Abstract
Endothelial dysfunction has been posited to play an important role in the pathogenesis of diabetic nephropathy (DN). Due to the heterogeneity of endothelial cells (ECs), it is difficult to generalize about endothelial responses to diabetic stimuli. At present, there are limited techniques fordirectly measuring EC function in vivo, so diagnosis of endothelial disorders still largely depends on indirect assessment of mediators arising from EC injury. In the kidney microcirculation, both afferent and efferent arteries, arterioles and glomerular endothelial cells (GEnC) have all been implicated as targets of diabetic injury. Both hyperglycemia per se, as well as the metabolic consequences of glucose dysregulation, are thought to lead to endothelial cell dysfunction. In this regard, endothelial nitric oxide synthase (eNOS) plays a central role in EC dysfunction. Impaired eNOS activity can occur at numerous levels, including enzyme uncoupling, post-translational modifications, internalization and decreased expression. Reduced nitric oxide (NO) bioavailability exacerbates oxidative stress, further promoting endothelial dysfunction and injury. The injured ECs may then function as active signal transducers of metabolic, hemodynamic and inflammatory factors that modify the function and morphology of the vessel wall and interact with adjacent cells, which may activate a cascade of inflammatory and proliferative and profibrotic responses in progressive DN. Both pharmacological approaches and potential regenerative therapies hold promise for restoration of impaired endothelial cells in diabetic nephropathy.
Keywords: diabetic nephropathy, endothelial cell, eNOS, heterogeneity, kidney, microvascular complication, nitric oxide, VEGF
INTRODUCTION
Diabetic Nephropathy (DN) is the leading cause of chronic kidney diseasein the developed world and affects about 15–25% of type 1 and 30–40% of type 2 diabetic patients [1]. Despite extensive research, underlying pathogenic mechanisms have yet to be completely elucidated. Hyperglycemia per se, as well a metabolic consequences of hyperglycemia, such as Advanced Glycation End-products (AGEs), have been implicated in therenal pathological changes [2], various cells, including glomerular podocytes, mesangial and glomerular endothelial cells (GEnCs), as well as tubular epithelial cells, interstitial fibroblasts and vascular ECs have all been implicated in the development of DN [3]. The ECs play critical roles in many physiological functions: vascular tone adjustment, blood cell trafficking, hemostatic balance, permeability status, cell proliferation and survival, as well as being involved in mediation of innate and adaptive immunity. EC dysfunction promotes progression of DN [4]. A correlation between diabetes and vascular endothelial dysfunction has been confirmed in various studies [5-9]. There is suggestive evidence that endothelial dysfunction may even exist in subjects with normal glucose tolerance and with a family history of diabetes [10]. In addition to hyperglycemia, endothelial dysfunction might also be exacerbated by hypertension, dyslipidemia, obesity, micro albuminuria, inflammation and insulin resistance [11]. This review discusses the underlying mechanisms and consequences of endothelial dysfunction in diabetic nephropathy.
CHARACTER AND HETEROGENEITY OF RENAL ENDOTHELIAL CELLS
The endothelium is the thin layer lining the interior surface of blood vessels and lymphatic vessels [12]. ECs form the endothelium as an interface between circulating blood in the lumen vessel wall. In kidney, blood flows successively through the renal arteries, interlobular arteries, and afferent arterioles to enter the glomerular capillary tufts and then exits glomeruli via efferent arterioles, which give rise to the plexus of peritubular capillaries, the vasa recta. ECs from renal arteries, arterioles, capillaries, venules, veins and glomerular capillaries each have distinctive phenotypic features. In spite of accumulating research on endothelial dysfunction, relatively little attention has been paid to varying phenotypes regulated by location and time, so called “endothelial heterogeneity”[13, 14]. The heterogeneity is also species and tissue dependent. Moreover, EC may possibly transdifferentiate into other cell types or vice versa in pathologic conditions [15].
Structural Heterogeneity of Endothelial Cells
Endothelial shape and thickness may vary among vascular beds. Electron microscopy demonstrates elongated, spindle-shaped ECs in rat arterioles, irregularly shaped ECs in capillaries and comparatively large, elliptical or irregularly shaped ECs in post-capillary venules [16]. The intercellular junctions of ECs are either continuous or discontinuous. Brain, skin, cardiac, and pulmonary endothelium in arteries, veins, and capillaries is non-fenestrated and continuous. The density of fenestrae also depends on vascular phenotype. Glomerular capillary endothelium is fenestrated and continuous [17].
ECs also have a diversity of other cellular components. Connexins, a family of structurally related transmembrane proteins that assemble to form gap junctions, have a different pattern in ECs from glomerular afferent and efferent arterioles, which could contribute to the altered renal autoregulation in DN [18]. Plasma lemmal vesicle (PV)-1 protein is an endothelium-specific integral membrane glycoprotein, enriched on the endothelium of renal peritubular capillaries during development, which is fenestrated with diaphragms; it is absent from adult GEnCs, which are also fenestrated but not apertured by diaphragms [19]. Glycocalyx is the glycoprotein oating the luminal surface of the glomerular capillaries; its heterogeneous distribution along the vascular tree can also be seen by electron microscopy [20]. The EC common marker, von Wille brand factor (vWF) has an uneven distribution indifferent types of vessels [21, 22], although the physiologic significance remains incompletely understood. eNOS expression in ECs of the renal medulla (vasa recta) appears to be stronger than in cortex (glomeruli and peritubular capillaries) [23].
Functional Heterogeneity of Endothelial Cells
Endothelium not only forms a passive barrier, dynamically regulating permeability of the microvasculature [24] but also acts as an active signal transducer for leukocyte trafficking [25], modulating hemostasis [26] and playing a pivotal role in angiogenesis and vasculogenesis, such that it is recognized as a multifunctional paracrine and endocrine “organ” that responds to metabolic, hemodynamic and inflammatory stimuli [27]. Phenotypic variation among endothelial cells may be related to their location in the vascular tree. In general, ECs in post capillary venules, where shear stress is lowest, are mainly responsible for mediating adhesion and recruiting leukocytes [28], while those in arterioles are primarily for vasomotor tone. There are two major functions for the renal endothelium- oxygen/nutrient delivery and filtration [29]. In contrast to other vascular beds, glomerular capillaries serve predominantly as a sieve of fluids and solutes. GEnCs covering 20% of the endothelial surface serve as a barrier for efficient absorption, secretion, and filtering [17]. After approximately 30% of the blood volume is filtered by the glomerulus, blood enters the efferent arterioles with increased viscosity. At each step from the hyperosmolar, hypoxic depths of the inner medulla to cortex, ECs in individual compartments perform different functions to maintain kidney homeostasis. Therefore, it is not surprising that ECs derived from each intrarenal compartment demonstrate individual chemokine expression patterns, mediating compartment-specific T cell and monocyte recruitment in inflammatory injury [30]. This variability may also lead to differential susceptibility to apoptosis and differential responses to microenvironment changes or stimuli [28].
In summary, the vasculature in the kidney is not only distinct from that of other organs, but also displays striking intra-renal heterogeneity in term of surface phenotype and protein expression in different vascular compartments. Understanding this heterogeneity may help to further direct research in EC dysfunction in progressive kidney injury and properly translate the results from bench to bedside.
RENAL ENDOTHELIAL DYSFUNCTION IN DN
Micro- and macrovascular impairment are major complications in diabetic mellitus. The former involves small vessels, such as capillaries, the latter predominately large vessels, such as arteries and veins. Nephropathy has been recognized as a common microvascular complication of diabetes. The so-called “silent phase” of DN usually leads to an underestimation of the underlying EC disorder [31].
How to Measure Renal EC Dysfunction?
As discussed above, renal EC functions vary according to their phenotype and compartmentalization in kidney. In vitro experiments are able to provide direct measurement of vasodilation/vasoconstriction from isolated vessels and characteristics of both structural and functional characteristics of cultured ECs– from their morphology to proliferation, migration, adhesion, permeability, matrix secretion and angiogenesis properties. However, caution must be taken when these data are translated to clinical situations, because commonly used culture conditions may activate or transform endothelial phenotypes [32]. In vivo, new techniques to measure peripheral circulation non-invasively, such as peripheral arterial tonometry and brachial artery flow-mediated dilatation (FMD), have been developed in order to assess vascular health and endothelial function [33, 34], but their value to predict the risk factor in DN is still debated [35]. No gold standards have been developed yet to evaluate EC function in vivo. In general, EC function is largely evaluated experimentally by: 1) assessment of the functional consequences of EC activity; 2) measurement of the concentration of chemical mediators for EC function [11]; and 3) testing competence of endothelial progenitor cells (EPCs), which may mediate regeneration, since EC has limited intrinsic capacity of self-repair with a low proliferative potential [36].
Endothelial Dysfunction-Related Pathophysiologic Abnormalities in DN
DN is a serious and progressive “microvascular” complication from both type 1 and type 2 diabetes mellitus. Its pathophysiologic alterations manifest as microalbuminuria and hyperfiltration at early stages followed by deterioration to end-stage renal disease. Microalbuminuria is usually the first signal of renal complications and may progress to overt albuminuria [37, 38]. Approximately one fourth of people with type 2 diabetes have albuminuria, and the rate is still rising by 2% to 3% per year [39, 40]. Albuminuria can result from higher intra-glomerular pressure and glomerular basement membrane (GBM) permeability, and may be indirectly influenced by interactions of ECs with mesangial cell and podocytes in a paracrine fashion [41]. In type 2 diabetes, markers of endothelial dysfunction occur in patients with normal urine albumin excretion [42], which supports the hypothesis that endothelial dysfunction may not be a simple consequence, but may also play a key etiologic role in the vasculopathy [11].
Animal experiments have suggested that dilatation of the afferent glomerular arteriole is mainly responsible for the hyperfiltration response, via increasing intraglomerular pressure and renal blood flow [43, 44]. Renal hyperfiltration has been proposed to be a common factor in early diabetes associated with vascular dysfunction, which may eventually lead to a decline of renal function and the development of glomerulosclerosis and tubulointerstitial fibrosis [45-47]. Endothelial dysfunction also diminishes the an tiatherogenic ability of ECs, which may also contribute to the abnormal renal function.
Vascular Lesion-Associated Pathologic Changes in DN
In addition to mesangial expansion, GBM thickening as a consequence of extracellular matrix accumulation, and Kimmelstiel–Wilson lesionsor global glomerulosclerosis are common pathologic features in DN [48, 49]. Dissociation of endothelial cells may disrupt the connections between the mesangial area and the GBM. Nodular sclerosis (Kimmelstiel–Wilson lesions) or global glomerulosclerosisis seen in late stages of DN. Atherosclerosis links endothelial injury, dysfunction and activation [27], and arteriolosclerosis in both afferent and efferent is recognized as characteristic of vascular lesions in DN [48]. However, hyalinosis of the efferent arteriole is relatively specific for DN, since afferent medial thickness may also be associated with concurrent hypertension [49] and is also seen in other settings [48, 50]. Intraglomerular capillary pressure secondary to an increased glomerular filtration rate is influenced by the constriction or relaxation of both glomerular afferent and efferent arteriole, but the latter may be more sensitive to angiotensin II, resulting in relatively decreased afferent arteriolar resistance and higher glomerular capillary pressure [51].
Endothelial-Myofibroblast Transition (EndoMT)
During EndoMT, endothelial cells lose endothelial markers (such as CD31 and vascular endothelial cadherin), while exhibiting mesenchymal markers, including α-smooth muscle actin (α-SMA). EndoMT has been suggested to play an important role in organ fibrosis and cancer progression [52]. Kidney fibrosis in DN, resulting from excess fibrous connective tissue, is a major sign of an advanced stage of disease and may develop in both the tubulointerstitial space and glomerulus. Zeisberg et al., presented the first evidence of possible EndMT in diabetic kidney fibrosis [53]: in a 6-month STZ-induced diabetic mouse model, they found that about 40% of all fibroblast-specific protein-1-positive and 50% of the α-SMA-positive cells co-labeled with CD31, implying that EndoMT may exist in the development and progression of DN. Based on these studies, EndoMT was considered as a potential new player in diabetic renal fibrosis. However, confirmation in human disease and elucidation of the underlying molecular pathways of EndoMT leading to renal fibrosis remain to be elucidated. Debate on the source of fibrosis-generating myofibroblasts (either from endothelial cells or vascular pericytes) in vivo is still raging [54].
