Abstract
Background
During cardiac arrest, end-tidal carbon dioxide (ETCO2) monitoring is recommended as a chest compression performance indicator. However, its frequency of use during out-of-hospital cardiac arrest (OHCA) and its benefits have never been evaluated in real clinical situations.
Objective
We investigated OHCA patients in Taiwan to evaluate the frequency of ETCO2 monitoring and its effects on sustained return of spontaneous circulation (ROSC).
Methods
We sampled the Taiwan National Health Insurance claims database, which contains 1 million beneficiaries. All adult beneficiaries older than 18 years who presented with OHCA and received chest compression between 1 January 2005 and 31 December 2012 were enrolled. We further identified patients with ETCO2 monitoring and matched each 1 with 20 patients who did not receive ETCO2 monitoring based on their propensity scores. A simple conditional logistic regression model was applied to compare the odds ratio (OR) for sustained ROSC in the matched cohorts.
Results
A total of 5041 OHCA patients were enrolled. The frequency of ETCO2 monitoring has increased since 2010 but still is low. After matching, 53 patients with ETCO2 monitoring and 1060 without ETCO2 monitoring were selected. The OR of sustained ROSC in the ETCO2 group was significantly increased (2.38, 95 % CI 1.28–4.42).
Conclusion
Patients who received ETCO2 monitoring during OHCA had a higher possibility of sustained ROSC, but the overall use of ETCO2 monitoring is still low despite strong recommendations for its use.
Electronic supplementary material
The online version of this article (doi:10.1186/s13049-015-0187-y) contains supplementary material, which is available to authorized users.
Keywords: End-tidal carbon dioxide, Cardiac arrest, Out-of-hospital cardiac events, Capnography
Introduction
Out-of-hospital cardiac arrest (OHCA) is a major cause of morbidity and mortality around the world. In the United States, the estimated annual incidence of OHCA ranges from 300,000 to 350,000 each year [1, 2]. Wider application of the improved algorithms in the Advanced Cardiac Life Support (ACLS) recommendations, such as early defibrillation and high-quality cardiopulmonary resuscitation (CPR), have led to increased survival rates among OHCA patients [3–5]. Because CPR consistency is an important factor, end-tidal carbon dioxide (ETCO2) monitoring has recently been suggested as an adjunctive tool for monitoring the effectiveness of chest compressions during resuscitations [3, 6].
The height of the ETCO2 level during CPR is well correlated with cardiac output during chest compression [7–9], and feedback about an inadequate level can help the team to evaluate possible causes such as misplaced or displaced tracheal tube, fatigue of the team member, suboptimal chest compressions, cardiac tamponade, or pneumothorax. In this way the resuscitation can be individualized, and better CPR delivery may be achieved. However, to our knowledge, despite the strong recommendations from ACLS, the frequency of ETCO2 use during OHCA and its possible influence on CPR quality and survival, have not been evaluated in population-based studies.
In this study, a large administrative database was used to assess sustained ROSC in OHCA patients who were treated with ETCO2 monitoring in Taiwan. We hypothesized that use of ETCO2 monitoring may be associated with a higher possibility of sustained ROSC because of real-time feedback about the quality of chest compression. The results of this study may help clinicians to place more emphasis on the use of ETCO2 monitoring in frequently encountered situations.
Methods
Ethics statement
This study was initiated after its protocol was approved by the Institutional Review Board of Dalin Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Taiwan, and was conducted in conformity with the Declaration of Helsinki.
Database
The National Health Insurance (NHI) program was implemented in Taiwan in 1995 and provides compulsory universal health insurance. It enrolls about 99 % of the Taiwanese population and contracts with 97 % of all the country’s medical providers [10, 11]. The database contains comprehensive information about all insured subjects, including sex, date of birth, residential or work area, dates of clinical visits, diagnoses identified by International Classification of Diseases (Ninth Revision) Clinical Modification (ICD-9-CM) diagnostic codes, details of prescribed medications and procedures administered, expenditure amounts, and outcome at hospital discharge (i.e., recovered, died, or transferred out) [12]. A random sample of 1,000,000 people who received health benefits from the NHI program was selected based on calendar-year 2005 reimbursement data and was considered representative of the entire population; according to the Taiwan National Health Research Institute, the group did not differ statistically from the larger cohort in age, sex, or health care costs [13, 14]. This sample was used as our study cohort.
