Abstract
BACKGROUND AND OBJECTIVES:
Opportunities to improve health care quality and contain spending may differ between high and low resource users. This study’s objectives were to assess health care and spending among children with Medicaid insurance by their resource use.
METHODS:
Retrospective cross-sectional analysis of 2012 Medicaid health administrative data from 10 states of children ages 11 months to 18 years. Subjects were categorized into 4 spending groups, each representing ∼25% of total spending: the least expensive 80% of children (n = 2 868 267), the next 15% expensive (n = 537 800), the next 4% expensive (n = 143 413), and the top 1% (n = 35 853). We compared per-member-per-month (PMPM) spending across the groups using the Kruskal–Wallis test.
RESULTS:
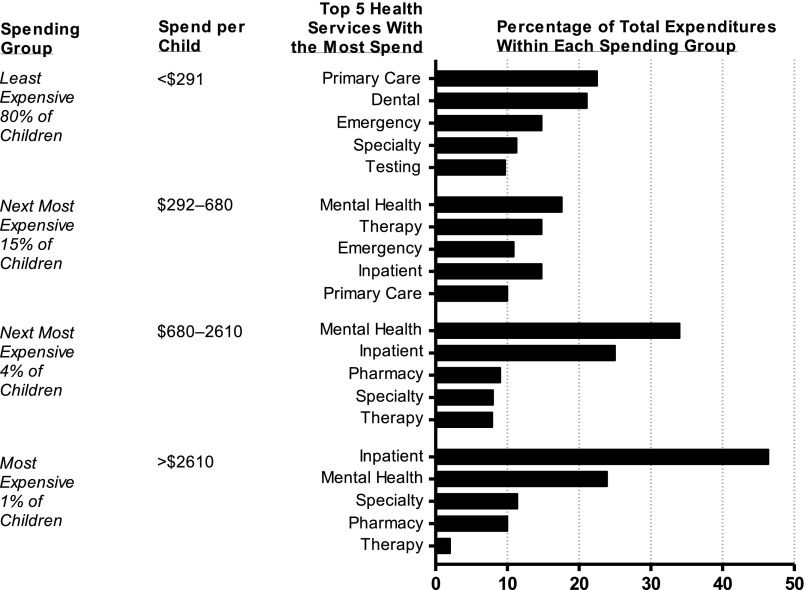
PMPM spending was $68 (least expensive 80%), $349 (next 15%), $1200 (next 4%), and $6738 (top 1%). Between the least and most expensive groups, percentages of total spending were higher for inpatient (<1% vs 46%) and mental health (7% vs 24%) but lower for emergency (15% vs 1%) and primary (23% vs 1%) care (all Ps < .001). From the least to most expensive groups, increases in PMPM spending were smallest for primary care (from $15 to $33) and much larger for inpatient ($0.28 to $3129), mental health ($4 to $1609), specialty care ($8 to $768), and pharmacy ($4 to $699).
CONCLUSIONS:
As resource use increases in children with Medicaid, spending rises unevenly across health services: Spending on primary care rises modestly compared with other health services. Future studies should assess whether more spending on primary care leads to better quality and cost containment for high resource users.
What’s Known on This Subject:
Most pediatric health care costs are concentrated in a small group of children with high resource use. Little is known about how types of health services experienced by these children compare with children who have lower resource use.
What This Study Adds:
Low and high resource users with Medicaid are similar in the amount of spending on primary and dental care and dramatically differ in spending on hospital, mental health, specialty, and pharmacy care.
Health care spending is projected to account for one-fifth of the United States’ gross national product by the beginning of the next decade.1 Spending is distributed unevenly across patients, with more dollars spent on patients with chronic and complex medical problems.2 The patients with the highest spending are commonly called high resource users (HRUs). HRUs are increasingly targeted for enrollment in initiatives to improve their health care and contain their costs.3 This is because HRUs are perceived to experience high rates of preventable emergency department (ED) visits and hospitalizations.4,5 Reducing preventable encounters is thought to be best achieved by improving outpatient care management and coordination.6
Among children, the top 1% most expensive patients account for one-third of pediatric health care spending.7,8 Child HRUs are a heterogeneous group with many rare, complex chronic conditions9,10 and a variety of intensive, expensive health care needs.11 Hospital care accounts for nearly 80% of health care spending for these children.8,12 Many child HRUs experience frequent ED visits and recurrent inpatient admissions with high readmission rates.10,13,14
Reductions in hospital and ED use have been reported with high-intensity outpatient care management for subgroups of HRU children.15–18 Despite this finding, 40% of children with complex chronic conditions may not have an annual primary care visit.19
To help inform specific outpatient interventions to achieve quality improvement and cost containment for child HRUs, answers are needed to questions such as, “How does primary care use for child HRUs compare with that of children with lower resource use?” and “How does the distribution of spending compare between high and low resource use children?” Medicaid programs, as the largest insurers of children in the United States, may have particular motivation to better understand child health care spending as they align financial incentives with outpatient case management targeting child HRUs.20–22 The objectives of this study are to describe the clinical attributes and the health care spending and utilization of children with HRU who use Medicaid and to compare the distribution of spending and health service utilization across children with high and low resource use.
