This comprehensive review of infectious and noninfectious syndromes associated with illicit drug use focuses on underrecognized complications of common illicit drugs and constellations of syndromes associated with emerging illicit drugs.
Keywords: illicit drug use, injection drug use, skin and soft-tissue infections, altered mental status, substance abuse
Abstract
Illicit drug use can result in a wide range of medical complications. As the availability, synthesis, and popularity of illicit drugs evolve over time, new syndromes associated with their use may mimic infections. Some of these symptoms are anticipated drug effects, and others are complications of adulterants mixed with drugs or complications from the method of using drugs. Some illicit drugs are associated with rare infections, which are difficult to diagnosis with standard microbiological techniques. The goal of this review is to orient a wide range of clinicians—including general practitioners, emergency medicine providers, and infectious diseases specialists—to complications of illicit drug use that may be underrecognized. Improving awareness of infectious and noninfectious complications of illicit drug can expedite diagnosis and medical treatment of persons who use drugs and facilitate targeted harm reduction counseling to prevent future complications.
In 2013, an estimated 24.6 million Americans aged ≥12 years (9.4% of the total population) were active illicit drug users [1]. Rates of morbidity and mortality associated with illicit drug use especially from use of opiates and heroin, is increasing in the United States [2, 3]. In contrast to demographics of drug use from 10 years ago, the most dramatic increases in illicit drug use have been recorded among young white persons living in rural areas [4, 5].
The methods of illicit drug use—including but not limited to smoking, snorting, injecting, and “skin popping”—are risk factors for infectious diseases. There are several well-known infectious complications of injection drug use, including tissue and bloodstream infections, bacterial endocarditis, human immunodeficiency virus (HIV), and viral hepatitis [6]. There are also underrecognized (and some newly emerging) complications of commonly used illicit drugs, including cocaine and marijuana, which can cause patterns of multisystem organ dysfunction similar to infectious syndromes. Furthermore, several emerging illicit drugs, including synthetic cannabinoids, cathinone derivatives, and piperazine derivatives, are not detected with simple urine or blood toxicology screens and can cause symptoms that mimic infections; synthetic cannabinoids, in particular, are increasing in popularity (38% of persons in substance abuse treatment programs report use), with major increases in hospitalizations and deaths reported in the United States since 2011 [7, 8].
Diagnosis and treatment of clinical syndromes related to illicit drug use are hampered by lack of validated toxicology screens, in addition to reluctance of persons who use drugs (PWUD) to report their drug use history and lack of knowledge among providers that these new illicit drugs and syndromes exist. The goal of this review is to give clinicians a foundation of knowledge to inform future clinical assessments and decision making in PWUD who present for medical care. We will discuss symptoms associated with emerging illicit drugs and underrecognized complications of commonly used drugs, and we will review these underrecognized complications in the context of the infectious disease syndromes they may mimic, including skin/soft-tissue infections, pneumonia, meningitis, and gastroenteritis. Through out this paper we use the term illicit drug use because it is widely accepted and commonly used in the litera ture, but it does have negative connotations; providers should be aware of this and try to decrease stigmatization in patient interactions. As defined by the federal agency SAMHSA [Substance Abuse and Mental Health Services Administration], illicit drug use is the use of illegal drugs or the misuse or abuse of prescription drugs; drugs include marijuana/hashish, cocaine/crack,heroin, hallucinogens, inhalants, and prescription—type psychotherapeutics—pain relievers, tranquilizers, stimulants, and sedatives-used nonmedically.
METHODS
Literature Search
We developed a search strategy for Medical Subject Heading (MeSH) terms and free text key words relevant to illicit drug use, including the following terms: drug abuse, illicit drug use, endocarditis, polysubstance abuse, emerging drugs of abuse, rare complications, toxicities, novel psychoactive substances, bath salts, synthetic cathinones, synthetic cannabinoids, jelling-up, crush-resistant, krokodil, cocaine, heroin, marijuana, methamphetamine, adulterants, levamisole, black tar heroin, anthrax, and tetanus. We searched the PubMed database for all relevant articles, published until June 2015 containing individual key words and combinations of above key words.
Emerging Illicit Drugs and Adulterants
Before discussing the presenting symptoms that may be seen in PWUD, it is important to review some of the emerging illicit drugs and adulterants. Details about their history, methods of use, mechanisms of action, desired effects, and adverse effects are provided in Table 1.
Table 1.
Emerging Illicit Drugs
| Name | History | Street Names | Method of Use | Mechanism of Actions | Desired Effects | Adverse Effects/Reactions |
|---|---|---|---|---|---|---|
| Cathinones: methcathinone, mephedrone, methylenedioxy-pyrovalerone, methylone, ethylone, butylone, methedrone [9–11] | Identified in 1975 as the principal psychoactive component of Khat (Catha edulis) leaves; first synthesized in 1928, explored for their stimulant, antidepressant and appetite suppressant properties | Khat, bath salts, ivory wave, vanilla sky, white rush, white lightning, white dove, meow meow, M-CAT, bubbles, cloud 9, explosion, impact, energy 1, bloom, blue silk | Oral; intranasal; can be inhaled, intravenous, intramuscular, or rectal |
Similar to amphetamines and catecholamines; inhibition of vesicular monoamine transporters for serotonin, dopamine, and norepinephrine; release of intracellular neurotransmitter stores; inhibition of MAO | Stimulation, euphoria, friendliness, sexual arousal, and perceptual disturbances | Anxiety, paranoia, hallucinations, psychosis, aggression, impaired working memory, bruxism, seizures, hypertension, tachycardia, coronary vasospasm, dysrhythmia, rhabdomyolysis, acute kidney injury, hyponatremia, hyperkalemia, metabolic acidosis, hyperthermia serotonin syndrome, disseminated intravascular coagulation, multiorgan failure, death |
| Cannabinoids [9, 11–13] | Derivatives of THC, first synthesized in the 1940s and studied for treatment of pain, anxiety and nausea | K2, spice, happy tiger incense, smoke, aroma, Aztec fire, black mamba, blueberry posh, Bombay blue, blaze, bliss, eclipse, krypton, Mr Smiley, Yucatan fire, Zohar, sensation vanilla | Ingested orally or smoked | Alteration in sensory perception and processing of stimuli in the hippocampus, amygdala, and prefrontal cortex via reduction of GABA release and increase in dopamine and glutamate release | Euphoria, relaxation, disinhibition, altered perception and consciousness; similar to marijuana | Anxiety, confusion, agitation, mood dysregulation, paranoia, psychosis (including long term), perceptual disturbances, suicidal ideation, sedation, memory impairment, tremors, seizures, nausea, vomiting, diaphoresis, xerostomia, mydriasis, tachycardia, hypertension, chest pain, acute MI, acute kidney injury, respiratory depression, tachyphylaxis, death |
