Abstract
AIM: To study the different therapy for different types of ulcerative colitis (UC) in China.
METHODS: Among 102 UC patients, 42 chronic relapse type UC patients were randomly divided into olsalazine sodium treatment group (n = 21) and SASP group (n = 21). Clinical effects and safety were observed in the 2 groups. Forty-two first episode type UC patients were randomly divided into Heartleaf houttuynia herb treatment group (n = 21) and SASP group (n = 21). Clinical effects were observed in the 2 groups while ultrastructure of colonic mucosa, ICAM-1 and the pressure of distant colon were studied in Heartleaf houttuynia herb group. Eighteen patients (8 males, 10 females) with refractory UC and unresponsive to high-dose prednisolone and sulfasalazine therapy more than one month were treated with Kangshuanling (7200 U/d). Prednisolone was gradually stopped and sulfasalazine was maintained. Stool frequency, rectal bleeding, colonoscopy, general well-being, histology were observed and CD62p, CD63, CD54, Pgp-170 (flow cytometry), TXA2 (RIA), blood platelet aggregation rate and thrombosis length in vitro were assessed.
RESULTS: In the 42 chronic relapse type UC patients, the overall clinical effects of olsalazine sodium group (complete remission in 16, improvement in 4, inefficiency in 1) were better than those of SASP group (complete remission in 10, improvement in 4, inefficiency in 7, P < 0.05). Symptomatic remission of olsalazine sodium group (complete remission in 15, partial remission in 5, inefficiency in 1) was better than that of SASP group (complete remission in 10, partial remission in 5, inefficiency in 6, P < 0.05). The colonoscopic remission of olsalazine sodium group(complete remission in 11, partial remission in 9, inefficiency in 1) was better than that of SASP group (complete remission in 7, partial remission in 8, inefficiency in 6, P < 0.05). The histologic remission of olsalazine sodium group (complete remission in 13, partial remission in 7, inefficiency in in 1) was better than that of SASP group (complete remission in 6, partial remission in 10, inefficiency in 5, P < 0.05). The side effects of gastrointestinal tract in olsalazine sodium group were less than those of SASP group except for frequency of watery diarrhea. No other side effects were observed in olsalazine sodium group while ALT increase, WBC decrease and skin eruption were observed in SASP group. Two patients relapsed in olsalazine sodium group while 8 cases relapsed in SASP group during the flow-up period (from six months to one year). In the 42 first episode type UC patients, the clinical effect of Heartleaf houttuynia herb group (complete remission in 20, 95.2%; improvement in 1, 4.8%) was better than that of SASP group (complete remission in 15, 72.4%, improvement in 5, 23.8%; inefficiency in 1, 3.8%, P < 0.01). The time of stool frequency recovering to normal (5.6 ± 3.3 d), and blood stool disappearance (6.7 ± 3.8 d) and abdominal pain disappearance (6.1 ± 3.5 d) in Heartleaf houttuynia herb group was all shorter than that in SASP group (9.5 ± 4.9 d, 11.7 ± 6.1 d, 10.6 ± 5.3 d, P < 0.01). Heartleaf houttuynia herb could inhibit the epithelial cell apoptosis of colonic mucous membrane and the expression of ICAM-1 (45.8% ± 5.7% vs 30.7% ± 4.1%, P < 0.05). Compared with normal persons, the mean promotive speed of contraction wave stepped up (4.6 ± 1.6 cm/min vs 3.2 ± 1.8 cm/min, P < 0.05) and the mean amplitude of the wave decreased (14.2 ± 9.3 kPa vs 18.4 ± 8.0 kPa, P < 0.05) in active UC patients. After treatment with Heartleaf houttuynia herb, these 2 indexes improved significantly (17.3 ± 8.3 kPa, 3.7 ± 1.7 cm/min, P < 0.05). In normal persons, the postprandial pressure of sigmoid (2.9 ± 0.9 kPa) was higher than that of descending colon (2.0 ± 0.7 kPa) and splenic flexure (1.7 ± 0.6 kPa), while the colonic pressure (1.5 ± 0.5 kPa, 1.4 ± 0.6 kPa, 1.3 ± 0.6 kPa) decreased significantly (P < 0.05) in active UC patients. After treatment with Heartleaf houttuynia herb, the colonic pressure (2.6 ± 0.8 kPa, 1.8 ± 0.6 kPa, 1.6 ± 0.5 kPa) recovered to normal. The pain threshold of distant colon (67.3 ± 18.9 mL) in active UC patients decreased significantly compared with that of normal persons (216.2 ± 40.8 mL, P < 0.05) and recovered to normal after treatment with Heartleaf houttuynia herb(187.4 ± 27.2 mL, P < 0.05). In the 18 refractory UC patients with platelet activation, after more than 4 wk of combined Kangshuanling and sulfasalazine therapy, 16 patients achieved clinical remission, with a highly significant statistical difference (P < 0.01) between pre-and post-treatment mean scores for all disease parameters: stool frequency (8.2/d vs 1.6/d), rectal bleeding (score 2.7 vs 0.3), colonoscopy (score 2.6 vs 1.1), histology (score 12.0 vs 5.0), general well being (score 4.0 vs 0.6) and CD62p (8.0% ± 3.1% vs 4.1% ± 1.8%), CD63 (6.3% ± 2.1% vs 3.2% ± 1.6%), TXA2 (548 ± 85 ng/L vs 390 ± 67 ng/L), platelet aggregation rate (43.2% ± 10.7% vs 34.8% ± 8.1%), thrombosis length in vitro (2.3 ± 0.6 cm vs 1.8 ± 0.3 cm), CD54 in blood (26.9% ± 6.9% vs 14.4% ± 5.1%), CD54 in tissues (51.1% ± 6.2% vs 23.1% ± 4.1%), Pgp-170 in blood (18.9% ± 3.9% vs 10.4% ± 2.7%), Pgp-170 in tissues (16.5% ± 3.2% vs 10.2% ± 2.3%, P < 0.01 or 0.05).
CONCLUSION: Based on the characteristics of UC cases in China, different therapy should be given to different types of UC with expected satisfactory results.
INTRODUCTION
Ulcerative colitis (UC) is a common digestive disease in Western countries. It was believed that the occurrence of UC was rare in China. But recent reports reveal that UC cases have increased remarkably[1,2]. According to our study, UC cases from 1991 to 2000 have increased 2.7 times compared with those from 1981 to 1990[3-5]. Due to the fact that the etiology and mechanism of UC are still not quite clear, and there is no specific treatment available, the disease usually becomes chronic with repeated relapses, thus seriously endangering patient’s health[6-25]. SASP and corticosteriod, despite their widespread use in the treatment of UC, do not offer an ideal cure because of its long course of treatment, various adverse reactions as well as tendency to relapse when medication stops. The emphasis laid on the study of UC, therefore, is to find an effective drug with fewer adverse reactions in accord with the characteristics of UC cases in China. The diagnosis and treatment of UC still remain a challenge to clinicians[26-34]. Respecting treatment and improvement of curative effect in refractory cases, lower of relapse rate and reduction of side effects of aminosalicylic acid and corticosteroids are questions to be encountered. Based upon the characteristics of UC cases in China, we adopted the method of giving different therapy to different types of UC, hoping to get better therapeutic results.
