Abstract
The Social Phobia Inventory (SPIN; Connor et al., 2000) is a well-validated instrument for assessing severity of Social Anxiety Disorder (SAD). However, evaluations of its factor structure have produced inconsistent results and this aspect of the scale requires further study. Primary care patients with SAD (N = 397) completed the SPIN as part of baseline assessment for the Coordinated Anxiety Learning and Management study (Roy-Byrne et al., 2010). These data were used for exploratory and confirmatory factor analysis of the SPIN. A 3-factor model provided the best fit for the data and factors were interpreted as Fear of Negative Evaluation, Fear of Physical Symptoms, and Fear of Uncertainty in Social Situations. Tests of a second-order model showed that the three factors loaded strongly on a single higher-order factor presumed to reflect Social Anxiety. Findings are consistent with theories identifying fear of negative evaluation as the core feature of SAD, and with evidence that anxiety sensitivity and intolerance of uncertainty further contribute to SAD severity.
Keywords: Social Anxiety Disorder, Social Phobia, Assessment, Exploratory Factor Analysis, Confirmatory Factor Analysis
Graphical Abstract
1. Introduction
Social Anxiety Disorder (SAD; previously called “Social Phobia”) is a common, distressing, and disabling disorder (Ruscio et al., 2008; Sherbourne et al., 2010; Stein & Kean, 2000; Stein & Stein, 2008). Fear of negative evaluation is conceptualized as a core feature of SAD and is required for diagnosis (American Psychiatric Association, 2013; Heimberg et al., 2014). This concern may lead to fear and avoidance of a wide variety of social and performance situations (e.g., public speaking, interacting with authority figures, conversing with unfamiliar people). When exposed to a feared situation, individuals with SAD may experience physiological arousal and symptoms that they believe will be detected by other people such as blushing, sweating, and trembling. The fear, avoidance, and physiological symptoms associated with SAD can lead to substantial disruption of occupational/school and interpersonal functioning and diminished quality of life (Hendriks et al., 2014; Sherbourne et al., 2010; Stein & Kean, 2000).
A comprehensive assessment of SAD includes a clinical interview, behavioral assessment, and administration of self-report scales (McCabe, Ashbaugh, & Antony, 2010). Many self-report scales have been developed for the purpose of evaluating the severity of SAD symptoms. One that is commonly used in clinical research is the Social Phobia Inventory (SPIN; Connor et al., 2000), a 17-item scale that asks respondents to rate the severity of their general concerns about being criticized or embarrassed, fear and avoidance of specific social situations, and distress about physical symptoms commonly associated with SAD.
Psychometric studies of the SPIN have indicated favorable internal consistency, test-retest reliability, convergent validity, discriminant validity, and sensitivity to clinical change (Antony, Coons, McCabe, Ashbaugh, & Swinson, 2006; Connor et al., 2000). However, evaluations of the SPIN's factor structure have produced inconsistent results (Caballo, Salazar, Irurtia, Arias, & Nobre, 2013; Carleton, Collimore, Asmundson, et al., 2010; Connor et al., 2000; Osorio, Crippa, & Loureiro, 2010; Radomsky et al., 2006). The scale authors originally posited that the scale would assess 3 dimensions: fear, avoidance, and physiological arousal. Contrary to this prediction, a principal components analysis (PCA) of their own data from 148 respondents diagnosed with SAD identified 5 components, which they conceptualized as fears of: talking to strangers, criticism and embarrassment, physiological changes, authority figures, and public speaking/being the center of attention (Connor et al., 2000). A later PCA of the SPIN (Brazilian Portuguese translation) based on data from 88 university students diagnosed with SAD also found a 5-component structure (Osorio et al., 2010); however, composition of the components differed from that reported by Connor et al.
Subsequent investigators have pointed out the limitations of the PCA approach (Carleton, Collimore, Asmundson, et al., 2010) and have used exploratory factor analysis (EFA) and confirmatory factor analysis (CFA) to evaluate the scale's structure. One CFA based on data from a non-clinical, undergraduate sample found support for the 3-factor structure that was originally hypothesized by the scale authors (Radomsky et al., 2006). However, attempts to confirm this 3-factor structure [or the 5-factor structure suggested by Connor et al.'s (2000) PCA] in other undergraduate samples were unsuccessful (Caballo et al., 2013; Carleton, Collimore, Asmundson, et al., 2010). Moreover, Carleton et al. reported that neither of those models provided a good fit for data from a clinical sample of 355 respondents diagnosed with SAD.
Given these results, Carleton et al. (2010) conducted a rigorous EFA using a randomly selected subsample of their clinical respondents. They applied strict criteria for item retention, and 7 of the 17 SPIN items were eliminated due to either low communalities (<.40) or salient cross-loadings (≥.32). All items referring to physiological symptoms were dropped at this stage. The remaining items loaded onto 3 factors described as “Fear/Avoidance”, “Criticism/Embarrassment”, and “Authority”. With some well-justified modifications (e.g., correlating the error terms between similarly worded items), this 3-factor model was confirmed in both the other half of the clinical sample and in the undergraduate sample. The revised 10-item SPIN (SPIN-R) correlated very strongly with the original SPIN (r = .95).
The methods used by Carleton et al. (2010) were well-justified; however, a few limitations of that investigation should be addressed. First, the final factor structure of the SPIN-R included one factor (“Authority”) that was comprised of only 2 items with very similar wording. The validity of a latent factor with those attributes is questionable (Brown, 2015; Costello & Osborne, 2005). CFA allows for detection and modeling of covariance among items that is attributable to sources other than a shared latent factor; in this case, the possibility of a method effect due to similar item wording should be considered (Brown, 2015; Campbell-Sills & Brown, 2005). Second, although Carleton et al. pointed out that redundant items may be a problem for the SPIN, the SPIN-R retained several redundant items and instead dropped items with unique content (e.g., those related to physical manifestations of anxiety; public speaking). Moreover, the removal of the items assessing distress related to physical symptoms may diminish the construct validity and clinical utility of the scale. Concern about physical symptoms is a prominent aspect of the clinical presentation in some cases of SAD and has implications for treatment planning. Therefore, retention of items assessing that domain would be clinically useful. Finally, the clinical sample in the Carleton et al. investigation included only respondents with principal diagnoses of generalized SAD who presented to a specialty anxiety treatment and research center. A sample that also includes individuals presenting with SAD that is more circumscribed in its focus (i.e., “non-generalized”) and with SAD that is secondary to other principal disorders would be more representative of the larger clinical population of socially anxious individuals.
