Abstract
Sit-to-stand exercise (STS) is a common activity of daily living. The objectives of the present study were: 1) to assess the validity of aerobic fitness measurements based on anaerobic thresholds (ATs), during incremental sit-to-stand exercise (ISTS) with and without arm support compared with an incremental cycle-ergometer (CE) test; and 2) to examine the reproducibility of the AT measured during the ISTSs. Twenty-six healthy individuals randomly performed the ISTS and CE test. Oxygen uptakes at the AT (AT-VO2) and heart rate at the AT (AT-HR) were determined during the ISTSs and CE test, and repeated-measures analyses of variance and Tukey’s post-hoc test were used to evaluate the differences between these variables. Pearson correlation coefficients were used to assess the strength of the relationship between AT-VO2 and AT-HR during the ISTSs and CE test. Data analysis yielded the following correlations: AT-VO2 during the ISTS with arm support and the CE test, r = 0.77 (p < 0.05); AT-VO2 during the ISTS without arm support and the CE test, r = 0.70 (p < 0.05); AT-HR during the ISTS with arm support and the CE test, r = 0.80 (p < 0.05); and AT-HR during the ISTS without arm support and the CE test, r = 0.66 (p < 0.05). The AT-VO2 values during the ISTS with arm support (18.5 ± 1.9 mL·min-1·kg-1) and the CE test (18.4 ± 1.8 mL·min-1·kg-1) were significantly higher than those during the ISTS without arm support (16.6 ± 1.8 mL·min-1·kg-1; p < 0.05). The AT-HR values during the ISTS with arm support (126 ± 10 bpm) and the CE test (126 ± 13 bpm) were significantly higher than those during the ISTS without arm support (119 ± 9 bpm; p < 0.05). The ISTS with arm support may provide a cardiopulmonary function load equivalent to the CE test; therefore, it is a potentially valid test for evaluating AT-VO2 and AT-HR in healthy, young adults.
Key points.
The ISTS is a simple test that varies only according to the frequency of standing up, and requires only a small space and a chair.
The ISTS with arm support is valid and reproducible, and is a safe test for evaluating AT in healthy young adults.
For evaluating the AT, the ISTS may serve as a valid alternative to conventional CPX, using either a cycle ergometer or treadmill, in cases where the latter methods are difficult to implement.
Key words: Sit-to-stand, cycle ergometer, anaerobic threshold, correlations, reproducibility, validity
Introduction
Aerobic fitness measurements, such as maximal oxygen uptake (VO2 max) and anaerobic threshold (AT), are evaluated to determine an exercise intensity for training and to help understand the effects of the exercise interventions in cardiac rehabilitation and for lifestyle diseases (Wasserman et al., 2012). Aerobic fitness can be assessed by cardiopulmonary exercise testing (CPX) using either gas exchange analysis or determination of blood lactate concentration. Common forms of ergometry include cycle (CE) or treadmill testing, and these are regarded as the ‘gold standard’ in clinical practice, as well by performance on field tests such as the incremental shuttle walking test (ISWT) (Singh et al., 1994; Wasserman et al., 2012). CPX provides an accurate measurement of VO2 max and AT. However, it is not widely available for use in clinical settings, because it is expensive and requires trained staff and specialized equipment (Goto et al., 2007). Furthermore, traditional modes of testing may not be suitable for elderly and/or frail patients, who cannot cycle or walk safely (Sinconolfi et al., 1982 1; Wasserman et al., 2012). Sinconolfi et al. (1982) found that some participants, who were ≥ 39 years old struggled to perform 2 minutes of exercise during the cycle ergometer test because pedaling against a resistance was too difficult, citing both a lack of coordination and experience; therefore, test values underestimated aerobic fitness in this patient group. Conversely, field tests, which are simpler, inexpensive, and do not require complicated instrumentation, are commonly used in clinical settings (Singh et al., 1994). However, field tests generally require a large space and cannot be used for patients who cannot walk safely.
Sit-to-stand (STS) exercise uses the repetitive motion of standing up and sitting down in a chair, a common activity of daily living. STS exercise can be performed by a large number of patients. In addition, it only requires a small space and chair, and the exercise intensity can be easily adjusted by changing the patients’ sit-to-stand speed or the chair’s height (Kamimura and Akiyama, 2011; Nakamura et al., 2014). A STS test has been used to measure lower body strength in older adults and stroke patients in previous studies (Bohannon et al., 2011; Jones et al., 1999). In these latter studies, participants were encouraged to complete as many full stands as possible within a 30-s time limit from a chair with a seat height of 43.2 cm. However, few studies have used a STS test to assess aerobic fitness.
