Abstract
Cholangiocytes-the epithelial cells which line the bile ducts-are increasingly recognized as important transporting epithelia actively involved in the absorption and secretion of water, ions, and solutes. This recognition is due in part to the recent development of new experimental models. New biologic concepts have emerged including the identification and topography of receptors and flux proteins on the apical and/or basolateral membrane which are involved in the molecular mechanisms of ductal bile secretion. Individually isolated and/or perfused bile duct units from livers of rats and mice serve as new, physiologically relevant in vitro models to study cholangiocyte transport. Biliary tree dimensions and novel insights into anatomic remodeling of proliferating bile ducts have emerged from three-dimensional reconstruction using CT scanning and sophisticated software. Moreover, new pathologic concepts have arisen regarding the interaction of cholangiocytes with pathogens such as Cryptosporidium parvum. These concepts and associated methodologies may provide the framework to develop new therapies for the cholangiopathies, a group of important hepatobiliary diseases in which cholangiocytes are the target cell.
INTRODUCTION
The liver contains two types of epithelia: hepatocytes, accounting for -65% of the liver cell population; and intrahepatic bile duct cells, or cholangiocytes, the epithelial cells that line the intrahepatic biliary tree and account for -5% of the liver cell population.
In the past decade, interest in cholangiocyte pathobiology has exploded due to: (i) the development of new experimental techniques that allow hypotheses related to cholangiocyte biology to be directly addressed (Figure 1); (ii) the recognition that cholangiocytes are critically important to normal liver function, especially solute and water transport, cell-cycle phenomena, cell signaling, and interactions with other cells, matrix components, foreign organisms and xenobiotics; and (iii) the appreciation that cholangiocytes represent the major target of a group of serious genetic and acquired diseases termed the cholangiopathies. In a coordinated series of hypothesis-driven studies, we have explored selective aspects of cellular processing by cholangiocytes focusing on proteins (receptors, channels, exchangers, transporters, junctional proteins, molecular motors, pro/anti-apoptotic molecules) that we hypothesized were likely critically important in cholangiocyte secretion, absorption, intracellular transport, and structural modifications. Thus, we briefly review here a variety of novel in vivo and in vitro experimental models that have allowed us to expand our understanding of how cholangiocytes function and what happens when disease alters their normal physiology. Several more extensive reviews on cholangiocyte pathobiology are referenced for readers interested in more comprehensive reviews.
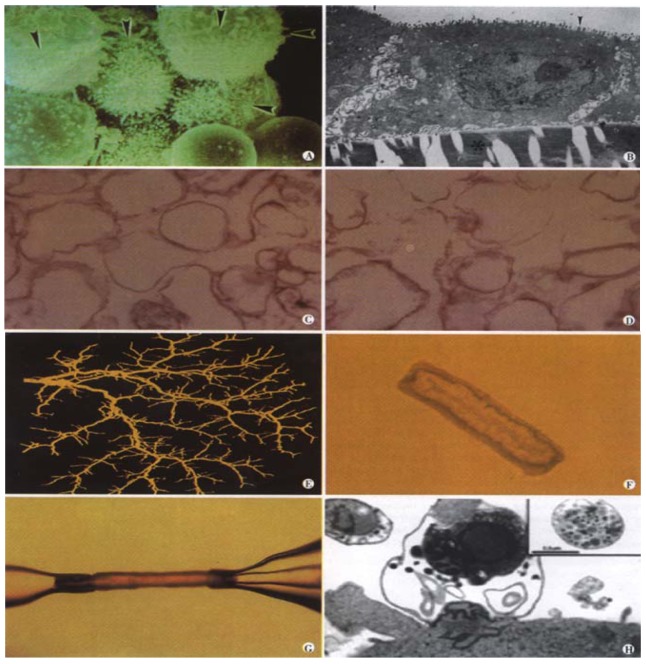
Figure 1.