The Coordinated Anxiety Learning and Management (CALM) study is a randomized, controlled, effectiveness trial of a collaborative care intervention for anxiety disorders in primary care (Craske et al., 2011; Roy-Byrne et al., 2010; Sullivan et al., 2007). The sample recruited for CALM was large and demographically diverse. A diagnosis of SAD, generalized anxiety disorder (GAD), panic disorder (PD), or posttraumatic stress disorder (PTSD) was required for inclusion in the study; however, many other mental disorder diagnoses were represented (e.g., the majority of participants had co-occurring mood disorders; Roy-Byrne et al., 2010). All participants with a principal or additional diagnosis of SAD completed the SPIN as part of their baseline assessment; this affords a valuable opportunity for further evaluation of the scale's factor structure in a clinical sample.
2. Method
2.1. Participants
During the period of June 2006 through April 2008, the CALM study enrolled 1,004 patients from 17 primary care clinics located in or near Seattle, WA; Los Angeles, CA; San Diego, CA; and Little Rock, AR (for more information on the CALM study design and primary outcomes, see Sullivan et al., 2007 and Roy-Byrne et al., 2008, respectively). Participants were referred to the study by their primary care provider; in some clinics, referral was facilitated by the use of a 5-item anxiety screening instrument (Means-Christensen, Sherbourne, Roy-Byrne, Craske, & Stein, 2006). All participants provided informed consent to participate, and the study protocol was approved by the Internal Review Boards of all participating institutions (University of Washington, University of California Los Angeles, University of California San Diego, University of Arkansas for Medical Sciences, and RAND Corporation).
Referred patients were included in the CALM study if they were aged 18-75, spoke either English or Spanish, met DSM-IV diagnostic criteria for GAD, PD, PTSD, or SAD, and scored 8 or higher on the Overall Anxiety Severity and Impairment Scale (OASIS; Campbell-Sills et al., 2009). Patients were excluded if they were actively suicidal; met criteria for psychotic, Bipolar I, or substance use disorders (except alcohol and marijuana abuse, which were permitted). Patients with unipolar mood disorders were not excluded unless they indicated that were not interested in treatment focused on their anxiety. The current analysis utilizes data from participants who met criteria for SAD and thus completed the SPIN at the baseline assessment. A total of 403 CALM participants completed the SPIN; however, a small proportion (1.5%; n = 6) had incomplete data and were excluded from the current analysis. Table 1 presents the demographic and diagnostic characteristics of the final 397 participants.
Table 1.
Demographic and clinical characteristics of the study sample (N = 397)
| Characteristics | No. (%) of Participants1 |
|---|---|
| Age, mean (SD) | 40.81 (12.69) |
| Gender | |
| Female | 281 (70.8%) |
| Male | 116 (29.2%) |
| Education2 | |
| < High school | 25 (6.3%) |
| 12 years | 63 (15.9%) |
| > 12 years | 307 (77.3%) |
| Race/Ethnicity | |
| Hispanic | 87 (21.9%) |
| African American | 47 (11.8%) |
| White | 210 (52.9%) |
| Other | 53 (13.4%) |
| Marital status | |
| Married/Cohabiting | 192 (48.4%) |
| Not married/cohabiting | 205 (51.6%) |
| Co-occurring disorders | |
| Panic Disorder | 182 (45.8%) |
| Generalized Anxiety Disorder | 284 (71.5%) |
| Posttraumatic Stress Disorder | 79 (19.9%) |
| Major Depressive Disorder | 275 (69.3%) |
| SPIN score, mean (SD) | 38.34 (13.34) |
Note. SD = standard deviation; SPIN = Social Phobia Inventory.
For continuous measures, mean (SD) is reported in lieu of No. (%)
Two participants had missing education data and thus category values do not total 397.
2.2. Measures
Diagnoses were established according to DSM-IV criteria using the Mini International Neuropsychiatric Interview (MINI), version 5.0 (Sheehan et al., 1998). Reliability and validity of anxiety and mood disorder diagnoses obtained with the MINI is satisfactory (Sheehan et al., 1998). The MINI was administered by one of the CALM study's Anxiety Clinical Specialists, who received formal training in MINI administration (including diagnostic reliability testing) and ongoing assessment supervision with a study psychologist or psychiatrist.
The focus of this study is the 17-item SPIN (Connor et al., 2000), which measures fear, avoidance, and distress related to physical symptoms associated with SAD. Items of the SPIN are paraphrased in Table 2. Each item is rated on a scale from “not at all” to “extremely” (0 to 4) with a reference timeframe of the past week. Prior investigations indicate that the SPIN has good to excellent internal consistency, test-retest reliability, convergent validity, discriminant validity, and sensitivity to clinical change (Antony et al., 2006; Connor et al., 2000).
Table 2.
Latent structure of 16 retained items of the Social Phobia Inventory (SPIN): Exploratory factor analysis in subsample 1 (n = 200)
| Promax-rotated factor loadings | |||||
|---|---|---|---|---|---|
| SPIN Item | Paraphrased Item Content | Item mean (0-4) | Fear of Negative Evaluation | Fear of Physical Symptoms | Fear of Uncertainty in Social Situations |
| 15 | Fear of embarrassment/looking stupid | 2.65 | .877 | −.031 | −.148 |
| 5 | Scared of criticism | 2.55 | .830 | −.088 | −.041 |
| 12 | Do anything to avoid criticism | 2.37 | .713 | −.036 | .036 |
| 6 | Avoid doing things for fear of embarrassment | 2.60 | .706 | .098 | .018 |
| 16 | Avoid speaking to authority figures | 1.75 | .640 | .038 | −.010 |
| 14 | Fear of doing things with others watching | 2.30 | .567 | .159 | .110 |
| 1 | Afraid of people in authority | 1.51 | .559 | −.012 | .114 |
| 17 | Distressed by trembling | 2.04 | −.096 | .814 | −.022 |
| 7 | Distressed by sweating | 1.72 | .071 | .684 | −.025 |
| 13 | Bothered by heart palpitations | 1.84 | −.094 | .601 | .224 |
| 2 | Bothered by blushing | 1.40 | .309 | .470 | −.182 |
| 8 | Avoid parties | 2.45 | −.233 | .001 | .977 |
| 3 | Scared of parties | 2.38 | .113 | −.012 | .761 |
| 4 | Avoid unfamiliar people | 2.41 | .269 | −.045 | .542 |
| 9 | Avoid being center of attention | 2.90 | .155 | .068 | .487 |
| 10 | Scared to talk to strangers | 1.85 | .370 | .043 | .454 |
Note. Primary factor loadings are in bold; a minimum loading of .35 was considered salient. Salient cross-loadings are italicized.