Study population
The population sample was followed from 1 January 2003 to 31 December 2012 (a total of 10 years). For our study cohort, we first identified individuals who were still alive in 2005 and were older than 18 years at the time of OHCA. OHCA was defined by the ICD-9-CM codes ventricular fibrillation (427.4), cardiac arrest (427.5), and sudden death (798.0–798.9) in outpatient clinic records. To avoid including patients who had Do Not Attempt Resuscitation orders, no chance of survival, and coding errors, we excluded patients on whom no chest compression was attempted. ETCO2 monitoring was defined by the charge record for continuous capnography during the visits. For each charge record of ETCO2, the institutes could claim for about US$ 14 from the Bureau of National Health Insurance. After exclusions, we identified 83 patients who received ETCO2 monitoring and 4958 who did not receive such monitoring. In order to identify sustained ROSC, each patient was tracked if he or she was hospitalized after OHCA (Fig. 1).
Fig. 1.
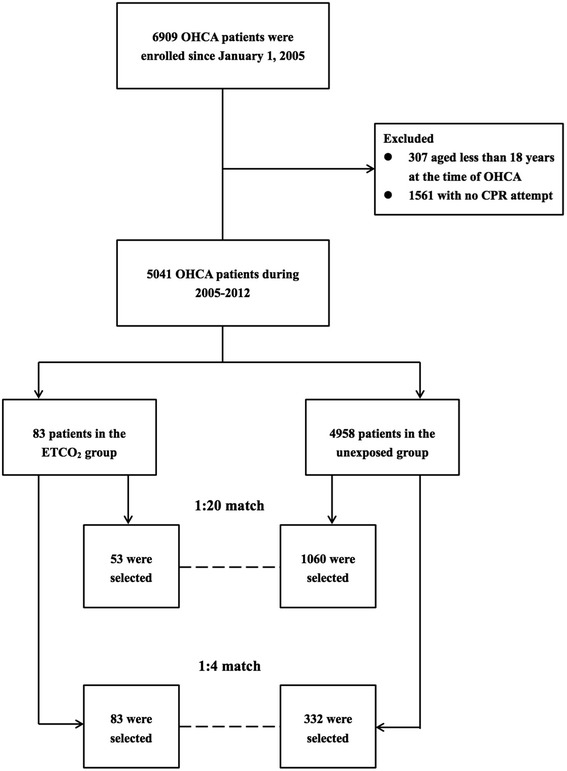
Flow diagram of the population-based study
Prespecified covariates
In order to investigate a significant influence on survival associated with ETCO2-monitoring, we included several covariates in the analysis; age, sex, calendar year, urbanization level (i.e., urban, suburban, and rural), health care institutes, and socioeconomic status (SES). Income-related insurance payment amounts were used as a proxy measure of individual SES at follow-up. People were divided into 3 groups: (1) low SES: payment lower than US$571 per month (New Taiwan Dollars [NT$] 20,000); (2) moderate SES: payment between US$571 and US$1141 per month (NT$ 20,000–40,000); and (3) high SES: payment of US$1142 or more per month (NT$40,001 or more) [12]. The health care institutes visited by patients were classified into 4 levels (medical centers, regional hospitals, local hospitals, and clinics) based on hospital accreditation. Two additional covariates that may be related to sustained ROSC following resuscitation, the CPR duration and attempted defibrillation, were identified based on charge records. Finally, the prevalence of selected comorbid conditions (i.e., diabetes, hypertension, coronary artery disease, hyperlipidemia, malignancies, heart failure, atrial fibrillation, intracranial hemorrhage, ischemic stroke, chronic renal insufficiency, and liver cirrhosis) and the Charlson Comorbidity Index (CCI) score were determined using discharge diagnoses either during outpatient clinic visits or hospitalizations before 1 January 2005. The CCI is a scoring system that assigns weights to important concomitant diseases; it has been validated for use in studies that employ ICD-9-CM data [14, 15].
