Abstract
AIM: Transforming growth factor (TGF) β1 is involved in a variety of important cellular functions, including cell growth and differentiation, angiogenesis, immune function and extracellular matrix formation. However, the role of TGF-β1 as an angiogenic factor in colorectal cancer is still unclear. We investigate the relationship between transforming growth factor β1 and angiogenesis by analyzing the expression of transforming growth factor (TGF) β1 in colorectal cancer, as well as its association with VEGF and MVD.
METHODS: The expression of TGF-β1, VEGF, as well as MVD were detected in 98 colorectal cancer by immunohistochemical staining. The relationship between the TGF-β1 expression and VEGF expression, MVD was evaluated. To evaluate the effect of TGF-β1 on the angiogenesis of colorectal cancers.
RESULTS: Among 98 cases of colorectal cancer, 37 were positive for TGF-β1 (37.8%), 36 for VEGF (36.7%), respectively. The microvessel counts ranged from 19 to 139.8, with a mean of 48.7 (standard deviation, 21.8). The expression of TGF-β1 was correlated significantly with the depth of invasion, stage of disease, lymph node metastasis, VEGF expression and MVD. Patients in T3-T4, stage III-IV and with lymph node metastasis had much higher expression of TGF-β1 than patients in T1-T2, stageI-II and without lymph node metastasis (P < 0.05). The positive expression rate of VEGF (58.3%) in the TGF-β1 positive group is higher than that in the TGF-β1 negative group (41.7%, P < 0.05). Also, the microvessel count (54 ± 18) in TGF-β1 positive group is significantly higher than that in TGF-β1 negative group (46 ± 15, P < 0.05). The microvessel count in tumors with both TGF-β1 and VEGF positive were the highest (58 ± 20, 36-140, P < 0.05). Whereas that in tumors with both TGF-β1 and VEGF negative were the lowest (38 ± 16, 19-60, P < 0.05).
CONCLUSION: TGF-β1 might be associated with tumor progression by madulating the angiogenesis in colorectal cancer and TGF-β1 may be used as a possible biomarker.
INTRODUCTION
Angiogenesis is essential for tumor growth and metastasis[1-6]. An association between poor prognosis and increase in microvascular density (MVD) of tumor has been reported in certain tumors[5-10]. This neoangiogenesis depends on the production of angiogenic factors by tumor cells and normal cells[7-15]. Vascular endothelial growth factor (VEGF) also plays a key role in angiogenesis of tumor[3-20], but the role of transforming growth factor-β1 is not clear yet. Now the expression of TGF-β1 and VEGF, MVD were detected in 98 colorectal cancer by immunohistochemical staining, in order to investigate the correlation of TGF-β1 and angiogenesis in colorectal cancer.
MATERIALS AND METHODS
Patients
All total of 98 colorectal adenocarcinoma patients who had undergone surgical resection in the Affiliated Zhongnan Hospital of Wuhan University (Wuhan) from July 1998 to December 2000 were included. There were 53 male and 45 female, with an age range from 23 to 74 years (mean, 56 ± 11.2 years). Among the 98 adenocarcinoma patients, 17 were well differentiated, 47 moderately differentiated and 34 poorly differentiated. According to Dukes stage criteria, 34 cases were stage I, 29 stage II, 30 stage III and 5 stage IV.
