Abstract
Objective/purpose
To evaluate the association of statin use with progression of age-related macular degeneration (AMD).
Design
Preplanned, prospective cohort study within a controlled clinical trial of oral supplementation for age-related eye diseases.
Subjects
Age-Related Eye Disease Study 2 participants, aged 50 to 85 years.
Methods
Factors, including age, gender, smoking status, aspirin use, and history of diabetes, hypertension, heart disease, angina, and stroke, all known to be associated with statin use, were included in a logistic regression model to estimate propensity scores for each participant. Age-adjusted proportional hazards regression models, with and without propensity score matching, were performed to evaluate the association of statin use with progression to late AMD. Analyses were also performed adjusting for the competing risk of death.
Main Outcome Measures
Baseline and annual stereoscopic fundus photographs were assessed centrally by masked graders for the development of late AMD, either neovascular AMD or geographic atrophy (GA).
Results
Of the 3791 participants (2462 with bilateral large drusen and 1329 with unilateral late AMD at baseline), 1659 (43.8%) were statin users. The overall analysis, with no matching of propensity scores and no adjustment for death as a competing risk, showed that statin use was not associated with progression to late AMD (hazard ratios [HR] of 1.08, 95% confidence intervals [CI] of 0.83–1.41, P=0.56). When matched for propensity scores and adjusted for death as a competing risk, the result was not statistically significant with HR: 0.81, 95% CI: 0.55–1.20, P=0.29. Further subgroup analyses of persons with or without late AMD at baseline to the various components of late AMD (neovascular, central geographic atrophy, or any geographic atrophy) also showed no statistically significant association of statin use with progression to AMD.
Conclusions
Statin use was not statistically significantly associated with the progression to late AMD in the AREDS2 participants, and these findings are consistent with the findings in the majority of previous studies. Statins have been demonstrated to reduce the risks of cardiovascular disease, but our data do not provide evidence of a beneficial effect on slowing AMD progression.
Introduction
Age-related macular degeneration (AMD), a progressive disease that results in central vision loss, is the leading cause of blindness in persons over the age of 60 years in the United States.1 The pathogenesis of AMD is unknown. Associated risk factors include increasing age, cigarette smoking, hypertension, increased body mass index, lower educational level, presence of lens opacities, and others2–5. The use of antioxidant vitamins and minerals, known as the Age-Related Eye Disease Study (AREDS) supplement, reduces the risk of progression to late AMD, suggesting that oxidative stress may play a role in AMD.6 The association of genetic polymorphism in the complement pathway involving complement factor H and many other complement factors suggest that local or systemic inflammatory pathways may also be important in the pathogenesis of AMD.7–11 This potential inflammatory pathway is further supported by the statistically significant association of elevated serum C-Reactive Protein (CRP) with AMD in the Women’s Health Study, Rotterdam Study, and AREDS.4,7,8,12,13
Statins, or 3-hydroxy-3-methylglutaryl-coenzyme A reductase inhibitors, currently the most commonly prescribed lipid-lowering class of drugs,14 are proven to lower serum lipids and reduce cardiovascular morbidity and mortality.15 The main role of statins is to inhibit 3-hydroxy-3-methyl-glutaryl-CoA reductase in the liver, down-regulating lipid metabolism.16 However, this class of drugs has exhibited unexpected anti-inflammatory, antioxidative, and anti-angiogenic effects.17–20 Pathological studies in AMD have also demonstrated the accumulation of lipids in Bruch’s membrane similar to the atherosclerotic changes of cardiovascular disease21–23, suggesting that statins might have an effect on AMD. Previous observational studies demonstrated that statin use was associated with a protective effect on AMD24–33; however, other studies were not confirmatory.34–37 Lipid lowering with 40 mg of simvastatin in a small proof of concept study, was associated with a possible beneficial effect especially for those persons with bilateral intermediate AMD and those with genotype of the risk alleles for Complement Factor H (CFH) for progression to late AMD.38
The Age-Related Eye Disease Study 2 (AREDS2) was a prospective, multi-centered clinical trial that tested oral supplements of omega-3 fatty acids and lutein/zeaxanthin for the treatment of AMD and cataract.39 These participants were followed for a median of 5 years and the observational data from this study provided the opportunity to investigate the effect of statins on progression to late AMD.
Methods
Study population
The study design for AREDS2 is detailed in a previous report but briefly summarized here.39 Between 2006 and 2008, 4203 participants ranging from 50 to 85 years of age were enrolled at 82 retinal specialty clinics in the United States. At enrollment, participants were included if they had either bilateral large drusen or unilateral late AMD in one eye and large drusen in the fellow eye. Institutional review board approval was obtained at each clinical site, and written informed consents for the research were obtained from all study participants.
The AREDS2 participants were randomly assigned to placebo, lutein/zeaxanthin, docosahexaenoic acid (DHA) plus eicosapentaenoic acid (EPA) or the combination. At the baseline and each annual study visits, comprehensive eye exams were performed, including stereoscopic fundus photographs by certified photographers. These images were assessed by trained graders using a standardized protocol at the University of Wisconsin Fundus Photograph Reading Center. The main study outcome is the development of late AMD as graded from annual fundus photographs.
In AREDS2, late AMD was defined as having at least 2 features of neovascularization including serous detachment of the sensory retina, hemorrhage, retinal pigment epithelial detachment, fibrous tissue, or hard exudates; or geographic atrophy of an area of 360 μm or greater in diameter, involving the center of the macula; or a history of treatment for neovascular AMD. In this study we used the recently recommended and more inclusive definition of “late AMD”, which includes any definite GA in the definition, not just central GA.12
Questionnaires administered at the baseline and annual study visits were used to collect information on nutrition, medications, adverse events, and treatment compliance, among others. Telephone calls were performed twice in the first year of randomization and annually thereafter to collect information about adverse events as well as treatment for AMD and incidence of cataract surgery between the study visits.
Statistical methods
We included only participants who had no missing values to evaluate the effect of statins on eyes with intermediate AMD on the progression to late AMD. Baseline patient characteristics were compared between statin users and non-users using the t-test for continuous variables (age) and χ2 test for categorical variables including gender, race, education level, smoking status, diabetes, non-steroidal anti-inflammatory drug (NSAID) use, acetaminophen use, hypertension (defined as >140 mmHg systolic and/or >90 mmHg diastolic blood pressures), congestive heart failure, coronary heart disease, angina, history of myocardial infarction (MI), and history of stroke.
Propensity score approach can be used to reduce or eliminate the effects of confounding when using observational data (e.g., statin use) to estimate treatment effects.40 In order to reduce the effects of confounding for statin use, we used logistic regression to estimate propensity scores, which range from zero to one and indicate the probability that a participant is a statin user, based upon the risk factors listed above. Values closer to one indicate a higher likelihood of a participant using statins. After developing the propensity score for statin users and non-users, we matched statin users to non-users using the propensity scores in order to mimic characteristics of a controlled clinical trial.41 Applied in the context of statin usage in AREDS2, propensity matching approach consisted of forming match sets of statin user and non-statin users who share a similar value for the propensity score. Baseline characteristics were included in the matching model which excluded data that could not be matched.
This propensity score matching is a second method to attempt to control for the confounding from the variables in the propensity score that are both associated with statin use and with progression of AMD. The matching was done using a Greedy Matching Technique (Parsons LS. Reducing Bias in a Propensity Score Matched-Pair Sample Using Greedy Matching Techniques. Paper presented at: Proceedings of the Twenty-Sixth Annual SAS Users Group International Conference, 2001; Long Beach, CA).
Age-adjusted proportional hazards regression models were used to evaluate the effect of statin use on progression to any late AMD, including neovascular AMD and GA, in the entire cohort. Additional analyses were conducted separately for the development of neovascular AMD and GA. The competing risk of death was taken into account using the macro of Kohl and Heinze to fit a proportional sub-distribution hazards model.42,43 Hazard ratios (HRs) were calculated with 95% confidence intervals (CIs) with P < 0.05 being considered significant for all analyses.
Analyses were performed both matching and not matching statin users and non-users by the propensity scores, in addition to adjusting for death as a competing risk. Analyses were also performed separately for the two groups: participants with bilateral large drusen and participants with unilateral late AMD. No adjustments were made for multiplicity of analyses. All analyses were conducted using SAS version 9.3 (SAS Institute Inc).
Results
Of the 3791 participants included in this analysis, progression to late AMD by the end of the study occurred in 1650 (869 any geographic atrophy, 479 central geographic atrophy, and 998 neovascular AMD). Each participant could have any combination of the late forms of AMD. Associations of possible confounders with statin use are shown in Table 1. The result from proportional hazards regression model on the entire cohort, adjusting for the propensity scores, age, baseline AMD status, showed no association of statin use with the development of late AMD (hazard ratios [HR]: 1.08, 95% confidence interval [CI] of 0.83–1.41, P=0.56) (Table 2). Similar models were developed separately for the association of statin use with the components of late AMD: any GA, central GA and neovascular AMD. Statin use was not statistically significantly associated with the development of any of these outcomes, with or without accounting for the competing risk of death (Table 2).
Table 1.
Baseline Characteristics of the AREDS2 Participants included in the Unmatched Analyses.
| All participants (N = 3791) | Bilateral Large Drusen (N = 2462) | Unilateral Late AMD (N = 1329) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Statin use | Statin use | Statin use | |||||||
| No (N=2132) [N (%)] | Yes (N=1659) [N (%)] | P value | No (N=1436) [N (%)] | Yes (N=1026) [N (%)] | P value | No (N=696) [N (%)] | Yes (N=633) [N (%)] | P value | |
| Age (mean ± SD) | 72.3 ± 8.1 | 73.5 ± 7.3 | <.0001 | 71.2 ± 8.3 | 72.5 ± 7.4 | 0.0001 | 74.5 ± 7.4 | 75.3 ± 6.7 | 0.0408 |
| Female | 1302 (61.1%) | 847 (51.1.%) | <.0001 | 916 (63.8%) | 524 (51.1%) | <.0001 | 386 (55.5%) | 323 (51.0%) | 0.1057 |
| White race | 2065 (96.9%) | 1594 (96.1%) | 0.1963 | 1389 (96.7%) | 985 (96.0%) | 0.3407 | 676 (97.1%) | 609 (96.2%) | 0.3503 |
| Education | 0.0678 | 0.1253 | 0.8312 | ||||||
| High school or less | 642 (30.1%) | 557 (33.6%) | 374 (26.0%) | 304 (29.6%) | 268 (38.5%) | 253 (40.0%) | |||
| At least some college | 1019 (47.8%) | 763 (46.0%) | 709 (49.4%) | 491 (47.9%) | 310 (44.5%) | 272 (43.0%) | |||
| Post-graduate | 471 (22.1%) | 339 (20.4%) | 353 (24.6%) | 231 (22.5%) | 118 (17.0%) | 108 (17.1%) | |||
| Smoking | 0.0011 | 0.0043 | 0.3676 | ||||||
| Never | 986 (46.2%) | 669 (40.3%) | 705 (49.1%) | 435 (42.4%) | 281 (40.4%) | 234 (37.0%) | |||
| Former | 1010 (47.4%) | 880 (53.0%) | 652 (45.4%) | 530 (51.7%) | 358 (51.4%) | 350 (55.3%) | |||
| Current | 136 (6.4%) | 110 (6.6%) | 79 (5.5%) | 61 (5.9%) | 57 (8.2%) | 49 (7.7%) | |||
| Diabetes | 146 (6.8%) | 347 (20.9%) | <.0001 | 84 (5.8%) | 198 (19.3%) | <.0001 | 62 (8.9%) | 149 (23.5%) | <.0001 |
| NSAID use | 241 (11.3%) | 168 (10.1%) | 0.2464 | 157 (10.9%) | 116 (11.3%) | 0.7714 | 84 (12.1%) | 52 (8.2%) | 0.0206 |
| Acetaminophen use | 178 (8.3%) | 172 (10.4%) | 0.0332 | 118 (8.2%) | 100 (9.7%) | 0.1879 | 60 (8.6%) | 72 (11.4%) | 0.0937 |
| Aspirin use | 837 (39.3%) | 1000 (60.3%) | <.0001 | 580 (40.4%) | 646 (63.0%) | <.0001 | 257 (36.9%) | 354 (55.9%) | <.0001 |
| Hypertension | 1018 (47.7%) | 1164 (70.2%) | <.0001 | 632 (44.0%) | 694 (67.6%) | <.0001 | 386 (55.5%) | 470 (74.2%) | <.0001 |
| Congestive heart failure | 45 (2.1%) | 70 (4.2%) | 0.0002 | 27 (1.9%) | 41 (4.0%) | <.0001 | 18 (2.6%) | 29 (4.6%) | 0.0492 |
| Coronary heart disease | 73 (3.4%) | 277 (16.7%) | <.0001 | 43 (3.0%) | 173 (16.9%) | <.0001 | 30 (4.3%) | 104 (16.4%) | <.0001 |
| Angina | 44 (2.1%) | 129 (7.8%) | <.0001 | 18 (1.3%) | 73 (7.1%) | <.0001 | 26 (3.7%) | 56 (8.8%) | 0.0001 |
| History of myocardial infarction | 55 (2.6%) | 187 (11.3%) | <.0001 | 25 (1.7%) | 113 (11.0%) | <.0001 | 30 (4.3%) | 74 (11.7%) | 0.0001 |
| History of stroke | 66 (3.1%) | 117 (7.1%) | <.0001 | 40 (2.8%) | 74 (7.2%) | <.0001 | 26 (3.7%) | 43 (6.8%) | 0.0121 |
SD = standard deviation; NSAID = non-steroidal anti-inflammatory drug; Hypertension defined as >140 systolic and/or >90 diastolic blood pressures.
