Abstract
OBJECTIVE
To develop a method for calculating the number of healthcare-associated infections (HAIs) that must be prevented to reach a HAI reduction goal and identifying and prioritizing healthcare facilities where the largest reductions can be achieved.
SETTING
Acute care hospitals that report HAI data to the Centers for Disease Control and Prevention’s National Healthcare Safety Network.
METHODS
The cumulative attributable difference (CAD) is calculated by subtracting a numerical prevention target from an observed number of HAIs. The prevention target is the product of the predicted number of HAIs and a standardized infection ratio goal, which represents a HAI reduction goal. The CAD is a numeric value that if positive is the number of infections to prevent to reach the HAI reduction goal. We calculated the CAD for catheter-associated urinary tract infections for each of the 3,639 hospitals that reported such data to National Healthcare Safety Network in 2013 and ranked the hospitals by their CAD values in descending order.
RESULTS
Of 1,578 hospitals with positive CAD values, preventing 10,040 catheter-associated urinary tract infections at 293 hospitals (19%) with the highest CAD would enable achievement of the national 25% catheter-associated urinary tract infection reduction goal.
CONCLUSION
The CAD is a new metric that facilitates ranking of facilities, and locations within facilities, to prioritize HAI prevention efforts where the greatest impact can be achieved toward a HAI reduction goal.
Healthcare-associated infections (HAIs) are a significant cause of morbidity, mortality, and avoidable health care costs.1–3 HAI prevention is a national priority4 and is one of the Centers for Disease Control and Prevention’s (CDC) 10 Winnable Battles.5 In 2009, the US Department of Health and Human Services developed the National Action Plan to Prevent HAIs: Road Map to Elimination.4 In 2010, CDC, in collaboration with clinical and public health partners, outlined several strategies to move toward the goal of HAI elimination, with an emphasis on using HAI surveillance data to target prevention efforts and to measure progress.6
For HAI surveillance, CDC’s National Healthcare Safety Network (NHSN) is used by CDC and its public health partners and has gained increasingly representative data owing to federal and state reporting mandates.7 NHSN provides data at the levels of healthcare facility, state, region, and nation for identifying priorities for HAI reduction and measuring progress of prevention efforts. The primary metric used for these purposes is the standardized infection ratio (SIR).8 Although the SIR is highly useful as a comparative metric and for measuring progress, as a ratio of observed to predicted infections, it does not represent an absolute burden of HAIs. In particular, a high SIR can result for a facility with relatively low exposure volume (eg, urinary catheter–days in the case of CAUTI) that may not indicate a large number of observed HAIs. Therefore, targeting facilities on the basis of SIR alone may not be an efficient regional or national strategy for reducing HAIs.
In an effort to use data for action to identify and prioritize healthcare facilities where prevention efforts can yield the largest impact, CDC has introduced the Targeted Assessment for Prevention (TAP) strategy. This strategy uses a new metric stemming from the SIR, called the cumulative attributable difference (CAD), to identify hospitals with the largest excesses in HAIs in relation to achieving a HAI reduction goal. The objective of this report is to describe the CAD, its calculation, and its use in the TAP strategy.
METHODS
Surveillance Data
To illustrate the calculation and use of the CAD, we chose to use catheter-associated urinary tract infections (CAUTIs) that were reported to NHSN from intensive care unit (ICU) and non-ICU locations in 2013, the most recent calendar year for which CAUTI data are complete.9 Reporting of CAUTI from ICUs to NHSN became required in January 2012 for acute care hospitals participating in the Centers for Medicare & Medicaid Services Inpatient Prospective Payment Systems Inpatient Quality Reporting program.9 As of 2014, public health departments in 16 states also require hospitals in their jurisdictions to report CAUTI data to NHSN, and most of these mandates include ICU and non-ICU patient care locations.
Development of a New Metric
To calculate the number of infections that must be prevented to achieve a HAI reduction goal, we defined the CAD as the difference between an observed number of HAIs and a numerical prevention target. The prevention target is a product of the predicted number of HAIs and a SIR goal.
