Abstract
This study examined the long-term outcomes of a nonclinical sample of anxious children (N=61) who were randomized by school to 9 weeks of group cognitive-behavioral therapy (CBT) for children, group CBT for children plus parent training, or no-treatment control. Parents and children completed measures of anxiety symptoms at baseline, posttreatment, and at 3-month, 6-month, 12-month, 2-year, and 3-year posttreatment follow-ups. Piecewise longitudinal growth curve analyses were applied to the data. When the two CBT groups were combined and compared with control, the combined treatment group showed significantly greater reduction in children’s anxiety severity based on the parent ratings in the first longitudinal phase. However, on the parent Clinician Severity Rating gains were maintained to three years. Child report revealed no significant differences between groups on anxiety reduction. This study maintained a small no-treatment control group during the entire follow-up period. From parental perspective only, school-based group CBT appeared to be beneficial in decreasing severity of anxiety symptoms and maintaining gains over time.
Keywords: anxiety, cognitive-behavioral therapy, school-based intervention, follow-up study
Introduction
Anxiety disorders are among the most common psychiatric disorders in children with prevalence rates ranging from 6% to 20% based on several large epidemiological studies (1). Having one anxiety disorder may place a child on an aberrant developmental trajectory with increasing risk for additional psychopathology and functional impairment (2). Cognitive-behavioral therapy (CBT) is the first-line psychosocial treatment for youths with anxiety disorders (3, 4). Based on randomized controlled trials, CBT has been demonstrated to be effective in decreasing anxiety symptoms and facilitating remission of generalized anxiety disorder (GAD), separation anxiety disorder (SAD), and/or social anxiety disorder in children and adolescents (5).
We found eight long term follow-up (LTFU) studies of CBT for pediatric anxiety disorders (6–13). These studies suggest durability of acute treatment gains across follow-up periods of two to seven years (14, for review). For example, 6-year follow-up of the Child Adolescent Multimodal Study (CAMS) was recently published (13). CAMS (N = 488) compared the effectiveness of 12 weeks of CBT, sertraline, CBT plus sertraline, and pill placebo for pediatric anxiety disorders (5). At posttreatment, 55% on sertraline, 60% who received CBT, 81% who received CBT plus sertraline, and 24% on placebo were rated as responders. CAMS treatment was offered to placebo nonresponders after the acute treatment phase. Since 86% of the placebo group had received CAMS treatment by 6-year follow-up, no control group was included in analyses of outcome at LTFU. At 6-year follow-up there was no difference in outcome between the three active treatment conditions with about half of all participants in remission (13).
Of the eight LTFU studies, only Dadds et al. (8) and Barrett et al. (7) included control groups during the entire follow-up period. Most LTFU studies of CBT for pediatric anxiety disorders do not have a control group because the studies offer CBT to control participants after the active treatment. Without a control group, it is difficult to determine if outcomes are due to the intervention or other factors (e.g., passage of time, maturation). The current study maintains a small control group over the entire 3-year follow-up period.
This study evaluates the long term outcomes of school-based interventions for anxiety in children. Advantages of providing mental health interventions in the school setting include easy access to treatment, a gateway to more specialized services and community care, and reduction of stigma associated with treatment (15, 16). School-based CBT is effective for youths with anxiety disorders (15, 17–20).
Bernstein and colleagues (21) examined posttreatment outcomes for 61 children ages seven to eleven years from a nonclinical sample who were randomly assigned by school to a nine-week manualized group CBT for children, group CBT for children plus parent training, or no-treatment control. At posttreatment, group CBT for children and group CBT for children plus parent training were significantly more effective than no-treatment control in decreasing children’s anxiety symptomatology and in facilitating remission of anxiety diagnoses. In the short-term follow-up of this study, participants were compared at 3-, 6-, and 12-months posttreatment (22). At 6-month follow-up, families in the control group were offered CBT. Half of the control families chose to receive treatment and half declined. The combined CBT group compared with control sustained significant improvement in anxiety severity across a 12-month period.
The current study is a 3-year LTFU study of the 61 children who participated in the treatment study of Bernstein and colleagues (21). Participants were assessed at 2- and 3-year posttreatment. Using latent growth curve modeling, we were able to exclude 1-year, 2-year, and 3-year follow-up data from the 12 controls who received treatment after six months and still include all their earlier data in the analyses. This allowed us to include all participants who were randomized to the three treatment conditions at baseline (intent-to-treat) and minimize possible bias that may occur when selecting only the 12 controls who did not receive treatment after 6-month follow-up as a control group. It was hypothesized that both group CBT plus parent training and group CBT alone would be more effective than no-treatment control as measured by decrease in severity of anxiety symptoms and maintenance of gains over time.
