Abstract
AIM: To investigate the influence of hepatic arterial blockage on blood perfusion of transplanted cancer in rat liver and the expression of vascular endothelial growth factor (VEGF) and matrix metalloproteinase-1 (MMP-1), and to explore the mechanisms involved in transarterial embolization (TAE)-induced metastasis of liver cancer preliminarily.
METHODS: Walker 256 carcinosarcoma was transplanted into rat liver to establish the liver cancer model. Hepatic arterial ligation (HAL) was used to block the hepatic arterial blood supply and simulate TAE. Blood perfusion of tumor in control, laparotomy control, and HAL group was analyzed by Hoechst 33342 labeling assay, the serum VEGF level was assayed by ELISA, the expression of VEGF and MMP-1 mRNA was detected by in situ hybridization.
RESULTS: Two days after HAL, the number of Hoechst 33342 labeled cells which represent the blood perfusion of tumor directly and hypoxia of tumor indirectly in HAL group decreased significantly compared with that in control group (329 ± 29 vs 384 ± 19, P < 0.01). The serum VEGF level in the HAL group increased significantly as against that of the control group (93 ng·L-1 ± 44 ng·L-1 vs 55 ng·L-1 ± 19 ng·L-1, P < 0.05). The expression of VEGF and MMP-1 mRNA in the tumor tissue of the HAL group increased significantly compared with that of the control and the laparotomy control groups (P < 0.05). The blood perfusion data of the tumor, represented by the number of Hoechst 33342 labeled cells, showed a good linear inverse correlation with the serum VEGF level (r = -0.606, P < 0.05) and the expression of VEGF mRNA in the tumor tissue (r = -0.338, P < 0.01).
CONCLUSION: Blockage of hepatic arterial blood supply results in decreased blood perfusion and increased expression of metastasis-associated genes VEGF and MMP-1 of transplanted liver cancer in rats. Decreased blood perfusion and hypoxia may be the major cause of up-regulated expression of VEGF.
INTRODUCTION
Primary liver cancer (PLC) is one of the most common cancers in Asia. Patients with PLC usually have very poor prognoses, and the overall 5-year survival rate was not more than 5% worldwide[1-3]. Surgery is considered as the only potential cure. However, the resection rate for PLC is only 10%-30%. Transarterial embolization (TAE) is one of the main non-surgical treatments for liver cancer in Asia via selectively blocking of the hepatic arterial blood supply of the tumor. However, a prospective controlled study showed that TAE enhanced the rate of lung metastases and accelerated metastases in patients with PLC[4]. Other reports also showed that preoperative TAE for resectable PLC or TAE after curative resection of PLC could result in introhepatic recurrence or extrahepatic metastasis, and a shorter survival[5,6]. Metastases induced by TAE will undoubtedly reduce the long-term efficacy of TAE for PLC, but the mechanisms responsible for that have not been previously reported and there is no good method to inhibit metastasis.
In the present study, we have observed the influence of hepatic arterial ligation (HAL) which simulate TAE on metastasis related genes expression in Walker 256 tumor transplanted in rat liver to explore the mechanisms involved in TAE-induced metastasis of liver cancer preliminarily.
MATERIALS AND METHODS
Tumor model and treatment schedule
An implanted liver cancer model was obtained from Shanghai Medical Industry Research Institute, China. Male pathogen-free Wistar rats, weighing 100-120 g, were anesthetized with pentobarbital sodium (40 mg/kg). Following midline laparotomy, Walker 256 carcinosarcoma (about 1 mm3) was implanted into one hepatic lobe of the rat. Seven days later, the rats that developed tumors were divided randomly into 3 groups:a control group without any treatment (n = 8), a laparotomy control group (n = 4) which underwent laparotomy only, and a HAL group (n = 8). In the HAL group, after anesthesia and laparotomy, the proper hepatic artery was ligated by a sewing line.