Propensity score methods
In this study, the propensity score was the conditional probability for using ETCO2 monitoring in the presence of possible confounders. The prespecified covariates were added into a multivariable logistic regression model to predict the probability of ETCO2 use. The predicted probability from the model was used as the propensity score for each patient. We then matched each patient in the ETCO2 group to 20 patients in the untreated group with the closest propensity score using a standard greedy-matching algorithm [16] and compared the probability of survival benefits between these groups.
Statistical analysis
The SAS statistical package, version 9.4 (SAS Institute, Inc., Cary, NC, USA) was used for data analysis. All covariates were taken as categorical variables except age, calendar year, CPR duration, and propensity score, which were treated as continuous variables. Categorical variables were compared using Pearson’s chi-square test, and continuous variables were assessed using the t test to determine baseline heterogeneity in the 2 groups. Simple conditional logistic regression models were then used to calculate the ORs of sustained ROSC and survival to hospital discharge for patients with ETCO2 use in the matched group.
In order to further assess the robustness of our results, we sampled another cohort by matching each patient in the ETCO2 group to 4 patients in the untreated group using the same method (Fig. 1). We compared the crude ORs and risk differences of survival benefits among 2 matched cohorts and the original group to evaluate if the results are similar. We also evaluated the extent of the effect of a potentially unmeasured confounder in accounting for the results [17]. A two-tailed P value of 0.05 was considered significant.
Results
The distribution of demographic characteristics and selected morbidities in both groups is shown in Table 1. There were 6909 episodes of OHCA during the 8-year period. The population incidence of OHCA in Taiwan was 86.3 per 100,000 person-years. After exclusion, there were 83 patients in the ETCO2 group and 4958 in the untreated group. The overall baseline characteristics are similar between the 2 groups, except the patients monitored with ETCO2 were more likely to have liver cirrhosis. In addition, patients who visited medical centers also had a higher probability of receiving ETCO2 monitoring. The proportion of ETCO2 use gradually increased after 2010 but still was low. In 2012, only 5.8 % of OHCA patients received ETCO2 monitoring (Table 2). Detailed information about the frequency of ETCO2 use are summerized in the Additional file 1. After resuscitation, 658 patients (13 %) had records of sustained ROSC, including 25 patients in the ETCO2 group and 633 in the untreated group. Among them, 1 patient (4 %) in the ETCO2 group and 96 (15.2 %) in the untreated group had a record of survival to hospital discharge, respectively. The crude odds ratio (OR) of sustained ROSC for the ETCO2 group was 2.95 (95 % CI 1.83–4.74).
Table 1.
Baseline characteristics of the ETCO2 group and the untreated group
| Variables | ETCO2 group | Untreated group | P value | ||
