Abstract
Severe acute basilar artery occlusion (BAO) has a high mortality rate but as yet no effective treatment has been developed. This study aimed to evaluate the feasibility and safety of combined mechanical thrombectomy, intra-arterial thrombolysis, and emergent stent placement for patients with severe acute BAO. Eighteen patients who were unconscious after confirmed onset of BAO and who were given arterial interventional treatment from March 2011 to June 2013 at our department were included in this study. The mean age was 59.56 years (range: 31–76 years) and patients were in a critical physical condition upon admission, and had a mean National Institutes of Health Stroke Scale (NIHSS) score of 25.94 (range: 18–35). All patients were treated with mechanical thrombectomy, 10 of whom received mechanical thrombectomy only. Of the others, eight were also treated with intra-arterial thrombolysis, three were treated with emergent stent placement, and 17 were treated with recanalization with an achieved recanalized rate of 94.4%. The average number of passes through the stent was 1.5 (range: 1–3) and five patients died (27.8%). Thirteen patients survived, and the mean NIHSS score was 6.54 (range: 0–16). Seven patients showed a modified Rankin Scale score ≤2, and the rate of good prognoses was 38.9%. In the treatment of patients with severe acute BAO, intra-arterial mechanical thrombectomy combined with thrombolysis or stent placement are effective strategies to restore blood flow and preserve life, and these strategies have a low incidence of complications.
Keywords: Acute basilar artery occlusion, Emergent stent placement, Intra-arterial thrombolysis, Thrombectomy
1. Introduction
Acute basilar artery occlusion (BAO) is a common condition that has a higher mortality rate than hemisphere infarction. Overall, 80–90% of patients who have acute BAO die due to lack of effective treatment [1]. BAO has a high mortality rate, high morbidity rate, and is a severe illness with a poor prognosis [2].
The early recanalization of occluded vessels in acute BAO is important to improve the clinical outcomes and reduce mortality. Intravenous or intra-arterial thrombolysis has been confirmed to reduce mortality and improve the therapeutic effect in acute stroke, but the effect on large vessel occlusion is poor [3–5]. Mechanical thrombectomy is an acceptable management technique for acute BAO with a longer therapeutic window and a higher recanalization rate [6–7]. Emergent stent placement remains controversial, but some studies have reported an improved recanalization rate, and low rates of complications and restenosis [5].
In the present study, we retrospectively analyzed 18 patients who lost consciousness after the onset of confirmed BAO and who were treated with mechanical thrombectomy or combined methods from March 2011 to June 2013 in our department. We analyzed the clinical features, treatment procedures, prognostic results, and technical feasibility of these treatment methods.
2. Methods
2.1. Patients
We reviewed patients with acute cerebral infarction who underwent intra-arterial treatment from March 2011 to June 2013 in our department. We selected patients from those who lost consciousness after the onset of acute cerebral infarction and those with confirmed acute BAO for analysis.
All patients were examined by brain CT scan on arrival to exclude intracranial hemorrhage.
The inclusion criteria were as follows: (1) a National Institutes of Health Stroke Scale (NIHSS) score ≥8; (2) arrival at the hospital within 8 hours of symptom onset; (3) age ≤80 years; (4) detection of BAO on transcranial Doppler ultrasonography and/or MRI; and (5) signed informed consent from each patient or family member prior to treatment.
Exclusion criteria were as follows: (1) a large brainstem infarction (more than half of the area of the brainstem on at least one axial CT scan and/or MRI); (2) a recent history (within 4 weeks) or presence of intracranial hemorrhage or hemorrhagic infarction; (3) a long duration following onset (≥12 hours); (4) a significant improvement in clinical symptoms before thrombolytic therapy; (5) systemic active bleeding or a platelet count <60 × 109/L; or (6) severe cardiac dysfunction, diabetic hemorrhagic retinopathy, or liver or kidney dysfunction.