Kamimura et al. (2011) examined the relationship between oxygen uptake (VO2) and STS frequency during STS exercise and ATs during the CE test, and reported that the workrate associated with an STS frequency between 24–30 times/min during STS exercise corresponded to AT values during a CE test. Furthermore, in a previous study, we investigated the steady state VO2 in several speeds of standing up, and the steady state VO2 could not be confirmed at standing up frequencies greater than 24 times/min (Nakamura et al., 2014). However, to our knowledge, no reports are available on whether a STS test can determine aerobic fitness. If the validity of a simple test using STS exercise to evaluate aerobic fitness is established, similar to the ISWT (Singh et al., 1994), then the aerobic fitness of a greater number of subjects could be evaluated in clinical practice. As the first step in establishing the validity of a STS test as an aerobic fitness measurement, an evaluation of AT during STS exercise is necessary. Therefore, based on the findings from a previous study (Nakamura et al., 2014), we developed the incremental (I) STS exercise protocol for measuring aerobic fitness (Table 1).
Table 1.
Protocol for the incremental sit-to-stand exercise (ISTS).
| Level | Time (seconds) | Standing up frequency (times/min) | Sum standing up (times) |
|---|---|---|---|
| 1 | 45 | 6 | 4 |
| 2 | 90 | 8 | 10 |
| 3 | 135 | 10 | 17 |
| 4 | 180 | 12 | 26 |
| 5 | 225 | 14 | 36 |
| 6 | 270 | 16 | 48 |
| 7 | 315 | 18 | 61 |
| 8 | 360 | 20 | 76 |
| 9 | 405 | 22 | 92 |
| 10 | 450 | 24 | 110 |
| 11 | 495 | 26 | 129 |
| 12 | 540 | 28 | 150 |
| 13 | 585 | 30 | 172 |
| 14 | 630 | 32 | 196 |
| 15 | 675 | 34 | 221 |
| 16 | 720 | 36 | 248 |
Moreover, the effect of using arm support on the physical workload during the STS exercise remains unclear. Although two studies measuring cardiorespiratory responses during the STS exercise did not use arm support, using arm support during the STS exercise has benefits. Firstly, it reduces the burden on the subject’s knee joints (Arborelius et al., 1992; O’Meara et al., 2006), which is useful in clinical practice. Secondly, when using an arm support, the muscles of both the upper and lower extremities are used. Without arm support, only the muscles of the lower extremities are used. The exercise mode used for testing affects many physiological responses to exercise. For example, combining arm with leg exercise results in a greater VO2max than leg exercise alone (Nagle et al., 1984). Additionally, the AT is 35% higher in a CE test than in a corresponding arm crank test (Orr et al., 2013). Similarly, Sugiyama et al. (2013) reported that VO2 values at the same walking speed were significantly higher during Nordic walking, using poles to push-off, compared to normal walking. It is often assumed that the primary reason for this difference is the amount of muscle mass that is activated during the exercise (Nagle et al., 1984; Hill et al., 2014; Orr et al., 2013). A greater understanding of the impact of the use of arm support during STS exercise on aerobic fitness measures is critical to developing valid methods for evaluating aerobic fitness.
Therefore, the purposes of the present study were: 1) to investigate the validity of aerobic fitness measurements during the ISTS with and without arm support, based on AT values, compared with the CE test; and 2) to examine the reproducibility of the AT values measured during the ISTSs. We hypothesized that there would be strong relationships between the AT values determined by the ISTSs and CE test.
Methods
Study design
This cross-sectional study was conducted at Shinshu University, and was approved by the Shinshu University School of Medicine’s Ethics Committee and Matsumoto City Hospital’s Ethics Committee. All the volunteers were familiarized with the experimental procedures, and written informed consent was obtained.
Subjects
An appropriate sample size was estimated based on the aforementioned hypothesis. Assuming a standardized effect size for Pearson’s correlation analysis of 0.70 in order to achieve a statistical power of 80% with a two-sided significance level of 0.05, we estimated that approximately 13 subjects were required (Hulley et al., 2013).
Twenty-six healthy young college students (13 men and 13 women) were recruited for the validity study of the ISTSs for evaluating AT (group A). Of those, 10 (7 men and 3 women) were recruited for the reproducibility study of the ISTSs (group B). The selection criteria were as follows: 1) aged 20–29 years, 2) students enrolled at Shinshu University, 3) no history of bone, joint, or cardiorespiratory disease that would impede exercise, and 4) willing to provide voluntarily consent to participate. Table 2 shows the subjects’ physical characteristics for groups A and B.
Table 2.
Physical characteristics of all subjects included in the study. Values are presented as mean (±standard deviation).
| Group A (n = 26) | Group B (n = 10) | |||
|---|---|---|---|---|
| All (n=26) | Men (n=13) | Women (n=13) | All (n=10) | |
| Age (years) | 21.0 (1.4) | 21.2 (1.3) | 20.8 (1.5) | 21.6 (2.0) |
| Height (m) | 166.4 (8.8) | 173.6 (5.8) | 159.2 (3.8) | 169.5 (8.3) |
| Weight (kg) | 56.3 (7.0) | 61.8 (4.1) | 50.9 (4.5) | 56.7 (7.5) |
| Sitting height (cm) | 87.9 (4.8) | 91.0 (4.7) | 84.8 (2.4) | 89.9 (3.8) |
| Height of chair (cm) | 42.5 (2.0) | 43.6 (1.9) | 41.3 (1.3) | 42.9 (1.9) |
| BMI (kg·m-2) | 20.3 (1.9) | 20.6 (2.0) | 20.1 (1.7) | 19.7 (2.3) |
BMI, body mass index. Group A, the validity study of the incremental sit-to-stand exercises . (ISTSs) for evaluating the aerobic threshold (AT). Group B, the reproducibility study of the ISTSs for evaluating the AT.