Experimental in vitro models of biliary epithelia. (a) A scanning electron micrograph of a group of isolated cholangiocytes after separation using immunomagnetic beads. Note that the prominent microvilli (arrowheads) are limited to one side of the cells. Mag = 4400. (b) A transmission electron micrograph cross-section of normal rat cholangiocytes in culture demonstrates characteristics of polarized cells with apical microvilli (arrowheads) and numerous basolateral intercellular interdigitations near the collagen coated filter denoted by *, (Bar = 2 mm, Mag = 7500). (c) (d) A transmission electron micrograph of apical (c) and basolateral (d) plasma membrane domains revealed similar homogenous vesiculated membranes of varied shapes and sizes without apparent contamination of other organelles (Bar = 0.5 mm, Mag = 22500). (e) A three-dimensional reconstructed image of the intrahepatic biliary tree isolated from normal rat liver. (f) A light micrograph of an unstained isolated bile duct unit from rat liver. After overnight culture, the two ends seal forming an enclosed unit. A single layer of epithelial cells with a thin outer layer of connective tissue surrounds the lumen. (g) A microperfused intrahepatic bile duct unit isolated from rat liver, manually dissected and cannulated with micropipettes. (h) Transmission electron micrograph of C. parvum infection of cultured human cholangiocytes. A parasitophorous vacuole contains a developing parasite stage which is intracellular but extracytoplasmic. A macrogamet is shown in the inset, demonstrating development of sexual stages of the parasite. Bar = 1 mm.
IN VIVO MODELS
The rat biliary tree has been shown to undergo selective proliferation in response to different experimental stimuli such as bile duct ligation (BDL)[1], 70% hepatectomy[2], carbon tetrachloride treatment[3], and feeding of α-naphthylisothiocyanate (ANIT)[4,5]. As best we know, the proliferated cholangiocytes retain a normal cholangiocyte phenotype. The bile duct ligated rat model has been useful in initiating studies on the effect of hormones on bile secretion. Infusion of secretin and somatostatin results in a choleretic and cholestatic response, respectively, in the bile duct ligated but not sham-operated rat, due not only to an increased number of cells but an increased expression of the receptors for secretin and somatostatin on individual cholangiocytes[6-8]. Much less is known about how the mouse biliary tree responds to hormones. To further explore the regulatory mechanisms of ductal bile secretion, it was necessary to develop additional novel in vitro experimental models.
IN VITRO MODELS
Freshly Isolated Cells
The development of in vitro models of biliary epithelia essentially began with the ability to isolate cholangiocytes of high purity from normal rat, mouse and human liver[9,10]. This experimental model allowed direct studies on the effects of hormones on cholangiocytes which demonstrated among other things, that secretin stimulated exocytosis via a cyclic AMP mechanism, and that this effect was blocked by somatostatin[11].
The technique of counter-flow elutriation has allowed refinement of cell isolation techniques from normal or BDL rats[12,13] by allowing separation of subpopulations of cholangiocytes which differ in size. Using this model, we have provided evidence that these small, medium and large cholangiocytes originate from different portions of the intrahepatic biliary ductal system. Using molecular and physiological approaches, we have also demonstrated that these subpopulations of cholangiocytes differ in their transport and proliferative capabilities[12,13].
Cholangiocyte cDNA Library
A unique cDNA library has been constructed from highly purified cholangiocytes isolated from rats subjected to bile duct ligation for 2 weeks[14]. Total cellular RNA was extracted from cholangiocytes and poly(A)+ mRNA isolated. Subsequently, the poly(A)+ mRNA was reverse transcribed and directionally cloned. The cholangiocyte cDNA library allows screening and sequencing of positive clones for numerous molecules yet to be identified.
Cultured Cells
Freshly isolated cells maintained in short-term culture provided the opportunity to perform patch-clamp studies yielding novel insights into the electrophysiology of cholangiocytes[15]. Established long-term cultured cholangiocytes can be grown on semi-permeable cell culture filters by which they quickly reach confluence, maintain morphologic polarity and develop adequate transepithelial electrical resistance, making them a prototype for use in transport studies. This model has been utilized to characterize the uptake of glucose and bile acids and to study water transport[16-19].