Materials and Methods
Participants
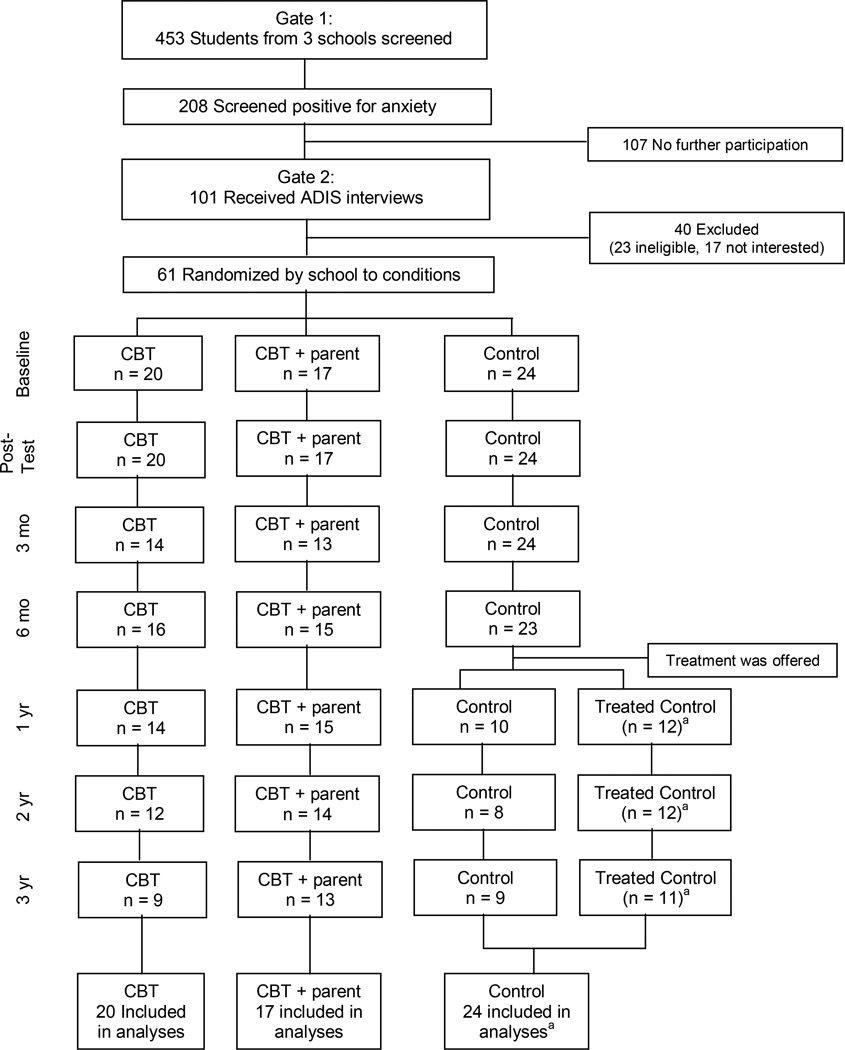
The Institutional Review Board of the University approved this protocol. The methodology is described in previous publications (21, 22). Students from three public elementary schools in the same district participated. Schools were matched on number of students, percentage of minority students, and percentage of students who receive free or reduced rate lunches (i.e., measure of lower socioeconomic status). Written consent and assent were obtained from the parents and children, respectively, for the screening and treatment (21) and follow-up (22). Figure 1 outlines the study design and flow of participants. Students were screened using the Multidimensional Anxiety Scale for Children (MASC) (23). They were identified as anxious with a MASC Total Anxiety T score of 58 or more and/or teacher nomination as one of the three most anxious children in the classroom. The cutoff of 58 was selected in order to identify children with subthreshold and threshold levels of anxiety symptoms. Two hundred eight of 453 children screened positive for anxiety. ADIS Child and Parent Interview Schedules were administered to 101 of these students and 61 were enrolled. Inclusion criteria required DSM-IV diagnoses of SAD, GAD, and/or social anxiety disorder or “features” (one or more, but not all criteria) of one of these anxiety disorders and associated composite clinician severity rating (CSR) of 2 to 6 on the ADIS.
Figure 1.