Exercise protocols
All subjects performed the ISTSs with and without arm support in a random sequence (according to a protocol developed from a previous study) and a CE test with a minimum of 3 and a maximum of 14 days separating the tests (Nakamura et al., 2014). Ten of the 26 students performed the ISTSs with and without arm support once more between the three day to two-week interval. The subjects were asked to fast for 2 h prior to each exercise test.
During the ISTS with arm support, subjects were instructed to use both hands on the pole to push off; however, we did not limit how much force they used. The pole was adjusted to a specific height such that the elbows of the subjects were at right angles in the standing position. Conversely, during the ISTS without arm support, the subjects were asked to cross their arms in front of their chest during exercise to prevent any involuntary movement of the arms (Kamimura and Akiyama, 2011; Nakamura et al., 2014). Accordingly, subjects had to touch each ‘target’ in the upright and seated position in order to define the STS motion (Figure 1). Participants’ feet were placed in a comfortable position and were set shoulder width apart. The chair height for the ISTSs was adjusted to the level of the upper end of the participants’ fibular head (Kamimura and Akiyama, 2011; Nakamura et al., 2014). The ISTS protocol consisted of 3 min of rest, followed by 3 min of warm-up, and then 12 min of exercise. The frequency during the ISTS was 6 times/min during the warm-up period and was 6–36 times/min during the 12-min exercise period (Table 1) (Nakamura et al., 2014). The frequency of standing up was controlled by audio signals via a metronome.
Figure 1.
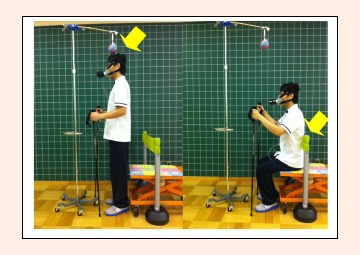
The position of the incremental sit-to-stand exercise (ISTS) with arm support. The subjects had to touch each target (yellow arrows) in the upright and sitting positions.
During the CE test, a ramp exercise protocol was used with a cycle ergometer (Aerobike 75XLII; Combi, Tokyo, Japan). Following 3 min of seated rest, the subject commenced a 3 min warm-up at 10 watts. After the warm-up period, the power output in the ramp test was increased by 20 watts/min (Wasserman et al., 2012; Ito et al., 2013). The subjects maintained a cadence of 60 pedal revolutions/min throughout the test.
The criteria for the suspension of the test were as follows: 1) when it corresponded to the general discontinuance criteria for exercise tests (American College of Sports Medicine, 2013); 2) when the heart rate (HR) reached 80% of the predicted maximum HR [206 – (0.67 × age)] (Gellish et al., 2007); or 3) when a subject missed the pacing given by the metronome for the third time in a row (Kamimura and Akiyama, 2011; Nakamura et al., 2014); and 4) when the subject became unable to maintain a cadence of 60 pedal revolutions/min.
Measurements included expired gases, HR, systolic blood pressure (SBP), diastolic blood pressure (DBP), and the Borg 15-point category rating of perceived exertion scale (RPE) (Borg, 1970). Subjects were instructed to provide RPE estimations corresponding to subjective feelings of RPE-ventilatory effort and RPE-leg muscular fatigue (Borg, 1970; Green et al., 2003). During testing, expired gases such as oxygen uptake (VO2), carbon dioxide output (VCO2), and HR were continuously monitored. Heart rate was measured using a belt HR monitor (H2 Heart Rate Sensor; Polar, Finland). Expired gases were measured using a breath-by-breath analyzer (AT1100, Anima; Tokyo, Japan). The gas analyzer was calibrated prior to and following each test using precision reference gases. The breath-by-breath expired gas data were converted into time series data. The data sets were calculated using the gas analysis software for the AT1100, in which the variable moving average was performed. A nine-point moving average of the data was applied to the calculation for the respiratory gas parameters. SBP and DBP at rest and immediately after completion of the exercise and the RPE scales and double product ([DP] = HR × SBP) immediately after completion of the exercise were measured to confirm the safety of the exercise (Gobel et al., 1978). The temperature in the exercise room was maintained between 21 and 24ºC.
The AT point was determined by two evaluators using the following criteria derived from gas exchange analysis: 1) the point when the minute ventilation VE/VO2 curve, having been flat or decreasing, begins to rise as the VE/VCO2 curve remains constant or decreases; 2) the point when the end tidal PETCO2-work rate curve is slowly rising or constant, but the PETO2-work rate curve, having been declining or flat, begins to rise; 3) the point when VCO2 increased in volume greater than that of the VO2 volume; and 4) the point when the RER value versus exercise time, which was flat or slowly increasing, begins to increase more sharply (Wasserman et al., 1984; Beaver et al., 1986). All VO2 measures were relative to body mass (mL/min/kg). AT-VO2 and AT-HR were determined during the ISTSs and CE tests.