MATERIALS AND METHODS
Total cases
A total of 102 UC patients (42 chronic relapse type, 42 first episode type, 18 refractory type) were studied, their diagnoses conformed to the criteria of Lennard-Jones[28].
Chronic relapse type
Among the 42 chronic relapse type cases, 19 were males and 23 females with an average age of 32.6 years. They had a UC history of 6 mo to 5 years and bloody diarrhea, abdominal pain of varying degrees. Pathological changes above the sigmoid were found in 12 and 30 patients by colonoscopic examinations, respectively. Lesions were characterized by ulcerations, crypt abscesses, non-specific inflammation and atypical hyperplasia, etc. They were randomly divided into treatment group which received olsalazine sodium capsules (Tianjin Lisheng Pharmaceutical Co., Ltd. 250 mg) were used twice a day (1.0 g/d) for 8 wk, and comparison group received sulfasalazine (1.0) 4 times a day for 8 wk. There was no significant difference in the severity of symptoms between olsalazine group (11 mild, 8 moderate, 2 severe) and SASP group (13 mild, 7 moderate, 1 severe, Ridit analysis, P > 0.05). For patients who could not tolerate diarrhea of 2-3 times a day, 1-2 bills of imodium were given daily, but not more than 10 d. Patients were seen before and after 1, 2, 4, 6, 8 wk of treatment. Symptoms and physical signs were recorded. Colonoscopy was done 3 d before treatment and within 3 d after completion of treatment. A total of 7 items were observed and recorded. Purulent secretion and pseudopolyp were classified into 2 grades. Ulcer, erosion, mucous bleeding, hyperemic edema and vascular bluring were classified into grades 0, 1, 2, 3, 4 based upon the severity (0 = nil, 1 = mild, 2 = moderate, 3 = relative severe, 4 = severe). Routine blood and stool tests were performed before and after 1, 2, 4, 6 and 8 wk of treatment. Coagulation time and erythrocyte sedimentation rate were examined before and after 4 and 8 wk of treatment. Blood serum potassium, sodium, chloride, anhydride, urea nitrogen, ALT and total bilirubin were examined before and after 8 wk of treatment. Histological examination with grading of its changes was performed on colonoscopic biopsy specimens before and after treatment (grade 0: no polymorphonuclear cell, grade 1: some polymorphonuclear cells in lamina propria, grade 2: obvious polymorphonuclear cells infiltration in lamina propria involving more than 50% of recesses, grade 3: massive polymorphonuclear cells with recess abscess, grade 4: obvious acute inflammation with ulcer). Criteria of therapeutic efficacy were adopted that proposed by Chinese Society of Gastroenterology[35] (complete remission: subsidence of clinical symptoms with relative normal mucous membrane in colonoscopy, effective: basically without symptoms and mild mucousal inflammatory reaction or pseudopolyp formation upon colonoscopy, ineffective: no improvement in clinical symptoms, colonoscopic and pathologic examinations). Complete clinical remission: after 8 wk treatment, defecation 0-2 times a day, with no gross blood or microscopic red cells in stool; partial remission: after 8 wk of treatment, defecation 3-4 times a day, with no gross blood in stool but less than 10 RBC per high power microscopic field; no improvement: defecation 5 times or more per day with gross bloody stool. Colonoscopic remission: complete remission(among the 7 items, 5 or more lowered by a grade after treatment), partial remission (3-4 items lowered by a grade after treatment), no remission (0-2 items lowered by a grade after treatment). Histological remission: complete remission (pathological grade lowered after treatment, being grades 0-1), partial remission (pathological grade lowered after treatment, but still > 1), no remission (no change before and after treatment). Adverse reactions record: nausea, diarrhea, insomnia, abdominal pain, dizziness, rash, lumbar soreness, edema, etc. Their time of occurrence, severity, duration and measures taken for treatment were recorded.
First episode type
Among the 42 cases of first episode type, 16 were males and 26 females with average age of 31.4 years. They had a UC history of 1 mo to a year, and all had bloody diarrhea, abdominal pain of different degrees. Lesions above the sigmoid were found in 2 patients by colonoscopic examination, while pathological changes were found below the sigmoid in 40 patients. Lesions were characterized by ulceration, crypt abscesses, non-specific inflammation and atypical hyperplasia, etc. They were randomly divided into treatment group that received treatment of heartleaf houttuynia (2 kg/L, pH4.0-6.0, Nanfang pharmaceutical Co., Ltd.) enema (20 mL diluted with NS 100 mL, once every evening before sleep for 1-2 mo), and SASP group that administered 1 g of SASP four times a day for 1-2 mo. Clinical observations included frequency of defecation, bloody stool, and general condition. Theraputic effects[28]: complete remission (complete disappearance of symptoms with mucous membrane returned to normal in colonoscopy), partial remission (abatement of symptoms with conditions of mucous membrane improved, only a small amount of red blood cells and leucocytes found in routine stool test), no remission(no obvious changes both in symptoms and in colonoscopy). Ultrastructure[7] Microvilli, mitochondria and apoptosis were observed under electronic microscopy. Content of CD54 (ICAM-1, Immunotech) in colonic mucous membrane was examined according to our methods[15].
PC Polygraph HR (CTD-SYNECTICS, Sweden) was used to examine colonic motility. Distances between the 8 tracts (outer diameter 8 mm and side hole diameter 1 mm) of manometric tube were 5 cm, medication that would affect gastrointestinal motility was suspended at least for 3 d before the examination. Intestinal tract was cleaned in the afternoon prior to the examination and food intake was suspended during the day of examination. Manometric tube was inserted to colonic splenic flexure as guided by colonoscopy. Colonic motility of each patient was recorded one hour before meal and two hours after meal, the result was then analyzed by Polygram and Windows Polygram. Contractions above 6.67 kPa and spreading to side holes 10 cm away were regarded as propulsive contractions, while contractions below 1.33 kPa were not considered so as to minimize the effect of respiration. Baseline was automatically set up by computer, which calculated the mean oscillation amplitude every 30 min before and after meals. Hand injectors were used to fill air of 20 mL each time to the self-made rubber air pocket with the maximum capacity of 120 mL at 30 s intervals. Patients’ feeling of expansion of air pocket was recorded(cognitive, defecation and pain threshold values).
Refractory UC patients with platelet activation
Among the 18 refractory UC patients, there were 8 males and 10 females aged 20 to 52 years (mean 32.4 years), including 10 cases of severe UC, and 8 moderately severe UC. Duration of diseases ranged from 7 mo to 10 years (mean 4.3 years). Rectal bleeding, diarrhea, mucus stool, abdominal pain were the main symptoms. Three patients were associated with thromboembolic diseases. All patients were treated with high-dose corticosteroid and sulfasalazine for more than 4 wk without effect, sulfasalazine was maintained in combination with Kangshuanling sublingual tablet (low molecular heparin, produced by Shandong Songling Pharmaceutic Factory, 2 tablets, 3 times daily (7200 U/d) for 15 d, then 1 tablet, 3 times daily (3600 U/d) for more than 4 wk). Prednisolone was tapered and stopped.
