Abstract
Outcomes of cardiopulmonary resuscitation (CPR) in hospitalized patients with ESRD requiring maintenance dialysis are unknown. Outcomes of in-hospital CPR in these patients were compared with outcomes in the general population using data from the Nationwide Inpatient Sample (NIS; 2005–2011). The study population included all adults (≥18years old) from the general population and those with a history of ESRD. Baseline characteristics, in-hospital complications, and discharge outcomes were compared between the two groups. The effects of in-hospital CPR on mortality, length of stay, hospitalization charges, and discharge destination were analyzed. Yearly national trends in survival, discharge to home, and length of stay were also examined using the Cochran–Armitage trend test. During the study period, 56,069 patients with ESRD underwent in-hospital CPR compared with 323,620 patients from the general population. Unadjusted in-hospital mortality rates were higher in patients with ESRD (73.9% versus 71.8%, P<0.001) on univariate analysis. After adjusting for age, gender, and potential confounders, patients with ESRD had higher odds of mortality (odds ratio, 1.24; 95% confidence interval, 1.11 to 1.3; P<0.001). Survival after CPR improved in the year 2011 compared with 2005 (31% versus 21%, P<0.001). Multivariate analysis also revealed that a greater proportion of patients with ESRD who survived were discharged to skilled nursing facilities. In conclusion, outcomes after in-hospital CPR are improving in patients with ESRD but remain worse than outcomes in the general population. Patients with ESRD who survive are more likely to be discharged to nursing homes.
Keywords: cardiovascular, chronic dialysis, epidemiology and outcomes
Ventricular arrhythmias and sudden and cardiac death necessitating cardiopulmonary resuscitation (CPR) are common occurrences in patients on maintenance dialysis.1,2 Such events mostly occur during dialysis and only 56% of these patients present to the hospital alive, with 24% of those surviving to the hospital discharge and 15% alive at least 1year after the event.1 However, few data are available on the outcomes of CPR in hospitalized patients with ESRD. The existing literature consists of small and older studies that do not reflect current standards of CPR practices. In a study of 74 patients with ESRD undergoing CPR in both hospital and dialysis units, 37% survived the initial resuscitation; 6% were alive at the time of hospital discharge, and 3% were still living 6 months later.3 Patients without ESRD had similar immediate (27%) survival and survival to hospital discharge was not significantly better (6% in patients on dialysis and 30% in patients without ESRD). However, post-CPR survival at 6 months was significantly better in patients without ESRD (2% in patients on dialysis versus 23% in patients without ESRD, P=0.044).3 Another study analyzed the outcomes of 12 CPR attempts in patients with ESRD who had cardiac arrest in the dialysis unit. Four patients died within the first 48 hours, seven were alive at the time of hospital discharge, and five were living 2 months later.4 Tzamaloukas et al. examined 53 patients on maintenance dialysis undergoing 56 CPR episodes: survival was 50% in the dialysis unit (6/12), 44% in the intensive care unit (1/5), 20% in the emergency room (1/5), and zero in hospital wards (0/12).5 CPR guidelines and algorithms receive regular updates, and it is not known whether the data from the previous small-scale studies are applicable in the current era. Outcomes of in-hospital CPR may be different from CPR outcomes in dialysis units but knowledge of outcomes of in-hospital CPR in patients on dialysis is limited. Larger studies that are devoid of single-center institutional biases and that reflect the current standards of in-hospital CPR practices are needed to answer this question. The present study aims to fill this literature gap by using a large nationally representative data set.
Results
Characteristics of CPR Recipients
From 2005 to 2011, 56,069 patients with ESRD received in-hospital CPR, compared with 323,620 patients from the general population. Patients’ demographics and comorbid conditions are listed in Table 1. Patients with ESRD were younger with a mean age of 64 years versus 67 years, P<0.0001. A higher percentage of African Americans and Latin Americans were in the ESRD group. Patients with ESRD were less likely to have private health maintenance organization insurance or no insurance and more likely to have Medicaid/Medicare. Chronic obstructive pulmonary disease, obesity, solid tumor with metastasis, metastatic cancer, alcohol abuse, and nicotine dependence were more common in the general population group; all other comorbid conditions were more common among patients with ESRD. The patients with ESRD had a higher Charlson comorbidity index than the general population (Table 1).
Table 1.