The highest exercise VO2 and HR were defined as the average value obtained during the last 30 s of testing.
Statistical analysis
Statistical analysis was performed using SPSS software for Windows (SPSS Inc., version 18.0J, Chicago, IL, USA). The values are presented as means ± standard deviations and medians (interquartile ranges). The Shapiro-Wilk test was used to determine normality of values. Pearson’s correlation test was performed to assess the strength of the relationship between the AT-VO2 and the AT-HR during the ISTSs (with or without arm support) and during the CE test. Repeated-measures analyses of variance were applied for AT-VO2 and AT-HR across the exercise conditions. If an F value was significant, a post-hoc Tukey’s procedure was used to determine which test differences were significant (P<0.05). Intraclass correlation coefficients (ICC) (1,1) (95% confidence interval [CI]) for AT-VO2 and AT-HR obtained in the first and second ISTSs with or without arm support were used to determine the reproducibility of the ISTSs. Friedman tests or repeated-measures analyses of variance were used to compare the physiological workload values obtained during the ISTSs and CE test.
Results
The AT of all the subjects was measured before the test was terminated. Twelve of 26 subjects during ISTS with arm support and thirteen of 26 during ISTS without arm support completed the ISTSs before their HR reached 80% of the predicted maximum HR. The rest of the subjects finished the ISTSs when their HR reached 80% of the predicted maximum HR. For the CE test, all subjects finished when their HR reached 80% of the predicted maximum HR.
The correlations between each variable were as follows: AT-VO2 values during the ISTS with arm support and the CE test, r = 0.77 (p < 0.05) (Figure 2); AT-VO2 values during the ISTS without arm support and the CE test, r = 0.70 (p < 0.05) (Figure 3); AT-HR during the ISTS with arm support and the CE test, r = 0.80 (p < 0.05); and AT-HR during the ISTS without arm support and the CE test, r = 0.66 (p < 0.05).
Figure 2.
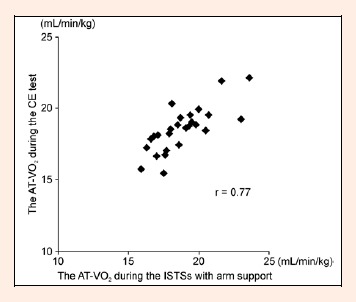
The correlation between the anerobic threshold (AT) for oxygen uptake VO2 during the incremental sit-to-stand exercise (ISTS) with arm support and the cycle-ergometer (CE) test (n = 26).
Figure 3.
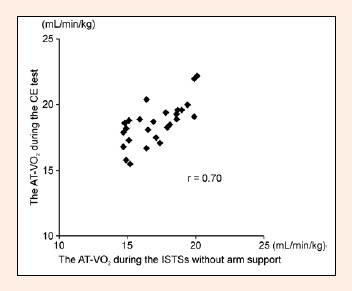
The correlation between the aerobic threshold (AT) for oxygen uptake (VO2) during the incremental sit-to-stand exercise (ISTS) without arm support and the cycle-ergometer (CE) test (n = 26).
The AT-VO2 values during the ISTS with arm support and the CE test results were significantly higher than those during the ISTS without arm support (p < 0.05). The AT-HR during the ISTS with arm support and the CE test results were significantly higher than those during the ISTS without arm support (p < 0.05) (Table 3).
Table 3.
Comparison of the anaerobic threshold (AT) for oxygen uptake (VO2) and the AT for heart rate (HR) between the incremental sit-to-stand exercises (ISTSs) and cycle-ergometer (CE) test. Values are presented as mean (± standard deviation) (n = 26).
| ISTS (without arm support) |
ISTS (with arm support) |
CE | ||
|---|---|---|---|---|
| AT-VO2 (mL/min/kg) | All | 17.1 (1.8) a, b | 18.8 (1.9) a | 18.6 (1.6) b |
| Men | 17.2 (1.9) a, b | 19.1 (2.5) a | 18.8 (2.0) b | |
| Women | 16.9 (1.8) a, b | 18.5 (1.3) a | 18.4 (1.0) b | |
| AT-HR (bpm) | All | 120.3 (9.6) a, b | 125.7 (10.3) a | 125.8 (12.6) b |
| Men | 119.0 (10.8) a, b | 125.8 (12.6) a | 124.0 (15.3) b | |
| Women | 119.5 (6.0) a, b | 125.5 (8.0) a | 127.5 (9.4) b | |
a, b, the difference (p < 0.05) between the text symbols.
The ICCs (1,1) (95% CI) used to verify agreement of the AT-VO2 between the test and retest of the ISTS with and without arm support were 0.92 (0.74–0.98) and 0.82 (0.45–0.95), respectively. The ICCs of the AT-HR between the test and retest in the ISTS with and without arm support were 0.83 (0.48–0.95) and 0.81 (0.44–0.95), respectively.