Methods
Immunohistochemistry All the tissue specimens were fixed in 100 mL·L-1 neutral formalin and embedded in paraffin. Five-micrometer-thick sections were treated with xylene, dehydrated in ethanol. Tissue sections were washed three times in 0.05 mol·L-1 PBS, incubated in endogenous peroxidase blocking solution. Non-specific antibody binding was blocked by pretreatment with PBS containing 5 g·L-1 bovin serum albumin. Sections were then rinsed in PBS and incubated overnight at 4 °C with diluted anti-TGF-β1 protein polyclonal antibody, anti-VEGF protein polyclonal antibody and anti-CD34 protein monoclonal antibody. These steps were performed using immunostain kit according to the manufacturers instructions. PBS was used as substitutes of protein antibody for negative control groups. The sections were examined under light microscopy. Anti-TGF-β1 protein polyclonal antibody were purchased from Bosden Co (Wuhan). Anti-VEGF protein polyclonal antibody, anti-CD34 protein monoclonal antibody, and S-P detection kit were purchased from Fuzhou Maixin Co. Anti-TGF-β1 protein polyclonal antibody was diluted to 1:100. Anti-VEGF protein polyclonal antibody and anti-CD34 protein monoclonal antibody were impromptu type.
Results Positive signal was located in the cytoplasm or/and cell membrane. Immunoreactivity was graded as follows: +, ≥ 10% stained tumor cells; -, < 10% o stained tumor cells[21-23]. The microvessel counting procedures have been described in the published studies[21-24]. Briefly, the stained sections were screened at a magnification of × 100 (× 10 objective and × 10 ocular lens) under a light microscope to identify the 3 regions of the section with the highest microvessel density. Microvessels were counted in these areas at a magnification of × 200, and the average numbers of microvessels were recorded. The average number is known as MVD of the tumor.
Statistical analysis The difference between each group was analyzed by Chi-square test and correlativity. Significant difference was taken of P < 0.05.
RESULTS
TGF-β1 expression in colorectal cancer and clinicopathologic findings
TGF-β1 was localized mainly in the cytoplasm and cell membrane of the tumor cells (Figure 1). TGF-β1 expression was detected in 37 tumors (37.8%). The correlation between TGF-β1 expression and the clinicopathologic findings was shown in Table 1. The expression of TGF-β1 was correlated significantly with the depth of invasion, stage of disease and lymph node metastasis. Patients in T3-T4, stage III-IV and with lymph node metastasis had much higher TGF-β1 than patients in T1-T2, stage I-II and without lymph node metastasis (P < 0.05). The expression of TGF-β1 was not correlated with age, gender and differentiation degree of the tumor.
Figure 1.
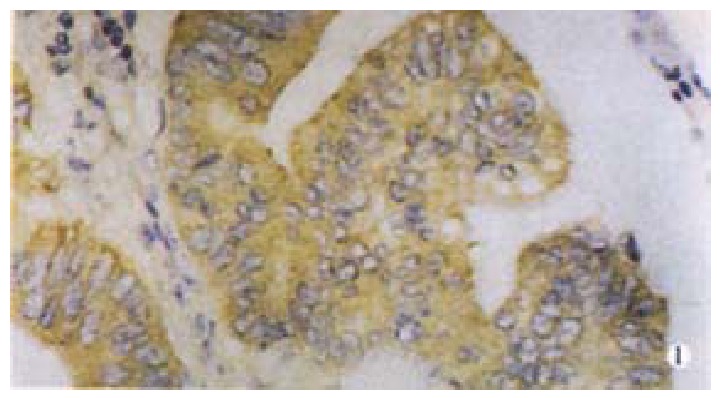
TGF-β1 mainly in cytoplasm and membrane of tumor cells, × 400
Table 1.