2.2. Endovascular procedure
All of the procedures were performed under local anesthesia using a transfemoral approach, and a 6 French guide catheter was placed in the proximal vertebral artery. To prevent the occurrence of a new thromboembolic event during the procedure, a mixture of 2000 international units heparin and 0.9% normal saline (1000 mL) were administered continuously through the guiding catheter. The microcatheter and microwire (ev3, Plymouth, MN, USA) were introduced into the target vessel. The Solitaire AB stent (ev3) was introduced into the microcatheter so that the device could be deployed to completely cover the occluded segment. Deployment of the stent was maintained for at least 3 minutes before retrieval. The microcatheter and stent were gently withdrawn, the guiding catheter was pulled out of the sheath with the stent in it, and the flushing was stopped. At the same time, an assistant applied negative pressure using a 50 cc syringe through the guiding catheter to prevent the development of new embolism by lost clots (Fig. 1).
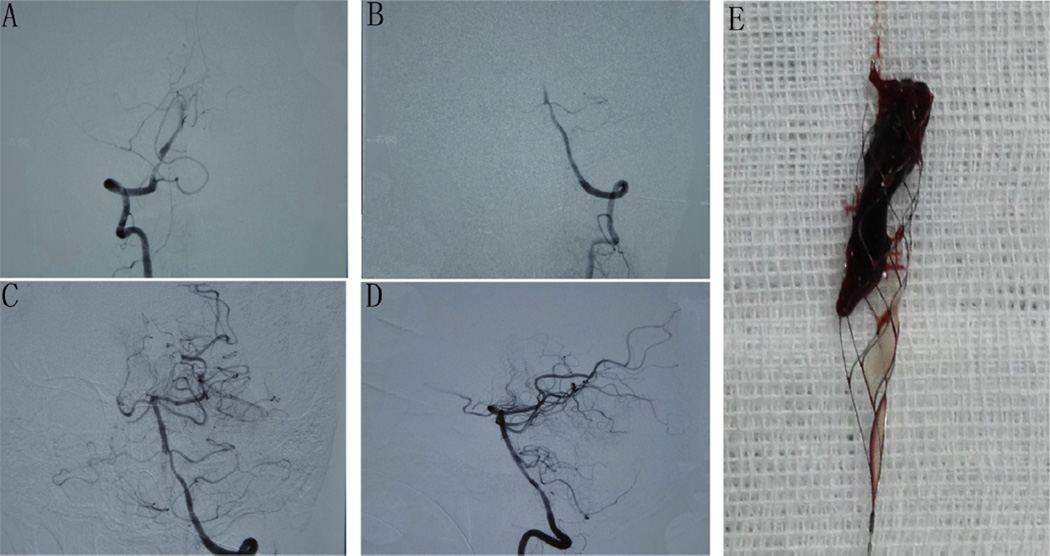
Fig. 1.
Digital subtraction angiography of basilar artery occlusion before and after treatment with mechanical thrombectomy. (A) Anteroposterior and (B) lateral views before treatment showing basilar artery occlusion and underfilled distal arteries. (C) Anteroposterior and (D) lateral views after treatment showing recanalization of the basilar artery, bilateral posterior cerebral artery, superior cerebellar artery, and anterior inferior cerebellar. (E) Photograph of the stent and thrombosis.
The angiographic runs were repeated to assess revascularization, distal emboli, and vessel injury. When the recanalization of occluded vessels was unsatisfactory, mechanical thrombectomy was carried out again. When obvious stenosis was noted, permanent stent (ev3) deployment and balloon (Boston Scientific Corporation, Natick, MA, USA) angioplasty were considered.
2.3. Outcome measures
The NIHSS score was assessed on admission and at discharge by a neurologist. Assessment of the modified Rankin Scale (mRS) was performed 3 months after treatment. A mRS of 0 to 2 was defined as a good neurological outcome, and a mRS of 3 to 6 was defined as a poor outcome.
2.4. Statistical analysis
Values are presented as the mean ± standard deviation. Statistical analysis was performed using the Statistical Package for the Social Sciences version 16.0 (SPSS, Chicago, IL, USA).