Methods
Study Design, Patients, and Setting
This study is a retrospective, cross-sectional analysis of the 2012 Truven MarketScan Medicaid Database. The MarketScan Medicaid Database contains complete paid medical and prescription drug claims from 10 states, including fee-for-service (FFS) and Medicaid managed care (MMC) plans. Data validity and integrity are maintained by Truven, with audits conducted to assess and remove invalid diagnosis and procedure codes. This study included 3 585 333 children ages 0 to 18 years enrolled continuously for ≥11 months in Medicaid in 2012. Study subjects resided in 10 deidentified states representing all geographic regions of the United States. Children qualified for Medicaid based on low family income or the child having a disability; accordingly, children in Medicaid tend to have higher rates of chronic conditions. Because the MarketScan Medicaid Database contains exclusively deidentified data, this study was exempt from review by the Institutional Review Board at the University of Arkansas for Medical Sciences.
Outcome Measures
The main outcomes were health care spending and utilization. We assessed the outcomes overall (ie, the total across all health services) and by 14 specific health services (listed alphabetically): dental, durable medical equipment, ED, facility (ie, payment made to a health care facility), home health, hospice, inpatient (exclusive of mental health), mental health (all professional and facility claims originating from mental health and substance abuse providers across the care continuum), outpatient laboratory testing, pharmacy (outpatient only, exclusive of mental health), primary care, specialty care (including all outpatient specialty care), therapy (including physical, occupational, and all outpatient therapies), and transport.
Spending was reported for each health service as the total gross payment. Utilization was described as the proportion of patients using a specific health service, the frequency (eg, the number of hospitalizations for each patient) of use, and the duration (eg, the number of days spent in the hospital) of use.
Main Independent Variable
Based on existing literature and the Pareto principle,12,23 we ranked each child in ascending order of total Medicaid spending and then divided the cohort into 4 spending groups: the least expensive 80% of children (n = 2 868 267), the next 15% more expensive (n = 537 800), the next 4% more expensive (n = 143 413), and the top 1% most expensive (n = 35 853). Each group accounted for ∼25% of total spending. Groups 3 and 4 together are the 5% most expensive children with Medicaid. Group 4, the most expensive 1% of patients, is labeled HRU.
Demographic and Clinical Characteristics of the Children
Demographic characteristics included age, gender, race or ethnicity (white, non-Hispanic; black, non-Hispanic; Hispanic; and other), and type of Medicaid plan (FFS vs MMC). MMCs included health maintenance organizations and full or partial capitated plans. Clinical characteristics included the presence of a chronic condition, technology assistance, and a disability. To identify chronic conditions, we used the Agency for Healthcare Research and Quality’s Chronic Condition Indicator classification system,24–26 which dichotomizes ∼14 000 International Classification of Diseases, Ninth Revision diagnosis codes into chronic or nonchronic conditions and aggregates chronic conditions into 1 of 18 mutually exclusive clinical groups. The Chronic Condition Indicator defines chronic conditions as those lasting ≥12 months that place limitations on self-care, independent living, and social interaction or are associated with the need for ongoing intervention with medical products, services, and special equipment. To identify technology assistance, we used diagnosis codes that indicated the presence of a medical device (eg, gastrostomy, tracheostomy) used to maintain a child’s health.8,27 Disability was identified by the response of “blind/disabled individual” for Medicaid eligibility.
Statistical Analyses
We summarized categorical variables by using frequencies and percentages, and we summarized continuous variables with medians and interquartile ranges (IQRs). We compared the distribution of categorical variables across spending categories by using the χ2 test. For continuous variables, we used the nonparametric Kruskal–Wallis test because the data were not normally distributed. Per-member-per-month (PMPM) spending was calculated by summing the specific spending of a population over a year, dividing by 12, then dividing by the number of enrollees in the population. We performed analyses on enrollees from all 10 states in the database by using SAS version 9.3 (SAS Institute, Inc, Cary, NC).