No significant differences were observed among the ISTS with arm support, ISTS without arm support, and CE test with regard to HR, SBP, DBP at rest, and Borg score immediately after completion of exercise. There was a significant effect (p < 0.05) of exercise protocol on the highest exercise VO2. The highest exercise HR and SBP immediately after exercise were significantly lower (p < 0.05) during the ISTS without arm support than the CE test, and the DP immediately after exercise was significantly lower for the ISTS with and without arm support compared with the CE test (Table 4).
Table 4.
Physiological work load of the incremental sit-to-stand exercises (ISTSs) and cycle-ergometer (CE) test at rest and after exercise testing. Values are presented as mean (± standard deviation) and median (interquartile range) (n= 26).
| ISTS (without arm support) |
ISTS (with arm support) |
CE | ||
|---|---|---|---|---|
| Rest | HR (bpm) | 78(8) | 76(7) | 78(7) |
| SBP (mmHg) | 120.0 (11.0) | 120.7 (10.4) | 121.5 (9.2) | |
| DBP (mmHg) | 70.2 (5.6) | 70.1 (7.7) | 70.2 (7.0) | |
| Highest exercise | VO2 (mL·min-1·kg-1) | 23.1 (1.4) a, b | 24.1 (1.4) a, c | 28.0 (1.9) b, c |
| HR (bpm) | 150(8) b | 153(9) | 157(4) b | |
| After completion of the exercise testing | SBP (mmHg) | 141.0 (9.6) b | 143.1 (8.6) | 145.1 (9.1) b |
| DBP (mmHg) | 73.7 (6.7) | 75.2 (6.4) | 76.3 (5.9) | |
| DP | 21093 (2430) b | 21214 (2183) c | 22043 (1681) b,c | |
| Borg scale | Ventilatory effort | 14 (13–14) | 14 (13–14) | 14 (14–15) |
| Fatigue of legs | 13 (13–14) | 12 (12–13) | 15 (14–15) | |
HR, heart rate; SBP, systolic blood pressure; DBP, diastolic blood pressure; DP, double product; RPE, rating of perceived exertion.
a, b, c, the difference (p < 0.05) between the text symbols.
Discussion
This is the first study to investigate the utility of an incremental and externally controlled test using STS exercise for evaluating the anaerobic threshold in healthy young individuals.
Validity of the incremental sit-to-stand exercises
The AT of all subjects was determined during the ISTSs and CE test. Ito et al. (2013) reported standard values of AT in the normal Japanese population, and showed that the AT-VO2 values during the CE test were 19.1 ± 3.6 mL·min-1·kg-1 in men and 17.5 ± 2.6 mL·min-1·kg-1 in the women. The AT-VO2 values during the ISTS with arm support and CE test in the present study were similar to those previously reported by Ito et al. (2013).
There were significant high correlations (r = 0.70–0.77) for the AT-VO2 values between the ISTSs and CE test, whereas there were significant moderate to high correlations (r = 0.66–0.80) for the AT-HR values between the ISTSs and CE test. Many studies have investigated the relationship between aerobic fitness and exercise using different exercise modalities, e.g., cycle ergometry, treadmill (Glassford et al., 1965), arm crank (Orr et al., 2013), and stepper exercise (Billinger et al., 2008). For instance, Glassford et al. (1965) reported a significant correlation between a CE test and treadmill test for VO2 max (r = 0.65–0.74). Additionally, Orr et al. (2013) reported a significant correlation between arm crank and CE tests for AT (r = 0.60), both of which are common rhythmic exercises in which the physical load and rate are controlled externally and incrementally. The ISTS test is also an incrementally and externally controlled test similar to both the CE and treadmill protocols, and a significant relationship between the AT values during the ISTS test and a CE test was confirmed in the present study.
On the other hand, the AT-VO2 during ISTS with arm support was similar to that seen during the CE test, whereas the AT-VO2 during the ISTS without arm support was about 8% lower. Many studies have indicated that the VO2max and AT-VO2 are different between exercise modalities (Hill et al., 2014; Ito et al., 2013; Muraki et al., 2004; Nagle et al., 1984; Orr et al., 2013). The amount of muscle mass used, along with the type and distribution of active motor units involved in the exercise and the frequency of muscle contractions, may be the source of the differences observed between the different exercise modes (Hill et al., 2014; Muraki et al., 2004; Nagle et al., 1984; Orr et al., 2013). Moreover Muraki et al. (2004) studied muscle oxygen saturation, oxyhemoglobin, and deoxyhemoglobin during arm and leg exercise in young women, and reported that anaerobic metabolism occurred at a lower power output during arm exercise. They also concluded that aerobic fitness measures such as VO2max and AT during arm ergometry was limited due to early oxygen utilization. This may be because of the greater recruitment of type-2 muscle fibres with arm exercise compared with leg exercise. Type-2 fibres are metabolically less efficient than type-1 fibres (Kushmerick et al., 1992), and a greater recruitment of type-2 motor units occurs during exercise with a higher intramuscular tension (Ahlquist et al., 1992). As exercise intensity increases, a higher muscle force is required to continueexercise when using a smaller muscle mass, such as with arm compared to leg ergometry. In many studies where a combined arm and leg exercise was compared to cycling only, a greater VO2max was observed in the combined exercise than in leg only exercise (Gleser et al., 1974; Nagle et al., 1984). Nagle et al. (1984) showed that 10–20% of arms and 80–90% legs contributed to the total power output during the combined exercise. In the present study, the proportional contribution of the arms and legs to total power output during ISTS was unclear; however, the ISTS using arm support can elicit greater VO2 values compared with not using arm support. The ISTS test with arm support, in which a larger muscle mass is used compared to the ISTS test without arm support, may delay the onset of peripheral fatigue and reduce the recruitment of type-2 motor units compared to the ISTS test without arm support. For these reasons, the ISTS test with arm support is potentially more stressful to the cardiopulmonary system than the ISTS test without arm support, and may provide a cardiopulmonary function load equivalent to a CE test.