|---|---|---|---|---|---|
| (n = 83) | (n = 4958) | ||||
| Male, no. (%) | 44 | 53.0 | 3138 | 63.3 | 0.054 |
| Mean age in years (SD) | 71.3 | 15.2 | 67.9 | 17.6 | 0.088 |
| Attempted defibrillation, no. (%) | 14 | 16.9 | 878 | 17.7 | 0.842 |
| Mean CPR time (10 min) (SD) | 2.4 | 1.4 | 2.4 | 1.6 | 0.927 |
| Socioeconomic status, no. (%) | 0.236 | ||||
| Low | 56 | 67.5 | 3586 | 72.3 | |
| Moderate | 26 | 31.3 | 1212 | 24.5 | |
| High | 1 | 1.2 | 160 | 3.2 | |
| Urbanization level, no. (%) | 0.118 | ||||
| Urban | 26 | 31.3 | 1174 | 23.7 | |
| Suburban | 29 | 35.0 | 2259 | 45.6 | |
| Rural | 28 | 33.7 | 1525 | 30.7 | |
| Diabetes, no. (%) | 25 | 30.1 | 1255 | 25.3 | 0.318 |
| Hypertension, no. (%) | 43 | 51.8 | 2434 | 49.1 | 0.624 |
| Coronary artery disease, no. (%) | 16 | 19.3 | 1075 | 21.7 | 0.598 |
| Hyperlipidemia, no. (%) | 21 | 25.3 | 893 | 18.0 | 0.087 |
| Malignancies, no. (%) | 6 | 7.2 | 231 | 4.7 | 0.273 |
| Heart failure, no. (%) | 1 | 1.2 | 255 | 5.1 | 0.105 |
| Atrial fibrillation, no. (%) | 3 | 3.6 | 107 | 2.2 | 0.368 |
| Charlson comorbidity index score, no. (%) | 0.821 | ||||
| 0 | 25 | 30.1 | 1631 | 32.9 | |
| 1 | 24 | 28.9 | 1307 | 26.4 | |
| ≥ 2 | 34 | 41.0 | 2020 | 40.7 | |
| Intracerebral hemorrhage, no. (%) | 1 | 1.2 | 108 | 2.2 | 0.545 |
| Ischemic stoke, no. (%) | 16 | 19.3 | 887 | 17.9 | 0.744 |
| Chronic renal insufficiency, no. (%) | 2 | 2.4 | 233 | 4.7 | 0.326 |
| Liver cirrhosis, no. (%) | 16 | 19.3 | 550 | 11.1 | 0.019 |
| Health care institutes, no. (%) | <0.001 | ||||
| Medical centers | 36 | 43.4 | 1108 | 22.3 | |
| Regional hospitals | 41 | 49.4 | 2497 | 50.4 | |
| Local hospitals | 6 | 7.2 | 1333 | 26.9 | |
| Clinics | 0 | 0 | 20 | 0.4 | |
| Mean propensity score (SD) | 0.046 | 0.041 | 0.016 | 0.021 | <0.001 |
Table 2.
Frequency of ETCO2 use
| Frequency of ETCO2 use | ||||
|---|---|---|---|---|
| Year | ETCO2 use | Untreated group | ||
| NO. | % | NO. | % | |
| 2005 | 7 | 1.32 | 522 | 98.68 |
| 2006 | 2 | 0.35 | 571 | 99.65 |
| 2007 | 5 | 0.86 | 574 | 99.14 |
| 2008 | 7 | 1.04 | 666 | 98.96 |
| 2009 | 0 | 0 | 643 | 100 |
| 2010 | 7 | 1.07 | 646 | 98.93 |
| 2011 | 14 | 2.03 | 675 | 97.97 |
| 2012 | 41 | 5.84 | 661 | 94.16 |
Next, 53 patients in the ETCO2 group and 1060 in the untreated group were selected after propensity score matching algorithm. In the subcohort, 165 patients survived, including 15 in the ETCO2 group and 150 in the untreated group. Among them, 1 patient (6.7 %) in the ETCO2 group and 22 (14.7 %) in the untreated group had a record of survival to hospital discharge, respectively. The basic characteristics of these 2 subgroups are summarized in Table 3. After matching, all baseline characteristics were similar between the 2 groups. A simple conditional logistic regression model was used to estimate the OR for sustained ROSC and remained significantly higher in patients with ETCO2 use (2.38, 95 % CI 1.28–4.42, P = 0.006). A simple conditional logistic regression model was again used to estimate the OR of survival to hospital discharge but failed to find treatment benefit regarding ETCO2 use (OR 0.91, 95 % CI 0.12–6.90 P = 0.924).
Table 3.