Relationship between expression of TGF-β1 and clinicopathologic findings
| Clinic-pathologic parameters |
TGF-β1 expression(%) |
|
| Positive(n = 37) | Negative(n = 61) | |
| Male | 20 (37.8) | 33 (62.3) |
| Female | 17 (37.8) | 28 (62.2) |
| Age (y) | 55 ± 13 | 57 ± 12 |
| Histology: differentiation | ||
| Well | 9 (52.9) | 8 (47.1) |
| Moderate | 15 (31.9) | 32 (68.1) |
| Poor | 13 (38.2) | 21 (61.8) |
| Depth of invasion | ||
| T1-T2 | 17 (28.3) | 43 (71.7) |
| T3-T4 | 20 (52.6) | 18 (47.4) a |
| Lymph node metastasis | ||
| Present | 18 (51.4) | 17 (48.6) |
| Absent | 19 (30.2) | 44 (69.8) a |
| Dukes Stage | ||
| I | 8 (23.5) | 26 (76.5) |
| II | 9 (31.1) | 20 (68.9) |
| III + IV | 20 (57.1) | 15 (42.9) a |
| VEGF expression | ||
| Positive | 21 (58.3) | 15 (41.7) |
| Negative | 16 (25.8) | 46 (74.2) a |
| MVD (-x ± s) | 54 ± 18 | 46 ± 15a |
P < 0.05, vs positive
Relationship between TGF-β1 expression, VEGF expression and MVD
VEGF was localized mainly in the cytoplasm and cell membrane of the tumor cells (Figure 2). VEGF expression was detected in 36 tumors (36.7%), and TGF-β1 expression was correlated closely with VEGF expression (Table 1). The positive expression rate of VEGF (58.3%) in the positive TGF-β1 group was higher than that in the negative TGF-β1 group (41.7%, P < 0.05).
Figure 2.
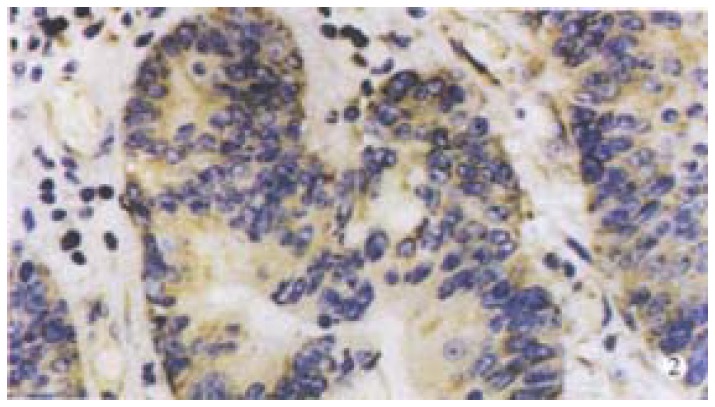
VEGF expression mainly in cytoplasm and membrane of tumor cell, × 400
The number of the microvessel counts in all cases were 19-140 (± s, 49 ± 22). Moreover, the microvessel counts were 54 ± 18 in TGF-β1 positive tumors and 46 ± 15 in TGF-β1 negative tumors (P < 0.05, Table 1). TGF-β1 expression, VEGF expression and MVD were significantly correlated one another (r = 0.5816, 0.2619 and 0.5182, respectively. P < 0.05). The microvessel counts in tumors with both positive TGF-β1 and VEGF were the highest (58 ± 20, 36-140; P < 0.05). The microvessel counts in tumors with both negative TGF-β1 and VEGF were the lowest (38 ± 16, 19-60; P < 0.05). The microvessel counts in tumors with positive TGF-β1 and negative VEGF were 25-128 (49 ± 18), and that in tumors with negative TGF-β1 and positive VEGF were 31-133 (50 ± 20), lower than that in tumors with both positive TGF-β1 and VEGF (P < 0.05).
DISCUSSION
The process of angiogenesis is the outcome of an imbalance between positive and negative angiogenic factors produced by both tumor cells and normal cells. Numerous angiogenic factors have been described. Of these, VEGF play a key role in the angiogenesis in the colorectal cancer[3-25]. VEGF is a multi-functional cytokine, and has direct relationship with angiogenesis. The factors that regulate VEGF expression in tumor and non-tumor cells have now been elucidated[20-31]. The TGF-β s represent a family of multifunctional cytokines that modulate the growth and function of many cells, including those with malignant transformation. The over-expression of TGF-β1 has been reported in tissue from patients with different carcinoma, and is believed to play a role in tumor transformation and progression, as well as in tumor regression[23-33]. Studied the correlation of TGF-β1 and angiogenesis of gastric cancer, and found TGF-β1 might regulate angiogenesis through an up-regulation of the expression of VEGF. A direct correlation between TGF-β1 expression and microvessel counts had not been identified in the current study[20-30]. TGF-β1 has no relationship with VEGF expression in breast cancer tissue, but is correlated with the expression of platelet-derived growth factor, and co-regulate angiogenesis[20-24]. The modulating mechanisms of TGF-β1 in angiogenesis are not entirely the same in different type of tumor.