The present findings indicated that ISTS with arm support is a potentially valid test for determining the AT-VO2 and AT-HR in healthy young men and women.
Reproducibility of the incremental sit-to-stand exercises
Current data demonstrated high test-retest reliabilities (ICCs = 0.81–0.92) between the repeated AT-VO2 and AT-HR values during the ISTSs. One reason for this finding is probably because the ISTS is an externally paced test, and the exercise load was controlled by external signals in common with other CPX. Davis et al. (1976) showed that the test-retest reliability of AT-VO2 values during CPX in healthy young individuals was high (r = 0.72–0.74). The high ICCs in the present study between the AT-VO2 and AT-HR values during the ISTSs are similar to those reported during CPX testing (Davis et al., 1976). In contrast, the reproducibility between the 6 minute walking distance (MWD) test; 6MWD1 and 6MWD2 was lower than that between the 6MWD2 and 6MWD3, possibly because the six minute walk-test was conducted as a self-paced test – which may be affected by motivation and/or learning (Bellet et al., 2012; Kervio et al., 2003). Another reason for the high ICCs for AT-VO2 and AT-HR values during the ISTSs may be related to chair height and the speed set during the ISTSs, which were appropriate for healthy young people. However, because the 95% CI in the ICCs of the AT values during the ISTSs were wide (95% CI in ICCs = 0.44–0.98) while the ICCs are high, a further study on a larger group is needed to clarify the reproducibility of the AT-VO2 and AT-HR values obtained during ISTSs. Furthermore, the use of arm support and its position (height) during the ISTS may need to be further defined, in order to enhance reproducibility.
Safety of the incremental sit-to-stand exercises
Since no subjects reached the discontinuance criteria, this protocol was considered to have a safe physical workload for healthy young individuals.
DP after exercise was significantly lower for the ISTS with and without arm support compared to the CE test. Gobel et al. (1978) showed that the myocardial oxygen consumption correlated well with DP, thus we hypothesize that the myocardial oxygen consumption during the ISTSs may be lower than that during the CE test. In the present study, RPE-leg muscular fatigue after exercise in ISTS testing was lower than that in CE testing. This finding suggests that the load on the legs during ISTS testing is lower than that during cycle ergometry, and ISTS testing may be more beneficial for patients who have difficulty cycling. Furthermore, RPE-leg muscular fatigue in ISTS testing was lower than the RPE-ventilatory effort. The results of ISTS testing could be more a measure of cardiopulmonary fitness than lower extremity strength or endurance, and may more appropriately reflect aerobic fitness.
Study limitations and future research
The present study had some limitations. Namely, only healthy young individuals were recruited; therefore, further studies using an older population is needed to develop the ISTS as an aerobic fitness measure suitable for elderly and frail patients. Furthermore, because knee pain may be provoked when the elderly perform the ISTS, the height of the chair and frequency of the sit-to-stand speed will need to be adjusted. Yoshioka et al. (2014) reported that during sit-to-stand, the peak hip and knee joint moments decrease inversely, relative to chair height within the range of normal to high seat height. A further study investigating the effect of different seat heights during the ISTS test on VO2 values is needed. In addition, in order to be functionally useful for elderly and frail patients, and to enhance the reproducibility of ATs determined during the ISTS test, arm position and arm use during the test needs further investigation.
To further validate this new, simple method using STS exercise to evaluate aerobic fitness (as the anaerobic threshold), additional studies investigating the relationship between performance and aerobic fitness during the ISTS and CE tests are necessary. The results of the present study provide a foundation for the use of the ISTS test for the assessment of aerobic fitness.
Conclusion
This is the first study to evaluate aerobic fitness using incremental sit-to-stand exercise. The present study demonstrates that the relationships between AT values during the ISTS and CE tests were significant and strong, and that the AT-VO2 during the ISTS test with arm support was similar to that measured in the CE test. Findings indicate that the ISTS with arm support is a potentially valid, reproducible, and safe test for evaluating the AT in healthy young adults as an alternative to conventional CPX using either cycle or treadmill ergometry in situations where these methods are difficult to implement.