Markers of EC Dysfunction
In addition to renal pathological abnormalities, chemical mediators can be utilized to estimate EC function. Renal endothelium secretes numerous vasoactive substances, such as the vasodilators, prostacyclin (PGI2) and nitric oxide (NO), and the vasoconstrictor, endothelin (ET)-1. Increased urinary and plasma endothelin are linked to renal damage progression in diabetic animal models [55] and patients with type 2 DN [56], while decreased urine PGI2 excretion has been reported in diabetic patients [57] and animal models [58]. NO is a particularly important molecular marker and endothelium-derived mediator in DN, due to its vasodilator, anti-platelet, anti-proliferative, anti-adhesive, permeability-decreasing and anti-inflammatory properties [59]. NO derived from L-arginine, is a free radical gaseous molecule and is synthesized by the action of nitric oxide synthases (NOS) [60]. Although both eNOS (endothelial NOS) and iNOS (inducible NOS) are expressed in EC, studies in mice with specific eNOS or iNOS deletion suggested thateNOS plays a predominant role in VEGF-induced angiogenesis and vascular permeability [61]. Alterations in eNOS-driven NO production and/or bioactivity are a well-accepted component of diabetic endothelial dysfunction [62]. In spite of the conflicting reports regarding eNOS gene regulation in animal model of diabetes mellitus, with reports of unchanged [63], diminished [64, 65] or increased [66, 67] expression, we and others have found that eNOS insufficiency accelerates nephropathy in mouse models of both type 1 and type 2 diabetes [68]. ADMA (asymmetric dimethylarginine), a product of arginine methylation, represents an endogenous inhibitor of endothelial NO synthase [69], and elevated plasma levels have been found in patients with type 1 [70] or type 2 [71] DN, although it is remains uncertain whether alterations in ADMA levels are causal or are simply increased as a consequence of impaired renal function [72].
Given the broad function of renal EC and the complicated endothelial pathophysiology observed in DN, hemostatic (plasminogen activator and its endogenous inhibitor, PAI-1), inflammation (IL-1β, IL-6 and TNF-α) and oxidative stress biomarkers are also of significance in EC research. It is likely that new biomarkers will emerge to assist risk prediction, prognosis and pharmaceutical responses in EC injury.
MECHANISMS OF RENAL ENDOTHELIAL INJURY DURING DN
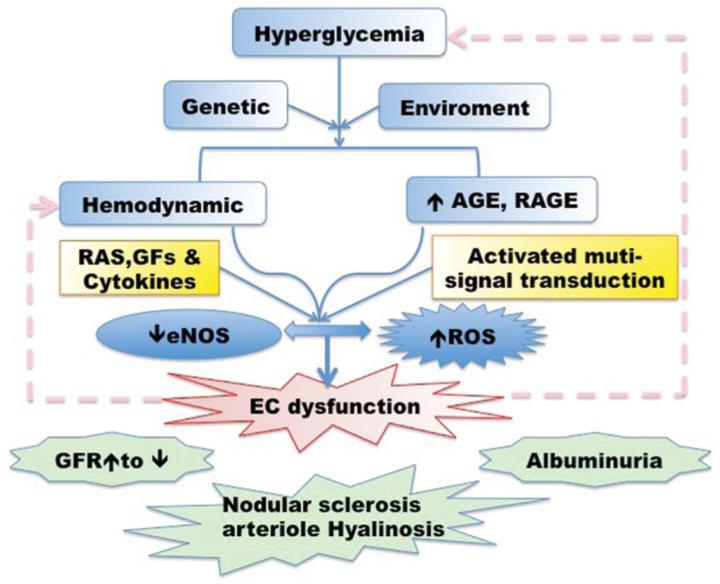
Glucose acutely autoregulates its uptake into muscle cells [73] but may not have similar autoregulation in endothelial cells [74]; thus, hyperglycemia may increase the intracellular accumulation of glucose and its metabolites in ECs. Extended exposure to high glucose may result in increased susceptibility to vascular endothelial cell injury in diabetes. The pathogenesis of diabetic EC injury is a complicated process, with multiple signal pathways being activated and numerous mediators being involved (Fig. 1).
Fig. (1). Pathogenesis of Renal EC dysfunction during DN.
Hyperglycemia, along with its metabolites and other stimuli, activates various signaling pathways and induces numerous growth factors, cytokines, ROS generation and eNOS impairment, leading to renal EC dysfunction. Injured ECs may further contribute to the progression of DN in turn. RAS: renin-angiotensin System; GFs: growth factors; eNOS: endothelial Nitric Oxide; AGE: advanced glycation end products; RAGE: the receptor of AGE; ROS: reactive oxygen species; GFR: glomerular filtration rate.
Etiology of Diabetic Renal Endothelial Impairment
Both genetic and environmental factors are involved in the development of endothelial dysfunction during DN. A large multiethnic populations genome-wide association study (The Family Investigation of Nephropathy and Diabetes study) mapped genes underlying susceptibility to DNA and found the strongest evidence for linkage to chromosomes 7q21.3, 10p15.3, 14q23.1 and 18q22.3 [75]. Association of chromosome 18q22.3 with DN in type 2 diabetes was also confirmed in Turkish patients [76]. Environmental factors, such as smoking [77] and high fat diet [78] may also be important factors that superimpose to produce microvascular complications. Nevertheless, there is no doubt that chronic hyperglycemia and the subsequent metabolic derangements play a major role in diabetic EC injury and can lead to the over production of advanced glycation end products (AGE), activated protein kinase C (PKC) signaling cascades and accumulated reactive oxygen species (ROS). Hemodynamic alterations along with renin-angiotensin system (RAS) regulation seem to be another pivotal contributor to dysfunction of renal endothelium in both glomerular afferent and efferent arteries.
Hyperglycemia Activated Signal Pathways
Various signal pathways are activated during DN; here we concentrate on the three signaling pathways likely to be involved in endothelial dysfunction:
The DAG (Diacylglycerol)/PKC (Protein Kinase C) Pathway
PKC comprises a superfamily of isoenzymes, activated by cofactors such as DAG and phosphatidyl serine. Hyperglycemia, along with other metabolic and hemodynamic factors, induces an elevation in DAG, which activates the PKC pathway. PKC plays an important role inthe regulation of endothelial permeability, vasoconstriction, cell growth, angiogenesis, and leukocyte adhesion [79]. Indirectly, high glucose-induced reactive oxygen species (ROS) contribute to vascular dysfunction via a PKC-dependent activation of nicotinamide adenine dinucleotide phosphate (NADPH) oxidase [80]. Multiple PKC isoforms have been documented to be involved in mediation of endothelial dysfunction in diabetic nephropathy. Based on experiments with isoform-specific knock-out mice and a specific PKC-β inhibitor (ruboxistaurin, a bisindolylmaleimide) treatment, PKC-α activation appears crucial for the development of albuminuria, whereas PKC-β activation appears to be mainly involved in mesangial expansion, basement membrane thickening and renal hypertrophy in the development of DN [81]. Activation of other PKC isoforms: PKC-δ and -ε by hyperglycemia-induced oxidative stress has also been reported in diabetic rat kidney [82], but the linkage of other PKC isoforms with diabetic vascular dysfunctions remains under investigation [83-85].
The Polyol Pathway
Hyperglycemia increases glucose metabolism via the polyol pathway, causing the accumulation of intracellular sorbitol. It has been suggested that elevated levels of sorbitol increase superoxide production, interfere with NO bioavailability and promote PGH2 (prostaglandin H2) /TXA2 (thromboxane A2) release [86], which disturbs regulation of arterial vasomotor responses. Hence activation of the polyol pathway may contribute to the development of microvascular dysfunction in diabetes mellitus. Inhibition of aldose reductase, a key enzyme in the polyol pathway, attenuated proteinuria, decreased GBM thickening in diabetic rats [87] and reduced glomerular hyperfiltration in humans [88].
TGF-β (Transforming Growth Factor-β) Signaling
Hemodynamic alterations and hyperglycemia and its associated metabolic alterations stimulate secretion of inflammatory molecules, including TGF-β1, in diabetic animal models [89] and in patients [90]. Increased TGF-β1 promotes extra cellular matrixprotein accumulation in the vasculature [91], activates Smad (Mothers against decapentaplegic homolog) -2 and Smad-3 and is involved in angiogenesis by mediating the balance of the proangiogenic factor, VEGF, and antiangiogenic growth factor, thrombospondin-1 (TSP-1) [92]. TGF-β signaling may also interact with other signal pathways [93]. Various anti-TGF-β1 approaches are under investigation in clinical trials [94]. Hopefully they will lead to potential therapeutic innovations. However, activation of the TGF-β1-Smad signaling pathway also induces upregulation of eNOS in endothelial cells [95], which may be beneficial to ECs. Inhibition of TGF-β could be a double-edged sword in DN, due to its anti-proliferative and anti-inflammatory properties [96].
Impairment of eNOS/NO Bioactivity
There are multiple mechanisms by which hyperglycemia may impair NO production in renal ECs. Hyperglycemia-induced eNOS impairment leads to increased oxidative stress and scavenging of NO, which represents initiation event(s) for development of endothelial dysfunction [97]. There is increasing evidence of eNOS /NO dysfunction during DN [98, 99]. Patients with either type 1 or 2 diabetes exhibit abnormal endothelium dependent vasodilation [100]. Studies from our own group and others have demonstrated accelerated glomerular injury in diabetic mice with eNOS deficiency, which strongly supports a key role for eNOS dysfunction in the pathogenesis of DN [68a, 101]. Investigation in patients with type 2 DN suggested that certain eNOS gene polymorphisms are linked to eNOS function and associated with advanced DN [102]. Nevertheless, there are conflicting reports for eNOS gene expression in animal diabetic models: with eNOS expression described to be either unchanged [63], diminished [64, 65] or increased [66, 67]. Regulation of eNOS bioactivity is multifactorial. In our study from glomeruli of db/db mice at 34 weeks, there was no significant change in eNOS monomer expression, but a significant decrease in the dimerized form [99]. Under physiological conditions, eNOS functions as a “homodimer”. Coupled eNOS transports electron from a flavin-containing reductase domain to a heme-containing oxygenase domain. Homodimer uncoupling leads to superoxide anion (O2−) formation instead of NO production [103]. Optimal concentrations of the eNOS substrate, L-arginine and the co-factor tetrahydrobiopterin (BH4) are essential to maintain eNOS dimerization. Active eNOS requires formation of a homodimer through a linkage between the N-terminal oxygenase domains; BH4 stabilizes formation of the eNOS dimer, increases NOS affinity for L-arginine, and undergoes distinct redox transitions with the heme group [104]. When either the essential substrate, L-arginine, or the essential cofactor, BH4, is limited, electron transfer from eNOS flavins becomes uncoupled from L-arginineoxidation, and superoxide is produced from the oxygenase domain [60, 103, 105], which may further reduce NO bioactivity and increase oxidative stress within endothelial cells by scavenging NO and forming peroxynitrite [106]. Insufficient L-arginine may link to onset of microalbuminuriain type 2 diabetic patients [107]; and long term L-arginine supplementation therapy has been shown to improve vascular function and glucose homeostasis instreptozotocin-induced diabetic rats [108] and diabetic patients [109]. Reduced BH4 has been observed in diabetic rats [109a, 110], with more profound depletion in endothelial cells than plasma [109a]. Acute intraarterial infusion of BH4 induced acute increases in forearm blood flow in response to endothelium-dependent vasodilators in patients with type 2 diabetes [111]. Sepiapterin is the immediate precursor of BH4 via the biopterin salvage pathway, but is less sensitive to oxidative stress than BH4 [112]. Our recent studies provided further evidence for a direct beneficial role of both arginine and BH4 supplement, sepiapterin on GEnCs in DN, independent of vasodilation [99].