| Krokodil (desomorphine) [14, 15] | Introduced as an analgesic in the 1940s, withdrawn in 1952 over concerns about addictive potential. | Krok, Russian magic | Injected subcutaneously or intravenously; also ingested orally | Potent mu-opioid agonist | Euphoria, relaxation, analgesia | Sedation, miosis, flushing, paresthesia, constipation, urinary retention, nausea/vomiting, allergic reactions, seizures, respiratory depression, pneumonia, septicemia, coronary artery burst, meningitis, ulcers and gangrene, rotting gums and tooth loss, bone infection |
| Piperazine derivatives [11, 16] | Initially developed as antihelminthics, also explored for their antidepressant properties | Legal ecstasy, party pills | Orally ingested | Central serotonogic effects; increased release and reuptake inhibition of dopamine, serotonin, and norepinephrine | Hallucinations, stimulation, euphoria | Hallucinations, confusion, anxiety, insomnia, dizziness, headaches, seizures, nausea/vomiting, shortness of breath, palpitations, sinus tachycardia, QT prolongation, seizures, hyponatremia, serotonin syndrome, hyperthermia, rhabdomyolysis, renal failure, disseminated intravascular coagulation |
| Salvia divinorum [9, 11, 16, 17] | Member of the mint family endemic to Mexico; historically used for its mind-altering effects | Salvia, diviner's sage, mystic sage, magic mint, Sally D, Maria pastora, Purple sticky | Most commonly smoked; also chewed and/or swallowed | Selective kappa opioid receptor agonist | Trancelike state, hallucinations, altered perception of self and environment, mood improvement | Hallucinations, confusion, anxiety, dysphoria, paranoia, psychosis, unmasked schizophrenia, language impairments, drowsiness, headache, diuresis |
| Levamisole [18–22] | Veterinary antihelminthic developed in the 1960s and currently approved by the FDA only as adjuvant chemotherapy | None | Adulterant | Immunostimulatory and immunomodulatory properties, increases brain dopamine levels; produces amphetaminelike metabolites | Increases cocaine bulk, enhances effects of cocaine | Agranulocytosis, vasculopathy, dermatological lesions, renal injury, leukoencephalopathy |
| Clenbuterol [23–25] | Veterinary agent developed in the 1970s for reactive airway disease in humans/animals; used illicitly by ranchers to increase mass of cattle, and by body builders | None | Adulterant | β2-Agonist | Enhance heroin bulk; weight loss, increase muscle mass | Agitation, tachycardia, palpitations, chest pain, myocardial injury, neuromuscular symptoms |
Abbreviations: FDA, Food and Drug Administration; GABA, gamma-Aminobutyric acid; MAO, monoamine oxidase inhibitor; MI, myocardial infarction; THC, tetrahydrocannabinol.
Complications of Illicit Drug Use
Table 2 summarizes the complications of illicit drug use that can mimic infectious syndromes.
Table 2.
Complications of Illicit Drug Use That Can Mimic Infectious Syndromes
| Syndrome | Agent | Clinical Features | Laboratory and Imaging Findings |
|---|---|---|---|
| Skin and soft-tissue syndromes | |||
| Skin ulceration | Krokodil [14] | Rash with scaly, green appearance, ulcerations, destruction of skin, muscle, cartilage, gangrene and skin sloughing | Nonspecific |
| Vasculitis | Levamisole [18, 20, 21] | Characteristic lesions are stellate lesion with erythematous borders and a necrotic center frequent on ears and cheeks | Agranulocytosis; positive titers of pANCA, cANCA, anti-cardiolipin, ANA, and anti-dsDNA; evidence of acute kidney injury in acute tubular necrosis pattern |
| Cocaine [26] | Urticarial vasculitis, Churg-Strauss vasculitis, necrotizing granulomatous vasculitis, palpable purpura, Buerger disease | Nonspecific | |
| Pneumonia and other pulmonary syndromes | |||
| Crack lung [27, 28] | Cocaine | Within 48 h of cocaine smoking: fever, dyspnea, pleuritic chest pain, hemoptysis, hypoxemia, respiratory failure | Imaging shows diffuse alveolar infiltrates, interlobular septal thickening, peribronchial nodules, ground glass opacities, nonspecific consolidation BAL with eosinophila, hemosiderin-laden macrophages, IgE deposition, hyaline membrane formation peripheral eosinophila |
| Subclinical alveolar hemorrhage [27, 28] | Cocaine (chronic use) | Largely asymptomatic; possible hemoptysis or nonspecific pulmonary symptoms | Diffuse alveolar hemorrhage with hemosiderin-laden macrophages in BAL fluid |
| Bronchospasm [27] | Cocaine | Bronchospasm with presentation resembling asthma; can be severe | Nonspecific |
| Pulmonary edema [28, 29] | Cocaine, amphetaminelike substances, heroin | Shortness of breath, cough | Radiographic evidence of bilateral or unilateral pulmonary edema; BAL fluid may reveal high protein concentrations |
| Pulmonary granulomatosis [27, 29] | Various drugs (intravenous drug injection or inhalation) | Pulmonary hypertension; interstitial fibrosis | Biopsy shows perivascular granulomatosis |
| Sepsis-like syndromes | |||
| Cotton fever [30–32] | Heroin | Fever, other typical sepsis features typically occurs 10–30 min after injection; usually self-limited | Leukocytosis, other sepsis features, negative blood cultures |
| Sympathomimetic effects [9–12, 33, 34] | MDMA, piperazine derivatives, synthetic cannabinoids, cathinone derivatives |
Tachycardia, hyperthermia, maybe be rhabdomyolysis with acute kidney injury | Synthetic cannabinoids, cathinone derivatives and piperazine derivatives not detected in standard urinary toxicology screens |
| Neurological syndromes | |||
| Stroke [11, 35] | Cocaine, methamphetamine, MDMA, synthetic cannabinoids, cathinone derivatives, marijuana | Abrupt onset of focal neurological symptoms, possibly accompanied by change in mental status or loss of consciousness | Evidence of ischemic or hemorrhagic stroke on brain imaging |
| Cranial nerve palsies [36, 37] | Black tar heroin contaminated with botulism and tetanus | Cranial neuropathy (including diplopia, opthalmoplegia, ptosis, and facial nerve palsy); may be accompanied by cellulitis, with possible necrotizing fasciitis and gangrene | Nonspecific |
| Seizures [9–11, 33] | Synthetic cannabinoids, cathinone derivatives, piperazine derivatives | Seizures; possibly status epilepticus | Synthetic cannabinoids and cathinone derivatives not detected in standard urinary toxicology screens |
| Leukoencephalopathy | Heroin [38] | Altered mental status, restlessness, apathy, cerebellar speech disturbance, ataxia, hyperactive reflexes, spasticity, tremor, choreoathetoid movements, hypotonia, areflexia, respiratory failure | Mild CSF pleocytosis; cerebellar signal abnormalities on MR images |
| Levamisole-adulterated cocaine [22] | Confusion, altered mental status, language impairment, visual changes, focal neurological deficits | White matter lesions on MR images, primarily affecting frontal lobes | |
| Gasteroenteritis syndromes | |||
| Intestinal ischemia [39, 40] | Methamphetamine, cocaine | Acute abdomen, abdominal pain, nausea, vomiting, diarrhea, melena, bloody stool, fevers, signs of shock | Colitis or abdominal perforation on imaging |
| Cannabinoid hyperemesis syndrome [41, 42] | Marijuana, synthetic cannabinoids | Abdominal pain, nausea and vomiting with relief of symptoms during warm bathing or showering | Marijuana but not synthetic cannabinoids at standard toxicology screening |
Abbreviations: ANA, antinuclear antibody; BAL, bronchoalveolar lavage; cANCA, cytoplasmic antineutrophil cytoplasmic antibodies; CSF, cerebrospinal fluid; IgE, immunoglobulin E; MDMA, 3,4-methylenedioxy-methamphetamine; MR, magnetic resonance; pANCA, perinuclear anti-neutrophil cytoplasmic antibodies.
