Abstract
AIM: To investigate the molecular mechanism of cell adaptation and rapid replication of hepatitis A virus strain H2 in KBM17 cells.
METHODS: Virus of strain H2 at passage 7 was consecutively passaged in KBM17 cells for 22 passages, every passage was incubated for 14 d. Antigenic and infectious titers of every passage and one-step growth dynamics of passage 22 were determined with ELISA. Genomes of passage 6, passage 12, passage 18 and passage 22 were sequenced and compared with H2K7.
RESULTS: During continuous passage of vaccine strain H2 at passage K7 in KMB17 cells, infectious and antigenic titers increased with the increase of passages, infectious titers at day 14 reached 6.77 LgCCID50ml-1 for passage 6 (P6), 7.0 LgCCID50ml-1 for passage 12 (P12), 7.33 LgCCID50ml-1 for passage 18 (P18) and 7.83 LgCCID50ml-1 for passage 22 (P22), respectively. The one-step growth dynamics showed that replicating peak of P22 appeared at day 14 with infectious titers of 7.83 LgCCID50ml-1 and antigenic titer of 1:1024. After passage 22 a new cell-adapted variant (P22) of H2K7 with rapid and shortened replication cycle from 28 d to 14 d was obtained. Sequencing and comparisons of genomes of P6, P12, P18 and P22 showed that mutational numbers in genomes of different passages increased with adaptive passages, and mutations scattered over the genome. In comparison with that of K7, P6 had only 6 nucleotides (nt) mutations, P12 had 7 mutational changes, in addition to 6 same mutations with P6, there appeared a new mutation in 5'NTR at nucleotide position 591 resulting in a nucleotide exchange from A to G. P18 had 10 nt mutations, among the 10 mutations, 7 mutational changes were same as with P12, three new mutational changes appeared in the genome, one in 5'NTR, one in 3C coding region, one in 3D coding region, at P22 there appeared 18 nucleotide changes in the genome, on the basis of P18, there occured additional 8 nucleotide mutations, two in 5'NTR, three in 2C, one in 3A, one in 3C and one in 3D. The results suggested that although H2K7 was already an attenuated strain, the mutations of genome is not sufficient to completely adapt the KMB17, further mutations caused rapid replication adaptation.
CONCLUSION: 18-nt changes scattering over the genome are cooperatively responsible for further adaptation characterized by rapid and shortened replication cycle from 28 d to 14 d in KMB17 cells. The mutations in 2C coding region play more important role in increase of infectious titer than other mutations, the mutations in 2B coding region show less important role than it usually does in cell adaptation, nucleotide changes in 5’NTR seem to be not relevant to cell adaptation during initial stages (before P6), but do in late stages.
INTRODUCTION
Hepatitis A virus (HAV), one of the two members of genus Hepatovirus, is enterically transmitted primarily through the fecal/oral route causing sporadic and epidemic acute hepatitis in humans[1,2]. Human HAV is a nonenveloped icosahedral particle of 27-32 nm in diameter with a single-stranded, 7.5-kb positive-sense RNA genome with a long 5' terminal nontranslated RNA segment (5'NTR) and a short 3'NTR with a poly (A) tail[1]. Similar to other picornaviruses, the HAV genome contains one large open reading frame encoding a polyprotein of about 250 kD, which is co-and posttranslationally cleaved into smaller structural proteins (2A, 2B and 2C) and nonstructural proteins (3A, 3B, 3C and 3D) by virus-encoding proteinases[3].
HAV has been adapted to grow in a variety of primate cell lines[4], but in contrast to that of other picornaviruses, the replication cycle of wild-type HAV isolated from infected human in cell culture is extremely low and inefficient. After prolonged incubation and several passages in cell culture, a persistent infection with low virus yields and little apparent impact on cellular growth and metabolism is normally established[5]. Only a few HAV strains have been reported to cause cytophethesis in vitro[6,7].
Unlike other picornaviruses, although HAV can be adapted to grow in a variety of primate cell lines, cell-adapted variants still grow poorly in cell culture. The molecular mechanisms of adaptation and slow replication cycle are still not completely understood.
That the genomes of a number of wild types and cell-adapted HAV strains have been completely or almost completely sequenced made it possible to determine the nucleotide changes responsible for cell adaptation. By sequence comparison of different cell-adapted variants[8-19], and studies with chimeric HAV composed of sequence from wild-type and cell culture-adapted variants[20-22], mutations increasing virus replication in cell culture were identified. The adaptation of HAV to grow in cell culture is associated with a number of cooperative mutations over the whole genome, but the mutations within 5'NTR containing regulatory internal ribosome entry segment (IRES) for viral translation[23], and within 2B and 2C coding regions encoding enzymes for viral RNA replication[24], play more important role in cell adaptation. Moreover, the mutations in 2B and 2C coding regions were proven to be necessary for adaptation of growth in cell culture of HAV variants[10,11,21], the mutations in 5'NTR had no independent effect, but cooperatively acted with 2B and 2C coding regions to enhance replication in cell culture[21,24]. To study further the molecular mechanisms of cell adaptation of HAV in cell culture, a cell-adapted variant of live HAV attenuated vaccine strain H2 was used for consecutive passage for 22 passages in human embryonic lung diploid fibroblast KMB17, during passages the replicating peak cycle was shortened from 28 d to 14 d, the genomes of different passages, 6th passage (HAVH2K7P6), 12th passage (HAVH2K7P12), 18th passage (HAVH2K7P 18) and 22nd passage (HAVH2K7P22), were sequenced and compared to identify the adaptive mutations.
MATERIALS AND METHODS
Cell
Human embryo lung diploid fibroblast strain (KMB17)[25] was used at passage 24-35 in this research.