Staining of perfused vessels with Hoechst 33342
The perfusion marker Hoechst 33342 (Sigma, USA) was dissolved in sterile saline immediately before use. Two days after HAL, all rats from all three groups were anesthetized and then their abdominal cavity was opened. The inferior vena cava was punctured to collect 0.5 mL blood and to inject 0.2 mL Hoechst 33342 (at a concerntration of 6.25 g·L-1). The hepatic lobes bearing tumor were excised 1 min after injection of Hoechst 33342 to prevent diffusion of Hoechst 33342 into adjacent non-perfused vascular structures. Hoechst 33342 is removed very rapidly from the circulation (half-time of 2 min) and is very stable, once bound to DNA. Thus, Hoechst 33342 specifically labels the nuclei of endothelial cells and nuclei of the cells adjacent to the vessel walls, thereby delinealing the perfused vessels[7-9]. The tumors were excised and frozen in liquid nitrogen and then stored at -80 °C until tumors were sectioned. Frozen sections (5 μm) were cut and Hoechst 33342 labeled cells were visualized and photographed under a fluorescence microscope equipped with a camera with 365 nm excitation and 420 nm emission filters showing blue fluorescence. Four high power fields under the fluorescence microscope were photographed and Hoechst 33342 labeled cells were counted. The mean number of labeled cells reflected the blood perfusion of tumor and has been shown to be inversely related to the level of hypoxia in tumor[7].
In situ hybridization (ISH) detection
ISH kits (Boster, China) were used to detect vascular endothelial growth factor (VEGF) and matrix metalloprotenase-1 (MMP-1) mRNA expression. Experiments were performed following the manufacturer’s instructions. Briefly, frozen sections (5 μm) were taken from the tumor and fixed with 40 g·L-1 polyformaldehyte in PBS (0.1 mol·L-1) for 30 min, then digested in pepsin for 3 min at 37 °C. The material was prehybridized for 2 h and then hybridized with Digoxin labeled probe overnight at 40 °C. After hybridization, sections were washed with 2 × SSC, 0.2 × SSC, and then incubated with rabbit anti-Digoxin antibody, biotinylated secondary antibody IgG, SABC. Slides were stained with DAB and studied under a light microscope equipped with a camera. A positive stain should be present as intracytoplasmic. The level of mRNA expression was evaluated by two of the authors on blinded sections and was expressed as a positive staining rate.
Serum VEGF assay with ELISA
Blood samples collected from the inferior vena cava of rats were pooled, coagulated, and centrifuged at 1000 × g for 10 min. After the serum was aspirated, the VEGF level was assayed with an ELISA kit (MEGA, USA). Experiments were performed following the manufacturer’s instructions.
Statistical analysis
The number of Hoechst 33342 labeled cells, the percentage of positive staining cells of ISH detection, and the serum VEGF level were expressed as mean ± SD. The difference between mean values were co mpared by Student’s t test. A P value less than 0.05 was considered to be statistically significant. Linear regression was used for the correlation assessment. Statistical analyses were performed using SPSS software.
RESULTS
Blood perfusion of tumor
The mean number of Hoechst 33342 labeled cells represents the blood perfusion of tumor, and indirectly represents the level of hypoxia in tumor. The lower number of labeled cells suggests an impaired blood perfusion and a higher level of hypoxia in tumor. The mean number of Hoechst 33342 labeled cells in the control, the laparotomy control, and the HAL groups were 384 ± 19, 369 ± 27, and 329 ± 29, respectively. The number of labeled cells in the HAL group decreased significantly compared with that in the control and the laparotomy control groups (P < 0.05, Table 1 and Figure 1). This suggests a decreased blood perfusion and a more serious hypoxia of tumor after HAL.
Table 1.
Number of Hoechst labeled cells, serum VEGF, and VEGF, MMP-1 mRNA expression in tumor (-x ± s)
| Groups | n | Hoechst 33342 labeled cells | Serum VEGF (ng·L-1) | VEGF mRNA | MMP-1 mRNA |
| Control | 8 | 384 ± 19 | 55 ± 19 | 0.34 ± 0.14 | 0.24 ± 0.17 |
| Laparotomy control | 4 | 369 ± 27 | 70 ± 40 | 0.19 ± 0.17 | 0.30 ± 0.02 |
| HAL | 8 | 329 ± 29bc | 93 ± 44a | 0.51 ± 0.15ad | 0.47 ± 0.11bc |
P < 0.05,
P < 0.01 vs control group;
P < 0.05,
P < 0.01 vs laparotomy control group.