Skin and Soft-Tissue Infections and Manifestations
Injection drug use is a common cause of skin and soft-tissue infections with both gram-positive skin flora and gram-negative enteric flora, dependent on the materials used to process and use the drug. Gram-positive infections from Staphlococcus aureus and Streptococcus pyogenes are the most common and result from introduction of skin flora past the epidermis into deeper tissues (discussed below in Sepsis-Like Syndromes). The risk of infection increases with larger needles, which can sometimes be used if the drug is too thick and clogs in the needle (“jelling up the dope”) [43]. Any clinical encounter with a PWUD should incorporate a review of harm reduction techniques, including cleaning the skin with alcohol before injecting and using bleach and water to disinfect syringes.
Two less common causes of severe skin-based infection are clostridial infections and anthrax. Clostridial infections can progress rapidly from cellulitis to necrotizing fasciitis or gas gangrene. Several outbreaks have been documented in the Western United States among black tar heroin users who inject using “skin popping,” the practice of injecting drugs subcutaneously, intradermally, or (rarely) intramuscularly [44]. Clostridial spores are introduced when black tar heroin is cut with brown material (eg, shoe polish, wood pulp, coffee grounds, or dirt) to increase bulk. Typically heroin is heated and dissolved in water before use, but clostridial spores can survive this process and even begin germination [6]. The most commonly involved clostridial species is Clostridium botulinum (also discussed below in the section below on neurological manifestations), but gangrene has also been reported from Clostridium perfringens, Clostridium sordellii, and Clostridium novyi [36, 37, 44–48]. Biopsy of the infected area can reveal black tar deposits in the tissue (Figure 1).
Figure 1.
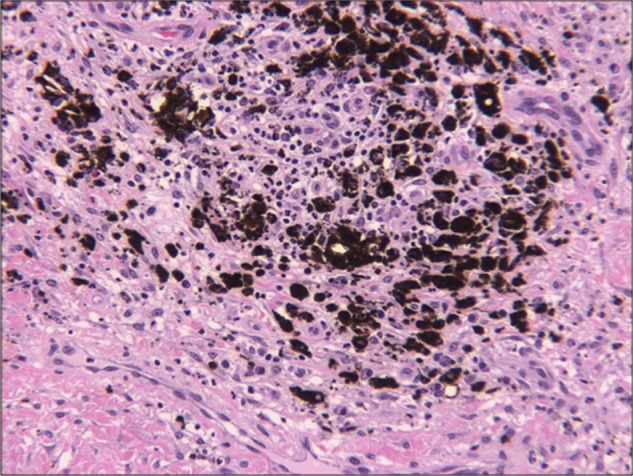
Tissue biopsy specimen from the shoulder of a patient with recent subcutaneous injection of tar heroin (400× photomicrograph).
Injectional anthrax infection was first described in Norway in 2000 in a group of PWUD who injected heroin subcutaneously. There have been 2 subsequent outbreaks, one in 2009 in the United Kingdom and another in 2012 in Northern Europe, Germany, and the United Kingdom [49, 50]. Although injectional anthrax can progress to secondary bacteremia, the initial presentation is a unique clinical syndrome lacking the classic black-crusted painless eschar of traditional cutaneous anthrax. Presenting symptoms are significant edema, necrosis, and blistering, potentially leading to compartment syndrome or necrotizing fasciitis. Imaging and soft-tissue exploration show edematous muscle and subcutaneous tissue with or without necrosis and without collections or abscesses. Other symptoms include nausea, vomiting, abdominal pain, and variable neurological syndromes, including meningitis and intracranial hemorrhage [49].
Two emerging illicit drugs should be considered when evaluating a PWUD with skin or soft-tissue symptoms. The first is the semisynthetic opioid derivative desomorphine, colloquially known as “krokodil.” The name derives from the green scaly appearance of the skin seen after injection, often accompanied by ulceration of skin, muscle, and cartilage. Tissue damage results from contamination with substances such as paint thinner, lighter fluid, gasoline, lead, zinc, and hydrochloric acid, which are used in the preparation of this drug. Damaged skin can become gangrenous, leading to sloughing of tissue down to the bone, often requiring extensive amputation [14]. Use of krokodil was first reported in Russia in 2003, and by 2013 cases were reported in Europe and the United States (Arizona, Utah, Oklahoma, and Illinois) [15].
The second drug that should be considered is levamisole, an increasingly common adulterant detected in the majority of cocaine seized in the United States and worldwide [18, 19]. Levamisole is a popular adulterant because it is inexpensive, similar in appearance to cocaine, and enhances cocaine's effects. Use of levamisole-adulterated cocaine, including snorting, injecting, or smoking, may lead to several complications related to an induced vasculopathy. Dermatological manifestations may include fixed drug eruptions, lichen planus, ulceration, nodules, erythema nodosum leprosum, nonspecific maculopapular rashes, and hemorrhagic bullae [18, 20]. The characteristic lesions are rapidly progressive cutaneous ecchymoses, raised purpura, and bullae resulting in a distinct stellate lesion with erythematous borders and a necrotic center, which have a predilection for the ears and cheeks (Figures 2 and 3) [18, 20, 21]. In addition to the dermatological manifestations, agranulocytosis, leukoencephalopathy, and acute kidney injury (suspected to be from renal tubular necrosis) can also be caused by levamisole [21]. Most patients with complications from levamisole have autoantibodies, including but not limited to pANCA, cANCA, anti-cardiolipin, antinuclear antibody, and anti–double-stranded DNA [20].
