Somatic symptoms disorders exist in every discipline of medicine and comprise a substantial percentage of medical visits, clinical testing, and disability contributing to the high cost of healthcare and human suffering (1). Medically “unexplained” symptoms are seen in about one-third of outpatient neurology visits with nearly one-fifth of these formally diagnosed with functional neurologic symptoms (2). Psychogenic nonepileptic seizures (PNES) are the largest subgroup of functional neurologic disorders and are responsible for a big burden of healthcare expenses, estimated at approximately $900 million annually (3). Over the past 5 to 10 years, a promising shift in the focus of clinical research on treatment has occurred for PNES. Unfortunately, despite emerging evidence-based treatments, health outcomes remain quite poor, and getting patients to follow up with psychiatric care continues to be problematic. Even when patients successfully follow through for their first treatment appointments, the dropout rate for ongoing care hovers around 50% (4).
The reasons for treatment drop-off are not well understood. Patients with nonepileptic seizures are a complex and heterogeneous group, often with lower education, substance use, unemployment, chronic psychiatric difficulties, and trauma/abuse—all groups that are more likely to be nonadherent. In general, many PNES patients do not understand or accept their symptoms as psychologically based, and this may put them at odds with their treating providers. Many of these factors are intrinsic to the underlying psychopathology. However, there are also provider-dependent factors contributing to the poor follow-up. One likely factor is that once the diagnosis is confirmed, the needed transition from the traditional focus—that of ruling out epilepsy to getting patients to understand, accept, and follow up with treatment—is not well executed by the providers. The communication between doctor and patient may be an important factor in the success of the transition of care. This is not a new idea, yet little research has focused on this specific topic. It is clear from the literature that patient–doctor communication is one of the biggest factors predicting adherence to treatment (5). In addition, improving therapeutic alliance has shown to improve adherence to treatment for post-traumatic stress disorder (PTSD) as well as other conditions (6). Patients repeatedly intersect with providers who do not believe their symptoms are real and think that all that is necessary is that a correct diagnosis be delivered. Other psychiatric disorders, such as depression or anxiety, are not handled as though patients are deliberately producing symptoms. Being taken seriously was shown to be the most important contributing factor in coping with diagnosis (7).
What may be different about PNES and perhaps all functional disorders is the assumption that there is no bonafide illness. Do these physicians' attitudes and assumptions reinforce poor outcomes? Our attitudes are insidious, and the negative or unhelpful ones can readily emerge during frustrating interactions with challenging patients. Patient factors, such as previous experience with psychiatric treatment, not understanding, or unwillingness to accept the diagnosis may also play an important role in keeping patients from staying in treatment. Given how common functional neurologic disorders are, and the published difficulty in getting patients to adhere to treatments, the American Epilepsy Society (AES) has decided to focus a Q-PULSE survey on patterns of communication of the PNES diagnosis in practice and training.
Methods
The Quantitative Practical Use-Driven Learning Survey in Epilepsy (Q-PULSE) panel was established in 2012 to help provide expert opinion for important and practical clinical questions where evidence-based data is lacking. The Q-PULSE panel felt that practice around nonepileptic seizures was quite variable and along with the Nonepileptic Seizure workgroup of the AES practice management committee, they designed a 7-item questionnaire. One hundred and forty-six epilepsy experts from level-4 epilepsy centers all across the United States were asked to respond to questions about education and communication practices with PNES. The survey opened July 9, 2015, and closed August 3, 2015.
Results
The response rate was 86%. The 7 questions with the responses appear below.
Discussion
The first question asked was whether patients are informed of the possible PNES diagnosis before video EEG (v-EEG) diagnosis, if clinically appropriate (see Figure 1). In most other arenas of medicine, springing a completely new diagnosis—one that may be devastating for the patient—would be unusual after the entire workup is completed. Only 10% of responders said that they “always” introduce the possibility of PNES when relevant. Forty-three percent of the panel occasionally mention PNES in the differential diagnosis before the v-EEG diagnosis. The hidden bias here is that the doctor believes this to be good news. However, patients generally do not look at PNES as a “good news” diagnosis and must understand it to be more stigmatizing than epilepsy. Therefore, neglecting to introduce the potential PNES diagnosis during the workup phase may signify the first important breakdown in the patient–doctor communication/alliance. Introducing a mental health provider while the workup is taking place and discussing the possibility of PNES early may facilitate acceptance of the disorder by introducing a psychiatric differential diagnosis in a nonstigmatized way (8).