Pre- and post-treatment scores were calculated for the following disease parameters[36]: (1) Stool frequency (average number per day for the past week); (2) Rectal bleeding (0: absent, 1: streak of blood on stools occationally, 2: obvious blood on stool frequently, 3: complete bloody stools); (3) Colonoscopic appearance 0: normal vascular pattern, 1: mild lesion (loss of vascular pattern, mucosal edema, no bleeding), 2: moderate lesion (granularity and friability of the mucosa), 3: severe lesion (discrete ulceration and spontancous bleeding); (4) Histological grading: serial biopsies from rectum and colon were taken. Five histological changes seen in UC (cellular infiltrate in lamina propria, cryptitis, crypt abscess formation, goblet cell depletion, and regenerative hyperplasia of epithelium). Each was scored from 0 (absent) to 3 (severe). A total UC score of 5 or less indicated mild disease; 5-10, moderate; and 10-15, severe disease. And (5) General health status (0: excellent, 1: good, 2: poor, 3: poorer, 4: very poor, 5: poorest).
To assess platelet activation and aggregability[22,37], we used a sensitive flow cytometric technic designed to render minimize sample handling and render fixation unnecessary to quantify platelet activation. Blood samples were incubated 10 min before venesection with fluorescein isothiocyanate (FITC) conjugated antibodies to the platelet surface antigens, P-selectin (CD62P) and CD63 (Immunotech, Marseilles, France). Analysis was made 15 min before venesection using a BD (Becton Dickinson Immonocytometry Systems) FAC scan. TXA-2 (Suzhou Medical College) was measured using RIA method, samples were taken without tourniquet into chilled tubes containing 1:9 anticoagulant/antiaggregant solution (trisodium cirrate 3.8%), centrifuged for 15-30 min, later at 4 °C for 30 min to minimize in vitro activation, supernatant was decanted off and stored at -20 °C for assay within 3 mo. Platelet aggregation rates (PAR) and thrombosis length (TL) in vitro were assessed by XSN-RII instrument according to the manufecturer’s instructions. CD54 and Pgp-170 in blood and tissues were measured using flow cytometric technique according to our previous report[15] and literature[38,39].
Statistical analysis
T test and Ridit analysis were adopted. Student’s t test and Friedman test were used to assess the significance of differences between mean pre- and post-treatment parameters.
RESULTS
Chronic relapse type UC
In the 42 chronic relapse type UC patients, the total clinical effect of olsalazine sodium group (completely remission in 16 cases, improvement in 4 patients, inefficiency in one case) was better than that of SASP group (completely remission in 10 cases, improvement in 4, inefficiency in 7, P < 0.05). The clinical symptomatic remission of olsalazine sodium group (complete remission in 15 cases, partial in 5, inefficiency in one) was better than that of SASP group (complete remission in 10 cases, partial in 5, inefficiency in 6, P < 0.05). The colonoscopic remission of olsalazine sodium group (complete remission in 11 cases, partial in 9, inefficiency in 1) was better than that of SASP group (complete remission in 7 cases, partial in 8, inefficiency in 6, P < 0.05). The colonoscopic images of pre and post treatment with olsalazine are shown in Figure 1. The histologic remission of olsalazine sodium group (complete remission in 13 cases, partial in 7, inefficiency in 1) was better than that of SASP group (complete remission in 6 cases, partial in 10, inefficiency in 5, P < 0.05). The side effects of gastrointestinal tract in olsalazine sodium group were less than those of SASP group (abdominal discomfort: 3 vs 15, heartburn 1 vs 7, nausea 2 vs 5) except for frequency of watery diarrhea (5 vs 1). No other side effects were observed in olsalazine sodium group while increased ALT (1 case), decreased WBC (1 case) and skin eruption (2 cases) were observed in SASP group. Two patients relapsed in olsalazine sodium group while 8 cases relapsed in SASP group during the flow-up period (from 6 mo to 1 year).
Figure 1.
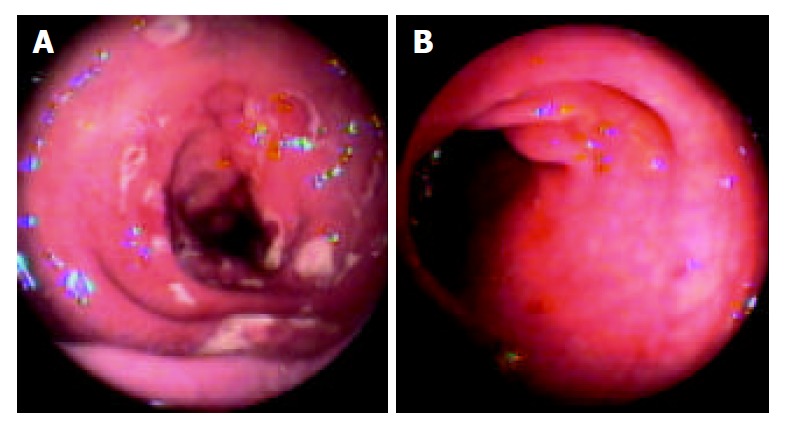
Colonoscopic image before and after treatment of osalazine. A: Colonoscopic image before treatment of osalazine; B: Colonoscopic image after treatment of osalazine for 4 wk.
First episode type UC
In the 42 first episode type UC patients, the clinical effect of Heartleaf houttuynia herb group (complete remission in 20 cases, 95.2%; improvement in 1 case, 4.8%) was better than that of SASP group (complete remission in 15 cases, 72.4%; improvement in 5 cases, 23.8%; inefficiency in 1 case, 3.8%, P < 0.01). The time of stool frequency recovering to normal (5.6 ± 3.3 d), blood stool disappearance time (6.7 ± 3.8 d) and abdominal pain disappearance time (6.1 ± 3.5 d) in Heartleaf houttuynia herb group were all shorter than those in SASP group (9.5 ± 4.9 d, 11.7 ± 6.1 d, 10.6 ± 5.3 d, P < 0.01). Pathological changes of ultrastructure, such as swollen mitochondria with depleted ridge, shortened microvilli, maldevelopment of goblet cells and increased epithelial cell apoptosis (Figure 2) could be found on the surface of mucous membrane and recess prior to Heartleaf houttuynia herb injection treatment, which recovered to normal gradually after treatment (Figure 3).
Figure 2.
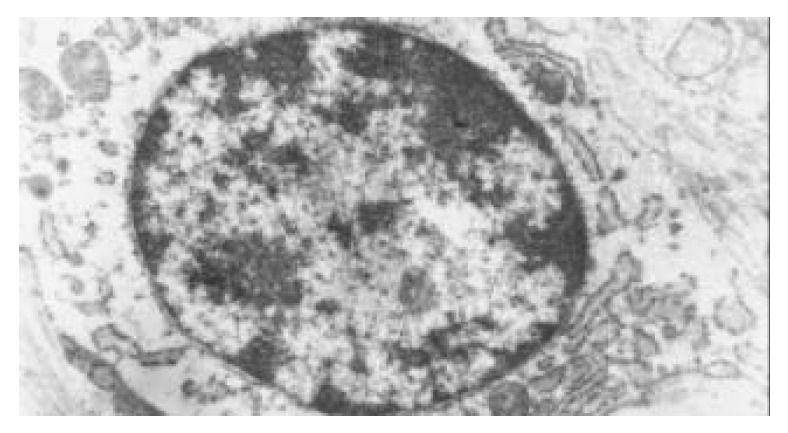
Epithelial cell apoptosis and swollen mitochondria with depleted ridge in UC patients.
Figure 3.