Diagram of study participant flow. aOne-year, two-year and three-year follow-up data from the 12 controls who received treatment after 6-month follow-up were excluded from the analyses.
Participants were randomized by school to group CBT for children (n = 20), group CBT for children plus parent training (n = 17), or no treatment control (n = 24). Children participated in a 9-week treatment study (21). Child group CBT was a 9-week anxiety intervention plus two booster sessions using the manualized FRIENDS program (24). In the group CBT plus parent training, parents participated in a concurrent parent training group. FRIENDS is a manualized group CBT program for anxious children (24). FRIENDS was adapted from the Coping Koala Group Program (25) which was developed from the Coping Cat Program (26). Our study expanded the parent intervention of FRIENDS by adding content about management of parental anxiety, identification of ways a family is affected by the child’s anxiety, and behavioral contracting. Child and parent groups were conducted after school or in the early evening at the schools. Families were compensated at each assessment for completion of semistructured diagnostic interviews and rating scales.
Baseline analyses using ANOVAs and chi-square tests showed no significant differences between the three treatment conditions on demographic information, anxiety impairment/severity, and diagnostic status. The children were mostly white (97%) and had an average Hollingshead socioeconomic status (27) of 40.5 ± 8.4 corresponding to middle class. The majority (62%) of the children came from two-parent households, 33% were from divorced-parent households, and 5% resided with single mothers who never married. At baseline, 75% met DSM-IV criteria and 25% were subthreshold for one or more anxiety diagnoses.
After the 6-month follow-up assessment, participants in the control group (n = 24) were offered CBT. Twelve of the 24 control families chose to participate in CBT with seven randomized to CBT plus parent training and five randomized to CBT only. Independent sample t tests and chi-square tests revealed no baseline differences on demographic and anxiety severity between the 12 control children who agreed to participate and the 12 control children who chose not to participate in treatment after 6-month follow-up.
Procedures
Follow-up assessments were conducted in homes, schools, or community libraries at 3-month, 6-month, 1-year, 2-year, and 3-year posttreatment by independent evaluators who were blind to treatment condition and response to treatment after the 9-week intervention. ADIS was not given at 3-month follow-up. Completion rates of assessment at each follow-up wave were 84% (3 months), 89% (6 months), 84% (1 year), 75% (2 years) and 69% (3 years).
Training of Independent Evaluators
Independent evaluators had the following credentials: master’s degree in psychology, doctoral student in psychology, or bachelor’s degree with graduate courses in psychology. Four to eight weeks of training was provided to the independent evaluators. All ADIS interviews were audiotaped and reliability checks were completed on 20% of the tapes. Kappa coefficients (interrater reliability) of inclusionary diagnoses ranged from 0.80 to 1.00.
Instruments
ADIS
ADIS is a clinician-administrated semistructured interview used to evaluate anxiety and other disorders. The ADIS was administered to the child and the parent separately by the same independent evaluator. Participants were randomly assigned to independent evaluators at each assessment point. All independent evaluators conducted interviews with children at each of the three schools. CSR, a measure of severity/impairment, was determined for each ADIS anxiety diagnosis for which symptoms were endorsed by the child and/or parent. Range of CSR is 0 to 8. Ratings of 4 and above are in the clinically significant range. Evidence of good psychometric properties of the ADIS has been reported elsewhere (28, 29).
MASC
Parents and children rate 39 items related to the child’s anxiety symptoms over the last two weeks. Items are scored on four-point scales (0 = never to 3 = often). The parent version has moderate to strong internal reliability across subscales (30) while the child version has high divergent and convergent validities and adequate test-retest reliability (23). Alpha reliabilities were .90 for the parent version and .87 for the child version. The MASC manual converts raw scores to T scores (31). T scores of 65 or above indicate clinically significant symptoms.
Parent SCARED
Parent SCARED includes 41 items of the child’s anxiety symptoms (α = .92). It is reported that SCARED has good internal consistency test-retest reliability, discriminant validity, and moderate parent-child agreement (32). Items are rated on three-point scales (0 = not true to 2 = very true).
Services Questionnaire
This measure which was developed for use in the current study was completed by parents at 2- and 3-year follow-ups. The Services Questionnaire was used to assess whether the children received any off-protocol services or medications for psychiatric problems since the study began.