Results
Study Population Characteristics
The 3 585 333 children with Medicaid in the study (Table 1) had a median age of 9 years (IQR 4, 14). Just over half (50.3%, n = 1 803 935) were female, and 42.6% (n = 1 528 901) were white, non-Hispanic. With respect to chronic conditions, 52.5% (n = 1 882 348) had ≥1 chronic condition, 13.8% (n = 494 396) had 2 chronic conditions, and 8.4% (n = 300 407) had ≥3 chronic conditions. Medical technology assisted 0.5% (n = 16 347) of the children, and 5.5% (n = 197 929) were eligible for Medicaid because of a disability. Of the children, 59.8% were enrolled in an MMC program. When compared with children in FFS programs, children in MMC programs had clinical attributes suggestive of lower medical complexity (Supplemental Table 4).
TABLE 1.
Demographic and Clinical Characteristics of Children in Medicaid by Spending Group
| Characteristic | Overall Cohort | Spending Groups of Children in Medicaida | |||
|---|---|---|---|---|---|
| Least Expensive 80% of Children (24.4% of Spending) | Most Expensive 20% of Children | ||||
| Next 15% (23.6% of Spending) | Next 4% (21.6% of Spending) | Top 1% (30.4% of Spending) | |||
| Overall N | 3 585 333 | 2 868 267 | 537 800 | 143 413 | 35 853 |
| Age, median y (IQR) | 9 (4, 14) | 9 (4, 13) | 8 (3, 14) | 12 (6, 17) | 13 (7, 17) |
| Race or ethnicity, N (%) | |||||
| White, non-Hispanic | 1 528 901 (42.6) | 1 180 722 (41.2) | 263 469 (49) | 68 315 (47.6) | 16 395 (45.7) |
| Black, non-Hispanic | 1 233 071 (34.4) | 1 016 030 (35.4) | 162 079 (30.1) | 44 800 (31.2) | 10 162 (28.3) |
| Hispanic | 358 389 (10.0) | 299 857 (10.5) | 48 370 (9.0) | 8439 (5.9) | 1723 (4.8) |
| Other | 464 972 (13.0) | 371 658 (13) | 63 882 (11.9) | 21 859 (15.2) | 7573 (21.1) |
| Male, N (%) | 1 781 398 (49.7) | 1 411 557 (49.2) | 276 233 (51.4) | 72 216 (50.4) | 21 392 (59.7) |
| Number of chronic conditions, N (%) | |||||
| 0 | 1 702 985 (47.5) | 1 621 354 (56.5) | 73 849 (13.7) | 7296 (5.1) | 486 (1.4) |
| 1 | 1 087 545 (30.3) | 853 438 (29.8) | 187 582 (34.9) | 40 298 (28.1) | 6227 (17.4) |
| 2 | 494 396 (13.8) | 296 525 (10.3) | 153 128 (28.5) | 37 734 (26.3) | 7009 (19.5) |
| ≥3 | 300 407 (8.4) | 96 950 (3.4) | 123 241 (22.9) | 58 085 (40.5) | 22 131 (61.7) |
| Assisted with medical technology, N (%) | 16 347 (0.5) | 1046 (0.1) | 2664 (0.5) | 4869 (3.4) | 7768 (21.7) |
| Eligible for Medicaid because of a disability, N (%) | 197 929 (5.5) | 90 470 (3.2) | 50 055 (9.3) | 37 876 (26.4) | 19 528 (54.5) |
| Medicaid managed care, N (%) | 2 143 423 (59.8) | 1 714 739 (59.8) | 321 513 (59.8) | 85 737 (59.8) | 21 434 (59.8) |
Demographics and clinical characteristics varied significantly (P < .001) across spending groups for each health service.
Age increased significantly (P < .001) across the spending groups, from a median of 9 years (IQR 4, 13) in the lowest spending group (ie, least expensive 80% of children) to a median of 13 years (IQR 7, 17) in the HRU group (ie, most expensive 1% of children). Just under half (49.2%) of children in the lowest spending group were male, rising to 59.7% for the HRU group (P < .001). Only 3.4% of children in the lowest spending group had ≥3 chronic conditions, rising to 61.7% of the HRU spending group (P < .001). Similar differences between the lowest and highest spending groups were seen for technology assistance (<0.1% vs 21.7%, P < .001) and eligibility for Medicaid due to a disability (3.2% vs 54.5%, P < .001).