The role of TGF-β1 in angiogenesis of colorectal cancer is not identified yet. This study found that the expression of VEGF and MVD in positive TGF-β1 group are significantly higher than that in TGF-β1 negative group. The expression of TGF-β1 is significantly positively correlated with the expression of VEGF. It demonstrated that TGF-β1 may be correlated indirectly with angiogenesis through an up-regulation of the expression of VEGF. The expression of TGF-β1 is also significantly positively correlated with MVD in colorectal cancer. It demonstrates that TGF-β1 may modulate angiogenesis directly or indirectly through up-regulating the expression of other angiogenic factors. The microvessel counts in tumors that were both positive TGF-β1 and VEGF were the highest of all. It demonstrates that TGF-β1 and VEGF may co-modulate the angiogenesis.
TGF-β1 expression was detected in 37 tumors (37.8%). The expression of TGF-β1 was correlated significantly with the depth of invasion, stage of disease and lymph node metastasis. Patients in T3-T4, stage III-IV and with lymph node metastasis had much higher expression of TGF-β1 than patients in T1-T2, stageI-II and without lymph node metastasis (P < 0.05).
Footnotes
Supported by Hubei province Natural Science Foundation, No. 2000J054
Edited by Wu XN
References
- 1.Grunstein J, Roberts WG, Mathieu-Costello O, Hanahan D, Johnson RS. Tumor-derived expression of vascular endothelial growth factor is a critical factor in tumor expansion and vascular function. Cancer Res. 1999;59:1592–1598. [PubMed] [Google Scholar]
- 2.Karpanen T, Egeblad M, Karkkainen MJ, Kubo H, Ylä-Herttuala S, Jäättelä M, Alitalo K. Vascular endothelial growth factor C promotes tumor lymphangiogenesis and intralymphatic tumor growth. Cancer Res. 2001;61:1786–1790. [PubMed] [Google Scholar]
- 3.Siemeister G, Schirner M, Weindel K, Reusch P, Menrad A, Marmé D, Martiny-Baron G. Two independent mechanisms essential for tumor angiogenesis: inhibition of human melanoma xenograft growth by interfering with either the vascular endothelial growth factor receptor pathway or the Tie-2 pathway. Cancer Res. 1999;59:3185–3191. [PubMed] [Google Scholar]
- 4.Masood R, Cai J, Zheng T, Smith DL, Hinton DR, Gill PS. Vascular endothelial growth factor (VEGF) is an autocrine growth factor for VEGF receptor-positive human tumors. Blood. 2001;98:1904–1913. doi: 10.1182/blood.v98.6.1904. [DOI] [PubMed] [Google Scholar]
- 5.Leenders W, van Altena M, Lubsen N, Ruiter D, De Waal R. In vivo activities of mutants of vascular endothelial growth factor (VEGF) with differential in vitro activities. Int J Cancer. 2001;91:327–333. doi: 10.1002/1097-0215(200002)9999:9999<::aid-ijc1052>3.3.co;2-n. [DOI] [PubMed] [Google Scholar]
- 6.Veikkola T, Karkkainen M, Claesson-Welsh L, Alitalo K. Regulation of angiogenesis via vascular endothelial growth factor receptors. Cancer Res. 2000;60:203–212. [PubMed] [Google Scholar]