FIGURE 1.
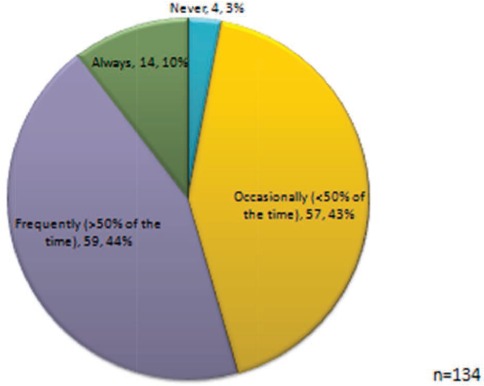
In your center, if clinically appropriate, the possibility of psychogenic nonepileptic seizures (PNES) is discussed with the patient prior to video EEG.
The second question inquires about how the diagnosis is generally delivered once confirmed by the v-EEG (see Figure 2). Over 70% responded that only the neurologist gives the diagnosis, and nearly 80% try to present the diagnosis to the patient and family member, if available. This result is not that surprising since many centers do not have a psychiatrist evaluate the patient in the hospital, and the neurologist is responsible for admitting and diagnosing the patient. However, given that PNES is a psychiatric condition and many patients have emotional difficulties, the neurologist may not feel best equipped to help patients understand their diagnosis (8).
FIGURE 2.
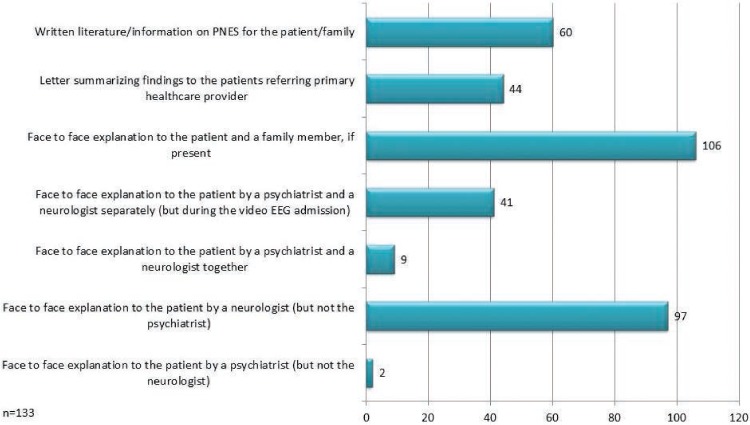
At your center, delivery of the diagnosis of PNES (after confirmation by video EEG) is generally . . . . (Check all that apply.)
Question three asks for key phrases that are used during the communication of the diagnosis (see Figure 3). Most experts responded that the events are not treated with AEDs (92%), the events are not deliberately produced (87%), the events are real and commonly encountered (82%), and they have psychological origin (79%). Areas in need of further study might include whether the common response by experts that PNES diagnosis is good news that the events are not real seizures (67%) affects outcome. It may be good news for the neurologist who may no longer plan to follow the patient, but the literature seems to suggest that patients do not believe this is good news. There is an underlying assumption that if the seizures are not “real seizures,” then they must be fake. Despite abandoning the term “pseudoseizures,” the underlying theme of “faking” remains within the communication of “not real.”
FIGURE 3.