3. Results
Eighteen acute BAO patients (12 men and six women) who were unconscious and in a critical condition upon admission to our department between March 2011 and June 2013 were included in the present study. Patient characteristics and clinical results are presented in Table 1. The patient age was 59.56 ± 10.35 years (range: 31–76 years). Ten patients with hypertension, five with diabetes, and seven with heart disease were reported. Seven patients with sudden unconsciousness onset, six with dizziness followed by unconsciousness, and five with dizziness and limb weakness followed by unconsciousness were observed. The mean NIHSS score was 27.08 (range: 20–35) at admission. Nine patients were treated under local anesthesia, and three patients were changed to general anesthesia because of dysphoria.
Table 1.
Characteristics of the basilar occlusion patients
| Patient | Age (sex) | Baseline NIHSS | rtPA dosage (mg) | ESP | PTR (hours) | STP (hours) | NIHSS at discharge | mRS at 3 months |
|---|---|---|---|---|---|---|---|---|
| 1 | 67 (M) | 20 | None | No | 2.2 | 2 | 12 | 4 |
| 2 | 70 (F) | 30 | None | No | 4.5 | 3.4 | Dead | 6 |
| 3 | 68 (M) | 35 | 20 | Yes | 3.8 | 2.7 | Dead | 6 |
| 4 | 76 (M) | 22 | 20 | No | 1.2 | 3.2 | 10 | 3 |
| 5 | 54 (F) | 28 | 20 | No | 4.3 | 4.3 | Dead | 6 |
| 6 | 56 (M) | 26 | 20 | No | 2.4 | 4.1 | 4 | 1 |
| 7 | 56 (F) | 30 | 10 | No | 1.8 | 2.4 | 16 | 5 |
| 8 | 46 (M) | 22 | None | Yes | 2 | 3 | 0 | 0 |
| 9 | 57 (F) | 30 | 13 | No | 2.7 | 4.2 | 8 | 3 |
| 10 | 58 (M) | 24 | 20 | No | 3.4 | 2 | 3 | 2 |
| 11 | 31 (M) | 32 | 30 | Yes | 4.5 | 2.8 | Dead | 6 |
| 12 | 56 (M) | 25 | None | No | 1.5 | 2.2 | 2 | 1 |
| 13 | 55 (F) | 18 | None | No | 2 | 2.6 | 4 | 2 |
| 14 | 65 (M) | 22 | None | No | 1.6 | 3.5 | 6 | 4 |
| 15 | 71 (F) | 20 | None | No | 3.2 | 5.0 | Dead | 6 |
| 16 | 60 (M) | 25 | None | No | 3.0 | 4.2 | 7 | 3 |
| 17 | 67 (M) | 30 | None | No | 2.8 | 3.2 | 5 | 2 |
| 18 | 59 (M) | 28 | None | No | 2.4 | 3.6 | 8 | 3 |
ESP = emergent stent placement, F = female, M = male, mRS = modified Rankin scale, NIHSS = National Institutes of Heath Stroke Scale, PTR = time from femoral puncture to recanalization, rtPA = recombinant tissue plasminogen activator, STP = time from onset of symptoms to groin puncture.
All 18 patients were treated with mechanical thrombectomy, 10 of whom were treated with mechanical thrombectomy only. Of the others, eight patients were also treated with intra-arterial thrombolysis, three patients were treated with emergent stent placement, and 17 patients achieved recanalization with a recanalization rate of 94.4%. The average number of passes through the stent was 1.5 (range: 1–3). Five patients died (27.8%), and the mean NIHSS score was 6.54 (range: 0–16). Seven patients had a mRS of ≤2. One patient developed subarachnoid hemorrhage after surgery and died.
The time from the onset of symptoms to femoral puncture was 3.24 ± 0.873 hours. The time from femoral artery puncture to flow restoration was 2.74 ± 1.03 hours. Vasospasm occurred in one patient during surgery, and papaverine saline solution was perfused through the catheter immediately. The vasospasm was controlled, and this patient obtained a good result.
4. Discussion
Acute BAO is an infrequent type of acute stroke, often associated with high morbidity and high mortality even when treated with antiplatelet agents and systemic anticoagulation [1,2]. There is a strong association between revascularization and prognosis [9,10]. According to a systematic analysis by Lindsberg et al. [8], the likelihood of survival is only 2% without revascularization; hence, the recanalization of BAO is by far the best way to preserve life.