Health Service Use
Examples of the percentages of children using selected health services included 4.5% (n = 160 967) hospital care, 19.4% (n = 695 622) mental health, 34.7% (n = 1 243 574) ED, 53.0% (n = 1 899 464) dental care, 55.9% (n = 2 002 723) specialty care, 62.8% (n = 2 250 212) pharmacy, and 74.8% (n = 2 681 806) primary care (Table 2). A larger percentage of children in the highest spending group, compared with children in the lowest spending group, used hospital care (53.1% vs 0.3%, P < .001), mental health services (71.4% vs 12.2%, P < .001), specialty care (87.2% vs 49.9%, P < .001), and pharmacy (93.1% vs 56.2%, P < .001). Larger percentages of children in the highest spending group used other types of health services as well, but with smaller absolute differences than the health services described earlier (eg, primary care, 81.2% vs 71.9%, P < .001; and ED care, 51.2% vs 29.2%, P < .001).
TABLE 2.
Health Care Utilization for Children in Medicaid by Spending Group
| Health Service | Overall Cohort | Spending Groups of Children With Medicaida | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Least Expensive 80% of Children | Most Expensive 20% of Children | |||||||||
| Next 15% | Next 4% | Top 1% | ||||||||
| % Using | Median Encounters Among Users (IQR) | % Utilizing | Median Encounters Among Users (IQR) | % Using | Median Encounters Among Users (IQR) | % Using | Median Encounters Among Users (IQR) | % Using | Median Encounters Among Users (IQR) | |
| Hospitalizations | 4.5 | 1 (1, 1) | 0.3 | 1 (1, 1) | 13.9 | 1 (1, 1) | 41.6 | 1 (1, 1) | 53.1 | 2 (1, 3) |
| Hospital days | — | 3 (2, 4) | — | 2 (1, 2) | — | 2 (2, 3) | — | 3 (2, 6) | — | 14 (7, 32) |
| Mental health care | 19.4 | 8 (3, 25) | 12.2 | 4 (2, 8) | 42.7 | 16 (5, 33) | 63.8 | 61 (18, 105) | 71.4 | 155 (25, 314) |
| Specialty care | 55.9 | 3 (1, 5) | 49.9 | 2 (1, 4) | 78.4 | 4 (2., 8) | 82.3 | 6 (3, 13) | 87.2 | 11 (4, 68) |
| Pharmacy | 62.8 | 5 (2, 11) | 56.2 | 4 (2, 8) | 88.1 | 10 (5, 19) | 90.8 | 16 (7, 32) | 93.1 | 30 (13, 57) |
| Primary care | 74.8 | 4 (2, 8) | 71.9 | 4 (2, 7) | 87.6 | 6 (3, 12) | 82.7 | 6 (2, 11) | 81.2 | 5 (2, 11) |
| Dental | 53.0 | 4 (8, 12) | 51.8 | 4 (7, 11) | 59.1 | 5 (9, 15) | 53.4 | 4 (8, 12) | 51.4 | 4 (7, 12) |
| Emergency department | 34.7 | 5 (3, 10) | 29.2 | 5 (3, 8) | 56.8 | 8 (4, 16) | 56.8 | 10 (4, 21) | 51.2 | 10 (4, 21) |
—, no value.
Health care utilization varied significantly (P < .001) across spending groups for each health service.
Study findings of the quantity of selected health services used by children are shown in Table 2. From the lowest to the highest spending group, the number of primary care encounters among users increased modestly, from 4 ((IQR 2, 7) to 5 (IQR 2, 11) (P < .001). Larger differences in the frequency of health care use were observed with other health services. For example, children in the lowest 80% spending group who were admitted to the hospital had a median of 1 (IQR 1, 1) hospitalization and a median of 2 (IQR 1, 2) inpatient days in 2012. In contrast, children in the top 1% spending group who were admitted to the hospital had a median of 2 (IQR 1, 3) hospitalizations, with a median of 14 (IQR 7, 32) inpatient days. Children in the lowest versus the highest spending group who used mental health services had a median of 4 (IQR 2, 8) versus 155 (IQR 25, 314) encounters. From the lowest to highest spending group, the median number of ED encounters for those who used ED services increased from 5 (IQR 3, 8) to 10 (IQR 4, 21) (P < .001). A lower percentage of children in MMC used hospital services, mental health care, and specialty care, compared with children in Medicaid FFS plans (Supplemental Table 5).
Patterns in Health Care Spending Across the 4 Spending Groups
The total per-member-per-month (PMPM) cost for the entire study population was $222. Inpatient and mental health care accounted for the largest percentages of total spending at 22.1% ($49 PMPM) and 20.5% ($45 PMPM), respectively (Table 3). Other services that were substantial contributors to overall spending included specialty care (9.8%, $22 PMPM), pharmacy (8.9%, $20 PMPM), primary care (8.6%, $19 PMPM), dental care (7.5%, $17 PMPM), and ED (7.3%, $16 PMPM).