Demographic, clinical and hospital characteristics in patients with and without ESRD undergoing CPR Nationwide Inpatient Sample 2005–2011
| Characteristics | With ESRD | Without ESRD | P Value |
|---|---|---|---|
| Overall number (%) | 56,069 | 323,620 | |
| Age mean (95% CI) | 64 (64 to 65) | 67 (66 to 67) | <0.001 |
| Women | 26,235 (46.8) | 153,216 (47.4) | 0.3 |
| Race/ethnicity | |||
| Whites | 19,277 (39.6) | 189,524 (69.5) | <0.001 |
| African Americans | 18,271 (37.5) | 43,199 (15.8) | |
| Latin Americans | 7288 (15.0) | 23,905 (8.8) | |
| Others | 3860 (7.9) | 16,179 (5.9) | |
| Comorbid conditions | |||
| Hypertension | 45,796 (81.7) | 150,262 (46.4) | <0.001 |
| Diabetes mellitus | 13,868 (24.7) | 67,698 (20.9) | <0.001 |
| Dyslipidemia | 1355 (2.4) | 14,917 (4.6) | <0.001 |
| Atrial fibrillation | 11,228 (20.0) | 66,517 (20.6) | 0.2 |
| Congestive heart failure | 18,201 (32.5) | 57,839 (17.9) | <0.001 |
| Deficiency anemias | 21,085 (37.6) | 52,880 (16.3) | <0.001 |
| Valvular heart disease | 4674 (8.3) | 16,590 (5.1) | <0.001 |
| Peripheral vascular disease | 11,062 (19.7) | 26,274 (8.1) | <0.001 |
| Chronic lung disease | 11,152 (19.9) | 86,120 (26.6) | <0.001 |
| Fluid and electrolyte disorder | 25,442 (45.4) | 124,774 (38.6) | <0.001 |
| Hyperkalemia | 8941(16.0) | 11,526 (3.6) | <0.001 |
| Liver disease | 2841 (5.1) | 11,169 (3.5) | <0.001 |
| Coagulopathy | 8279 (14.8) | 30,479 (9.4) | <0.001 |
| AIDS | 527 (0.9) | 857 (0.3) | <0.001 |
| Obesity | 4121 (7.3) | 25,702 (7.9) | 0.04 |
| Paralysis | 2077 (3.7) | 13,156 (4.1) | <0.1 |
| Solid tumor without metastasis | 813 (1.4) | 11,718 (3.6) | <0.001 |
| Metastatic cancer | 727 (1.3) | 15,573 (4.8) | <0.001 |
| Alcohol abuse | 957 (1.7) | 18,987 (5.9) | <0.0001 |
| Nicotine dependence | 1605 (2.9) | 31,323 (9.7) | <0.0001 |
| Coronary artery disease | 23,112 (41.2) | 126,294 (39.0) | <0.001 |
| Dementia | 570 (1.0) | 9312 (2.9) | <0.001 |
| Malnutrition | 7216 (12.9) | 27,160 (8.4) | <0.001 |
| Charlson comorbidity score-mean (SD) | 7±5 | 5±5 | <0.001 |
| Charlson comorbidity index | |||
| 0–3 | 3831 (6.8) | 88,339 (27.3) | <0.001 |
| 4–6. | 20,821 (37.2) | 182,253 (56.3) | |
| ≥7 | 31,417 (56.0) | 53,028 (16.4) | |
| Hospital bed size | |||
| Small | 5393 (9.7) | 34,536 (10.7) | <0.001 |
| Medium | 12,683 (22.7) | 81,753 (25.4) | |
| Large | 37,667 (67.6) | 205,550 (63.9) | |
| Insurance status | |||
| Medicare/Medicaid | 49,526 (88.3) | 228,192 (70.5) | <0.001 |
| Private health maintenance organization | 5401 (9.6) | 65,984 (20.4) | |
| No insurance | 1080 (1.9) | 28,890 (8.9) | |
| Hospital regions | |||
| Northeast | 9764 (17.4) | 64,980 (20.1) | <0.003 |
| Midwest | 9438 (16.8) | 60,392 (18.7) | |
| South | 23,085 (41.2) | 124,761 (38.6) | |
| West | 13,783 (24.6) | 73,488 (22.7) | |
| Teaching status | |||
| Nonteaching | 29,783 (53.4) | 183,489 (57.0) | 0.002 |
| Teaching | 25,960 (46.6) | 138,350 (43.0) |
In-Hospital Complications, Length of Stay and Hospitalization Charges
Table 2 shows the rates of complications in the two patient groups. It cannot be determined from the data set if these procedures/complications occurred before or after CPR but they were captured during the same hospitalization. Some, but not all, in-hospital complications were more common among patients on dialysis than in the general population. Patients on dialysis experiencing CPR had more episodes of gastrointestinal bleeding, sepsis, and deep vein thrombosis but other complications were more common in the group without ESRD. A higher proportion of patients on dialysis were intubated (69% versus 63.1%, P<0.001) and received blood transfusions (23.2% versus 18.9%, P<0.001). Fewer dialysis patients underwent procedures such as cardiac catheterization (6% versus 10%, P<0.001), coronary angioplasty (5.6% versus 2.1%, P<0.001), and coronary artery bypass grafting (2% versus 1.1%, P<0.001). There was no statistical difference between teaching and nonteaching hospitals in terms of the frequency of performed cardiac procedures, mainly cardiac angiography, cerebral angiography, coronary angioplasty, and coronary artery bypass grafting (data not shown).
Table 2.
In-hospital complications, procedures, and discharge outcomes in patients with and without ESRD undergoing CPR: Nationwide Inpatient Sample 2005–2011
| Complication, Procedures, and Outcomes | With ESRD | Without ESRD | P Value |
|---|---|---|---|
| In-hospital complications | |||
| Pneumonia | 9965 (17.8) | 57,316 (17.7) | 0.9 |
| Deep venous thrombosis | 1660 (3.0) | 3875 (1.2) | <0.001 |
| Cardiogenic shock | 3126 (5.6) | 21,695 (6.7) | <0.001 |
| Urinary tract infection | 5174 (9.2) | 42,376 (13.1) | <0.001 |
| Sepsis | 18,664 (33.3) | 51,674 (16.0) | <0.001 |
| Pulmonary embolism | 1209 (2.2) | 16,110 (5.0) | <0.001 |
| Myocardial infarction | 10,278 (18.3) | 65,577 (20.3) | <0.001 |
| Unstable angina | 5 (0.008) | 242 (0.07) | <0.001 |
| Rib fractures | 295 (0.5) | 4861 (1.5) | <0.001 |
| Pneumothorax | 765 (1.4) | 8344 (2.6) | <0.001 |
| Cardiac tamponade | 213 (0.4) | 1513 (0.5) | 0.2 |
| Persistent vegetative state | 174 (0.3) | 1384 (0.4) | 0.1 |
| Gastrointestinal bleeding | 3232 (5.8) | 16,805 (4.4) | 0.02 |
| Stroke | 3539 (6.3) | 23,684 (7.3) | 0.002 |
| In-hospital procedures | |||
| Cardiac catheterization | 3377 (6.0) | 32,337 (10.0) | <0.001 |
| Cerebral angiography | 120 (0.2) | 2037 (0.6) | <0.001 |
| Percutaneous transluminal coronary angioplasty | 1154 (2.1) | 18,204 (5.6) | <0.001 |
| Coronary artery bypass grafting | 631 (1.1) | 6449 (2.0) | <0.001 |
| Valvular repair | 450 (0.8) | 3606 (1.1) | 0.004 |
| Valve replacement | 359 (0.6) | 2843 (0.9) | 0.009 |
| Intubation | 38,686 (69.0) | 204,283 (63.1) | <0.001 |
| Tracheostomy | 332 (0.6) | 1438 (0.4) | <0.1 |
| Gastrostomy | 1968 (3.5) | 10,837 (3.3) | 0.4 |
| Blood transfusion | 12,994 (23.2) | 61,092 (18.9) | <0.001 |
| Induced hypothermia | 226(0.4) | 1713 (0.5) | 0.1 |
| Length of stay in days | Median =6, SD = 32, IQR (2–14) | Median = 4, SD = 26, IQR (1–9) | <0.001 |
| Hospital charges in $ | Median=57,761, SD=337,387, IQR (25,603–126,384) | Median=38,747, SD=240,909, IQR (17,520–878,77) | <0.001 |
| Withdrawal of care | 1760 (3.1) | 9159 (2.8) | 0.1 |
| Discharge disposition | |||
| Home/self-care | 6236 (11.1) | 44,359 (13.7) | <0.001 |
| Skilled nursing facility | 8103 (14.5) | 45,666 (14.1) | |
| Unknown | 262 (0.5) | 984 (0.3) | |
| In-hospital mortality | 41,459 (73.9) | 232,460 (71.8) |
IQR, interquartile range.