Post-translational regulation also plays a vital role in control of eNOS bioactivity due to its a long half-life at baseline (10–35 h) [113]. eNOS is subject to a variety of posttranslational regulatory mechanisms, including reversible enzyme acylation, regulation of subcellular localization, protein–protein interactions, S-nitrosylation and phosphorylation [114]. Our studies in both diabetic mouse glomeruli and high glucose-stimulated GEnCs demonstrated a decrease in eNOS phosphorylation at Ser1179 without a significant alteration at Thr497. Akt-dependent phosphorylation of eNOS at Ser1179 is critical for endothelium-dependent relaxation [115], while phosphorylation at Thr497 is considered inhibitory [116]. Reduced phosphorylation of eNOS at Ser1179 has previously been reported in moderately hyperglycemic diabetic rats [117]. These post-translation modifications may contribute to eNOS dysfunction.
eNOS activity is also regulated by its location within the cell. Under baseline conditions, eNOS predominately localizes to the plasma membrane, but it may traffic into the cytoplasm in response to certain stimuli. Microenvironments in cytoplasmic regions of the Golgi, the mitochondria and the nucleus may be less optimal for NO production, primarily due to insufficient access to calcium-calmodulin [118]. Caveolin-1 (Cav-1) has been suggested to be an inhibitor of eNOS in some phenotypes of ECs; conjugated Cav-1-eNOS in caveolae maydecrease eNOS-dependent NO release [119]. eNOS activity may also be inhibited by its endogenous inhibitor, ADMA (Asymmetric Dimethylarginine). Elevated plasma ADMA has been found in patients with both types DN [71, 72, 120].
Oxidative Stress
The imbalance between NO and reactive oxygen species (ROS) generation is a central pathophysiologic denominator in diabetic endothelial dysfunction. High glucose increases ROS production in ECs [2], and reduces endogenous antioxidant systems [121], resulting in oxidative stress. The superoxide anion may interact with NO, generating peroxynitrite [122]. Peroxynitrite is increased in patients with type 2 diabetes [123] and diabetic mice [99] and peroxynitrite-mediated endothelial dysfunction has been reported in DN [124]. It is well known that hyperglycemia leads to increased AGEs and upregulates its receptor, RAGE. ROS stimulates the formation of AGEs [125]. Furthermore, ROS oxidizes BH4 to an inactive metabolite, promoting eNOS uncoupling [126], in addition to inactivating prostacyclin synthetase [127].
Interaction of Renal ECs with Other Cells in DN
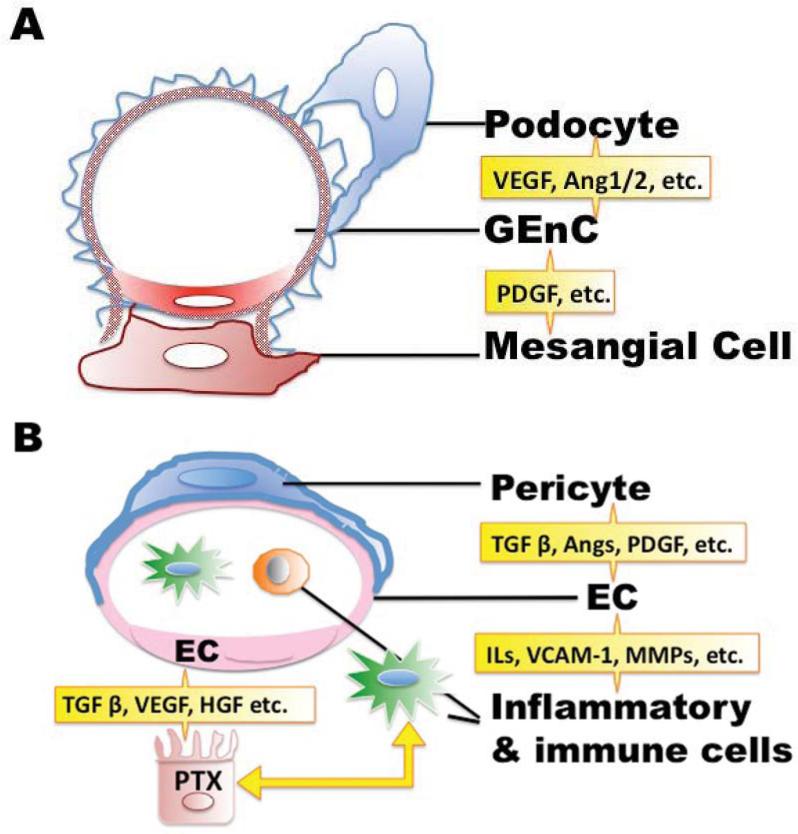
In kidney, ECs is in close contact with other renal resident and blood cells. Together, they not only provide a permeability barrier, but also act as multifunctional paracrine and endocrine regulators, coordinating immune responses, hemostasis, angiogenesis, extracellular matrix accumulation and modulation of blood flow and vascular tone (Fig. 2). Growth factors, cytokines and diabetic vasoactive agents mediate the cross talk [128], including angiogenesis factors, such as vascular endothelial growth factor (VEGF) and pro- or anti-inflammatory cytokines, such as tumor necrosis factor (TNF)-α.
Fig. (2). Interaction of renal ECs with adjacent cells.
A. In glomeruli, GEnCs are surrounded by the interdigitated foot process from podocytes. Glomerular mesangial cells (glomerular pericytes) are located in the area between GEnCs. The injured endothelium serves as an active signal transducer for metabolic, hemodynamic and inflammatory factors that modify the function and morphology of the vessel wall and interacts with adjacent cells. Growth factors involved in this crosstalk include VEGF:Vascular endothelial growth factor; Ang: Angiopoietins and PDGF: Platelet-derived growth factor. B. Pericytes are embedded within the vascular basement membrane of blood microvessels. Circulating and renal resident inflammatory/immune cells, pericytes and renal ECs interact each other, influence to effect tissue repair/fibrosis processes. Pro-inflammatory, pro-fibrotic and adhesive cytokines, metalloproteinases, and growth factors mediate this communication.VCAM-1: Vascular cell adhesion molecule-1, ILs: interleukins, MMPs: Matrix metalloproteinases. PTX: proximal tubular cell, HGF: hepatic growth factor.
Cross-Talk of GEnCs with Podocytes and Mesangial Cells
The glomerular filtration barrier is a multicomponent apparatus [129]; renal glomerular capillaries consist of three layers: a fenestrated endothelium, the intervening glomerular basement membrane, and podocytes. Intraglomerular mesangial cells are located in the interstitium between GEnCs (Fig. 2A). Podocytes generate several angiogenic growth factors, such as vascular endothelial growth factor (VEGF-A), and Angiopoetin-1 (Ang-1) [130], while GEnCs express corresponding receptors. There are several members (at least A, B, C, D) of the VEGF family; VEGF –A appears to play the major role in podocyte-EC interactions. Podocyte derived VEGF–A regulates GEnCs function mainly via paracrine action [131], although the contribution via autocrine VEGF–A signaling to normal barrier function cannot be completely excluded. Elevated VEGF–A has been reported in the initial phases of diabetes [132], while a subsequent decrease has been documented in numerous human or animal studies [133-135].
Elevated VEGF has been shown in a diabetic mouse model with NOS deficiency [136], while NO attenuated VEGF–A induced endothelial proliferation [137]. This condition of low NO bioavailability associated with high VEGF-A expression was termed as “uncoupling of VEGF-A with NO” [135]. Both activation and inhibition of the VEGF-A dependent signal transduction cause functional defects of the renal glomeruli [138, 139]. Initial upregulation of glomerular VEGF-A expression may increase glomerular permeability, while the subsequent decreases in receptor-bound VEGF on the endothelium may underlie inability of effective capillary repair with more advanced disease [140]. Despite a few studies showing marked amelioration of albuminuria in somediabetic animal models from inhibition of VEGF activity by neutralizing antibodies or small molecule inhibitors of VEGF receptor kinase signaling [141, 142], VEGF displayed protective effects for glomerular microvasculature in diabetes overall; deletion of VEGF-A in type 1 diabetic mice promotes endothelial injury, accelerating the progression of glomerular lesion [143].
Another podocyte-derived angiogenesis growth factor, Ang-1, also contributes to the maintenance of the integrity of the glomerular filtration barrier [144]. Ang-2, from the same angiopoietin family, is also expressed in the kidney during development, but is significantly downregulated in adult [145]. Ang-2 is a competitive antagonist of Ang-1, since both of them share the same receptor in ECs [144]. Upregulated Ang-2 that stimulates vascular permeability has been reported in DN [146]. Imbalance of Ang-1/2 may underlie dysfunctional crosstalk between podocytes and GEnCs during DN.
Mesangial cells provide structural support for glomerular capillary loops and respond to capillary stretch, possibly playing an important role inregulation of glomerular flow and pressure. Hyperglycemia-activated mesangial cells are responsive to the increased EC-derived PDGF (platelet-derived growth factor), the major mediator between mesangial cells and GEnC [147]. It has been suggested that GEnC promote mesangial cell growth via a PDGF-Like substance [148].
Cross-Talk between Renal Proximal Tubular Cells (PTCs) and Endothelial Cells
Diabetic injury initially is detected in glomeruli, but the decline of renal function correlates with the degree of renal tubule interstitial fibrosis [149]. There is direct evidence of high glucose-induced collagen secretion by PTC [150]. Peritubular capillaries are essential for renal transport, reabsorption and oxygen supply to the tubules [151]. Recently, Tasnim et al., investigated the interactions between renal tubular epithelial cells and adjacent endothelial cells in a co-culture system and found that primary cultured renal proximal tubular cells stimulated endothelial cells to express a functionally balanced combination of various factors, including VEGF, TGF-β along with its antagonist α2-macroglobulin and HGF (Hepatocyte growth factor). In turn, endothelial cells appeared to promote survival, proliferation and differentiation of the proximal tubule cells [152].
Interaction of ECs with Inflammatory Cells
Diabetes has been recognized as an inflammatory process [153]. Vascular cell adhesion molecule-1 (VCAM-1) was found to be upregulated in patients with DN [154], which may promote the adhesion of inflammatory cells to the endothelium and recruit circulating immune cells into the diabetic kidney. Renal tissue macrophages, T cells, and neutrophils, along with reactive oxygen species, pro-inflammatory cytokines, metalloproteinases, and growth factors, modulate the local response and promote inflammation and fibrosis within the diabetic kidney [153].
EC-Pericyte Communication
Pericytes are vascular mural cells embedded within the vascular basement membrane of blood microvessels (Fig. 2B). In the kidney, they are localized in the tubulointerstitial space on peritubular capillaries. Mesangial cells are categorized as specialized pericytes within the glomerulus [155]. These cells closely contact with the endothelium, regulating vascular development, stabilization, maturation, and remodeling. Endothelial–pericyte communication largely depends on growth factors, including TGF β, angiopoietins, PDGF, spingosine-1-phosphate, and Notch ligands along with their respective receptors [156]. Among them, PDGF receptor-β (PDGFRβ) is critically involved in pericyte recruitment and proliferation [157]. It has been suggested that pericytes play a central role in diabetic complications. Loss of pericytes is one of the first observable changes in diabetic retinopathy, ultimately followed by increased vascular permeability [158]. Knockout of PDGF-B or PDGFR-β results in deformity of pericyte-like mesangial cells, leading to defective glomerulogenesis and glomerulosclerosis [159]. Duffield et al., recently described renal pericytes as a major source of myofibroblast precursors in the kidney [54, 155].