Two additional self-report measures were used for tests conducted to assess the validity of our interpretations of latent variables. These were the Anxiety Sensitivity Index (ASI; Reiss, Peterson, Gursky, & McNally, 1986), which measures fear of anxiety symptoms and their consequences; and the Generalized Anxiety Disorder Severity Scale (GADSS) which measures severity of worry and other symptoms of generalized anxiety (Shear, Belnap, Mazumdar, Houck, & Rollman, 2006). Both of these measures have demonstrated satisfactory reliability and validity in adult samples with anxiety disorders (Andreescu et al., 2008; Reiss et al., 1986; Shear et al., 2006).
2.3. Statistical Analysis/Design of the Current Study
We first conducted EFA in a randomly selected subsample of participants, as we could not justify moving straight to CFA given the inconsistency of prior findings. Following EFA, we conducted CFA in the remaining participants. We hypothesized that, in order to achieve good model fit, correlated error would need to be specified for SPIN items with similar wording. To evaluate this possibility, a CFA model without correlated error was specified and modification indices were inspected to identify localized points of ill fit. A sequential approach to refining the CFA model was then taken, in which only the path associated with the largest modification index was freed and the model re-evaluated before any further refinements were made (Brown, 2015; Campbell-Sills & Brown, 2005; Joreskog, 1993). In the event that we found a structure with 3 or more factors, we planned to use CFA to evaluate the hypothesis that these factors would load onto a higher-order factor representing the construct of Social Anxiety.
The random subsample for EFA was generated in SPSS (version 20.0) by using the “Random sample of cases” option within the “Select Cases” function, and specifying a desired sample of approximately 50% of all cases. Pearson's chi-square and t-tests were conducted to evaluate whether the EFA subsample (n = 200) differed from the CFA subsample (n = 197) on demographic or clinical characteristics. For both EFA and CFA, the sample variance-covariance matrices were analyzed using Mplus 3 (Muthén & Muthén, 2004). Maximum likelihood estimation and promax rotation were used. Overall fit of EFA models was evaluated using the root-mean-square error of approximation (RMSEA) and the root-mean-square residual (RMR). Fit of CFA models was evaluated using the root-mean-square error of approximation (RMSEA), standardized root-mean-square residual (SRMR), and comparative fit index (CFI). The chi-square test is reported for the EFA and CFA models, but not relied upon to evaluate model fit due to its oversensitivity to sample size and the fact that it tests for perfect fit. The selected fit indices provide different types of information (i.e., absolute fit, fit adjusting for model parsimony, fit relative to a null model), and when combined they provide a reliable and conservative evaluation of model fit (Jaccard & Wan, 1996). Final acceptance or rejection of models was based on joint consideration of: conventional criteria for good model fit (RMSEA close to or below .06, SRMR close to or below .08; CFI close to or above .95) (Hu & Bentler, 1999), strength of parameter estimates (i.e., primary factor loadings ≥ .35, few cross-loadings ≥ .35), and conceptual interpretability of the solution.
3. Results
3.1. Preliminary analysis
Random assignment of individual cases to groups for use in EFA and CFA resulted in two subsamples that were comparable on demographic and clinical variables. There were no significant differences between subsamples 1 and 2 with respect to age, gender, race/ethnicity, education level, marital status, co-occurring diagnoses (PD, GAD, PTSD, MDD), or total SPIN score (all ps > .30).
3.2. Exploratory factor analysis
EFA was conducted with a range of 1 to 6 factors specified. Eigenvalues > 1 for the unrotated correlation matrix were 7.00, 1.66, and 1.52 (next highest eigenvalues = 0.99 and 0.87). Although the Kaiser-Guttman rule and scree plot suggested the presence of 3 factors, we did not rely on these indices for model selection and examined fit statistics and pattern matrices for all models.
The 6-factor model did not converge on a valid solution. The 5-factor model provided good overall fit for the data but had other problematic features (e.g., several factors defined by <3 items; multiple salient cross-loadings). The 4-factor model provided reasonable overall fit [Χ2 (74) = 172.68, p < .001; RMSEA = 0.082 (90% CI 0.066-0.098); RMR = .038] and had no cross-loading items, but included a factor comprised of just 2 items related to speaking with authority figures (items 1 and 16). We had hypothesized that spurious factors might emerge as a result of similar wording, and planned to address this in CFA through specification of correlated error between such items. We therefore rejected the 4-factor model due to the likelihood that one factor was an artifact of highly similar item wording.
Of the remaining models, the 3-factor model provided the best fit for the data [Χ2 (88) = 240.30, p < .001; RMSEA = 0.093 (90% CI 0.079-0.107); RMR = .048)]. The RMR indicated good absolute fit; however, the RMSEA suggested less satisfactory fit when a parsimony correction was imposed. All SPIN items except one had salient loadings on one of the three factors (all primary loadings ≥ .45), with one item displaying a modest cross-loading of .36. The item without a salient loading assessed avoidance of giving speeches and had the highest mean score of all SPIN items (3.04; indicating an average of “very much”). Given the absence of a salient loading (maximum loading = .26) – and because restricted range was a problem in this socially anxious sample – we decided to drop item 11 and repeat the analysis.
When the 16 retained SPIN items were subjected to EFA, eigenvalues > 1 for the unrotated correlation matrix were 6.65, 1.65, and 1.51 (next highest eigenvalues = 0.93 and 0.87). The Kaiser-Guttman rule and scree plot thus suggested the presence of 3 latent factors; examination of fit statistics and pattern matrices also favored a 3-factor model. Fit was comparable to that of the 3-factor model based on all 17 SPIN items [Χ2 (75) = 215.70, p < .001; RMSEA = 0.097 (90% CI 0.082-0.112); SRMR = .048]. The 3 factors were interpreted as representing Fear of Negative Evaluation (items 1, 5, 6, 12, 14, 15, 16), Fear of Physical Symptoms (items 2, 7, 13, and 17), and Fear of Uncertainty in Social Situations (3, 4, 8, 9, 10). Item means and item-factor loadings are displayed in Table 2. Correlations among the 3 factors ranged from .47 to .56, supporting examination of a higher-order factor structure in CFA.