Statistical Analysis
Test of group equivalence and analysis of attrition were conducted using chi-square test (categorical), ANOVA (continuous), and Kruskal-Wallis test (non-normally distributed variables). Fisher’s Exact test for a 2×2 contingency table was applied to the service utilization data. In the current study, twelve control participants decided to receive treatment after the 6-month follow-up. A decision was made to exclude their 1-year, 2-year and 3-year follow-up data but include all their earlier data in the analyses, which was not affected by the treatment. We used a statistical approach to estimate the missing data (e.g., maximum-likelihood estimation, see below). Although the missingness was due to project design, this method allowed us to include all participants in the analyses and reduce additional bias associated with listwise deletion of cases with missing data.
Latent growth curve modeling (LGCM) was used to test intervention effects on the anxiety outcomes. This statistical approach allows for the modeling of both individual differences in the rate of change over time (within-subject) and intervention effects (between-subject) simultaneously. Mplus 6.0 (33) was used to evaluate the group difference between intervention and control conditions in the repeatedly measured outcomes assessed from baseline to 3-year posttreatment follow-up. Maximum-likelihood estimation was used to estimate all models. Examination of normality of distribution showed that parent- and child-reports of the CSR had non-normal distributions that were positively skewed with a mode of zero. Therefore, a Poisson distribution was applied to the analyses. All participants’ data were included in the analyses using full-information maximum likelihood (FIML) for missing data. The majority of missing data in this study was due to project design. Therefore, FIML was used in the context of missing not at random (MNAR). Analysis of missing data pattern using Little’s chi-squared test showed that there were no significant patterns of missing data [χ2 (df = 938) = 875.77, p = .927].
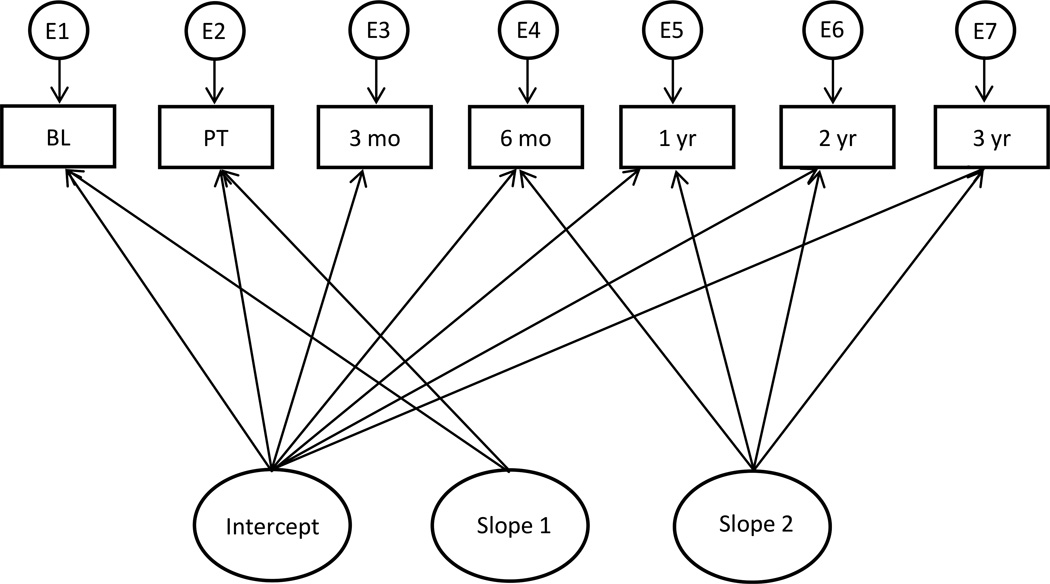
Inspection of the raw means over time showed that there were two distinctive phases of rates of change: the first phase showed a steep reduction in anxiety outcomes from baseline to 3-month follow-up (MASC, SCARED) or from baseline to 12-month follow-up (CSR), while the second phase showed a relatively flat rate of change from 3- (or 12-) month to 3-year posttreatment follow-up. Therefore, we compared the goodness of fit for models with linear growth, nonlinear quadratic growth, and piecewise linear growth. Chi-square test, comparative fit index (CFI; 34) and the root mean square error of approximation (RMSEA; 35) were used to determine best fitting model for the continuous variables (SCARED and MASC). Akaike information criteria (AIC) and Bayesian information criteria (BIC) were used to establish the best fitting model for the CSR data where a Poisson distribution was applied. Adequacy of model fit is indicated by a non-significant chi-square test statistic, CFI ≥ 0.95 and RMSEA < 0.08 (36). For AIC and BIC, smaller values indicated better fit. Piecewise linear growth model was shown to be the best fitting model for all five outcome variables and was thus used to evaluate the long-term intervention effects. Figure 2 depicts a piecewise growth model used in the study. To test treatment effects at specific assessment points, we estimated the models with the intercepts centered after the first phase (mid-point intercept) and at 3-year follow-up (end-point intercept). For all analyses, two-tailed alpha of < .05 was utilized for significance. Cohen’s d was calculated for effect sizes (37).