Table 2.
Results of the Age-Adjusted Proportional Hazards Regression of the Effect of Statin Use on AMD progression based on AMD Subtype: Hazard Ratios and 95% Confidence Limits for Unmatched for Statin Use Propensity Scores.
| All participants N=3791 |
Bilateral Large Drusen N = 2462 |
Unilateral Late AMD N = 1329 |
||||
|---|---|---|---|---|---|---|
| Hazard Ratio | 95% CI | Hazard Ratio | 95% CI | Hazard Ratio | 95% CI | |
| Any late age-related macular degeneration | ||||||
| Without accounting for the competing risk of death | 1.08 | 0.83–1.41 | 1.00 | 0.72–1.41 | 1.20 | 0.79–1.83 |
| Accounting for the competing risk of death | 0.94 | 0.72–1.22 | 0.84 | 0.60–1.18 | 1.08 | 0.71–1.65 |
| Any geographic atrophy | ||||||
| Without accounting for the competing risk of death | 1.21 | 0.85–1.73 | 1.13 | 0.74–1.73 | 1.42 | 0.74–2.73 |
| Accounting for the competing risk of death | 1.06 | 0.74–1.51 | 0.96 | 0.62–1.48 | 1.29 | 0.66–2.49 |
| Central geographic atrophy | ||||||
| Without accounting for the competing risk of death | 1.08 | 0.67–1.74 | 1.03 | 0.59–1.80 | 1.24 | 0.49–3.16 |
| Accounting for the competing risk of death | 0.92 | 0.57–1.48 | 0.85 | 0.48–1.49 | 1.14 | 0.45–2.87 |
| Neovascular age-related macular degeneration | ||||||
| Without accounting for the competing risk of death | 1.24 | 0.89–1.73 | 1.34 | 0.86–2.09 | 1.11 | 0.66–1.86 |
| Accounting for the competing risk of death | 1.07 | 0.80–1.50 | 1.12 | 0.73–1.74 | 1.00 | 0.60–1.67 |
CI = confidence interval.
Matching occurred with both participants in the bilateral large drusen group (n=1546), both in the unilateral AMD group (n=944), and one in the bilateral large drusen group and one in the other group (n=22). The baseline characteristics of these participants are displayed in Table 3. The previously statistically significant differences in the covariates, comparing statin users and the statin non-users, are no longer statistically significant, indicating the propensity matching has controlled for confounders. One problem with the propensity score matching is that although the age between statin users and non-users was similar as a whole, there was a large range in the age difference for individual pairs of propensity-matched participants, ranging from 0–30 years. Because older age is highly associated with an increased risk of development of AMD (P < 0.0001 for any AMD, any GA, central GA, and neovascular AMD), we adjusted the propensity score matched proportional hazards regression models for age.
Table 3.
Baseline Characteristics of Propensity Score-Matched Participants for Statin Use in the Entire Cohort and also in the Groups Stratified by the Baseline AMD Status.
| All participants (N = 2512)* | Bilateral Large Drusen (N = 1546) | Unilateral Late AMD (N = 944) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Statin use | Statin use | Statin use | |||||||
| No (N=1256) [N (%)] | Yes (N=1256) [N (%)] | P value | No (N=773) [N (%)] | Yes (N=773) [N (%)] | P value | No (N=472) [N (%)] | Yes (N=472) [N (%)] | P value | |
| Age (mean ± SD) | 73.3 ± 7.8 | 73.2 ± 7.4 | 0.8016 | 72.1 ± 8.2 | 72.0 ± 7.4 | 0.7559 | 75.2 ± 6.8 | 75.2 ± 6.8 | 0.9493 |
| Female | 727 (57.9%) | 697 (55.5%) | 0.2271 | 453 (58.6%) | 433 (56.0%) | 0.3038 | 264 (55.9%) | 262 (55.5%) | 0.8957 |
| White race | 1215 (96.7%) | 1213 (96.6%) | 0.8016 | 750 (97.0%) | 744 (96.2%) | 0.3973 | 460 (97.5%) | 462 (97.9%) | 0.6661 |
| Education | 0.9848 | 0.8919 | 0.8659 | ||||||
| High school or less | 412 (32.8%) | 416 (33.1%) | 220 (28.5%) | 228 (29.5%) | 185 (39.2%) | 187 (39.6%) | |||
| At least some college | 593 (47.2%) | 591 (47.1%) | 382 (49.4%) | 379 (49.0%) | 211 (44.7%) | 204 (43.2%) | |||
| Post-graduate | 251 (20.0%) | 249 (19.8%) | 171 (22.1%) | 166 (21.5%) | 76 (16.1%) | 81 (17.2%) | |||
| Smoking | 0.7388 | 0.8257 | 0.7291 | ||||||
| Never | 564 (44.9%) | 545 (43.4%) | 359 (46.4%) | 351 (45.4%) | 192 (40.7%) | 183 (38.8%) | |||
| Former | 613 (48.8%) | 628 (50.0%) | 372 (48.1%) | 375 (48.5%) | 243 (51.5%) | 255 (54.0%) | |||
| Current | 79 (6.3%) | 83 (6.6%) | 42 (5.4%) | 47 (6.1%) | 37 (7.8%) | 34 (7.2%) | |||
| Diabetes | 143 (11.4%) | 137 (10.9%) | 0.7037 | 77 (10.0%) | 67 (8.7%) | 0.3815 | 62 (13.1%) | 67 (14.2%) | 0.6357 |
| NSAID use | 126 (10.0%) | 136 (10.8%) | 0.5139 | 78 (10.1%) | 81 (10.5%) | 0.8017 | 46 (9.7%) | 49 (10.4%) | 0.7455 |
| Acetaminophen use | 130 (10.4%) | 115 (9.2%) | 0.3131 | 74 (9.6%) | 68 (8.8%) | 0.5973 | 55 (11.7%) | 52 (11.0%) | 0.7581 |
| Aspirin use | 685 (54.5%) | 668 (53.2%) | 0.4962 | 441 (57.1%) | 431 (55.8%) | 0.6080 | 232 (49.2%) | 288 (48.3%) | 0.7945 |
| Hypertension | 818 (65.1%) | 811 (64.6%) | 0.7699 | 481 (62.2%) | 483 (62.5%) | 0.9164 | 331 (70.1%) | 322 (68.2%) | 0.5259 |
| Congestive heart failure | 34 (2.7%) | 40 (3.2%) | 0.4790 | 21 (2.7%) | 22 (2.8%) | 0.8771 | 15 (3.2%) | 16 (3.4%) | 0.8551 |
| Coronary heart disease | 72 (5.7%) | 84 (6.7%) | 0.3212 | 42 (5.4%) | 47 (6.1%) | 0.5851 | 30 (6.4%) | 29 (6.1%) | 0.8930 |
| Angina | 42 (3.3%) | 45 (3.6%) | 0.7434 | 17 (2.2%) | 16 (2.1%) | 0.8603 | 25 (5.3%) | 25 (5.3%) | 1.0000 |
| History of myocardial infarction | 54 (4.3%) | 58 (4.6%) | 0.6990 | 25 (3.2%) | 31 (4.0%) | 0.4141 | 30 (6.4%) | 29 (6.1%) | 0.8930 |
| History of stroke | 60 (4.8%) | 68 (5.4%) | 0.4679 | 36 (4.7%) | 37 (4.8%) | 0.9046 | 25 (5.3%) | 33 (7.0%) | 0.2782 |
SD = standard deviation; NSAID = non-steroidal anti-inflammatory drug; Hypertension defined as >140 systolic and/or >90 diastolic blood pressures.
includes 22 participants who were matched based on propensity score with one of the pair from the bilateral large drusen group and the other from the unilateral AMD group.
Results of the propensity score matched proportional hazards regression models are shown in Table 4. The only statistically significant association found was for the outcome of any late AMD in the subgroup of patients with large drusen in both eyes in the model accounting for the competing risk of death: HR: 0.53, 95% CI 0.31–0.89, P=0.02.
Table 4.
Results of the Age-Adjusted Proportional Hazards Regression of the Effect of Statin Use on AMD Progression Based on AMD Subtype: Hazard Ratios and 95% Confidence Limits for Matched Statin Use Propensity Scores.
| All participants N = 2512* |
Bilateral Large Drusen N = 1546 |
Unilateral Late AMD N = 944 |
||||
|---|---|---|---|---|---|---|
| Hazard Ratio | 95% CI | Hazard Ratio | 95% CI | Hazard Ratio | 95% CI | |
| Any late age-related macular degeneration | ||||||
| Without accounting for the competing risk of death | 0.92 | 0.62–1.36 | 0.63 | 0.37–1.05 | 1.22 | 0.67–2.20 |
| Accounting for the competing risk of death | 0.81 | 0.55–1.20 | 0.53 | 0.31–0.89 | 1.12 | 0.62–2.01 |
| Any geographic atrophy | ||||||
| Without accounting for the competing risk of death | 1.07 | 0.63–1.82 | 0.74 | 0.38–1.43 | 1.86 | 0.76–4.56 |
| Accounting for the competing risk of death | 0.94 | 0.55–1.62 | 0.64 | 0.32–1.26 | 1.75 | 0.72–4.24 |
| Central geographic atrophy | ||||||
| Without accounting for the competing risk of death | 0.88 | 0.43–1.82 | 0.90 | 0.38–2.15 | 1.18 | 0.32–4.41 |
| Accounting for the competing risk of death | 0.76 | 0.37–1.56 | 0.76 | 0.32–1.83 | 1.14 | 0.32–4.09 |
| Neovascular age-related macular degeneration | ||||||
| Without accounting for the competing risk of death | 1.07 | 0.65–1.76 | 0.86 | 0.44–1.69 | 1.36 | 0.66–2.82 |
| Accounting for the competing risk of death | 0.92 | 0.57–1.52 | 0.73 | 0.38–1.42 | 1.25 | 0.06–2.59 |
CI = confidence interval.
includes 22 participants who were matched based on propensity score with one of the pair from the bilateral large drusen group and the other from the unilateral AMD group.