Figure 1.
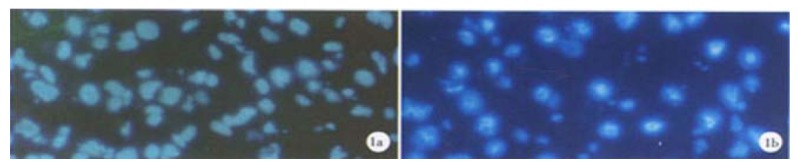
Hoechst 33342 labeled cells. A: Control animals; B: HAL group, decreased number of labeled cells means decreased vascular supply.
VEGF and MMP-1 mRNA expression
ISH showed both VEGF and MMP-1 mRNA expressed in the implanted tumor of control and laparotomy control groups. There was no significant difference between these two groups (P > 0.05). The expression of VEGF and MMP-1 in the HAL group was elevated significantly compared with values in the control and the laparotomy control groups (P < 0.05). Results of their expression in the different groups are shown in Table 1, and Figure 2 and Figure 3.
Figure 2.
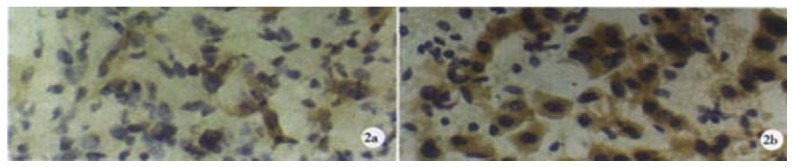
VEGF mRNA in hybridization. A: Low expression in tumor of control animals; B: HAL group, a higher VEGF expression.
Figure 3.
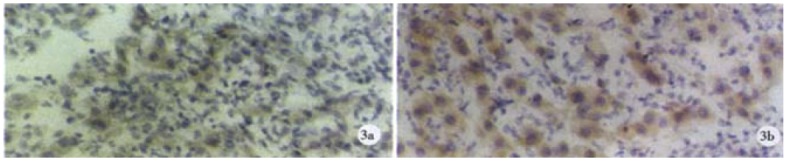
MMP-1 mRNA in hybridization. A: Low expression in tumor of control animals; B: HAL group, a higher MMP-1 expression.
Serum VEGF level
The serum VEGF level was 55 ng·L-1 ± 19 ng·L-1 in the control group, and 70 ng·L-1 ± 40 ng·L-1 in the laparotomy control group, which was elevated slightly, but not significantly, as compared to the control group. While in the HAL group, the level of serum VEGF was 93 ng·L-1 ± 44 ng·L-1, which was elevated significantly when compared with the control group (P < 0.05, Table 1).
Correlation between blood perfusion and VEGF, MMP-1 expression
There was a positive correlation between the serum VEGF level and the expression level of VEGF mRNA in tumor tissue (r = 0.206, P < 0.05). The blood perfusion data of tumor, represented by number of Hoechst 33342 labeled cells, showed a good linear inverse correlation with the serum VEGF level (r = -0.606, P < 0.05) and VEGF mRNA expression in tumor tissue (r = -0.338, P < 0.01). These data suggest that deteriorating blood perfusion and increased hypoxia of tumor correlated with a higher level of VEGF expression. There was no linear correlation between the number of Hoechst 33342 labeled cells and MMP-1 mRNA expression in tumor tissue.
DISCUSSION
TAE is an excellent debulking procedure and destroys malignant cells by selectively blocking the blood perfusion of the liver cancer. However, TAE can not block the blood supply of liver cancer and eliminate tumor cells completely, because the liver cancer receives the blood supply not only from the hepatic artery, but also from the port vein. Besides, it has been found that TAE could promote metastases of liver cancer[4-6]. Thus, the long-term efficacy of TAE was disappointing: the 5-year survival rate was not above 20%[10-14]. Even in several prospective randomized trials, TAE failed to improve significantly the survival of patients with PLC[15,16]. Currently, the mechanisms involved in TAE-induced metastases of PLC are unknown. Understanding the mechanisms will facilitate the development of methods for blocking metastases and promoting long-term efficacy of TAE for treatment of liver cancer.