Virus Strain
Hepatitis A virus strain H2, an attenuated strain at passage K7, was derived from the fecal specimen of a patient with hepatitis A in Hangzhou, China. After isolation and passage in a culture of newborn monkey (Macaca Mulatta) kidney cells, adaptation to grow in human embryo lung diploid fibroblast (KMB17), and serial passage at a low temperature (32 °C) in KMB17 cells, the strain became attenuated[25] and licensed for production of live attenuated HAV vaccine.
H2 strain passage and rapidly replicating adaptation in KMB17 cells
KMB17 cells were grown in 25 cm2 flask (Nunc, Weisbaden, germany) using Eagle’ Minimal Essential Medium supplemented with penicillin (100 U/mL), streptomycin (100 μg/mL), and 10% heat-inactivated newborn calf serum, and passaged every four days. HAV H2M20K7 with 28-day replication cycle were seeded onto KMB17 confluent monolayer cells, after 37 °C absorption for 2 h, maintenance medium with 2% newborn calf serum were added, and seeded cells were cultured at 35 °C for 14 d. The virus was harvested at the 14th day, and then seeded onto the monolayer cells again, the virus was serially passaged for 22 passages with 14-day cycle. The antigen titers and infectious titers were detected with ELISA[26,27]. The virus at 6th, 12th, 18th, 22nd passage were designated as HAVH2K7P6 (P6), HAVH2K7P12 (P12), HAVH2K7P18 (P18) and HAVH2K7P22 (P22), respectively. The respective genomes were cloned and sequenced.
One-step growth dynamics
KMB17 cells were infected with a multiplicity of infection (MOI) of 5. The titer was assayed by inoculating the cells grown in 25 cm2 flask (Nunc, Weisbaden, germany), and infection was checked 4 wk after inoculation by ELISA[26,27].
Primers and sequencing strategy
Primers were designed according to the sequence of H2K7[29] with Goldkey software (Table 1), The sequencing strategy was showed as Figure 1.
Table 1.
The primers used for amplification of HAV genomic RNA
| Cloned fragments | Primers | Sequences |
| A (0.8 kb) | A1 | 5'-CGCCGGCGTTCAAGAGGGGTGTCCGGAG-3' |
| A2 | 5'-GAATCTCAATGCCAAATCTTGC-3' | |
| B (0.5 kb) | B1 | 5'-TCTGAGGTACTCAGGGGC-3' |
| B2 | 5'-CAGTCAATGATGCTATAGAACC-3' | |
| C (1.1 kb) | C1 | 5'-CCAACAGGGGGGATTGATC-3' |
| C2 | 5'-CGTTAGAAGGAGAGGTCAATC-3' | |
| D (1.0 kb) | D1 | 5'-CCCTGGATTTCTGACACTCC-3' |
| D2 | 5'-CAGTGGATAACATGGCATTTG-3' | |
| E (1.1 kb) | E1 | 5'-GTCTGTCACAGAACAATCAGAG-3' |
| E2 | 5'-GATCCCAGAACAGATATCTCTTAA-3' | |
| F (1.2 kb) | F1 | 5'-GTTAAGAGATATCTGTTCTGGATC-3' |
| F2 | 5'-CCATCCTCCAACGAGCACTCC-3' | |
| G (1.2 kb) | G1 | 5'-CAGTTCTTTAGTCATGACAGTTG-3' |
| G2 | 5'-GCCATTGGATCAATTTCAGC-3' | |
| H (1.1 kb) | H1 | 5'-GAGTCCCATTTATCATCACA-3' |
| H2 | 5'-GTCCAATCAGATCAAGATTATC-3' | |
| I (0.5 kb) | I1 | 5'-GATTCTCTGTTATGGAGATG-3' |
| I2 | 5'-TTTTTTTTTTTTTTTTTTTTTATTT-3' |
(1): A-I represent 9 amplified fragments of HAV; (2) 1 and 2 represent positively and negatively oriented primers
Figure 1.
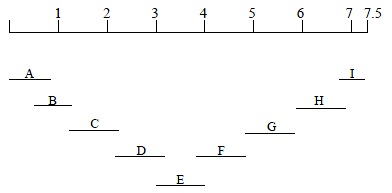
Sequencing strategy of HAV genome. A-I represent 9 amplified fragments of HAV
Antigen-capture PCR amplification of the genomes
cDNA synthesis and cloning Antigen-capture PCR were used to prepare cDNA of genome of different passages[29] with some modifications. Sterile 0.5-mL conical tube (Ependorf) was coated 100 μL of human anti-HAV IgG diluted 1:1000 in 50 mM sodium carbonate buffer (pH9.6). After 4 h of incubation at 37 °C, the unbound IgG was removed, and 150 μL of 1% bovine serum albumin (Sigma) diluted in the buffer was added. After 1 h at 37 °C, the tube was washed three times with 300 μL of PBS (pH7.4) containing 0.05% Tween 80. purified HAV (100 μL) was then added, and the preparation was incubated overnight at 4 °C. The tube was washed six times with 500 μL of a 40 mM Tris (pH8.4)-40 mM KCl-7 mM MgCl2 solution. Then 100 μL of water was added and tube was heated to 95 °C for 5 min to disrupt captured viruses and melt any second structures within the viral RNA. The first strand cDNA was synthesized using SuperScriptTM Preamplification System kit (Gibco, Life Technologies), following the instruction by manufacturer. The clones of different fragments were performed by PCR in a mixture (50 μL) including 5 μL 10 × LA PCR buffer, 8 μL 2.5 mM dNTPs, 2 μL template of RT-PCR products, 300 nM positive-sense primer, 300 nM negative-sense primer and 2.5 U LA Taq DNA polymerase (TaKaRa), additing water to 50 μL. The reaction mixture was subjected to 95 °C for 5 min, then 30 automated cycles of denaturation at 95 °C for 30 s, annealing at 50 °C for 30 s, and extention at 72 °C for 1 min or 1 min 30 s., The final reaction was incubated at 72 °C for 10 min. After the PCR products were recovered and purified, the fragments were ligated into pGEM-T Vector (Promega). The resulting products were transformed into competent E. coli DH5α cells. Three ampicillin-resistant clones were picked out for each fragment. The size of inserts in positive clones was estimated with restriction enzyme site at either side of the inserted fragment. Rapid plasmid preparations were made with the Wizard plasmid purification kit (Promega).
