Abstract
Carpal tunnel syndrome (CTS) is the most common entrapment neuropathy and a frequent cause of sick leaves because of work-related hand overload. That is why an early diagnosis and adequate treatment (conservative or surgical) are essential for optimal patient management.
Aim
The aim of the study is to assess the usefulness of high-frequency ultrasound in CTS for the assessment of patient eligibility for surgical treatment.
Material and methods
The study involved 62 patients (50 women and 12 men, aged 28–70, mean age 55.2) with scheduled surgeries of CTS on the basis of clinical symptoms, physical examination performed by a neurosurgeon and a positive result of EMG testing. The ultrasound examinations of the wrist were performed in all these patients. On the basis of the collected data, the author has performed multiple analyses to confirm the usefulness of ultrasound imaging in assessing patient eligibility for surgical treatment of CTS.
Results
US examinations showed evidence of median nerve compression at the level of the carpal tunnel in all of the examined patients. This was further confirmed during surgical procedures. The mean value of the cross-sectional area at the proximal part of the pisiform bone was 17.45 mm2 (min. 12 mm2, max. 31 mm2). Nerve hypoechogenicity proximal to the nerve compression site was visible in all 62 patients (100%). Increased nerve vascularity on the transverse section was present in 50 patients (80.65%).
Conclusions
Ultrasonography with the use of high-frequency transducers is a valuable diagnostic tool both for assessing patient eligibility for surgical treatment of CTS, and in postoperative assessment of the treatment efficacy.
Keywords: median nerve, carpal tunnel syndrome, entrapment neuropathy, ultrasound
Abstract
Zespół kanału nadgarstka (ZKN) jest najczęstszą neuropatią uciskową i częstą przyczyną zwolnień lekarskich z powodu przeciążenia ręki związanego z pracą. Optymalne postępowanie w tym zespole zależy od wczesnego rozpoznania i podjęcia odpowiedniego leczenia (zachowawczego lub operacyjnego).
Cel pracy
Celem pracy jest określenie przydatności badania USG z zastosowaniem głowicy wysokiej częstotliwości w kwalifikowaniu do operacyjnego leczenia ZKN.
Materiał i metoda
Materiał pracy stanowi grupa 62 pacjentów (50 kobiet i 12 mężczyzn w wieku od 28 do 70 lat; średnia wieku 55,2 roku) zakwalifikowanych do operacyjnego leczenia ZKN na podstawie objawów klinicznych i badania fizykalnego przeprowadzonego przez neurochirurga oraz pozytywnego wyniku badania EMG. Wykonano badanie USG u wszystkich tych chorych. Na podstawie uzyskanych danych przeprowadzono liczne analizy, mające na celu potwierdzenie przydatności badania USG w kwalifikowaniu do leczenia operacyjnego ZKN.
Wyniki
U wszystkich osób z grupy badanej uwidoczniono w badaniu USG ucisk nerwu pośrodkowego na poziomie kanału nadgarstka, który potwierdzono podczas zabiegu operacyjnego. Średnia wartość pola przekroju nerwu pośrodkowego na poziomie bliższej części grochowatej wynosiła 17,45 mm2 (min. 12 mm2, max. 31 mm2). Obniżenie echogeniczności nerwu pośrodkowego powyżej miejsca ucisku stwierdzono u wszystkich 62 pacjentów (100%). Cechy wzmożonego unaczynienia nerwu na przekroju poprzecznym występowały u 50 osób (80,65%).
Wnioski
Badanie USG z zastosowaniem głowicy wysokiej częstotliwości jest wartościową metodą diagnostyki obrazowej w kwalifikowaniu do operacyjnego leczenia zespołu kanału nadgarstka.
Introduction
Carpal tunnel syndrome (CTS) is a group of clinical symptoms that result from median nerve injury due its compression in the carpal tunnel(1).