Isolated Organelles
In order to perform more rigorous transport studies and to generate accurate kinetic transport parameters (i.e., Km and Vmax), we developed techniques for isolating vesicles enriched in either the apical or the basolateral domain of cholangiocytes starting either with whole rat liver or with cholangiocytes in culture[20,21]. An initial application of these vesicles was to generate kinetic values for sodium-dependent taurocholate uptake, a process that we demonstrated occurs in apical but not basolateral vesicles[17]. This tool allows continued studies to localize and functionally evaluate transport processes in cholangiocytes.
Intrahepatic Bile Duct Units
Experiments using intact intrahepatic bile duct units isolated by mechanical and enzymatic techniques from normal rats to study biliary epithelial transport physiology have been previously described[22]. An advantage of this model is that we can not only control the lumenal contents (by manipulating components of the perfusate) but we can independently and simultaneously modify the basolateral milieu (by manipulating components of the bathing buffer). With this approach, we were able to detect changes in intralumenal pH and electrolyte concentrations in response to agonists. We could also demonstrate water transport across this epithelial barrier in response to osmotic gradients, the characteristics of which (kinetics, temperature independence and mercury sensitivity) all suggested the presence of water selective channel proteins (i.e., aquaporins) (AQP) on the membranes of cholangiocytes. Using quantitative computer-assisted image analysis to measure expansion and reduction of lumenal area as a reflection of water movement, we have demonstrated that water movement across the bile duct units is transcellular and channel-mediated[13].
We have subsequently expanded this model using a microperfusion technique and an epifluorescence detection system[24]. With this modification, we have demonstrated the movement of water into (secretion) and out of (absorption) the lumen of the perfused ducts in response to inward and outward osmotic gradients. The calculation of both net water movement (Jv) and osmotic water permeability (Pf) provide evidence that the measured bi-directional fluxes reflect water movement through water channels.
In addition, we have demonstrated that isolated bile duct units actively absorb solutes such as bile acids and glucose, and transport ions such as bicarbonate. We have also shown that lumenal perfusion of ATP and other nucleotides activates P2Y ATP receptors on the apical cholangiocyte plasma membrane and induces increases in [Ca2+]i and net ductular alkalization, suggesting that ductal bile secretion is regulated by these signaling molecules[25].
This technique has now been adapted to the mouse in which we can reproducibly isolate and microperfuse intact bile duct units from normal mouse liver with the anticipated application to transgenic or knockout mouse models[26]. Transgenic mice continue to be developed in which there is a selective knockout of one or more aquaporin water channels[27]. The isolated and perfused bile duct unit model would allow us to test the hypothesis that knockout mice lacking AQP1 and AQP4 water channels or perhaps other naturally expressed aquaporins may have substantially reduced choleretic and cholestatic responses to hormones since the flux of water molecules through these water channels should be absent.
The isolation of intact, polarized intrahepatic bile duct units from both rat and mouse allows the direct study of secretory and absorptive activities of the bile ducts in a way which most closely approximates the normal biliary ductal system.
Three-Dimensional Modeling
Although cholangiocyte functional and morphological heterogeneity likely contributes to the selective involvement of different portions of the biliary tree in the cholangiopathies, our understanding of the nature and mechanisms for normal and abnormal anatomical remodeling of the biliary tree is limited. To better define the heterogeneous nature of the biliary tree, we utilized a computer-aided three-dimensional imaging technique, first described in a study of the normal human biliary tree[28], to perform quantitative anatomical studies of the rat intrahepatic biliary system[29].
Computer generated three-dimensional reconstruction of the intrahepatic biliary tree using microscopic-computed tomography scanning and sophisticated software allowed us to generate key biliary tract dimensions (length, surface area, duct diameter, volume) and branching patterns (distance from the junction of intra- and extrahepatic ducts, number of bile duct branches and branching angles).