DNA sequencing and analysis
Sequencing strategy was shown in Figure 1. Oligonucleotide primers specific for HAV and primers corresponding to the T7/SP6 promoter region of pGEM®-T Vector were used to sequence the Inserted and identified HAV fragment. A Taq DyeDeoxy Terminator Cycle sequencing kit and a 377 DNA sequencer (Perkin Elmer) were used to determine nucleotide sequences. To eliminate the possibility of errors in the sequence due to Taq polymerase for PCR, at least three clones of each amplified fragment derived from two individual PCR products were sequenced. Also to correctly determine the sequence of extreme 5 terminus of HAV genome, a 5'RACE reaction was used to obtain the a cDNA fragment from 5'NTR of genome with 5’-Full RACE Core Set (TaKaRa). Analysis, alignment and translation in the amino acids of the obtained nucleotide sequences were done using the sequence analysis program OMEGA (Oxford Molecular).
RESULTS
Dynamical characteristics of adaptive enhancement of H2K7 replication in KMB17 cells
Although HAV has been adapted to grow in cell culture, even cell culture adapted variants grow considerably slowly with low virus yields and characterized by an asynchronous onset of replication[30,31]. HAV usually established ersistent infection in cell culture with protracted replication cycle, but replication cycle of maximal accumulation of HAV in cell culture was dually shortened with the increase of passages, even cytopathic effect (CPE) appeared[32-35]. Attenuated HAV strain H2K7 didot cause CPE in KMB17 cells, its replicating peak of was days, the infectious titer reached. 0 LgCCID50ml-1. In this study, attenuated strain H2 at passage K7 were passaged in KMB17 cells every fourteen days. At last the change of incubation cycle, from 28 d to 14 d, resulted in the increase of both antigenic and infectious titers. At first passage of adaptation (P1) the antigenic and infectious titers were only 1:16 ELISA units (ELI.U) and 5.83 LgCCID50ml-1, respectively, at P6 the antigenic and infectious titers gradually increased o 1:64 ELI.U and 6.77 LgCCID50ml-1, respectively, at P12 obvious enhancement of antigenic and infectious titers (1:256 ELI.U and 7.0 LgCCID50ml-1, respectively) occured, More enhancement appeared at P18 with 1:512 ELI.U and 7.33 LgCCID50ml-1, respectively, at P22 antigenic and infectious titers reached the highest levels of 1:1024 ELI.U and 7.83 LgCCID50ml-1, respectively (Table 2). During the whole passages no CPE appeared. Furthermore, one-step growth dynamics showed that at P22 at days 2, 4, 6, 8, 10, 12 14 of culture antigenic and infectious titers gradually increased, at day 14 antigenic and infectious titers reached the highest levels of 1:1024 ELI.U and 7.8 LgCCID50ml-1, respectively, afterwards, the infectious titer gradually decreased, but antigenic titer remained unchanged until day 26 (Table 3). The increases of antigenic and infectious titers with consecutive passage showed that strain H2K7 had been further adapted successfully in KMB17 cells with shortened replication cycle of 28 d to 14 d.
Table 2.
Titers of different passages of HAVH2K7 on KMB17 for 14 d.
| Passages | Antigen titers | Infectious titers (LgCCID50/mL) |
| 1 | 1:16 | 5.83 |
| 2 | 1:8 | 5.5 |
| 3 | 1:16 | 5.67 |
| 4 | 1:32 | 6.0 |
| 5 | 1:32 | 6.5 |
| 6 | 1:64 | 6.77 |
| 7 | 1:64 | 6.67 |
| 8 | 1:64 | 6.5 |
| 9 | 1:64 | 6.67 |
| 10 | 1:128 | 6.83 |
| 11 | 1:128 | 7.0 |
| 12 | 1:256 | 7.0 |
| 13 | 1:256 | 7.17 |
| 14 | 1:256 | 7.0 |
| 15 | 1:256 | 7.17 |
| 16 | 1:256 | 7.0 |
| 17 | 1:512 | 7.17 |
| 18 | 1:512 | 7.33 |
| 19 | 1:512 | 7.5 |
| 20 | 1:512 | 7.67 |
| 21 | 1:1024 | 7.67 |
| 22 | 1:1024 | 7.83 |
Table 3.