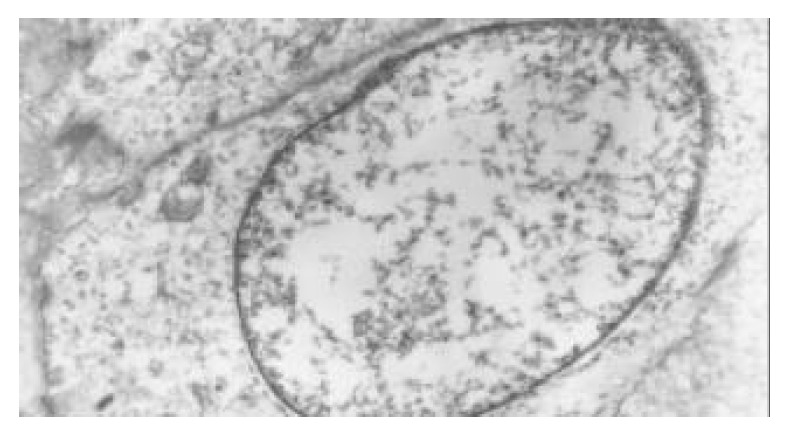
Gradual recovery of epithelial cells to normal after treatment with Heartleaf houttuynia herb injection.
Heartleaf houttuynia herb could inhibit the expression of CD54 (ICAM-1) of colonic mucous membrane (45.8 ± 5.7 vs 30.7% ± 4.1%, P < 0.05, Figure 4).
Figure 4.
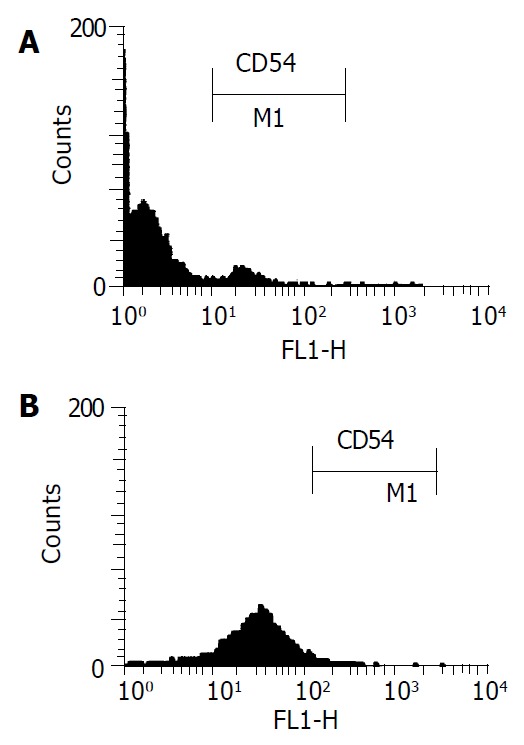
Expression of CD54 (ICAM-1) in colonic mucous membrane of UC patients before and after treatment of Heartleaf houttuynia herb. A: Increased expression of CD54 in colonic mucous membrane of UC patients before treatment of Heartleaf houttuynia herb; B: Decreased expression of CD54 in colonic mucous membrane of UC patients after treatment of Heartleaf houttuynia herb.
Compared with normal persons, the mean promotive speed of contraction wave stepped up (4.6 ± 1.6 cm/min vs 3.2 ± 1.8 cm/min, P < 0.05) and the mean amplitude of wave decreased (14.2 ± 9.3 kPa vs 18.4 ± 8.0 kPa, P < 0.05) in active UC patients. After treatment of Heartleaf houttuynia herb, these 2 indexes improved significantly (17.3 ± 8.3 kPa, 3.7 ± 1.7 cm/min, P < 0.05). In normal persons, the post-meal pressure of sigmoid (2.9 ± 0.9 kPa) was higher than that of descending colon (2.0 ± 0.7 kPa) and splenic flexure (1.7 ± 0.6 kPa), while the respective colonic pressures (1.5 ± 0.5 kPa, 1.4 ± 0.6 kPa, 1.3 ± 0.6 kPa) were significantly decreased (P < 0.05) in active UC patients. After treatment of Heartleaf houttuynia herb, the colonic pressures (2.6 ± 0.8 kPa, 1.8 ± 0.6 kPa, 1.6 ± 0.5 kPa) recovered to normal.
The pain threshold of distant colon (67.3 ± 18.9 mL) in active UC patients decreased significantly compared with that in normal persons (216.2 ± 40.8 mL, P < 0.05) and recovered to normal after treatment of Heartleaf houttuynia herb (187.4 ± 27.2 mL, P < 0.05. There were no adverse reactions in Heartleaf houttuynia herb therapy, while SASP therapy had adverse reactions such as heartburn (5 cases), increased ALT (1 case), decreased WBC (1case) and rash (2 cases).
Refractory UC patients with platelet activation
Sixteen patients achieved clinical remission (normal stool frequency and no rectal bleeding) after combined treatment of Kangshuanling sublingual tablets with sulfasalazine. Two patients had reduced rectal bleeding only. The average time of marked improvement and remission was 3 wk (1-5 wk), and 6 wk ( 1-12 wk), respectively. Rectal bleeding ceased in 16 patients (4 patients within 7-14 d, the others within 2-6 wk). Sixteen patients improved in general health condition earlier than bowel symptoms. There was highly significant improvement in mean scores for all disease parameters (Table 1).
Table 1.
Therapeutic effects of Kangshuanling sublingual tablets on refractory UC patients
| Group | Stool frequency (times/d) | Rectal bleeding (score) | Colonoscopy (score) | Histology (score) | Well-being (score) |
| Pre-treatment | 8.2 | 2.7 | 2.6 | 12.0 | 3.9 |
| Post-treatment | 1.6b | 0.3b | 1.1b | 5.0b | 0.7b |
P < 0.01 vs pretreatment.
Blood contents of CD62p, CD63, TXA2, platelet aggregation rate (PAR) and thrombosis length (TL) in vitro
All the indexes in refractory UC patients increased significantly as compared with the normal controls (P < 0.01). After treatment with Kangshuanling sublingual tablets, all the parameters of UC patients decreased (P < 0.05, but CD62P and CD63 remained higher than normal (P < 0.05, Table 2, Figure 5).
Table 2.
Effects of Kangshuanling sublingual tablet on CD62P and CD63, TXA2, platelet aggregation rate (PAR) and thrombosis length (TL) in vitro in UC patients (mean ± SD)
| Group | CD62p (%) | CD63 (%) | TXA2 (ng/L) | PAR (%) | TL (cm) |
| UC patients | |||||
| Pre-treatment | 8.0 ± 3.1b | 6.3 ± 2.1b | 548.2 ± 84.9b | 43.2 ± 10.1b | 2.3 ± 0.6b |
| Post-treatment | 4.1 ± 1.8a,d | 3.2 ± 1.6a,d | 390.1 ± 67.0d | 34.8 ± 8.1d | 1.8 ± 0.3d |
| Normal controls | 1.9 ± 0.4 | 1.6 ± 0.8 | 340.2 ± 40.4 | 34.1 ± 9.1 | 1.7 ± 0.4 |
P < 0.05,
P < 0.01 vs normal controls;
P < 0.01 vs pretreatment.
Figure 5.