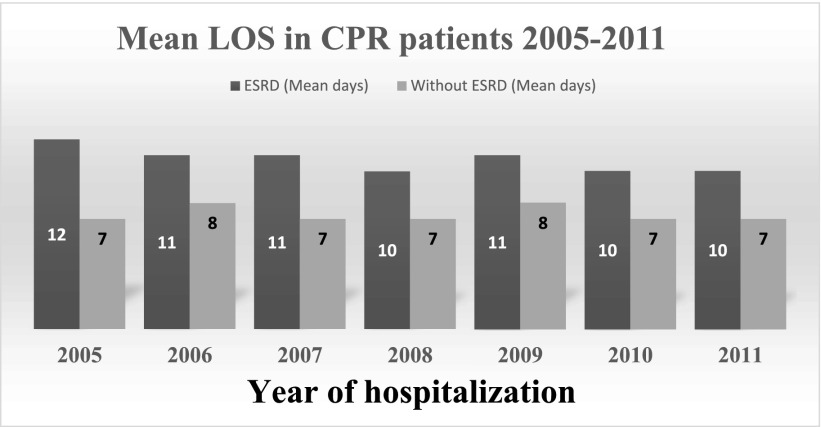
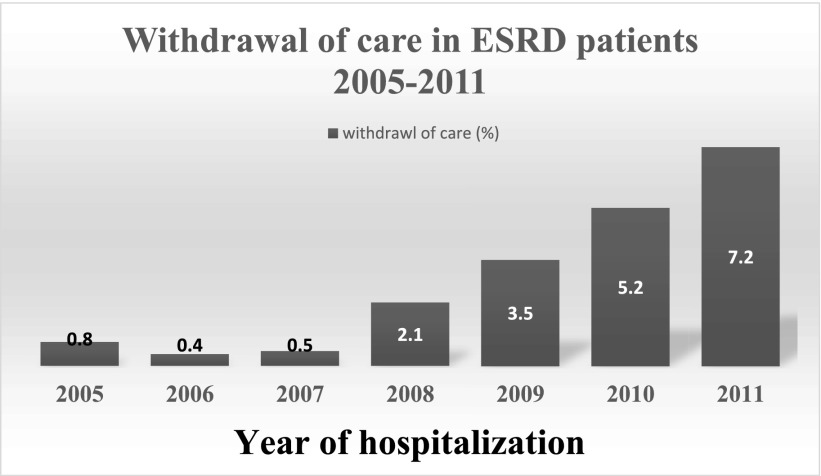
Mean length of stay for all-cause hospitalization in which patients underwent CPR was significantly higher in patients with ESRD: 11±32 days versus 7±26 days (P<0.001). Mean length of stay was not significantly different in 2011 compared with 2005: 10 days in 2011 versus 12 days in 2005 (P=0.1) (Figure 1). Mean hospitalization charges in US dollars were higher in the patients with ESRD: $105,629 ($102,802–$108,456) versus $75,145 ($74,308–$75,983), P<.001. In the linear regression analysis for both patients with ESRD and those without ESRD, hospitalization charges were directly associated with length of hospitalization (P<0.001) after adjusting for age, gender, race/ethnicity, year of hospitalization, and all the variables that were significant in univariate analysis. Withdrawal of care was more common in 2011 compared with 2005: 7.2% versus 0.8%, P<0.001 (Figure 2).
Figure 1.
Mean length of stay in patients with ESRD undergoing CPR during 2005–2011. Mean length of stay was not significantly different: 10 days in 2011 versus 12 days in 2005 (P=0.1).
Figure 2.
Withdrawal of care trend in patients undergoing CPR during 2005–2011, expressed in percentage. In the year 2011, 7.2% of patients with ESRD withdrew care as compared with 0.8% in 2005, P<0.001.