- 7.Teraoka H, Sawada T, Nishihara T, Yashiro M, Ohira M, Ishikawa T, Nishino H, Hirakawa K. Enhanced VEGF production and decreased immunogenicity induced by TGF-beta 1 promote liver metastasis of pancreatic cancer. Br J Cancer. 2001;85:612–617. doi: 10.1054/bjoc.2001.1941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McEarchern JA, Kobie JJ, Mack V, Wu RS, Meade-Tollin L, Arteaga CL, Dumont N, Besselsen D, Seftor E, Hendrix MJ, et al. Invasion and metastasis of a mammary tumor involves TGF-beta signaling. Int J Cancer. 2001;91:76–82. doi: 10.1002/1097-0215(20010101)91:1<76::aid-ijc1012>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 9.Ying YQ, Zhou X, Wu P. Huang WB. Significance of TGF-a and TGF-β1 expressions in the tissue of colorectal cancer. Shijie Huaren Xiaohua Zazhi. 2001;9:223–225. [Google Scholar]
- 10.Wang SM, Wu JS, Yao X, He ZS, Pan BR. Effect of TGFa, EGFR anti-sense oligodeoxynucleotides on colon cancer cell line. Shijie Huaren Xiaohua Zazhi. 1999;7:522–524. [Google Scholar]
- 11.Wang CH, Zhang XM, Zhan M, Tang FX. TGF-β1 and its receptor expression in human colorectal cancer. Shijie Huaren Xiaohua Zazhi. 2001;9:462–463. [Google Scholar]
- 12.Yu BM, Zhao R. Molecular biology of colorectal carcinoma. Shijie Huaren Xiaohua Zazhi. 1999;7:173–175. [Google Scholar]
- 13.Yang JH, Rao BJ, Wang Y, Tu XH, Zhang LY. Clinical significance of defecting the circulating cancer cells in peripheral blood from colorectal cancer. Shijie Huaren Xiaohua Zazhi. 2000;8:187–189. [Google Scholar]
- 14.Jia L, Chen TX, Sun JW, Na ZM, Zhang HH. Relationship between microvessel density and proliferating cell nuclear antigen and prognosis in colorectal cancer. Shijie Huaren Xiaohua Zazhi. 2000;8:74–76. [Google Scholar]
- 15.Maehara Y, Kakeji Y, Kabashima A, Emi Y, Watanabe A, Akazawa K, Baba H, Kohnoe S, Sugimachi K. Role of transforming growth factor-beta 1 in invasion and metastasis in gastric carcinoma. J Clin Oncol. 1999;17:607–614. doi: 10.1200/JCO.1999.17.2.607. [DOI] [PubMed] [Google Scholar]
- 16.Rodeck U, Nishiyama T, Mauviel A. Independent regulation of growth and SMAD-mediated transcription by transforming growth factor beta in human melanoma cells. Cancer Res. 1999;59:547–550. [PubMed] [Google Scholar]
- 17.Sheen-Chen SM, Chen HS, Sheen CW, Eng HL, Chen WJ. Serum levels of transforming growth factor beta1 in patients with breast cancer. Arch Surg. 2001;136:937–940. doi: 10.1001/archsurg.136.8.937. [DOI] [PubMed] [Google Scholar]
- 18.Shim KS, Kim KH, Han WS, Park EB. Elevated serum levels of transforming growth factor-beta1 in patients with colorectal carcinoma: its association with tumor progression and its significant decrease after curative surgical resection. Cancer. 1999;85:554–561. doi: 10.1002/(sici)1097-0142(19990201)85:3<554::aid-cncr6>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 19.Kadambi A, Mouta Carreira C, Yun CO, Padera TP, Dolmans DE, Carmeliet P, Fukumura D, Jain RK. Vascular endothelial growth factor (VEGF)-C differentially affects tumor vascular function and leukocyte recruitment: role of VEGF-receptor 2 and host VEGF-A. Cancer Res. 2001;61:2404–2408. [PubMed] [Google Scholar]