3.3. Confirmatory factor analysis
The second subsample (n = 197) was used for CFA. Based on the EFA results, we specified a 3-factor model with paths from the Fear of Negative Evaluation factor to items 1, 5, 6, 12, 14, 15, and 16; from Fear of Physical Symptoms to items 2, 7, 13, and 17; and from Fear of Uncertainty in Social Situations to items 3, 4, 8, 9, and 101. The factors were permitted to inter-correlate. We expected that paths would need to be freed between the residuals of similarly worded items in order to achieve good CFA model fit. Indeed, the 3-factor model with no correlated error did not fit the data well [Χ2 (101) = 367.08, p < .001; RMSEA = 0.12 (90% CI 0.10-0.13); SRMR = .076; CFI = .83] and modification indices (MIs) indicated several points of strain in the model pertaining to items with similar wording.
Based on our error theory and corroborating evidence from modification indices, we sequentially freed paths between the residuals of items 1 and 16, items 4 and 10, items 5 and 12, and items 3 and 8. Statistics for the revised model indicated satisfactory model fit [Χ2 (97) = 194.08, p < .001; RMSEA = 0.071 (90% CI 0.057-0.086); SRMR = .062; CFI = .94]. All items had salient loadings on their respective factors (.39-.82) and correlations among the residuals of similarly worded items were significant (ps < .01). Factor determinacies were good (.90-.94) and factor correlations were large (.58-.71). Modification indices did not suggest any further points of strain in this model.
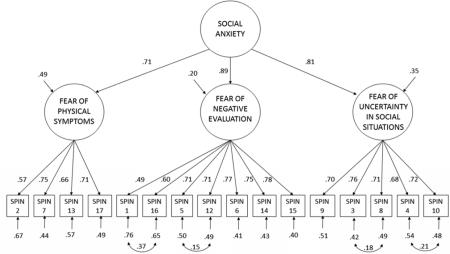
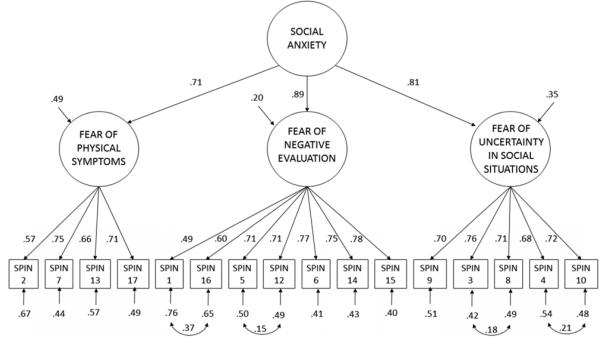
We next tested a second-order CFA model with a path from the posited higher-order factor (Social Anxiety) to the 3 lower-order factors. Although this model is just-identified (i.e., statistical fit is identical to that of the model with 3 inter-correlated factors), we felt it was substantively meaningful to estimate the magnitude and significance of the higher-order factor loadings as well as the relationship of the higher-order Social Anxiety factor to the SPIN items. Results showed that the determinacy of the Social Anxiety factor was good (.90). Fear of Negative Evaluation, Fear of Physical Symptoms, and Fear of Uncertainty in Social Situations loaded strongly on the higher-order Social Anxiety factor (loadings = .90, .74, and .79, respectively; ps < .001).
To further assess the hierarchical structure, we examined the magnitude of factor loadings of the individual SPIN items on the higher-order Social Anxiety factor. A Schmid-Leiman transformation was conducted to obtain residualized loadings between the items and their corresponding lower-order factors, after partialling out variance explained by Social Anxiety (Brown, 2015). Results suggested that the higher-order factor explained substantial variance in all SPIN items (factor loadings = .35-.70). Residualized primary loadings of items that comprised the Fear of Physical Symptoms and Fear of Uncertainty in Social Situations factors remained in the salient range (.37-.50). However, residualized loadings of the Fear of Negative Evaluation items dropped below the salient range (.17-.33), suggesting that Fear of Negative Evaluation did not explain unique salient variance in the items once the variance attributable to Social Anxiety was accounted for. An important caveat is that the Schmid-Leiman transformation gives explanatory preference to the higher-order factor. The very high correlation between the Fear of Negative Evaluation and Social Anxiety factors also must be considered in interpreting these results (see section 4).
The final second-order CFA model was re-tested in the full sample of 397 in order to obtain the most accurate parameter estimates (see Figure 1). Fit statistics were similar to those obtained with subsample 2 [Χ2 (97) = 286.48, p < .001; RMSEA = 0.070 (90% CI 0.061-0.080); SRMR = .053; CFI = .94]. Factor determinacies were comparable (.89-.94), and all parameter estimates were statistically significant (see Figure 1). The higher-order and residualized primary factor loadings of all retained items are presented in Table 3.
Figure 1.
Completed standardized solution of the confirmatory factor analysis (CFA) model in the full sample (N = 397). All parameter estimates shown are statistically significant (p's < .001).
Table 3.
Higher-order factor loadings and residualized primary loadings of the 16 retained SPIN items in the total sample (N = 397)
| Residualized primary loadings | |||||
|---|---|---|---|---|---|
| SPIN Item | Paraphrased Item Content | Social Anxiety (Higher-order factor loading) | Fear of Negative Evaluation | Fear of Physical Symptoms | Fear of Uncertainty |
| 15 | Fear of embarrassment/looking stupid | .69 | .35 | ||
| 5 | Scared of criticism | .63 | .32 | ||
| 6 | Avoid doing things for fear of embarrassment | .68 | .34 | ||
| 12 | Do anything to avoid criticism | .63 | .32 | ||
| 16 | Avoid speaking to authority figures | .53 | .27 | ||
| 14 | Fear of doing things with others watching | .67 | .34 | ||
| 1 | Afraid of people in authority | .44 | .22 | ||
| 17 | Distressed by trembling | .51 | .50 | ||
| 7 | Distressed by sweating | .53 | .52 | ||
| 13 | Bothered by heart palpitations | .47 | .46 | ||
| 2 | Bothered by blushing | .41 | .40 | ||
| 8 | Avoid parties | .57 | .42 | ||
| 3 | Scared of parties | .61 | .45 | ||
| 4 | Avoid unfamiliar people | .55 | .40 | ||
| 9 | Avoid being center of attention | .56 | .42 | ||
| 10 | Scared to talk to strangers | .58 | .43 | ||
Note. Loadings of SPIN items on their corresponding lower-order factors were transformed using the Schmid-Leiman procedure.