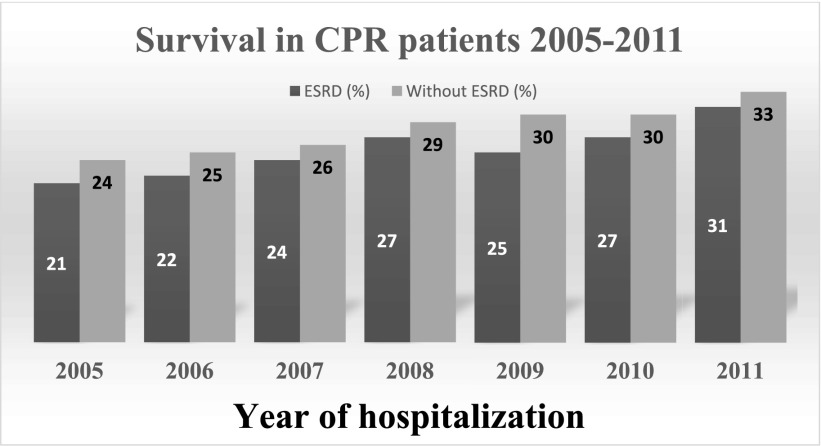
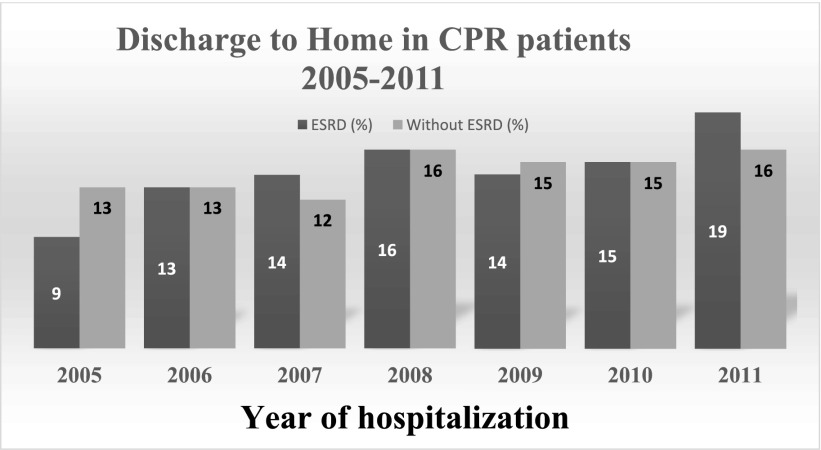
Survival to Discharge and Discharge Destination
Higher in-hospital mortality was observed in patients with ESRD in both univariate and multivariate analyses (Tables 2 and 3). However, survival improved in 2011 compared with the previous years (31% in 2011 versus 21% in 2005, P<0.001) (Figure 3). On multivariate analysis, a higher proportion of the survivors in the ESRD group were discharged to skilled nursing facilities, including both nursing and rehabilitation facilities (Table 3) (odds ratio (OR), 1.13; 95% confidence interval, 1.1 to 1.25); P<0.04). Age <65 years, African-American and Latin-American race, cardiac catheterization, and hospital teaching status were the significant factors associated with the discharge-to-home status on multivariate analysis (Table 4). In the year 2011, 19% of patients with ESRD were discharged home compared with 9% in 2005, P<0.0001(Figure 4). On further subanalysis (data not shown), patients undergoing CPR in teaching hospitals had similar odds of mortality (OR, 0.92; 95% confidence interval (95% CI), 0.85 to 1.12; P=0.2) and lower odds of discharge to nursing homes (OR, 0.76; 95% CI, 0.66 to 0.83; P<0.0001), whereas higher odds of mortality (OR, 1.44; 95% CI, 1.23 to 1.63; P<0.0001) and discharge to nursing homes (OR, 2.14; 95% CI, 1.73 to 2.61; P<0.04) were observed in the patients in intensive care units.
Table 3.
Effect of ESRD on outcomes in patients undergoing cardiopulmonary resuscitation. Nationwide Inpatient Sample 2005–2011
| Outcomes | Unadjusted | Adjusted for age and gender | Adjusted for age, gender, and potential confounders | ||||
|---|---|---|---|---|---|---|---|
| OR (95% CI) | P Value | OR (95% CI) | P Value | OR(95% CI) | P Value | ||
| Model 1 | Analysis comprising all patients | ||||||
| In-hospital mortality | 1.15 (1.03 to 1.24) | <0.001 | 1.14 (1.12 to 1.24) | <0.001 | 1.24 (1.11 to 1.31) | <0.001 | |
| Model 2 | Analysis comprising alive patients | ||||||
| Nursing facility | 1.22 (1.13 to 1.34) | <0.001 | 1.32 (1.24 to 1.51) | <0.001 | 1.13 (1.03 to 1.24) | 0.04 | |
Figure 3.
Survival trend in patients undergoing CPR during 2005–2011, expressed in percentage. Survival improved in 2011 (31% in the year 2011 versus 21% in the year 2005, P<0.001).
Table 4.
Factors associated with discharge to home in patients with ESRD undergoing CPR
| Determinants | Unadjusted OR and 95% CI | P Value | Multivariate adjusted OR and 95% CI | P Value |
|---|---|---|---|---|
| Age, years | ||||
| Age >65 | Reference | Reference | ||
| Age <65 | 1.8 (1.5–2.1) | <0.001 | 1.7 (1.4–2.0) | <0.001 |
| Race | ||||
| White | Reference | Reference | ||
| African Americans | 1.3 (1.1–1.5) | 0.01 | 1.2 (1.1–1.5) | 0.03 |
| Latin Americans | 1.3 (1.1–1.6) | 0.01 | 1.4 (1.1–1.7) | 0.02 |
| Comorbidity | ||||
| Coagulopathy | 0.7 (0.6–0.9) | 0.003 | 0.8 (0.6–1.0) | <0.1 |
| Nicotine dependence | 2.6 (1.7–4.1) | <0.001 | 2.4 (1.4–4.0) | 0.001 |
| In-hospital complication | ||||
| Myocardial infarction | 0.7 (0.6–0.8) | 0.0002 | 0.6 (0.5–0.8) | <0.001 |
| Sepsis | 0.5 (0.4–0.6) | <0.001 | 0.7 (0.6–0.9) | 0.003 |
| Pneumonia | 0.7 (0.6–0.9) | <0.001 | 0.8 (0.7–0.9) | 0.04 |
| In-hospital procedure | ||||
| Cardiac catheterization | 1.5 (1.2–1.9) | 0.002 | 1.4 (1.1–1.9) | 0.01 |
| Percutaneous transluminal coronary angioplasty | 1.7 (1.1–2.7) | <0.01 | 1.8 (1.1–2.9) | 0.02 |
| Mechanical ventilation | 0.3 (0.2–0.3) | <0.001 | 0.3 (0.2–0.4) | <0.001 |
| Transfusion | 0.6 (0.5–0.7) | <0.001 | 0.7 (0.6–0.9) | 0.001 |
| Hospital teaching status | ||||
| Nonteaching | Reference | Reference | ||
| Teaching | 1.3 (1.1–1.6) | <0.001 | 1.5 (1.2–1.9) | <0.001 |
Figure 4.