- 20.Saito H, Tsujitani S, Oka S, Kondo A, Ikeguchi M, Maeta M, Kaibara N. The expression of transforming growth factor-beta1 is significantly correlated with the expression of vascular endothelial growth factor and poor prognosis of patients with advanced gastric carcinoma. Cancer. 1999;86:1455–1462. doi: 10.1002/(sici)1097-0142(19991015)86:8<1455::aid-cncr11>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 21.Zhuang ZH, Chen YL, Wang CD, Chen YG. Expression of TGF-β1 and TGF?receptorIin gastric carcinoma and precancerous lesions. Shijie Huaren Xiaohua Zazhi. 1999;7:507–509. [Google Scholar]
- 22.Xiong B, Yuan HY, Hu MB, Zhang F. Serum levels of transforming growth factor-β1 correlating with T cell subsets and natural killer aell activity in colorectal cancer. Shijie Huaren Xiaohua Zazhi. 2001;9:1194–1195. [Google Scholar]
- 23.Ariazi EA, Satomi Y, Ellis MJ, Haag JD, Shi W, Sattler CA, Gould MN. Activation of the transforming growth factor beta signaling pathway and induction of cytostasis and apoptosis in mammary carcinomas treated with the anticancer agent perillyl alcohol. Cancer Res. 1999;59:1917–1928. [PubMed] [Google Scholar]
- 24.Liu DH, Zhang W, Su YP, Zhang XY, Huang YX. Constructions of eukaryotic expression vector of sense and antisense VEGF165 and its expression regulation. Shijie Huaren Xiaohua Zazhi. 2001;9:886–891. [Google Scholar]
- 25.Wan SM, Sun SH, Deng MD, Ge QL, Yang YJ. TGF-β1 and PDGF-A expression in gastric cancer tissue and prognosis. Shijie Huaren Xiaohua Zazhi. 2002;10:36–39. [Google Scholar]
- 26.Si XH, Yang LJ. Extraction and purification of TGFbeta and its effect on the induction of apoptosis of hepatocytes. World J Gastroenterol. 2001;7:527–531. doi: 10.3748/wjg.v7.i4.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wu K, Liu BH, Zhao DY, Zhao Y. Effect of vitamin E succinate on expression of TGF-beta1, c-Jun and JNK1 in human gastric cancer SGC-7901 cells. World J Gastroenterol. 2001;7:83–87. doi: 10.3748/wjg.v7.i1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu F, Liu JX, Cao ZC, Li BS, Zhao CY, Kong L, Zhen Z. Relationship between TGF-β1, serum indexes of liver fibrosis and hepatic tissue pathology in patients with choronic liver diseases. Shijie Huaren Xiaohua Zazhi. 1999;7:519–521. [Google Scholar]
- 29.Liu XP, Song SB, Li G, Wang DJ, Zhao HL, Wei LX. Correlations of microvessel quantitation in colorectal tumors and clinicopathology. Shijie Huaren Xiaohua Zazhi. 1999;7:37–39. [Google Scholar]
- 30.Huang YX, Zhang GX, Lu MS, Fan GR, Chen NL, Wu GH. Increased expression of transforming growth factor-β1 in hepatocellular carcinoma. Huaren Xiaohua Zazhi. 1999;7:150–152. [Google Scholar]
- 31.Yan JC, Chen WB, Ma Y, Shun XH. Expression of vascular endothelial growth factor in liver tissues of hepatitis B. Huaren Xiaohua Zazhi. 1999;7:837–840. [PubMed] [Google Scholar]
- 32.Xiang DD, Wei YL, Li JF. Molecular mechanism of TGF-β1 on Ito cell. Huaren Xiaohua Zazhi. 1999;7:980–981. [Google Scholar]
- 33.Ma XM, Wang YL, Pan BR. Progress in VEGF studies. Huaren Xiaohua Zazhi. 1999;7:895–896. [Google Scholar]