According to various authors, ultrasound imaging (US) is at least as effective in CTS diagnosis as electrophysiological testing(2). What is more, it is non-invasive and painless, which renders it well-tolerated by patients. The literature discusses the usefulness of a range of CTS assessment parameters. They include: nerve cross-sectional area at the level of the proximal pisiform bone and proximal part of the pronator quadratus muscle, the presence of a “notch” sign and “inverted notch” sign, compression site, echogenicity and echotexture of the median nerve proximally to the compression site, evidence of increased vascularity of the median nerve above the compression site in a power Doppler examination and the movability of the median nerve in the carpal tunnel. The results concerning individual CTS parameters, presented by different authors, vary. That is the reason for conducting this study, in order to assess the usefulness of these parameters.
The publication was prepared on the basis of a doctoral dissertation entitled: High-frequency ultrasound in carpal tunnel syndrome: assessment of patient eligibility for surgical treatment by Katarzyna Kapuścińska, MD, PhD (defended on October, 8 2014 in Krakow, Poland).
Aim
The aim of the study was to assess the usefulness of high-frequency ultrasound in CTS for the assessment of patient eligibility for surgical treatment.
Material and methods
The study involved 62 patients (50 women and 12 men aged between 28 and 70; mean age 55.2) with a scheduled surgical procedures for CTS treatment. The patients were referred to the US Imaging Laboratory of the University Hospital in Kraków from the Neurosurgery Outpatient Clinic of the University Hospital in Krakow.
All patients were scanned by ultrasound with the use of a broadband linear transducer of high frequency (6–18 MHz, using the 18 MHz band). The author used a MyLab 70 system by Esaote. Blood flow was assessed with the power Doppler (PD). All US examinations were conducted with the same equipment in the US Imaging Laboratory of the Department of Medical Imaging at the University Hospital in Krakow.
Before the procedure, the following parameters were assessed: nerve cross-sectional area at the level of the proximal pisiform bone and proximal part of the pronator quadratus muscle (in mm2) and the difference between these values; the presence of a “notch” sign and “inverted notch” sign; the presence and localization of the compression site, echogenicity and echotexture of the median nerve proximally to the compression site; evidence of increased vascularity of the median nerve above the compression site in a power Doppler examination, and the movability of the median nerve in the carpal tunnel.
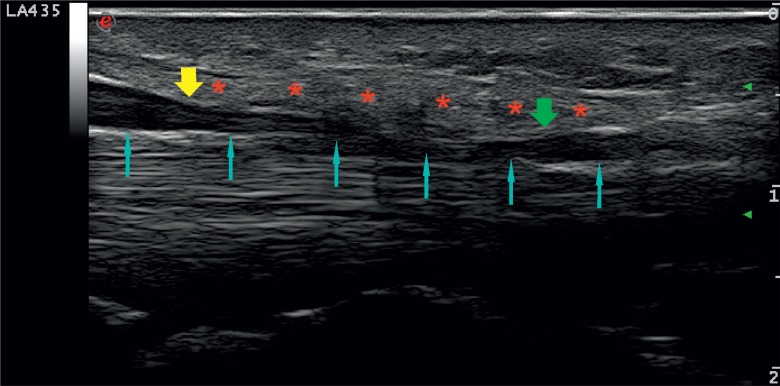
Nerve compression was evaluated in transverse and longitudinal sections. In the case of compression, the cross-sectional area of the nerve is lower at the compression level, the echogenicity is higher and the honeycomb appearance is not observed. Nerve narrowing can be seen in a longitudinal section (Fig. 1). The cross-sectional area is measured in the transverse section by circling the nerve under the outer epineurium with a cursor.
Fig. 1.
Longitudinal section. Median nerve compression at the carpal tunnel level: blue arrows – median nerve; yellow arrow – notch sign; green arrow – inverted notch sign; red arrow – flexor retinaculum
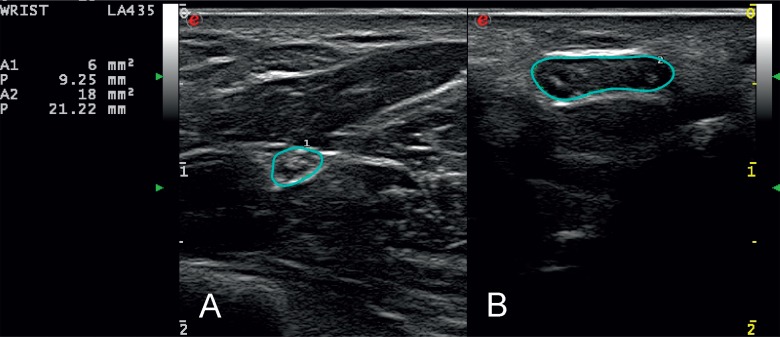
Thickening, hypoechogenicity and the loss of echotexture can be seen proximally and distally to the compression site (Fig. 2). The advancement of the US signs depends on the degree and duration of compression.