In summary, high glucose along with its metabolites and other stimuli activate various pathways via similar mechanisms in different cell types of the kidney; induce numerous growth factors, cytokines, ROS generation and eNOS impairment, leading to renal EC dysfunction. The injured endothelium acts as an active signal transducer for metabolic, hemodynamic and inflammatory factors that modify the function and morphology of the vessel wall and interacts with adjacent cells. The self-protective mechanisms in response to oxidant, chemical, and shear stress may in turn produce a cascade of factors that promote inflammatory, proliferative and profibrotic responses in progressive diseases. Hence EC dysfunction is considered as a potential contributor in the progression of DN [160] (Fig. 1).
POTENTIAL EC REGENERATIVE THERAPIES IN DN
With the development of regenerative medicine, studies have suggested potential strategies for EC regenerative therapy in DN [161]. In addition to the mechanism-based pharmacological and growth factors (or their inhibitors) therapeutic innovation mentioned previously, stem/progenitor cellular strategies may prove to be effective approaches to regeneration of ECs. Rat experiments have suggested that bone marrow-derived endothelial progenitor cells may participate in glomerular endothelial cell turnover [162]. However, the effect of endothelial progenitor cells in long-standing asymptomatic type 1 diabetic patients remains inconclusive [163]; it provides hope, but its long term safety and beneficial impact need to be cautiously evaluated.
ACKNOWLEDGEMENTS
These studies were supported by grants from the National Institutes of Health (DK38226, DK51265, DK62794, DK95785) by the Vanderbilt O'Brien Center (DK79341) and by funds from the Veterans Administration.
Footnotes
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
REFERENCES
- 1.Mohamed Q, Gillies MC, Wong TY. Management of diabetic retinopathy: a systematic review. JAMA. 2007;298(8):902–16. doi: 10.1001/jama.298.8.902. [DOI] [PubMed] [Google Scholar]
- 2.Nishikawa T, Edelstein D, Du XL, Yamagishi S, Matsumura T, Kaneda Y, Yorek MA, Beebe D, Oates PJ, Hammes HP, Giardino I, Brownlee M. Normalizing mitochondrial superoxide production blocks three pathways of hyperglycaemic damage. Nature. 2000;404(6779):787–90. doi: 10.1038/35008121. [DOI] [PubMed] [Google Scholar]
- 3.Kanwar YS, Wada J, Sun L, Xie P, Wallner EI, Chen S, Chugh S, Danesh FR. Diabetic nephropathy: mechanisms of renal disease progression. Exp. Biol. Med. (Maywood) 2008;233(1):4–11. doi: 10.3181/0705-MR-134. [DOI] [PubMed] [Google Scholar]
- 4.Calles-Escandon J, Cipolla M. Diabetes and endothelial dysfunction: a clinical perspective. Endocr. Rev. 2001;22(1):36–52. doi: 10.1210/edrv.22.1.0417. [DOI] [PubMed] [Google Scholar]
- 5.Hink U, Li H, Mollnau H, Oelze M, Matheis E, Hartmann M, Skatchkov M, Thaiss F, Stahl RA, Warnholtz A, Meinertz T, Griendling K, Harrison DG, Forstermann U, Munzel T. Mechanisms underlying endothelial dysfunction in diabetes mellitus. Circ. Res. 2001;88(2):E14–22. doi: 10.1161/01.res.88.2.e14. [DOI] [PubMed] [Google Scholar]
- 6.Thorand B, Baumert J, Chambless L, Meisinger C, Kolb H, Doring A, Lowel H, Koenig W. Elevated markers of endothelial dysfunction predict type 2 diabetes mellitus in middle-aged men and women from the general population. Arterioscler. Thromb. Vasc. Biol. 2006;26(2):398–405. doi: 10.1161/01.ATV.0000198392.05307.aa. [DOI] [PubMed] [Google Scholar]
- 7.Tan KC, Chow WS, Ai VH, Metz C, Bucala R, Lam KS. Advanced glycation end products and endothelial dysfunction in type 2 diabetes. Diabetes Care. 2002;25(6):1055–9. doi: 10.2337/diacare.25.6.1055. [DOI] [PubMed] [Google Scholar]
- 8.Song Y, Manson JE, Tinker L, Rifai N, Cook NR, Hu FB, Hotamisligil GS, Ridker PM, Rodriguez BL, Margolis KL, Oberman A, Liu S. Circulating levels of endothelial adhesion molecules and risk of diabetes in an ethnically diverse cohort of women. Diabetes. 2007;56(7):1898–904. doi: 10.2337/db07-0250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kelly R, Ruane-O'Hora T, Noble MI, Drake-Holland AJ, Snow HM. Differential inhibition by hyperglycaemia of shear stress- but not acetylcholine-mediated dilatation in the iliac artery of the anaesthetized pig. J. Physiol. 2006;573(Pt 1):133–45. doi: 10.1113/jphysiol.2006.106500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Caballero AE. Endothelial dysfunction in obesity and insulin resistance: a road to diabetes and heart disease. Obes. Res. 2003;11(11):1278–89. doi: 10.1038/oby.2003.174. [DOI] [PubMed] [Google Scholar]
- 11.Calles-Escandon J, Cipolla M. Diabetes and endothelial dysfunction: a clinical perspective. Endocr. Rev. 2001;22(1):36–52. doi: 10.1210/edrv.22.1.0417. [DOI] [PubMed] [Google Scholar]
- 12.Minami T, Aird WC. Endothelial cell gene regulation. Trends Cardiovasc. Med. 2005;15(5):174–84. doi: 10.1016/j.tcm.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 13.Aird WC. Phenotypic heterogeneity of the endothelium: II. Representative vascular beds. Circ. Res. 2007;100(2):174–90. doi: 10.1161/01.RES.0000255690.03436.ae. [DOI] [PubMed] [Google Scholar]
- 14.Aird WC. Phenotypic heterogeneity of the endothelium: I. Structure, function, and mechanisms. Circ. Res. 2007;100(2):158–73. doi: 10.1161/01.RES.0000255691.76142.4a. [DOI] [PubMed] [Google Scholar]
- 15.a Planat-Benard V, Silvestre JS, Cousin B, Andre M, Nibbelink M, Tamarat R, Clergue M, Manneville C, Saillan-Barreau C, Duriez M, Tedgui A, Levy B, Penicaud L, Casteilla L. Plasticity of human adipose lineage cells toward endothelial cells: physiological and therapeutic perspectives. Circulation. 2004;109(5):656–63. doi: 10.1161/01.CIR.0000114522.38265.61. [DOI] [PubMed] [Google Scholar]; b Wurmser AE, Nakashima K, Summers RG, Toni N, D'Amour KA, Lie DC, Gage FH. Cell fusion-independent differentiation of neural stem cells to the endothelial lineage. Nature. 2004;430(6997):350–6. doi: 10.1038/nature02604. [DOI] [PubMed] [Google Scholar]
- 16.McDonald DM. Endothelial gaps and permeability of venules in rat tracheas exposed to inflammatory stimuli. Am. J. Physiol. 1994;266(1 Pt 1):L61–83. doi: 10.1152/ajplung.1994.266.1.L61. [DOI] [PubMed] [Google Scholar]; b Hirata A, Baluk P, Fujiwara T, McDonald DM. Location of focal silver staining at endothelial gaps in inflamed venules examined by scanning electron microscopy. Am. J. Physiol. 1995;269(3 Pt 1):L403–18. doi: 10.1152/ajplung.1995.269.3.L403. [DOI] [PubMed] [Google Scholar]
- 17.Satchell SC, Braet F. Glomerular endothelial cell fenestrations: an integral component of the glomerular filtration barrier. Am. J. Physiol. Renal Physiol. 2009;296(5):F947–56. doi: 10.1152/ajprenal.90601.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang J, Hill CE. Differential connexin expression in preglomerular and postglomerular vasculature: accentuation during diabetes. Kidney Int. 2005;68(3):1171–85. doi: 10.1111/j.1523-1755.2005.00509.x. [DOI] [PubMed] [Google Scholar]
- 19.Stan RV, Kubitza M, Palade GE. PV-1 is a component of the fenestral and stomatal diaphragms in fenestrated endothelia. Proc. Natl. Acad. Sci. USA. 1999;96(23):13203–7. doi: 10.1073/pnas.96.23.13203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.van den Berg BM, Vink H, Spaan JA. The endothelial glycocalyx protects against myocardial edema. Circ. Res. 2003;92(6):592–4. doi: 10.1161/01.RES.0000065917.53950.75. [DOI] [PubMed] [Google Scholar]
- 21.Kumar S, West DC, Ager A. Heterogeneity in endothelial cells from large vessels and microvessels. Differentiation. 1987;36(1):57–70. doi: 10.1111/j.1432-0436.1987.tb00181.x. [DOI] [PubMed] [Google Scholar]
- 22.Yamamoto K, de Waard V, Fearns C, Loskutoff DJ. Tissue distribution and regulation of murine von Willebrand factor gene expression in vivo. Blood. 1998;92(8):2791–801. [PubMed] [Google Scholar]
- 23.Han KH, Lim JM, Kim WY, Kim H, Madsen KM, Kim J. Expression of endothelial nitric oxide synthase in developing rat kidney. Am. J. Physiol. Renal Physiol. 2005;288(4):F694–702. doi: 10.1152/ajprenal.00085.2004. [DOI] [PubMed] [Google Scholar]
- 24.Mehta D, Malik AB. Signaling mechanisms regulating endothelial permeability. Physiol. Rev. 2006;86(1):279–367. doi: 10.1152/physrev.00012.2005. [DOI] [PubMed] [Google Scholar]
- 25.McIntyre TM, Prescott SM, Weyrich AS, Zimmerman GA. Cell-cell interactions: leukocyte-endothelial interactions. Curr. Opin. Hematol. 2003;10(2):150–8. doi: 10.1097/00062752-200303000-00009. [DOI] [PubMed] [Google Scholar]
- 26.Gerlach H, Esposito C, Stern DM. Modulation of endothelial hemostatic properties: an active role in the host response. Annu. Rev. Med. 1990;41:15–24. doi: 10.1146/annurev.me.41.020190.000311. [DOI] [PubMed] [Google Scholar]
- 27.Sumpio BE, Riley JT, Dardik A. Cells in focus: endothelial cell. Int. J. Biochem. Cell Biol. 2002;34(12):1508–12. doi: 10.1016/s1357-2725(02)00075-4. [DOI] [PubMed] [Google Scholar]
- 28.Cines DB, Pollak ES, Buck CA, Loscalzo J, Zimmerman GA, McEver RP, Pober JS, Wick TM, Konkle BA, Schwartz BS, Barnathan ES, McCrae KR, Hug BA, Schmidt AM, Stern DM. Endothelial cells in physiology and in the pathophysiology of vascular disorders. Blood. 1998;91(10):3527–61. [PubMed] [Google Scholar]