One-step growth dynamics of HAVH2K7P22 on KMB17 cells
| Post inoculation days | Antigen titers | Infectious titers (LgCCID50/mL) |
| 2 | 1:8 | ND* |
| 4 | 1:16 | 6.0 |
| 6 | 1:32 | 6.67 |
| 8 | 1:128 | 7.17 |
| 10 | 1:512 | 7.5 |
| 12 | 1:1024 | 7.8 |
| 14 | 1:1024 | 7.17 |
| 16 | 1:1024 | 7.0 |
| 18 | 1:1024 | 7.0 |
| 20 | 1:1024 | 6.83 |
| 22 | 1:1024 | 7.0 |
| 24 | 1:1024 | 6.8 |
| 26 | 1:2048 | 6.5 |
*Not determined
Mutational Characteristics in Consecutive Passage of Rapid Replication of Strain H2 during Cell Culture Adaptation
The process of adaptation of HAV in cell culture was also a process of serials of mutations in genome and results in attenuation[11]. The rapidly adaptive passages of H2K7 in KMB17 cells caused the change of replication cycle, from 28 d to 14 d. The maximal virus yields appeared at 14 d at P22 (Table 3). In order to investigate whether the shortened replication cycle of H2K7P1-22 in cell adaptation was reflected by mutational changes in the genome, which was thought to be responsible for adaptation of HAV, and whether related mutations were responsible for the adjustment of shortened replication cycle, we sequenced and compared the entire genome of four passages (P6, P12, P18, P22), the mutations correlating with adaptation at different passages were identified. The results revealed that mutational numbers in genomes of different passages increased with adaptive passages, and mutations scattered throughout the whole genome. There were only 6 nucleotides mutations appeared in the genome of P6, and nucleotide identity was up to 99.93% in comparison with that of H2K7, as shown in (Table 4), two mutations occurred in VP2 coding region (at nucleotide position 858 with exchange from G to U, resulting in amino acid exchange from A to S, at nucleotide position 1178 with silent exchange from C to U, resulting in no amino acid exchange), one mutation in 2B coding region (at nucleotide position 4022 with exchange from U to C, resulting in amino acid exchange from C to I), one mutation in 2C coding region (at nucleotide position 4968 with exchange from A to C, resulting in amino acid exchange from N to H), one in 3A coding region (at nucleotide position 5193 with exchange from C to T, resulting in amino acid exchange from R to C), one in 3D coding region (at nucleotide position 7256 with silent exchange from A to U). When H2K7 was passaged up to P12, 7 mutations appeared, in addition to 6 same mutations with P6, there was a new mutation appeared in 5'NTR at nucleotide position 591 resulting in a nucleotide exchange from A to G. P18 had 10 nucleotide mutations occurred in the entire genome, among 10 mutations 7 mutational changes were the same with P12, three new mutational changes appeared in genome, one in 5'NTR (one at nucleotide position 33 with nucleotide exchange from C to U), one in 3C coding region (at nucleotide position 5715 with exchange from A to G, resulting in amino acid exchange from U to A), one in 3D coding region (at nucleotide position 6427 with exchange from U to G, resulting in amino acid exchange from V to G). At P22 there were 18 nucleotide changes appeared in the genome, on the basis of P18 additional 8 nucleotide mutations appeared, two in 5'NTR (at nucleotide position263 with exchange from U to C, and 378 with exchange from U to C), three in 2C coding region (at nucleotide position 4558 with exchange from A to C, resulting in amino acid exchange from Q to R, at nucleotide position 4802 with silent exchange from U to C, resulting in no amino acid exchange, at nucleotide position 4949 with silent exchange from A to U), one in 3A coding region (at nucleotide position 5217 with exchange from G to U, resulting in amino acid exchange from A to S), one in 3C coding region (at nucleotide position 5336 with silent exchange from G to A), one in 3D coding region (at nucleotide position 7256 with silent exchange from A to U).
Table 4.
Differences in the genome sequence and amino acids of the HAV H2 K7 with HAV H2K7 P6, HAV H2K7 P12, HAV H2K7 P18 and HAV H2 K7 P22
| Nucleotide position | Location |
Nucleotide |
Amino acids |
||||||||
| K7 | K7P6 | K7P12 | K7P18 | K7P22 | K7 | K7P6 | K7P12 | K7P18 | K7P22 | ||
| 33 | 5'NTR | C | C | C | U | U | |||||
| 263 | 5'NTR | U | U | U | U | C | |||||
| 378 | 5'NTR | U | U | U | U | C | |||||
| 591 | 5'NTR | A | A | G | G | G | |||||
| 646 | 5'NTR | A | A | A | U | U | |||||
| 858 | VP2 | G | U | U | U | U | A | S | S | S | S |
| 1178 | VP2 | C | U | U | U | U | I | I | I | I | I |
| 4022 | 2B | T | C | C | C | C | I | I | I | I | I |
| 4558 | 2C | A | A | A | A | C | Q | Q | Q | Q | P |
| 4802 | 2C | U | U | U | U | C | A | A | A | A | A |
| 4949 | 2C | A | A | A | A | U | T | T | T | T | T |
| 4968 | 2C | A | C | C | C | C | N | H | H | H | H |
| 5193 | 3A | C | U | U | U | U | R | C | C | C | C |
| 5217 | 3A | G | G | G | G | U | A | A | A | A | S |
| 5336 | 3C | G | G | G | G | A | L | L | L | L | L |
| 5715 | 3C | A | A | A | G | G | T | T | T | A | A |
| 6427 | 3D | U | U | U | G | G | V | V | G | G | G |
| 7256 | 3D | A | U | U | U | U | A | A | A | A | A |
Identity comparisons of genomes of different passages
Complete nucleotide sequence analysis of four-passage adaptive variants revealed an identity between H2K7 and P6 of 99.93%, between H2K7 and P12 of 99.9%, between H2K7 and P18 of 99.87%, and between H2K7 and P22 of 99.76%. The identity comparisons showed that mutations increased gradually with the increase of passages, but at high passage obvious mutations were concentrated in 5'NTR region, for example, P22 had 18 nucleotide mutations, 5 of 18 mutations appeared in 5'NTR region, the other mutations scattered throughout the coding region, during adaptive process no mutations appeared in VP4 coding region, VP3 coding region, VP1 coding region, 2A coding region, 3'NTR, the identities were 100% (Table 5).
Table 5.