Discussion
The results from the observational data from AREDS2 showed no statistically significant effect of statin use on progression to late AMD in persons at risk. The results for the endpoints of neovascular AMD or geographic atrophy were also very similar. Compared with previous studies evaluating this association, the AREDS2 had one of the largest numbers of persons with late AMD, and greater than 40% of the AREDS2 participants were statin users.
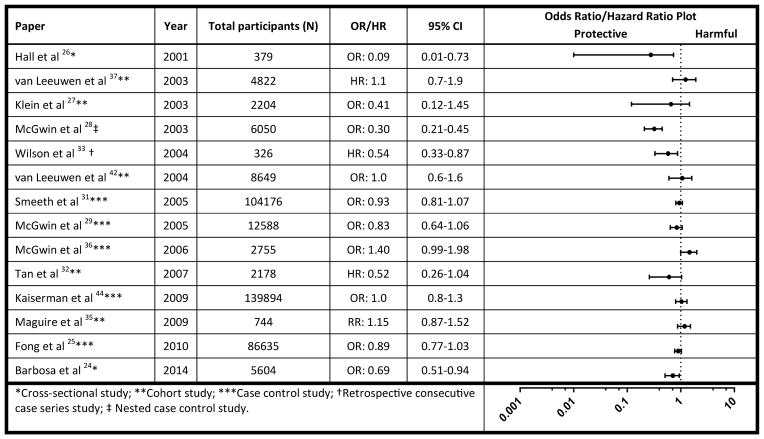
Following the initial report of the inverse association of statins with AMD by Hall et al,26 many of the subsequent reports suggested no statistically significant beneficial or harmful effect of statin use on the progression of AMD (Table 5). Some of the previous reports included large retrospective studies, but they were limited by the lack of validated methods to determine the diagnosis of late AMD because the diagnosis was based upon medical record reviews instead of the fundus photographs that were obtained in AREDS2.25,31,34,44 Another prospective study that had fundus photographs for detecting AMD lacked sufficient sample size because of small numbers of late AMD outcomes and participants taking statin.32
Table 5.
Summary of Previous Study Findings of Studies Evaluating the Association of Statin Use with Age-Related Macular Degeneration (AMD)
Cross-sectional study;
Cohort study;
Case control study;
Retrospective consecutive case series study;
Nested case control study.
The Complications of AMD Prevention Trial, the Rotterdam Study, and a study pooling three different prospective studies all found no effects of statins on AMD progression.35,37,45 These prospective studies also had fundus photographs that were graded with standardized protocol. However, these studies were again limited by the lack of large numbers of either statin users or participants with late AMD. The use of statins expanded considerably after the publication of the Scandinavian Simvastatin Survival Study (1994), which demonstrated the safety and efficacy of simvastatin. Subsequently, the use of statins increased markedly, as reflected in the high proportion of AREDS2 participants taking statins two decades later.15,46
This current AREDS2 study has limitations. We lacked information on former statin use, dosages of statins, and exact duration of treatment, although our annual questionnaire results suggested that perhaps 85% of these participants were on a statin for the average 5 year follow-up in this study. While the AREDS2 participants were part of a controlled randomized clinical trial, the data used for analyses were observational and subject to confounding. In order to control for confounding variables, common in observational studies, we used propensity scores and subsequent matching, although it was difficult to match for age by the propensity score. Because the risk factors for AMD are similar to risk factors for cardiovascular disease and statin use, it is difficult to tease out the effects of confounding entirely. We also lacked the power to evaluate the potential of statin therapy to reduce the progression to early AMD as we did not have persons with no AMD in this study population. Such a study would require an extremely large number of participants.
Ideally, the best way to evaluate the effects of statins on the progression to late AMD would be a randomized controlled clinical trial. However, randomizing people to statin use is not possible, at least for those with elevated lipids, because statin use has been demonstrated to be effective in this group. Although randomly assigning persons with normal lipid levels to statins would be feasible, there are both ethical issues and concern related to compliance for persons developing cardiovascular risk factors during the study that make this problematic. For now, the totality of evidence would suggest that statins have little influence on progression to late AMD. Because of the beneficial effects of statins in reducing the risk of cardiovascular disease and mortality, persons with AMD should be encouraged to take statins when medically indicated and to be monitored regularly for progression of AMD regardless of statin use.
Supplementary Material
Acknowledgments
Financial Support: Supported by the intramural program funds and contracts from the National Eye Institute/National Institutes of Health, Department of Health and Human Services, Bethesda Maryland (contract HHS-N-260-2005-00007-C; ADB contract NO1-EY-5-0007). Funds were generously contributed to these contracts by the following NIH institutes: Office of Dietary Supplements, National Center for Complementary and Alternative Medicine; National Institute on Aging; National Heart, Lung, and Blood Institute, and National Institute of Neurological Disorders and Stroke. The sponsor and funding organization participated in the design and conduct of the study; data collection, management, analysis and interpretation; and the preparation, review and approval of the manuscript.
This research was made possible through the NIH Medical Research Scholars Program, a public-private partnership supported jointly by the NIH and generous contributions to the Foundation for the NIH from Pfizer Inc, The Doris Duke Charitable Foundation, The Alexandria Real Estate Equities, Inc. and Mr. and Mrs. Joel S. Marcus, and the Howard Hughes Medical Institute, as well as other private donors. For a complete list, please visit the Foundation website at: http://fnih.org/work/education-training-0/medical-research-scholars-program.
Appendix 1 The Age-Related Eye Disease Study 2 (AREDS2) Research Group
(NEI) National Eye Institute
Emily Y. Chew, MD, Study Chair
Frederick L. Ferris III, MD, NEI Clinical Director
John Paul SanGiovanni, ScD, Project Officer
Elvira Agrón, MA, Statistician
Coordinating Center, The EMMES Corporation
Traci Clemons, PhD, Principal Investigator
Anne Lindblad, PhD, Co-Investigator
Robert Lindblad, MD, Chief Medical Officer
Nilay Shah, MD, Medical Monitor
Robert Sperduto, MD, Consultant
Wendy McBee, MA, AREDS2 Project Director
Gary Gensler, MS, Statistician
Molly Harrington, MS, Statistician
Alice Henning, MS, Genetics Project Director
Katrina Jones Data Manager
Kumar Thotapally Programmer
Diana Tull, MA, CPS, Administrative Coordinator
Valerie Watson Systems Coordinator
Kayla Williams Data Manager
Christina Gentry, Cognitive Function Specialist
Francine Kaufman Cog. Function/Data Mgr
Chris Morrison, Cognitive Function Specialist
Elizabeth Saverino Protocol Monitor
Sherrie Schenning Protocol Monitor
Fundus Photograph Reading Center
Barbara Blodi, MD, Co-PI
Ronald P. Danis, MD, Principal Investigator
Matthew Davis, MD, Co-PI
Amitha Domalpally Co-Director
Kathy Glander Research Project Mgr
Gregory Guilfoil Research Project Mgr
Larry D. Hubbard, MA, Assoc. Dir. Grading
Kristine Johnson Inventory Assistant
Ronald Klein, MD, Co-PI
Barbara Nardi Asst. to Ron Danis
Michael Neider Assoc. Dir. Photography
Nancy Robinson Assoc. Dir Operations
Eileen Rosensteel Inventory Assistant
Hugh Wabers Photographer
Grace Zhang AREDS2 Data Manager
(001) Vision Research Foundation
Alan J. Ruby, MD, (Site PI)
Antonio Capone, Jr., MD, (Ophthalmologist)
Bawa Dass, MD, (Ophthalmologist)
Kimberly Drenser, MD, PhD, (Ophthalmologist)
Bruce R. Garretson, MD, (Ophthalmologist)
Tarek S. Hassan, MD, (Ophthalmologist)
Michael Trese, MD, (Ophthalmologist)
George A. Williams, MD, (Ophthalmologist)
Jeremy Wolfe, MD, (Ophthalmologist)
Tina Bell (Clinic Coordinator)
Mary Zajechowski (Clinic Coordinator)
Dennis Bezaire (Photographer)
Fran McIver (Photographer)
Anthony Medina, CRA, (Photographer)
Jackie Pagett (Photographer)
Stephanie Hatch Smith (Photographer)
Lynn Swartz (Photographer)
Tom Treuter (Photographer)
(002) Charlotte Eye Ear Nose and Throat Associates
Andrew Antoszyk, MD, (Site PI)
Justin Brown, MD, (Ophthalmologist)
David J. Browning, MD, PhD, (Ophthalmologist)
Walter Holland, MD, (Ophthalmologist)
Angella Karow (Clinic Coordinator)
Kelly Stalford (Clinic Coordinator)
Angela Price, MPH, CCRC, Dir. Of Research
Sarah Ennis (Ophthalmic Technician)
Sherry Fredenberg (Ophthalmic Technician)
Jenna Herby (Ophthalmic Technician)
Uma Balasubramaniam (Photographer)
Loraine Clark (Photographer)
Donna McClain (Photographer)
Michael McOwen, CRA, (Photographer)
Lynn Watson (Photographer)
(003) Devers Eye Institute
Michael Klein, MD, (Site PI)
Steven T. Bailey, MD, (Ophthalmologist)
Thomas J. Hwang, MD, (Ophthalmologist)
Andreas Lauer, MD, (Ophthalmologist)
J. Timothy Stout, MD, PhD, FACS, (Ophthalmologist)
Patty McCollum (Clinic Coordinator)
Milt Johnson (Photographer)
Patrick B. Rice CRA (Photographer)
(004) Massachusetts Eye and Ear Infirmary
Ivana Kim, MD, (Site PI)
John Loewenstein, MD, (Ophthalmologist)
Joan Miller, MD, (Ophthalmologist)
Lucia Sobrin, MD, (Ophthalmologist)
Lucy Young, MD, PhD, (Ophthalmologist)
Jacqueline Sullivan (Clinic Coordinator)
Patricia Houlihan (Assistant Coordinator)
Linda Merry, RN, (Assistant Coordinator)
Ann Marie Lane (Office Manager)
Ursula Lord Bator, OD, (Ophthalmic Technician)
Claudia Evans, OD, (Ophthalmic Technician)
Sarah Brett (Photographer)
Charleen Callahan (Photographer)
Marcia Grillo (Photographer)
David Walsh (Photographer)