- 29.Molema G, Aird WC. Vascular heterogeneity in the kidney. Semin. Nephrol. 2012;32(2):145–55. doi: 10.1016/j.semnephrol.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 30.a Panzer U, Steinmetz OM, Reinking RR, Meyer TN, Fehr S, Schneider A, Zahner G, Wolf G, Helmchen U, Schaerli P, Stahl RA, Thaiss F. Compartment-specific expression and function of the chemokine IP-10/CXCL10 in a model of renal endothelial microvascular injury. J. Am. Soc. Nephrol. 2006;17(2):454–64. doi: 10.1681/ASN.2005040364. [DOI] [PubMed] [Google Scholar]; b Lim YC, Garcia-Cardena G, Allport JR, Zervoglos M, Connolly AJ, Gimbrone MA, Jr., Luscinskas FW. Heterogeneity of endothelial cells from different organ sites in T-cell subset recruitment. Am. J. Pathol. 2003;162(5):1591–601. doi: 10.1016/S0002-9440(10)64293-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Foggensteiner L, Mulroy S, Firth J. Management of diabetic nephropathy. J. R. Soc. Med. 2001;94(5):210–7. doi: 10.1177/014107680109400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Grant DS, Tashiro K, Segui-Real B, Yamada Y, Martin GR, Kleinman HK. Two different laminin domains mediate the differentiation of human endothelial cells into capillary-like structures in vitro. Cell. 1989;58(5):933–43. doi: 10.1016/0092-8674(89)90945-8. [DOI] [PubMed] [Google Scholar]
- 33.Kuvin JT, Patel AR, Sliney KA, Pandian NG, Sheffy J, Schnall RP, Karas RH, Udelson JE. Assessment of peripheral vascular endothelial function with finger arterial pulse wave amplitude. Am. Heart J. 2003;146(1):168–74. doi: 10.1016/S0002-8703(03)00094-2. [DOI] [PubMed] [Google Scholar]
- 34.Settergren M, Bohm F, Ryden L, Pernow J. Cholesterol lowering is more important than pleiotropic effects of statins for endothelial function in patients with dysglycaemia and coronary artery disease. Eur. Heart J. 2008;29(14):1753–60. doi: 10.1093/eurheartj/ehn166. [DOI] [PubMed] [Google Scholar]
- 35.Gordin D, Waden J, Forsblom C, Thorn L, Rosengard-Barlund M, Tolonen N, Saraheimo M, Harjutsalo V, Groop PH. Pulse pressure predicts incident cardiovascular disease but not diabetic nephropathy in patients with type 1 diabetes (The FinnDiane Study). Diabetes Care. 2011;34(4):886–91. doi: 10.2337/dc10-2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Avogaro A, Albiero M, Menegazzo L, de Kreutzenberg S, Fadini GP. Endothelial dysfunction in diabetes: the role of reparatory mechanisms. Diabetes Care. 2011;34(2):S285–90. doi: 10.2337/dc11-s239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.The Diabetes Control and Complications Trial Research Group The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N. Engl. J. Med. 1993;329(14):977–86. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 38.United Kingdom Prospective Diabetes Study (UKPDS) 13: Relative efficacy of randomly allocated diet, sulphonylurea, insulin, or metformin in patients with newly diagnosed non-insulin dependent diabetes followed for three years. BMJ. 1995;310(6972):83–8. [PMC free article] [PubMed] [Google Scholar]
- 39.Deshpande AD, Harris-Hayes M, Schootman M. Epidemiology of diabetes and diabetes-related complications. Phys. Ther. 2008;88(11):1254–64. doi: 10.2522/ptj.20080020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Adler AI, Stevens RJ, Manley SE, Bilous RW, Cull CA, Holman RR. Development and progression of nephropathy in type 2 diabetes: the United Kingdom Prospective Diabetes Study (UKPDS 64). Kid Intern. 2003;63(1):225–32. doi: 10.1046/j.1523-1755.2003.00712.x. [DOI] [PubMed] [Google Scholar]
- 41.Stehouwer CD. Endothelial dysfunction in diabetic nephropathy: state of the art and potential significance for non-diabetic renal disease. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association - European Renal Association. 2004;19(4):778–81. doi: 10.1093/ndt/gfh015. [DOI] [PubMed] [Google Scholar]
- 42.Neri S, Bruno CM, Leotta C, D'Amico RA, Pennisi G, Ierna D. Early endothelial alterations in non-insulin-dependent diabetes mellitus. Int. J. Clin. Lab. Res. 1998;28(2):100–3. doi: 10.1007/s005990050027. [DOI] [PubMed] [Google Scholar]
- 43.Anderson S, Jung FF, Ingelfinger JR. Renal renin-angiotensin system in diabetes: functional, immunohistochemical, and molecular biological correlations. Am. J. Physiol. 1993;265(4 Pt 2):F477–86. doi: 10.1152/ajprenal.1993.265.4.F477. [DOI] [PubMed] [Google Scholar]
- 44.Craven PA, Caines MA, DeRubertis FR. Sequential alterations in glomerular prostaglandin and thromboxane synthesis in diabetic rats: relationship to the hyperfiltration of early diabetes. Metabolism. 1987;36(1):95–103. doi: 10.1016/0026-0495(87)90070-9. [DOI] [PubMed] [Google Scholar]
- 45.Cherney DZ, Miller JA, Scholey JW, Nasrallah R, Hebert RL, Dekker MG, Slorach C, Sochett EB, Bradley TJ. Renal hyperfiltration is a determinant of endothelial function responses to cyclooxygenase 2 inhibition in type 1 diabetes. Diabetes Care. 2010;33(6):1344–6. doi: 10.2337/dc09-2340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Melsom T, Mathisen UD, Eilertsen BA, Ingebretsen OC, Jenssen T, Njolstad I, Solbu MD, Toft I, Eriksen BO. Physical Exercise, Fasting Glucose, and Renal Hyperfiltration in the General Population: The Renal Iohexol Clearance Survey in Tromso 6 (RENIS-T6). Clin. J. Am. Soc. Nephrol. 2012;7(11):1801–10. doi: 10.2215/CJN.02980312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hadi HA, Suwaidi JA. Endothelial dysfunction in diabetes mellitus. Vasc. Health Risk Manag. 2007;3(6):853–76. [PMC free article] [PubMed] [Google Scholar]
- 48.Tervaert TW, Mooyaart AL, Amann K, Cohen AH, Cook HT, Drachenberg CB, Ferrario F, Fogo AB, Haas M, de Heer E, Joh K, Noel LH, Radhakrishnan J, Seshan SV, Bajema IM, Bruijn JA. Pathologic classification of diabetic nephropathy. J. Am. Soc. Nephrol. 2010;21(4):556–63. doi: 10.1681/ASN.2010010010. [DOI] [PubMed] [Google Scholar]
- 49.Alsaad KO, Herzenberg AM. Distinguishing diabetic nephropathy from other causes of glomerulosclerosis: an update. J. Clin. Pathol. 2007;60(1):18–26. doi: 10.1136/jcp.2005.035592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stout LC, Kumar S, Whorton EB. Insudative lesions--their pathogenesis and association with glomerular obsolescence in diabetes: a dynamic hypothesis based on single views of advancing human diabetic nephropathy. Hum. Pathol. 1994;25(11):1213–27. doi: 10.1016/0046-8177(94)90039-6. [DOI] [PubMed] [Google Scholar]
- 51.Gnudi L. Cellular and molecular mechanisms of diabetic glomerulopathy. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association – Eur. Renal. 2012;27(7):2642–9. doi: 10.1093/ndt/gfs121. [DOI] [PubMed] [Google Scholar]
- 52.Zeisberg M, Neilson EG. Biomarkers for epithelial-mesenchymal transitions. J. Clin. Invest. 2009;119(6):1429–37. doi: 10.1172/JCI36183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zeisberg EM, Potenta SE, Sugimoto H, Zeisberg M, Kalluri R. Fibroblasts in kidney fibrosis emerge via endothelial-to-mesenchymal transition. J. Am. Soc. Nephrol. 2008;19(12):2282–7. doi: 10.1681/ASN.2008050513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zeisberg M, Duffield JS. Resolved: EMT produces fibroblasts in the kidney. J. Am. Soc. Nephrol. 2010;21(8):1247–53. doi: 10.1681/ASN.2010060616. [DOI] [PubMed] [Google Scholar]
- 55.Meli S, Bruno CM. Endothelin and diabetic nephropathy: a new pathogenetic factor? Panminerva Med. 2001;43(1):45–8. [PubMed] [Google Scholar]
- 56.Zanatta CM, Gerchman F, Burttet L, Nabinger G, Jacques-Silva MC, Canani LH, Gross JL. Endothelin-1 levels and albuminuria in patients with type 2 diabetes mellitus. Diabetes Res. Clin. Pract. 2008;80(2):299–304. doi: 10.1016/j.diabres.2007.12.024. [DOI] [PubMed] [Google Scholar]
- 57.Umeda F, Kuroki T, Nawata H. Prostaglandins and diabetic nephropathy. J. Diabetes Complicat. 1995;9(4):334–6. doi: 10.1016/1056-8727(95)80035-d. [DOI] [PubMed] [Google Scholar]
- 58.Tajiri Y, Umeda F, Inoguchi T, Nawata H. Effects of thromboxane synthetase inhibitor (OKY-046) on urinary prostaglandin excretion and renal function in streptozotocin-induced diabetic rat. J. Diabetes Complicat. 1994;8(2):126–32. doi: 10.1016/1056-8727(94)90062-0. [DOI] [PubMed] [Google Scholar]
- 59.Stehouwer CD. Endothelial dysfunction in diabetic nephropathy: state of the art and potential significance for non-diabetic renal disease. Nephrol. Dial. Transplant. 2004;19(4):778–81. doi: 10.1093/ndt/gfh015. [DOI] [PubMed] [Google Scholar]
- 60.Xu J, Xie Z, Reece R, Pimental D, Zou MH. Uncoupling of endothelial nitric oxidase synthase by hypochlorous acid: role of NAD(P)H oxidase-derived superoxide and peroxynitrite. Arterioscler. Thromb. Vasc. Biol. 2006;26(12):2688–95. doi: 10.1161/01.ATV.0000249394.94588.82. [DOI] [PubMed] [Google Scholar]
- 61.Fukumura D, Gohongi T, Kadambi A, Izumi Y, Ang J, Yun CO, Buerk DG, Huang PL, Jain RK. Predominant role of endothelial nitric oxide synthase in vascular endothelial growth factor-induced angiogenesis and vascular permeability. Proc. Natl. Acad. Sci. USA. 2001;98(5):2604–9. doi: 10.1073/pnas.041359198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Harrison DG. Cellular and molecular mechanisms of endothelial cell dysfunction. J. Clin. Invest. 1997;100(9):2153–7. doi: 10.1172/JCI119751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Janssens S, Flaherty D, Nong Z, Varenne O, van Pelt N, Haustermans C, Zoldhelyi P, Gerard R, Collen D. Human endothelial nitric oxide synthase gene transfer inhibits vascular smooth muscle cell proliferation and neointima formation after balloon injury in rats. Circulation. 1998;97(13):1274–81. doi: 10.1161/01.cir.97.13.1274. [DOI] [PubMed] [Google Scholar]
- 64.Ju H, Zou R, Venema VJ, Venema RC. Direct interaction of endothelial nitric-oxide synthase and caveolin-1 inhibits synthase activity. J. Biol. Chem. 1997;272(30):18522–5. doi: 10.1074/jbc.272.30.18522. [DOI] [PubMed] [Google Scholar]
- 65.Kashiwagi M, Shinozaki M, Hirakata H, Tamaki K, Hirano T, Tokumoto M, Goto H, Okuda S, Fujishima M. Locally activated renin-angiotensin system associated with TGF-beta1 as a major factor for renal injury induced by chronic inhibition of nitric oxide synthase in rats. J. Am. Soc. Nephrol. 2000;11(4):616–24. doi: 10.1681/ASN.V114616. [DOI] [PubMed] [Google Scholar]