Fig. 2.
Abnormal US presentation of the median nerve in the transverse section in CTS, proximal to the compression site. The nerve cross section is circled with a blue line. A. cross-sectional area at the level of the pronator quadratus muscle (6 mm2); B. cross-sectional area at the level of the pisiform bone (18 mm2)
The US criteria for median nerve compression at the carpal tunnel include(3):
increased cross-sectional area proximally to the compression site, usually at the level of the proximal pisiform bone; in normal conditions, the cross-sectional area of the median nerve is not greater than 9 mm2 (9–12 mm2);
a difference in median nerve cross-sectional areas between the level of the proximal pisiform bone and proximal part of the pronator quadratus muscle is at least 2 mm2;
nerve flattening – in the transverse section, the nerve is at least 3 times wider than it is thick; the thickness is not greater than 2 mm;
lower echogenicity and blurred echotexture proximally and distally;
increased vascularization in a PD examination;
- hourglass-like narrowing of the nerve in the longitudinal section, corresponding to the compression site. It can present as:
- a notch – an image of a sudden narrowing at the level of the proximal border of the compression site;
- an inverted notch – an image results from a sudden increase in nerve thickness at the level of the distal border of the compression site;
a decrease or absence of nerve movability in the carpal tunnel;
bulged flexor retinaculum to the level of at least 4 mm above the line that connects the ventral edge of the hook of the hamate bone with the tubercle of the trapezium.
Based on such data, the relationships between the following parameters were analyzed:
the median nerve compression site and the nerve cross-sectional area at the level of the pisiform bone;
increased vascularity of the median nerve above the compression site, assessed with the use of the power Doppler, and the cross-sectional area proximal to the compression site;
the movability of the median nerve at the level of the carpal tunnel in relation to the flexor tendons and retinaculum, and a difference in median nerve cross-sectional areas between the level of the proximal pisiform bone and proximal part of the pronator quadratus muscle.
All 62 patients underwent a procedure in the Department of Neurosurgery of the University Hospital in Krakow, Poland.
The statistical analysis showed that the data had a normal distribution, and therefore the following tests were applied: Student's t test for independent samples, single-factor analysis of variance (ANOVA), a post-hoc multiple comparison Tukey test, the χ2 test of independence and a ROC curve analysis.
Results with the significance level lower than or equal to 0.05 were deemed statistically significant (p ≤ 0.05). The statistical calculations were conducted with the use of a Statistica 10 PL and StatsDirect 2.7.9.
Results
The study population consisted of 50 women and 12 men, aged between 28 and 70, who had been diagnosed with CTS based on clinical signs and EMG findings.
The mean value of the cross-sectional area at the proximal part of the pronator quadratus muscle was 8.15 mm2 (min. 6 mm2, max. 12 mm2). The mean value of the cross-sectional area at the proximal part of the pisiform bone was 17.45 mm2 (min. 12 mm2, max. max. 31 mm2). The average difference in median nerve cross-sectional areas between the level of the pisiform bone and the pronator quadratus muscle was 9.31 mm2 (min. 3 mm2 – max. 24 mm2).
The median nerve compression at the carpal tunnel was diagnosed in all patients (100%).
The median nerve compression at the level of the hook of the hamate bone was found in 22 patients (35.5%); at the level of the hook of the hamate bone with deformation at the level of the pisiform bone – in 16 patients (25.8%); at the level of the hook of the hamate bone and pisiform bone – in 23 patients (37.1%) as well as at the level of the hook of the hamate bone, pisiform bone and the distal edge of the antebrachial fascia – in 1 person (1.6%).