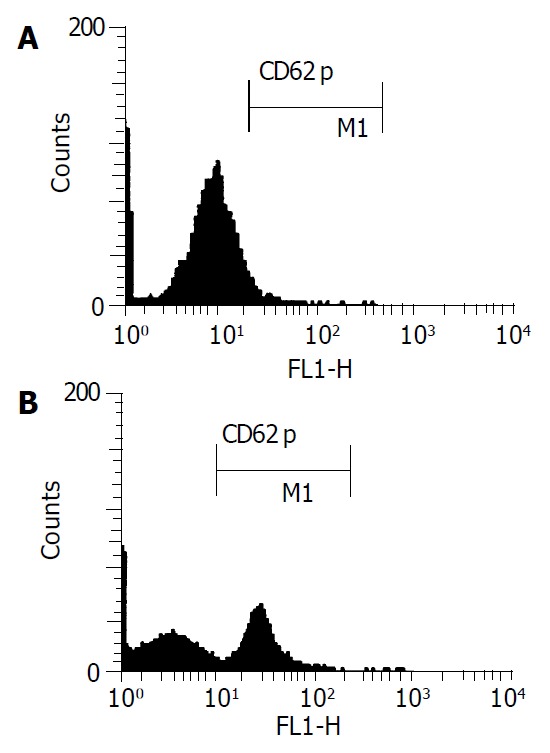
CD62p in blood of normal persons and active UC patients. A: CD62p in blood of normal persons; B: Significant increase of CD62p in blood of active UC patients.
CD54 and products of MDR expression (Pgp-170) in blood and tissues
Compared with normal persons (Figure 6A), CD54 elevated in both blood and tissues in refractory UC patients (P < 0.01), CD54 in tissues was higher than in blood (Figure 6B). After treatment with Kangshuanling sublingual tablets, CD54 was significantly decreased in both blood and tissues (P < 0.01), but still higher than that in normal controls (P < 0.05), (Table 3). Compared with normal persons (Figure 6C), Pgp-170 elevated in both blood and tissues in refractory UC patients (P < 0.01, Figure 6D), there was no difference between Pgp-170 in tissues and blood. After treatment with Kangshuanling sublingual tablets, Pgp-170 was significantly decreased in both blood and tissues (P < 0.05), but still higher than that of normal controls (P < 0.05), (Table 3).
Figure 6.
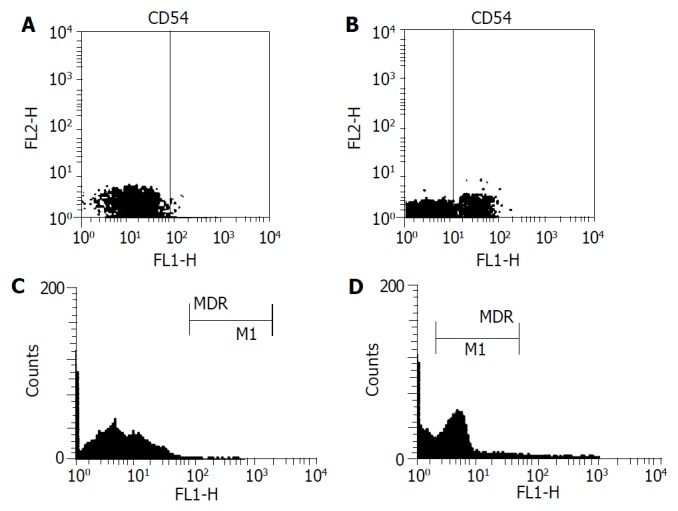
CD54 and MDR in tissues of normal persons and refrectory UC patients. A: CD54 in tissues of normal persons; B: Significant increase of CD54 in tissues of refrectory UC patients; C: MDR in tissues of normal persons; D: Significant increase of MDR in tissues of refrectory UC patients.
Table 3.
Effects of Kangshuanling sublingual tablets on CD54 in UC patients (mean ± SD, %)
| Group | Blood CD54 | Tissue CD54 | Blood Pgp-170 | Tissue Pgp-170 |
| UC patients | ||||
| Pre-treatment | 26.9 ± 6.9b | 51.1 ± 6.2b | 18.9 ± 3.9b | 16.5 ± 3.2b |
| Post-treatment | 14.4 ± 5.1a,d | 23.1 ± 4.1a,d | 10.4 ± 2.7a,c | 10.2 ± 2.3a,c |
| Normal controls | 6.2 ± 3.7 | 8.8 ± 3.2 | 6.2 ± 2.2 | 6.8 ± 3.1 |
P < 0.05,
P < 0.01 vs normal controls;
P < 0.05 vs pre-treatment,
P < 0.01 vs pre-treatment.
Complications
No complications were found during the treatment with Kangshuanling sublingual tablets.
DISCUSSION
SASP is still widely used in the treatment of chronic relapse type ulcerative colitis, with advantages such as quick effect and high clinical remission rate. However, its effect is not satisfactory in some chronic cases and has various adverse reactions. In addition, UC usually relapses when medication is stopped. Therefore, we should place emphasis in the study of UC on more effective drugs with less adverse reactions[2,27-31]. At present, the cause and pathogenesis of UC are unclear[1-15], nonspecific anti-inflammatory drugs, in a relatively long period, will still remain as the main drugs for treating UC. While the curative effect of traditional aminosalicylic acid has been affirmed, its side reactions are too many. Main approaches today centered on enhancing the curative effect and reducing side reactions by developing new preparations and changing routes of administration[1]. SASP, when taken orally, is cleaved by bacteria in the colon into 5-ASA and Sulfapyridine. The former is the effective component of SASP, and the latter is the carrier of 5-ASA, which may cause such side reactions as sulfanilamide allergy, gastrointestinal upset, hepatorenal impairment, thus affecting its clinical application. In the present study, the above mentioned side reactions in various degrees were also seen in the SASP group. Therefore, to achieve a satisfactory curative effect but without toxicity, the best therapy for UC is to administer 5-ASA that does not contain sulfapyridine and to make it working on diseased areas directly. 5-ASA, however, is usually absorbed rapidly, hence unable to reach inflamed mucous membrane. So, the question posed for the development of new drugs for UC, is how to make 5-ASA reaching and working on the diseased area. Olsalazine sodium gives an answer to this problem, for it is the prodrug of 5-ASA, formed by 2-molecules of 5-ASA jointed by diazo bond. When it is taken orally, only a very small amount is absorbed before reaching colon (absorbing rate < 5%). It does not decompose and its biological utilization rate in the body is extremely low. When it reaches the colon, bacterial enzymes in the colon split the diazo bond, liberating the two-molecules of 5-ASA. It has no side effects of SASA, while maintaining the same curative effects. Olsalazine sodium has been on market for more than 10 years and its curative effect on UC and safety have been widely accepted. Domestic olsalazine sodium is a fourth grade new drug jointly developed by Tianjin Lisheng Pharmaceutical Co., Ltd. and Tianjing Medical Research Institute. The fourth grade new drug with the trade name “Changmei”, in capsule form was put into market in 2000. This study centered on the clinical effects and safety of olsalazine sodium in patients with chronic UC. Our results indicated that olsalazine sodium was superior to SASP in overall clinical response rate, amelioration of clinical symptoms, colonoscopic examination and histology test. In addition, it has fewer side effects on digestive tract and is unharmful to liver function, WBC and skin. The cause of the increased watery stool frequencies may be related with sodium salt, which inhibits intestinal absorption of water. It mainly occurs at the beginning of medication or during increase of dosage. This side effect, however, does not affect the continuing medication. Patients’ worries may be eliminated when the cause is explained. To increase medication frequencies or to take medicine after meal may ameliorate or eliminate this symptom. Imodium may also be given temporarily to some patients to maintain curative effect. In China, the chronic relapse type accounted for 52.6% of all UC cases[3], maintenance treatment may lower relapse rate. In summary, this study shows that the curative effect and safty of domestic olsalazine sodium is superior to SASP in the treatment of chronic UC. It boosts remission rate, lowers relapse rate and causes fewer side effect, especially applicable to patients who are irresponsive or allergic to SASP therapy.