Figure 2.
Piecewise growth model describing the outcome trajectory as a two-phase model with the first slope capturing changes from baseline to 3 months post-treatment and the second slope capturing changes from 3 months to 3 years post-intervention.
Results
Attrition Analysis
The rate of attrition by the time of the 3-year follow-up was 23.5% for the CBT plus parent training, 55% for the CBT-only and 25% for the control group [χ2(2) = 4.86, p = .088]. Comparisons at baseline between those who were retained versus those who dropped out showed no significant group differences in age, sex, baseline diagnostic status, socioeconomic status and baseline scores of anxiety severity.
Outcome Analysis
Initial piece-wise LGCM analyses comparing CBT plus parent training and CBT-only produced no significant group differences in any of the growth curve estimates for the five outcome variables, except that there was one difference in the child-rated MASC 2nd phase slope (p = .044).1 Thus, to improve model convergence and simplify the LGCM, analyses were repeated by collapsing both treatment groups and comparing them with the control group. Table 1 presents the means and standard deviations of the outcome variables for the combined treatment group and control condition. Table 2 shows the summary of the piecewise linear growth curve analyses.
Table 1.
Means and standard deviations on outcome measures for collapsed treatment and control groups from baseline to 3-year follow-up
| Group | Parent SCARED | Parent MASC | Child MASC | Parent CSR | Child CSR |
|---|---|---|---|---|---|
| Baseline | |||||
| Treatment (n = 37) | 25.06 (13.38) | 51.92 (16.56) | 52.68 (8.42) | 3.24 (1.64) | 3.68 (1.87) |
| Control (n = 24) | 21.25 (9.64) | 50.46 (12.62) | 51.29 (10.08) | 3.29 (1.60) | 2.96 (2.18) |
| Posttreatment | |||||
| Treatment (n = 37) | 16.62 (9.99) | 44.54 (17.66) | 51.56 (11.25) | 2.05 (1.76) | 1.57 (1.71) |
| Control (n = 24) | 21.04 (10.80) | 53.00 (12.70) | 49.08 (10.50) | 2.58 (2.08) | 2.13 (1.92) |
| 3-month follow-up | |||||
| Treatment (n = 27) | 14.60 (11.68) | 40.72 (18.53) | 46.32 (11.19) | -- | -- |
| Control (n = 24) | 19.04 (12.13) | 47.42 (13.82) | 50.58 (8.77) | -- | -- |
| 6-month follow-up | |||||
| Treatment (n = 31) | 14.23 (10.04) | 40.73 (15.99) | 46.77 (9.96) | 1.29 (1.75) | 0.81 (1.40) |
| Control (n = 23) | 18.86 (12.81) | 49.82 (15.24) | 47.23 (11.49) | 2.43 (2.11) | 0.77 (1.41) |
| 1-year follow-up | |||||
| Treatment (n = 29) | 14.21 (9.41) | 41.89 (15.81) | 45.64 (8.66) | 0.79 (1.24) | 0.24 (0.83) |
| Control (n = 10)a | 23.20 (11.71) | 54.22 (14.51) | 48.00 (9.57) | 1.80 (1.87) | 0.56 (1.33) |
| 2-year follow-up | |||||
| Treatment (n = 26) | 13.44 (7.96) | 42.56 (12.54) | 47.24 (14.01) | 1.69 (2.17) | 0.77 (1.56) |
| Control (n = 8)a | 20.50 (8.18) | 50.50 (8.78) | 55.25 (13.52) | 2.63 (2.77) | 0.75 (1.39) |
| 3-year follow-up | |||||
| Treatment (n = 22) | 12.75 (11.07) | 37.50 (16.13) | 48.42 (14.11) | 0.86 (1.42) | 1.05 (1.86) |
| Control (n = 9)a | 16.29 (8.98) | 49.67 (17.30) | 48.63 (13.16) | 1.89 (2.26) | 1.89 (2.67) |
1-, 2-, and 3-year follow-up data from 12 control participants who received treatment after 6-month posttreatment were excluded from analyses.
Table 2.