Figure 2.

Leg ulcerations attributed to levamisole-adulterated cocaine.
Figure 3.

Rash attributed to levamisole-adulterated cocaine.
Vasculitis is another common skin and soft-tissue manifestation that can be related to illicit drug use. Cocaine-induced midline destructive lesions, such as nasal septal and palatal perforations, are well-recognized effects of snorting cocaine that can mimic granulomatosis with polyangiitis, characterized by ANCA positivity (specifically, anti–human neutrophil elastase) [27]. Cocaine has also been reported to cause urticarial vasculitis, Churg-Strauss vasculitis, necrotizing granulomatous vasculitis, palpable purpura, Buerger disease, and scleroderma, which are either induced or unmasked by unknown mechanisms [26]. A rare complication of marijuana use is local arteritis, most often affecting the lower limbs, and may present as Raynaud phenomenon or as claudication followed by development of ulcers or gangrene, resembling Buerger disease [51]. The proposed mechanisms for these manifestations are related to vasoconstriction or actions of a contaminant [26].
Clinical Mimics of Pneumonia
PWUD presenting with shortness of breath or pleuritic chest pain may have complications of drug use other than pneumonia. One common syndrome called “crack lung” is a characteristic acute pulmonary manifestation that occurs after smoking crack cocaine. It is characterized by fever, dyspnea, pleuritic chest pain, and hemoptysis that can progress to hypoxemia and respiratory failure. Symptoms usually occur within 48 hours of crack cocaine use [27, 28]. Imaging can show diffuse bilateral alveolar infiltrates, interlobular septal thickening, peribronchial nodules, ground glass opacities, or nonspecific consolidation. Bronchoalveolar lavage is similarly nonspecific [27, 28]. Inhalation of cocaine can also be associated with a chronic, often subclinical, diffuse alveolar hemorrhage, for which proposed mechanisms include vasoconstriction, pulmonary infarction, and cocaine-induced thrombocytopenia [27, 28]. Bronchospasm is a separate and distinct entity from crack lunch which has been reported with use of freebase cocaine (cocaine heated to remove impurities) in both known asthmatics and nonasthmatics. There have also been several reported cases of new-onset severe acute asthma within a few months after the start of heroin use [29].
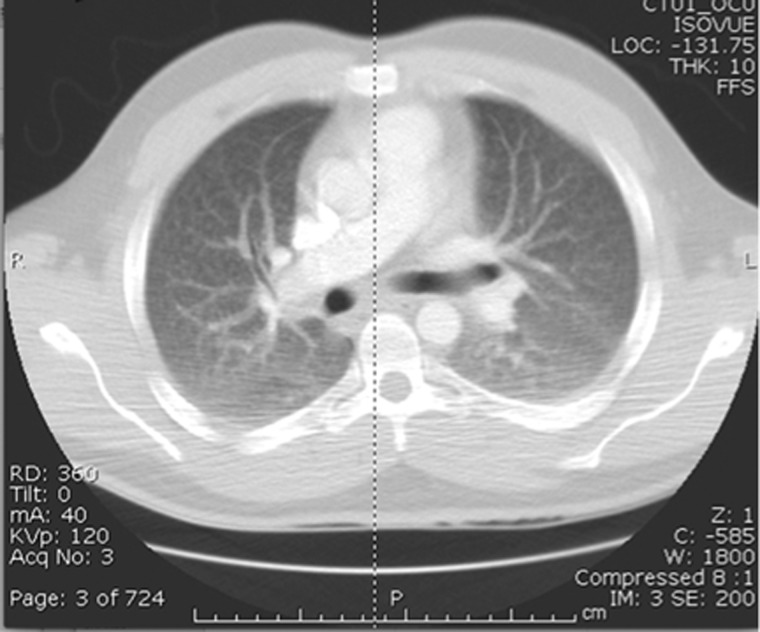
In addition to crack lung, other complications of illicit drug use may present with respiratory symptoms. Intravenous stimulant use is associated with pulmonary foreign body granulomas, pulmonary artery muscular hypertrophy, and fibrous intimal proliferation and has been linked to idiopathic pulmonary hypertension [27, 52, 53]. Pulmonary vascular granulomatosis is caused by embolization or inhalation of the drug itself, contaminants, or insoluble filler materials (such as silica, cellulose, and talc) into the lungs and other organs (Figure 4). Pulmonary vascular granulomatosis can progress to a pneumoconiosis-like interstitial fibrosis or pulmonary hypertension, both of which can be severe or fatal [27]. Pulmonary edema has been reported with use of stimulants (eg, cocaine and amphetamines), as well as heroin [27, 28]. Barotrauma-related injuries, including pneumomediastinum, pneumothorax, and pneumopericardium have been reported after the use of MDMA (3,4-methylenedioxy-methamphetamine), heroin, cocaine, and marijuana [28]. Direct puncture of the lung while performing "pocket shots" (ie, injection directly into the jugular or subclavian veins) can also lead to direct lung injury [27].
Figure 4.
Computed tomographic scan of patient with pulmonary granulomatosis from cocaine adulterated with talc.
Sepsis-Like Syndromes
The first concern for PWUD presenting with a sepsis-like syndrome should be bacteremia. The most common routes of infection are direct injection of bacteria via dirty and/or shared equipment and local spread from a cellulitis or soft-tissue infection. The most common causes of bacteremia in PWUD are S. aureus and S. pyogenes, although other types of oral and gastrointestinal flora (including Candida species) from licking needles or using dirty water can also cause a septic presentation [54–57]. PWUD can also present with bloodstream infections caused by less common organisms, such as Lactobacillius, Cornyebacteria, and Bacillus (very rarely, Bacillus anthracis), which should be considered as well as the more common bacterial causes and not discounted as a possible contaminant [58–62]. We have recently seen several cases of nontuberculous atypical mycobacterial bacteremias clustered among intravenous drug users hospitalized for drug-related bacterial infections and receiving antibiotics through peripherally inserted central catheters. These patients had fever and tachycardia, and Gram stains of their blood showed gram-positive rods that were originally mistaken for contaminant until sent to specialty laboratories for identification.