TABLE 3.
PMPM Health Care Spending for Children in Medicaid by Spending Group
| Health Service | PMPM Spendinga | Distribution of Spendingb,c | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Overall Cohort | Spending Group | Overall Cohort | Spending Group | |||||||
| Least Expensive 80% | Most Expensive 20% | Least Expensive 80% | Most Expensive 20% | |||||||
| Next 15% | Next 4% | Top 1% | Next 15% | Next 4% | Top 1% | |||||
| Inpatient and emergency care | ||||||||||
| Hospital | $49 | <$1 | $37 | $300 | $3129 | 22.1% | 0.4% | 10.5% | 25.0% | 46.4% |
| ED | $16 | $10 | $38 | $49 | $49 | 7.3% | 14.8% | 10.9% | 4.1% | 0.7% |
| Outpatient care | ||||||||||
| Mental | $45 | $4 | $61 | $416 | $1609 | 20.5% | 6.5% | 17.6% | 34.6% | 23.9% |
| Specialty | $22 | $8 | $28 | $96 | $768 | 9.8% | 11.3% | 8.0% | 8.0% | 11.4% |
| Primary | $19 | $15 | $35 | $31 | $33 | 8.6% | 22.5% | 10.0% | 2.6% | 0.5% |
| Dental | $17 | $14 | $29 | $20 | $17 | 7.5% | 21.1% | 8.2% | 1.7% | 0.3% |
| Pharmacy and medical equipment | ||||||||||
| Pharmacy | $20 | $4 | $31 | $111 | $699 | 8.9% | 6.6% | 8.9% | 9.3% | 10.4% |
| Durable medical equipment | $3 | $2 | $4 | $8 | $28 | 1.2% | 2.8% | 1.2% | 0.7% | 0.4% |
| Home and community care | ||||||||||
| Therapy | $14 | $1 | $52 | $95 | $132 | 6.3% | 1.9% | 14.8% | 7.9% | 2.0% |
| Home care | $2 | <$1 | <$1 | $10 | $126 | 0.8% | <0.1% | 0.1% | 0.8% | 1.9% |
| Hospice | <$1 | <$1 | <$1 | <$1 | $3 | <0.1% | <0.1% | <0.1% | <0.1% | <0.1% |
| Other | ||||||||||
| Testing | $12 | $7 | $27 | $45 | $81 | 5.4% | 9.7% | 7.7% | 3.7% | 1.2% |
| Facility | $3 | $1 | $5 | $12 | $34 | 1.2% | 1.9% | 1.5% | 1.0% | 0.5% |
| Transport | $1 | <$1 | $2 | $8 | $30 | 0.5% | 0.5% | 0.6% | 0.6% | 0.4% |
PMPM spending varied significantly (P < .001) across the 4 spending groups for all health services except hospice.
Shown are the column percentages of spending across health services for each of the 4 spending categories.
The distribution of spending varied significantly (P < .001) across the 4 spending groups for all health services except hospice.
The range of spending was <$292 PMPM for the lowest spending group to >$2610 PMPM for the highest spending group. The distribution of spending across the care continuum varied between the 4 spending groups (Table 3). The percentage of total spending attributable to inpatient care increased from 0.4% in the lowest 80% spending group to 46.4% for the top 1% spending group (P < .001). Similarly, mental health spending increased from 6.5% to 23.9% of total spending across these 2 groups (P < .001). The percentage of total spending on primary care decreased from 22.5% for the lowest 80% spending group to 0.5% for the 1% top spending group (P < .001). Similarly, ED spending decreased from 14.8% to 0.7% of total spending across the same groups (P < .001). For the lowest 80% spending group, the 5 health services comprising the highest proportions of spending were primary care, dental, ED, specialty, and testing (Fig 1). In contrast, for the top 1% spending group, the 5 health services with the highest proportions of spending were hospital care, mental health, specialty, pharmacy, and therapies.
FIGURE 1.
Distribution of spending for health care services by spending group for children in Medicaid.
Individual patient (ie, PMPM) spending increased within each service category from the lowest to highest spending group (Table 3). The rise in spending was modest for primary, dental, and ED care. Dental PMPM spending increased from $14 to $17 for the lowest and highest spending groups. Primary care PMPM spending increased from $15 to $33, and ED PMPM costs increased from $10 to $49 across the same groups. The rise in spending was much larger for other types of health services. For inpatient care, the PMPM spending increased from <$1 to $3129 for the lowest and highest spending groups. Mental health PMPM spending increased from $4 to $1609, specialty care PMPM spending increased from $8 to $768, and pharmacy PMPM spending rose from $4 to $699 across the same groups.