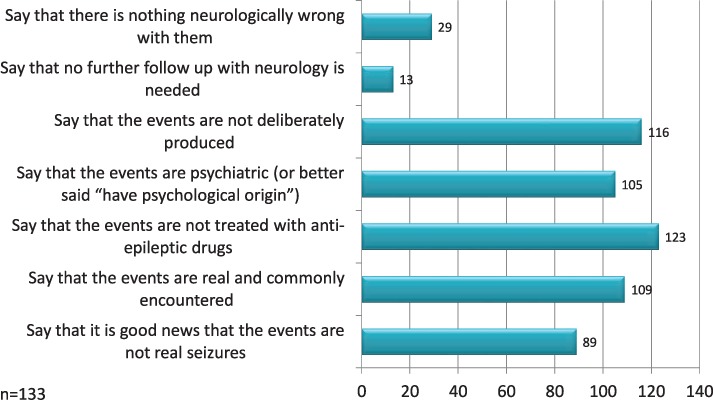
What are the key phrases that you try to incorporate when communicating the diagnosis of PNES (without comorbid epilepsy)? (Please check all that apply.)
Question four asks about the appropriate follow-up for patients once the diagnosis of PNES is rendered (see Figure 4). Over one-fifth of the experts believe that only mental health and not neurological follow-up is needed. A majority of experts were not bothered (no follow-up needed) by patients who doubted their diagnosis or who had not connected with a mental health provider. In the new world of careful hand-offs and transitioning of patients, we are sending a clear message that we do not really care what happens after the diagnosis is made and that we are completely finished with the patient. In many respects, this physician response represents a reenactment of past neglect and abandonment that many PNES patients have suffered. Traditional psychodynamic theory may conceptualize this response as a reaction to the countertransference evoked by these patients.
FIGURE 4.
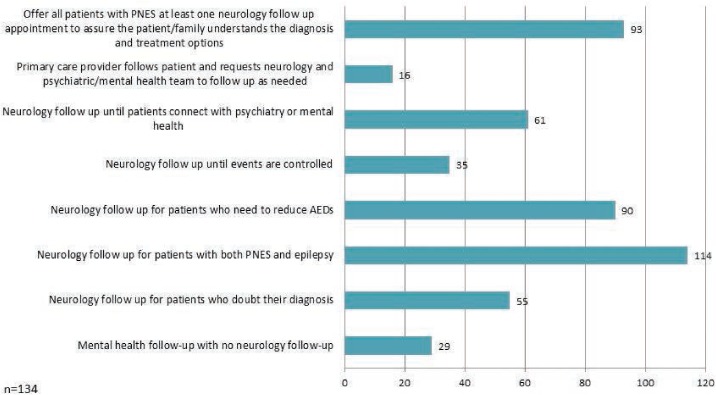
What is the appropriate follow-up for PNES to confirm and treat the underlying conversion disorder after the communication of the diagnosis? (Please check all that apply.)
For the fifth question, over half of the patients did not meet with a psychiatrist regarding the PNES diagnosis at time of hospital discharge, and 42% were told to make an appointment with someone of their choosing (see Figure 5). Given how poorly this diagnosis is understood among mental health providers, it is likely that providers will not know what to do when and if the patient arrives for their first appointment.
FIGURE 5.
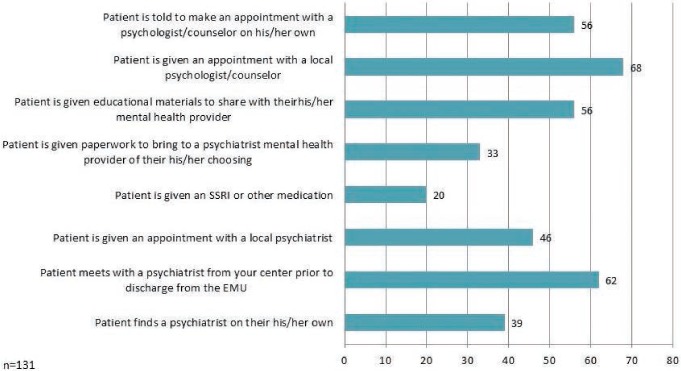
If mental health follow-up is recommended at your center, how do you approach this? (Please check all that apply.)