Kamella Lau Zimmerman (Photographer)
(005) Texas Retina Associates
Gary Edd Fish, MD, JD, (Site PI)
Rajiv Anand, MD, (Ophthalmologist)
Lori E. Coors, MD, (Ophthalmologist)
Dwain G. Fuller, MD, (Ophthalmologist)
Rand Spencer, MD, (Ophthalmologist)
Robert C. Wang, MD, (Ophthalmologist)
Karen Duignan (Clinic Coordinator)
Sally Arceneaux, COA, (Assistant Coordinator)
Hank Aguado, CRA, (Photographer)
Nicholas Hesse (Photographer)
Michael Mackens (Photographer)
Brian Swan (Photographer)
(006) National Eye Institute
Wai T. Wong, MD, PhD, (Site PI)
Catherine Cukras, MD, (Ophthalmologist)
Monica Dalal, MD, (Ophthalmologist)
Naima Jacobs-El, MD, (Ophthalmologist)
Catherine Meyerle, MD, (Ophthalmologist)
Benjamin Nicholson, MD, (Ophthalmologist)
Henry Wiley, MD, (Ophthalmologist)
Katherine Hall Shimel, RN, COT, MSN, (Clinic Coordinator)
Angel Garced, RN, (Assistant Coordinator)
Janice Oparah, RN, (Assistant Coordinator)
Greg Short, COMT, (Assistant Coordinator)
Alana Temple, RN, (Assistant Coordinator)
Babilonia Ayukawa, RN, (Phlebotomist)
Guy Foster, COT, (Ophthalmic Technician)
Darryl Hayes, COA, (Ophthalmic Technician)
Dessie Koutsandreas (Ophthalmic Technician)
Roula Nashwinter (Ophthalmic Technician)
John Rowan (Ophthalmic Technician)
Emily Y. Chew, MD, Study Chair (Project Sponsor Staff (NEI))
Michael Bono (Photographer)
Denise Cunningham (Photographer)
Marilois Palmer (Photographer)
Alicia Zetina (Photographer)
(007) Ingalls Memorial Hospital
David H. Orth, MD, (Site PI)
Kourous Rezaei, MD, Co-PI (Site Co-PI)
Joseph Civantos, MD, (Ophthalmologist)
Sohail Hasan, MD, PhD, (Ophthalmologist)
Kirk Packo, MD, (Ophthalmologist)
Celeste Figliulo (Clinic Coordinator)
Pam Stanberry (Phlebotomist)
Tara Farmer (Photographer)
Kiersten Nelson (Photographer)
Shannya Townsend-Patrick (Photographer)
(008) Bascom Palmer Eye Institute
Philip Rosenfeld, MD, PhD, (Site PI)
Royce Chen, MD, (Ophthalmologist)
Rishi Doshi, MD, (Ophthalmologist)
Sander Dubovy, MD, (Ophthalmologist)
Brian T. Kim, MD, (Ophthalmologist)
Matthew Lowrance, DO, (Ophthalmologist)
Andrew Moshfeghi, MD, (Ophthalmologist)
Zayna Nahas, MD, (Ophthalmologist)
Gary Schienbaum, MD, (Ophthalmologist)
John Vishak, MD, (Ophthalmologist)
Christina Weng, MD, (Ophthalmologist)
Zohar Yehoshua, MD, (Ophthalmologist)
Belen Rodriguez (Clinic Coordinator)
Jose Rebimbas (Assistant Coordinator)
Jane Gleichauf, RN, (Phlebotomist)
Mike Kicak (Ophthalmic Technician)
Jason Mena (Ophthalmic Technician)
Tim Odem (Ophthalmic Technician)
Elizabeth Sferza-Camp (Ophthalmic Technician)
Alicia Disgdiertt (Photographer)
Jim Oramas (Photographer)
Isabel Rams (Photographer)
Stephanie Thatcher (Photographer)
(009) The Retina Division at the Wilmer Eye Institute
Susan B. Bressler, MD, (Site PI)
Neil M. Bressler, MD, (Ophthalmologist)
Daniel Finkelstein, MD, (Ophthalmologist)
Steven H Sherman, MD, (Ophthalmologist)
Sharon Solomon, MD, (Ophthalmologist)
Howard S. Ying, MD, (Ophthalmologist)
Rita Denbow (Clinic Coordinator)
Deborah Phillips (Assistant Coordinator)
Elizabeth Radcliffe (Phlebotomist)
Judy Belt (Photographer)
Dennis Cain (Photographer)
David Emmert (Photographer)
Mark Herring (Photographer)
Jacquelyn McDonald (Photographer)
(010) Emory University Eye Center
G. Baker Hubbard, MD, (Site PI)
Chris S Bergstrom, MD, (Ophthalmologist)
Blaine Cribbs, MD, (Ophthalmologist)
Andrew Hendrick, MD, (Ophthalmologist)
Brandon Johnson, MD, (Ophthalmologist)
Philip Laird, MD, (Ophthalmologist)
Sonia Mehta, MD, (Ophthalmologist)
Timothy Olsen, MD, (Ophthalmologist)
Justin Townsend, MD, (Ophthalmologist)
Jion Yan, MD, (Ophthalmologist)
Steven Yeh, MD, (Ophthalmologist)
Linda Curtis, BSM, (Clinic Coordinator)
Judy Brower (Assistant Coordinator)
Hannah Yi (Assistant Coordinator)
Jannah Rutter Dobbs (Photographer)
Debbie Jordan (Photographer)
(011) Elman Retina Group, PA
Michael J. Elman, MD, (Site PI)
Robert A Liss, MD, (Ophthalmologist)
JoAnn Starr (Clinic Coordinator)
Jennifer Belz (Assistant Coordinator)
Charlene Putzulo (Assistant Coordinator)
Teresa Coffey (Ophthalmic Technician)
Ashley Davis (Ophthalmic Technician)
Pamela Singletary (Ophthalmic Technician)
Giorya Shabi Andreani (Photographer)
Theresa Cain (Photographer)
Daniel Ketner (Photographer)
Peter Sotirakos (Photographer)
(012) University of Wisconsin
Suresh Chandra, MD, (Site PI)
Barbara A. Blodi, MD, (Site Co-PI)
Michael M. Altaweel, MD, (Ophthalmologist)
Ronald P. Danis, MD, (Ophthalmologist)
Justin L. Gottlieb, MD, (Ophthalmologist)
Michael Ip, MD, (Ophthalmologist)
Ronald Klein, MD, (Ophthalmologist)
T. Michael Nork, MD, (Ophthalmologist)
Thomas S. Stevens, MD, (Ophthalmologist)
Kathryn Burke (Clinic Coordinator)
Shelly Olson (Clinic Coordinator)
Kristine Dietzman (Assistant Coordinator)
Barbara Soderling (Assistant Coordinator)
Guy Somers, RN, (Assistant Coordinator)
Angie Wealti (Assistant Coordinator)
Denise Krolnik (Photographer)
John Peterson (Photographer)
Sandra Reed (Photographer)
(013) UPMC Eye Center
Thomas Friberg, MD, (Site PI)
Andrew Eller, MD, (Ophthalmologist)
Denise Gallagher, MD, (Ophthalmologist)
Leanne Labriola, DO, (Ophthalmologist)
Melissa Pokrifka (Clinic Coordinator)
Aron Gedansky (Assistant Coordinator)
Natalie Anthony (Photographer)
Cassandra Grzybowski (Photographer)
Dawn Matthews (Photographer)
Sharon Murajda-Jumba (Photographer)
Jessica Toro (Photographer)
(014) Texas Retina Associates
Gary Edd Fish, MD, JD, (Site PI)
David G. Callanan, MD, (Ophthalmologist)
Wayne A. Solley, MD, (Ophthalmologist)
Patrick Williams, MD, (Ophthalmologist)
Sandy Lash (Clinic Coordinator)
Bob Boleman (Photographer)
Chris Dock (Photographer)
(015) Texas Retina Associates
Gary Edd Fish, MD, JD, (Site PI)
Michel Shami, MD, (Ophthalmologist)
Brenda Arrington (Clinic Coordinator)
Ashaki Meeks (Ophthalmic Technician)
(017) Vision Research Foundation
Alan J. Ruby, MD, (Site PI)
Alan R Margherio, MD, (Ophthalmologist)
Paul Raphaelian, MD, (Ophthalmologist)
Debra Markus (Clinic Coordinator)
Justin Langdon (Ophthalmic Technician)
Elizabeth Truax (Ophthalmic Technician)
Sandy Lewis (Photographer)
Brad Terry (Photographer)
(018) Vision Research Foundation
Alan J. Ruby, MD, (Site PI)
Amy Noffke, MD, (Ophthalmologist)
Kean Oh, MD, (Ophthalmologist)
Ramin Sarrafizadeh, MD, PhD, (Ophthalmologist)
Scott Sneed, MD, (Ophthalmologist)
Julie Hammersley, RN, (Clinic Coordinator)
Serena Neal (Assistant Coordinator)
Mary Doran (Ophthalmic Technician)
Nan Jones (Ophthalmic Technician)
Lisa Preston (Ophthalmic Technician)
Heather Jessick (Photographer)
Tanya Tracy Marsh (Photographer)
(020) Center for Retina and Macular Disease
Michael Tolentino, MD, (Site PI)
Adam Berger, MD, (Ophthalmologist)
Richard Hamilton, MD, (Ophthalmologist)
David Misch, MD, (Ophthalmologist)
Suk Jin Moon, MD, (Ophthalmologist)
Dawn Sutherland (Clinic Coordinator)
Vera Dilts (Assistant Coordinator)
Sara Henderson (Assistant Coordinator)
Esmeralda Medina (Assistant Coordinator)
Donald Trueman (Assistant Coordinator)
Laura Holm, LPN, (Ophthalmic Technician)
Jason Strickland (Photographer)
(021) Delaware Valley Retina Associates
Darmakusuma Ie, MD, (Site PI)
Jeffrey L. Lipkowitz MD(Ophthalmologist)
Kekul B. Shah, MD, (Ophthalmologist)
Susan Geraghty (Clinic Coordinator)
Beverly Sannazzaro (Clinic Coordinator)
Morgan Harper (Ophthalmic Technician)
Krista Bayer (Photographer)
(022) Eldorado Retina Associates, PC
Mary B. Lansing, MD, (Site PI)
Lauren B. Fox (Clinic Coordinator)
Rebecca Lee (Photographer)
(023) Georgia Retina, PC
Jay B. Stallman, MD, FACS, (Site PI)
Michael Jacobson, MD, (Ophthalmologist)
Sean Koh, MD, (Ophthalmologist)
Scott Lampert, MD, (Ophthalmologist)
John Miller, MD, (Ophthalmologist)
Mark Rivellese, MD, (Ophthalmologist)
Atul Sharma, MD, (Ophthalmologist)
Robert A. Stoltz, MD, (Ophthalmologist)
Stephanie Vanderveldt, MD, (Ophthalmologist)
Leslie Marcus (Clinic Coordinator)
Starr Hendricks (Assistant Coordinator)
Ryan Hollman (Assistant Coordinator)
Grethel Betanzos (Ophthalmic Technician)
Leslie Ellorin (Ophthalmic Technician)
Shelly Fulbright (Ophthalmic Technician)
Debbie McCormick (Photographer)
(024) Henry Ford Health System - Eye Care Services
Paul A. Edwards, MD, (Site PI)
Julianne Hall (Clinic Coordinator)
Mary Monk (Clinic Coordinator)
Melanie Gutkowski (Assistant Coordinator)
Melina Mazurek (Assistant Coordinator)
Janet Murphy (Assistant Coordinator)
Katherine Gusas (Office Manager)
Crystal Moffett (Office Manager)
David Burley (Photographer)
Nicole Chesney (Photographer)
Katie Kilgo (Photographer)
Brian Rusinek (Photographer)
Bradley Stern (Photographer)
Tracy Troszak (Photographer)
Rhonda Baker-Levingston (Pharmacist)
(025) Paducah Retinal Center
Carl W. Baker, MD, (Site PI)
Tracey Caldwell (Clinic Coordinator)
Tammy Walker (Assistant Coordinator)
Lynnette F. Lambert (Ophthalmic Technician)
Tracey Martin (Ophthalmic Technician)
Mary Jill Palmer (Ophthalmic Technician)
Tana Williams (Photographer)
(026) Retina Associates of Cleveland
Michael A Novak, MD, (Site PI)
Joseph Coney, MD, (Ophthalmologist)
David G. Miller, MD, (Ophthalmologist)
Scott Pendergast, MD, (Ophthalmologist)
Lawrence Singerman, MD, (Ophthalmologist)
Nicholas Zakov, MD, (Ophthalmologist)
Hernando Zegarra, MD, (Ophthalmologist)
Kim DuBois (Clinic Coordinator)
Susan Rath (Clinic Coordinator)