Discussion
The findings from this multistate analysis of children in Medicaid suggest that as health resource use increases across patients, spending rises unevenly across different types of health services. For example, spending on primary and dental care was similar for low and high resource users. In contrast, spending on hospital, mental health, specialty, and pharmacy care was substantially less for low versus high resource users. For child HRUs, primary care made up 0.5% of total health care spending, and inpatient, mental health, specialty, and pharmacy spending made up >90% of spending. More investigation is needed to assess the appropriateness of this distribution of spending and to investigate whether more spending on primary care could lead to better quality of care and cost containment for HRUs.
Our findings are consistent with literature suggesting that medical complexity is a common attribute among the most expensive children with Medicaid.19,28 In the current study, the top 1% spending group had the highest concentration of attributes that are consistent with medical complexity, including multiple chronic conditions, use of medical technology, and the presence of a disability. Moreover, congruent with the health care needs of children with medical complexity, almost all children in the top 1% spending group incurred spending on pharmacy care, specialty care, and diagnostic testing.8,11 Hospital care accounted for the largest percentage of spending for the top 1% spending group, consistent with a previous study of children with medical complexity in Medicaid.19
Although the current study complements existing literature by describing the distribution of spending across the care continuum for children in Medicaid, the study does not evaluate the appropriateness of this distribution. A number of studies suggest that more spending on primary care and outpatient care management might improve the health of child HRUs and mitigate their use of hospital and ED care.15–18 Nearly 1 in 5 of these children in the current study did not have a primary care visit. Investigation of efforts to improve their access and use of primary care might be warranted (eg, some children might reside in a rural or underserved medical area with limited access to primary care). The HRU children who used primary care did so recurrently (a median of 5 annual primary care visits [IQR 2, 11]), making it less clear whether more primary care might be beneficial to them. Moreover, only half of the top 1% spending group in our study used the hospital or ED. Therefore, efforts to reduce hospital and ED use through better primary care might not apply to all child HRUs in Medicaid.29
Our findings underscore the important role of mental health services among child HRUs in Medicaid. Three-quarters of child HRUs used mental health services, which accounted for the highest or second highest percentage of total spending in 3 of the 4 spending groups. Mental health is known to account for a large percentage of health care spending in children with Medicaid,30 and mental health expenditures in the hospital and ED are increasing over time.31 Subsequent assessment of health care spending and use for child HRUs with mental health problems may be important to conduct. Improved outcomes and less health care spending in adults with mental health problems through increased access and use of primary care have been reported.32 Best practices to optimize the mental health of children through primary care, especially children with coexisting chronic medical conditions, remain under investigation.33
This study has several limitations. The eligibility criteria restrict enrollment of infants and do not fully capture high-cost NICU stays. Specific types of primary care visits (eg, well-child vs urgent care) were not distinguishable in the database. Spending and encounters for care coordination activities (eg, proactive care planning, shared decision-making) could not be identified. Non–face-to-face health care encounters between patients and clinicians could not be assessed. The findings of this study for children with Medicaid may not generalize to children with private insurance. The deidentified data precluded identification of the states in which the children resided. The distribution of spending and health care encounters of children living in states not included in our study may be different. There may be variation across states in the amount of covered health services for children (eg, limits on the amount of home health services). States may have different methods of categorizing their Medicaid spending, which could lead to potential inconsistency in the way that spending is reported in the database. Some health care services may be funded under a public system other than Medicaid (eg, mental health services offered in the public school system), which may have led to potential undercounting of certain costs. The current study is not positioned to examine reasons for differences in utilization patterns between FFS and MMC enrollees. Finally, the database contains costs and health services but not health outcomes. Future studies with more clinically rich data are needed to delineate important relationships between spending and outcomes.
Despite these limitations, those seeking to improve quality of care and contain costs in child HRUs may find the results of the current study useful. As primary care clinicians are increasingly encouraged to coordinate and manage care for child HRUs,20,34,35 additional investigation of the current penetration, scope, and frequency of those activities is warranted. If a substantial percentage of child HRUs have unmet care coordination and management needs, then realigning access to and payment for those activities might be beneficial. Depending on the specific attributes of each child HRU, primary care may or may not be the most appropriate setting for increased payment and resources. Regardless of clinical setting, health care spending for child HRUs should be directed toward the health services that most effectively optimize their health and well-being.
Conclusions
As resource use increases in children with Medicaid, spending rises unevenly across health services. Spending on primary care rises modestly compared with other health services. Future studies should assess whether more spending on primary care, or other outpatient and community care, leads to better quality of care and cost containment for some HRUs.