Baseline characteristics in the propensity-matched cohort
| Variables | ETCO2 group | Untreated group | P value | ||
|---|---|---|---|---|---|
| (n = 53) | (n = 1060) | ||||
| Male, no. (%) | 27 | 50.9 | 644 | 60.8 | 0.154 |
| Mean age in years (SD) | 68.9 | 15.9 | 69.6 | 16.7 | 0.776 |
| Attempted defibrillation, no. (%) | 11 | 20.8 | 183 | 17.3 | 0.513 |
| Mean CPR time (10 min) (SD) | 2.7 | 1.4 | 2.5 | 1.6 | 0.394 |
| Socioeconomic status, no. (%) | 0.864 | ||||
| Low | 38 | 71.7 | 727 | 68.6 | |
| Moderate | 14 | 26.4 | 316 | 29.8 | |
| High | 1 | 1.9 | 17 | 1.6 | |
| Urbanization level, no. (%) | 0.929 | ||||
| Urban | 13 | 24.5 | 276 | 26.0 | |
| Suburban | 23 | 43.4 | 469 | 44.3 | |
| Rural | 17 | 32.1 | 315 | 29.7 | |
| Diabetes, no. (%) | 11 | 20.8 | 272 | 25.7 | 0.424 |
| Hypertension, no. (%) | 26 | 49.1 | 521 | 49.2 | 0.989 |
| Coronary artery disease, no. (%) | 10 | 18.9 | 200 | 18.9 | 1.000 |
| Hyperlipidemia, no. (%) | 10 | 18.9 | 211 | 19.9 | 0.853 |
| Malignancies, no. (%) | 3 | 5.7 | 44 | 4.2 | 0.594 |
| Heart failure, no. (%) | 1 | 1.9 | 19 | 1.8 | 0.959 |
| Atrial fibrillation, no. (%) | 1 | 1.9 | 16 | 1.5 | 0.827 |
| Charlson Comorbidity Index score, no. (%) | 0.935 | ||||
| 0 | 19 | 35.9 | 355 | 33.5 | |
| 1 | 15 | 28.3 | 305 | 28.8 | |
| ≥ 2 | 19 | 35.9 | 400 | 37.7 | |
| Intracerebral hemorrhage, no. (%) | 1 | 1.9 | 26 | 2.5 | 0.794 |
| Ischemic stoke, no. (%) | 8 | 15.1 | 198 | 18.7 | 0.512 |
| Chronic renal insufficiency, no. (%) | 2 | 3.8 | 36 | 3.4 | 0.883 |
| Liver cirrhosis, no. (%) | 4 | 7.6 | 128 | 12.1 | 0.320 |
| Health care institutes, no. (%) | 0.959 | ||||
| Medical centers | 15 | 28.3 | 288 | 27.2 | |
| Regional hospitals | 32 | 60.4 | 639 | 60.3 | |
| Local hospitals | 6 | 11.3 | 133 | 12.6 | |
| Clinics | 0.0209 | 0.0125 | 0.0207 | 0.0125 | 0.917 |
Crude ORs and risk differences among the original group and two matched cohorts were found to be similar. The results are summarized in Table 4. Sensitivity analyses showed that an unmeasured confounder present in 10 % of the study population would be required to elevate the possibility of sustained ROSC by a factor of 3.2. Among patients with ETCO2 use, the confounder also would have to be approximately 3.2 times more prevalent than that among the untreated group in order to explain a lower 95 % confidence limit HR of 1.28 (Fig. 2).
Table 4.
Comparison of ORs and risk differences among the original group and matched cohorts
| ETCO2 group (n) | Untreated group (n) | ORs (95 % CI) | Risk differences (95 % CI) | ||
|---|---|---|---|---|---|
| Original group | ROSC(+) | 25 | 633 | 2.95 (1.83–4.74) | 0.17 (0.07–0.27) |
| ROSC(−) | 58 | 4325 | |||
| 1:4 matched cohort | ROSC(+) | 25 | 56 | 2.12 (1.23–3.68) | 0.13 (0.02–0.23) |
| ROSC(−) | 58 | 276 | |||
| 1:20 matched cohort | ROSC(+) | 15 | 150 | 2.39 (1.29–4.46) | 0.14 (0.02–0.26) |
| ROSC(−) | 38 | 910 |
Fig. 2.