In various forms of liver disease, including the cholangiopathies, proliferation of cholangiocytes is a common pathological response[1,30,31]. The anatomical basis and remodeling process which occurs in response to various stimuli remain unclear. We have since applied the three-dimensional reconstruction of the biliary tree to rats in whom selective cholangiocyte proliferation was induced by ANIT feeding[4,5]. The anatomical remodeling and quantitative observations after selective cholangiocyte proliferation suggest that the proliferation process involves sprouting of new side branches. Recently three-dimensional modeling has been applied to generate data for the hepatic artery and portal vein within the same liver (Masyuk, LaRusso unpublished). This descriptive study allowed key findings on the length of vascular segments, diameter of blood vessel segments and volume of the hepatic artery and portal vein, associated with experimentally-induced cholangiocyte proliferation.
Three-dimensional reconstruction will provide complementary data that, at a minimum, will yield structural information on biliary tract architecture and biliary mapping (i.e.,which branches of the biliary tree are involved in absorption or secretion, the mechanisms by which ducts proliferate in response to injury, and the impact of these modifications on the peribiliary vasculature.) The significance of these studies relates not only to the intrinsic value of understanding cholangiocyte physiology but also to providing a biologic rationale for why onlycertain segments of the biliary tree are involved in the individual cholangiopathies. Primary biliary cirrhosis, for example, leads to destruction of interlobular bile ducts, while intrahepatic cholestasis induced by drugs affects principally the cholangiocytes that line small bile ducts[30,32,33].
In Vitro Infection Model of Biliary Cryptosporidiosis
Using monolayers of human cholangiocytes derived from normal liver and immortalized by SV40 transformation, we developed an in vitro infection model of biliary cryptosporidiosis[34]. Cryptosporidiosis is an infectious disease caused by Cryptosporidium parvum (C. parvum), an emerging parasite which causes self-limited diarrhea in immunocompetent subjects and potentially life-threatening syndromes in immunocompromised individuals, primarily those with acquired immunodeficiency syndrome (AIDS). Despite the magnitude and severity of cryptosporidial infection, the pathogenesis is poorly understood, and there is currently no effective therapy. Using this novel infection model, we found that C. parvum sporozoites (derived from oocysts excysted in vitro) attach to the apical surface of biliary epithelia, invade the cells, reside in a parasitophorous vacuole, and undergo both sexual and asexual development.
C. parvum attachment to cholangiocytes involves interactions between specific glycoproteins on cholangiocytes and C. parvum sporozoite lectins while the invasion into cholangiocytes works through actin-dependent membrane spreading mediated by cortactin and RhoGTP-binding proteins[34-36]. While C. parvum is cytopathic to uninfected cells adjacent to infected cholangiocytes via Fas/FasL-dependent apoptosis, the organism prevents cell death of infected cells by inhibiting apoptosis via activation of NF-κB[37,38]. This model provides a useful system for the development of novel therapeutic strategies for C. parvum induced enterology and AIDS-cholangiopathy.
CONCLUSION
Advances in medical knowledge most often are preceded by advancements in technology and experimental models. Results from experiments using these new models and methods have clarified which flux proteins are expressed in cholangiocytes, their intracellular topography and segmental distribution, what molecules control their cellular compartmentalization, and their physiologic relevance to ductal bile formation. In addition, the information has provided a theoretical framework for development of novel therapeutic strategies for the cholangiopathies, a group of cholestatic genetic/acquired hepatobiliary diseases in which the cholangiocyte is the principal target of diverse destructive processes.
Abbreviations
ANIT a-naphthylisothiocyanate
AQP aquaporin
BDL bile duct ligation
C. parvum Cryptosporidium parvum
ACKNOWLEDGEMENTS
We greatly appreciate the secretarial assistance of Deb Hintz in preparation of this manuscript.
