see them as important as other issues. Another reason could be that in a real visit, patients develop a relationship with their oncologists during treatment and some social discussions may have happened earlier. In a simulated assessment of a real visit, a physician may have felt awkward bringing up social issues at this point in the relationship, reasoning that they would have already been discussed. Our goal is not to create a scripted consultation whose activities are obsessively adhered to, but rather to always affirm the patient-centered session in which issues and concerns relevant to each patient are focused on.
Limitations of this study include the time-limited SPA and the limitations of utilizing a pre–postdesign exist, including teaching to the posttest, and attributing positive change to participant maturation and learning the test rather than knowledge gain. Although we showed through an exemplary video in the didactic presentation that the survivorship consultation can be completed in a total of 15 min, physicians may have felt as if they did not have enough time in the SPA to demonstrate all of the skills that had been taught. The selection of 15 min was pragmatic and intended to reassure the busy clinician that a lot can be achieved in discussing survivorship in a limited amount of time. Further, some oncologists may have performed differently due to the artificiality of the SPA. In the real world of the clinic, the amount of time needed to discuss survivorship care plans will surely vary by patient and clinician. Our hope would be that it is always patient centered and fully responsive to each person’s need. Additionally, in order to address the limitations of a traditional pre–postdesign, we utilized different SPAs at pre- and posttests. Our study is a proof of concept endeavor, rather than something immediately generalizable to other cancer types.
An additional limitation of this study is this pilot was conducted at two comprehensive cancer centers. Dissemination of this pilot study to community-based centers could be done through at least two different methods. Train-the-trainer courses offered to physicians/educators from other centers would allow those instructors to take the course back to their home institution. Alternatively, a web-based module could be developed for broad dissemination.
The implementation of this CST intervention is only the first step in our larger study. Kirkpatrick has described four levels of outcome for educational interventions: (1) initial reaction or sense of self-efficacy, (2) new learning or actual skill acquisition, (3) new behaviors or transfer into the clinic, and (4) societal changes with better patient outcomes [32, 33]. We were able to test immediately whether this intervention would lead to learning (Kirkpatrick’s level 1 and 2); the second phase of this larger study involves the oncologists having these consultations with real lymphoma patients transitioning to survivorship (Kirkpatrick’s level 3) and subsequently measuring the effects at the patient level (Kirkpatrick’s level 4). Thus, in this second phase, we will ascertain whether the oncologists are able to transfer these learned skills from the laboratory in which they were learned to real clinic settings. Throughout the second phase of the study, we are recording the oncologists’ communication in their survivorship visits and are providing them with continual feedback on their communication to ensure fidelity to the model in which they were trained. In the third phase of the study, we will follow patients who participate in survivorship consultations with these physicians, comparing their outcomes to those of patients of physicians in the control group. We hope to prove that the CST intervention will shape the knowledge and health beliefs that the lymphoma survivor takes forward with them, potentially improving their adherence to physicians’ recommendations.
Acknowledgments
The project described was supported by Award Number R01CA151899 from the National Cancer Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health. The funders played no role in the design, conduct, or analysis of the study, nor in the interpretation and reporting of the study findings. The researchers were independent from the funders. All authors, external and internal, had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
Conflict of interest
The authors declare that they have no competing interests.
Adherence to ethical standards
All procedures, including the informed consent process, were conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Footnotes
Implications
Practice: Oncologists should create individualized survivorship care plans that include a written summary of the treatment received and recommendations regarding surveillance and management of late effects, and utilize them during consultations with cancer survivors and transitioning patients.
Policy: In order to implement American Society for Clinical Oncology’s recommendation for the use of survivorship care plans, training of oncologists in utilization of care plans should be mandated.
Research: Researchers should investigate oncologists’ use of survivorship care plans in consultations with cancer survivors in clinics and the effects on patient outcomes such as growth in knowledge about disease and treatment and adherence to physicians’ recommendations posttreatment.
References
- 1.Institute of Medicine. Cancer survivorship care planning. www.iom.edu. 2005. 13 Dec 2013.
- 2.Institute of Medicine. Employment and health insurance concerns. www.iom.edu. 2005. 4 Dec 2013.