Summary of piece-wise linear growth curve analyses: group effects on initial phase slope, mid-point intercept, and 2nd phase slope
| Model Parameter | Parent SCARED | Parent MASC | Child MASC | Parent CSR | Child CSR |
|---|---|---|---|---|---|
| Initial phase slope (SE) | −.675 (.232)** | −.480 (.200)* | −.340 (.332) | −.431 (.164)** | −.082 (.142) |
| Mid-point intercept (SE)a | −.298 (.129)* | −.276 (.126)* | −.047 (.152) | −.363 (.138)** | −.052 (.122) |
| 2nd phase slope (SE) | .214 (.214) | .050 (.198) | .016 (.269) | .393 (.383) | −.045 (.202) |
Note: SE = standard error. Group was coded as 1 = treatment and 0 = control.
Mid-point intercept was set at 3-month posttreatment for parent SCARED, parent and child MASC, and at 1-year posttreatment for parent and child CSR.
p < .05,
p < .01.
Parent Ratings of Anxiety in Children
SCARED
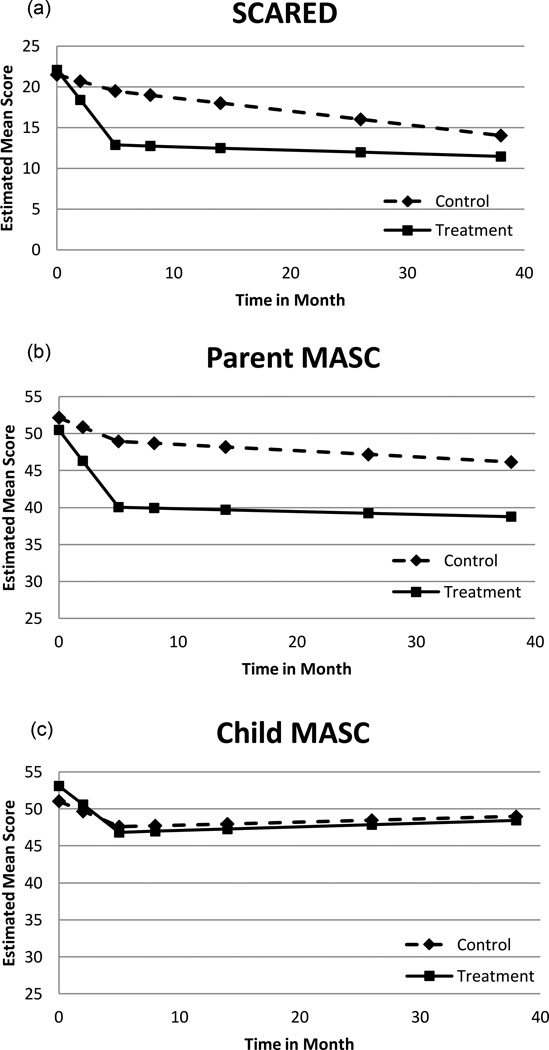
Goodness-of-fit statistics of the piecewise LGCM showed adequate fit of the model to the data [χ2 (21, N = 61) = 27.02, p = .17, CFI = 0.979 and RMSEA = 0.069]. Significant treatment effect was detected for the initial phase slope (from baseline to 3-month follow-up) and for the difference at 3-month follow-up (Table 2). The results indicated that the combined CBT treatment group showed significantly more improvement over time during the initial phase, and had significantly lower SCARED scores at 3-month posttreatment compared with the control group (d = 0.69). There was no significant group difference in the second-phase slope, indicating that both groups had similar rates of change from 3-month to 3-year follow-up. Figure 3 (a) shows the estimated mean trajectories of the complete data for the treatment and control groups. When treatment effect was tested for difference at the 3-year follow-up (end point), no significant group difference was detected (d = 0.27).
Figure 3.
Estimated trajectories of SCARED, parent MASC, and child MASC mean scores for the treatment and control groups.
MASC
The chi-square test suggested adequate fit of the model [χ2(23, N = 61) = 24.17, p = .39]. Other fit indices also supported the optimal fit of the model (CFI = 0.995, RMSEA = 0.029). Treatment effect was significant during the initial phase slope (from baseline to 3-month follow-up) and for the difference at 3-month follow-up (Table 2). The results indicated that during the initial phase the combined CBT treatment group had greater improvement over time and at 3-month follow-up the treatment group had significantly lower MASC scores compared with the control group (d = 0.70). Treatment effect was not significant during the second phase and the estimate was close to zero, indicating that both groups maintained their level of MASC scores from 3-month to 3-year follow-up [Figure 3 (b)]. When intercept was centered at end-point (3-year follow-up), there was no significant group difference (d = 0.58).