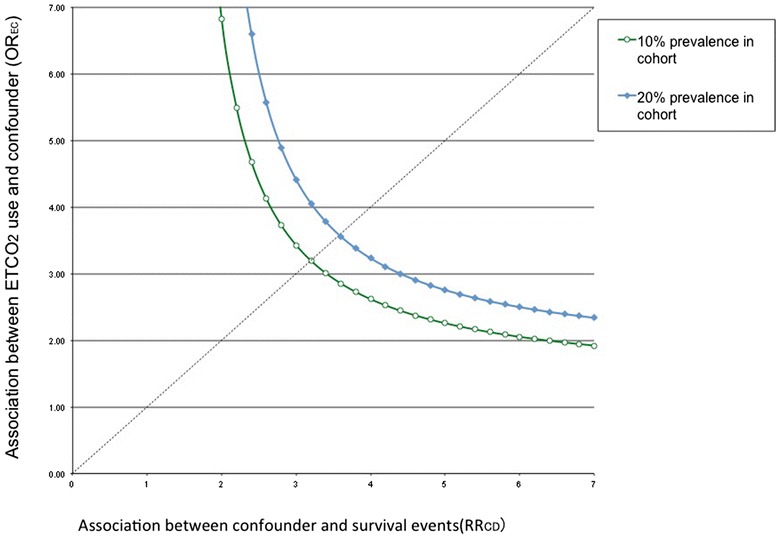
Sensitivity analyses for an unmeasured confounding factor
Discussion
The ACLS guideline for using ETCO2 monitoring during CPR provides the basis on which providers can have real-time feedback about the quality of chest compressions, thus offering patients a better chance of survival [18, 19]. To our knowledge, ours is the first study regarding possible survival benefits with ETCO2 monitoring in real clinical situations. In this study, we evaluated the sustained ROSC of patients in Taiwan who received ETCO2 monitoring following OHCA. The database corresponded well to the characteristics of the whole population; therefore, loss of follow-up or selection bias were not concerns. Although the overall survival rates of OHCA patients in Asia were found to be low [20], patients with ETCO2 monitoring during resuscitation still had a higher possibility of sustained ROSC (OR 2.38, 95 % CI 1.28–4.42). Although there were relatively few patients in the treatment group, based on our sample size of matched cohort and ORs the statistical power still achieved 1.0.
ETCO2 monitoring by itself cannot directly improve the quality of CPR administered. However, based on the real-time feedback about the patient’s ETCO2 level, the code team can adjust their management to achieve better chest compression quality, which may in turn result in a better outcome. Moreover, ETCO2 monitoring may also serve as a proxy for better team performance because teams or institutes that use ETCO2 monitoring may have better insights about the importance of CPR performance and thus may have better outcomes. Increased CPR quality may increase the probability of the return of spontaneous circulation. However, in the absence of data linking ETCO2 measurements with the quality markers of chest compressions in our study, no causality inference can be drawn currently.
This study is also the first one based on national data about the use of capnography during OHCA. Despite of the strong recommendation for its use, ETCO2 monitoring in OHCA patients is still low in Taiwan. Even in 2012, the overall percentage of ETCO2 monitoring was only 5.84 %. According to the recommendations of the ACLS guidelines and the possible survival benefits found in this study, further emphasis should be placed on the routine use of ETCO2 monitoring during OHCA.
Limitations
First, our findings were generated from administrative data. The definitions of OHCA were based on ICD-9-CM codes, which are useful for insurance reimbursement but may not be exact substitutes for precise operative definitions. There is also lack of data whether ETCO2 monitoring was performed during or after chest compressions. We validated the selection processes by analyzing 150 medical records of patients with OHCA randomly selected from the electronic database from 2010 to 2012 at Dalin Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation. All 118 patients who were charged with chest compression had documented CPR records. Among 69 patients with ETCO2 charge records, the confirmation of use was found by documented CO2 levels during resuscitations. All 42 patients with records of hospitalization were alive before admissions. These selection processes yielded positive predictive values of 100 %.
Second, the percentage of ETCO2 monitoring in our study cohort was only 1.6 %, which may be an underestimate of the true number of patients who actually were monitored. In clinical practice in Taiwan, procedures are charged either by healthcare or administrative staff. In a busy situation such as resuscitation, staff may forget to charge for the ETCO2 monitoring in some patients. Although the extent of crossover to the treatment category cannot be assessed in this study, according to the intention-to-treat analytical principle, the result in this study would show only a bias toward a null result, and the estimation of OR would be more conservative than the actual number reported.