- 3.Coleman D, Shigemasa S. Cancer survivorship requires long-term follow-up. Hawaii Med J. 2007;66(4):104. [PubMed] [Google Scholar]
- 4.Twombly R. What’s in a name: who is a cancer survivor? J Natl Cancer Inst. 2004;96(19):1414–1415. doi: 10.1093/jnci/96.19.1414. [DOI] [PubMed] [Google Scholar]
- 5.Greenberg DB, Kornblith AB, Herndon JE, Zuckerman E, Schiffer CA, Weiss RB, et al. Quality of life for adult leukemia survivors treated on clinical trials of cancer and leukemia group B during the period 1971–1988: predictors for later psychologic distress. Cancer. 1997;80(10):1936–1944. doi: 10.1002/(SICI)1097-0142(19971115)80:10<1936::AID-CNCR10>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 6.Kornblith AB, Powell M, Regan MM, Bennett S, Krasner C, Moy B, et al. Long-term psychosocial adjustment of older vs younger survivors of breast and endometrial cancer. Psychooncology. 2007;16(10):895–903. doi: 10.1002/pon.1146. [DOI] [PubMed] [Google Scholar]
- 7.Liavaag AH, Dorum A, Fossa SD, Trope C, Dahl AA. Controlled study of fatigue, quality of life, and somatic and mental morbidity in epithelial ovarian cancer survivors: how lucky are the lucky ones? J Clin Oncol. 2007;25(15):2049–2056. doi: 10.1200/JCO.2006.09.1769. [DOI] [PubMed] [Google Scholar]
- 8.Costanzo ES, Lutgendorf SK, Mattes ML, Trehan S, Robinson CB, Tewfik F, et al. Adjusting to life after treatment: distress and quality of life following treatment for breast cancer. Br J Cancer. 2007;97(12):1625–1631. doi: 10.1038/sj.bjc.6604091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Connors JM. State-of-the-art therapeutics: Hodgkin’s lymphoma. J Clin Oncol. 2005;23(26):6400–6408. doi: 10.1200/JCO.2005.05.016. [DOI] [PubMed] [Google Scholar]
- 10.Sehn LH, Berry B, Chhanabhai M, Fitzgerald C, Gill K, Hoskins P, et al. The revised International Prognostic Index (R-IPI) is a better predictor of outcome than the standard IPI for patients with diffuse large B-cell lymphoma treated with R-CHOP. Blood. 2007;109(5):1857–1861. doi: 10.1182/blood-2006-08-038257. [DOI] [PubMed] [Google Scholar]
- 11.Moskowitz CH, Schoder H, Teruya-Feldstein J, Sima C, Iasonos A, Portlock CS, et al. Risk-adapted dose-dense immunochemotherapy determined by interim FDG-PET in advanced-stage diffuse large B-cell lymphoma. J Clin Oncol. 2010;28(11):1896–1903. doi: 10.1200/JCO.2009.26.5942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dunleavy K, Pittaluga S, Maeda LS, Advani R, Chen CC, Hessler J, et al. Dose-adjusted EPOCH-rituximab therapy in primary mediastinal B-cell lymphoma. N Engl J Med. 2013;368(15):1408–1416. doi: 10.1056/NEJMoa1214561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mols F, Aaronson NK, Vingerhoets AJ, Coebergh JW, Vreugdenhil G, Lybeert ML, et al. Quality of life among long-term non-Hodgkin lymphoma survivors: a population-based study. Cancer. 2007;109(8):1659–1667. doi: 10.1002/cncr.22581. [DOI] [PubMed] [Google Scholar]
- 14.Hammond CT, Beckjord EB, Arora NK, Bellizzi KM, Jeffery DD, Aziz NM. Non-Hodgkin's lymphoma survivors’ fertility and sexual function-related information needs. Fertil Steril. 2008;90(4):1256–1258. doi: 10.1016/j.fertnstert.2007.08.081. [DOI] [PubMed] [Google Scholar]
- 15.Doorduijn J, Buijt I, Holt B, Steijaert M, Uyl-de Groot C, Sonneveld P. Self-reported quality of life in elderly patients with aggressive non-Hodgkin’s lymphoma treated with CHOP chemotherapy. Eur J Haematol. 2005;75(2):116–123. doi: 10.1111/j.1600-0609.2005.00438.x. [DOI] [PubMed] [Google Scholar]
- 16.Merli F, Bertini M, Luminari S, Mozzana R, Berte R, Trottini M, et al. Quality of life assessment in elderly patients with aggressive non-Hodgkin's lymphoma treated with anthracycline-containing regimens. Report of a prospective study by the Intergruppo Italiano Linfomi. Haematologica. 2004;89(8):973–978. [PubMed] [Google Scholar]