In recent years, many in vitro studies showed that hypoxia could enhance the metastatic ability of cancer cells by different mechanisms. It was reported that hypoxia stimulated carcinoma cell invasiveness by way of up-regulation of urokinase receptor expression[17,18]. Hypoxia is the most important stimulus for the up-regulation of VEGF, one of the key cytokines for angiogenesis[19-21]. Hypoxia could also induce the expression of other genes that promote angiogenesis and metastasis, such as basic fibroblast growth factor (bFGF) and angiogenin in tumor cells[22-24]. Rofstad et al[25] found that hypoxia could induce metastasis of human melanoma cells via VEGF-mediated angiogenesis. In vivo research also suggested that hypoxia may be one of the important stimuli of metastases. Hypoxia of tumor correlated with the expression of VEGF[26-29], which was found to be correlated with metastases of the tumor and poor prognosis[30-34]. Hypoxia in the squamous cell carcinoma of the uterine cervix with lymph node metastases was more serious than that in the carcinoma without lymph node metastases[35]. Thus, we hypothesized that the inefficient vascular supply after TAE would result in hypoxia of some of the liver cancer cells, as it blocks the blood supply incompletely. We also suggest that hypoxia caused by TAE may induce metastasis-associated factors, such as VEGF mediated metastases of liver cancer. It was found that the serum VEGF level in patients with liver cancer elevated 7 days after TAE therapy[36]. In the present study, we blocked the hepatic arterial blood supply of implanted cancer in rat liver by HAL to simulate TAE therapy, and found that the blood perfusion decreased. This appears to suggest a more serious hypoxia. The expression of VEGF, both in serum and in tumor tissue, increased 2 days after the blockage of the arterial blood supply. Furthermore, we found that there was an inverse correlation between the blood perfusion of tumor and the serum VEGF level or VEGF mRNA expression in tumor tissues. These data indicate that hypoxia after HAL may be the major cause of the elevated expression of VEGF. The results of our study provide evidence for our hypothesis preliminarily. The hypoxia after TAE should be detected directly by hypoxyprobe-1[37,38], and if the hypoxia and expression of VEGF play a direct role in the mechanisms involved in TAE-induced metastases of liver cancer requires further studies. MMP is a secreted or transmembrane protein that is capable of digesting extracellular matrix and basement membrane and was associated with invasion and metastases of human tumor, such as hepatocellular carcinoma and colon cancer[39-46]. It has been found that hypoxia could increase cellular invasiveness by inducing the expression of MMP[47-50]; but there was no report about the change of MMP expression in liver cancer after TAE or HAL therapy. In the present study, we found that the expression of MMP-1 in tumor tissue increased 2 days after the blockage of the arterial blood supply, but there was no linear correlation between the blood perfusion of the tumor and MMP-1 mRNA expression in tumor tissue. Which is the cause of elevated MMP-1 expression and whether it played a direct role in the mechanisms involved in TAE-induced metastasis need further study.
In conclusion, the blood perfusion of implanted liver cancer in rats decreases and the expression of metastases-associated genes VEGF and MMP-1 increases after blockage therapy of the hepatic arterial blood supply. Decreased blood supply and hypoxia may be the main cause of VEGF expression. A more complete understanding of the mechanisms involved in TAE-induced metastasis may lead to an enhancement of the long-term effects of TAE on liver cancer.
ACKNOWLEDGMENTS
We would like to thank Mrs. Margaret-Hiatt Rosen, Director of Admission, the Mead School, Stamford, USA, for her correction of the English translation of the paper.