Acknowledgements
We thank for the staff for their assistance in data collection, the participants, rehabilitation staff of Matsumoto City Hospital, and the students of Shinshu University.
Biographies

Keisuke NAKAMURA
Employment
Department of Rehabilitation, Matsumoto City Hospital
Degree
MS, PhD student
Research interest
Exercise therapy
E-mail: keipons55@yahoo.co.jp

Masayoshi OHIRA
Employment
Department of Physical Therapy, School of Health Sciences, Shinshu University
Degree
MA
Research interest
Exercise therapy
E-mail: mohira@shinshu-u.ac.jp

Yoshiharu YOKOKAWA
Employment
Department of Physical Therapy, School of Health Sciences, Shinshu University
Degree
PhD
Research interest
Public health, Health science, Gerontology
E-mail: fhakuba@shinshu-u.ac.jp

Yuya NAGASAWA
Employment
Department of Rehabilitation, Matsumoto City Hospital
Degree
RPT
Research interest
Exercise therapy
E-mail: shinn_yu_ra@yahoo.co.jp
References
- Ahlquist L.E., Bassett D.R., Sufit R., Nagle F.J., Thomas D.P. (1992) The effect of pedaling frequency on glycogen depletion rates in type I and type II muscle fibers during submaximal cycle exercise. European JournalofApplied Physiology 65, 360-364. [DOI] [PubMed] [Google Scholar]
- American College of Sports Medicine. (2013) Interpretation of Results. ACSM’s Guidelines for Exercise Testing and Prescription. Pescatello L.S., Arena R., Riebe D., Thompson P.D. 9th edition Philadelphia: Lippincott Williams & Wilkins; 87. [DOI] [PubMed] [Google Scholar]
- Arborelius U.P., Wretenberg P., Lindberg F. (1992) The effects of armrests and high seat heights on lower-limb joint load and muscular activity during sitting and rising. Ergonomics 35, 1377-1391. [DOI] [PubMed] [Google Scholar]
- Beaver W.L., Wasserman K., Whipp B.J. (1986) A new method for detecting anaerobic threshold by gas exchange. Journal of Applied Physiology 60, 2020-2027. [DOI] [PubMed] [Google Scholar]
- Bellet R.N., Adams L., Morris N.R. (2012) The 6-minute walk test in outpatient cardiac rehabilitation: validity, reliability and responsiveness - a systematic review. Physiotherapy 98, 277-286. [DOI] [PubMed] [Google Scholar]
- Billinger S.A., Loudon J.K., Gajewski B.J. (2008) Validity of a total body recumbent stepper exercise test to assess cardiorespiratory fitness. Journal ofStrengthand Conditioning Research 22, 1556-1562. [DOI] [PubMed] [Google Scholar]
- Bohannon R.W. (2011) Test-retest reliability of the five-repetition sit-to-stand test: A systematic review of the literature involving adults. Journal of Strength and Conditioning Research 25, 3205-3207. [DOI] [PubMed] [Google Scholar]
- Borg G. (1970) Perceived exertion as an indicator of somatic stress. Scandinavian Journal of Rehabilitation Medicine 2, 92-98. [PubMed] [Google Scholar]
- Davis J.A., Vodak P., Wilmore J.H., Vodak J., Kurtz P. (1976) Anaerobic threshold and maximal aerobi c power for three modes of exercise. Journal of Applied Physiology 41, 544-550. [DOI] [PubMed] [Google Scholar]
- Gellish R.L., Goslin B.R., Olson R.E., McDonald A., Russi G.D., Moudgil V.K. (2007) Longitudinal modeling of the relationship between age and maximal heart rate. Medicine and Science in Sports and Exercise 39, 822-829. [DOI] [PubMed] [Google Scholar]
- Glassford R.G., Baycroft G.H., Sedgwick A.W., Macnab R.B. (1965) Comparison of maximal oxygen uptake values determined by predicted and actual methods. Journal of Applied Physiology 20, 509-513. [DOI] [PubMed] [Google Scholar]
- Gleser M.A., Horstman D.H., Mello R.P. (1974) The effect on VO2max of adding arm work to maximal leg work. Medicine and Science in Sports 6, 104-107. [PubMed] [Google Scholar]
- Gobel F.J., Norstrom L.A., Nelson R.R., Jorgensen C.R., Wang Y. (1978) The rate-pressure product as an index of myocardial oxygen consumption during exercise in patients with angina pectoris. Circulation 57, 549-556. [DOI] [PubMed] [Google Scholar]
- Goto Y., Saito M., Iwasaka T., Daida H., Kohzuki M., Ueshima K., Makita S., Adachi H., Yokoi H., Omiya K., Mikouchi H., Yokoyama H., Japanese Cardiac Rehabilitation Survey Investigators. (2007) Poor implementation of cardiac rehabilitation despite broad dissemination of coronary interventions for acute myocardial infarction in Japan. Circulation Journal 71, 173-179. [DOI] [PubMed] [Google Scholar]