Lori Revella (Clinic Coordinator)
Tammy Brink (Ophthalmic Technician)
Kim Drury (Ophthalmic Technician)
Lisa Hogue (Ophthalmic Technician)
Mary Ilc (Ophthalmic Technician)
Connie Keller (Ophthalmic Technician)
Elizabeth McNamara (Ophthalmic Technician)
Vivian Tanner (Ophthalmic Technician)
Tamara Cunningham (Photographer)
John DuBois (Photographer)
Gregg Greanoff (Photographer)
Trina Nitzsche (Photographer)
Sheila Smith-Brewer (Photographer)
(027) Retina Associates of Kentucky
Ricky D. Isernhagen, MD, (Site PI)
John W. Kitchens, MD, (Ophthalmologist)
Thomas W. Stone, MD, (Ophthalmologist)
William J. Wood, MD, (Ophthalmologist)
Diana Holcomb (Clinic Coordinator)
Virginia Therrien (Office Manager)
Michelle Buck, COT, (Ophthalmic Technician)
Jeanne Van Arsdall (Ophthalmic Technician)
Edward Slade, CRA, COA, (Photographer)
(029) Retina Center Northwest
Todd E. Schneiderman, MD, (Site PI)
David J. Spinak, MD, (Ophthalmologist)
Jackie Gaedke (Clinic Coordinator)
Heather Davis Brown (Assistant Coordinator)
Dan Helgren (Assistant Coordinator)
Jenifer Garrison Pangelinan (Photographer)
(030) Retina Group of Florida
Lawrence Halperin, MD, (Site PI)
Scott Anagnoste, MD, (Ophthalmologist)
Mandeep Dhalla, MD, (Ophthalmologist)
Krista Rosenberg, MD, (Ophthalmologist)
Barry Taney, MD, (Ophthalmologist)
W. Scott Thompson, MD, (Ophthalmologist)
Jaclyn Lopez (Clinic Coordinator)
Monica Hamlin (Assistant Coordinator)
Monica Lopez (Assistant Coordinator)
Jamie Mariano, COA, (Ophthalmic Technician)
Evelyn Quinchia (Ophthalmic Technician)
Patricia Aramayo (Photographer)
Rita Veksler (Photographer)
(031) Retina Northwest, PC
Michael Lee, MD, (Site PI)
Richard Dreyer, MD, (Ophthalmologist)
Irvin Handelman, MD, (Ophthalmologist)
Colin Ma, MD, (Ophthalmologist)
Mark Peters, MD, (Ophthalmologist)
Stephen Hobbs III (Clinic Coordinator)
Amanda Milliron (Assistant Coordinator)
Marcia Kopfer (Ophthalmic Technician)
Michele Connaughton (Photographer)
A. Christine Hoerner (Photographer)
R. Joseph Logan (Photographer)
Harry J. Wohlsein (Photographer)
(032) Retina-Vitreous Associates Medical Group
David Boyer, MD, (Site PI)
Thomas G. Chu, MD, PhD, (Ophthalmologist)
Pouya Dayani, MD, (Ophthalmologist)
David Liao, MD, (Ophthalmologist)
Roger L. Novack, MD, PhD, (Ophthalmologist)
Firas M. Rahhal, MD, (Ophthalmologist)
Richard Roe, MD, (Ophthalmologist)
Homayoun Tabandeh, MD, (Ophthalmologist)
Janet Bayramyan (Clinic Coordinator)
Tammy Gasparyan (Assistant Coordinator)
Connie Hoang (Assistant Coordinator)
Janet Kurokouchi (Assistant Coordinator)
Tammy Eileen Lo (Assistant Coordinator)
Richard Ngo (Assistant Coordinator)
Mary Ann Nguyen (Assistant Coordinator)
Michael Peyton (Assistant Coordinator)
Charles Yoon (Assistant Coordinator)
Julio Sierra (Ophthalmic Technician)
Adam Zamboni (Ophthalmic Technician)
Jeff Kessinger (Photographer)
Eric Protacio (Photographer)
Adam Smucker (Photographer)
(033) Retina Vitreous Consultants
Pamela Rath, MD, (Site PI)
Robert Bergren, MD, (Ophthalmologist)
Bernard Doft, MD, (Ophthalmologist)
Judy Liu, MD, (Ophthalmologist)
Karl Olsen, MD, (Ophthalmologist)
Lori Merlotti (Clinic Coordinator)
Willia Ingram (Assistant Coordinator)
Kellianne Marfisi (Ophthalmic Technician)
Kimberly Yeckel (Ophthalmic Technician)
Heather Schultz Carmelo (Photographer)
Amanda Fec (Photographer)
Keith McBroom (Photographer)
David Steinberg (Photographer)
(034) Sarasota Retina Institute
Marc Levy, MD, (Site PI)
Jody Abrams, MD, (Ophthalmologist)
Melvin Chen, MD, (Ophthalmologist)
Waldemar Torres, MD, (Ophthalmologist)
Peggy Jelemensky (Clinic Coordinator)
Mark Prybylski (Ophthalmic Technician)
Tara Raphael (Ophthalmic Technician)
Diana Appleby (Photographer)
Charlotte Rodman (Photographer)
Mark Sneath, COA, (Photographer)
(035) Scott and White Memorial Hospital
Robert H. Rosa, Jr., MD, (Site PI)
Vanessa Hoelscher (Clinic Coordinator)
Adelia Castano (Ophthalmic Technician)
Jocelyn Parker (Photographer)
(036) Southeastern Retina Associates, PC
John Hoskins, MD, (Site PI)
Nicholas Anderson, MD, (Ophthalmologist)
Joseph Googe, Jr., MD, (Ophthalmologist)
Tod A McMillan, MD, (Ophthalmologist)
James Miller Jr., MD, (Ophthalmologist)
Stephen Perkins, MD, (Ophthalmologist)
Kristina Oliver (Clinic Coordinator)
Jennifer Beerbower (Ophthalmic Technician)
Bruce Gilliland, OD, (Ophthalmic Technician)
Cecile Hunt (Ophthalmic Technician)
Mike Jacobus (Photographer)
Raul Lince (Photographer)
Christopher Morris (Photographer)
Sarah Oelrich (Photographer)
Jerry Whetstone (Photographer)
(037) Southern California Desert Retina Consultants, MC
Clement K. Chan, MD, (Site PI)
Steven Lin, MD, (Ophthalmologist)
Kim Walther (Clinic Coordinator)
Tiana Gonzales (Assistant Coordinator)
Lenise Myers (Ophthalmic Technician)
Kenneth Huff, COA, (Photographer)
(038) Retina Consultants of Houston
David M. Brown, MD, (Site PI)
Eric Chen, MD (Ophthalmologist)
Matthew S. Benz, MD, (Ophthalmologist)
Richard H. Fish, MD, FACS, (Ophthalmologist)
Rosa Y. Kim, MD, (Ophthalmologist)
James Major Jr, MD, (Ophthalmologist)
Tien Pei Wong, MD, (Ophthalmologist)
Charles Wycoff, MD, PhD, (Ophthalmologist)
Cassandra Cone (Clinic Coordinator)
Debbie Goates Gilaspia (Assistant Coordinator)
Nubia Landaverde (Assistant Coordinator)
Robert Smith (Assistant Coordinator)
Deneva Zamora (Assistant Coordinator)
Veronica Sneed (Ophthalmic Technician)
Melina Vela (Ophthalmic Technician)
Eric Kegley (Photographer)
(039) Wake Forest University Eye Center
Craig Greven, MD, (Site PI)
Shree Kurup, MD, (Ophthalmologist)
Charles Richards, MD, (Ophthalmologist)
Madison Slusher, MD, (Ophthalmologist)
Cara Everhart (Clinic Coordinator)
Joan Fish, RN, CCRC, (Assistant Coordinator)
Mark Clark (Photographer)
David Miller (Photographer)
Marshall Tyler, CRA, FOPS, (Photographer)
(040) West Coast Retina Medical Group, Inc
J. Michael Jumper, MD, (Site PI)
Arthur D. Fu, MD, (Ophthalmologist)
Robert N. Johnson, MD, (Ophthalmologist)
Brandon Lujan, MD, (Ophthalmologist)
H. Richard McDonald, MD, (Ophthalmologist)
Rosa Rodriguez (Clinic Coordinator)
Nina Ansari (Ophthalmic Technician)
Jeanifer Joaquin (Ophthalmic Technician)
Silvia Linares (Ophthalmic Technician)
Lizette Lopez (Ophthalmic Technician)
Jessica Sabio (Ophthalmic Technician)
Sean Grout (Photographer)
Chad Indermill (Photographer)
Yesmin Urias (Photographer)
Roberto Zimmerman (Photographer)
(041) Veterans Affairs - Northern California Health Care System
Linda Margulies, MD, (Site PI)
Sara J. Schmidt, PharmD, (Clinic Coordinator)
Joy L. Meier, PharmD, (Assistant Coordinator)
Sherry L. Hadley COT(Ophthalmic Technician)
(042) Mid-America Retina Consultants, PA
William Rosenthal, MD, (Site PI)
Barbara Johnson, RN, (Clinic Coordinator)
Lois Swafford (Office Manager)
Richard Shields, RN, (Ophthalmic Technician)
R. Scott Varner (Photographer)
(043) New York Eye and Ear Infirmary
Richard Rosen, MD, (Site PI)
Ronald Gentile, MD, (Ophthalmologist)
Melissa Rivas (Clinic Coordinator)
Katy W. Tai, CRC, (Assistant Coordinator)
Wanda Carrasquillo-Boyd (Photographer)
Robert Masini (Photographer)
(044) Ophthalmic Consultants of Long Island
Glenn Stoller, MD, (Site PI)
Ken Carnevale, MD, (Ophthalmologist)
Diane M. LaRosa, CRNO, (Clinic Coordinator)
Barbara Burger, RN, CCRC, (Assistant Coordinator)
Tereza Conway (Assistant Coordinator)
Carla Del Castillo (Assistant Coordinator)
Julissa Diaz (Assistant Coordinator)
Susan Jones (Assistant Coordinator)
Nina Mondoc (Assistant Coordinator)
Charlene Balfour (Ophthalmic Technician)
CH Vitha (Ophthalmic Technician)
Jennifer Lutz (Photographer)
Barbara McGinley (Photographer)
(045) The Research Foundation of SUNY/SB
Fadi El Baba, MD, (Site PI)
Ann Marie Lavorna (Clinic Coordinator)
Renee Jones (Assistant Coordinator)
Jean Lewis (Assistant Coordinator)
Ruth Tenzler, RN, BSN, (Assistant Coordinator)
Mary Salvas-Mladek, CRA, (Ophthalmic Technician)
Diane Van Kesteren, COA, (Ophthalmic Technician)
(046) Western Carolina Retinal Associates
W. Copley McLean, Jr., MD, (Site PI)
W. Zachery Bridges, Jr., MD, (Ophthalmologist)
Cameron Stone, MD, (Ophthalmologist)
Denise Ammons (Clinic Coordinator)
Mary Lamy (Assistant Coordinator)
Andrea Menzel (Assistant Coordinator)
Lea Doll Raymer (Assistant Coordinator)
Barbara Campbell (Ophthalmic Technician)
Lisa Hawkins (Ophthalmic Technician)
Leslie Rickman (Ophthalmic Technician)
Lorraine Sherlin (Ophthalmic Technician)
Paula Price (Photographer)
Albert Sinyai (Photographer)
(047) Dean McGee Eye Institute
Ronald Kingsley, MD, (Site PI)
Reagan H. Bradford, Jr., MD, (Ophthalmologist)
Robert E. Leonard II, MD, (Ophthalmologist)
Sonny Icks (Clinic Coordinator)
Vanessa Bergman (Ophthalmic Technician)
Brittany Ross (Ophthalmic Technician)
Russ Burris (Photographer)
Amanda Butt (Photographer)
Rob Richmond (Photographer)
(048) Northwestern University, Ophthalmology
Alice Lyon, MD, (Site PI)
Manjot Gill, MD, (Ophthalmologist)
Lee Jampol, MD, (Ophthalmologist)
Rukhsana Mizra, MD, (Ophthalmologist)
Zuzanna Rozenbajgier (Clinic Coordinator)
Jeremy Chapman (Assistant Coordinator)
Lori Kaminski (Assistant Coordinator)
Andrea Degillio (Photographer)
Evica Simjanoski, CRA, (Photographer)
(049) Ophthalmic Consultants of Boston
Jeffrey Heier, MD, (Site PI)
Hyung Cho, MD, (Ophthalmologist)
Tina Scheufele Cleary, MD, (Ophthalmologist)