Footnotes
Supported by Science and Technology Development Fund of Shanghai Municipality, No. 004119086
Edited by Ma JY
References
- 1.Faivre J, Forman D, Estève J, Obradovic M, Sant M. Survival of patients with primary liver cancer, pancreatic cancer and biliary tract cancer in Europe. EUROCARE Working Group. Eur J Cancer. 1998;34:2184–2190. doi: 10.1016/s0959-8049(98)00330-x. [DOI] [PubMed] [Google Scholar]
- 2.Chen J, Sankaranrayanan R, Li W. [Population-based survival analysis of primary liver cancer in a high-incidence area-Qidong, China during 1972-1991] Zhonghua Yufang Yixue Zazhi. 1997;31:149–152. [PubMed] [Google Scholar]
- 3.El-Serag HB, Mason AC, Key C. Trends in survival of patients with hepatocellular carcinoma between 1977 and 1996 in the United States. Hepatology. 2001;33:62–65. doi: 10.1053/jhep.2001.21041. [DOI] [PubMed] [Google Scholar]
- 4.Liou TC, Shih SC, Kao CR, Chou SY, Lin SC, Wang HY. Pulmonary metastasis of hepatocellular carcinoma associated with transarterial chemoembolization. J Hepatol. 1995;23:563–568. doi: 10.1016/0168-8278(95)80063-8. [DOI] [PubMed] [Google Scholar]
- 5.Hanazaki K, Kajikawa S, Shimozawa N, Mihara M, Shimada K, Hiraguri M, Koide N, Adachi W, Amano J. Survival and recurrence after hepatic resection of 386 consecutive patients with hepatocellular carcinoma. J Am Coll Surg. 2000;191:381–388. doi: 10.1016/s1072-7515(00)00700-6. [DOI] [PubMed] [Google Scholar]
- 6.Lai EC, Lo CM, Fan ST, Liu CL, Wong J. Postoperative adjuvant chemotherapy after curative resection of hepatocellular carcinoma: a randomized controlled trial. Arch Surg. 1998;133:183–188. doi: 10.1001/archsurg.133.2.183. [DOI] [PubMed] [Google Scholar]
- 7.Rijken PF, Bernsen HJ, Peters JP, Hodgkiss RJ, Raleigh JA, van der Kogel AJ. Spatial relationship between hypoxia and the (perfused) vascular network in a human glioma xenograft: a quantitative multi-parameter analysis. Int J Radiat Oncol Biol Phys. 2000;48:571–582. doi: 10.1016/s0360-3016(00)00686-6. [DOI] [PubMed] [Google Scholar]
- 8.Bernsen HJ, Rijken PF, Hagemeier NE, van der Kogel AJ. A quantitative analysis of vascularization and perfusion of human glioma xenografts at different implantation sites. Microvasc Res. 1999;57:244–257. doi: 10.1006/mvre.1999.2143. [DOI] [PubMed] [Google Scholar]
- 9.Durand RE, Raleigh JA. Identification of nonproliferating but viable hypoxic tumor cells in vivo. Cancer Res. 1998;58:3547–3550. [PubMed] [Google Scholar]
- 10.Ueno K, Miyazono N, Inoue H, Nishida H, Kanetsuki I, Nakajo M. Transcatheter arterial chemoembolization therapy using iodized oil for patients with unresectable hepatocellular carcinoma: evaluation of three kinds of regimens and analysis of prognostic factors. Cancer. 2000;88:1574–1581. [PubMed] [Google Scholar]
- 11.Poon RT, Ngan H, Lo CM, Liu CL, Fan ST, Wong J. Transarterial chemoembolization for inoperable hepatocellular carcinoma and postresection intrahepatic recurrence. J Surg Oncol. 2000;73:109–114. doi: 10.1002/(sici)1096-9098(200002)73:2<109::aid-jso10>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 12.Savastano S, Miotto D, Casarrubea G, Teso S, Chiesura-Corona M, Feltrin GP. Transcatheter arterial chemoembolization for hepatocellular carcinoma in patients with Child's grade A or B cirrhosis: a multivariate analysis of prognostic factors. J Clin Gastroenterol. 1999;28:334–340. doi: 10.1097/00004836-199906000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Sithinamsuwan P, Piratvisuth T, Tanomkiat W, Apakupakul N, Tongyoo S. Review of 336 patients with hepatocellular carcinoma at Songklanagarind Hospital. World J Gastroenterol. 2000;6:339–343. doi: 10.3748/wjg.v6.i3.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guo WJ, Yu EX. Evaluation of combined therapy with chemoembolization and irradiation for large hepatocellular carcinoma. Br J Radiol. 2000;73:1091–1097. doi: 10.1259/bjr.73.874.11271902. [DOI] [PubMed] [Google Scholar]