Discharge to home trend in patients undergoing CPR during 2005–2011, expressed in percentage. In the year 2011, 19% of patients with ESRD were discharged home as compared with 9% in the year 2005, P<0.001.
Discussion
In comparison with the general population, a higher proportion of patients on dialysis undergoing in-hospital CPR died during the hospitalization. The length of, and charges for, hospitalization were also higher in these patients and more of the patients on dialysis were discharged to nursing facilities (Tables 2 and 3). Despite high mortality, survival and discharge to home status were significantly better in 2011 compared with the previous years.
The present study confirms the previously published literature showing that dialysis status is associated with lower survival after CPR. In one study of 24 patients on dialysis, CPR events were studied between the years 1979 and 1990 in both in-hospital and affiliated outpatient dialysis unit settings.6 Eighteen patients (75%) were initially resuscitated successfully but only 11 patients (45.8%) were alive 24 hours after resuscitation, and two patients (8.3%) survived more than 1month, but none of them were alive at the time of hospital discharge. In a single-center study3 of 74 dialysis patients experiencing CPR in both outpatient dialysis and hospital settings, 37% were successfully resuscitated initially but only 6% survived to hospital discharge. The 26% survival to hospital discharge in the present study may be higher than the previously reported literature because only in-hospital CPR was studied and patients were excluded whose primary diagnosis was cardiopulmonary arrest. This methodology was used to exclude biases associated with in-the-field CPR. The study also comprises a much larger number of patients, which may account for some of the variability in the results.
Clearly, patients on dialysis may arrest in the dialysis unit during or after a hemodialysis treatment and others have reported on outcomes following CPR in dialysis units.1,3 In one study, survival of in-dialysis-unit CPR was around 15%.1 Although the cause of cardiopulmonary arrest in the dialysis unit versus the hospital may or may not differ, there are no contemporary studies of survival following in-dialysis-unit CPR. The present study’s data set could not capture CPR events in the dialysis units and additional studies are needed to address this issue.
Data from the general population indicate that survival after CPR is improving, probably as a result of better CPR techniques.7 The International Liaison Committee on Resuscitation and the American Heart Association guidelines for CPR and emergency cardiovascular care were changed in 2005 and reiterated in 2010. Changes included reducing the initial number of back-to-back rhythm analyses and shocks, eliminating rhythm and pulse checks immediately after each shock, increasing the ratio of chest compressions to ventilation from 15:2 to 30:2, and doubling the required period of CPR between successive rhythm evaluations.8,9 The observed higher survival in the present study is in large part due to changes in CPR technique that have led to a small but significant increase in overall survival among all in-hospital patients with ESRD who had received CPR. Despite this overall improved survival following in-hospital CPR, patients with ESRD continue to do poorly compared with the general hospital population (Table 1). This was previously shown in small, single-center studies3,4 and persists despite some overall improvement in post-CPR survival between 2005 and 2011. The poorer survival seen in patients with ESRD could be a result of high comorbidity burden (Table 1). However, survival did not improve after adjustment of age, gender, and comorbidities in the multivariate analysis, indicating a direct plausible effect of ESRD status. In the general population, advanced age is a predictor of failure to survive after in-hospital CPR.10 Interestingly, in our cohort, patients with ESRD were younger than the general population but still had higher mortality. In one large meta-analysis of survival after in-hospital CPR, sepsis on the day before resuscitation was a major risk factor for the poor CPR-related survival.11 In our cohort, more patients with ESRD had sepsis, which could be one explanation for their poor survival. We did not see a high frequency of rib fractures, which is a predictor of early termination of the CPR procedure.12 It could still be possible that medical professionals fear rib fractures in patients with ESRD because of concomitant bone disease and therefore CPR efforts are terminated earlier in patients on dialysis. Our data set does not provide information on CPR duration or on the cause of cardiorespiratory arrest, preventing further analysis. It could also be hypothesized that we have a negative bias toward the ESRD status in terms of survival outcomes which may affect our CPR efforts. In addition, our data set does not allow us to analyze the effect of cardio-protective medications such as β-blockers, calcium-channel blockers, and renin-angiotensin system blocking drugs, which have been shown to improve survival after cardiac arrest in patients on dialysis.13 More studies are needed to answer these questions, but prognostic information about poor survival needs to be discussed with patients on dialysis.
To our knowledge, improved CPR outcomes in patients with ESRD that are related to the time period in which the CPR was performed have not been previously described. Despite better survival in 2011 compared with 2005, overall CPR outcomes remain poor in patients on dialysis. Our two main outcomes, i.e., survival and discharge to home status, were better in 2011 compared with the previous years. Hence, the time-frame during which CPR outcomes were examined likely contributed to the differences in outcomes shown in our study compared with earlier, single-center reports.
In a subanalysis of outcome differences between patients with ESRD who were in intensive care units and those who were not, we observed higher odds of mortality and discharge to nursing homes in patients in intensive care units, which likely represents a sicker patient population. In a separate multivariate analysis between teaching and nonteaching hospitals, we found lower odds of discharge to nursing homes in teaching hospitals. There were no statistically significant differences in the rates of cardiac interventions between the teaching and nonteaching hospitals for cardiac angiography, cerebral angiography, coronary angioplasty, and coronary artery bypass grafting (data not shown). Although more research is needed on this issue as a whole, teaching hospitals have better outcomes than nonteaching hospitals for patients with breast cancer, cerebrovascular accidents, and mixed diagnoses.14
We found that a higher proportion of patients with ESRD were discharged to nursing facilities. Our study supports the previous literature illustrating progressive functional decline punctuated by episodes of acute hospitalization in dialysis patients.15 However, our findings differ from a single-center, United States-based, intensive care study in which chronic dialysis dependency was not a significant risk factor for discharge to nursing homes.16 As our study consists of a larger patient cohort over several years, the higher likelihood of discharge to a nursing facility in patients on dialysis surviving CPR is probably common and should be communicated with the patients and their families during CPR discussions.