With intra-arterial treatment, we found that acute occlusion mostly occurs because of atherosclerosis, and complete recanalization is difficult to achieve through intra-arterial thrombolysis alone. The present study shows that mechanical thrombectomy with a self-expanding retrievable intracranial Solitaire AB stent is safe and effective [11–13]. We obtained a good treatment result using a Solitaire AB stent to treat BAO: 17 of 18 patients achieved revascularization, and the NIHSS score improved to >10 in 12 of 13 surviving patients. Roth et al. [14] reported a recanalization rate using Solitaire thrombectomy of 90.9%, an improvement of the NIHSS score to >10 in 63.6% of patients at the time of discharge, and a 90 day mRS ≤2 in 50% of patients. Patients were more likely to achieve vascular recanalization if they underwent combined atrial fibrillation and Solitaire AB stent thrombectomy.
In cases of obvious vascular stenosis in which recanalization could not be achieved by thrombectomy, the emergent stent placement method was used as an alternative. However, we tried to avoid emergency stenting in our treatment process, as it may increase the risk of hemorrhage and occlusions [5,16]. In the present study, three patients were treated with emergent stent placement, two of whom died and one of whom achieved a good outcome. It may be that these patients who needed emergent stent placement were all in a serious condition, and their vessels were already in poor condition. It is critical to perform follow-up treatment after stent placement, including anticoagulant and anti-platelet treatment. Emergent stent placement remains controversial and needs to be verified through further investigation.
Intracranial hemorrhage is a serious complication of intra-arterial treatment. The MERCI trial reported that 9.8% of patients developed symptomatic intracranial hemorrhage [17,18]. Bae et al. [15] reported only one patient with non-symptomatic intracranial hemorrhage from 40 patients undergoing thrombectomy. The present study focused on BAO, and no surgical errors or intracranial hemorrhages were observed during surgery, although one patient developed subarachnoid hemorrhage after surgery, and another developed vasospasm during surgery (8.3%), but this improved with papaverine saline solution.
Digital subtraction angiography was performed under local anesthesia. The subarachnoid hemorrhage case might have been due to high blood pressure associated with patient dysphoria, suggesting that general anesthesia was necessary.
Our results indicate that self-expanding Solitaire stents used for mechanical thrombectomy are safe and effective for the treatment of severe acute BAO patients. Combining thrombolysis and stent placement can be an effective strategy to restore blood flow and save the patient’s life.
Acknowledgements
We thank all the workers in the department of Digital Subtraction Angiography for their excellent technical support. This work was supported by grants from the Emerging Project Committee of Science and Technology of Tanggu District of Tianjin (2012XQ15-07).
Footnotes
Conflicts of Interest/Disclosures
The authors declare that they have no financial or other conflicts of interest in relation to this research and its publication.
References
- 1.Mortimer AM, Bradley M, Renowden SA. Endovascular therapy for acute basilar artery occlusion: a review of the literature. J Neurointerv Surg. 2012;4:266–273. doi: 10.1136/neurintsurg-2011-010090. [DOI] [PubMed] [Google Scholar]
- 2.Hacke W, Zeumer H, Ferbert A, et al. Intra-arterial thrombolytic therapy improves outcome in patients with acute vertebrobasilar occlusive disease. Stroke. 1988;19:1216–1222. doi: 10.1161/01.str.19.10.1216. [DOI] [PubMed] [Google Scholar]
- 3.Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359:1317–1329. doi: 10.1056/NEJMoa0804656. [DOI] [PubMed] [Google Scholar]