Identitiy comparisons of nucleotide sequence of HAVH2K7 with HAVH2K7P6 and HAVH2K7P22
| Genomic region | HAVH2K7P6 (%) | HAVH2K7P12 (%) | HAVH2K7P18 (%) | HAVH2K7P22 (%) |
| GENOME | 99.93 | 99.9 | 99.87 | 99.76 |
| 5'NTR | 100 | 99.86 | 99.59 | 99.32 |
| VP4 ENCODING | 100 | 100 | 100 | 100 |
| VP2 ENCODING | 99.71 | 99.71 | 99.71 | 99.71 |
| VP3 ENCODING | 100 | 100 | 100 | 100 |
| VP1 ENCODING | 100 | 100 | 100 | 100 |
| 2A ENCODING | 100 | 100 | 100 | 100 |
| 2B ENCODING | 99.74 | 99.74 | 99.74 | 99.74 |
| 2C ENCODING | 99.9 | 99.9 | 99.9 | 99.6 |
| 3A ENCODING | 99.42 | 99.42 | 99.42 | 98.84 |
| 3B ENCODING | 100 | 100 | 100 | 98.53 |
| 3C ENCODING | 100 | 100 | 99.85 | 99.85 |
| 3D ENCODING | 99.94 | 99.86 | 99.86 | 99.86 |
| 3'UTR | 100 | 100 | 100 | 100 |
DISCUSSION
Although the wild-type HAV grew poorly in cell culture, it usually did not cause CPE, and tended to establish persistent infection, after consecutive passages cell-adaptive variants were characterized with higher replication yield, rapid replication cycle and attenuation[19], and nucleotide mutations increased with adaptive passages[17]. On this basis, the development of a live attenuated hepatitis A vaccine (H2 strain) showed good immumogenicity and protective efficacy[36]. a variant of vaccine strain H2 was isolated in the consecutive passages in KMB17 cells without CPE and characterized with rapid replication cycle of 14 d, higher infectious titer of 7.8 LgCCID50ml-1.
From the viewpoint of evolution, cell adaptation of HAV depends on the interaction of HAV and cell, the internal cell environments form a selective pressure on the virus, in order to survive the viral genome gradually mutates to form new phenotype to adapt cell environments, so the accumulations of mutation with increasing passages result in more adaptive phenotype, more rapid replication cycle and higher virus yield. In accordance with this, in a continued passage process of vaccine strain H2 at passage K7 in KMB17 cells, with the increase of infectious titers the mutational numbers of genomes of different passages increased, P6 had 6 mutations with infectious titer of 6.77 LgCCID50ml-1, P12 had 7 mutations with infectious titer of 7.0 LgCCID50ml-1, P18 had 10 mutations with infectious titer of 7.33 LgCCID50ml-1, P22 had 18 mutations with infectious titer of 7.8 LgCCID50ml-1. One-step growth dynamics of P22 also showed that 18 mutations of P22 resulted in shortening the replication cycle from 28 d to 14 d. The results suggested that although H2K7 was already an attenuated strain, the mutations of genome was not sufficient to completely adapt the KMB17, only further mutations increased its adaptive ability in cell KMB17. The sequencing and analysis of genomes of different passages of several cell culture-adapted variants of the HM175 strain of HAV also showed that with the increase of infectious titers the mutational numbers of genomes of different passages increased[9,19,24].
In contrast to the other viruses of picornaviruses, mutations of cell adaptation of HAV scattered throughout the whole genome and cooperatively acted to enhance the growth of virus in cells. Sequencing of cell culture-adapted variants of the HM175 strain of HAV showed that P16 had 19 mutations[24], P35 had 25 mutations[19] and P59 had 42 mutations[9], P6 of cell culture-adapted variants of the H2 strain in KMB17 had 6 mutations, P12 had 7 mutations, P18 had 10, P22 had 18, although different strains in different cells had different mutations, these variants shared common mutations in 5'NTR and in 2B, 2C, 3A, 3B, 3C, 3D coding region of the genomes. Experiments with chimeric infectious cDNA clones indicated that the mutations in both 5'NTR and in 2B, 2C, 3A, 3B, 3C, 3D coding region contributed to the ability of the virus to grow in cells of African green monkey kidney lineage[11,12]. These results revealed that mutations in 5'NTR and in 2B, 2C, 3A, 3B, 3C, 3D coding region of the genomes played more important role than others in cell adaptation.
The 5'NTR of HAV forms a highly ordered secondary and presumably tertiary structure, and contains elements necessary for both viral translation and RNA replication[37], HAV translation is initiated in a cap-independent fashion by a mechanism that involves the binding of the 40 s ribosomal subunit at a site located hundreds of bases downstream of the 5’end of the RNA which has been termed a ribosomal landing pad or an internal ribosome entry segment (IRES)[23,37,38]. Mutations analysis of 5'NTR showed that the IRES of 450 nucleotides was located downstream of nucleotide (nt) 161 and extended to within 40 nt of the first initiator AUG[38-40]. The efficient translation activity by IRES necessitates the interaction of secondary and presumably tertiary RNA structure with a set of specific eukaryotic translation initiation factors and also noncanonical host factors[39-41]. Therefore, it is likely that these 5'NTR mutations enhance translation by altering the affinity of the RNA for cellular proteins that either positively or negatively influence the activity of the IRES.