Darin Goldman, MD, (Ophthalmologist)
Chirag Shah, MD, (Ophthalmologist)
Trexler Topping, MD, (Ophthalmologist)
Marissa Weber, MD, (Ophthalmologist)
Torsten Wiegand, MD, PhD, (Ophthalmologist)
Jeremy Schindelheim (Clinic Coordinator)
Joy Bankert (Assistant Coordinator)
Jennifer Stone (Assistant Coordinator)
Alison Nowak (Office Manager)
Sandy Chong (Ophthalmic Technician)
Lindsay Williams (Ophthalmic Technician)
Steven Bennett (Photographer)
Dennis Donovan (Photographer)
Margaret Graham (Photographer)
Cullen Jones (Photographer)
(050) Pacific Eye Associates
Anne Fung, MD, (Site PI)
Jan-Kristine Bayabo (Clinic Coordinator)
Razelda Bosch (Assistant Coordinator)
Esperanza Cruz (Assistant Coordinator)
Ashley Emerson (Assistant Coordinator)
Alycia Fleming (Ophthalmic Technician)
Denice Barsness (Photographer)
Jorge Rodriguez (Photographer)
Marina Soboleva (Photographer)
(051) Penn State M.S. Hershey Medical Center
Ingrid U. Scott, MD, MPH, (Site PI)
Esther Bowie, MD, (Ophthalmologist)
Kimberly A Neely, MD, PhD, (Ophthalmologist)
David A. Quillen, MD, (Ophthalmologist)
Laura Walter (Clinic Coordinator)
Timothy Bennett (Photographer)
James Strong (Photographer)
(052) Palmetto Retina Center
John Wells, III, MD, (Site PI)
Lloyd Clark, MD, (Ophthalmologist)
David Johnson, MD, (Ophthalmologist)
Peggy Miller (Clinic Coordinator)
Mallie Taylor (Assistant Coordinator)
Tiffany Swinford (Ophthalmic Technician)
Robbin Spivey (Photographer)
(053) Pennsylvania Retina Specialists, PC
Michael Banach, MD, (Site PI)
Lawrence Ho, MD, (Ophthalmologist)
Richard Lanning, MD, (Ophthalmologist)
Thomas R Pheasant, MD, (Ophthalmologist)
Jay G Prensky, MD, (Ophthalmologist)
Steven Truong, MD, (Ophthalmologist)
Julia Teatsworth, COT, (Clinic Coordinator)
Michelle Dietrich (Assistant Coordinator)
Ann Wasilus (Phlebotomist)
Ann Miller (Ophthalmic Technician)
Megan Rakes (Ophthalmic Technician)
Teresa Slagle (Ophthalmic Technician)
Michelle Richards (Photographer)
Patricia Schuessler (Photographer)
Lacy Stover (Photographer)
(054) Retina Consultants, PLLC
Paul Beer, MD, (Site PI)
Naomi S. Falk, MD, (Ophthalmologist)
Mary Beth Shannon (Clinic Coordinator)
Jeannie Olmeda (Ophthalmic Technician)
Don Berdeen (Photographer)
Joseph F. Fisher, Jr. (Photographer)
(055) University of Iowa
James Folk, MD, (Site PI)
Stephen Russell, MD, (Ophthalmologist)
Barbara Taylor (Clinic Coordinator)
Connie Hinz (Assistant Coordinator)
Jean Walshire (Assistant Coordinator)
Heather Stockman (Ophthalmic Technician)
Bruce Critser (Photographer)
Stefani Karakas (Photographer)
Cindy Montague (Photographer)
Randy Verdick (Photographer)
(056) Wills Eye Hospital/Mid Atlantic Retina
Omesh Gupta, MD, (Site PI)
Joseph Maguire, MD, (Site PI)
Christopher Brady, MD, (Ophthalmologist)
Francis Char DeCroos, MD, (Ophthalmologist)
Michael Dollin, MD, (Ophthalmologist)
Sunir Garg, MD, (Ophthalmologist)
Adam Gerstenblith, MD, (Ophthalmologist)
Julia Haller, MD, (Ophthalmologist)
Allen C. Ho, MD, (Ophthalmologist)
Jason Hsu, MD, (Ophthalmologist)
Richard Kaiser, MD, (Ophthalmologist)
John Pitcher, MD, (Ophthalmologist)
Carl Regillo, MD, (Ophthalmologist)
Rajiv Shah, MD, (Ophthalmologist)
Marc Spirn, MD, (Ophthalmologist)
William Tasman, MD, (Ophthalmologist)
James Vander, MD, (Ophthalmologist)
Noga Senderowitsch (Clinic Coordinator)
Michele Formoso (Assistant Coordinator)
Michelle Markun (Assistant Coordinator)
Cedric George
Christina Centinaro (Ophthalmic Technician)
Lisa Grande (Ophthalmic Technician)
Stefanie Carey (Photographer)
Elaine Liebenbaum (Photographer)
(057) Doheny Eye Institute USC
SriniVas Sadda, MD, (Site PI)
Mark Humayun, MD, PhD, (Ophthalmologist)
Rachel Sierra (Clinic Coordinator)
Elizabeth Corona (Assistant Coordinator)
Margaret Padilla (Assistant Coordinator)
Moonseok Nu (Office Manager)
Sylvia Ramos (Ophthalmic Technician)
Cullen Barnett (Photographer)
Glenn Currie (Photographer)
Cornelia Gottlieb (Photographer)
(058) The Retina Group of Washington
Richard Garfinkel, MD, (Site PI)
Daniel Berinstein, MD, (Ophthalmologist)
Marcus Colyer, MD, (Ophthalmologist)
William Deegan, III, MD, (Ophthalmologist)
Michael Min-Shyue Lai, MD, (Ophthalmologist)
Robert Murphy, MD, (Ophthalmologist)
Michael Osman, MD, (Ophthalmologist)
Michael Rivers, MD, (Ophthalmologist)
Reginald Sanders, MD, (Ophthalmologist)
Manfred A. von Fricken, MD, (Ophthalmologist)
Debbie Oliver (Clinic Coordinator)
Jeanne Kirshon (Assistant Coordinator)
Tanya Alexander Snowden (Assistant Coordinator)
Thomas Blondo (Ophthalmic Technician)
Alysia Cronise (Ophthalmic Technician)
Vanessa Denny (Ophthalmic Technician)
Kylie Mendez (Ophthalmic Technician)
Janine Newgen (Ophthalmic Technician)
Justin Davis (Photographer)
Mike Flory (Photographer)
Robert Frantz (Photographer)
Bryan Murphy (Photographer)
Steve Rauch (Photographer)
(060) The Medical College of Wisconsin
Judy E. Kim, MD, (Site PI)
Jane Bachman, OD, (Ophthalmologist)
Thomas B. Connor, Jr., MD, (Ophthalmologist)
Dennis P. Han, MD, (Ophthalmologist)
Kimberly Stepian, MD, (Ophthalmologist)
David V. Weinberg, MD, (Ophthalmologist)
William J. Wirostko, MD, (Ophthalmologist)
Krissa Packard (Clinic Coordinator)
Tracy Kaczanowski (Assistant Coordinator)
Vesper Williams (Assistant Coordinator)
Vicki Barwick (Ophthalmic Technician)
Judy Flanders (Ophthalmic Technician)
Dennis Backes (Photographer)
Joe Beringer (Photographer)
Kristy Keller (Photographer)
Kathy Selchert (Photographer)
(061) John Moran Eye Center
Paul Bernstein, MD, PhD, (Site PI)
Michael Teske, MD, (Ophthalmologist)
Albert Vitale, MD, (Ophthalmologist)
Susan Allman, COA, (Clinic Coordinator)
Bonnie Carlstrom COA (Assistant Coordinator)
Kimberley Wegner (Assistant Coordinator)
Anne Haroldsen (Office Manager)
Deborah Harrison, MS, (Office Manager)
Cyrie Fry (Photographer)
James Gilman, CRA, (Photographer)
Glen Jenkins (Photographer)
Paula Morris, CRA, (Photographer)
(063) Loma Linda University
Michael Rauser, MD, (Site PI)
Joseph Fan, MD, (Ophthalmologist)
Mukesh Suthar, MD, (Ophthalmologist)
Gisela Santiago (Clinic Coordinator)
Kara Rollins Halsey (Assistant Coordinator)
Christy Quesada (Assistant Coordinator)
William Kiernan, OD, (Ophthalmic Technician)
Jesse Knabb (Photographer)
(064) Baylor College of Medicine
Richard Alan Lewis, MD, MS, (Site PI)
Cindy Dorenbach, COT, (Clinic Coordinator)
Steven Spencer, COMT, (Ophthalmic Technician)
Dana Barnett (Photographer)
Joseph Morales, CRA, (Photographer)
(066) Carolina Retina Center
Barron C. Fishburne, MD, (Site PI)
Jeffrey G. Gross, MD, (Ophthalmologist)
Michael A. Magee, MD, (Ophthalmologist)
Amy Flowers (Clinic Coordinator)
Angie McDowell (Ophthalmic Technician)
Randall Price (Photographer)
(067) Case Western Reserve University
Suber Huang, MD, MBA, (Site PI)
Johnny Tang, MD, (Ophthalmologist)
Shawn Wilker, MD, (Ophthalmologist)
Cherie Hornsby (Clinic Coordinator)
Lisa Ferguson (Assistant Coordinator)
Kirk Krogstad (Assistant Coordinator)
Riva Adamovsky (Ophthalmic Technician)
Peggy Allchin (Ophthalmic Technician)
Kathleen Carlton (Ophthalmic Technician)
Claudia Clow (Ophthalmic Technician)
Kelly Sholtis (Ophthalmic Technician)
Stephanie Burke (Photographer)
Mark Harrod (Photographer)
Stacie Hrvatin (Photographer)
Geoffrey Pankhurst (Photographer)
(069) Eye Foundation of Kansas City
Nelson R. Sabates, MD, (Site PI)
Michael Cassell, MD, (Ophthalmologist)
Komal Desai, MD, (Ophthalmologist)
Abraham Poulose, MD, (Ophthalmologist)
Felix Sabates, MD, (Ophthalmologist)
Yin Chen (Clinic Coordinator)
Gary Gallimore, COMT, (Photographer)
Yolanda Konior (Photographer)
(070) Jones Eye Institute - UAMS
Nicola Kim, MD, (Site PI)
Sami Uwaydat (Ophthalmologist)
Deborah Troillett (Clinic Coordinator)
Karen Aletter (Photographer)
(071) Kresge Eye Institute
Robert N. Frank, MD, (Site PI)
Gary Abrams, MD, (Ophthalmologist)
James Puklin, MD, (Ophthalmologist)
Asheesh Tewari, MD, (Ophthalmologist)
Cheryl Milanovic (Clinic Coordinator)
Melanie Bailey (Photographer)
David Griffith (Photographer)
Dena McDonald (Photographer)
Kit Morehead (Photographer)
Zlatan Sadikovic (Photographer)
Lisa Schillace (Photographer)
Elizabeth Silvis (Photographer)
(072) Colorado Retina Associates PC
Brian Joondeph, MD, (Site PI)
Nancy Christmas, MD, (Ophthalmologist)
David Johnson, MD, (Ophthalmologist)
Alan Kimura, MD, (Ophthalmologist)
Mimi Liu, MD, (Ophthalmologist)
Stephen Petty, MD, (Ophthalmologist)
John Zilis, MD, (Ophthalmologist)
Jenny Benitez (Clinic Coordinator)
Cassandra Berryman Catlett (Assistant Coordinator)
Eric Fluegel, RN, (Assistant Coordinator)
Shane Mowry (Photographer)
Hoang Nguyen (Photographer)
David Reflow (Photographer)
(074) UNC Department of Ophthalmology
Odette M. Houghton, MD, (Site PI)
Seema Garg, MD, PhD, (Ophthalmologist)
Maurice B. Landers, MD, (Ophthalmologist)
Travis Meredith, MD, (Ophthalmologist)
Sandy Barnhart, MPH, (Clinic Coordinator)
Megha Karmalkar (Assistant Coordinator)
Debra Cantrell (Photographer)
Rona Lyn Esquejo-Leon (Photographer)
Linda Manor (Pharmacist)
Sue Pope (Pharmacist)
David Stines (Pharmacist)
Amelia Stokely (Pharmacist)
(075) University Health Care - Mason Eye Institute
Dean Hainsworth, MD, (Site PI)
Dyann Helming (Clinic Coordinator)
Debbie Eichelberger (Office Manager)
Mary Paige Leaton (Ophthalmic Technician)