Footnotes
Supported by grants DK24031 and DK57993 (N. F. LaRusso) from the National Institutes of Health and by the Mayo Foundation
Edited by Zhu LH
References
- 1.Alpini G, Phillips JO, LaRusso NF. The biology of biliary epithelia.Edited by Arias IM, Boyer JL, Fausto N, Jakoby WB, Schachter DA, Shafritz DA. The Liver: Biology and Pathobiology. New York: Raven Press. 1994:623–653. [Google Scholar]
- 2.Lesage G, Glaser SS, Gubba S, Robertson WE, Phinizy JL, Lasater J, Rodgers RE, Alpini G. Regrowth of the rat biliary tree after 70% partial hepatectomy is coupled to increased secretin-induced ductal secretion. Gastroenterology. 1996;111:1633–1644. doi: 10.1016/s0016-5085(96)70027-6. [DOI] [PubMed] [Google Scholar]
- 3.LeSage GD, Benedetti A, Glaser S, Marucci L, Tretjak Z, Caligiuri A, Rodgers R, Phinizy JL, Baiocchi L, Francis H, et al. Acute carbon tetrachloride feeding selectively damages large, but not small, cholangiocytes from normal rat liver. Hepatology. 1999;29:307–319. doi: 10.1002/hep.510290242. [DOI] [PubMed] [Google Scholar]
- 4.Desmet VJ, Krstulović B, Van Damme B. Histochemical study of rat liver in alpha-naphthyl isothiocyanate (ANIT) induced cholestasis. Am J Pathol. 1968;52:401–421. [PMC free article] [PubMed] [Google Scholar]
- 5.Kossor DC, Goldstein RS, Ngo W, DeNicola DB, Leonard TB, Dulik DM, Meunier PC. Biliary epithelial cell proliferation following alpha-naphthylisothiocyanate (ANIT) treatment: relationship to bile duct obstruction. Fundam Appl Toxicol. 1995;26:51–62. doi: 10.1006/faat.1995.1074. [DOI] [PubMed] [Google Scholar]
- 6.Alpini G, Ulrich CD, Phillips JO, Pham LD, Miller LJ, LaRusso NF. Upregulation of secretin receptor gene expression in rat cholangiocytes after bile duct ligation. Am J Physiol. 1994;266:G922–G928. doi: 10.1152/ajpgi.1994.266.5.G922. [DOI] [PubMed] [Google Scholar]
- 7.Tietz PS, Alpini G, Pham LD, Larusso NF. Somatostatin inhibits secretin-induced ductal hypercholeresis and exocytosis by cholangiocytes. Am J Physiol. 1995;269:G110–G118. doi: 10.1152/ajpgi.1995.269.1.G110. [DOI] [PubMed] [Google Scholar]
- 8.Tietz PS, Hadac EM, Miller LJ, LaRusso NF. Upregulation of secretin receptors on cholangiocytes after bile duct ligation. Regul Pept. 2001;97:1–6. doi: 10.1016/s0167-0115(00)00109-9. [DOI] [PubMed] [Google Scholar]
- 9.Ishii M, Vroman B, LaRusso NF. Isolation and morphologic characterization of bile duct epithelial cells from normal rat liver. Gastroenterology. 1989;97:1236–1247. doi: 10.1016/0016-5085(89)91695-8. [DOI] [PubMed] [Google Scholar]
- 10.Vroman B, LaRusso NF. Development and characterization of polarized primary cultures of rat intrahepatic bile duct epithelial cells. Lab Invest. 1996;74:303–313. [PubMed] [Google Scholar]
- 11.Kato A, Gores GJ, LaRusso NF. Secretin stimulates exocytosis in isolated bile duct epithelial cells by a cyclic AMP-mediated mechanism. J Biol Chem. 1992;267:15523–15529. [PubMed] [Google Scholar]
- 12.Alpini G, Roberts S, Kuntz SM, Ueno Y, Gubba S, Podila PV, LeSage G, LaRusso NF. Morphological, molecular, and functional heterogeneity of cholangiocytes from normal rat liver. Gastroenterology. 1996;110:1636–1643. doi: 10.1053/gast.1996.v110.pm8613073. [DOI] [PubMed] [Google Scholar]