In our study in the continuous cell adaptation of H2K7, the sequencing showed that increased infectious titers with the increased passages of H2K7 in KMB17 cells correlated well with the increased mutations in 5'NTR. P6 had no mutations in 5'NTR with infectious titer of 6.77 LgCCID50ml-1, P12 had 1 mutation in 5'NTR (nt 591) with infectious titer of 7.0 LgCCID50ml-1, P18 had 3 mutations in 5'NTR (nt 33, 591, 646) with infectious titer of 7.33 LgCCID50ml-1, P22 had 5 mutations in 5'NTR (nt 33, 263, 378, 591, 646) with infectious titer of 7.8 LgCCID50ml-1, in addition to 1 mutation (nt 33 of P18 and P22), all mutations appeared in IRES. According to the viewpoint mentioned above, one mutation (nt 591) in IRES of P12 may change the secondary and presumably tertiary structure of 5'NTR of K7, this changed IRES structure enhance the affinity of K7 RNA with cellular proteins, resulting in the enhancement of translation, among 3 mutations in 5'NTR of P18, 2 mutations in IRES further enhance the affinity of K7 RNA with cellular proteins, resulting in further enhancement of translation, among all mutations in 5'NTR of different passages, 4 mutations in IRES of P22 produce the most efficient affinity of RNA with cellular proteins, yielding the maximal progeny virus. A comparison with the modelof 5'NTR of RNA secondary structure of the HAV genome, proposed by Ali et al[39], suggest that the G to U mutation (nt 646) of 5'NTR of P22, located in the terminal part of the 5'NTR (loop V), could lead to an RNA duplex folding stabilized by an additional basepairing, resulting in further increase of infectious titer. Consistent with our result, Graff et al[42] also showed that increased mutations in IRES of different-passage GBM/Hp8/24 played a role in enhancement of infectious titer and a common G to U mutation (nt 646) of 5'NTR of strain GBM appeared in GBM/Hp8/6, but mutations of different positions of 5'NTR of different HAV strains in different cells may reflect the different interactions of 5'NTR with different cellular proteins. It is worth noting that P6 had no mutation in 5'NTR, but the infectious titer only reached 6.77 LgCCID50ml-1, 0.9 LgCCID50ml-1 more than that at P1, indicating less important role of 5'NTR in early cell adaptation. Consistent with our result, Frings et al[4] found that after 5-passage adaptation of primate cell-adapted hepatitis A virus strain HM175 to its growth in guinea pig cells, the infectious titer reached 6.3 LgCCID50ml-1, but no mutation in 5'NTR. Taken together with our result, it suggest that during early adaptation there were different ways to improve HAV fit with a specific complement of host cell factors and that growth restrictions in defined host cells had not been determined solely by regulatory interactions of cellular factors with 5'NTR sequence, which concerned mainly cap-independent translation initiation.
Previous studies showed that 2B and 2C coding region mutations are essential for cell adaptation of HAV, mutations in other regions have no independent effect, but act cooperatively with mutations in 2B and 2C coding region to enhance replication[43].2B and 2C coding region are found to have 251 and 335 amino acids, respectively. Protein 2B is involved in the rearrangement of cellular membrane[3]. Protein 2C is considered to have helicase and NTPase activities[3]. The functions of 2B and 2C suggest that the mutations in these two regions play important roles in cell adaptation of HAV. During continuous passages from P6-P22 of H2K7, 4 mutations appeared in 2C coding region, two were silent mutations, two resulted in two- amino acid substitutions, one was common in P6, P12, P18 and P22, one mutation at nt 4558 from A to C only appeared in P22, causing amino acid substitution from Q to P, this substitution may enhance the function of 2C, and further increase the infectious titer at P22. In contrast to the previous results[15], in sequence of entire genome of 4 passages (P6, P12, P18, P22), only one mutation appeared in 2B coding region at nt 4022 from U to C, but not resulting in amino acid mutation, this might suggest that 2B protein play less important role than 2C in KMB17 cell adaptation of H2K7.
Mutations in 3A coding region of the isolate in Italy correlated with CPE[35], but our result showed that although mutations in 3A coding region appeared, even a unique amino acid mutation from A to S occurred at P22, no CPE appeared at all passages of H2K7 in KMB17 cell culture. The mechanism remains unknown. The other mutations in 3A, 3C, 3D coding region of P22 may cooperatively act to further enhance the virus replication.
Comparisons of entire genome of P22 with those of continuous passages of GBM and HM175 in different cells showed that although the mutations existed in the same 5’NTR, 2B, 2C, 3A, 3B, 3C, 3D coding regions, most of the mutational sites were different, these differences revealed different interaction of HAV with different cellular proteins under different selective pressures.
From our investigations of sequence analysis of consecutive H2K7 passages and a comparison of their growth characteristics, we can conclude that 18-nt changes scattering over the genome are cooperatively responsible for further adaptation characterized by rapid and shortened replication cycle from 28 d to 14 d in KMB17 cells, the mutations in 2C coding region play more important roles in increase of infectious titer than other mutations, the mutations in 2B coding region show less important role than it usually does in cell adaptation, nucleotide changes in 5’NTR seem not to be relevant during initial stages (before P6) of cell adaptation because of the significant enhancement in infectious titer not correlating with the mutations in this region, but in late passage (P22) mutations in 5'NTR which seem to affect obviously the replication cycle of H2K7 in cell adaptation.