- 4.Schonewille WJ, Wijman CA, Michel P, et al. Treatment and outcomes of acute basilar artery occlusion in the Basilar Artery International Cooperation Study (BASICS): a prospective registry study. Lancet Neurol. 2009;8:724–730. doi: 10.1016/S1474-4422(09)70173-5. [DOI] [PubMed] [Google Scholar]
- 5.Shi M, Wang S, Zhu H, et al. Emergent stent placement following intra-arterial thrombolysis for the treatment of acute basilar artery occlusion. J Clin Neurosci. 2012;19:152–154. doi: 10.1016/j.jocn.2011.03.040. [DOI] [PubMed] [Google Scholar]
- 6.Nogueira RG, Smith WS MERCI and Multi MERCI Writing Committee. Safety and efficacy of endovascular thrombectomy in patients with abnormal hemostasis: pooled analysis of the MERCI and multi MERCI trials. Stroke. 2009;40:516–522. doi: 10.1161/STROKEAHA.108.525089. [DOI] [PubMed] [Google Scholar]
- 7.Rha JH, Saver JL. The impact of recanalization on ischemic stroke outcome: a meta-analysis. Stroke. 2007;38:967–973. doi: 10.1161/01.STR.0000258112.14918.24. [DOI] [PubMed] [Google Scholar]
- 8.Lindsberg PJ, Mattle HP. Therapy of basilar artery occlusion: a systematic analysis comparing intra-arterial and intravenous thrombolysis. Stroke. 2006;37:922–928. doi: 10.1161/01.STR.0000202582.29510.6b. [DOI] [PubMed] [Google Scholar]
- 9.Schulte-Altedorneburg G, Hamann GF, Mull M, et al. Outcome of acute vertebrobasilar occlusions treated with intra-arterial fibrinolysis in 180 patients. AJNR Am J Neuroradiol. 2006;27:2042–2047. [PMC free article] [PubMed] [Google Scholar]
- 10.Smith WS. Intra-arterial thrombolytic therapy for acute basilar occlusion: pro. Stroke. 2007;38:701–703. doi: 10.1161/01.STR.0000247897.33267.42. [DOI] [PubMed] [Google Scholar]
- 11.Bae GS, Kwon HJ, Kang CW, et al. Mechanical thrombectomy using a solitaire stent in acute ischemic stroke; initial experience in 40 patients. J Cerebrovasc Endovasc Neurosurg. 2012;14:164–169. doi: 10.7461/jcen.2012.14.3.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Menon BK, Kochar P, Ah-Seng A, et al. Initial experience with a self-expanding retrievable stent for recanalization of large vessel occlusions in acute ischemic stroke. Neuroradiology. 2012;54:147–154. doi: 10.1007/s00234-010-0835-x. [DOI] [PubMed] [Google Scholar]
- 13.Park H, Hwang GJ, Jin SC, et al. A retrieval thrombectomy technique with the Solitaire stent in a large cerebral artery occlusion. Acta Neurochir (Wien) 2011;153:1625–1631. doi: 10.1007/s00701-011-0999-0. [DOI] [PubMed] [Google Scholar]
- 14.Roth C, Papanagiotou P, Behnke S, et al. Stent-assisted mechanical recanalization for treatment of acute intracerebral artery occlusions. Stroke. 2010;41:2559–2567. doi: 10.1161/STROKEAHA.110.592071. [DOI] [PubMed] [Google Scholar]
- 15.Bae GS, Kwon HJ, Kang CW, et al. Mechanical thrombectomy using a solitaire stent in acute ischemic stroke; initial experience in 40 patients. J Cerebrovasc Endovasc Neurosurg. 2012;14:164–169. doi: 10.7461/jcen.2012.14.3.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Levy EI, Hanel RA, Boulos AS, et al. Comparison of periprocedure complications resulting from direct stent placement compared with those due to conventional and staged stent placement in the basilar artery. J Neurosurg. 2003;99:653–660. doi: 10.3171/jns.2003.99.4.0653. [DOI] [PubMed] [Google Scholar]
- 17.Smith WS, Sung G, Saver J, et al. Mechanical thrombectomy for acute ischemic stroke: final results of the Multi MERCI trial. Stroke. 2008;39:1205–1212. doi: 10.1161/STROKEAHA.107.497115. [DOI] [PubMed] [Google Scholar]
- 18.Penumbra Pivotal Stroke Trial Investigators. The penumbra pivotal stroke trial: safety and effectiveness of a new generation of mechanical devices for clot removal in intracranial large vessel occlusive disease. Stroke. 2009;40:2761–2768. doi: 10.1161/STROKEAHA.108.544957. [DOI] [PubMed] [Google Scholar]