Nerve hypoechogenicity above the compression site was visible in all 62 patients (100%), and blurred echotexture was detected in 48 patients (77.42%).
Increased nerve vascularity on the transverse section was present in 50 cases (80.65%).
The movability of the nerve was restricted in 46 patients (74.2%) and it was completely blocked in 16 cases (25.8%).
There were statistically significant differences (p < 0.001) in cross-sectional areas depending on the compression site.
The post hoc multiple comparison tests revealed that there was a statistically significant difference between the median nerve cross-sectional area measured at the compression site on level of the hook of the hamate bone (mean 13.7 mm2) and cross-sectional area measured at the compression site on the level of the pisiform bone (mean 21.1 mm2).
Increased vascularity was significantly (p = 0.005) correlated with the difference between cross-sectional areas and was present when the differences were lower.
The ROC curve analysis showed that the difference in cross-sectional areas was discriminative for increased vascularity of the nerve, and that the optimal cut-off point for increased vascularity was 10 mm2 (with the sensitivity of 80% and specificity of 66.7%).
The cut-off point of a 10 mm2 difference in cross-sectional areas at the level of the pisiform bone distinguished examinations with increased vascularity in the nerve in a statistically significant way (p = 0.001).
The lack of median nerve movability in the carpal tunnel was observed when the differences between cross-sectional areas were greater in a statistically significant way (p < 0.001). The mean difference in the group of patients with restricted nerve movability was 7.2 mm2 (min. 3 mm2 – max. 13 mm2). The mean difference between the cross-sectional areas in the group of patients with absent nerve movability was 15.3 mm2 (min. 6 mm2 – max. 24 mm2).
Discussion
In the meta-analysis, entitled No correlation between sonographic and electrophysiological parameters in carpal tunnel syndrome, Żyluk et al. have not found any unambiguous correlation between EMG and US examinations, i.e. they have not observed any relationship between the intensity of changes in an electrodiagnostic test and the occurrence of given features of compression in a US examination(4). Also, Claes believes that ultrasound cannot replace EMG(5). In her study, a US examination was normal in 42.9% of patients with CTS. The disadvantage of this technique is the impossibility to assess nerve movability in the carpal tunnel in a dynamic examination.
Koyuncuoglu, in turn, claims that US is a valuable method in the CTS diagnosis in patients with clinical signs of CTS and negative electrodiagnostic tests(6).
The role of US is also emphasized by Toros in the commentary to the publication mentioned above (Commentary on Zyluk et al. No correlation between sonographic and electrophysiological parameters in carpal tunnel syndrome)(7). He believes that the failure to visualize median nerve compression in patients with clinical signs of CTS indicates an initial stage of the syndrome, in which conservative treatment may be sufficient. The lack of US evidence of median nerve compression should not be treated as a failure of this method but as a confirmation of an early advancement stage, which is probably reversible.
In the study material presented above, US examinations conducted before the procedures of carpal tunnel release confirmed its compression in 100% of cases. In the author's personal opinion, an ultrasound examination should be the method of the first choice in patients manifesting clinical signs of CTS; electrodiagnostic testing could be used only in doubtful cases. A similar opinion was expressed by Lange in the paper entitled Carpal tunnel syndrome diagnosed using ultrasound as a first-line exam by the surgeon(8). The author claims that a US examination can be conducted during the first visit.
Moreover, Smidt and Visser(9) as well as Pastare et al.(10) suggest that a US examination should be a screening test in the diagnosis of CTS.
The parameter that is the most frequently assessed in US examinations in CTS patients is the cross-sectional area on the pisiform bone level. Most studies suggest that the value between 9 and 12 mm2 is a cut-off point for a CTS diagnosis.
Ziswiler et al. claim that a cross-sectional area of the median nerve that is greater than 10 mm2 helps diagnose CTS with 82% sensitivity and 87% specificity of an electrodiagnostic test. The cross-sectional area lower than 8 mm2 allows CTS to be ruled out, and the area greater than 12 mm2 indicates that CTS is highly likely(11).