OBSERVED =observed number of HAI in a healthcare facility or patient care location within a facility in a defined period; PREDICTED = statistically predicted number of HAIs in a healthcare facility or patient care location within a facility in the same defined period (derived from the standard US population)8; SIRgoal=goal SIR, which represents a HAI reduction goal (eg, Department of Health and Human Services national reduction goal for CAUTI =25%, which translates to a goal SIR of 0.75).4
Because the CAD measure is based on a simple additive scale, its values can range from −∞ to +∞. A positive CAD value represents the number of infections in a patient care location or facility in a defined period that must be prevented to reach a HAI reduction goal. These infections are presumed to be preventable with current prevention guidelines, and eliminating them would help reach a target reduction goal. In contrast, a negative CAD value in a location or facility for a given period implies that fewer HAIs occurred than are statistically predicted and the SIR goal has been reached or exceeded. Additional information on computing variations of the CAD metric using different SIR goal multipliers is described in the appendix. Although the goal SIR may be tailored to the prevention goals of a specific facility or organization, we used the CAD calculation with the Department of Health and Human Services CAUTI reduction goal as the SIR multiplier, unless otherwise specified.
Appendix.
Calculating the Cumulative Attributable Difference (CAD) Metric With 3 Different SIR Goals Among 3 Hypothetical Hospitals Participating in NHSN Catheter-Associated Urinary Tract Infections (CAUTI) Surveillance
| CAD | Equation | Hospital A | Hospital B | Hospital C |
|---|---|---|---|---|
| CAD = Observed–(Predicted*SIRgoal) | Observed no. = 6 (4 in ICUs, 2 in non-ICUs) Predicted no. = 2 (1 in ICUs, 1 in non-ICUs) SIR = 6/2 = 3.0 |
Observed no. = 20 (12 in ICUs, 8 in non-ICUs) Predicted no. = 10 (6 in ICUs, 4 in non-ICUs) SIR = 20/10 = 2.0 |
Observed no. = 8 (2 in ICUs, 6 in non-ICUs) Predicted no. = 10 (5 in ICUs, 5 in non-ICUs) SIR = 8/10 = 0.8 |
|
| I. CAD | ||||
| Number of CAUTIs that must be prevented given SIRgoal = 1.0 (the national baseline) |
CAD = Observed–(Predicted*SIRgoal ) | CAD = 6−(2 × 1.0) = 4 | CAD = 20−(10 × 1.0) = 10 | CAD = 8–(10 × 1.0) = −2 |
| Number of CAUTIs that must be prevented given SIRgoal = 1.057 (the 2013 national SIR) |
CAD = Observed–(Predicted*SIRgoal) | CAD = 6−(2 × 1.057) = 3.88 |
CAD = 20–(10 × 1.057) = 9.4 |
CAD = 8–(10 × 1.057) = − 2.6 |
| Number of CAUTIs that must be prevented given SIRgoal = 0.75 (the HHS target) |
CAD = Observed–(Predicted*SIRgoal) | CAD = 6–(2 × 0.75) = 4.5 | CAD = 20–(10 × 0.75) = 12.5 |
CAD = 8−(10 × 0.75) = 0.5 |
|
II. CAD, stratified by location type (ICU vs non-
ICU) |
||||
| Number of CAUTIs that must be prevented given SIRgoal = 1.18 (the 2013 national SIR in ICUs) and 0.8 (the 2013 national SIR in non-ICUs) |
CAD = [Observed – (Predicted*SIRgoal)]ICU + [Observed – (Predicted*SIRgoal)]non-ICU |
ICU
CAD ICU = 4−(1 × 1.2) = 2.8 |
ICU
CAD ICU = 12–(6 × 1.2) = 4.8 |
ICU
CAD ICU = 2–(5 × 1.2) = −4 |
|
Non-ICU
CAD non-ICU = 2–(1 × 0.8) = 1.2 CAD = 2.8 + 1.2 = 4.0 |
Non-ICU
CAD non-ICU = 8–(4×0.8) = 4.8 CAD = 4.8 + 4.8 = 9.6 |
Non-ICU
CAD non-ICU = 6–(5 × 0.8) = 2 CAD = − 4+2 = −2 |
NOTE. Although the Targeted Assessment for Prevention strategy may be implemented to achieve a chosen standardized infection ratio (SIR) goal, the ultimate goal should be aimed toward elimination of healthcare-associated infections. ICU, intensive care units; NHSN, National Healthcare Safety Network; non-ICU, non–intensive care units.
Evaluating CAD for Prioritizing National Prevention Efforts
Using national NHSN CAUTI data, we ranked hospitals in descending order of their CAD values. To evaluate the relative efficiency of the CAD metric compared with the SIR in prioritizing prevention efforts to reach the national CAUTI 25% reduction goal, we selected hospitals that had not reached this goal with SIR greater than 0.75 (n =1,578), ranked them by the CAD and SIR metrics in descending order, and determined the number of hospitals needed to target to reach the national goal by each metric. Selecting hospitals each with a SIR greater than 0.75 allowed for calculation of positive CAD values at the facility level that were oriented to the national CAUTI SIR goal and supported more meaningful comparison. All statistical analyses were conducted using SAS, version 9.3 (SAS Institute, Cary, NC).