According to our statistics, the first episode type accounted for 34.8% of all ulcerative colitis cases in China[3]. The disease mostly starts in rectum and sigmoid colon. When Heartleaf houttuynia enema is used, it can work on diseased areas directly. In this way, it not only can avoid the effects of pH and enzyme on the medicine, but also can make the herb absorbed completely and prolong the time of drug action. Then, colonic mucous membrane will recover gradually to normal with healing of the ulcers. Volatile oil extract of fresh Heartleaf houttuynia is used to produce Heartleaf houttuynia injection. Its utility components (Houttuynin, lauraldehyde, quercitrin, isoquercitrin, etc.) are higher than that of Heartleaf houttuynia herb with widespread pharmacological actions. For instance, relaxation of intestinal smooth muscle could relieve enterospasm, prolong the retention time of intestinal contents, alleviate and eliminate the symptoms of diarrhea and abdominal pain[8,24,25]. Quercitrin and isoquercitrin can ameliorate capillary fragility for haemostasis, which lead to the stoppage of bloody stool. Pathological changes, such as swollen mitochondria with depleted ridge, shortened microvilli, maldevelopment of goblet cells and increased epithelial cell apoptosis could be found on the surface of mucous membrane and recess prior to Heartleaf houttuynia herb injection treatment. All these results in malabsorption of water with symptoms of diarrhea, while the increase of epithelial cell apoptosis can lead to the formation of ulcer due to damage of the colonic mucous membrane barrier. The expression of CD54 can further promote the inflammatory reaction. After treatment with Heartleaf houttuynia herb injection, epithelial cell apoptosis[11], swollen mitochondria, shortened microvilli and the expression of CD54 could recover to normal gradually, which led to plerosis of colonic mucous membrane and healing of ulcer, the effect was superior to that of SASP. Heartleaf houttuynia herb is not only a medicine, but also a safe edible plant. The pH and osmotic pressure of the injection are close to those of intrinsic human environment, so there are no adverse reactions in Heartleaf houttuynia herb therapy, while SASP therapy may have side effects such as the heartburn, increased ALT, decrease WBC and rash.
UC patients often have symptoms of diarrhea, abdominal pain and tenesmus. Are these symptoms related to colonic motility disturbance? In this study, compared with the normal persons, the mean promotive speed of contraction wave stepped up and the mean amplitude of wave decreased in active UC patients, which led to diarrhea. The gastrocolic hyperreflex resulted in awareness of defecation and abdominal pain after eating that could be relieved after defecation. These two indexes improved significantly after treatment with Heartleaf houttuynia herb (P < 0.05). In normal persons, the postprandial pressure of sigmoid was higher than that of descending colon and splenic flexure, the pressure gradiant and segmental construction made the colonic contents mixed and milled to expose to the colonic mucous membrane fully. Reabsorption of water and electrolytes were thus promoted. In active UC patients, the colonic pressure was significantly decreased (P < 0.05), and there was no pressure gradient in different colonic loci which could lead to disturbance of reabsorption of water and electrolytes. Diarrhea occurred due to the decrease of segmental construction and also inflammation of colonic mucosa occurred. The pain threshold of distant colon in active UC patients decreased significantly compared with that of normal persons, indicating that the distant colonic sensibitity was increased. So, a small amount of intestinal contents could stimulate defecation reflex, leading to symptoms of diarrhea[23], abdominal pain and tenesmus. After treatment with Heartleaf houttuynia herb, the colonic pressure and pain threshold recovered to normal due to the following reasons. Heartleaf houttuynia caused relaxation of intestinal smooth muscle which could relieve the enterospasm, prolong the retention time of intestinal contents, alleviate and eliminate the symptoms of diarrhea and abdominal pain. Our prophase study proved that Heartleaf houttuynia herb could improve the colonic motility disturbance of UC rats. In this study, the remission of diarrhea and abdominal pain might be partly related to this. Heartleaf houttuynia herb also has anti-inflammatory actions as we have proven in our previous animal study, which led to the remission of symptoms.
The main component of Kangshuangling sublingual tablets is low molecular mass (molecular mass ranged from 5-15 ku, peak ranged from 5-8 ku) heparin substance. Each tablet contains 1 200IU LMWH, which can be absorbed by the sublingual mucosa, so it not only has no first-pass effects by the liver compared with oral LMWH used in our previous study[29], but also has no inconvenience of injection. Heparin, a group of sulphated glycosaminoglycans, in addition to its physiological effects and anticoagulant, antithromboembolic, antiallergic, antiviral, antiendotoxic and immunoregulative biological activities, has been found with a wide range of potentially anti-inflammatory effects, including inhibition of neutrophil elastase and inactivation of chemokines[40]. Compared with heparin, LMWH has higher antithromboembolic effects, longer half life period, less bleeding tendency, higher bioavailability, easier absorption by sublingual administration, as well as anti inflammatory effects[29,41]. Previous reports[29] on improvement of UC patients treated with heparin prompted us to perform a pilot study of Kangshuangling sublingual tablets to find a more convenient and effective drug for patients with refractory UC. The observed response to Kangshuangling sublingual tablets was paradoxical. Sixteen of 18 patients with refractory UC unresponsive to high-dose prednisolone and sulfasalazine therapy for more than 4 wk achieved clinical remission and became asymptomatic after treatment of Kangshuangling sublingual tablets in combination with sulfasalazine. Contrary to the traditional idea that heparin could enhance bleeding, rectal bleeding was the first symptom to be improved by Kangshuangling sublingual tablets. The results were similar to other reports of heparin treatment[42,43].
If Kangshuangling sublingual tablets have a therapeutic effect on UC, their mechanism of action should shed some lights on the elusive pathogenesis of this disease. Several thrombophilic features of UC that suggest the effect of Kangshuangling sublingual tablets on colitic symptoms may be attributable to their anticoagulant and antithrombotic properties. Evidences of a thrombotic process in UC included: reports of a hypercoagulable state[20,22], an increased incidence of thromboembolic event[44], and ischemic complications such as toxic megacolon and pyoderma gangrenosum. In this study, the membrane marks of platelet activity CD62p and CD63 were increased significantly, and the derivative of active platelet TXA2 was also elevated, suggesting that blood platelet TXA2 was in an active state, which not only led to a hypercoagulable state and an increased incidence of thromboembolic events, but also enhanced inflammatory reaction[20,22]. Activated hyperaggregable platelets in the mesenteric circulation could amplify the inflammatory cascade by promoting neutrophil recruitment and chemotaxis. P-selectin has an established action as the adhesion molecule for neutrophils, and circulating platelet aggregates may contribute to ischemic damage and infarction by occluding the intestinal microvasculature. Platelets derived thromboxane A2 may also contribute to ischemia by inducing local vasoconstriction. After treatment with Kangshuangling sublingual tablets, all these parameters dropped markedly, suggesting that the therapeutic effect of LMWH was partly related to inhibition of platelet activity, and improvement of hypercoagulable state, leding to the remission of clinical symptoms. But the membrane marks of platelet CD62p and CD63 were still higher than those of the normal controls. Whether it has predictive value for recurrence or prognosis should be further studied.