- 15.Pelletier G, Ducreux M, Gay F, Luboinski M, Hagège H, Dao T, Van Steenbergen W, Buffet C, Rougier P, Adler M, et al. Treatment of unresectable hepatocellular carcinoma with lipiodol chemoembolization: a multicenter randomized trial. Groupe CHC. J Hepatol. 1998;29:129–134. doi: 10.1016/s0168-8278(98)80187-6. [DOI] [PubMed] [Google Scholar]
- 16.Bruix J, Llovet JM, Castells A, Montañá X, Brú C, Ayuso MC, Vilana R, Rodés J. Transarterial embolization versus symptomatic treatment in patients with advanced hepatocellular carcinoma: results of a randomized, controlled trial in a single institution. Hepatology. 1998;27:1578–1583. doi: 10.1002/hep.510270617. [DOI] [PubMed] [Google Scholar]
- 17.Graham CH, Forsdike J, Fitzgerald CJ, Macdonald-Goodfellow S. Hypoxia-mediated stimulation of carcinoma cell invasiveness via upregulation of urokinase receptor expression. Int J Cancer. 1999;80:617–623. doi: 10.1002/(sici)1097-0215(19990209)80:4<617::aid-ijc22>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 18.Kroon ME, Koolwijk P, van der Vecht B, van Hinsbergh VW. Urokinase receptor expression on human microvascular endothelial cells is increased by hypoxia: implications for capillary-like tube formation in a fibrin matrix. Blood. 2000;96:2775–2783. [PubMed] [Google Scholar]
- 19.Gunningham SP, Currie MJ, Han C, Turner K, Scott PA, Robinson BA, Harris AL, Fox SB. Vascular endothelial growth factor-B and vascular endothelial growth factor-C expression in renal cell carcinomas: regulation by the von Hippel-Lindau gene and hypoxia. Cancer Res. 2001;61:3206–3211. [PubMed] [Google Scholar]
- 20.Rössler J, Breit S, Havers W, Schweigerer L. Vascular endothelial growth factor expression in human neuroblastoma: up-regulation by hypoxia. Int J Cancer. 1999;81:113–117. doi: 10.1002/(sici)1097-0215(19990331)81:1<113::aid-ijc19>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 21.Vasir B, Aiello LP, Yoon KH, Quickel RR, Bonner-Weir S, Weir GC. Hypoxia induces vascular endothelial growth factor gene and protein expression in cultured rat islet cells. Diabetes. 1998;47:1894–1903. doi: 10.2337/diabetes.47.12.1894. [DOI] [PubMed] [Google Scholar]
- 22.Le YJ, Corry PM. Hypoxia-induced bFGF gene expression is mediated through the JNK signal transduction pathway. Mol Cell Biochem. 1999;202:1–8. doi: 10.1023/a:1007059806016. [DOI] [PubMed] [Google Scholar]
- 23.Hartmann A, Kunz M, Köstlin S, Gillitzer R, Toksoy A, Bröcker EB, Klein CE. Hypoxia-induced up-regulation of angiogenin in human malignant melanoma. Cancer Res. 1999;59:1578–1583. [PubMed] [Google Scholar]
- 24.Brahimi-Horn C, Berra E, Pouysségur J. Hypoxia: the tumor's gateway to progression along the angiogenic pathway. Trends Cell Biol. 2001;11:S32–S36. doi: 10.1016/s0962-8924(01)02126-2. [DOI] [PubMed] [Google Scholar]