Glossary
- ED
emergency department
- FFS
fee for service
- HRU
high resource user
- IQR
interquartile range
- MMC
Medicaid managed care
- PCP
primary care physician
- PMPM
per member per month
Footnotes
Dr Kuo conceptualized and designed the study and drafted the initial manuscript; Dr Hall acquired the data, conducted the initial analyses, analyzed and interpreted the study data, and revised the manuscript for important intellectual content; Drs Agrawal, Cohen, Feudtner, Goodman, and Neff analyzed and interpreted the study data and revised the manuscript for important intellectual content; Dr Berry conceptualized and designed the study, analyzed and interpreted the data, and drafted the manuscript; and all authors approved the final manuscript as written.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Dr Berry was supported by the Eunice Kennedy Shriver National Institute for Child Health and Human Development (K23HD058092) and the Agency for Healthcare Research and Quality (R21HS23092). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Sisko AM, Keehan SP, Cuckler GA, et al. National health expenditure projections, 2013–23: faster growth expected with expanded coverage and improving economy. Health Aff (Millwood). 2014;33(10):1841–1850 [DOI] [PubMed] [Google Scholar]
- 2.Moses H III, Matheson DH, Dorsey ER, George BP, Sadoff D, Yoshimura S. The anatomy of health care in the United States. JAMA. 2013;310(18):1947–1963 [DOI] [PubMed] [Google Scholar]
- 3.Liptak GS, Shone LP, Auinger P, Dick AW, Ryan SA, Szilagyi PG. Short-term persistence of high health care costs in a nationally representative sample of children. Pediatrics. 2006;118(4). Available at: www.pediatrics.org/cgi/content/full/118/4/e1001 [DOI] [PubMed] [Google Scholar]
- 4.Super-utilizers get red carpet treatment. Hosp Case Manag. 2014;22(1):4–5 [PubMed] [Google Scholar]
- 5.Hasselman D. 2013 Super-Utilizer Summit: Common Themes From Innovative Complex Care Management Programs. Hamilton, NJ: Center for Health Care Strategies; 2013 [Google Scholar]
- 6.Berwick DM, Hackbarth AD. Eliminating waste in US health care. JAMA. 2012;307(14):1513–1516 [DOI] [PubMed] [Google Scholar]
- 7.Taylor EF, Lake T, Nysenbaum J, Petersen G, Meyers D. Coordinating Care in the Medical Neighborhood: Critical Components and Available Mechanisms. Rockville, MD: Agency for Healthcare Research and Quality; June 2011. [Google Scholar]
- 8.Cohen E, Berry JG, Camacho X, Anderson G, Wodchis W, Guttmann A. Patterns and costs of health care use of children with medical complexity. Pediatrics. 2012;130(6). Available at: www.pediatrics.org/cgi/content/full/130/6/e1463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stille C, Turchi RM, Antonelli R et al. ; Academic Pediatric Association Task Force on Family-Centered Medical Home . The family-centered medical home: specific considerations for child health research and policy. Acad Pediatr. 2010;10(4):211–217 [DOI] [PubMed] [Google Scholar]
- 10.Kenney GM, Ruhter J, Selden TM. Containing costs and improving care for children in Medicaid and CHIP. Health Aff (Millwood). 2009;28(6):w1025–w1036 [DOI] [PubMed] [Google Scholar]
- 11.Cohen E, Kuo DZ, Agrawal R, et al. Children with medical complexity: an emerging population for clinical and research initiatives. Pediatrics. 2011;127(3):529–538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Neff JM, Sharp VL, Muldoon J, Graham J, Myers K. Profile of medical charges for children by health status group and severity level in a Washington State Health Plan. Health Serv Res. 2004;39(1):73–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berry JG, Hall DE, Kuo DZ, et al. Hospital utilization and characteristics of patients experiencing recurrent readmissions within children’s hospitals. JAMA. 2011;305(7):682–690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Neuman MI, Alpern ER, Hall M, et al. Characteristics of recurrent utilization in pediatric emergency departments. Pediatrics. 2014;134(4). Available at: www.pediatrics.org/cgi/content/full/134/4/e1025 [DOI] [PubMed] [Google Scholar]
- 15.Klitzner TS, Rabbitt LA, Chang RK. Benefits of care coordination for children with complex disease: a pilot medical home project in a resident teaching clinic. J Pediatr. 2010;156(6):1006–1010 [DOI] [PubMed] [Google Scholar]