Lastly, Q-PULSE experts were asked how they teach resident trainees about PNES (see Figures 6 and 7). The overwhelming majority reported that they provide at most, one formal lecture, and this lecture is mainly for the purpose of differential diagnosis (93%). Most programs (70%) educated their residents about PNES as part of bedside teaching or through videos. Delivering the diagnosis and the challenges these patients embody were the focus for the great majority (86%), but given that these professionals will be the ultimate experts at confirming the diagnosis, this response should have been 100% (see Figure 7). Almost half of the experts stated that part of the teaching focus is on the wasted resources caused by PNES. The not-so-subtle message conveyed is that patients with epilepsy are the only ones deserving of neurologists' time, whereas those with PNES are wasting our time and resources. How to help patients transition their care from neurology to psychiatry should be an important focus in the training of future PNES diagnosticians. Acquiring these skills can equip neurologists in the initiation of PNES treatment, while the strong emphasis on overutilization of resources without training on solutions can reinforce negative attitudes.
FIGURE 6.
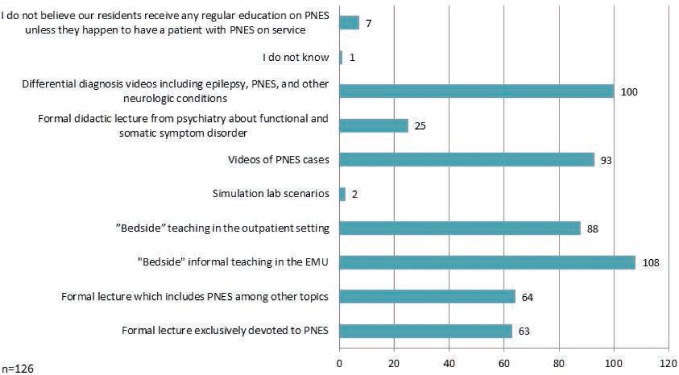
How do you teach residents about PNES? (Check all that apply.)
FIGURE 7.
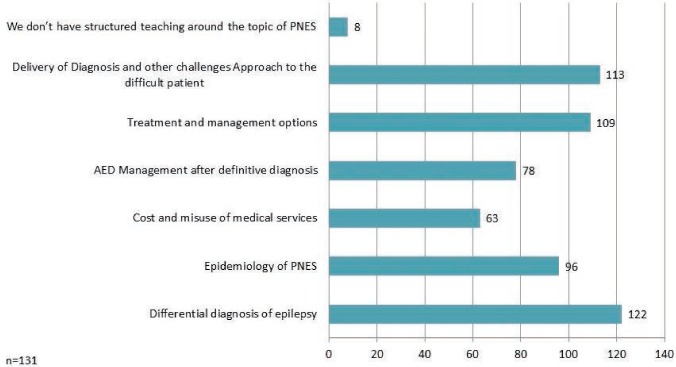
When teaching about PNES, which topics do you focus on? (Check all that apply.)
Little data are available about how long neurologists should follow these PNES patients, how best to communicate the diagnosis, and whether these issues impact outcome. Patients and trainees experience negative biases toward PNES through family members and through their professional role models, respectively. This is ineffective and needs to be addressed. Although immediate resolution of PNES events might infrequently occur with diagnosis, the need for more sustainable relief from seizures and the underlying psychopathology, is more likely the rule (9), and adherence to treatment follow-up is what is needed. Additionally, structured communication paradigms can be well received by patients (10).
So are we perpetuating poor outcomes through this negative bias? Without understanding what we do, we will never really know if we are contributing to the problem rather than improving it. Patients know when their doctors do not believe them. Residents learn by imitation. If we are mainly using bedside teaching without a formal curriculum, we may be perpetuating negative messages about these patients. Education is a powerful tool for change. It has been shown to decrease negative attitudes for psychiatric or other stigmatized conditions (11). Modifying residency curricula to train on these issues may lead to improvement in patient care and healthcare delivery. While ACGME milestones were created to document competencies and are beginning to be implemented, there is still a dearth of materials for training residents in functional disorders. Currently, there are no ABPN standards for residency curricula for diagnosis and treatment of PNES or other functional neurological symptoms disorders. Our training should include clear directives regarding communications between doctor and patient to enable a new generation of doctors to change the negative attitudes surrounding PNES toward more effective outcomes.