CD54 antigen could react with 85-110 ku integral membrane glycoprotein, and it is also known as an intercellular adhesion molecule-1 (ICAM-1) expressed on endothelial cells and both resting (weak) and activated (moderate) lymphocytes and monocytes[15]. CD54 is ligand for the leukocyte function antigen-1 (CD11a). Its expression was up-regulated upon stimulation by inflammatory mediators such as cytokines and LPS, and it was involved in B cell-T cell co-stimulatory interactions. In this study, CD54 elevated significantly in blood and tissues of UC patients, being higher in tissues than in blood. Therefore, it could reflect the inflammation of intestinal mucosa. After treatment with Kangshuangling sublingual tablets, CD54 dropped significantly in both blood and tissues, indicating that Kangshuangling sublingual tablets could relieve the inflammatory activity in refractory UC patients who received high-dose prednisolone and sulfasalazine therapy for a long period (more than 4 wk) without significant improvement and were regarded as corticosteroid-resistant refractory cases of UC. It was reported that heparin could also inhibit c-reactive protein (CRP), tumor necrosis factor (TNF) and L-selectin of UC patients. The detailed mechanisms by which anti-inflammatory properties of oral L MWH are mediated in UC remain to be elucidated further.
The multidrug resistance (MDR) gene coding for a drug efflux pump P-glycoprotein 170(Pgp-170) expressed on the surface of lymphocytes and intestinal epithelial cells[38,39]. In this study, Pgp-170 was elevated significantly in blood and tissues of refractory UC patients. Poor response to medical therapy of certain UC patients might be related to MDR expression because glucocorticoids are known Pgp-170 substrates. There was no difference of Pgp-170 in tissues and blood, indicating that peripheral blood lymphocyte (PBL) MDR remained stable over time and was not influenced by disease activity or glucocorticoid therapy, both PBL and mucosal MDR expression appeared independent of disease activity, and there was a significant correlation between PBL and MDR expression and intestinal epithelial lymphocyte and epithelial cell expression[38,39]. After treatment with Kangshuangling sublingual tablets, Pgp-170 dropped significantly in both blood and tissues, indicating that Kangshuangling sublingual tablet could inhibit the expression of MDR, but Pgp-170 was still higher than that of the normal controls, indicating that PBL and mucosal MDR may play an important role in determining the response of refractory UC patients to glucocorticoid therapy. From these results, we conclude that Kangshuanling sublingual tablets may play a role in treating refractory UC with activated platelets, the mechanism is partly related to the inhibition of platelet activity, hypercoagulable state, MDR expression, and its anti-inflammatory effects. No complications are found to be associated with the use of Kangshuanling sublingual tablets. It is still the focus of study in treating refractory UC with the Chinese features[3].
Footnotes
Supported by Youth Research Foundation of the Public Health Bureau of Shandong Province, No. 2001CA2EFB2
Edited by Wang XL Proofread by Xu FM
References
- 1.Jiang XL, Wang ZK, Qin CY. Current research and strategy on ulcerative colitis in China. Shijie Huaren Xiaohua Zazhi. 2000;8:610–613. [Google Scholar]
- 2.Jiang XL, Quan QZ, Liu T, Dong XC. Recent advances in re-search of ulcerative colitis. Shijie Huaren Xiaohua Zazhi. 2000;8:216–218. [Google Scholar]
- 3.Jiang XL, Cui HF. An analysis of 10218 ulcerative colitis cases in China. World J Gastroenterol. 2002;8:158–161. doi: 10.3748/wjg.v8.i1.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jiang XL, Cui HF. Features of ulcerative colitis cases in China: An analysis of 10218 cases. Shijie Huaren Xiaohua Zazhi. 2001;9:869–873. [Google Scholar]
- 5.Jiang XL. Strength the analysis of digestive diseases. Shijie Huaren Xiaohua Zazhi. 2001;9:864–868. [Google Scholar]
- 6.Jiang XL, Cui HF. A new chronic ulcerative colitis model produced by combined methods in rats. World J Gastroenterol. 2000;6:742–746. doi: 10.3748/wjg.v6.i5.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jiang XL, Quan QZ, Wang D, Sun ZQ, Wang YJ. A new ulcer-ative colitis model induced by compound method and the change of immune and ultrastructure. Shijie Huaren Xiaohua Zazhi. 1999;7:381. [Google Scholar]
- 8.Jiang XL, Quan QZ, Wang D, Sun ZQ, Wang YJ, Qi F. Experi-mental study of heartleaf houttuynia herb on ulcerative colitis. Shijie Huaren Xiaohua Zazhi. 1999;7:786. [Google Scholar]
- 9.Jiang XL, Quan QZ, Sun ZQ, Wang YJ, Qi F, Wang D, Zhang XL. Expression of lymphocyte apoptosis in patients with ul-cerative colitis. Shijie Huaren Xiaohua Zazhi. 1999;7:903–904. [Google Scholar]
- 10.Jiang XL, Quan QZ, Cheng GR, Sun ZQ, Wang YJ, Wang YP. Expression of apoptosis on biopsy tissue in patients with ul-cerative colitis. Shijie Huaren Xiaohua Zazhi. 2000;8:107–108. [Google Scholar]
- 11.Jiang XL, Pan BR, Ma JY, Ji ZH, Ma LS. Review for the 20th century and prospect for the 21st century of digestology. Shijie Huaren Xiaohua Zazhi. 2000;8:1161–1176. [Google Scholar]
- 12.Xu NZ. Expression of adhesion molecules in tissues and pe-ripheral lymphocyte of patients with ulcerative colitis. Huaren Xiaohua Zazhi. 1998;6(Suppl 7):54–55. [Google Scholar]
- 13.Jiang XL, Quan QZ, Sun ZQ, Wang YJ, Qi F, Wang D, Zhang XL. Detection of soluble CD44v6 in patients with inflamma-tory bowel disease. Shijie Huaren Xiaohua Zazhi. 1999;7:1028. [Google Scholar]
- 14.Jiang XL, Quan QZ, Chen GR, Sun ZQ, Wang YJ, Qi F, Wang D. Detection of CD44v6 on biopsy tissue can't differ ulcerative colitis from Chron's disease. Zhonghua Xiaohua Neijing Zazhi. 2000;19:298–299. [Google Scholar]
- 15.Jiang XL, Quan QZ, Chen GR, Yin GP, Sun ZQ, Wang YJ. Detec-tion of CD54, CD44 on biopsy tissues in patients with ulcerative colitis. Zhonghua Xiaohua Neijing Zazhi. 1998;15:292–294. [Google Scholar]