3.4. Validation of Subscales
The proposed subscales displayed good internal consistency (Cronbach's alpha = .87, .77, and .86 for Fear of Negative Evaluation, Fear of Physical Symptoms, and Fear of Uncertainty in Social Situations, respectively). Two measures were available that permitted preliminary validation of our interpretations of the latent factors. We first tested the prediction that ASI scores would correlate more strongly with Fear of Physical Symptoms than with the other two factors. The correlation of ASI with Fear of Physical Symptoms (r = .61) was indeed significantly larger than its correlation with Fear of Negative Evaluation (r = .42; z = 6.49, one-tailed p < .001 for test of difference between two dependent correlation coefficients; Steiger, 1980) and Fear of Uncertainty in Social Situations (r = .33; z = 4.95, one-tailed p < .001). Intolerance of uncertainty was not measured in the CALM study, but this construct has been found to relate significantly to GAD severity. We thus tested the prediction that GADSS scores would correlate more strongly with Fear of Uncertainty in Social Situations than with the other two factors. The correlation of GADSS with Fear of Uncertainty in Social Situations (r = .49) was significantly larger than its correlation with Fear of Negative Evaluation (r = .41; z = 1.71, one-tailed p < .05) and Fear of Physical Symptoms (r = .39; z = 1.87, one-tailed p < .05).
4. Discussion
The current study adds to the literature on the psychometric properties of the Social Phobia Inventory (Connor et al., 2000); providing evidence that the SPIN items assess multiple latent dimensions that contribute to defining the broader construct of social anxiety. Specifically, we found evidence that the SPIN items capture: (1) fear of negative evaluation, (2) distress related to physical symptoms of anxiety, and (3) fear of uncertainty in social situations.
The overall approach to factor analysis in the current study was to emphasize conceptual interpretability of the EFA and CFA solutions as much as statistical fit. The first retained factor was interpreted as representing the latent variable “Fear of Negative Evaluation”. It was comprised of items assessing fear and avoidance of criticism or embarrassment, as well as items assessing fear and avoidance of doing things while being observed and of interacting with authority figures. While not stated overtly, the possibility of being evaluated (negatively or otherwise) is implied in scenarios that involve working while being observed or interacting with authority figures. Thus, this factor appeared conceptually coherent and well-defined by a diverse range of items that addressed this theme both explicitly (item 5, 6, 12, and 15) and implicitly (items 1, 14, and 16).
Fear of negative evaluation features prominently in theoretical accounts of social anxiety (Clark & Wells, 1995; Hofmann & Barlow, 2002; Rapee & Heimberg, 1997). Consensus regarding the centrality of this construct to SAD led to revision of the diagnostic criteria for SAD in DSM-5 to explicitly state, “The individual fears that he or she will act in a way or show anxiety symptoms that will be negatively evaluated” (American Psychiatric Association, 2013). Members of the DSM-5 anxiety disorders sub-workgroup explained that the revised definition refers to “negative evaluation” because this term encompasses not only embarrassment and humiliation (the focus of the corresponding criterion in DSM-IV), but also rejection and offending others, which can be concerns of individuals with SAD (Heimberg et al., 2014). In line with conceptualizations of fear of negative evaluation being a key feature of SAD, this factor explained the largest proportion of variance in the SPIN items in EFA and displayed the strongest relationship with the higher-order factor representing Social Anxiety in CFA.
The second retained factor was labeled Fear of Physical Symptoms. This factor was coherent in that all items referred to physical manifestations of anxiety. A latent dimension representing Fear of Physical Symptoms is conceptually plausible from multiple standpoints. It converges with clinical consensus that individuals with SAD vary in the extent to which their concerns center on physical symptoms that could either disrupt their performance or be noticeable to others in social situations. Empirical work further suggests that the physical symptoms associated with SAD impact overall disorder severity; for example, patients with SAD who endorse situational panic attacks report increased fear, avoidance, distress, and impairment compared to patients with SAD who do not report situational panic (Jack, Heimberg, & Mennin, 1999). The Fear of Physical Symptoms factor likely captures anxiety sensitivity, which is most commonly associated with panic disorder but also has been posited to play a role in SAD (Clark & Wells, 1995; Wells & Papageorgiou, 2001). Indeed, this factor displayed the strongest association with scores on the ASI. Finally, Fear of Physical Symptoms relates discernably to self-focused attention, which is understood to contribute to SAD (Clark & Wells, 1995; Hofmann & Barlow, 2002) and includes monitoring of both physical reactions and outward behaviors.
The third factor was the least straightforward to interpret; we ultimately labeled it Fear of Uncertainty in Social Situations. It was comprised of items assessing fear and avoidance of parties, strangers, and being the center of attention. We hypothesized that a unique and unifying aspect of these situations was a higher-than-usual degree of unpredictability with respect to how the social situation would unfold. Parties, interactions with unfamiliar people, and being the center of attention are contexts in which the novelty and variety of others (conversational partners, observers or audience members) may contribute to anxiety. For instance, at parties the person with SAD might anticipate encountering unfamiliar people whose behavior would exacerbate their anxiety (e.g., conversational partners who ask many personal questions, or who are extremely shy themselves) or whose reactions are unexpectedly negative (e.g., misinterpreting or taking offense to comments made by the subject). These more unpredictable situations contrast with social encounters in familiar settings with known others (e.g., interactions with close friends or co-workers), which in their regularity are more predictable and thereby anxiety-reducing.
This third latent variable may relate to the well-established construct Intolerance of Uncertainty (IU), which has been conceptualized as a trans-diagnostic risk factor for anxiety disorders (Carleton, 2012) and incorporated into recent theoretical accounts of SAD (Teale Sapach, Carleton, Mulvogue, Weeks, & Heimberg, 2015). Notably, IU has been shown to predict social anxiety severity even after controlling for fear of negative evaluation (Boelen & Reijntjes, 2009; Carleton, Collimore, & Asmundson, 2010; Teale Sapach et al., 2015). In the current study, Fear of Uncertainty in Social Situations displayed a stronger relationship than the other SPIN factors to GAD severity, a domain that has a long-established association with IU (Dugas et al., 2005).
While the 3-factor model provided the best fit for the current data, it is possible that other important latent dimensions of Social Anxiety exist but are not adequately represented by the SPIN items. For instance, there may in fact be a distinct latent variable underlying fears that arise in relation to authority figures. While other studies have retained a separate “Authority” factor defined by two items, we found that the two authority items had statistically significant and salient loadings on the Fear of Negative Evaluation factor, as well as additional covariance that was modeled by correlating the items’ residuals. Though we believe that this model is more defensible than one that posits a distinct latent factor based on two similarly worded items, it is notable that the latent variables in the current model explained relatively low proportions of variance in these two items (R2 = .24 and .35). However, in order for a stable and valid factor to emerge, the SPIN would need more items assessing the unique dimension hypothesized to underlie fears and avoidance of authority figures.