Child Rating of Anxiety
MASC
Fit statistics indicated that the piecewise LGCM had appropriate model fit [χ2 (23, N = 61) = 23.23, p = .45, CFI = 0.998 and RMSEA = 0.013]. Results of the LGCMs showed no significant treatment effect for the initial and second phase slopes, and at the 3-month and 3-year follow-ups (Table 2). The results indicated that there were no significant group differences in the rates of change during the initial and second phases and in their mean scores at 3-month (d = 0.08) and 3-year posttreatment (d = 0.05) [Figure 3 (c)].
Anxiety Severity and Impairment from the ADIS
Parent CSR
Poisson distribution for non-normal variable was applied to the LGCM. Results of the piecewise LGCM showed a significant treatment effect during the initial phase and at 12-month follow-up (mid-point intercept) (Table 2). These results indicated that during the initial phase the combined CBT treatment group showed greater improvement over time and at 12-month follow-up the CBT group had significantly lower CSR scores compared with the control group (d = 0.48). There was no significant group difference in slopes during the second phase. End-point analysis showed that the groups remained significantly different at 3-year follow-up: the CBT group continued to have significantly lower CSR scores than the control group (estimate = -.208, SE = .087, p < .05, d = 0.39).
Child CSR
Piecewise LGCMs testing the treatment effect showed no significant group differences for the initial and second phase slopes, and at the 12-month and 3-year follow-ups (Table 2). The results indicated that both groups showed similar rates of change during the initial and second phases and had no significant differences in their mean scores at 12-month (d = 0.21) and 3-year posttreatment (d = 0.34).
Service Utilization
Frequencies and percent of participants who utilized services posttreatment are presented in Table 3. A total of 48 parents (treatment group n = 27, control group n = 21) completed the questionnaire at the 2-year and/or 3-year follow-up. One child in the combined treatment group and one child in the control group received SSRI plus off-protocol therapy. Five children in the combined treatment group versus no children in the control group received off-protocol therapy only. Fisher’s Exact tests revealed no statistically significant group differences in service utilization, although group difference approached significance with the treatment group being more likely to receive off-protocol therapy without medication.
Table 3.
Off-protocol service utilization during the study for the combined treatment and control groups
| Service | Treatment (n=27) n (%) |
Control (n=21) n (%) |
Fisher’s Exact p |
|---|---|---|---|
| SSRI and therapy | 1 (3.7) | 1 (4.8) | 1.00 |
| Therapy | 5 (18.5) | 0 (0) | .06 |
| Psychiatric hospitalization | 0 (0) | 0 (0) | -- |
| Respite care | 0 (0) | 0 (0) | -- |
| IEP | 5 (18.5) | 2 (10.0) | .68 |
Note: Data were collected at 2-year and 3-year follow-ups. IEP=Individualized education program; SSRI=selective serotonin reuptake inhibitor.
Discussion
The present study examined the long-term effects of school-based interventions for anxious children. Comparisons showed that the combined treatment group had significantly greater reduction in children’s anxiety severity during the initial phase of the study (from baseline to 3-month follow-up or from baseline to 1-year follow-up) based on parent rating scales. While the combined treatment group maintained its gains until the 3-year follow-up assessment, the control group showed slow but steady improvements over time. There was a significant difference between the two groups at the 3-year follow-up on the parent CSR, a measure of anxiety severity and impairment, with the combined treatment group maintaining a significantly lower score compared with the control group. On the parent MASC and parent SCARED, there were no significant differences between the two groups at 3 years.
Improvement with CBT was primarily documented on parent-report measures. No significant treatment effects were detected on the child-report measures. Inspection of the means on the child-reported MASC and CSR revealed that both the combined treatment group and the control group showed reduction in severity of anxiety symptoms over time.
Results across time showed significant improvement in anxiety symptomatology between the combined treatment group and control, but only in the first longitudinal phase. This may indicate that booster sessions need to be extended long term. In our study, CBT booster sessions were offered at 1- and 3-month posttreatment. It is possible that the booster sessions were effective in reducing anxiety levels during the initial phase of the study (i.e., up to 1 year posttreatment). Future research is needed to determine optimal number and timing of booster sessions for CBT in school settings.