Interestingly, rates of withdrawal of care were not significantly different between patients with ESRD and the general population after CPR (Table 2). However, within the cohort of patients with ESRD, withdrawal of care increased from 2005 to 2011 (Figure 4). This is a novel finding and may represent improved end-of-life care communication by the medical community.
Our study has several limitations as it is based on an administrative data set and relies on accuracy of coding. These limitations have been discussed elsewhere.17 For maintenance dialysis patient sensitivity and positive predictive values of International Classification of Disease, 9th Revision, Clinical Modification (ICD-9) codes are good but variable across studies (sensitivity median, 81%; positive predictive value median, 96%).18 We excluded patients with acute renal failure from the ESRD group and the ICD-9 code of AKI has a specificity of 90%.19 The sensitivity and specificity of CPR code is variable across hospitals but has been consistently used in the literature.20,21 Our findings of improved outcomes are consistent with the more recently published literature, lending reliability to our results. Our results do not provide information about patients’ functional status at the time of discharge. However, discharge to a nursing home correlates with poor functional status,22 suggesting more of the patients on dialysis had a poorer functional status upon discharge. It is important to understand that our study lacks information on other important CPR-related outcomes such as readmission rates, and survival at 1, 3, 6, and 12 months, which provide useful prognostic information. More studies are needed to address these issues. It is important to note that our CPR cohort only includes patients with ESRD who underwent in-hospital CPR. Our study findings cannot be generalized for the CPR-related outcomes in outpatient dialysis units.
Patients with ESRD also had higher mean hospital charges, which were directly associated with a longer hospital course. In this data set, total hospitalization charges represent the amount that hospitals billed for services, not how much hospital services actually cost or the specific amounts received in reimbursement. These charges include hospital overhead costs, charity care, and bad debt; physicians’ professional fees are not included.
Interestingly, although intubation and blood transfusions were more common among patients on dialysis, many interventions, such as cardiac procedures, were less common among these patients. The reasons for these differences are not discernible from the data but may suggest, as others have reported, that high comorbidity among patients with dialysis may lead to fewer interventions.23
In patients on dialysis, CPR events occurred more often in teaching hospitals, large hospitals, and in the south and west regions (Table 2). The reasons for these differences are unclear. However, healthcare intensity varies by geographic area24 and is higher among older adults initiating dialysis in the hospital.25 Post-CPR withdrawal of care was not statistically different in patients with ESRD compared with the general population, a finding which has not previously been reported.
Ours is the largest study aimed at analyzing the outcomes of in-hospital CPR in patients on maintenance dialysis. Our data are derived from a nationally representative sample and are devoid of institutional bias. Our results are therefore generalizable and provide important information to physicians engaged in advance care planning discussions with patients and families involving the usefulness of in-hospital CPR.
In summary, we observed higher odds of mortality and discharge to nursing home in patients on dialysis undergoing in-hospital CPR. In 2011, survival, discharge to home, and mean length of stay improved but nearly 74% of patients died in the hospital. Our study adds to the existing literature by providing more details about the contemporary success rates of CPR in a large sample of dialysis patients. These statistics can be used to facilitate complex and challenging patient/provider discussions on advance care planning involving choices for CPR in stable or acute situations in the hospital or intensive care settings. Additional studies are needed to analyze post-CPR quality of life and long-term outcomes.
Concise Methods
We obtained Institutional Review Board exempt status for the present study from the Cleveland Clinic Institutional Review Board committee. The analysis was based on data files from National Inpatient Sample (NIS), 2005–2011. A comprehensive synopsis on NIS data is available at http://www.hcup-us.ahrq.gov. NIS is the largest all-payer inpatient-care database created by the Agency for Healthcare Research and Quality. It contains yearly discharge data from more than 1000 short-term and non-Federal hospitals, which approximates a 20% stratified sample of United States hospitals. Each hospitalization is treated as an individual entry in the database and is coded with one principal diagnosis, up to 14 secondary diagnoses, and 15 procedural diagnoses associated with that stay. NIS encompasses information for all patients regardless of payer, including private insurance and the uninsured. It also includes hospital information: teaching or nonteaching, rural or urban, large or small volume and private or publicly owned. Discharge weights are provided to facilitate the projection of national estimates, along with information necessary to calculate the variance of estimates. Further details about discharge weights can be accessed at the website.
We used the ICD-9-CM primary or secondary procedure codes 99.60 to identify the adult patients (≥18 years) who underwent CPR. Patients who had cardiopulmonary arrest (427.50) as a primary diagnosis were excluded to avoid including patients who experienced an out-of-hospital event in our analysis.20 We also used the ICD-9-CM primary or secondary diagnosis code (585.6) to identify patients with ESRD and the procedure codes (54.98 for peritoneal dialysis and 39.95 for hemodialysis) to identify patients on dialysis. We excluded all cases with ICD-9-CM primary or secondary diagnosis codes of CKD III (585.3), IV (585.4), and V (585.5), unspecified CKD (585.9), AKI (585.6), and renal transplant (556.1–556.9, 996.81 and V42.0). Patients undergoing CPR were divided into two groups: dialysis and non-dialysis.
Study variables included patient age, gender, race/ethnicity; comorbidities obtained from Agency for Healthcare Research and Quality comorbidity data files including diabetes mellitus, hypertension, congestive heart failure, chronic lung disease, deficiency anemias (iron, B12 and folate deficiency related anemia, valvular heart disease, peripheral vascular disease, fluid and electrolyte disorders, liver disease, AIDS, obesity, paralysis, solid tumor without metastasis, metastatic cancer, alcohol abuse, and coagulopathy. ICD-9-CM secondary diagnosis codes were used to identify patients with atrial fibrillation (427.3), coronary artery disease (410–414), nicotine dependence (305.1), dementia (290.0–290.40, 294.1, and 331.0), malnutrition (260.0 and 263.9), hyperkalemia (276.6), and dyslipidemia (272.0). We used the Charlson Comorbidity26 Index to identify the burden of comorbid conditions (Table 1). This index uses 17 comorbid conditions with differential weighting and total scores ranging from 0 to 33, with higher scores representing greater comorbidity burden. In accordance with the previous literature,27 we excluded kidney disease when calculating the index because that was already included as patient characteristic. Patients were also categorized based on insurance status into Medicare/Medicaid, private/health maintenance organization, or no insurance.