A final observation is that the item assessing avoidance of public speaking did not load on any of the three factors in our model. This was likely due to restricted range in this clinical sample, whose participants’ average response indicated “very much” avoidance of giving speeches. While this item was eliminated for the purpose of model testing, we do not necessarily advocate dropping this item from the SPIN as it may be clinically relevant to measure change in this item.
4.1. Higher-order CFA
A second-order CFA was conducted to test whether the correlations among the 3 latent dimensions could be explained by a single higher-order factor representing Social Anxiety. This model allowed for estimation of the relative contributions of Fear of Negative Evaluation, Fear of Physical Symptoms, and Fear of Uncertainty in Social Situations to defining the broader construct of Social Anxiety. Results showed that each of the 3 factors loaded strongly (>.70) on Social Anxiety. Indeed, the association between the latent Fear of Negative Evaluation and Social Anxiety factors (.89 in the full sample) raises the question of whether these constructs can be reliably discriminated. Moreover, once variance explained by the higher-order Social Anxiety factor was accounted for, the unique variance in SPIN items explained by the Fear of Negative Evaluation factor fell below the salient range. The overlap between Fear of Negative Evaluation and Social Anxiety admittedly complicates interpretation of the CFA findings, but is not unexpected given that SAD is largely defined by fear of negative evaluation. From face validity and clinical utility standpoints, we still advocate use of the SPIN items in question to assess Fear of Negative Evaluation specifically as opposed to Social Anxiety more generally.
4.2. Conclusions, Limitations, and Future Directions
Overall, the current results suggest that when using the SPIN in clinical samples, 16 of the original 17 items can be used to yield a score representing overall severity of SAD. Subsets of those items can then be used to measure Fear of Negative Evaluation, Fear of Physical Symptoms, and Fear of Uncertainty in Social Situations. In addition to having a strong conceptual basis, these subscales are expected to be clinically useful. Table 4 provides examples of how cognitive-behavioral therapy for SAD could be tailored based on the proposed SPIN subscale scores.
Table 4.
Illustration of clinical utility of SPIN subscale scores: Tailoring cognitive-behavioral therapy
| Subscale Score | Further assessment/Case conceptualization | Treatment Indications |
|---|---|---|
| Fear of Negative Evaluation is HIGH | Focus on elaborating the specific feared consequences of negative evaluation (e.g., experiencing embarrassment or humiliation, being socially isolated, losing one's job, forgetting the rest of one's speech) | Work toward identifying core beliefs that make negative evaluation seem highly likely or consequential Fear and Avoidance Hierarchy should include situations that strongly activate these concerns As situational exposure progresses, incorporate criticism and other negative feedback into exposure scenarios Foster acceptance of the inevitability of occasional negative evaluation and problem-solve coping with negative feedback |
| Fear of Physical Symptoms is HIGH Note: If combined with LOW Fear of Negative Evaluation, consider additional diagnostic assessment focused on the differential between Panic Disorder and SAD |
Assess full range of physical symptoms associated with anxiety to determine whether patient is concerned about symptoms other than those assessed by the SPIN (blushing, heart palpitations, sweating, trembling/shaking) Determine feared outcomes of symptoms (e.g., they will be noticed by others, they will prevent normal speech or other social behavior) |
Consider conducting interoceptive exposure if patient fears the symptoms themselves Incorporate symptom provocation during situational exposure (e.g., induce sweating before interacting with a stranger) and also expose the patient to feared outcomes (e.g., conversation partner remarks that the patient is blushing). Video-record exposures to provide realistic information about the degree to which physical symptoms are noticeable |
| Fear of Uncertainty in Social Situations is HIGH | Conduct detailed inquiry about feared scenarios that could arise in situations that involve unfamiliar people or settings (e.g., having to “break into” an ongoing conversation at a party; encountering a highly critical observer when the center of attention) | Psychoeducational component of treatment could include discussion of anxiety being a response to unpredictability; and when this can be helpful vs. counterproductive Fear and Avoidance Hierarchy should include graded variations of situations where the person may interact with groups, strangers, and/or be the focus of attention Exposures should include confederates who model a wide variety of response styles (e.g., quiet conversation partner) and include unpredictable or novel events (e.g., audience member interrupts or walks out during speech) |
The factor analytic results also point toward ways in which the SPIN could be abridged without diminishing its construct validity. Specifically, several items could be selected to represent each latent factor; obvious candidates would be the items with the most robust loadings on their corresponding factors. Development and evaluation of an abridged version of the SPIN was beyond the scope of this study, but is an interesting direction for future research.
A particular strength of this study is the demographic, geographic, and clinical diversity of the sample. Although all respondents met criteria for SAD, many co-occurring disorders were permitted and SAD was not required to be the principal diagnosis for all respondents. Thus, a wide range of presentations of SAD were represented.
The current results also must be interpreted with certain limitations in mind. First, sample size was insufficient to allow for EFA replication before CFA. Consistent EFA results across two randomly selected subsamples would have provided a more solid basis for CFA model specification. The current results require replication in other samples of individuals with clinically significant SAD symptoms. Our assessment of the validity of the proposed subscales was preliminary and limited to measures available in the CALM assessment battery. Those results require replication and extension; for example, associations of the proposed subscales with additional well-validated measures such as the Anxiety Sensitivity Index-3 (Taylor et al., 2007) and the Intolerance of Uncertainty Scale (Buhr & Dugas, 2002) should be examined. Future investigations with larger sample sizes also should pursue measurement invariance testing in CFA to determine if the factor structure of the SPIN varies for members of different demographic groups (e.g., based on gender or race/ethnicity).
In summary, factor analysis of SPIN data from a sample of primary care patients with SAD suggests that this instrument measures the higher-order construct of Social Anxiety as well as three lower-order dimensions of Fear of Negative Evaluation, Fear of Physical Symptoms, and Fear of Uncertainty in Social Situations. These hypothesized latent variables are concordant with underlying dimensions of SAD (and anxiety more globally) that have been described in the literature. The Fear of Negative Evaluation factor and the higher-order Social Anxiety factor appear to have low discriminant validity, which complicates interpretation of the results but is understandable given the centrality of fear of negative evaluation to the construct of social anxiety. Scores on the proposed subscales of the SPIN may prove useful in tailoring empirically-supported treatments for SAD.
Highlights.