- 13.Alpini G, Ulrich C, Roberts S, Phillips JO, Ueno Y, Podila PV, Colegio O, LeSage GD, Miller LJ, LaRusso NF. Molecular and functional heterogeneity of cholangiocytes from rat liver after bile duct ligation. Am J Physiol. 1997;272:G289–G297. doi: 10.1152/ajpgi.1997.272.2.G289. [DOI] [PubMed] [Google Scholar]
- 14.Pham L, Lazaridis K, LaRusso NF, deGroen PC. Development and character-ization of a cDNA library prepared from isolated rat cholangiocytes. Gastroenterology. 1997;112:A1358. [Google Scholar]
- 15.Balan V, Larkin J, Pham L, Vroman B, McNiven MA, LaRusso NF. Identifica-tion of Rab3d in intrahepatic bile duct epithelial cells: Implications for exocy-tosis and bile secretion. Gastroenterology. 1994;106:A863. [Google Scholar]
- 16.Lazaridis KN, Pham L, Vroman B, de Groen PC, LaRusso NF. Kinetic and molecular identification of sodium-dependent glucose transporter in normal rat cholangiocytes. Am J Physiol. 1997;272:G1168–G1174. doi: 10.1152/ajpgi.1997.272.5.G1168. [DOI] [PubMed] [Google Scholar]
- 17.Lazaridis KN, Pham L, Tietz P, Marinelli RA, deGroen PC, Levine S, Dawson PA, LaRusso NF. Rat cholangiocytes absorb bile acids at their apical domain via the ileal sodium-dependent bile acid transporter. J Clin Invest. 1997;100:2714–2721. doi: 10.1172/JCI119816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lazaridis KN, Tietz P, Wu T, Kip S, Dawson PA, LaRusso NF. Alternative splicing of the rat sodium/bile acid transporter changes its cellular localization and transport properties. Proc Natl Acad Sci USA. 2000;97:11092–11097. doi: 10.1073/pnas.200325297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marinelli RA, Pham LD, Tietz PS, LaRusso NF. Expression of aquaporin-4 water channels in rat cholangiocytes. Hepatology. 2000;31:1313–1317. doi: 10.1053/jhep.2000.7986. [DOI] [PubMed] [Google Scholar]
- 20.Tietz PS, Holman RT, Miller LJ, LaRusso NF. Isolation and characterization of rat cholangiocyte vesicles enriched in apical or basolateral plasma membrane domains. Biochemistry. 1995;34:15436–15443. doi: 10.1021/bi00047a007. [DOI] [PubMed] [Google Scholar]
- 21.Tietz P, Levine S, Holman R, Fretham C, LaRusso NF. Characterization of apical and basolateral plasma membrane domains derived from cultured rat cholangiocytes. Anal Biochem. 1997;254:192–199. doi: 10.1006/abio.1997.2431. [DOI] [PubMed] [Google Scholar]
- 22.Roberts SK, Kuntz SM, Gores GJ, LaRusso NF. Regulation of bicarbonate-dependent ductular bile secretion assessed by lumenal micropuncture of isolated rodent intrahepatic bile ducts. Proc Natl Acad Sci USA. 1993;90:9080–9084. doi: 10.1073/pnas.90.19.9080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cova E, Gong A, Marinelli RA, LaRusso NF. Water movement across rat bile duct units is transcellular and channel-mediated. Hepatology. 2001;34:456–463. doi: 10.1053/jhep.2001.27092. [DOI] [PubMed] [Google Scholar]
- 24.Masyuk AI, Gong AY, Kip S, Burke MJ, LaRusso NF. Perfused rat intrahepatic bile ducts secrete and absorb water, solute, and ions. Gastroenterology. 2000;119:1672–1680. doi: 10.1053/gast.2000.20248. [DOI] [PubMed] [Google Scholar]