- Green J.M., Crews T.R., Bosak A.M., Peveler W.W. (2003) Overall and differentiated ratings of perceived exertion at the respiratory compensation threshold: effects of gender and mode. European Journal of Applied Physiology 89, 445-450. [DOI] [PubMed] [Google Scholar]
- Hill D.W., Vingren J.L. (2014) Effects of exercise mode and participant sex on measures of anaerobic capacity. Journal of Sports Medicine and Physical Fitness 54, 255-263. [PubMed] [Google Scholar]
- Hulley S.B., Cummings S.R., Browner W.S., Grady D.G., Newman T.B. (2013) Designing clinical research. 4th edition Lippincott Williams & Wilkins, Philadelphia. [Google Scholar]
- Ito H., Ajisaka R., Koike A., Makita S., Omiya K., Kato Y., Adachi H., Nagayama M., Maeda T., Tajima A., Harada N., Taniguchi K., Committee on Exercise Prescription for Patients (CEPP) Members. (2013) Heart rate and blood pressure response to ramp exercise and exercise capacity in relation to age, gender, and mode of exercise in a healthy population. Journal of Cardiology 61, 71-78. [DOI] [PubMed] [Google Scholar]
- Jones C.J., Rikli R.E., Beam W.C. (1999) A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Research Quarterly Exercise and Sport 70, 113-119. [DOI] [PubMed] [Google Scholar]
- Kamimura S., Akiyama S. (2011) The relationship between sit-to-stand frequency and anaerobic threshold determined by cycle ergometer. Journal of Physical Therapy Science 23, 53-55. [Google Scholar]
- Kervio G., Carre F., Ville N.S. (2003) Reliability and intensity of the six-minute walk test in healthy elderly subjects. Medicine and Science Sports and Exercise 35, 169-174. [DOI] [PubMed] [Google Scholar]
- Kushmerick M.J., Meyer R.A., Brown T.R. (1992) Regulation of oxygen consumption in fast- and slow-twitch muscle. American Journal of Physiology - Cell Physiology 263, C598-C606. [DOI] [PubMed] [Google Scholar]
- Muraki S., Tsunawake N., Yamasaki M. (2004) Limitation of muscle deoxygenation in the triceps during incremental arm cranking in women. European Journal of Applied Physiology 91, 246-252. [DOI] [PubMed] [Google Scholar]
- Nagle F.J., Richie J.P., Giese M.D. (1984) VO2max responses in separate and combined arm and leg air-braked ergometer exercise. Medicine and Science in Sports Exercise 16, 563-566. [PubMed] [Google Scholar]
- Nakamura K., Ohira M., Yokokawa Y. (2014) The effect of different standing up frequencies in sit-to-stand exercise on oxygen uptake. Journal of Physical Therapy Science 26, 1631-1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Meara D, Smith R.M. (2006) The effects of unilateral grab rail assistance on the sit-to-stand performance of older aged adults. Human Movement Science 25, 257-274. [DOI] [PubMed] [Google Scholar]
- Orr J.L., Williamson P., Anderson W., Ross R., McCafferty S., Fettes P. (2013) Cardiopulmonary exercise testing: arm crank vs cycle ergometry. Anaesthesia 68, 497-501. [DOI] [PubMed] [Google Scholar]
- Siconolfi S.F., Cullinane R.M., Carleton R.A., Thompson P.D. (1982) Assessing VO2 max in epidemiologic studies: modification of the Astrand-Rhyming test. Medicine and Science in Sports and Exercise 14, 335-338. [PubMed] [Google Scholar]
- Singh S.J., Morgan M.D., Hardman A.E., Rowe C., Bardsley P.A. (1994) Comparison of oxygen uptake during a conventional treadmill test and the shuttle walking test in chronic airway limitation. European Respiratory Journal 7, 2016-2020. [PubMed] [Google Scholar]
- Sugiyama K., Kawamura M., Tomita H., Katamoto S. (2013) Oxygen uptake, heart rate, perceived exertion, and integrated electromyogram of the lower and upper extremities during level and Nordic walking on a treadmill. Journal of Physiological Anthropology 32, 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasserman K., Hansen J.E., Sue D.Y., Stringer W.W., Sietsema K.E., Sun X., Whipp B.J. (2012) Principles of exercise testing and interception. 4th edition Lippincott Williams & Wilkins, Philadelphia: 129-153. [Google Scholar]
- Wasserman K. (1984) The anaerobic threshold measurement to evaluate exercise performance. American Review of Respiratory Disease 129, S35-S40. [DOI] [PubMed] [Google Scholar]
- Yoshioka S., Nagano A., Hay D.C., Fukashiro S. (2014) Peak hip and knee joint moments during a sit-to-stand movement are invariant to the change of seat height within the range of low to normal seat height. BioMedical Engineering OnLine 13, 27. [DOI] [PMC free article] [PubMed] [Google Scholar]