In order to avoid the dependence of the nerve diameter on patient's height, weight and constitution type, the cross-sectional area at the level of the proximal pisiform bone should be compared with that at the level of the proximal pronator muscle. This parameter was described by Klauser(12); a significant difference is at least 2 mm2. In this study, all patients met this criterion.
The assessment of the echotexture and echogenicity is another parameter. With an increase in the cross-sectional area due to nerve edema, its echogenicity decreases and the echotexture becomes blurred. According to Mallouhi, decreased echogenicity above the compression site is characterized by 80% sensitivity and 65% specificity(13).
Another commonly used criterion is the presence of a “notch” or “inverted notch” sign in the longitudinal section of the nerve and its flattening in the transverse section. The notch and inverted notch signs result from edema and increased cross-sectional area proximally and distally to the compression site (i.e. in the place where the nerve is narrowed and flattened). According to Mallouhi, nerve flattening is considered a significant sign if the cross section of the nerve is 3 times greater than its thickness(13). The same authors(13) claim that nerve flattening at the compression site is characterized by the sensitivity of 60% and specificity of 76%. Naranjo(14) reports the values of 65% and 47%, respectively. In the author's own study, the notch sign was detected in all patients. The inverted notch sign was observed in 47 cases (75.81%).
Another sign of an entrapment neuropathy is increased vascularization of the median nerve in a PD examination. Mallouhi reports that it is characterized by 95% sensitivity and 71% specificity in diagnosing CTS(13). This is confirmed by Ghasemi-Esfe(15) (sensitivity 83%, specificity 89%) and Joy(16) (sensitivity 83%).
The analysis of the examinations conducted in patients enrolled in this study has shown that hypervascularization is present when the median nerve is less swollen and when the difference in the cross-sectional areas between the level of the pronator quadratus muscle and the level of the pisiform bone is lower. It can be therefore concluded that hypervascularization is more common in initial stages of this entrapment neuropathy and disappears in its chronic form.
Moreover, the possibility of conducting a dynamic US examination and assessing median nerve movability in the carpal tunnel are also significant. In normal conditions, the median nerve moves freely within the carpal tunnel. Due to increased pressure in the tunnel, the movability is gradually more and more restricted, and finally it is blocked.
The author assessed the changes of the median nerve position in the carpal tunnel during active and passive movements of the wrist and fingers. All patients manifested impaired median nerve movability.
Conclusions
Ultrasound imaging with the use of high-frequency transducers is a valuable diagnostic tool for assessing patient eligibility for surgical treatment of carpal tunnel syndrome. It enables the assessment of the morphology and vascularization of the median nerve, helps identify entrapment and localize the compression site, and allows median nerve movability against adjacent structures to be evaluated. Moreover, this modality enables the median nerve entrapment to be confirmed in patients with clinical symptoms of CTS.
Conflict of interest
Authors do not report any financial or personal links with other persons and organizations, which might affect negatively the content of this publication and/or claim authorship rights to this publication.