If a person who has a history of drug use presents with a sepsis-like syndrome with no growth in blood cultures, there are other illicit drug complications to consider. “Cotton fever” is a syndrome first characterized in 1975, which includes fevers and leukocytosis in the absence of positive blood cultures [30]. It characteristically occurs 10 to 30 minutes after injection of heroin. Its cause is related to the practice of using cotton to filter out particulate matter when drawing up liquid heroin and then heating the used cotton to extract residual drops of heroin that are injected, a practice colloquially referred to as “shooting the cotton” [31, 32]. Research has shown that a gram-negative bacterium, Enterobacter agglomerans, colonizes the cotton plant and produces an endotoxin, which may be responsible for the fevers [63]. The syndrome is usually self-limited, yet the symptoms may be worrisome and lead PWUD to seek emergency care [32, 64].
Tachycardia and hyperthermia are common adverse effects of MDMA (also known as Ecstasy or Molly). Several of the emerging drugs, including synthetic cannabinoids, cathinone derivatives, and piperazine derivatives, can also cause hyperthermia and tachycardia and have been further linked to cases of serotonin syndrome. Urine toxicology assays used at most hospitals will not detect these drugs, so if there is a concern about illicit drug use, it is important to specifically ask the patient about these substances [9, 10, 33]. One clue that a person with hyperthermia and tachycardia might be using these drugs is acute kidney injury secondary to rhabdomyolysis. In a similar manner to cocaine, MDMA, cathinone derivatives, synthetic cannabinoids, and piperazine derivatives may cause rhabdomyolysis and acute kidney injury by increasing skeletal muscle use and metabolic demand while also causing vasoconstriction, resulting in hypoperfusion and poor heat dissipation [12, 34]. Tachycardia, agitation and chest pain can also be seen in persons exposed to clenbuterol (β2-agonist similar in chemical structure ephedrine), which is used illicitly by bodybuilders to increase muscle mass and lose weight and also used as a bulking agent for heroin [23, 24].
Clinical Mimics of Meningitis, Encephalitis, and Other Neurological Syndromes
Altered mental status is common in PWUD presenting to the emergency room and often leads to concern about possible meningitis or encephalitis. In addition to central nervous infections, healthcare providers should consider other causes of altered mental status, including stroke, movement disorders, and seizures caused by illicit drug use or withdrawal syndromes.
Cocaine and methamphetamine use are well-known causes of cerebral vasospasm and stroke, but other illicit drugs, such as marijuana, synthetic cathinones, and cathinone derivatives, have also been linked with cerebrovascular complications. Ischemic and hemorrhagic strokes have also been observed with MDMA use, possibly related to similar sympathomimetic mechanisms or high fever triggering disseminated intravascular coagulation [35]. There are also a few distinct neurological syndromes that present with specific nerve involvement and could be mistaken for strokes. Although decreasing in incidence, clostridial infection from Clostridium tetani and C. botulinum should be considered in PWUD presenting with cranial nerve involvement or muscle weakness [44, 65, 66]. There have been several outbreaks of black tar heroin–related tetanus and botulism in California, China, Saudi Arabia, and Western Europe [66–69]. Withdrawal from heroin can cause acute esotropia, or strabismus, which typically resolves after the withdrawal period is over [70]. In persons who injected crush-resistant opiates, 2 cases have been reported of opiate-associated hearing loss, thought to be secondary to cochlear ischemia [71].
Common causes of seizures include benzodiazepine and alcohol withdrawal. Less recognized causes of seizures include sympathomimetic, drugs such as synthetic cannabinoids, cathinone derivatives, and piperazine derivatives [11]. Between 1 January and 22 April 2015, the American Association for Poison Control Centers released surveillance data showing dramatic increases (229%) in the number of calls related to exposure to synthetic cannabinoids compared with the same time frame in the previous year [72, 73]. Several states health departments, including those in New York, Colorado, and Georgia, have issued alerts about symptoms that can results from ingestion, including severe agitation, hallucinations, seizures and tremors [74–76].
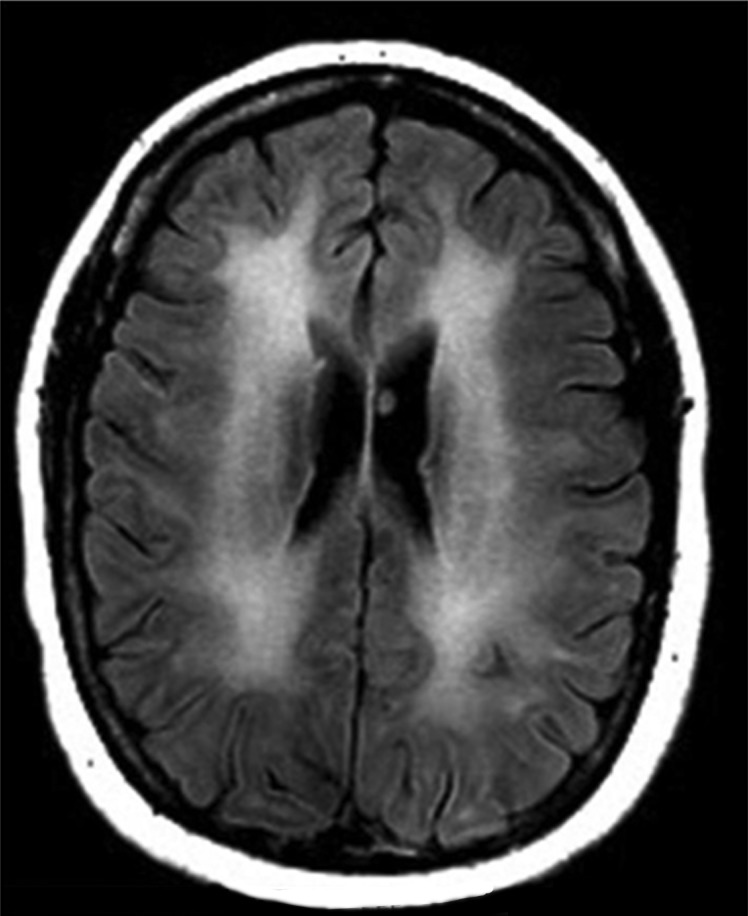
Both heroin and cocaine can be associated with leukoencephalopathy, although the imaging findings and clinical presentation may be slightly different. Leukoencephalopathy associated with heroin use is characterized by demyelination in the cerebellum or limbic system and white matter edema and is suspected to be due to oligodendrocyte mitochondrial dysfunction and apoptosis. The clinical presentation of heroin-associated leukoencephalopathy, also known as “chasing the dragon” is characterized by restlessness, apathy, cerebellar speech disturbances, ataxia, hyperactive reflexes, spasticity, tremors, and choreoathetoid movements, eventually leading to hypotonia, areflexia, and possible respiratory failure. This clinical picture is associated with a mild cerebrospinal fluid pleocytosis and cerebellar signal abnormalities at magnetic resonance imaging (Figure 5) [38]. Leukoencephalopathy from cocaine—thought to be mostly related to levamisole adulteration—has magnetic resonance imaging findings of spongiform leukoencephalopathy with white matter lesions similar to toxic-metabolic injury, primarily affecting the frontal lobe [22].