The results of this Q-PULSE survey begin to explore gaps in our knowledge surrounding our practice with PNES. Based on this survey, it seems clear that research and education are needed in the area of communicating the diagnosis to the patient, as well as the impact of this communication on outcomes. The interaction with PNES patients can be quite complex, and neurology training to date has not included education in this area. We are beginning to see a return of psychiatry and neurology working together for the common good of the patient, integrating multidisciplinary teams to offer the best experts at the right times. At present, we do not know whether patient outcomes will be improved by creating curricula aimed at different groups of trainees, but we still need to have guidelines for best practices for communicating the diagnosis, engaging them in treatment, and how long the neurologist should follow these patients.
Footnotes
Editor's Note: Authors have a Conflict of Interest disclosure which is posted under the Supplemental Materials (190KB, pdf) link.
References
- 1.Carson AJ, Best S, Postma K, Stone J, Warlow C, Sharpe M. The outcome of neurology outpatients with medically unexplained symptoms: A prospective cohort study. J Neurol Neurosurg Psychiatry. 2003;74:897–900. doi: 10.1136/jnnp.74.7.897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stone J, Carson A, Duncan R, Coleman R, Roberts R, Warlow C, Hibberd C, Murray G, Cull R, Pelosi A, Cavanagh J, Matthews K, Goldbeck R, Smyth R, Walker J, Macmahon AD, Sharpe M. Symptoms “unexplained by organic disease” in 1144 new neurology out-patients: How often does the diagnosis change at follow-up? Brain. 2009;132(pt 10):2878–2888. doi: 10.1093/brain/awp220. [DOI] [PubMed] [Google Scholar]
- 3.Martin RC, Gilliam FG, Kilgore M, Faught E, Kuzniecky R. Improved health care resource utilization following video-EEG-confirmed diagnosis of nonepileptic psychogenic seizures. Seizure. 1998;7:385–390. doi: 10.1016/s1059-1311(05)80007-x. [DOI] [PubMed] [Google Scholar]
- 4.Baslet G, Prensky E. Initial treatment retention in psychogenic non-epileptic seizures. J Neuropsychiatry Clin Neurosci. 2013;25:63–67. doi: 10.1176/appi.neuropsych.11090223. [DOI] [PubMed] [Google Scholar]
- 5.Ong LM, de Haes JC, Hoos AM, Lammes FC. Doctor-patient communication: A review of the literature. Soc Sci Med. 1995;40:903–918. doi: 10.1016/0277-9536(94)00155-m. [DOI] [PubMed] [Google Scholar]
- 6.Keller SM, Zoellner LA, Feeny CN. Understanding factors associated with early therapeutic alliance in PTSD treatment: Adherence, childhood sexual abuse history, and social support. J Consult Clin Psychol. 2010;78:974–979. doi: 10.1037/a0020758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Karterud HN, Knizek BL, Nakken KO. Changing the diagnosis from epilepsy to PNES: Patients' experiences and understanding of their new diagnosis. Seizure. 2010;19:40–46. doi: 10.1016/j.seizure.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 8.Quinn MC, Schofield MJ, Middleton W. Permission to speak: Therapists' understandings of psychogenic nonepileptic seizures and their treatment. J Trauma and Dissoc. 2010;11:108–123. doi: 10.1080/15299730903491322. [DOI] [PubMed] [Google Scholar]
- 9.Farias ST, Thieman C, Alsaadi TM. Psychogenic nonepileptic seizures: Acute change in event frequency after presentation of the diagnosis. Epilepsy Behav. 2003;4:424–429. doi: 10.1016/s1525-5050(03)00143-4. [DOI] [PubMed] [Google Scholar]
- 10.Hall-Patch L, Brown R, House A, Howlett S, Kemp S, Lawton G, Mayor R, Smith P, Reuber M, NEST collaborators Acceptability and effectiveness of a strategy for the communication of the diagnosis of psychogenic nonepileptic seizures. Epilepsia. 2010;51:70–78. doi: 10.1111/j.1528-1167.2009.02099.x. [DOI] [PubMed] [Google Scholar]
- 11.Morrison A, Roman B, Borges N. Psychiatry and emergency medicine: Medical student and physician attitudes toward homeless persons. Acad Psychiatry. 2012;36:211–215. doi: 10.1176/appi.ap.10080112. [DOI] [PubMed] [Google Scholar]