- 66.Keynan S, Hirshberg B, Levin-Iaina N, Wexler ID, Dahan R, Reinhartz E, Ovadia H, Wollman Y, Chernihovskey T, Iaina A, Raz I. Renal nitric oxide production during the early phase of experimental diabetes mellitus. Kidney Int. 2000;58(2):740–7. doi: 10.1046/j.1523-1755.2000.00220.x. [DOI] [PubMed] [Google Scholar]
- 67.Kiff RJ, Gardiner SM, Compton AM, Bennett T. The effects of endothelin-1 and NG-nitro-L-arginine methyl ester on regional haemodynamics in conscious rats with streptozotocin-induced diabetes mellitus. Br. J. Pharmacol. 1991;103(2):1321–6. doi: 10.1111/j.1476-5381.1991.tb09787.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.a Zhao HJ, Wang S, Cheng H, Zhang MZ, Takahashi T, Fogo AB, Breyer MD, Harris RC. Endothelial nitric oxide synthase deficiency produces accelerated nephropathy in diabetic mice. J. Am. Soc. Nephrol. 2006;17(10):2664–9. doi: 10.1681/ASN.2006070798. [DOI] [PMC free article] [PubMed] [Google Scholar]; b Mohan S, Konopinski R, Yan B, Centonze VE, Natarajan M. High glucose-induced IKK-Hsp-90 interaction contributes to endothelial dysfunction. Am. J. Physiol. Cell Physiol. 2009;296(1):C182–92. doi: 10.1152/ajpcell.00575.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Vallance P, Leone A, Calver A, Collier J, Moncada S. Accumulation of an endogenous inhibitor of nitric oxide synthesis in chronic renal failure. Lancet. 1992;339(8793):572–5. doi: 10.1016/0140-6736(92)90865-z. [DOI] [PubMed] [Google Scholar]
- 70.Tarnow L, Hovind P, Teerlink T, Stehouwer CD, Parving HH. Elevated plasma asymmetric dimethylarginine as a marker of cardiovascular morbidity in early diabetic nephropathy in type 1 diabetes. Diabetes Care. 2004;27(3):765–9. doi: 10.2337/diacare.27.3.765. [DOI] [PubMed] [Google Scholar]
- 71.Hanai K, Babazono T, Nyumura I, Toya K, Tanaka N, Tanaka M, Ishii A, Iwamoto Y. Asymmetric dimethylarginine is closely associated with the development and progression of nephropathy in patients with type 2 diabetes. Nephrol. Dial. Transplant. 2009;24(6):1884–8. doi: 10.1093/ndt/gfn716. [DOI] [PubMed] [Google Scholar]
- 72.Krzyzanowska K, Mittermayer F, Schernthaner GH, Brunner S, Brix JM, Aschauer S, Hollerl F, Wolzt M, Schernthaner G. Renal function but not asymmetric dimethylarginine is independently associated with retinopathy in type 2 diabetes. Cardiol. Res. Pract. 2011;2011:260191. doi: 10.4061/2011/260191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Itani SI, Saha AK, Kurowski TG, Coffin HR, Tornheim K, Ruderman NB. Glucose autoregulates its uptake in skeletal muscle: involvement of AMP-activated protein kinase. Diabetes. 2003;52(7):1635–40. doi: 10.2337/diabetes.52.7.1635. [DOI] [PubMed] [Google Scholar]
- 74.Alpert E, Gruzman A, Riahi Y, Blejter R, Aharoni P, Weisinger G, Eckel J, Kaiser N, Sasson S. Delayed autoregulation of glucose transport in vascular endothelial cells. Diabetologia. 2005;48(4):752–5. doi: 10.1007/s00125-005-1681-y. [DOI] [PubMed] [Google Scholar]
- 75.Iyengar SK, Abboud HE, Goddard KA, Saad MF, Adler SG, Arar NH, Bowden DW, Duggirala R, Elston RC, Hanson RL, Ipp E, Kao WH, Kimmel PL, Klag MJ, Knowler WC, Meoni LA, Nelson RG, Nicholas SB, Pahl MV, Parekh RS, Quade SR, Rich SS, Rotter JI, Scavini M, Schelling JR, Sedor JR, Sehgal AR, Shah VO, Smith MW, Taylor KD, Winkler CA, Zager PG, Freedman BI. Genome-wide scans for diabetic nephropathy and albuminuria in multiethnic populations: the family investigation of nephropathy and diabetes (FIND). Diabetes. 2007;56(6):1577–85. doi: 10.2337/db06-1154. [DOI] [PubMed] [Google Scholar]
- 76.Vardarli I, Baier LJ, Hanson RL, Akkoyun I, Fischer C, Rohmeiss P, Basci A, Bartram CR, Van Der Woude FJ, Janssen B. Gene for susceptibility to diabetic nephropathy in type 2 diabetes maps to 18q22.3-23. Kidney Int. 2002;62(6):2176–83. doi: 10.1046/j.1523-1755.2002.00663.x. [DOI] [PubMed] [Google Scholar]
- 77.Orth SR, Schroeder T, Ritz E, Ferrari P. Effects of smoking on renal function in patients with type 1 and type 2 diabetes mellitus. Nephrol. Dial. Transplant. 2005;20(11):2414–9. doi: 10.1093/ndt/gfi022. [DOI] [PubMed] [Google Scholar]
- 78.Zhang HM, Dang H, Kamat A, Yeh CK, Zhang BX. Geldanamycin derivative ameliorates high fat diet-induced renal failure in diabetes. PLoS One. 2012;7(3):e32746. doi: 10.1371/journal.pone.0032746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Li J, Gobe G. Protein kinase C activation and its role in kidney disease. Nephrology (Carlton) 2006;11(5):428–34. doi: 10.1111/j.1440-1797.2006.00673.x. [DOI] [PubMed] [Google Scholar]
- 80.Inoguchi T, Sonta T, Tsubouchi H, Etoh T, Kakimoto M, Sonoda N, Sato N, Sekiguchi N, Kobayashi K, Sumimoto H, Utsumi H, Nawata H. Protein kinase C-dependent increase in reactive oxygen species (ROS) production in vascular tissues of diabetes: role of vascular NAD(P)H oxidase. J. Am. Soc. Nephrol. 2003;14(8 Suppl 3):S227–32. doi: 10.1097/01.asn.0000077407.90309.65. [DOI] [PubMed] [Google Scholar]
- 81.Menne J, Meier M, Park JK, Haller H. Inhibition of protein kinase C in diabetic nephropathy--where do we stand? Nephrol. Dial. Transplant. 2009;24(7):2021–3. doi: 10.1093/ndt/gfp150. [DOI] [PubMed] [Google Scholar]
- 82.Ha H, Yu MR, Choi YJ, Lee HB. Activation of protein kinase c-delta and c-epsilon by oxidative stress in early diabetic rat kidney. Am. J. Kidney Dis. 2001;38(4 Suppl 1):S204–7. doi: 10.1053/ajkd.2001.27446. [DOI] [PubMed] [Google Scholar]
- 83.Meier M, Menne J, Haller H. Targeting the protein kinase C family in the diabetic kidney: lessons from analysis of mutant mice. Diabetologia. 2009;52(5):765–75. doi: 10.1007/s00125-009-1278-y. [DOI] [PubMed] [Google Scholar]
- 84.Meier M, Menne J, Park JK, Haller H. Nailing down PKC isoform specificity in diabetic nephropathy two's company, three's a crowd. Nephrol. Dial. Transplant. 2007;22(9):2421–5. doi: 10.1093/ndt/gfm320. [DOI] [PubMed] [Google Scholar]
- 85.Geraldes P, King GL. Activation of protein kinase C isoforms and its impact on diabetic complications. Circ. Res. 2010;106(8):1319–31. doi: 10.1161/CIRCRESAHA.110.217117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Toth E, Racz A, Toth J, Kaminski PM, Wolin MS, Bagi Z, Koller A. Contribution of polyol pathway to arteriolar dysfunction in hyperglycemia. Role of oxidative stress, reduced NO, and enhanced PGH(2)/TXA(2) mediation. Am. J. Physiol. Heart Circ. Physiol. 2007;293(5):H3096–104. doi: 10.1152/ajpheart.01335.2006. [DOI] [PubMed] [Google Scholar]
- 87.Mauer SM, Steffes MW, Azar S, Brown DM. Effects of sorbinil on glomerular structure and function in long-term-diabetic rats. Diabetes. 1989;38(7):839–46. doi: 10.2337/diab.38.7.839. [DOI] [PubMed] [Google Scholar]
- 88.Pedersen MM, Christiansen JS, Mogensen CE. Reduction of glomerular hyperfiltration in normoalbuminuric IDDM patients by 6 mo of aldose reductase inhibition. Diabetes. 1991;40(5):527–31. doi: 10.2337/diab.40.5.527. [DOI] [PubMed] [Google Scholar]
- 89.Cheng HF, Wang CJ, Moeckel GW, Zhang MZ, McKanna JA, Harris RC. Cyclooxygenase-2 inhibitor blocks expression of mediators of renal injury in a model of diabetes and hypertension. Kidney Int. 2002;62(3):929–39. doi: 10.1046/j.1523-1755.2002.00520.x. [DOI] [PubMed] [Google Scholar]
- 90.Sato H, Iwano M, Akai Y, Kurioka H, Kubo A, Yamaguchi T, Hirata E, Kanauchi M, Dohi K. Increased excretion of urinary transforming growth factor beta 1 in patients with diabetic nephropathy. Am. J. Nephrol. 1998;18(6):490–4. doi: 10.1159/000013415. [DOI] [PubMed] [Google Scholar]
- 91.Ziyadeh FN. Mediators of diabetic renal disease: the case for tgf-Beta as the major mediator. J. Am. Soc. Nephrol. 2004;15(1):S55–7. doi: 10.1097/01.asn.0000093460.24823.5b. [DOI] [PubMed] [Google Scholar]
- 92.Nakagawa T, Li JH, Garcia G, Mu W, Piek E, Bottinger EP, Chen Y, Zhu HJ, Kang DH, Schreiner GF, Lan HY, Johnson RJ. TGF-beta induces proangiogenic and antiangiogenic factors via parallel but distinct Smad pathways. Kidney Int. 2004;66(2):605–13. doi: 10.1111/j.1523-1755.2004.00780.x. [DOI] [PubMed] [Google Scholar]
- 93.Soma J, Sato K, Saito H, Tsuchiya Y. Effect of tranilast in early-stage diabetic nephropathy. Nephrol. Dial. Transplant. 2006;21(10):2795–9. doi: 10.1093/ndt/gfl325. [DOI] [PubMed] [Google Scholar]
- 94.Santibanez JF, Quintanilla M, Bernabeu C. TGF-beta/TGF-beta receptor system and its role in physiological and pathological conditions. Clin. Sci. (Lond) 2011;121(6):233–51. doi: 10.1042/CS20110086. [DOI] [PubMed] [Google Scholar]
- 95.Saura M, Zaragoza C, Cao W, Bao C, Rodriguez-Puyol M, Rodriguez-Puyol D, Lowenstein CJ. Smad2 mediates transforming growth factor-beta induction of endothelial nitric oxide synthase expression. Circ. Res. 2002;91(9):806–13. doi: 10.1161/01.res.0000040397.23817.e5. [DOI] [PubMed] [Google Scholar]
- 96.van Nieuwenhoven FA, Jensen LJ, Flyvbjerg A, Goldschmeding R. Imbalance of growth factor signalling in diabetic kidney disease: is connective tissue growth factor (CTGF, CCN2) the perfect intervention point? Nephrol. Dial. Transplant. 2005;20(1):6–10. doi: 10.1093/ndt/gfh570. [DOI] [PubMed] [Google Scholar]
- 97.Goligorsky MS, Chen J, Brodsky S. Workshop: endothelial cell dysfunction leading to diabetic nephropathy : focus on nitric oxide. Hypertension. 2001;37(2 Part 2):744–8. doi: 10.1161/01.hyp.37.2.744. [DOI] [PubMed] [Google Scholar]
- 98.Komers R, Anderson S. Paradoxes of nitric oxide in the diabetic kidney. Am. J. Physiol. Renal. Physiol. 2003;284(6):F1121–37. doi: 10.1152/ajprenal.00265.2002. [DOI] [PubMed] [Google Scholar]