- 17.Salz T, Oeffinger K, McCabe M, Layne T, Bach P. Survivorship care plans in research and practice. CA Cancer J Clin. 2012;62:101–117. doi: 10.3322/caac.20142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Keesing S, McNamara B, Rosenwax L. Cancer survivors’ experiences of using survivorship care plans: a systematic review of qualitative studies. J Cancer Surviv. 2015; 9: 260-268. [DOI] [PMC free article] [PubMed]
- 19.Blanch-Hartigan D, Forsythe LP, Alfano CM, Smith T, Nekhlyudov L, Ganz PA, et al. Provision and discussion of survivorship care plans among cancer survivors: results of a nationally representative survey of oncologists and primary care physicians. J Clin Oncol. 2014 doi: 10.1200/JCO.2013.51.7540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rowland JH, Hewitt M, Ganz PA. Cancer survivorship: a new challenge in delivering quality cancer care. J Clin Oncol. 2006;24(32):5101–5104. doi: 10.1200/JCO.2006.09.2700. [DOI] [PubMed] [Google Scholar]
- 21.Commission on Cancer . Cancer Program Standards 2012: Ensuring Patient-Centered Care. Chicago: American College of Surgeons; 2012. p. 2012. [Google Scholar]
- 22.Hewitt ME, Bamundo A, Day R, Harvey C. Perspectives on post-treatment cancer care: qualitative research with survivors, nurses, and physicians. J Clin Oncol. 2007;25:2270–2273. doi: 10.1200/JCO.2006.10.0826. [DOI] [PubMed] [Google Scholar]
- 23.Ganz PA, Hahn EE. Implementing a survivorship care plan for patients with breast cancer. J Clin Oncol. 2008;26(5):759–767. doi: 10.1200/JCO.2007.14.2851. [DOI] [PubMed] [Google Scholar]
- 24.Ganz PA, Earle CC, Goodwin PJ. Journal of Clinical Oncology update on progress in cancer survivorship care and research. J Clin Oncol. 2012;30(30):3655–3656. doi: 10.1200/JCO.2012.45.3886. [DOI] [PubMed] [Google Scholar]
- 25.Rosenbaum ME, Ferguson KJ, Lobas JG. Teaching medical students and residents skills for delivering bad news: a review of strategies. Acad Med. 2004;79(2):107–117. doi: 10.1097/00001888-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 26.Bylund CL, Brown R, Gueguen JA, Diamond C, Bianculli J, Kissane DW. The implementation and assessment of a comprehensive communication skills training curriculum for oncologists. Psychooncology. 2010;19(6):583–593. doi: 10.1002/pon.1585. [DOI] [PubMed] [Google Scholar]
- 27.Bylund CL, Brown RF, Bialer PA, Levin TT, Lubrano di Ciccone B, Kissane DW. Developing and implementing an advanced communication training program in oncology at a comprehensive cancer center. J Cancer Educ. 2011;26(4):604–611. doi: 10.1007/s13187-011-0226-y. [DOI] [PubMed] [Google Scholar]
- 28.Kissane DW, Bylund CL, Banerjee SC, Bialer P, Levin T, Maloney EK, et al. Special series (whole patient): communication skills training for oncology professionals. J Clin Oncol. 2012;30(11):1242–1247. doi: 10.1200/JCO.2011.39.6184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brown RF, Bylund CL. Communication skills training: describing a new conceptual model. Acad Med. 2008;83(1):37–44. doi: 10.1097/ACM.0b013e31815c631e. [DOI] [PubMed] [Google Scholar]
- 30.Sloan D. Use of an objective structured clinical examination (OSCE) to measure improvement in clinical competence during the surgical internship. Surgery. 1993; 114: 343 -350. [PubMed]
- 31.Razavi D. Brief psychological training for health care professionals dealing with cancer patients: a one year assessment. Gen Hosp Psychiatry. 1991;13(4):253–260. doi: 10.1016/0163-8343(91)90126-H. [DOI] [PubMed] [Google Scholar]
- 32.Kirkpatrick DL. Evaluation of training. In: Craig R, Bittlel I, editors. Training and Development Handbook. New York: McGraw Hill; 1967. [Google Scholar]
- 33.Konopasek L, Rosenbaum M, Encandela J, Cole-Kelly K. Evaluating communication skills training courses. In: Kissane DW, Bultz BD, Butow PN, Finaly IG, editors. Handbook of Communication in Oncology and Palliative Care. Oxford: Oxford University Press; 2010. pp. 683–693. [Google Scholar]