Figure 5.
Magnetic resonance image shows leukoencephalopathy from inhaled heroin use.
Clinical Mimics of Gastroenteritis
Illicit drug use can cause a variety of abdominal symptoms. Withdrawal from opiates may present like an infectious gastroenteritis with diaphoresis, nausea, vomiting, and diarrhea. Acute viral hepatitis B, C, or D can present with nausea, vomiting, and abdominal pain, and in the early stages patients may be seronegative despite high viral loads. “Body packing” or concealing illicit drugs such as narcotics or cocaine by swallowing them in bags can lead to intestinal obstruction in addition to acute overdose symptoms if the bags break. Both methamphetamine and cocaine are known to cause intestinal ischemia with subsequent infarct, necrosis, bleeding, or perforation as a result of splanchnic vasoconstriction and enhanced thrombosis [39, 40]. Chronic use of marijuana or synthetic cannabinoids is associated with cannabinoid hyperemesis syndrome, which presents with periods of nausea, vomiting, and abdominal pain, often associated with compulsive bathing or showering with hot water [41, 42].
CONCLUSIONS
It behooves all clinicians to stay up to date on complications of illicit drug use. Knowledge of emerging trends in illicit drug use can facilitate specific questions to assess both infectious and noninfectious risks and create a culturally sensitive and nonjudgmental atmosphere. In addition to addressing acute or subacute complications of drug use, encounters with PWUD represent a prime opportunity for counseling patients regarding the risks of continued drug use and making efforts to link them to treatment programs.
Notes
Acknowledgments. We thank Drs Michael Barza and Paul Trowbridge for their helpful input and for providing images, and we also thank Drs Deborah Forst and Ricky McFaline Figueroa for providing an image.
Financial support. This work was supported by the National Institutes of Health (Clinical and Translational Science Award UL1TR001064 and training grant T32 AI055412-10 and T32 AI007438-20) and Clinical Addiction Research and Education Program (R25 DA013582-14).
Potential conflicts of interest. A. G. W. receives grant support from Merck and Bristol-Myers Squibb. All other authors report no potential conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Substance Abuse and Mental Health Services Administration. Results from the 2013 National Survey on Drug Use and Health: summary of national findings. NSDUH series H-48 2014; HHS publication (SMA) 14–4863 Rockville, MD: Substance Abuse and Mental Health Services Administration, 2014. Available at: http://www.samhsa.gov/data/sites/default/files/NSDUHresultsPDFWHTML2013/Web/NSDUHresults2013.pdf. Accessed 4 September 2015. [Google Scholar]
- 2. Centers for Disease Control and Prevention. Injury prevention & control: prescription drug overdose: data overview. 2015. Available at: www.cdc.gov/drugoverdose/data/overdose/html. Accessed 2 July 2015.
- 3.Rudd RA, Paulozzi LJ, Bauer MJ et al. . Increases in heroin overdose deaths—28 states, 2010 to 2012. MMWR Morb Mortal Wkly Rep 2014; 63:849–54. [PMC free article] [PubMed] [Google Scholar]
- 4.Keyes KM, Cerda M, Brady JE, Havens JR, Galea S. Understanding the rural-urban differences in nonmedical prescription opioid use and abuse in the United States. Am J Public Health 2014; 104:e52–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cicero TJ, Kuehn BM. Driven by prescription drug abuse, heroin use increases among suburban and rural whites. JAMA 2014; 312:118–9. [DOI] [PubMed] [Google Scholar]
- 6.Gordon RJ, Lowy FD. Bacterial infections in drug users. N Engl J Med 2005; 353:1945–54. [DOI] [PubMed] [Google Scholar]
- 7.Trecki J, Gerona RR, Schwartz MD. Synthetic cannabinoid-related illnesses and deaths. N Engl J Med 2015; 373:103–7. [DOI] [PubMed] [Google Scholar]
- 8.Bonar EE, Ashrafioun L, Ilgen MA. Synthetic cannabinoid use among patients in residential substance use disorder treatment: prevalence, motives, and correlates. Drug Alcohol Depend 2014; 143:268–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aoun EG, Christopher PP, Ingraham JW. Emerging drugs of abuse: clinical and legal considerations. R I Med J (2013) 2014; 97:41–5. [PubMed] [Google Scholar]
- 10.Valente MJ, Guedes de Pinho P, de Lourdes Bastos M, Carvalho F, Carvalho M. Khat and synthetic cathinones: a review. Arch Toxicol 2014; 88:15–45. [DOI] [PubMed] [Google Scholar]
- 11.Nelson ME, Bryant SM, Aks SE. Emerging drugs of abuse. Disease-a-Month 2014; 60:110–32. [DOI] [PubMed] [Google Scholar]
- 12.Zawilska JB, Wojcieszak J. Spice/K2 drugs—more than innocent substitutes for marijuana. Int J Neuropsychopharmacol 2014; 17:509–25. [DOI] [PubMed] [Google Scholar]
- 13.Adams R, Harfenist M, Loewe S. New analogs of tetrahydrocannabinol. XIX. J Am Chem Soc 1949; 71:1624–8. [Google Scholar]
- 14.Grund JP, Latypov A, Harris M. Breaking worse: the emergence of krokodil and excessive injuries among people who inject drugs in Eurasia. Int J Drug Policy 2013; 24:265–74. [DOI] [PubMed] [Google Scholar]
- 15.Katselou M, Papoutsis I, Nikolaou P, Spiliopoulou C, Athanaselis S. A “krokodil” emerges from the murky waters of addiction: abuse trends of an old drug. Life Sci 2014; 102:81–7. [DOI] [PubMed] [Google Scholar]
- 16.Rosenbaum CD, Carreiro SP, Babu KM. Here today, gone tomorrow … and back again? a review of herbal marijuana alternatives (K2, Spice), synthetic cathinones (bath salts), kratom, Salvia divinorum, methoxetamine, and piperazines. J Med Toxicol 2012; 8:15–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zawilska JB, Wojcieszak J. Salvia divinorum: from Mazatec medicinal and hallucinogenic plant to emerging recreational drug. Hum Psychopharmacol 2013; 28:403–12. [DOI] [PubMed] [Google Scholar]