Chuck Hamm (Photographer)
(076) University of Tennessee HSC
Edward Chaum, MD, PhD, (Site PI)
Alessandro Iannaccone, MD, (Ophthalmologist)
Barbara Jennings, MA, OD, (Clinic Coordinator)
Tracy Murray (Ophthalmic Technician)
Joe Mastellone (Photographer)
(077) Fletcher Allen Health Care
Robert Millay, MD, (Site PI)
Brian Kim, MD, (Ophthalmologist)
Theresa Goddard (Clinic Coordinator)
Liza Jarrett Beaudette (Ophthalmic Technician)
Nina Changelian-Aitken (Ophthalmic Technician)
Fernando Corrada (Photographer)
Jason Dubuque (Photographer)
(078) Mayo Clinic
Raymond Iezzi, MD, (Site PI)
Sophie J. Bakri, MD, (Ophthalmologist)
Jose S. Pulido, MD, (Ophthalmologist)
Diane Vogen (Clinic Coordinator)
Rebecca Nielsen, LPN, (Assistant Coordinator)
Karin Berg (Ophthalmic Technician)
Jean Burrington, COA, (Ophthalmic Technician)
Shannon Howard, COA, (Ophthalmic Technician)
Joan Overend (Ophthalmic Technician)
Zbigniew Krason (Photographer)
Denise Lewison (Photographer)
Thomas Link, CRA, (Photographer)
(079) The Retina Institute
Kevin J. Blinder, MD, (Site PI)
Nicholas E. Engelbrecht, MD, (Ophthalmologist)
M. Gilbert Grand, MD, (Ophthalmologist)
Daniel P. Joseph, MD, PhD, (Ophthalmologist)
Gaurav K. Shah, MD, (Ophthalmologist)
Bradley Smith, MD, (Ophthalmologist)
Matthew Thomas, MD, (Ophthalmologist)
Rhonda Weeks (Clinic Coordinator)
Lynda Boyd (Ophthalmic Technician)
Dana Gabel (Photographer)
(080) Yale University Eye Center
Ron Adelman, MD, (Site PI)
John Huang, MD, (Ophthalmologist)
James Kempton, MD, (Ophthalmologist)
Aaron Parnes, MD, (Ophthalmologist)
Jennifer Dupont (Clinic Coordinator)
Elizabeth Perotti (Assistant Coordinator)
Victoria Donaldson (Ophthalmic Technician)
Kenneth Fong (Photographer)
Pamela Ossorio (Photographer)
(081) Vanderbilt Eye Institute
Anita Agarwal, MD, (Site PI)
Paul Sternberg, MD, (Ophthalmologist)
Sandy Owings (Clinic Coordinator)
Tony Adkins (Photographer)
Elaine Lok (Photographer)
Garvin Munn (Photographer)
Buddy Skellie (Photographer)
(082) UMDNJ
Neelakshi Bhagat, MD, MPH, (Site PI)
Monique S. Roy, MD, (Ophthalmologist)
Marco Zarbin, MD, PhD, (Ophthalmologist)
Catherine Fay (Clinic Coordinator)
Michael Lazar (Photographer)
Beth Malpica (Photographer)
Tatiana Mikheyav (Photographer)
(084) The University of Illinois
Lawrence Ulanski II, MD, (Site PI)
Jennifer Lim, MD, (Ophthalmologist)
Marcia Niec, BS CCRP, (Clinic Coordinator)
Tametha Johnson (Ophthalmic Technician)
Yesenia Ovando (Ophthalmic Technician)
Catherine Nail Carroll (Photographer)
Mark Janowicz (Photographer)
(085) Jules Stein Eye Institute
Steven Schwartz, MD, (Site PI)
David Cupp, MD, (Ophthalmologist)
Michael Gorin, MD, PhD, (Ophthalmologist)
Gad Heilweil, MD, (Ophthalmologist)
Hamid Hosseini, MD, (Ophthalmologist)
Jean-Pierre Hubschman, MD, (Ophthalmologist)
Allan Kreiger, MD, (Ophthalmologist)
Tara Young McCannel, MD, (Ophthalmologist)
Carolyn Pan, MD, (Ophthalmologist)
David Sarraf, MD, (Ophthalmologist)
Irena Tsui, MD, (Ophthalmologist)
Joshua Udoetek MD(Ophthalmologist)
Vinad Voleti, MD, (Ophthalmologist)
Logan Hitchcock (Clinic Coordinator)
Rosaleen Ostrick (Assistant Coordinator)
Melissa Chun, OD, (Ophthalmic Technician)
Jennie Kageyama, OD, (Ophthalmic Technician)
Nilo Davila (Photographer)
Kristin Lipka (Photographer)
Christina Shin (Pharmacist)
(086) Univ. of Alabama at Birmingham
Cynthia Owsley, PhD, (Site PI)
Michael Albert, Jr., MD, (Ophthalmologist)
Richard Feist, MD, (Ophthalmologist)
John Mason, MD, (Ophthalmologist)
Martin Thomley, MD, (Ophthalmologist)
Angelia Johnson (Clinic Coordinator)
Mark Clark (Assistant Coordinator)
Tracy Emond (Assistant Coordinator)
Joanna Hamela (Assistant Coordinator)
Angela Marsh (Office Manager)
Karen Searcey (Office Manager)
Kia Rookard (Ophthalmic Technician)
(087) UT Southwestern Medical Center
Yu-Guang He, MD, (Site PI)
Rafael L. Ufret-Vincenty, MD, (Ophthalmologist)
Mike Molai (Clinic Coordinator)
William Anderson (Photographer)
John Horna (Photographer)
(088) Ohio State University
Alan Letson, MD, (Site PI)
Colleen Cebulla, MD, PhD, (Ophthalmologist)
Susie Chang, MD, (Ophthalmologist)
Fred Davidorf, MD, (Ophthalmologist)
Jill Salerno (Clinic Coordinator)
Laura Sladoje (Office Manager)
Christina Stetson (Office Manager)
Jeri Perry (Ophthalmic Technician)
Scott Savage (Photographer)
(089) Duke University
Cynthia Toth, MD, (Site PI)
Glenn Jaffe, MD, (Ophthalmologist)
Stefanie Schuman, MD, (Ophthalmologist)
Neeru Sarin, MBBS, (Clinic Coordinator)
Jim Crowell (Photographer)
Tiffanie Keaton (Photographer)
Michael Kelly (Photographer)
Brian Lutman (Photographer)
Marriner Skelly (Photographer)
Lauren Welch (Photographer)
(090) University of California, Davis
Lawrence Morse, MD, PhD, (Site PI)
Allan Hunter, MD, (Ophthalmologist)
Susanna Soon-Chun Park MD, PhD (Ophthalmologist)
Cynthia Wallace (Clinic Coordinator)
Ember Dhillon (Assistant Coordinator)
Marisa Salvador (Assistant Coordinator)
Barbara Holderreed (Office Manager)
Karishma Chandra (Photographer)
Sashi Kaur (Photographer)
Ellen Redenbo (Photographer)
Smiley Hom (Pharmacist)
(091) Manhattan Eye, Ear and Throat Hospital
Michael Cooney, MD, (Site PI)
Irene Barbazetto, MD, (Ophthalmologist)
James M. Klancnik, Jr., MD, (Ophthalmologist)
John A. Sorenson, MD, (Ophthalmologist)
Lawrence Yannuzzi, MD, (Ophthalmologist)
Maria Scolaro (Clinic Coordinator)
Eugene Agresta (Photographer)
Nancy Gonzalez (Photographer)
(092) University of Florida
Sandeep Grover, MD, (Site PI)
K.V. Chalam, MD, PhD, (Ophthalmologist)
Shailesh Gupta, MD, (Ophthalmologist)
Christopher Lyons (Clinic Coordinator)
Wenhua Li (Assistant Coordinator)
Chirag Patel, MD, (Assistant Coordinator)
Jose Carrion (Photographer)
(093) Shiley Eye Center - UCSD
Henry Ferreyra, MD, (Site PI)
Amberly Rodriguez (Clinic Coordinator)
Iliana Molina (Assistant Coordinator)
Gabriel Balea (Photographer)
Pam Emory (Photographer)
Marlene Rico (Photographer)
Giorgio Siqueiros (Photographer)
(094) Scheie Eye Institute
Alexander J. Brucker, MD, (Site PI)
Joshua Dunaief, MD, (Ophthalmologist)
Juan Grunwald, MD, (Ophthalmologist)
Benjamin Kim, MD, (Ophthalmologist)
Albert M. Maguire, MD, (Ophthalmologist)
Brian VanderBeek, MD, (Ophthalmologist)
Sheri Drossner, MSW, (Clinic Coordinator)
Joan DuPont (Assistant Coordinator)
Rebecca Salvo (Assistant Coordinator)
Jim Berger (Photographer)
Cheryl Devine (Photographer)
Bill Nyberg (Photographer)
Laurel Weeney (Photographer)
(095) University of Rochester Eye Institute
David DiLoreto, MD, (Site PI)
Mina Chung, MD, (Ophthalmologist)
Valerie Davis (Clinic Coordinator)
Peter MacDowell (Assistant Coordinator)
George O Gara (Assistant Coordinator)
Daniel Castillo (Ophthalmic Technician)
Andrea Czubinski (Ophthalmic Technician)
Melissa Keim (Ophthalmic Technician)
Brandi Hardy (Photographer)
Rachel Grunhaus Hollar (Photographer)
Lynn Schueckler (Photographer)
(148) NorthShore University HealthSystems
Alice T. Lyon, MD, (Site PI)
Aaron Weinberg, MD, Site Co-PI
Mira Shiloach (Clinic Coordinator)
Nicole Pelkofer (Ophthalmic Technician)
Qin Zhou (Ophthalmic Technician)
Laura McPoland (Photographer)
(179) Washington University School of Medicine
Rajendra Apte, MD, PhD, (Site PI)
P. Kumar Rao, MD, (Ophthalmologist)
Sam Pistorius (Clinic Coordinator)
Jamie Kambarian (Assistant Coordinator)
Eve Adcock (Ophthalmic Technician)
Sarah Gould (Ophthalmic Technician)
Melanie Quinn (Ophthalmic Technician)
Rhonda Curtis (Photographer)
Amy Frost (Photographer)
Charla Meyer (Photographer)
Greg Rathert (Photographer)
Footnotes
Trial registration: none
Conflicts of Interest: No financial conflicts from members of the writing team.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Friedman DS, O’Colmain BJ, Muñoz B, et al. Prevalence of age-related macular degeneration in the United States. Arch Ophthalmol. 2004;122:564–72. doi: 10.1001/archopht.122.4.564. [DOI] [PubMed] [Google Scholar]
- 2.Ambati J, Ambati BK, Yoo SH, Ianchulev S, Adamis AP. Age-related macular degeneration: etiology, pathogenesis, and therapeutic strategies. Surv Ophthalmol. 2003;48:257–93. doi: 10.1016/s0039-6257(03)00030-4. [DOI] [PubMed] [Google Scholar]
- 3.Smith W, Mitchell P, Leeder SR. Dietary fat and fish intake and age-related maculopathy. Arch Ophthalmol. 2000;118:401–4. doi: 10.1001/archopht.118.3.401. [DOI] [PubMed] [Google Scholar]
- 4.Age-Related Eye Disease Study Research Group. Risk factors associated with age-related macular degeneration. A case-control study in the age-related eye disease study: Age-Related Eye Disease Study Report Number 3. Ophthalmology. 2000;107:2224–32. doi: 10.1016/s0161-6420(00)00409-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Klein R, Peto T, Bird A, Vannewkirk MR. The epidemiology of age-related macular degeneration. Am J Ophthalmol. 2004;137:486–95. doi: 10.1016/j.ajo.2003.11.069. [DOI] [PubMed] [Google Scholar]
- 6.Age-Related Eye Disease Study Research Group. A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Arch Ophthalmol. 2001;119:1417–36. doi: 10.1001/archopht.119.10.1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boekhoorn SS, Vingerling JR, Witteman JC, Hofman A, de Jong PT. C-reactive protein level and risk of aging macula disorder: The Rotterdam Study. Arch Ophthalmol. 2007;125:1395–401. doi: 10.1001/archopht.125.10.1396. [DOI] [PubMed] [Google Scholar]