The ICD-9-CM secondary diagnosis codes were used to identify patients with common hospitalization-associated complications such as myocardial ischemia (410.0–410.9), pneumonia (486, 481, 482.8, and 482.3), urinary tract infection (599.0, 590.9), sepsis (995.91, 996.64, 038, 995.92, and 999.3), deep venous thrombosis (451.1, 451.2, 451.81, 451.9, 453.1, 453.2, 453.8, and 453.9), stroke (430–437), cardiogenic shock (785.51), unstable angina (411.1 and 411.8), gastrointestinal bleeding (578.0–578.9), pneumothorax (512.0 and 512.9), rib fracture (807.00, 807.19), cardiac tamponade (423.3), persistent vegetative state (780.03), and pulmonary embolism (415.1). We used ICD-9-CM procedure code V66.7 (palliative care, end-of-life care, hospice care, or terminal care) to identify the patient who received “withdrawal of care”. This code has been validated previously and has sensitivity and specificity values of 81% and 97%, respectively.28
We also used procedure codes to estimate the percentage of patients who underwent in-hospital procedures such as cerebral angiography (88.41), cardiac catheterization (37.21–37.23), percutaneous transluminal coronary angioplasty (36.0 and 00.66), coronary artery bypass grafting (36.1), valvular repair (35.0–35.9), valvular replacement (35.2), intubation (96.04), tracheostomy (31.20–31.29), transfusion (99.04), induced hypothermia (99.81), and gastrostomy (431.1–431.9). Intensive care unit status was identified by using the following codes: mechanical ventilation (96.72), intubation (96.04), infusion of vasopressor agent (00.17), pulmonary artery pressure monitoring (89.63), pulmonary artery wedge monitoring (89.64), monitoring of cardiac output by oxygen consumption technique (89.67), monitoring of cardiac output by other technique (89.68), and arterial catheterization (38.91).
Hospitals were categorized by geographic region in the USA as Northeast, Midwest, West, and South. Facilities were considered teaching hospitals if they had an American Medical Association–approved residency program, were a member of the Council of Teaching Hospitals, or had a ratio of full-time-equivalent interns and residents to patients of 0.25 or higher. The hospitals were further characterized into small, medium, and large based on available hospital beds. Discharge status was categorized into home/self-care, nursing facility (including skilled nursing home, intermediate care facility, hospice, in-patient rehabilitation facility, long-term care hospital, transfer to another institute which is not specified), unknown, and in-hospital mortality.
The SAS 9.1 software (SAS Institute, Inc., Cary, NC) was used to convert NIS database data into weighted counts to generate national estimates, following Healthcare Cost and Utilization Project recommendations. We performed univariate analysis, chi-squared for categorical and t test for continuous variables to identify differences in study variables and endpoints between patients with or without ESRD. Two logistic regression models were created. Model one included all patients and logistic regression analysis was used to identify the association between ESRD and odds of in-hospital mortality. Model two included patients who were discharged alive and logistic regression analysis was used to identify the association between ESRD and odds of discharge to a nursing facility. The logistic regression model was adjusted for age (as a continuous variable), gender (as a categorical variable), and confounding factors (as a categorical variable). Confounding factors were defined as all the factors significant in univariate analysis based on a type I error of 0.05.
A logistic regression analysis was used to identify the association between patient and hospital characteristics and odds of “patients discharged to home”. All variables that were significant in the univariate analysis were added as “predictor variables” to a step-wise logistic regression model. These variables were retained in the final model if P value was <0.05. We performed a subanalysis comparing the CPR-related outcomes of patients with ESRD in teaching versus nonteaching hospitals and intensive care unit versus non-intensive care unit settings. Logistic regression analysis was used to identify the association between ESRD and odds of discharge to nursing facility and in-hospital mortality. The logistic regression model was adjusted in a similar fashion to that mentioned above. We also performed a trend analysis to determine any change in annual average survival rate, annual percentage of patients being discharged to nursing homes from 2005 through 2011 and any percent change in annual mean length of stay from 2005 through 2011. Analysis of the annual rates of withdrawal of care, using a Cochran–Armitage trend test was also performed.
Disclosures
None.