- 99.Cheng H, Wang H, Fan X, Paueksakon P, Harris RC. Improvement of endothelial nitric oxide synthase activity retards the progression of diabetic nephropathy in db/db mice. Kidney Int. 2012;82(11):1176–83. doi: 10.1038/ki.2012.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.a Clarkson P, Celermajer DS, Donald AE, Sampson M, Sorensen KE, Adams M, Yue DK, Betteridge DJ, Deanfield JE. Impaired vascular reactivity in insulin-dependent diabetes mellitus is related to disease duration and low density lipoprotein cholesterol levels. J. Am. Coll. Cardiol. 1996;28(3):573–9. doi: 10.1016/0735-1097(96)82380-1. [DOI] [PubMed] [Google Scholar]; b Williams SB, Cusco JA, Roddy MA, Johnstone MT, Creager MA. Impaired nitric oxide-mediated vasodilation in patients with non-insulin-dependent diabetes mellitus. J. Am. Coll. Cardiol. 1996;27(3):567–74. doi: 10.1016/0735-1097(95)00522-6. [DOI] [PubMed] [Google Scholar]
- 101.a Mohan S, Reddick RL, Musi N, Horn DA, Yan B, Prihoda TJ, Natarajan M, Abboud-Werner SL. Diabetic eNOS knockout mice develop distinct macro- and microvascular complications. Lab. Invest. 2008;88(5):515–28. doi: 10.1038/labinvest.2008.23. [DOI] [PubMed] [Google Scholar]; b Kanetsuna Y, Takahashi K, Nagata M, Gannon MA, Breyer MD, Harris RC, Takahashi T. Deficiency of endothelial nitric-oxide synthase confers susceptibility to diabetic nephropathy in nephropathy-resistant inbred mice. Am. J. Pathol. 2007;170(5):1473–84. doi: 10.2353/ajpath.2007.060481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ahluwalia TS, Ahuja M, Rai TS, Kohli HS, Sud K, Bhansali A, Khullar M. Endothelial nitric oxide synthase gene haplotypes and diabetic nephropathy among Asian Indians. Mol. Cell Biochem. 2008;314(1-2):9–17. doi: 10.1007/s11010-008-9759-8. [DOI] [PubMed] [Google Scholar]; b Zanchi A, Moczulski DK, Hanna LS, Wantman M, Warram JH, Krolewski AS. Risk of advanced diabetic nephropathy in type 1 diabetes is associated with endothelial nitric oxide synthase gene polymorphism. Kidney Int. 2000;57(2):405–13. doi: 10.1046/j.1523-1755.2000.00860.x. [DOI] [PubMed] [Google Scholar]; c Neugebauer S, Baba T, Watanabe T. Association of the nitric oxide synthase gene polymorphism with an increased risk for progression to diabetic nephropathy in type 2 diabetes. Diabetes. 2000;49(3):500–3. doi: 10.2337/diabetes.49.3.500. [DOI] [PubMed] [Google Scholar]
- 103.Munzel T, Daiber A, Ullrich V, Mulsch A. Vascular consequences of endothelial nitric oxide synthase uncoupling for the activity and expression of the soluble guanylyl cyclase and the cGMP-dependent protein kinase. Arterioscler. Thromb. Vasc. Biol. 2005;25(8):1551–7. doi: 10.1161/01.ATV.0000168896.64927.bb. [DOI] [PubMed] [Google Scholar]
- 104.Stuehr DJ, Wei CC, Wang Z, Hille R. Exploring the redox reactions between heme and tetrahydrobiopterin in the nitric oxide synthases. Dalton Trans. 2005;(21):3427–35. doi: 10.1039/b506355h. [DOI] [PubMed] [Google Scholar]
- 105.Alp NJ, Channon KM. Regulation of endothelial nitric oxide synthase by tetrahydrobiopterin in vascular disease. Arterioscler. Thromb. Vasc. Biol. 2004;24(3):413–20. doi: 10.1161/01.ATV.0000110785.96039.f6. [DOI] [PubMed] [Google Scholar]
- 106.Schmidt TS, Alp NJ. Mechanisms for the role of tetrahydrobiopterin in endothelial function and vascular disease. Clin. Sci. (Lond) 2007;113(2):47–63. doi: 10.1042/CS20070108. [DOI] [PubMed] [Google Scholar]
- 107.Baris N, Erdogan M, Sezer E, Saygili F, Mert Ozgonul A, Turgan N, Ersoz B. Alterations in L-arginine and inflammatory markers in type 2 diabetic patients with and without microalbuminuria. Acta diabetologica. 2009;46(4):309–16. doi: 10.1007/s00592-008-0089-9. [DOI] [PubMed] [Google Scholar]
- 108.Kohli R, Meininger CJ, Haynes TE, Yan W, Self JT, Wu G. Dietary L-arginine supplementation enhances endothelial nitric oxide synthesis in streptozotocin-induced diabetic rats. J. Nutr. 2004;134(3):600–8. doi: 10.1093/jn/134.3.600. [DOI] [PubMed] [Google Scholar]
- 109.a Wu G, Meininger CJ. Nitric oxide and vascular insulin resistance. Biofactors. 2009;35(1):21–7. doi: 10.1002/biof.3. [DOI] [PubMed] [Google Scholar]; b Lucotti P, Setola E, Monti LD, Galluccio E, Costa S, Sandoli EP, Fermo I, Rabaiotti G, Gatti R, Piatti P. Beneficial effects of a long-term oral L-arginine treatment added to a hypocaloric diet and exercise training program in obese, insulin-resistant type 2 diabetic patients. Am. J. Physiol. Endocrinol. Metab. 2006;291(5):E906–12. doi: 10.1152/ajpendo.00002.2006. [DOI] [PubMed] [Google Scholar]
- 110.Meininger CJ, Marinos RS, Hatakeyama K, Martinez-Zaguilan R, Rojas JD, Kelly KA, Wu G. Impaired nitric oxide production in coronary endothelial cells of the spontaneously diabetic BB rat is due to tetrahydrobiopterin deficiency. Biochem. J. 2000;349(Pt 1):353–6. doi: 10.1042/0264-6021:3490353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Heitzer T, Krohn K, Albers S, Meinertz T. Tetrahydrobiopterin improves endothelium-dependent vasodilation by increasing nitric oxide activity in patients with Type II diabetes mellitus. Diabetologia. 2000;43(11):1435–8. doi: 10.1007/s001250051551. [DOI] [PubMed] [Google Scholar]
- 112.Ferre J, Naylor EW. Sepiapterin reductase in human amniotic and skin fibroblasts, chorionic villi, and various blood fractions. Clin. Chim. Acta. 1988;174(3):271–82. doi: 10.1016/0009-8981(88)90053-8. [DOI] [PubMed] [Google Scholar]
- 113.a Li H, Wallerath T, Munzel T, Forstermann U. Regulation of endothelial-type NO synthase expression in pathophysiology and in response to drugs. Nitric Oxide. 2002;7(3):149–64. doi: 10.1016/s1089-8603(02)00111-8. [DOI] [PubMed] [Google Scholar]; b Searles CD. Transcriptional and posttranscriptional regulation of endothelial nitric oxide synthase expression. Am. J. Physiol. Cell Physiol. 2006;291(5):C803–16. doi: 10.1152/ajpcell.00457.2005. [DOI] [PubMed] [Google Scholar]
- 114.Thomas SR, Witting PK, Drummond GR. Redox control of endothelial function and dysfunction: molecular mechanisms and therapeutic opportunities. Antioxid. Redox Signal. 2008;10(10):1713–65. doi: 10.1089/ars.2008.2027. [DOI] [PubMed] [Google Scholar]
- 115.Luo Z, Fujio Y, Kureishi Y, Rudic RD, Daumerie G, Fulton D, Sessa WC, Walsh K. Acute modulation of endothelial Akt/PKB activity alters nitric oxide-dependent vasomotor activity in vivo. J. Clin. Invest. 2000;106(4):493–9. doi: 10.1172/JCI9419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Mount PF, Kemp BE, Power DA. Regulation of endothelial and myocardial NO synthesis by multi-site eNOS phosphorylation. J. Mol. Cell Cardiol. 2007;42(2):271–9. doi: 10.1016/j.yjmcc.2006.05.023. [DOI] [PubMed] [Google Scholar]
- 117.Komers R, Schutzer WE, Reed JF, Lindsley JN, Oyama TT, Buck DC, Mader SL, Anderson S. Altered endothelial nitric oxide synthase targeting and conformation and caveolin-1 expression in the diabetic kidney. Diabetes. 2006;55(6):1651–9. doi: 10.2337/db05-1595. [DOI] [PubMed] [Google Scholar]
- 118.Jagnandan D, Sessa WC, Fulton D. Intracellular location regulates calcium-calmodulin-dependent activation of organelle-restricted eNOS. Am. J. Physiol. Cell. Physiol. 2005;289(4):C1024–33. doi: 10.1152/ajpcell.00162.2005. [DOI] [PubMed] [Google Scholar]
- 119.Minshall RD, Sessa WC, Stan RV, Anderson RG, Malik AB. Caveolin regulation of endothelial function. Am. J. Physiol. Lung Cell Mol. Physiol. 2003;285(6):L1179–83. doi: 10.1152/ajplung.00242.2003. [DOI] [PubMed] [Google Scholar]
- 120.Lajer M, Tarnow L, Jorsal A, Teerlink T, Parving HH, Rossing P. Plasma concentration of asymmetric dimethylarginine (ADMA) predicts cardiovascular morbidity and mortality in type 1 diabetic patients with diabetic nephropathy. Diabetes Care. 2008;31(4):747–52. doi: 10.2337/dc07-1762. [DOI] [PubMed] [Google Scholar]
- 121.Schulze PC, Yoshioka J, Takahashi T, He Z, King GL, Lee RT. Hyperglycemia promotes oxidative stress through inhibition of thioredoxin function by thioredoxin-interacting protein. J. Biol. Chem. 2004;279(29):30369–74. doi: 10.1074/jbc.M400549200. [DOI] [PubMed] [Google Scholar]
- 122.Beckman JS, Koppenol WH. Nitric oxide, superoxide, and peroxynitrite: the good, the bad, and ugly. Am. J. Physiol. 1996;271(5 Pt 1):C1424–37. doi: 10.1152/ajpcell.1996.271.5.C1424. [DOI] [PubMed] [Google Scholar]
- 123.Szabo C, Zanchi A, Komjati K, Pacher P, Krolewski AS, Quist WC, LoGerfo FW, Horton ES, Veves A. Poly(ADPRibose) polymerase is activated in subjects at risk of developing type 2 diabetes and is associated with impaired vascular reactivity. Circulation. 2002;106(21):2680–6. doi: 10.1161/01.cir.0000038365.78031.9c. [DOI] [PubMed] [Google Scholar]
- 124.El-Remessy AB, Tawfik HE, Matragoon S, Pillai B, Caldwell RB, Caldwell RW. Peroxynitrite mediates diabetes-induced endothelial dysfunction: possible role of Rho kinase activation. Exp. Diabetes Res. 2010;2010:247861. doi: 10.1155/2010/247861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Anderson MM, Heinecke JW. Production of N(epsilon)-(carboxymethyl)lysine is impaired in mice deficient in NADPH oxidase: a role for phagocyte-derived oxidants in the formation of advanced glycation end products during inflammation. Diabetes. 2003;52(8):2137–43. doi: 10.2337/diabetes.52.8.2137. [DOI] [PubMed] [Google Scholar]
- 126.Alp NJ, Channon KM. Regulation of endothelial nitric oxide synthase by tetrahydrobiopterin in vascular disease. Arterioscler. Thromb. 2004;24(3):413–20. doi: 10.1161/01.ATV.0000110785.96039.f6. [DOI] [PubMed] [Google Scholar]