- 25.Dranoff JA, Masyuk AI, Kruglov EA, LaRusso NF, Nathanson MH. Polarized expression and function of P2Y ATP receptors in rat bile duct epithelia. Am J Physiol Gastrointest Liver Physiol. 2001;281:G1059–G1067. doi: 10.1152/ajpgi.2001.281.4.G1059. [DOI] [PubMed] [Google Scholar]
- 26.Gong AY, Masyuk AI, Splinter PL, LaRusso NF. Development and initial ap-plication of a microperfusion model of intrahepatic mouse bile duct units. Hepatology. 2000;32(4,Pt2):433A. [Google Scholar]
- 27.Verkman AS, Yang B, Song Y, Manley GT, Ma T. Role of water channels in fluid transport studied by phenotype analysis of aquaporin knockout mice. Exp Physiol. 2000;85 Spec No:233S–241S. doi: 10.1111/j.1469-445x.2000.tb00028.x. [DOI] [PubMed] [Google Scholar]
- 28.Ludwig J, Ritman EL, LaRusso NF, Sheedy PF, Zumpe G. Anatomy of the human biliary system studied by quantitative computer-aided three-dimensional imaging techniques. Hepatology. 1998;27:893–899. doi: 10.1002/hep.510270401. [DOI] [PubMed] [Google Scholar]
- 29.Masyuk TV, Ritman EL, LaRusso NF. Quantitative assessment of the rat intrahepatic biliary system by three-dimensional reconstruction. Am J Pathol. 2001;158:2079–2088. doi: 10.1016/S0002-9440(10)64679-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.LaRusso NF. Morphology, physiology, and biochemistry of biliary epithelia. Toxicol Pathol. 1996;24:84–89. doi: 10.1177/019262339602400112. [DOI] [PubMed] [Google Scholar]
- 31.Thung SN. The development of proliferating ductular structures in liver disease. An immunohistochemical study. Arch Pathol Lab Med. 1990;114:407–411. [PubMed] [Google Scholar]
- 32.Roberts SK, Ludwig J, Larusso NF. The pathobiology of biliary epithelia. Gastroenterology. 1997;112:269–279. doi: 10.1016/s0016-5085(97)70244-0. [DOI] [PubMed] [Google Scholar]
- 33.Birnbaum A, Suchy FJ. The intrahepatic cholangiopathies. Semin Liver Dis. 1998;18:263–269. doi: 10.1055/s-2007-1007162. [DOI] [PubMed] [Google Scholar]
- 34.Chen XM, Levine SA, Tietz P, Krueger E, McNiven MA, Jefferson DM, Mahle M, LaRusso NF. Cryptosporidium parvum is cytopathic for cultured human biliary epithelia via an apoptotic mechanism. Hepatology. 1998;28:906–913. doi: 10.1002/hep.510280402. [DOI] [PubMed] [Google Scholar]
- 35.Chen XM, LaRusso NF. Mechanisms of attachment and internalization of Cryptosporidium parvum to biliary and intestinal epithelial cells. Gastroenterology. 2000;118:368–379. doi: 10.1016/s0016-5085(00)70219-8. [DOI] [PubMed] [Google Scholar]
- 36.Chen XM, Huang BQ, Splinter PL, McNiven MA, LaRusso NF. Molecular mecha-nism of Cryptosporidium parvum invasion of biliary epithelia. Gastroenterology. 2001;120:A325. doi: 10.1016/s0016-5085(03)00662-0. [DOI] [PubMed] [Google Scholar]
- 37.Chen XM, Gores GJ, Paya CV, LaRusso NF. Cryptosporidium parvum induces apoptosis in biliary epithelia by a Fas/Fas ligand-dependent mechanism. Am J Physiol. 1999;277:G599–G608. doi: 10.1152/ajpgi.1999.277.3.G599. [DOI] [PubMed] [Google Scholar]
- 38.Chen XM, Levine SA, Splinter PL, Tietz PS, Ganong AL, Jobin C, Gores GJ, Paya CV, LaRusso NF. Cryptosporidium parvum activates nuclear factor kappaB in biliary epithelia preventing epithelial cell apoptosis. Gastroenterology. 2001;120:1774–1783. doi: 10.1053/gast.2001.24850. [DOI] [PubMed] [Google Scholar]