Exploratory and confirmatory factor analyses of the SPIN are presented
The sample was comprised of primary care patients with Social Anxiety Disorder
Results supported a 3-factor model of the SPIN
Factors reflected fears of negative evaluation, physical symptoms, and uncertainty
These factors loaded strongly on a higher-order factor reflecting Social Anxiety
Acknowledgments
This work utilized data from the Coordinated Anxiety Learning and Management (CALM) study, which was supported by grants U01 MH057835 (Dr. Stein) and U01 MH057858 (Dr. Roy-Byrne) from the National Institute of Mental Health, Bethesda, MD, USA. The authors wish to acknowledge the principal investigators from the other CALM study sites: Michelle G. Craske, PhD (University of California, Los Angeles), Cathy D. Sherbourne, PhD (RAND Corporation), and Greer Sullivan, MD (University of Arkansas for Medical Sciences).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Because item 10 had displayed a modest cross-loading on Fear of Negative Evaluation in EFA, we repeated the CFA specifying an additional path from Fear of Negative Evaluation to item 10; however, in the CFA subsample item 10 did not cross-load and model fit was degraded.
Disclosures. Dr. Roy-Byrne has in the last three years been Editor-In-Chief for Depression and Anxiety, Journal Watch Psychiatry, and UpToDate Psychiatry and received stock options from Valent Medical Solutions (a behavioral health EMR company). Dr. Stein has in the last three years been a consultant for Healthcare Management Technologies, Janssen, and Tonix Pharmaceuticals. The other authors have no disclosures.
Reference List
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 5th ed. Author; Washington, D.C.: 2013. [Google Scholar]
- Andreescu C, Belnap BH, Rollman BL, Houck P, Ciliberti C, Mazumdar S, Lenze EJ. Generalized anxiety disorder severity scale validation in older adults. Am J Geriatr Psychiatry. 2008;16(10):813–818. doi: 10.1097/JGP.0b013e31817c6aab. doi: 10.1097/JGP.0b013e31817c6aab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antony MM, Coons MJ, McCabe RE, Ashbaugh A, Swinson RP. Psychometric properties of the social phobia inventory: further evaluation. Behav Res Ther. 2006;44(8):1177–1185. doi: 10.1016/j.brat.2005.08.013. doi: 10.1016/j.brat.2005.08.013. [DOI] [PubMed] [Google Scholar]
- Boelen PA, Reijntjes A. Intolerance of uncertainty and social anxiety. J Anxiety Disord. 2009;23(1):130–135. doi: 10.1016/j.janxdis.2008.04.007. doi: 10.1016/j.janxdis.2008.04.007. [DOI] [PubMed] [Google Scholar]
- Brown TA. Confirmatory factor analysis for applied research. 2nd ed. Guilford; New York, NY: 2015. [Google Scholar]
- Buhr K, Dugas MJ. The Intolerance of Uncertainty Scale: psychometric properties of the English version. Behav Res Ther. 2002;40(8):931–945. doi: 10.1016/s0005-7967(01)00092-4. [DOI] [PubMed] [Google Scholar]
- Caballo VE, Salazar IC, Irurtia MJ, Arias B, Nobre L. The assessment of social anxiety through five self-report measures (LSAS-SR, SPAI, SPIN, SPS, and SIAS): A critical analysis of their factor structure. Behavioral Psychology. 2013;21(3):423–448. [Google Scholar]
- Campbell-Sills L, Brown TA. Latent variable approaches to studying the classification and psychopathology of mental disorders. In: Andrasik F, editor. Comprehensive handbook of personality and psychopathology, Volume II: Adult psychopathology. Wiley; New York, NY: 2005. pp. 21–35. [Google Scholar]
- Campbell-Sills L, Norman SB, Craske MG, Sullivan G, Lang AJ, Chavira DA, Stein MB. Validation of a brief measure of anxiety-related severity and impairment: the Overall Anxiety Severity and Impairment Scale (OASIS). J Affect Disord. 2009;112(1-3):92–101. doi: 10.1016/j.jad.2008.03.014. doi: 10.1016/j.jad.2008.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carleton RN. The intolerance of uncertainty construct in the context of anxiety disorders: theoretical and practical perspectives. Expert Rev Neurother. 2012;12(8):937–947. doi: 10.1586/ern.12.82. doi: 10.1586/ern.12.82. [DOI] [PubMed] [Google Scholar]
- Carleton RN, Collimore KC, Asmundson GJ. “It's not just the judgements--It's that I don't know”: intolerance of uncertainty as a predictor of social anxiety. J Anxiety Disord. 2010;24(2):189–195. doi: 10.1016/j.janxdis.2009.10.007. doi: 10.1016/j.janxdis.2009.10.007. [DOI] [PubMed] [Google Scholar]
- Carleton RN, Collimore KC, Asmundson GJ, McCabe RE, Rowa K, Antony MM. SPINning factors: factor analytic evaluation of the Social Phobia Inventory in clinical and nonclinical undergraduate samples. J Anxiety Disord. 2010;24(1):94–101. doi: 10.1016/j.janxdis.2009.09.003. doi: 10.1016/j.janxdis.2009.09.003. [DOI] [PubMed] [Google Scholar]
- Clark DM, Wells A. A cognitive model of social phobia. In: Heimberg RG, Liebowitz MR, Hope DA, Schneier FR, editors. Social phobia: Diagnosis, assessment, and treatment. Guilford; New York, NY: 1995. pp. 69–93. [Google Scholar]
- Connor KM, Davidson JR, Churchill LE, Sherwood A, Foa E, Weisler RH. Psychometric properties of the Social Phobia Inventory (SPIN). New self-rating scale. Br J Psychiatry. 2000;176:379–386. doi: 10.1192/bjp.176.4.379. [DOI] [PubMed] [Google Scholar]
- Costello AB, Osborne JW. Best practices in exploratory factor analysis: Four recommendations for getting the most from your analysis. Practical Assessment, Research, and Evaluation. 2005;10(7):1–9. [Google Scholar]
- Craske MG, Stein MB, Sullivan G, Sherbourne C, Bystritsky A, Rose RD, Roy-Byrne P. Disorder-specific impact of coordinated anxiety learning and management treatment for anxiety disorders in primary care. Arch Gen Psychiatry. 2011;68(4):378–388. doi: 10.1001/archgenpsychiatry.2011.25. doi: 10.1001/archgenpsychiatry.2011.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dugas MJ, Marchand A, Ladouceur R. Further validation of a cognitive-behavioral model of generalized anxiety disorder: diagnostic and symptom specificity. J Anxiety Disord. 2005;19(3):329–343. doi: 10.1016/j.janxdis.2004.02.002. doi: 10.1016/j.janxdis.2004.02.002. [DOI] [PubMed] [Google Scholar]