RESULTS
A total of 3,639 hospitals, predominantly general acute care hospitals followed by critical access hospitals, reported CAUTI surveillance data to NHSN in 2013 (Table 1). Approximately 65% of hospitals had fewer than 200 beds and approximately 70% were categorized as nonteaching hospitals.
Table 1.
Characteristics of Hospitals Conducting Catheter-Associated Urinary Tract Infection Surveillance and Hospitals Targeted to Reach the HHS National Reduction Goal, NHSN, 2013
| All NHSN Hospitals (n = 3,639) |
Hospitals targeted to reach the HHS reduction goal through the CAD metric (n = 293) |
|||
|---|---|---|---|---|
| Characteristics | n | % | n | % |
| Bed size | ||||
| 1–25 | 416 | 11.4 | ||
| 26–50 | 342 | 9.4 | ||
| 51–100 | 627 | 17.2 | 2 | 0.7 |
| 101–200 | 912 | 25.1 | 13 | 4.4 |
| 201–500 | 1,080 | 29.7 | 136 | 46.4 |
| 501–1,000 | 241 | 6.6 | 133 | 45.4 |
| > 1,000 | 15 | 0.4 | 9 | 3.1 |
| Missing | 6 | 0.2 | ||
| Teaching statusa | ||||
| Major teaching | 510 | 14.0 | 158 | 53.9 |
| Graduate teaching | 522 | 14.3 | 59 | 20.1 |
| Undergraduate teaching | 123 | 3.4 | 4 | 1.4 |
| Nonteaching | 2,484 | 68.3 | 72 | 24.6 |
| Hospital type | ||||
| Critical access | 329 | 9.0 | ||
| Children’s | 52 | 1.4 | ||
| General | 3,119 | 85.7 | 293 | 100.0 |
| Military | 28 | 0.8 | ||
| Oncology | 12 | 0.3 | ||
| Orthopedic | 18 | 0.5 | ||
| Psychiatric | 6 | 0.2 | ||
| Surgical | 50 | 1.4 | ||
| Veterans Affairs | 11 | 0.3 | ||
| Women’s and Children’s | 6 | 0.2 | ||
| Women’s | 8 | 0.2 | ||
| US Census regionsb | ||||
| Northeast | 586 | 16.1 | 72 | 24.6 |
| Midwest | 886 | 24.3 | 54 | 18.4 |
| South | 1,417 | 38.9 | 112 | 38.2 |
| West | 732 | 20.1 | 54 | 18.4 |
| Otherc | 18 | 0.5 | 1 | 0.3 |
NOTE. Cumulative attributable difference (CAD) = Observed – (Predicted *0.75). HHS, US Department of Health and Human Services; NHSN, National Healthcare Safety Network.
Major: Hospital is an important part of the teaching program of a medical school and the majority of medical students rotate through multiple clinical services; Graduate: Hospital is used by the medical school for graduate training programs only—that is, residency and/or fellowships.
Northeast: Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, and Vermont; Midwest: Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, and Wisconsin; South: Alabama, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, and West Virginia; West: Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, and Wyoming.
Armed Forces, Puerto Rico, and US Virgin Islands.
Of 3,639 reporting hospitals, 1,578 had positive CAD values, which summed to 14,206 CAUTIs. When these hospitals were ranked by the CAD metric, targeting the first 293 hospitals with the highest CAD values (Figure 1), which represents 10,040 infections, would achieve the national 25% reduction goal, and each targeted facility would need to reduce the percentage of CAUTIs (CAD ÷ observed number of infection ×100) by a median (interquartile range) of 57% (47%–66%). Most of the targeted hospitals were teaching hospitals with at least 200 beds (Table 1). In contrast, when these 1,578 hospitals were ranked by the SIR metric in descending order, preventing 10,040 CAUTIs would require targeting of 700 hospitals with the highest SIR values (Figure 1). Among these 700 hospitals, the median (interquartile range) percent reduction per facility needed to reach the CAUTI reduction goal was 62% (56%–70%). Limiting the analysis to a subset of hospitals with SIR significantly greater than 0.75 (P ≤.05) still resulted in a greater number of hospitals to target when ranking by SIR (n = 472) rather than by CAD (n = 293).
FIGURE 1.