- 127.Du X, Edelstein D, Obici S, Higham N, Zou MH, Brownlee M. Insulin resistance reduces arterial prostacyclin synthase and eNOS activities by increasing endothelial fatty acid oxidation. Clin. Investig. 2006;116(4):1071–80. doi: 10.1172/JCI23354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Kofler S, Nickel T, Weis M. Role of cytokines in cardiovascular diseases: a focus on endothelial responses to inflammation. Clin. Sci. (Lond) 2005;108(3):205–13. doi: 10.1042/CS20040174. [DOI] [PubMed] [Google Scholar]
- 129.Menon MC, Chuang PY, He CJ. The glomerular filtration barrier: components and crosstalk. Int. J. Nephrol. 2012;2012:749010. doi: 10.1155/2012/749010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Satchell SC, Anderson KL, Mathieson PW. Angiopoietin 1 and vascular endothelial growth factor modulate human glomerular endothelial cell barrier properties. J. Am. Soc. Nephrol. 2004;15(3):566–74. doi: 10.1097/01.asn.0000115397.22519.03. [DOI] [PubMed] [Google Scholar]
- 131.Sison K, Eremina V, Baelde H, Min W, Hirashima M, Fantus IG, Quaggin SE. Glomerular structure and function require paracrine, not autocrine, VEGF-VEGFR-2 signaling. J. Am. Soc. Nephrol. 2010;21(10):1691–701. doi: 10.1681/ASN.2010030295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Cooper ME, Vranes D, Youssef S, Stacker SA, Cox AJ, Rizkalla B, Casley DJ, Bach LA, Kelly DJ, Gilbert RE. Increased renal expression of vascular endothelial growth factor (VEGF) and its receptor VEGFR-2 in experimental diabetes. Diabetes. 1999;48(11):2229–39. doi: 10.2337/diabetes.48.11.2229. [DOI] [PubMed] [Google Scholar]
- 133.Lindenmeyer MT, Kretzler M, Boucherot A, Berra S, Yasuda Y, Henger A, Eichinger F, Gaiser S, Schmid H, Rastaldi MP, Schrier RW, Schlondorff D, Cohen CD. Interstitial vascular rarefaction and reduced VEGF-A expression in human diabetic nephropathy. J. Am. Soc. Nephrol. 2007;18(6):1765–76. doi: 10.1681/ASN.2006121304. [DOI] [PubMed] [Google Scholar]
- 134.Baelde HJ, Eikmans M, Lappin DW, Doran PP, Hohenadel D, Brinkkoetter PT, van der Woude FJ, Waldherr R, Rabelink TJ, de Heer E, Bruijn JA. Reduction of VEGF-A and CTGF expression in diabetic nephropathy is associated with podocyte loss. Kidney Int. 2007;71(7):637–45. doi: 10.1038/sj.ki.5002101. [DOI] [PubMed] [Google Scholar]
- 135.Nakagawa T, Kosugi T, Haneda M, Rivard CJ, Long DA. Abnormal angiogenesis in diabetic nephropathy. Diabetes. 2009;58(7):1471–8. doi: 10.2337/db09-0119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Nakagawa T, Sato W, Glushakova O, Heinig M, Clarke T, Campbell-Thompson M, Yuzawa Y, Atkinson MA, Johnson RJ, Croker B. Diabetic endothelial nitric oxide synthase knockout mice develop advanced diabetic nephropathy. J. Am. Soc. Nephrol. 2007;18(2):539–50. doi: 10.1681/ASN.2006050459. [DOI] [PubMed] [Google Scholar]
- 137.Bussolati B, Dunk C, Grohman M, Kontos CD, Mason J, Ahmed A. Vascular endothelial growth factor receptor-1 modulates vascular endothelial growth factor-mediated angiogenesis via nitric oxide. Am. J. Pathol. 2001;159(3):993–1008. doi: 10.1016/S0002-9440(10)61775-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Eremina V, Baelde HJ, Quaggin SE. Role of the VEGF--a signaling pathway in the glomerulus: evidence for crosstalk between components of the glomerular filtration barrier. Nephron Physiol. 2007;106(2):p32–7. doi: 10.1159/000101798. [DOI] [PubMed] [Google Scholar]
- 139.Ku CH, White KE, Dei Cas A, Hayward A, Webster Z, Bilous R, Marshall S, Viberti G, Gnudi L. Inducible overexpression of sFlt-1 in podocytes ameliorates glomerulopathy in diabetic mice. Diabetes. 2008;57(10):2824–33. doi: 10.2337/db08-0647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Hohenstein B, Hausknecht B, Boehmer K, Riess R, Brekken RA, Hugo CP. Local VEGF activity but not VEGF expression is tightly regulated during diabetic nephropathy in man. Kidney Int. 2006;69(9):1654–61. doi: 10.1038/sj.ki.5000294. [DOI] [PubMed] [Google Scholar]
- 141.de Vriese AS, Tilton RG, Elger M, Stephan CC, Kriz W, Lameire NH. Antibodies against vascular endothelial growth factor improve early renal dysfunction in experimental diabetes. J. Am. Soc. Nephrol. 2001;12(5):993–1000. doi: 10.1681/ASN.V125993. [DOI] [PubMed] [Google Scholar]
- 142.Sung SH, Ziyadeh FN, Wang A, Pyagay PE, Kanwar YS, Chen S. Blockade of vascular endothelial growth factor signaling ameliorates diabetic albuminuria in mice. J. Am. Soc. Nephrol. 2006;17(11):3093–104. doi: 10.1681/ASN.2006010064. [DOI] [PubMed] [Google Scholar]
- 143.Sivaskandarajah GA, Jeansson M, Maezawa Y, Eremina V, Baelde HJ, Quaggin SE. Vegfa Protects the Glomerular Microvasculature in Diabetes. Diabetes. 2012;61(11):2958–66. doi: 10.2337/db11-1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Satchell SC, Harper SJ, Tooke JE, Kerjaschki D, Saleem MA, Mathieson PW. Human podocytes express angiopoietin 1, a potential regulator of glomerular vascular endothelial growth factor. J. Am. Soc. Nephrol. 2002;13(2):544–50. doi: 10.1681/ASN.V132544. [DOI] [PubMed] [Google Scholar]
- 145.a Davis B, Dei Cas A, Long DA, White KE, Hayward A, Ku CH, Woolf AS, Bilous R, Viberti G, Gnudi L. Podocyte-specific expression of angiopoietin-2 causes proteinuria and apoptosis of glomerular endothelia. J. Am. Soc. Nephrol. 2007;18(8):2320–9. doi: 10.1681/ASN.2006101093. [DOI] [PubMed] [Google Scholar]; b Yuan HT, Suri C, Landon DN, Yancopoulos GD, Woolf AS. Angiopoietin-2 is a site-specific factor in differentiation of mouse renal vasculature. J. Am. Soc. Nephrol. JASN. 2000;11(6):1055–66. doi: 10.1681/ASN.V1161055. [DOI] [PubMed] [Google Scholar]
- 146.Lim HS, Lip GY, Blann AD. Angiopoietin-1 and angiopoietin-2 in diabetes mellitus: relationship to VEGF, glycaemic control, endothelial damage/dysfunction and atherosclerosis. Atherosclerosis. 2005;180(1):113–8. doi: 10.1016/j.atherosclerosis.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 147.Schlondorff D, Banas B. The mesangial cell revisited: no cell is an island. J. Am. Soc. Nephrol. 2009;20(6):1179–87. doi: 10.1681/ASN.2008050549. [DOI] [PubMed] [Google Scholar]
- 148.Nitta K, Uchida K, Tsutsui T, Kawashima A, Yumura W, Nihei H. Glomerular endothelial cells promote mesangial cell growth via a PDGF-Like substance. Life Sci. 1995;56(3):143–50. doi: 10.1016/0024-3205(94)00428-u. [DOI] [PubMed] [Google Scholar]
- 149.Bohle A, Wehrmann M, Bogenschutz O, Batz C, Muller CA, Muller GA. The pathogenesis of chronic renal failure in diabetic nephropathy. Investigation of 488 cases of diabetic glomerulosclerosis. Pathol. Res. Pract. 1991;187(2-3):251–9. doi: 10.1016/s0344-0338(11)80780-6. [DOI] [PubMed] [Google Scholar]
- 150.Wolf G, Neilson EG, Goldfarb S, Ziyadeh FN. The influence of glucose concentration on angiotensin II-induced hypertrophy of proximal tubular cells in culture. Biochem. Biophys. Res. Commun. 1991;176(2):902–9. doi: 10.1016/s0006-291x(05)80271-2. [DOI] [PubMed] [Google Scholar]
- 151.Nangaku M. Chronic hypoxia and tubulointerstitial injury: a final common pathway to end-stage renal failure. J Am. Soc. Nephrol. 2006;17(1):17–25. doi: 10.1681/ASN.2005070757. [DOI] [PubMed] [Google Scholar]
- 152.Tasnim F, Zink D. Cross talk between primary human renal tubular cells and endothelial cells in cocultures. Am. J. Physiol. Renal Physiol. 2012;302(8):F1055–62. doi: 10.1152/ajprenal.00621.2011. [DOI] [PubMed] [Google Scholar]
- 153.Galkina E, Ley K. Leukocyte recruitment and vascular injury in diabetic nephropathy. J. Am. Soc. Nephrol. 2006;17(2):368–77. doi: 10.1681/ASN.2005080859. [DOI] [PubMed] [Google Scholar]
- 154.Seron D, Cameron JS, Haskard DO. Expression of VCAM-1 in the normal and diseased kidney. Nephrol. Dial. Transplant. 1991;6(12):917–22. doi: 10.1093/ndt/6.12.917. [DOI] [PubMed] [Google Scholar]
- 155.Smith SW, Chand S, Savage CO. Biology of the renal pericyte. Nephrol. Dial. Transplant. 2012;27(6):2149–55. doi: 10.1093/ndt/gfs134. [DOI] [PubMed] [Google Scholar]
- 156.Armulik A, Abramsson A, Betsholtz C. Endothelial/pericyte interactions. Circ. Res. 2005;97(6):512–23. doi: 10.1161/01.RES.0000182903.16652.d7. [DOI] [PubMed] [Google Scholar]
- 157.Gaengel K, Genove G, Armulik A, Betsholtz C. Endothelial-mural cell signaling in vascular development and angiogenesis. Arterioscler. Thromb. 2009;29(5):630–8. doi: 10.1161/ATVBAHA.107.161521. [DOI] [PubMed] [Google Scholar]
- 158.Hammes HP. Pericytes and the pathogenesis of diabetic retinopathy. Horm. Metab. Res. 2005;37(1):39–43. doi: 10.1055/s-2005-861361. [DOI] [PubMed] [Google Scholar]
- 159.Richards OC, Raines SM, Attie AD. The role of blood vessels, endothelial cells, and vascular pericytes in insulin secretion and peripheral insulin action. Endocr. Rev. 2010;31(3):343–63. doi: 10.1210/er.2009-0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Nakagawa T, Tanabe K, Croker BP, Johnson RJ, Grant MB, Kosugi T, Li Q. Endothelial dysfunction as a potential contributor in diabetic nephropathy. Nat. Rev. Nephrol. 2011;7(1):36–44. doi: 10.1038/nrneph.2010.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Bassi R, Trevisani A, Tezza S, Ben Nasr M, Gatti F, Vergani A, Farina A, Fiorina P. Regenerative therapies for diabetic microangiopathy. Exp. Diabetes Res. 2012;2012:916560. doi: 10.1155/2012/916560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Ikarashi K, Li B, Suwa M, Kawamura K, Morioka T, Yao J, Khan F, Uchiyama M, Oite T. Bone marrow cells contribute to regeneration of damaged glomerular endothelial cells. Kidney Int. 2005;67(5):1925–33. doi: 10.1111/j.1523-1755.2005.00291.x. [DOI] [PubMed] [Google Scholar]
- 163.Reinhard H, Jacobsen PK, Lajer M, Tarnow L, Astrup AS, Kim WY, Pedersen N, Billestrup N, Mandrup-Poulsen T, Parving HH, Rossing P. Endothelial progenitor cells in longstanding asymptomatic type 1 diabetic patients with or without diabetic nephropathy. Nephron. Clin. Pract. 2011;118(3):c309–14. doi: 10.1159/000322667. [DOI] [PubMed] [Google Scholar]