- Heimberg RG, Hofmann SG, Liebowitz MR, Schneier FR, Smits JA, Stein MB, Craske MG. Social anxiety disorder in DSM-5. Depress Anxiety. 2014;31(6):472–479. doi: 10.1002/da.22231. doi: 10.1002/da.22231. [DOI] [PubMed] [Google Scholar]
- Hendriks SM, Spijker J, Licht CM, Beekman AT, Hardeveld F, de Graaf R, Penninx BW. Disability in anxiety disorders. J Affect Disord. 2014;166:227–233. doi: 10.1016/j.jad.2014.05.006. doi: 10.1016/j.jad.2014.05.006. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Barlow DH. Social phobia (Social anxiety disorder). In: Barlow DH, editor. Anxiety and its disorders: The nature and treatment of anxiety and panic (2nd ed.) 2nd ed. Guilford; New York, NY: 2002. pp. 454–476. [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural equation modeling. 1999;6:1–55. [Google Scholar]
- Jaccard J, Wan CK. LISREL approaches to interaction effects in multiple regression. Sage; Thousand Oaks, CA: 1996. [Google Scholar]
- Jack MS, Heimberg RG, Mennin DS. Situational panic attacks: impact on distress and impairment among patients with social phobia. Depress Anxiety. 1999;10(3):112–118. doi: 10.1002/(sici)1520-6394(1999)10:3<112::aid-da4>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- Joreskog KG. Testing structural equation models. In: Bollen KA, Long JS, editors. Testing structural equation models. Sage; Newbury Park, CA: 1993. pp. 294–316. [Google Scholar]
- McCabe RE, Ashbaugh AR, Antony MM. Specific and social phobia. In: Antony MM, Barlow DH, editors. Asessment and treatment planning for psychological disorders. 2nd ed. Guilford Press; New York, NY: 2010. pp. 186–223. [Google Scholar]
- Means-Christensen AJ, Sherbourne CD, Roy-Byrne PP, Craske MG, Stein MB. Using five questions to screen for five common mental disorders in primary care: diagnostic accuracy of the Anxiety and Depression Detector. Gen Hosp Psychiatry. 2006;28(2):108–118. doi: 10.1016/j.genhosppsych.2005.08.010. doi: 10.1016/j.genhosppsych.2005.08.010. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus 3 (Version 3) Author; Los Angeles: 2004. [Google Scholar]
- Osorio FL, Crippa JA, Loureiro SR. Evaluation of the psychometric properties of the Social Phobia Inventory in university students. Compr Psychiatry. 2010;51(6):630–640. doi: 10.1016/j.comppsych.2010.03.004. doi: 10.1016/j.comppsych.2010.03.004. [DOI] [PubMed] [Google Scholar]
- Radomsky AS, Ashbaugh AR, Saxe ML, Ouimet AJ, Golden ER, Lavoie SL. Psychometric properties of the French and English versions of the Social Phobia Inventory. Canadian Journal of Behavioural Science. 2006;38:354–360. [Google Scholar]
- Rapee RM, Heimberg RG. A cognitive-behavioral model of anxiety in social phobia. Behav Res Ther. 1997;35(8):741–756. doi: 10.1016/s0005-7967(97)00022-3. [DOI] [PubMed] [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behav Res Ther. 1986;24(1):1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Roy-Byrne P, Craske MG, Sullivan G, Rose RD, Edlund MJ, Lang AJ, Stein MB. Delivery of evidence-based treatment for multiple anxiety disorders in primary care: a randomized controlled trial. JAMA. 2010;303(19):1921–1928. doi: 10.1001/jama.2010.608. doi: 10.1001/jama.2010.608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruscio AM, Brown TA, Chiu WT, Sareen J, Stein MB, Kessler RC. Social fears and social phobia in the USA: results from the National Comorbidity Survey Replication. Psychol Med. 2008;38(1):15–28. doi: 10.1017/S0033291707001699. doi: 10.1017/S0033291707001699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shear K, Belnap BH, Mazumdar S, Houck P, Rollman BL. Generalized anxiety disorder severity scale (GADSS): a preliminary validation study. Depress Anxiety. 2006;23(2):77–82. doi: 10.1002/da.20149. doi: 10.1002/da.20149. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. quiz 34-57. [PubMed] [Google Scholar]
- Sherbourne CD, Sullivan G, Craske MG, Roy-Byrne P, Golinelli D, Rose RD, Stein MB. Functioning and disability levels in primary care out-patients with one or more anxiety disorders. Psychol Med. 2010;40(12):2059–2068. doi: 10.1017/S0033291710000176. doi: 10.1017/S0033291710000176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steiger JH. Tests for comparing elements of a correlation matrix. Pychological Bulletin. 1980;87:245–251. [Google Scholar]
- Stein MB, Kean YM. Disability and quality of life in social phobia: epidemiologic findings. Am J Psychiatry. 2000;157(10):1606–1613. doi: 10.1176/appi.ajp.157.10.1606. [DOI] [PubMed] [Google Scholar]
- Stein MB, Stein DJ. Social anxiety disorder. Lancet. 2008;371(9618):1115–1125. doi: 10.1016/S0140-6736(08)60488-2. doi: 10.1016/S0140-6736(08)60488-2. [DOI] [PubMed] [Google Scholar]
- Sullivan G, Craske MG, Sherbourne C, Edlund MJ, Rose RD, Golinelli D, Roy-Byrne PP. Design of the Coordinated Anxiety Learning and Management (CALM) study: innovations in collaborative care for anxiety disorders. Gen Hosp Psychiatry. 2007;29(5):379–387. doi: 10.1016/j.genhosppsych.2007.04.005. doi: 10.1016/j.genhosppsych.2007.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, Cardenas SJ. Robust dimensions of anxiety sensitivity: development and initial validation of the Anxiety Sensitivity Index-3. Psychol Assess. 2007;19(2):176–188. doi: 10.1037/1040-3590.19.2.176. doi: 10.1037/1040-3590.19.2.176. [DOI] [PubMed] [Google Scholar]
- Teale Sapach MJ, Carleton RN, Mulvogue MK, Weeks JW, Heimberg RG. Cognitive constructs and social anxiety disorder: beyond fearing negative evaluation. Cogn Behav Ther. 2015;44(1):63–73. doi: 10.1080/16506073.2014.961539. doi: 10.1080/16506073.2014.961539. [DOI] [PubMed] [Google Scholar]
- Wells A, Papageorgiou C. Social phobic interoception: effects of bodily information on anxiety, beliefs and self-processing. Behav Res Ther. 2001;39(1):1–11. doi: 10.1016/s0005-7967(99)00146-1. [DOI] [PubMed] [Google Scholar]