Acknowledgments
This research study was presented as a poster at the Annual Meeting of the American Society of Nephrology (November 11–16, 2014), in Philadelphia, PA.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
References
- 1.Davis TR, Young BA, Eisenberg MS, Rea TD, Copass MK, Cobb LA: Outcome of cardiac arrests attended by emergency medical services staff at community outpatient dialysis centers. Kidney Int 73: 933–939, 2008 [DOI] [PubMed] [Google Scholar]
- 2.Bleyer AJ, Russell GB, Satko SG: Sudden and cardiac death rates in hemodialysis patients. Kidney Int 55: 1553–1559, 1999 [DOI] [PubMed] [Google Scholar]
- 3.Moss AH, Holley JL, Upton MB: Outcomes of cardiopulmonary resuscitation in dialysis patients. J Am Soc Nephrol 3: 1238–1243, 1992 [DOI] [PubMed] [Google Scholar]
- 4.Lafrance JP, Nolin L, Senécal L, Leblanc M: Predictors and outcome of cardiopulmonary resuscitation (CPR) calls in a large haemodialysis unit over a seven-year period. Nephrol Dial Transplant 21: 1006–1012, 2006 [DOI] [PubMed] [Google Scholar]
- 5.Tzamaloukas AH, Murata GH, Avasthi PS: Outcome of cardiopulmonary resuscitation in patients on chronic dialysis. ASAIO Trans 37: M369–M370, 1991 [PubMed] [Google Scholar]
- 6.Lai M, Hung K, Huang J, Tsai T: Clinical findings and outcomes of intra-hemodialysis cardiopulmonary resuscitation. Am J Nephrol 19: 468–473, 1999 [DOI] [PubMed] [Google Scholar]
- 7.Girotra S, Nallamothu BK, Spertus JA, Li Y, Krumholz HM, Chan PS, American Heart Association Get with the Guidelines–Resuscitation Investigators : Trends in survival after in-hospital cardiac arrest. N Engl J Med 367: 1912–1920, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Field JM, Hazinski MF, Sayre MR, Chameides L, Schexnayder SM, Hemphill R, Samson RA, Kattwinkel J, Berg RA, Bhanji F, Cave DM, Jauch EC, Kudenchuk PJ, Neumar RW, Peberdy MA, Perlman JM, Sinz E, Travers AH, Berg MD, Billi JE, Eigel B, Hickey RW, Kleinman ME, Link MS, Morrison LJ, O’Connor RE, Shuster M, Callaway CW, Cucchiara B, Ferguson JD, Rea TD, Vanden Hoek TL: Part 1: executive summary: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 122[Suppl 3]: S640–S656, 2010 [DOI] [PubMed] [Google Scholar]
- 9.ECC Committee, Subcommittees and Task Forces of the American Heart Association : 2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 112[Suppl]: 1V-1–1V-5, 2005 [DOI] [PubMed] [Google Scholar]
- 10.Ebell MH, Afonso AM: Pre-arrest predictors of failure to survive after in-hospital cardiopulmonary resuscitation: a meta-analysis. Fam Pract 28: 505–515, 2011 [DOI] [PubMed] [Google Scholar]
- 11.Ebell MH, Becker LA, Barry HC, Hagen M: Survival after in-hospital cardiopulmonary resuscitation. A meta-analysis. J Gen Intern Med 13: 805–816, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moss AH: Informing the patient about cardiopulmonary resuscitation: when the risks outweigh the benefits. J Gen Intern Med 4: 349–355, 1989 [DOI] [PubMed] [Google Scholar]
- 13.Pun PH, Lehrich RW, Smith SR, Middleton JP: Predictors of survival after cardiac arrest in outpatient hemodialysis clinics. Clin J Am Soc Nephrol 2: 491–500, 2007 [DOI] [PubMed] [Google Scholar]
- 14.Papanikolaou PN, Christidi GD, Ioannidis JP: Patient outcomes with teaching versus nonteaching healthcare: a systematic review. PLoS Med 3: e341, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Holley JL: Palliative care in end-stage renal disease: illness trajectories, communication, and hospice use. Adv Chronic Kidney Dis 14: 402–408, 2007 [DOI] [PubMed] [Google Scholar]
- 16.Gehlbach BK, Salamanca VR, Levitt JE, Sachs GA, Sweeney MK, Pohlman AS, Charbeneau J, Krishnan JA, Hall JB: Patient-related factors associated with hospital discharge to a care facility after critical illness. Am J Crit Care 20: 378–386, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Qureshi AI, Chaudhry SA, Hassan AE, Zacharatos H, Rodriguez GJ, Suri MF, Lakshminarayan K, Ezzeddine MA: Thrombolytic treatment of patients with acute ischemic stroke related to underlying arterial dissection in the United States. Arch Neurol 68: 1536–1542, 2011 [DOI] [PubMed] [Google Scholar]
- 18.Vlasschaert ME, Bejaimal SA, Hackam DG, Quinn R, Cuerden MS, Oliver MJ, Iansavichus A, Sultan N, Mills A, Garg AX: Validity of administrative database coding for kidney disease: a systematic review. Am J Kidney Dis 57: 29–43, 2011 [DOI] [PubMed] [Google Scholar]
- 19.Waikar SS, Wald R, Chertow GM, Curhan GC, Winkelmayer WC, Liangos O, Sosa MA, Jaber BL: Validity of International Classification of Diseases, Ninth Revision, Clinical Modification Codes for Acute Renal Failure. J Am Soc Nephrol 17: 1688–1694, 2006 [DOI] [PubMed] [Google Scholar]
- 20.Kazaure HS, Roman SA, Sosa JA: Epidemiology and outcomes of in-hospital cardiopulmonary resuscitation in the United States, 2000–2009. Resuscitation 84: 1255–1260, 2013 [DOI] [PubMed] [Google Scholar]
- 21.Ehlenbach WJ, Barnato AE, Curtis JR, Kreuter W, Koepsell TD, Deyo RA, Stapleton RD: Epidemiologic study of in-hospital cardiopulmonary resuscitation in the elderly. N Engl J Med 361: 22–31, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Qureshi AI, Chaudhry SA, Sapkota BL, Rodriguez GJ, Suri MF. Discharge destination as a surrogate for Modified Rankin Scale defined outcomes at 3- and 12-months poststroke among stroke survivors. Arch Phys Med Rehabil 93(8): 1408–1413.e1, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chertow GM, Normand SL, McNeil BJ: “Renalism”: inappropriately low rates of coronary angiography in elderly individuals with renal insufficiency. J Am Soc Nephrol 15: 2462–2468, 2004 [DOI] [PubMed] [Google Scholar]
- 24.O’Hare AM, Rodriguez RA, Hailpern SM, Larson EB, Kurella Tamura M: Regional variation in health care intensity and treatment practices for end-stage renal disease in older adults. JAMA 304: 180–186, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wong SP, Kreuter W, O’Hare AM: Healthcare intensity at initiation of chronic dialysis among older adults. J Am Soc Nephrol 25: 143–149, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Deyo RA, Cherkin DC, Ciol MA: Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45: 613–619, 1992 [DOI] [PubMed] [Google Scholar]
- 27.Kumar G, Sakhuja A, Taneja A, Majumdar T, Patel J, Whittle J, Nanchal R, Milwaukee Initiative in Critical Care Outcomes Research (MICCOR) Group of Investigators : Pulmonary embolism in patients with CKD and ESRD. Clin J Am Soc Nephrol 7: 1584–1590, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Qureshi AI, Adil MM, Suri MF: Rate of utilization and determinants of withdrawal of care in acute ischemic stroke treated with thrombolytics in USA. Med Care 51: 1094–1100, 2013 [DOI] [PubMed] [Google Scholar]