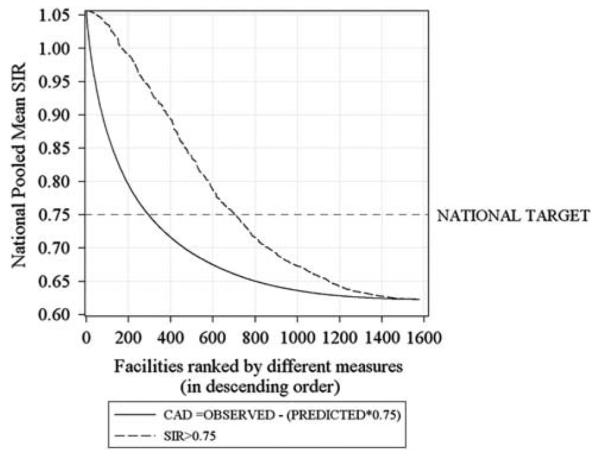
Impact on the 2013 national pooled mean standardized infection ratio (SIR) (2013 National SIR= 1.057) of catheter-associated urinary tract infections and number of hospitals needed to target to reach the national 25% reduction goal (Department of Health and Human Services goal) among acute care hospitals with SIR greater than 0.75 (n= 1,578), National Healthcare Safety Network. Graph lines represent hypothetical decline in national pooled mean SIR if number of infections that must be prevented to reach the Department of Health and Human Services goal are prevented in hospitals ranked by cumulative attributable difference (CAD) (solid line) and SIR (dashed line) in descending order. National target means the national 25% reduction goal for catheter-associated urinary tract infections.
DISCUSSION
We introduce a new metric, the CAD, and demonstrate how it can be used to efficiently target hospitals for prioritizing prevention interventions. The TAP strategy is a data-driven approach in which the CAD metric can focus initial HAI prevention efforts on a targeted number of hospitals that account for a disproportionate burden of infections. The CAD metric can also be used to identify the specific units within hospitals that are contributing to the HAI burden.
The CAD metric is complementary to the SIR metric and is based on its numerator (observed number of HAIs) and its denominator (predicted number of HAIs). The CAD provides an absolute value of the difference between the observed and numerical prevention target using a SIR goal multiplier for the predicted number that allows for an assessment of the magnitude of HAIs needed to prevent to reach a specific HAI reduction goal. By providing concrete facility-specific and location-specific goals, the CAD can help direct prevention resources to where they are most needed. The CAD metric is flexible in that the numerical prevention target can be adjusted using any SIR goal. In addition, the TAP strategy using the CAD is scalable and can be applied at the facility, system, regional, state, or national level.
Our evaluation of the potential impact on the national CAUTI SIR shows that a national goal could be achieved by targeting a smaller number of hospitals than if the SIR were used to rank hospitals. Therefore, the CAD complements the SIR by helping to target hospitals (and locations within a hospital) where prevention may have the biggest impact. In addition, a benefit of the CAD for hospitals and HAI prevention programs is having an understanding about the numbers of infections they need to prevent in a defined period to reach HAI reduction goals that can be stratified to the location level, enabling assessments of potential gaps in those targeted units that can be addressed with specific prevention strategies. In early 2015, CDC added TAP report functionality to the NHSN application, which enables NHSN users to run TAP reports at both the hospital and patient care location levels for several HAIs.10
Although NHSN surveillance data is ideally used for generating TAP reports, the hospital-level CAD can readily be computed from publicly available summary data, such as CMS’s Hospital Compare.11 However, groups that have access to NHSN data have the advantage of conducting real-time and more granular analyses to target HAI prevention efforts.
The CAD metric has several potential limitations. First, because the facility-level CAD measures absolute numbers of infections relative to a SIR goal and is influenced by risk exposure volume (ie, larger hospitals may preferentially be targeted), it is useful for guiding and prioritizing regional and national prevention efforts but should not be used as a comparative metric among hospitals for reporting purposes. Furthermore, this metric and strategy are not intended to obviate the need for infection prevention in other facilities or reduce the momentum of successful prevention efforts among facilities with low or negative CAD values. Second, the number of infections identified by the positive CAD value as necessary to prevent in order to reach a SIR goal may exceed the number that are readily preventable given available resources and current technology. The CAD varies depending on the SIR goal multiplier, which itself reflects a set of expectations and assumptions inherent in the choice of a prevention goal. However, in this report the estimated percent reduction per facility by setting the Department of Health and Human Services goal as a target may be achievable on the basis of recent CAUTI prevention data.12 Third, the facility-level CAD is a summary measure that may mask HAI prevention needs at the location level because of a canceling effect among positive and negative CAD values across patient care locations within a hospital. Therefore, computing location-specific CAD values can unmask and target efforts at specific units that may have a disproportionate burden of infections. Finally, use of facility-level CAD based on a subset of locations within a facility as a result of differential reporting requirements (eg, variable reporting for non-ICUs vs mandatory reporting for ICUs) may not accurately reflect prevention assessment for the entire facility. As reporting requirements gradually expand to non-ICU locations, data will become more representative facility-wide over time.