- 18.Gaertner EM, Switlyk SA. Dermatologic complications from levamisole-contaminated cocaine: a case report and review of the literature. Cutis 2014; 93:102–6. [PubMed] [Google Scholar]
- 19.Auffenberg C, Rosenthal LJ, Dresner N. Levamisole: a common cocaine adulterant with life-threatening side effects. Psychosomatics 2013; 54:590–3. [DOI] [PubMed] [Google Scholar]
- 20.Tran H, Tan D, Marnejon TP. Cutaneous vasculopathy associated with levamisole-adulterated cocaine. Clin Med Res 2013; 11:26–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ammar AT, Livak M, Witsil JC. Old drug new trick: levamisole-adulterated cocaine causing acute kidney injury. Am J Emerg Med 2015; 33:309.e3–4. [DOI] [PubMed] [Google Scholar]
- 22.González-Duarte A, Williams R. Cocaine-induced recurrent leukoencephalopathy. Neuroradiol J 2013; 26:511–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Spiller HA, James KJ, Scholzen S, Borys DJ. A descriptive study of adverse events from clenbuterol misuse and abuse for weight loss and bodybuilding. Subst Abus 2013; 34:306–12. [DOI] [PubMed] [Google Scholar]
- 24.Hoffman RS, Kirrane BM, Marcus SM. A descriptive study of an outbreak of clenbuterol-containing heroin. Ann Emerg Med 2008; 52:548–53. [DOI] [PubMed] [Google Scholar]
- 25.Manini A, Labinson RM, Kirrane B et al. . A novel neuromuscular syndrome associated with clenbuterol-tainted heroin. Clin Toxicol (Phila) 2008; 46:1088–92. [DOI] [PubMed] [Google Scholar]
- 26.Hennings C, Miller J. Illicit drugs: what dermatologists need to know. J Am Acad Dermatol 2013; 69:135–42. [DOI] [PubMed] [Google Scholar]
- 27.Tseng W, Sutter ME, Albertson TE. Stimulants and the lung: review of literature. Clin Rev Allergy Immunol 2014; 46:82–100. [DOI] [PubMed] [Google Scholar]
- 28.Mégarbane B, Chevillard L. The large spectrum of pulmonary complications following illicit drug use: features and mechanisms. Chem Biol Interact 2013; 206:444–51. [DOI] [PubMed] [Google Scholar]
- 29.Wolff AJ, O'Donnell AE. Pulmonary effects of illicit drug use. Clin Chest Med 2004; 25:203–16. [DOI] [PubMed] [Google Scholar]
- 30.Thomson BD. Medical complications following intravenous heroin. Ariz Med 1975; 32:798–801. [PubMed] [Google Scholar]
- 31.Shragg T. “Cotton fever” in narcotic addicts. JACEP 1978; 7:279–80. [DOI] [PubMed] [Google Scholar]
- 32.Harrison DW, Walls RM. “Cotton fever”: a benign febrile syndrome in intravenous drug abusers. J Emerg Med 1990; 8:135–9. [DOI] [PubMed] [Google Scholar]
- 33.Vandrey R, Dunn KE, Fry JA, Girling ER. A survey study to characterize use of Spice products (synthetic cannabinoids). Drug Alcohol Depend 2012; 120:238–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.O'Connor AD, Padilla-Jones A, Gerkin RD, Levine M. Prevalence of rhabdomyolysis in sympathomimetic toxicity: a comparison of stimulants. J Med Toxicol 2015; 11:195–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Esse K, Fossati-Bellani M, Traylor A, Martin-Schild S. Epidemic of illicit drug use, mechanisms of action/addiction and stroke as a health hazard. Brain Behav 2011; 1:44–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kimura AC, Higa JI, Levin RM, Simpson G, Vargas Y, Vugia DJ. Outbreak of necrotizing fasciitis due to Clostridium sordellii among black-tar heroin users. Clin Infect Dis 2004; 38:e87–91. [DOI] [PubMed] [Google Scholar]
- 37.Cooper JG, Spilke CE, Denton M, Jamieson S. Clostridium botulinum: an increasing complication of heroin misuse. Eur J Emerg Med 2005; 12:251–2. [DOI] [PubMed] [Google Scholar]
- 38.Bach AG, Jordan B, Wegener NA et al. . Heroin spongiform leukoencephalopathy (HSLE). Clin Neuroradiol 2012; 22:345–9. [DOI] [PubMed] [Google Scholar]
- 39.Prendergast C, Hassanein AH, Bansal V, Kobayashi L. Shock with intestinal ischemia: a rare complication of methamphetamine use. Am Surg 2014; 80:101–2. [PubMed] [Google Scholar]
- 40.Martinez-Vieira A, Camacho-Ramirez A, Diaz-Godoy A et al. . Bowel ischaemia and cocaine consumption; case study and review of the literature. Rev Esp Enferm Dig 2014; 106:354–8. [PubMed] [Google Scholar]
- 41.Galli JA, Sawaya RA, Friedenberg FK. Cannabinoid hyperemesis syndrome. Curr Drug Abuse Rev 2011; 4:241–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ukaigwe A, Karmacharya P, Donato A. A gut gone to pot: a case of cannabinoid hyperemesis syndrome due to K2, a synthetic cannabinoid. Case Rep Emerg Med 2014; 2014:167098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Furst RT, Nettey R, Wiebel W, Richmond C, Capers P. The “jelling-up” of dope: implications for the transmission of HIV among IDUs. Addict Res 1997; 4:309–20. [Google Scholar]
- 44.Gonzales Y, Tucker RD, Frazee B. View from the front lines: an emergency medicine perspective on clostridial infections in injection drug users. Anaerobe 2014; 30:108–15. [DOI] [PubMed] [Google Scholar]
- 45. Centers for Disease Control and Prevention. Update: Clostridium novyi and unexplained illness among injecting-drug users—Scotland, Ireland, and England, April-June 2000. MMWR Morb Mortal Wkly Rep 2000; 49:543–5. [PubMed] [Google Scholar]
- 46.Abrahamian FM. Update: Clostridium novyi and unexplained illness among injecting-drug users—Scotland, Ireland, and England, April-June 2000. Ann Emerg Med 2001; 37:107–9. [DOI] [PubMed] [Google Scholar]
- 47.Del Giudice P. Cutaneous complications of intravenous drug abuse. Br J Dermatol 2004; 150:1–10. [DOI] [PubMed] [Google Scholar]