- 25.Rofstad EK, Danielsen T. Hypoxia-induced metastasis of human melanoma cells: involvement of vascular endothelial growth factor-mediated angiogenesis. Br J Cancer. 1999;80:1697–1707. doi: 10.1038/sj.bjc.6690586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fukumura D, Xu L, Chen Y, Gohongi T, Seed B, Jain RK. Hypoxia and acidosis independently up-regulate vascular endothelial growth factor transcription in brain tumors in vivo. Cancer Res. 2001;61:6020–6024. [PubMed] [Google Scholar]
- 27.Cvetkovic D, Movsas B, Dicker AP, Hanlon AL, Greenberg RE, Chapman JD, Hanks GE, Tricoli JV. Increased hypoxia correlates with increased expression of the angiogenesis marker vascular endothelial growth factor in human prostate cancer. Urology. 2001;57:821–825. doi: 10.1016/s0090-4295(00)01044-x. [DOI] [PubMed] [Google Scholar]
- 28.Dunst J, Stadler P, Becker A, Kuhnt T, Lautenschläger C, Molls M, Haensgen G. Tumor hypoxia and systemic levels of vascular endothelial growth factor (VEGF) in head and neck cancers. Strahlenther Onkol. 2001;177:469–473. doi: 10.1007/pl00002428. [DOI] [PubMed] [Google Scholar]
- 29.Laderoute KR, Alarcon RM, Brody MD, Calaoagan JM, Chen EY, Knapp AM, Yun Z, Denko NC, Giaccia AJ. Opposing effects of hypoxia on expression of the angiogenic inhibitor thrombospondin 1 and the angiogenic inducer vascular endothelial growth factor. Clin Cancer Res. 2000;6:2941–2950. [PubMed] [Google Scholar]
- 30.Ishigami SI, Arii S, Furutani M, Niwano M, Harada T, Mizumoto M, Mori A, Onodera H, Imamura M. Predictive value of vascular endothelial growth factor (VEGF) in metastasis and prognosis of human colorectal cancer. Br J Cancer. 1998;78:1379–1384. doi: 10.1038/bjc.1998.688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.O-charoenrat P, Rhys-Evans P, Eccles SA. Expression of vascular endothelial growth factor family members in head and neck squamous cell carcinoma correlates with lymph node metastasis. Cancer. 2001;92:556–568. doi: 10.1002/1097-0142(20010801)92:3<556::aid-cncr1355>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 32.Fujimoto J, Sakaguchi H, Aoki I, Khatun S, Tamaya T. Clinical implications of expression of vascular endothelial growth factor in metastatic lesions of ovarian cancers. Br J Cancer. 2001;85:313–316. doi: 10.1054/bjoc.2001.1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Niu Q, Tang ZY, Ma ZC, Qin LX, Zhang LH. Serum vascular endothelial growth factor is a potential biomarker of metastatic recurrence after curative resection of hepatocellular carcinoma. World J Gastroenterol. 2000;6:565–568. doi: 10.3748/wjg.v6.i4.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Harada Y, Ogata Y, Shirouzu K. Expression of vascular endothelial growth factor and its receptor KDR (kinase domain-containing receptor)/Flk-1 (fetal liver kinase-1) as prognostic factors in human colorectal cancer. Int J Clin Oncol. 2001;6:221–228. doi: 10.1007/pl00012109. [DOI] [PubMed] [Google Scholar]
- 35.Sundfør K, Lyng H, Rofstad EK. Tumour hypoxia and vascular density as predictors of metastasis in squamous cell carcinoma of the uterine cervix. Br J Cancer. 1998;78:822–827. doi: 10.1038/bjc.1998.586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Suzuki H, Mori M, Kawaguchi C, Adachi M, Miura S, Ishii H. Serum vascular endothelial growth factor in the course of transcatheter arterial embolization of hepatocellular carcinoma. Int J Oncol. 1999;14:1087–1090. doi: 10.3892/ijo.14.6.1087. [DOI] [PubMed] [Google Scholar]
- 37.Raleigh JA, Chou SC, Bono EL, Thrall DE, Varia MA. Semiquantitative immunohistochemical analysis for hypoxia in human tumors. Int J Radiat Oncol Biol Phys. 2001;49:569–574. doi: 10.1016/s0360-3016(00)01505-4. [DOI] [PubMed] [Google Scholar]