- 16.Mosquera RA, Avritscher EB, Samuels CL, et al. Effect of an enhanced medical home on serious illness and cost of care among high-risk children with chronic illness: a randomized clinical trial. JAMA. 2014;312(24):2640–2648 [DOI] [PubMed] [Google Scholar]
- 17.Casey PH, Lyle RE, Bird TM, et al. Effect of hospital-based comprehensive care clinic on health costs for Medicaid-insured medically complex children. Arch Pediatr Adolesc Med. 2011;165(5):392–398 [DOI] [PubMed] [Google Scholar]
- 18.Gordon JB, Colby HH, Bartelt T, Jablonski D, Krauthoefer ML, Havens P. A tertiary care–primary care partnership model for medically complex and fragile children and youth with special health care needs. Arch Pediatr Adolesc Med. 2007;161(10):937–944 [DOI] [PubMed] [Google Scholar]
- 19.Berry JG, Hall M, Neff J, et al. Children with medical complexity and Medicaid: spending and cost savings. Health Aff (Millwood). 2014;33(12):2199–2206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Edwards ST, Abrams MK, Baron RJ, et al. Structuring payment to medical homes after the Affordable Care Act. J Gen Intern Med. 2014;29(10):1410–1413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cutler D. Analysis & commentary. How health care reform must bend the cost curve. Health Aff (Millwood). 2010;29(6):1131–1135 [DOI] [PubMed] [Google Scholar]
- 22.Homer CJ, Patel KK. Accountable care organizations in pediatrics: irrelevant or a game changer for children? JAMA Pediatr. 2013;167(6):507–508 [DOI] [PubMed] [Google Scholar]
- 23.Bethell CD, Read D, Blumberg SJ, Newacheck PW. What is the prevalence of children with special health care needs? Toward an understanding of variations in findings and methods across three national surveys. Matern Child Health J. 2008;12(1):1–14 [DOI] [PubMed] [Google Scholar]
- 24.Agency for Healthcare Research and Quality. Chronic condition indicator. Available at: www.hcup-us.ahrq.gov/toolssoftware/chronic/chronic.jsp. Accessed July 23, 2015
- 25.Chi MJ, Lee CY, Wu SC. The prevalence of chronic conditions and medical expenditures of the elderly by Chronic Condition Indicator (CCI). Arch Gerontol Geriatr. 2011;52(3):284–289 [DOI] [PubMed] [Google Scholar]
- 26.Friedman B, Jiang HJ, Elixhauser A, Segal A. Hospital inpatient costs for adults with multiple chronic conditions. Med Care Res Rev. 2006;63(3):327–346 [DOI] [PubMed] [Google Scholar]
- 27.Palfrey JS, Haynie M, Porter S, et al. Prevalence of medical technology assistance among children in Massachusetts in 1987 and 1990. Public Health Rep. 1994;109(2):226–233 [PMC free article] [PubMed] [Google Scholar]
- 28.Agrawal R, Smith T, Li Y, Cartland J. Rate of spending on chronic conditions among Medicaid and CHIP recipients. Pediatrics. 2014;134(1). Available at: www.pediatrics.org/cgi/content/full/134/1/e80 [DOI] [PubMed] [Google Scholar]
- 29.Bodenheimer T. Strategies to Reduce Costs and Improve Care for High-Utilizing Medicaid Patients: Reflections on Pioneering Programs. Hamilton, NJ: Center for Health Strategies, Inc; October 2013
- 30.Howell EM, Teich J. Variations in Medicaid mental health service use and cost for children. Adm Policy Ment Health. 2008;35(3):220–228 [DOI] [PubMed] [Google Scholar]
- 31.Torio CM, Encinosa W, Berdahl T, McCormick MC, Simpson LA. Annual report on health care for children and youth in the United States: national estimates of cost, utilization and expenditures for children with mental health conditions. Acad Pediatr. 2015;15(1):19–35 [DOI] [PubMed] [Google Scholar]
- 32.Twomey CD, Baldwin DS, Hopfe M, Cieza A. A systematic review of the predictors of health service utilisation by adults with mental disorders in the UK. BMJ Open. 2015;5(7):e007575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kelleher KJ, Stevens J. Evolution of child mental health services in primary care. Acad Pediatr. 2009;9(1):7–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Meyers D, Peikes D, Genevro J, et al. The Roles of Patient-Centered Medical Homes and Accountable Care Organizations in Coordinating Patient Care. Rockville, MD: Agency for Healthcare Research and Quality; 2010 [Google Scholar]
- 35.O’Donnell R. Reforming Medicaid for medically complex children. Pediatrics. 2013;131(suppl 2):S160–S162 [DOI] [PubMed] [Google Scholar]