- 48.Kalka-Moll WM, Aurbach U, Schaumann R, Schwarz R, Seifert H. Wound botulism in injection drug users. Emerg Infect Dis 2007; 13:942–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Berger T, Kassirer M, Aran AA. Injectional anthrax—new presentation of an old disease. Euro Surveill 2014; 19:20877. [DOI] [PubMed] [Google Scholar]
- 50.Abbara A, Brooks T, Taylor GP et al. . Lessons for control of heroin-associated anthrax in Europe from 2009–2010 outbreak case studies, London, UK. Emerg Infect Dis 2014; 20:1115–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Korantzopoulos P, Liu T, Papaioannides D, Li G, Goudevenos JA. Atrial fibrillation and marijuana smoking. Int J Clin Pract 2008; 62:308–13. [DOI] [PubMed] [Google Scholar]
- 52.Robertson CH Jr, Reynolds RC, Wilson JE III. Pulmonary hypertension and foreign body granulomas in intravenous drug abusers: documentation by cardiac catheterization and lung biopsy. Am J Med 1976; 61:657–64. [DOI] [PubMed] [Google Scholar]
- 53.Chin KM, Channick RN, Rubin LJ. IS methamphetamine use associated with idiopathic pulmonary arterial hypertension? Chest 2006; 130:1657–63. [DOI] [PubMed] [Google Scholar]
- 54.Pierrotti LC, Baddour LM. Fungal endocarditis, 1995–2000. Chest 2002; 122:302–10. [DOI] [PubMed] [Google Scholar]
- 55.Leen CL, Brettle RP. Fungal infections in drug users. J Antimicrob Chemother 1991; 28(suppl A):83–96. [DOI] [PubMed] [Google Scholar]
- 56.Swisher LA, Roberts JR, Glynn MJ. Needle licker's osteomyelitis. Am J Emerg Med 1994; 12:343–6. [DOI] [PubMed] [Google Scholar]
- 57.Bisbe J, Miro JM, Latorre X et al. . Disseminated candidiasis in addicts who use brown heroin: report of 83 cases and review. Clin Infect Dis 1992; 15:910–23. [DOI] [PubMed] [Google Scholar]
- 58.Gubler J, Huber-Schneider C, Gruner E, Altwegg M. An outbreak of nontoxigenic Corynebacterium diphtheriae infection: single bacterial clone causing invasive infection among Swiss drug users. Clin Infect Dis 1998; 27:1295–8. [DOI] [PubMed] [Google Scholar]
- 59.Ball SC, Sepkowitz K. Infection due to Bacillus cereus in an injection drug user with AIDS: bacteremia without morbidity. Clin Infect Dis 1994; 19:216–7. [DOI] [PubMed] [Google Scholar]
- 60.Shamsuddin D, Tuazon CU, Levy C, Curtin J. Bacillus cereus panophthalmitis: source of the organism. Rev Infect Dis 1982; 4:97–103. [DOI] [PubMed] [Google Scholar]
- 61.Juurlink DN, Borczyk A, Simor AE. Native valve endocarditis due to Corynebacterium striatum. Eur J Clin Microbiol Infect Dis 1996; 15:963–5. [DOI] [PubMed] [Google Scholar]
- 62.Verani DA, Carretto E, Bono L, Moggio G, Marone P. Lactobacillus casei endocarditis in an intravenous heroin drug addict: a case report. Funct Neurol 1993; 8:355–7. [PubMed] [Google Scholar]
- 63.Ferguson R, Feeney C, Chirurgi VA. Enterobacter agglomerans—associated cotton fever. Arch Intern Med 1993; 153:2381–2. [PubMed] [Google Scholar]
- 64.Torka P, Gill S. Cotton fever: an evanescent process mimicking sepsis in an intravenous drug abuser. J Emerg Med 2013; 44:e385–7. [DOI] [PubMed] [Google Scholar]
- 65.Rodolico C, Barca E, Fenicia L, Anniballi F, Sinardi AU, Girlanda P. Wound botulism in drug users: a still underestimated diagnosis. Neurol Sci 2010; 31:825–7. [DOI] [PubMed] [Google Scholar]
- 66. Centers for Disease Control and Prevention. Wound botulism—California, 1995. MMWR Morb Mortal Wkly Rep 1995; 44:889–92. [PubMed] [Google Scholar]
- 67.Sun KO. Outbreak of tetanus among heroin addicts in Hong Kong. J R Soc Med 1994; 87:494–5. [PMC free article] [PubMed] [Google Scholar]
- 68.Iqbal N. Tetanus in i.v. heroin users. Ann Saudi Med 2001; 21:296–9. [DOI] [PubMed] [Google Scholar]
- 69.Galldiks N, Nolden-Hoverath S, Kosinski CM et al. . Rapid geographical clustering of wound botulism in Germany after subcutaneous and intramuscular injection of heroin. Neurocrit Care 2007; 6:30–4. [DOI] [PubMed] [Google Scholar]
- 70.Shiferaw B, Bekele E, Syed S et al. . A case report of acute esotropia in a young woman following heroin withdrawal. Case Rep Med 2015; 2015:740710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.MacDonald LE, Onsrud JE, Mullins-Hodgin R. Acute sensorineural hearing loss after abuse of an inhaled, crushed oxymorphone extended-release tablet. Pharmacotherapy 2015; 35:e118–21. [DOI] [PubMed] [Google Scholar]
- 72. American Association of Poison Control Centers. American Association of Poison Control Centers issues warning about reemerging synthetic drugs, 2015. Available at: https://aapcc.s3.amazonaws.com/pdfs/releases/AAPCC_Synthetic_Cann_Press_Release_oElmCXq.pdf. Accessed 26 August 2015.
- 73.Law R, Schier J, Martin C, Chang A, Wolkin A. Notes from the field: increase in reported adverse health effects related to synthetic cannabinoid use—United States, January-May 2015. MMWR Morb Mortal Wkly Rep 2015; 64:618–9. [PMC free article] [PubMed] [Google Scholar]
- 74. New York City Department of Health and Mental Hygiene. Increase in synthetic cannabinoid (marijuana)-related adverse events and emergency department visits, New York City. 2015 advisory 6. Available at: https://s3.amazonaws.com/enp-network-assets/production/attachments/46861/original/Synthetic_cannabinoids-HAN-advisory_April_2015.pdf?2015. Accessed 26 August 2015.
- 75. Centers for Disease Control and Prevention. Notes from the field: severe illness associated with reported use of synthetic marijuana—Colorado, August-September 2013. MMWR Morb Mortal Wkly Rep 2013; 62:1016–7. [PMC free article] [PubMed] [Google Scholar]
- 76. Centers for Disease Control and Prevention. Notes from the field: severe illness associated with synthetic cannabinoid use—Brunswick, Georgia, 2013. MMWR Morb Mortal Wkly Rep 2013; 62:939. [PMC free article] [PubMed] [Google Scholar]