Footnotes
Edited by Wu XN
References
- 1.Yokosuka O. Molecular biology of hepatitis A virus: significance of various substitutions in the hepatitis A virus genome. J Gastroenterol Hepatol. 2000;15 Suppl:D91–D97. doi: 10.1046/j.1440-1746.2000.02141.x. [DOI] [PubMed] [Google Scholar]
- 2.O'Connor JA. Acute and chronic viral hepatitis. Adolesc Med. 2000;11:279–292. [PubMed] [Google Scholar]
- 3.Totsuka A, Moritsugu Y. Hepatitis A virus proteins. Intervirology. 1999;42:63–68. doi: 10.1159/000024967. [DOI] [PubMed] [Google Scholar]
- 4.Frings W, Dotzauer A. Adaptation of primate cell-adapted hepatitis A virus strain HM175 to growth in guinea pig cells is independent of mutations in the 5' nontranslated region. J Gen Virol. 2001;82:597–602. doi: 10.1099/0022-1317-82-3-597. [DOI] [PubMed] [Google Scholar]
- 5.Inoue K, Yoshiba M, Yotsuyanagi H, Otsuka T, Sekiyama K, Fujita R. Chronic hepatitis A with persistent viral replication. J Med Virol. 1996;50:322–324. doi: 10.1002/(SICI)1096-9071(199612)50:4<322::AID-JMV7>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 6.Anderson DA. Cytopathology, plaque assay, and heat inactivation of hepatitis A virus strain HM175. J Med Virol. 1987;22:35–44. doi: 10.1002/jmv.1890220106. [DOI] [PubMed] [Google Scholar]
- 7.Cromeans T, Fields HA, Sobsey MD. Replication kinetics and cytopathic effect of hepatitis A virus. J Gen Virol. 1989;70(Pt 8):2051–2062. doi: 10.1099/0022-1317-70-8-2051. [DOI] [PubMed] [Google Scholar]
- 8.Paul AV, Tada H, von der Helm K, Wissel T, Kiehn R, Wimmer E, Deinhardt F. The entire nucleotide sequence of the genome of human hepatitis A virus (isolate MBB) Virus Res. 1987;8:153–171. doi: 10.1016/0168-1702(87)90026-8. [DOI] [PubMed] [Google Scholar]
- 9.Ross BC, Anderson BN, Edwards PC, Gust ID. Nucleotide sequence of high-passage hepatitis A virus strain HM175: comparison with wild-type and cell culture-adapted strains. J Gen Virol. 1989;70(Pt 10):2805–2810. doi: 10.1099/0022-1317-70-10-2805. [DOI] [PubMed] [Google Scholar]
- 10.Emerson SU, McRill C, Rosenblum B, Feinstone S, Purcell RH. Mutations responsible for adaptation of hepatitis A virus to efficient growth in cell culture. J Virol. 1991;65:4882–4886. doi: 10.1128/jvi.65.9.4882-4886.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Emerson SU, Huang YK, McRill C, Lewis M, Purcell RH. Mutations in both the 2B and 2C genes of hepatitis A virus are involved in adaptation to growth in cell culture. J Virol. 1992;66:650–654. doi: 10.1128/jvi.66.2.650-654.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Day SP, Murphy P, Brown EA, Lemon SM. Mutations within the 5' nontranslated region of hepatitis A virus RNA which enhance replication in BS-C-1 cells. J Virol. 1992;66:6533–6540. doi: 10.1128/jvi.66.11.6533-6540.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chang KH, Brown EA, Lemon SM. Cell type-specific proteins which interact with the 5' nontranslated region of hepatitis A virus RNA. J Virol. 1993;67:6716–6725. doi: 10.1128/jvi.67.11.6716-6725.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tedeschi V, Purcell RH, Emerson SU. Partial characterization of hepatitis A viruses from three intermediate passage levels of a series resulting in adaptation to growth in cell culture and attenuation of virulence. J Med Virol. 1993;39:16–22. doi: 10.1002/jmv.1890390105. [DOI] [PubMed] [Google Scholar]
- 15.Morace G, Pisani G, Beneduce F, Divizia M, Panà A. Mutations in the 3A genomic region of two cytopathic strains of hepatitis A virus isolated in Italy. Virus Res. 1993;28:187–194. doi: 10.1016/0168-1702(93)90135-a. [DOI] [PubMed] [Google Scholar]
- 16.Graff J, Normann A, Feinstone SM, Flehmig B. Nucleotide sequence of wild-type hepatitis A virus GBM in comparison with two cell culture-adapted variants. J Virol. 1994;68:548–554. doi: 10.1128/jvi.68.1.548-554.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Graff J, Kasang C, Normann A, Pfisterer-Hunt M, Feinstone SM, Flehmig B. Mutational events in consecutive passages of hepatitis A virus strain GBM during cell culture adaptation. Virology. 1994;204:60–68. doi: 10.1006/viro.1994.1510. [DOI] [PubMed] [Google Scholar]
- 18.Cohen JI, Ticehurst JR, Purcell RH, Buckler-White A, Baroudy BM. Complete nucleotide sequence of wild-type hepatitis A virus: comparison with different strains of hepatitis A virus and other picornaviruses. J Virol. 1987;61:50–59. doi: 10.1128/jvi.61.1.50-59.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cohen JI, Rosenblum B, Ticehurst JR, Daemer RJ, Feinstone SM, Purcell RH. Complete nucleotide sequence of an attenuated hepatitis A virus: comparison with wild-type virus. Proc Natl Acad Sci USA. 1987;84:2497–2501. doi: 10.1073/pnas.84.8.2497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Funkhouser AW, Purcell RH, D'Hondt E, Emerson SU. Attenuated hepatitis A virus: genetic determinants of adaptation to growth in MRC-5 cells. J Virol. 1994;68:148–157. doi: 10.1128/jvi.68.1.148-157.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang H, Chao SF, Ping LH, Grace K, Clarke B, Lemon SM. An infectious cDNA clone of a cytopathic hepatitis A virus: genomic regions associated with rapid replication and cytopathic effect. Virology. 1995;212:686–697. doi: 10.1006/viro.1995.1526. [DOI] [PubMed] [Google Scholar]
- 22.Graff J, Normann A, Flehmig B. Influence of the 5' noncoding region of hepatitis A virus strain GBM on its growth in different cell lines. J Gen Virol. 1997;78(Pt 8):1841–1849. doi: 10.1099/0022-1317-78-8-1841. [DOI] [PubMed] [Google Scholar]