In summary, the measure and approach described in this report are intended to help intensify prevention efforts by setting priorities and maximizing available resources toward the goal of eliminating HAIs. The TAP strategy can be applied by individual hospitals or healthcare systems as part of their internal quality improvement efforts and by groups such as state health departments and quality improvement organizations as part of their prevention collaboratives. Once hospitals are identified and targeted using the CAD metric, the next steps in the TAP strategy are to assess the gaps in prevention in the targeted areas and to implement specific evidence-based strategies to address the gaps.10 CDC is actively working with partners to develop tools for these purposes.
ACKNOWLEDGMENTS
We thank the NHSN participants for their ongoing efforts to monitor infections and improve patient safety, and our colleagues in the Division of Healthcare Quality Promotion, National Center for Emerging and Zoonotic Infectious Diseases, who tirelessly support this unique public health network.
Financial support. The NHSN surveillance system is supported by the Division of Healthcare Quality Promotion, National Center for Emerging and Zoonotic Infectious Diseases, CDC.
Footnotes
Potential conflicts of interest. All authors report no conflicts of interest relevant to this article.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Magill SS, Edwards JR, Bamberg W, et al. Multistate point-prevalence survey of health care-associated infections. N Engl J Med. 2014;370:1198–1208. doi: 10.1056/NEJMoa1306801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marchetti A, Rossiter R. Economic burden of healthcare-associated infection in US acute care hospitals–societal perspective. J Med Econ. 2013;16:1399–1404. doi: 10.3111/13696998.2013.842922. [DOI] [PubMed] [Google Scholar]
- 3.Scott RD. The direct medical costs of healthcare-associated infections in U.S. hospitals and the benefits of prevention, 2009. Centers for Disease Control and Prevention. website. http://www.cdc.gov/HAI/pdfs/hai/Scott_CostPaper.pdf. Published March 2009. Accessed July 2014.
- 4.The National Action Plan to Prevent Health Care-Associated Infections Road Map to Elimination. US Department of Health and Human Services. website. http://www.health.gov/hai/prevent_hai.asp#hai_plan. Accessed December 2014.
- 5.Centers for Disease Control and Prevention Winnable Battles. http://www.cdc.gov/winnablebattles/. Accessed November 2014.
- 6.Cardo D, Dennehy PH, Halverson P, et al. Moving toward elimination of healthcare-associated infections: a call to action. Am J Infect Control. 2010;38:671–675. doi: 10.1016/j.ajic.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention National Healthcare Safety Network (NHSN) Centers for Disease Control and Prevention. website. http://www.cdc.gov/nhsn/. Accessed December 2014.
- 8.Centers for Disease Control and Prevention National Healthcare Safety Network (NHSN) e-news: SIRs special edition. Centers for Disease Control and Prevention. website. http://www.cdc.gov/nhsn/PDFs/Newsletters/NHSN_NL_OCT_2010SE_final.pdf. Accessed December 2014.
- 9.Centers for Disease Control and Prevention Operational guidance for acute care hospitals to report catheter-associated urinary tract infection (CAUTI) data to CDC’s NHSN for the purpose of fulfilling CMS’s hospital inpatient quality reporting (IQR) requirements. Centers for Disease Control and Prevention. website. http://www.cdc.gov/nhsn/pdfs/final-ach-cauti-guidance.pdf. Accessed December 2014.
- 10.Centers for Disease Control and Prevention The five “W”s of the targeted assessment for prevention (TAP) strategy. Centers for Disease Control and Prevention. website. http://www.cdc.gov/hai/prevent/tap.html. Accessed June 2015.
- 11.Centers for Medicare and Medicaid Services. Hospital Compare US Department of Health and Human Services. website. http://www.hospitalcompare.hhs.gov/. Accessed December 2014.
- 12.Umscheid CA, Mitchell MD, Doshi JA, Agarwal R, Williams K, Brennan PJ. Estimating the proportion of healthcare-associated infections that are reasonably preventable and the related mortality and costs. Infect Control Hosp Epidemiol. 2011;32:101–114. doi: 10.1086/657912. [DOI] [PubMed] [Google Scholar]