- 38.Shabsigh A, Ghafar MA, de la Taille A, Burchardt M, Kaplan SA, Anastasiadis AG, Buttyan R. Biomarker analysis demonstrates a hypoxic environment in the castrated rat ventral prostate gland. J Cell Biochem. 2001;81:437–444. [PubMed] [Google Scholar]
- 39.Jiang YF, Yang ZH, Hu JQ. Recurrence or metastasis of HCC: predictors, early detection and experimental antiangiogenic therapy. World J Gastroenterol. 2000;6:61–65. doi: 10.3748/wjg.v6.i1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ogata Y, Miura K, Ohkita A, Nagase H, Shirouzu K. Imbalance between matrix metalloproteinase 9 and tissue inhibitor of metalloproteinases 1 expression by tumor cells implicated in liver metastasis from colorectal carcinoma. Kurume Med J. 2001;48:211–218. doi: 10.2739/kurumemedj.48.211. [DOI] [PubMed] [Google Scholar]
- 41.Ohnishi Y, Tajima S, Ishibashi A. Coordinate expression of membrane type-matrix metalloproteinases-2 and 3 (MT2-MMP and MT3-MMP) and matrix metalloproteinase-2 (MMP-2) in primary and metastatic melanoma cells. Eur J Dermatol. 2001;11:420–423. [PubMed] [Google Scholar]
- 42.Ghilardi G, Biondi ML, Mangoni J, Leviti S, DeMonti M, Guagnellini E, Scorza R. Matrix metalloproteinase-1 promoter polymorphism 1G/2G is correlated with colorectal cancer invasiveness. Clin Cancer Res. 2001;7:2344–2346. [PubMed] [Google Scholar]
- 43.O-Charoenrat P, Rhys-Evans PH, Eccles SA. Expression of matrix metalloproteinases and their inhibitors correlates with invasion and metastasis in squamous cell carcinoma of the head and neck. Arch Otolaryngol Head Neck Surg. 2001;127:813–820. [PubMed] [Google Scholar]
- 44.Nordqvist AC, Smurawa H, Mathiesen T. Expression of matrix metalloproteinases 2 and 9 in meningiomas associated with different degrees of brain invasiveness and edema. J Neurosurg. 2001;95:839–844. doi: 10.3171/jns.2001.95.5.0839. [DOI] [PubMed] [Google Scholar]
- 45.Ye S, Dhillon S, Turner SJ, Bateman AC, Theaker JM, Pickering RM, Day I, Howell WM. Invasiveness of cutaneous malignant melanoma is influenced by matrix metalloproteinase 1 gene polymorphism. Cancer Res. 2001;61:1296–1298. [PubMed] [Google Scholar]
- 46.Yamamoto H, Itoh F, Iku S, Adachi Y, Fukushima H, Sasaki S, Mukaiya M, Hirata K, Imai K. Expression of matrix metalloproteinases and tissue inhibitors of metalloproteinases in human pancreatic adenocarcinomas: clinicopathologic and prognostic significance of matrilysin expression. J Clin Oncol. 2001;19:1118–1127. doi: 10.1200/JCO.2001.19.4.1118. [DOI] [PubMed] [Google Scholar]
- 47.Yamanaka M, Ishikawa O. Hypoxic conditions decrease the mRNA expression of proalpha1(I) and (III) collagens and increase matrix metalloproteinases-1 of dermal fibroblasts in three-dimensional cultures. J Dermatol Sci. 2000;24:99–104. doi: 10.1016/s0923-1811(00)00086-4. [DOI] [PubMed] [Google Scholar]
- 48.Canning MT, Postovit LM, Clarke SH, Graham CH. Oxygen-mediated regulation of gelatinase and tissue inhibitor of metalloproteinases-1 expression by invasive cells. Exp Cell Res. 2001;267:88–94. doi: 10.1006/excr.2001.5243. [DOI] [PubMed] [Google Scholar]
- 49.Koong AC, Denko NC, Hudson KM, Schindler C, Swiersz L, Koch C, Evans S, Ibrahim H, Le QT, Terris DJ, et al. Candidate genes for the hypoxic tumor phenotype. Cancer Res. 2000;60:883–887. [PubMed] [Google Scholar]
- 50.Himelstein BP, Koch CJ. Studies of type IV collagenase regulation by hypoxia. Cancer Lett. 1998;124:127–133. doi: 10.1016/s0304-3835(97)00463-1. [DOI] [PubMed] [Google Scholar]