Third, the overall percentage of sustained ROSC (13 %) is low compared with results reported in other publications [20, 21]. Results similar to ours were found in a study published by Huang et al. [22], and fewer shockable rhythms in that study may account for the similarity. Because of the limited number of cases, we failed to find benefits of ETCO2 monitoring on patients’ survival to hospital discharge. Further study should be conducted to evaluate if chest compression monitoring by ETCO2 can improve survival to hospital discharge and, perhaps, if it can be associated with better cerebral performance.
Fourth, for an observational study, confounding by indication may be a concern even after one applies propensity score matching to establish the comparability between groups that use ETCO2 monitoring or do not. For example, in patients with a lower likelihood of survival, physicians may be less likely to use ETCO2 monitoring during resuscitation. However, because the outcome of survival is not perfectly predictable beforehand, such an argument is not plausible. Moreover, because the baseline characteristics were similar between the ETCO2 group and the untreated group even before matching, we believe that resuscitation teams would use ETCO2 monitoring guidelines instead of clinical judgments.
Fifth, with the use of propensity score analyses to adjust for possible confounding, we also lost the ability to evaluate other possible covariates of survival. Finally, although we extensively adjusted for many possible covariates, unmeasured confounding and the possibility of overmatching may still exist. In our database, we were unable to obtain prehospital information such as bystander CPR, prehospital intubation, and duration of collapse.
Conclusion
Patients monitored with ETCO2 may have a higher possibility of sustained ROSC. However, the overall use of ETCO2 is still low despite strong recommendations in guidelines.
Abbreviations
- ACLS
Advanced cardiac life support
- CCI
Charlson comorbidity index
- CPR
Cardiopulmonary resuscitation
- ETCO2
End-tidal carbon dioxide monitoring
- ICD-9-CM
International Classification of Diseases (Ninth Revision) Clinical Modification
- NHI
National Health Insurance
- OHCA
Out-of-hospital cardiac arrest
- OR
Odds ratio
- SES
Socioeconomic status
Additional file
Frequency of ETCO2 use. (DOCX 28 kb)
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
JJC, YKL, and YCS provided manuscript formation. YKL provided study supervision. SWH provided study supervision. MYH and CYH provided data analysis. YCS provided interpretation. All authors read and approved the final manuscript.
References
- 1.Johnson NJ, Salhi RA, Abella BS, Neumar RW, Gaieski DF, Carr BG. Emergency department factors associated with survival after sudden cardiac arrest. Resuscitation. 2013;84:292–7. doi: 10.1016/j.resuscitation.2012.10.013. [DOI] [PubMed] [Google Scholar]
- 2.Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, et al. Heart disease and stroke statistics--2011 update: a report from the American Heart Association. Circulation. 2011;123:e18–209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Field JM, Hazinski MF, Sayre MR, Chameides L, Schexnayder SM, Hemphill R, et al. Part 1: executive summary: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S640–56. doi: 10.1161/CIRCULATIONAHA.110.970889. [DOI] [PubMed] [Google Scholar]
- 4.Bobrow BJ, Spaite DW, Berg RA, Stolz U, Sanders AB, Kern KB, et al. Chest compression-only CPR by lay rescuers and survival from out-of-hospital cardiac arrest. JAMA. 2010;304:1447–54. doi: 10.1001/jama.2010.1392. [DOI] [PubMed] [Google Scholar]
- 5.Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa) Circulation. 2004;110:3385–97. doi: 10.1161/01.CIR.0000147236.85306.15. [DOI] [PubMed] [Google Scholar]
- 6.Kodali BS, Urman RD. Capnography during cardiopulmonary resuscitation: current evidence and future directions. J Emerg Trauma Shock. 2014;7:332–40. doi: 10.4103/0974-2700.142778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shibutani K, Muraoka M, Shirasaki S, Kubal K, Sanchala VT, Gupte P. Do changes in end-tidal PCO2 quantitatively reflect changes in cardiac output? Anesth Analg. 1994;79:829–33. doi: 10.1213/00000539-199411000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Qvigstad E, Kramer-Johansen J, Tomte O, Skalhegg T, Sorensen O, Sunde K, et al. Clinical pilot study of different hand positions during manual chest compressions monitored with capnography. Resuscitation. 2013;84:1203–7. doi: 10.1016/j.resuscitation.2013.03.010. [DOI] [PubMed] [Google Scholar]
- 9.Einav S, Bromiker R, Weiniger CF, Matot I. Mathematical modeling for prediction of survival from resuscitation based on computerized continuous capnography: proof of concept. Acad Emerg Med. 2011;18:468–75. doi: 10.1111/j.1553-2712.2011.01067.x. [DOI] [PubMed] [Google Scholar]
- 10.National Health Insurance Database. http://w3.nhri.org.tw/nhird/en/index.htm. Accessed 11 June 2015.