- 8.Schaumberg DA, Christen WG, Buring JE, Glynn RJ, Rifai N, Ridker PM. High-sensitivity C-reactive protein, other markers of inflammation, and the incidence of macular degeneration in women. Arch Ophthalmol. 2007;125:300–5. doi: 10.1001/archopht.125.3.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hageman GS, Luthert PJ, Victor Chong NH, Johnson LV, Anderson DH, Mullins RF. An integrated hypothesis that considers drusen as biomarkers of immune-mediated processes at the RPE-Bruch’s membrane interface in aging and age-related macular degeneration. Prog Retin Eye Res. 2001;20:705–32. doi: 10.1016/s1350-9462(01)00010-6. [DOI] [PubMed] [Google Scholar]
- 10.Despriet DD, Klaver CC, Witteman JC, et al. Complement factor H polymorphism, complement activators, and risk of age-related macular degeneration. JAMA. 2006;296:301–9. doi: 10.1001/jama.296.3.301. [DOI] [PubMed] [Google Scholar]
- 11.Fritsche LG, Chen W, Schu M, et al. Seven new loci associated with age-related macular degeneration. Nat Genet. 2013;45:433–9. doi: 10.1038/ng.2578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seddon JM, George S, Rosner B, Rifai N. Progression of age-related macular degeneration: prospective assessment of C-reactive protein, interleukin 6, and other cardiovascular biomarkers. Arch Ophthalmol. 2005;123:774–82. doi: 10.1001/archopht.123.6.774. [DOI] [PubMed] [Google Scholar]
- 13.Mitta VP, Christen WG, Glynn RJ, et al. C-reactive protein and the incidence of macular degeneration: pooled analysis of 5 cohorts. JAMA Ophthalmol. 2013;131:507–13. doi: 10.1001/jamaophthalmol.2013.2303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaufman DW, Kelly JP, Rosenberg L, Anderson TE, Mitchell AA. Recent patterns of medication use in the ambulatory adult population of the United States: the Slone survey. JAMA. 2002;287:337–44. doi: 10.1001/jama.287.3.337. [DOI] [PubMed] [Google Scholar]
- 15.Pedersen TR, Kjekshus J, Berg K, et al. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S) Lancet. 1994;344:1383–9. [PubMed] [Google Scholar]
- 16.Grundy SM. HMG-CoA reductase inhibitors for treatment of hypercholesterolemia. N Engl J Med. 1988;319:24–33. doi: 10.1056/NEJM198807073190105. [DOI] [PubMed] [Google Scholar]
- 17.Werner N, Nickenig G, Laufs U. Pleiotropic effects of HMG-CoA reductase inhibitors. Basic Res Cardiol. 2002;97:105–16. doi: 10.1007/s003950200000. [DOI] [PubMed] [Google Scholar]
- 18.Jick H, Zornberg GL, Jick SS, Seshadri S, Drachman DA. Statins and the risk of dementia. Lancet. 2000;356:1627–31. doi: 10.1016/s0140-6736(00)03155-x. [DOI] [PubMed] [Google Scholar]
- 19.Sathasivam S, Lecky B. Statin induced myopathy. BMJ. 2008;337:a2286. doi: 10.1136/bmj.a2286. [DOI] [PubMed] [Google Scholar]
- 20.Coons JC. Hydroxymethylglutaryl-coenzyme A reductase inhibitors in osteoporosis management. Ann Pharmacother. 2002;36:326–30. doi: 10.1345/aph.1A071. [DOI] [PubMed] [Google Scholar]
- 21.Curcio CA, Millican CL, Bailey T, Kruth HS. Accumulation of cholesterol with age in human Bruch’s membrane. Invest Ophthalmol Vis Sci. 2001;42:265–74. [PubMed] [Google Scholar]
- 22.Curcio CA, Johnson M, Huang JD, Rudolf M. Aging, age-related macular degeneration, and the response-to-retention of apolipoprotein B-containing lipoproteins. Prog Retin Eye Res. 2009;28:393–422. doi: 10.1016/j.preteyeres.2009.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Malek G, Li CM, Guidry C, Medeiros NE, Curcio CA. Apolipoprotein B in cholesterol-containing drusen and basal deposits of human eyes with age-related maculopathy. Am J Pathol. 2003;162:413–25. doi: 10.1016/S0002-9440(10)63836-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barbosa DT, Mendes TS, Cíntron-Colon HR, et al. Age-related macular degeneration and protective effect of HMG Co-A reductase inhibitors (statins): results from the National Health and Nutrition Examination Survey 2005–2008. Eye (Lond) 2014;28:472–80. doi: 10.1038/eye.2014.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fong DS, Contreras R. Recent statin use and 1-year incidence of exudative age-related macular degeneration. Am J Ophthalmol. 2010;149:955–8. doi: 10.1016/j.ajo.2009.12.037. [DOI] [PubMed] [Google Scholar]
- 26.Hall NF, Gale CR, Syddall H, Phillips DI, Martyn CN. Risk of macular degeneration in users of statins: cross sectional study. BMJ. 2001;323:375–6. doi: 10.1136/bmj.323.7309.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Klein R, Klein BE, Tomany SC, Danforth LG, Cruickshanks KJ. Relation of statin use to the 5-year incidence and progression of age-related maculopathy. Arch Ophthalmol. 2003;121:1151–5. doi: 10.1001/archopht.121.8.1151. [DOI] [PubMed] [Google Scholar]
- 28.McGwin G, Jr, Owsley C, Curcio CA, Crain RJ. The association between statin use and age related maculopathy. Br J Ophthalmol. 2003;87:1121–5. doi: 10.1136/bjo.87.9.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McGwin G, Jr, Xie A, Owsley C. The use of cholesterol-lowering medications and age-related macular degeneration. Ophthalmology. 2005;112:488–94. doi: 10.1016/j.ophtha.2004.10.027. [DOI] [PubMed] [Google Scholar]
- 30.Pignone M, Phillips C, Mulrow C. Use of lipid lowering drugs for primary prevention of coronary heart disease: meta-analysis of randomised trials. BMJ. 2000;321:983–6. doi: 10.1136/bmj.321.7267.983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smeeth L, Cook C, Chakravarthy U, Hubbard R, Fletcher AE. A case control study of age related macular degeneration and use of statins. Br J Ophthalmol. 2005;89:1171–5. doi: 10.1136/bjo.2004.064477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tan JS, Mitchell P, Rochtchina E, Wang JJ. Statins and the long-term risk of incident age-related macular degeneration: the Blue Mountains Eye Study. Am J Ophthalmol. 2007;143:685–7. doi: 10.1016/j.ajo.2006.11.021. [DOI] [PubMed] [Google Scholar]
- 33.Wilson HL, Schwartz DM, Bhatt HR, McCulloch CE, Duncan JL. Statin and aspirin therapy are associated with decreased rates of choroidal neovascularization among patients with age-related macular degeneration. Am J Ophthalmol. 2004;137:615–24. doi: 10.1016/j.ajo.2003.10.025. [DOI] [PubMed] [Google Scholar]
- 34.Chodick G, Heymann AD, Flash S, Kokia E, Shalev V. Persistence with statins and incident cataract: a population-based historical cohort study. Ann Epidemiol. 2010;20:136–42. doi: 10.1016/j.annepidem.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 35.Maguire MG, Ying GS, McCannel CA, Liu C, Dai Y Complications of Age-related Macular Degeneration Prevention Trial (CAPT) Research Group. Statin use and the incidence of advanced age-related macular degeneration in the Complications of Age-related Macular Degeneration Prevention Trial. Ophthalmology. 2009;116:2381–5. doi: 10.1016/j.ophtha.2009.06.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McGwin G, Jr, Modjarrad K, Hall TA, Xie A, Owsley C. 3-hydroxy-3-methylglutaryl coenzyme a reductase inhibitors and the presence of age-related macular degeneration in the Cardiovascular Health Study. Arch Ophthalmol. 2006;124:33–7. doi: 10.1001/archopht.124.1.33. [DOI] [PubMed] [Google Scholar]
- 37.van Leeuwen R, Vingerling JR, Hofman A, de Jong PT, Stricker BH. Cholesterol lowering drugs and risk of age related maculopathy: prospective cohort study with cumulative exposure measurement. BMJ. 2003;326:255–6. doi: 10.1136/bmj.326.7383.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Guymer RH, Baird PN, Varsamidis M, et al. Proof of concept, randomized, placebo-controlled study of the effect of simvastatin on the course of age-related macular degeneration. PLoS One. 2013;8:e83759. doi: 10.1371/journal.pone.0083759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.AREDS2 Research Group. Chew EY, Clemons T, et al. The Age-Related Eye Disease Study 2 (AREDS2): study design and baseline characteristics (AREDS2 report number 1) Ophthalmology. 2012;119:2282–9. doi: 10.1016/j.ophtha.2012.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zanutto EL. A Comparison of Propensity Score and Linear Regression Analysis of Complex Survey Data. J Data Science. 2006;4:67–91. [Google Scholar]
- 41.Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46:399–424. doi: 10.1080/00273171.2011.568786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509. [Google Scholar]
- 43.Kohl M, Heinze G. [Accessed May 14, 2014];PSHREG: A SAS(R) macro for proportional and nonproportional substribution hazards regression with competing risk data. Available at: http://www.meduniwien.ac.at/user/maria.kohl/tr08_2012-PSHREG.pdf.
- 44.Kaiserman N, Vinker S, Kaiserman J. Statins do not decrease the risk for wet age-related macular degeneration. Curr Eye Res. 2009;34:304–10. doi: 10.1080/02713680902741670. [DOI] [PubMed] [Google Scholar]
- 45.van Leeuwen R, Tomany SC, Wang JJ, et al. Is medication use associated with the incidence of early age-related maculopathy? Pooled findings from 3 continents. Ophthalmology. 2004;111:1169–75. doi: 10.1016/j.ophtha.2003.10.024. [DOI] [PubMed] [Google Scholar]
- 46.Tobert JA. Lovastatin and beyond: the history of the HMG-CoA reductase inhibitors. Nat Rev Drug Discov. 2003;2:517–26. doi: 10.1038/nrd1112. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.