References
- 1.Żyluk A, Puchalski P. Historia naturalna zespołu kanału nadgarstka – przegląd piśmiennictwa. Pol Orthop Traumatol. 2010;75:261–266. [PubMed] [Google Scholar]
- 2.Kwon BC, Jung KI, Baek GH. Comparison of sonography and electrodiagnostic testing in the diagnosis of carpal tunnel syndrome. J Hand Surg Am. 2008;33:65–71. doi: 10.1016/j.jhsa.2007.10.014. [DOI] [PubMed] [Google Scholar]
- 3.Klauser AS, Faschingbauer R, Bauer T, et al. Entrapment neuropathies II: carpal tunnel syndrome. Semin Musculoskelet Radiol. 2010;14:487–500. doi: 10.1055/s-0030-1268069. [DOI] [PubMed] [Google Scholar]
- 4.Żyluk A, Walaszek I, Szlosser Z. No correlation between sonographic and electrophysiological parameters in carpal tunnel syndrome. J Hand Surg Eur Vol. 2014;39:161–166. doi: 10.1177/1753193413489046. [DOI] [PubMed] [Google Scholar]
- 5.Claes F, Kasius KM, Meulstee J, Verhagen WI. Comparing a new ultrasound approach with electrodiagnostic studies to confirm clinically defined carpal tunnel syndrome: a prospective, blinded study. Am J Phys Med Rehabil. 2013;92:1005–1011. doi: 10.1097/PHM.0b013e31829b4bd8. [DOI] [PubMed] [Google Scholar]
- 6.Koyuncuoglu HR, Kutluhan S, Yesildag A, Oyar O, Guler K, Ozden A. The value of ultrasonographic measurement in carpal tunnel syndrome in patients with negative electrodiagnostic tests. Eur J Radiol. 2005;56:365–369. doi: 10.1016/j.ejrad.2005.05.013. [DOI] [PubMed] [Google Scholar]
- 7.Toros T. Commentary on Zyluk et al. No correlation between sonographic and electrophysiological parameters in carpal tunnel syndrome; and Yalçın et al. Ultrasound diagnosis of ulnar neuropathy: comparison of symptomatic and asymptomatic nerve thickness. J Hand Surg Eur Vol. 2014;39:172–174. doi: 10.1177/1753193413513524. [DOI] [PubMed] [Google Scholar]
- 8.Lange J. Carpal tunnel syndrome diagnosed using ultrasound as a firstline exam by the surgeon. J Hand Surg Eur Vol. 2013;38:627–632. doi: 10.1177/1753193412469581. [DOI] [PubMed] [Google Scholar]
- 9.Smidt MH, Visser LH. Carpal tunnel syndrome: clinical and sonographic follow-up after surgery. Muscle Nerve. 2008;38:987–991. doi: 10.1002/mus.20982. [DOI] [PubMed] [Google Scholar]
- 10.Pastare D, Therimadasamy AK, Lee E, Wilder-Smith EP. Sonography versus nerve conduction studies in patients referred with a clinical diagnosis of carpal tunnel syndrome. J Clin Ultrasound. 2009;37:389–393. doi: 10.1002/jcu.20601. [DOI] [PubMed] [Google Scholar]
- 11.Ziswiler HR, Reichenbach S, Vögelin E, Bachmann LM, Villiger PM, Jüni P. Diagnostic value of sonography in patients with suspected carpal tunnel syndrome: a prospective study. Arthritis Rheum. 2005;52:304–311. doi: 10.1002/art.20723. [DOI] [PubMed] [Google Scholar]
- 12.Klauser AS, Halpern EJ, De Zordo T, et al. Carpal tunnel syndrome assessment with US: value of additional cross-sectional area measurements of the median nerve in patients versus healthy volunteers. Radiology. 2009;250:171–177. doi: 10.1148/radiol.2501080397. [DOI] [PubMed] [Google Scholar]
- 13.Mallouhi A, Pülzl P, Trieb T, Piza H, Bodner G. Predictors of carpal tunnel syndrome: accuracy of gray-scale and color Doppler sonography. AJR Am J Roentgenol. 2006;186:1240–1245. doi: 10.2214/AJR.04.1715. [DOI] [PubMed] [Google Scholar]
- 14.Naranjo A, Ojeda S, Rúa-Figueroa I, Garcia-Duque O, Fernández-Palacios J, Carmona L. Limited value of ultrasound assessment in patients with poor outcome after carpal tunnel release surgery. Scand J Rheumatol. 2010;39:409–412. doi: 10.3109/03009741003685632. [DOI] [PubMed] [Google Scholar]
- 15.Ghasemi-Esfe AR, Khalilzadeh O, Vaziri-Bozorg SM, Jajroudi M, Shakiba M, Mazloumi M, et al. Color and power Doppler US for diagnosing carpal tunnel syndrome and determining its severity: a quantitative image processing method. Radiology. 2011;261:499–506. doi: 10.1148/radiol.11110150. [DOI] [PubMed] [Google Scholar]
- 16.Joy V, Therimadasamy AK, Chan YC, Wilder-Smith EP. Combined Doppler and B-mode sonography in carpal tunnel syndrome. J Neurol Sci. 2011;308:16–20. doi: 10.1016/j.jns.2011.06.042. [DOI] [PubMed] [Google Scholar]