- 11.Lee YK, Lee CC, Chen CC, Wong CH, Su YC. High risk of ‘failure’ among emergency physicians compared with other specialists: a nationwide cohort study. Emerg Med J. 2013;30(8):620–2. doi: 10.1136/emermed-2012-201440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hou SW, Lee YK, Hsu CY, Lee CC, Su YC. Increased risk of acute pancreatitis in patients with chronic hemodialysis: a 4-year follow-up study. PLoS One. 2013;8:e71801. doi: 10.1371/journal.pone.0071801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cheng PL, Lin HY, Lee YK, Hsu CY, Lee CC, Su YC. Higher mortality rates among the elderly with mild traumatic brain injury: a nationwide cohort study. Scand J Trauma Resusc Emerg Med. 2014;22:7. doi: 10.1186/1757-7241-22-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee Y-K, Lee C-W, Huang M-Y, Hsu C-Y, Su Y-C. Increased risk of ischemic stroke in patients with mild traumatic brain injury: a nationwide cohort study. Scand J Trauma Resusc Emerg Med. 2014;22:66. doi: 10.1186/s13049-014-0066-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ng KJ, Lee YK, Huang MY, Hsu CY, Su YC. Risks of venous thromboembolism in patients with liver cirrhosis: a nationwide cohort study in Taiwan. J Thromb Haemost. 2014;13(2):206–13. doi: 10.1111/jth.12805. [DOI] [PubMed] [Google Scholar]
- 16.Lee YK, Chen CC, Lin HY, Hsu CY, Su YC. Propofol for sedation can shorten the duration of ED stay in joints reduction. Am J Emerg Med. 2012;30(8):1352–6. doi: 10.1016/j.ajem.2011.09.024. [DOI] [PubMed] [Google Scholar]
- 17.Schneeweiss S. Sensitivity analysis and external adjustment for unmeasured confounders in epidemiologic database studies of therapeutics. Pharmacoepidemiol Drug Saf. 2006;15:291–303. doi: 10.1002/pds.1200. [DOI] [PubMed] [Google Scholar]
- 18.Edelson DP, Litzinger B, Arora V, Walsh D, Kim S, Lauderdale DS, et al. Improving in-hospital cardiac arrest process and outcomes with performance debriefing. Arch Intern Med. 2008;168:1063–9. doi: 10.1001/archinte.168.10.1063. [DOI] [PubMed] [Google Scholar]
- 19.Abella BS, Edelson DP, Kim S, Retzer E, Myklebust H, Barry AM, et al. CPR quality improvement during in-hospital cardiac arrest using a real-time audiovisual feedback system. Resuscitation. 2007;73:54–61. doi: 10.1016/j.resuscitation.2006.10.027. [DOI] [PubMed] [Google Scholar]
- 20.Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010;81:1479–87. doi: 10.1016/j.resuscitation.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 21.Boyce LW, Vliet Vlieland TP, Bosch J, Wolterbeek R, Volker G, van Exel HJ, et al. High survival rate of 43 % in out-of-hospital cardiac arrest patients in an optimised chain of survival. Neth Heart J. 2015;23:20–5. doi: 10.1007/s12471-014-0617-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Huang C-H, Huei-Ming Ma M, Chen W-J. Out-of-hospital cardiac arrest in Taipei, Taiwan. Acta Cardiol Sinica. 2006;22:53–7. [Google Scholar]