- 16.Jiang XL, Quan QZ, Sun ZQ, Wang YJ, Qi F, Yin GP, Sun XM. Detection of adhesion molecules in tissues and peripheral blood of patients with ulcerative colitis. Zhonghua Weishengwu He Mianyixue Zazhi. 1998;18:156. [Google Scholar]
- 17.Jiang XL, Quan QZ, Sun ZQ, Wang YJ, Qi F. Effect of glucocor-ticoid on lymphocyte adhesion molecule phenotype expression in patients with ulcerative colitis. Zhongguo Weizhongbing Jijiu Yixu. 1998;10:366–368. [Google Scholar]
- 18.Jiang XL, Quan QZ, Sun ZQ, Wang YJ, Qi F, Chen GR, Gao TS, Pan X. Detection of P-selectin and CD63 in peripheral blood of patients with serve ulcerative colitis. Zhongguo Weizhongbing Jijiu Yixue. 1998;10:174–175. [Google Scholar]
- 19.Jiang XL, Quan QZ, Sun ZQ, Wang YJ. Detection of P-selectin and CD63 in patients with ulcerative colitis. Shanghai Mianyixue Zazhi. 1998;18:230. [Google Scholar]
- 20.Jiang XL, Quan QZ, Liu TT, Wang YJ, Sun ZQ, Qi F, Ren HB, Zhang WL, Zhang L. Detection of blood platelet activation in patients with ulcerative colitis. Xin Xiaohuabingxue Zazhi. 1997;5:736. [Google Scholar]
- 21.Jiang XL, Quan QZ, Wang D, Sun ZQ, Wang YJ. One case report of ulcerative colitis accompanied with acute myocardial infarction. Shijie Huaren Xiaohua Zazhi. 1999;7:963. [Google Scholar]
- 22.Jiang XL, Quan QZ, Sun ZQ, Wang YJ, Qi F. Relationship between syndrome-typing of ulcerative colitis and activation of platelet. Zhongyi Zazhi. 1997;38:730–731. [Google Scholar]
- 23.Jiang XL, Quan QZ, Wang YJ, Sun ZQ, Wang D, Qi F. Measure-ment of rectual and annual motility in patients with ulcerative colitis. Zhonghua Xiaohua Neijing Zazhi. 2000;17:170–171. [Google Scholar]
- 24.Jiang XL, Quan QZ, Dong XC, Liu T. Effects of houttuynia herb on rectual and annual motility in patients with ulcerative colitis. Zhongyiyao Xubao. 2000;4:43–44. [Google Scholar]
- 25.Jiang XL, Quan QZ, Wang D, Sun ZQ, Wang YJ, Qi F. Effect of heartleaf houttuynia herb on colonic pressure in rats with ul-cerative colitis. Shijie Huaren Xiaohua Zazhi. 1999;7:639. [Google Scholar]
- 26.Zhang ZD, Chen J, Zhong YW, Zhang ST. Strength the diagno-sis and treatment of ulcerative colitis. Shijie Huaren Xiaohua Zazhi. 2003;11:1027–1028. [Google Scholar]
- 27.Jiang XL. Diagnosis and treatment of ulcerative colitis. Shijie HuarenXiaohua Zazhi. 2000;8:332. [Google Scholar]
- 28.Jiang XL, Quan QZ, Wang ZK. Diagnosis, typing and effect criteria of ulcerative colitis. Shijie Huaren Xiaohua Zazhi. 2000;8:332–334. [Google Scholar]
- 29.Cui HF, Jiang XL. Treatment of corticosteroid-resistant ulcerative colitis with oral low molecular weight heparin. World J Gastroenterol. 1999;5:448–450. doi: 10.3748/wjg.v5.i5.448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jiang XL, Qin CY, Li GQ. Special treatment for ulcerative colitis. Shijie Huaren Xiaohua Zazhi. 2000;8:341–342. [Google Scholar]
- 31.Jiang XL, Liu T. Treatment of refractory ulcerative colitis with heparin. Shijie Huaren Xiaohua Zazhi. 1999;7:694. [Google Scholar]
- 32.Jiang XL, Quan QZ, Sun ZQ, Wang YJ, Shang RL, Qi F. Clinical study on ulcerative colitis treated with Heartleaf houttuynia herb injection. Shijie Huaren Xiaohua Zazhi. 2003;11:1207–1210. [Google Scholar]
- 33.Jiang XL, Quan QZ, Sun ZQ, Wang YJ, Shang RL, Qi F. A control study on ulcerative colitis treated with olsalazine sodium. Shijie Huaren Xiaohua Zazhi. 2003;11:1211–1213. [Google Scholar]
- 34.Jiang XL, Quan QZ, Sun ZQ, Wang YJ, Shang RL, Qi F. Treat-ment of refractory ulcerative colitis with Kangshuangling. Shijie Huaren Xiaohua Zazhi. 2003;11:1214–1218. [Google Scholar]
- 35.Chinese Society of Gastroenterology. Suggestion on the di-agnosis and treatment of inflammatory bowel diseases. Zhonghua Neike Zazhi. 2001;40:138–141. [Google Scholar]
- 36.Gaffney PR, Doyle CT, Gaffney A, Hogan J, Hayes DP, Annis P. Paradoxical response to heparin in 10 patients with ulcerative colitis. Am J Gastroenterol. 1995;90:220–223. [PubMed] [Google Scholar]
- 37.Collins CE, Cahill MR, Newland AC, Rampton DS. Platelets circulate in an activated state in inflammatory bowel disease. Gastroenterology. 1994;106:840–845. doi: 10.1016/0016-5085(94)90741-2. [DOI] [PubMed] [Google Scholar]
- 38.Farrell RJ, Murphy A, Long A, Donnelly S, Cherikuri A, O'Toole D, Mahmud N, Keeling PW, Weir DG, Kelleher D. High multidrug resistance (P-glycoprotein 170) expression in inflammatory bowel disease patients who fail medical therapy. Gastroenterology. 2000;118:279–288. doi: 10.1016/s0016-5085(00)70210-1. [DOI] [PubMed] [Google Scholar]
- 39.Yacyshyn B, Maksymowych W, Bowen-Yacyshyn MB. Differences in P-glycoprotein-170 expression and activity between Crohn's disease and ulcerative colitis. Hum Immunol. 1999;60:677–687. doi: 10.1016/s0198-8859(99)00036-1. [DOI] [PubMed] [Google Scholar]
- 40.Tyrell DJ, Kilfeather S, Page CP. Therapeutic uses of heparin beyond its traditional role as an anticoagulant. Trends Pharmacol Sci. 1995;16:198–204. doi: 10.1016/s0165-6147(00)89022-7. [DOI] [PubMed] [Google Scholar]
- 41.Jiang XL, Cui HF, Wang YJ, Quan QZ, Sun ZQ. Effects of oral low molecular weight heparin on hemorrheology of rabbit liver damaged by D-galuctosamine. Xin Xiaohuabingxue Zazhi. 1997;5:355–356. [Google Scholar]
- 42.Folwaczny C, Fricke H, Endres S, Hartmann G, Jochum M, Loeschke K. Anti-inflammatory properties of unfractioned heparin in patients with highly active ulcerative colitis: a pilot study. Am J Gastroenterol. 1997;92:911–912. [PubMed] [Google Scholar]
- 43.Evans RC, Wong VS, Morris AI, Rhodes JM. Treatment of corticosteroid-resistant ulcerative colitis with heparin--a report of 16 cases. Aliment Pharmacol Ther. 1997;11:1037–1040. doi: 10.1046/j.1365-2036.1997.00252.x. [DOI] [PubMed] [Google Scholar]
- 44.Koenigs KP, McPhedran P, Spiro HM. Thrombosis in inflammatory bowel disease. J Clin Gastroenterol. 1987;9:627–631. [PubMed] [Google Scholar]