- 23.Borman AM, Michel YM, Kean KM. Detailed analysis of the requirements of hepatitis A virus internal ribosome entry segment for the eukaryotic initiation factor complex eIF4F. J Virol. 2001;75:7864–7871. doi: 10.1128/JVI.75.17.7864-7871.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jansen RW, Newbold JE, Lemon SM. Complete nucleotide sequence of a cell culture-adapted variant of hepatitis A virus: comparison with wild-type virus with restricted capacity for in vitro replication. Virology. 1988;163:299–307. doi: 10.1016/0042-6822(88)90270-x. [DOI] [PubMed] [Google Scholar]
- 25.Mao JS, Dong DX, Zhang HY, Chen NL, Zhang XY, Huang HY, Xie RY, Zhou TJ, Wan ZJ, Wang YZ. Primary study of attenuated live hepatitis A vaccine (H2 strain) in humans. J Infect Dis. 1989;159:621–624. doi: 10.1093/infdis/159.4.621. [DOI] [PubMed] [Google Scholar]
- 26.Chen T, Zhong G, Yang X, Cao Y. [The hepatitis A virus isolated and adapted in human diploid fibroblast cells (KMB17)] Zhongguo Yixue Kexueyuan Xuebao. 1996;18:29–32. [PubMed] [Google Scholar]
- 27.Cederna JB, Klinzman D, Stapleton JT. Hepatitis A virus-specific humoral and cellular immune responses following immunization with a formalin-inactivated hepatitis A vaccine. Vaccine. 1999;18:892–898. doi: 10.1016/s0264-410x(99)00342-4. [DOI] [PubMed] [Google Scholar]
- 28.Kingsley DH, Richards GP. Rapid and efficient extraction method for reverse transcription-PCR detection of hepatitis A and Norwalk-like viruses in shellfish. Appl Environ Microbiol. 2001;67:4152–4157. doi: 10.1128/AEM.67.9.4152-4157.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kusov YY, Shatirishvili G, Dzagurov G, Gauss-Müller V. A new G-tailing method for the determination of the poly (A) tail length applied to hepatitis A virus RNA. Nucleic Acids Res. 2001;29:E57–E57. doi: 10.1093/nar/29.12.e57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Harmon SA, Summers DF, Ehrenfeld E. Detection of hepatitis A virus RNA and capsid antigen in individual cells. Virus Res. 1989;12:361–369. doi: 10.1016/0168-1702(89)90093-2. [DOI] [PubMed] [Google Scholar]
- 31.Cho MW, Ehrenfeld E. Rapid completion of the replication cycle of hepatitis A virus subsequent to reversal of guanidine inhibition. Virology. 1991;180:770–780. doi: 10.1016/0042-6822(91)90090-x. [DOI] [PubMed] [Google Scholar]
- 32.Cromeans T, Sobsey MD, Fields HA. Development of a plaque assay for a cytopathic, rapidly replicating isolate of hepatitis A virus. J Med Virol. 1987;22:45–56. doi: 10.1002/jmv.1890220107. [DOI] [PubMed] [Google Scholar]
- 33.Lemon SM, Murphy PC, Shields PA, Ping LH, Feinstone SM, Cromeans T, Jansen RW. Antigenic and genetic variation in cytopathic hepatitis A virus variants arising during persistent infection: evidence for genetic recombination. J Virol. 1991;65:2056–2065. doi: 10.1128/jvi.65.4.2056-2065.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nasser AM, Metcalf TG. Production of cytopathology in FRhK-4 cells by BS-C-1-passaged hepatitis A virus. Appl Environ Microbiol. 1987;53:2967–2971. doi: 10.1128/aem.53.12.2967-2971.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Venuti A, Di Russo C, del Grosso N, Patti AM, Ruggeri F, De Stasio PR, Martiniello MG, Pagnotti P, Degener AM, Midulla M. Isolation and molecular cloning of a fast-growing strain of human hepatitis A virus from its double-stranded replicative form. J Virol. 1985;56:579–588. doi: 10.1128/jvi.56.2.579-588.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhao YL, Meng ZD, Xu ZY, Guo JJ, Chai SA, Duo CG, Wang XY, Yao JF, Liu HB, Qi SX, et al. H2 strain attenuated live hepatitis A vaccines: protective efficacy in a hepatitis A outbreak. World J Gastroenterol. 2000;6:829–832. doi: 10.3748/wjg.v6.i6.829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Funkhouser AW, Schultz DE, Lemon SM, Purcell RH, Emerson SU. Hepatitis A virus translation is rate-limiting for virus replication in MRC-5 cells. Virology. 1999;254:268–278. doi: 10.1006/viro.1998.9548. [DOI] [PubMed] [Google Scholar]
- 38.Brown EA, Zajac AJ, Lemon SM. In vitro characterization of an internal ribosomal entry site (IRES) present within the 5' nontranslated region of hepatitis A virus RNA: comparison with the IRES of encephalomyocarditis virus. J Virol. 1994;68:1066–1074. doi: 10.1128/jvi.68.2.1066-1074.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ali IK, McKendrick L, Morley SJ, Jackson RJ. Activity of the hepatitis A virus IRES requires association between the cap-binding translation initiation factor (eIF4E) and eIF4G. J Virol. 2001;75:7854–7863. doi: 10.1128/JVI.75.17.7854-7863.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gosert R, Egger D, Bienz K. A cytopathic and a cell culture adapted hepatitis A virus strain differ in cell killing but not in intracellular membrane rearrangements. Virology. 2000;266:157–169. doi: 10.1006/viro.1999.0070. [DOI] [PubMed] [Google Scholar]
- 41.Yi M, Lemon SM. Replication of subgenomic hepatitis A virus RNAs expressing firefly luciferase is enhanced by mutations associated with adaptation of virus to growth in cultured cells. J Virol. 2002;76:1171–1180. doi: 10.1128/JVI.76.3.1171-1180.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Frings W, Dotzauer A. Adaptation of primate cell-adapted hepatitis A virus strain HM175 to growth in guinea pig cells is independent of mutations in the 5' nontranslated region. J Gen Virol. 2001;82:597–602. doi: 10.1099/0022-1317-82-3-597. [DOI] [PubMed] [Google Scholar]
- 43.Emerson SU, Huang YK, Purcell RH. 2B and 2C mutations are essential but mutations throughout the genome of HAV contribute to adaptation to cell culture. Virology. 1993;194:475–480. doi: 10.1006/viro.1993.1286. [DOI] [PubMed] [Google Scholar]