In contrast to our findings of no significant treatment differences in anxiety severity between group CBT with or without parent training at LTFU, Cobham and colleagues reported that children who received child-focused CBT plus parental anxiety management compared with those who received CBT alone were more likely to be free of their primary anxiety diagnosis at 3-year follow-up (38). Of note, no control group was included in the Cobham et al. LTFU study. Differences in findings may be due to methodological differences between studies. Children in the Cobham et al. study (N = 60) were required to meet diagnostic criteria for a primary anxiety diagnosis, whereas participants in our study needed a T-score of at least 58 on the MASC or a teacher nomination as a child with high anxiety. Also, while the Cobham et al. study excluded from data analyses those who were unreachable or dropped out, we included all participants in the LTFU analyses. In a review of parent involvement in nine CBT trials for anxiety disorders in youth, Barmish and Kendall (39) reported that child CBT plus parent interventions yielded effect sizes between small and large. The authors concluded that there are insufficient data to support that inclusion of parents is better than exclusion of parents in CBT for anxious children.
The current LTFU study had lower utilization of off-protocol treatments (25%) than the CAMS (70%). The number of participants who received off-protocol therapy was small, with only 5 (18.5%) in the combined CBT group and none in the control group. Of note, 5 students in the CBT group and 2 in the control group had an individualized educational plan at school. Although not significantly different (Table 3), these two findings suggest that participants in the combined CBT group were more likely than controls to engage in off-protocol services. Perhaps receiving school-based CBT heightened awareness about the potential benefits of other interventions for anxious children. Nevertheless, we are able to evaluate the long-term effects of the interventions without the confounding variable of high usage of off-protocol services.
Parent and youth ratings of child anxiety severity in our study were not congruent. Nevo and Manassis (14) emphasize the importance of collecting both parent and youth ratings to evaluate durability of treatment effects from different perspectives. Low concordance rates between parents and children on anxiety ratings have been reported in both clinical and community samples (40). Younger age, social desirability on the part of the child, and presence of internalizing symptoms rather than externalizing symptoms may reduce the level of parent-child agreement on psychiatric symptoms (41). Younger children tend to show less agreement with parents because of difficulty understanding and describing their feelings (42). Further, anxiety may compromise children’s cognitive processing and influence their ability to accurately report their anxiety (43). Anxious children commonly worry about how others perceive them and thus give socially desirable responses instead of providing valid self-reports (44, 45).
Other factors that are associated with increased discrepancy between parent- and child-report of anxiety include high levels of parental anxiety (46) and high levels of family stress (47). Some of the variables mentioned above likely contribute to our finding of significantly greater reduction in children’s anxiety severity over time in the combined treatment group compared with control group based on parents ratings but not on child ratings. Further research will help to elucidate which variables are most important in explaining low agreement between children and parents regarding severity of child anxiety symptoms.
Strengths of our study include a small no-treatment control group that helps to rule out passage of time, maturation, and spontaneous remission as explanations for benefits of active intervention over time. In addition, DSM-IV diagnostic criteria were employed across all assessment points providing greater clarity regarding diagnostic status relative to studies in which DSM-III-R criteria were employed at early time points and DSM-IV criteria were employed later. Similarly, youths were evaluated with the same measures across all follow-up points which improves the accuracy of comparisons across time. Furthermore, both parents and children completed the follow-up measures. In addition, monitoring of off-protocol services and the low rates of additional treatments used by both groups help assure that the long-term benefits, as demonstrated with the parent CSR, are due to effects of the acute treatment and not confounded by other services. Finally, retention rates for the current study were good, with 89% at 6 months compared with 79% at 6 months in the CAMS and 69% at 3 years compared with 59% at 6 years in the CAMS. Our high retention rates were likely due to incentives to families including payments for completing baseline, posttreatment, and follow-up assessments; dinner provided at school for families before the CBT sessions; and childcare for siblings provided during the CBT sessions.
There are several limitations of this study. The long-term control group was small. Twelve families agreed to continue in the control group with nine families remaining at 3-year follow-up. Although we included all 24 controls in the analyses using latent variable approach, replication of these results with a larger group of control participants would enhance confidence in the findings. Second, the statistical power to detect effects may have been compromised due to the small sample size (48). Replication of this study with a larger sample size is warranted. Third, LGCM using FIML in this study where half of the control participants’ follow-up data were excluded may have yielded biased estimates. The non-significant results of the analysis of missing data pattern provided some empirical support that the use of FIML may have reduced additional estimation bias associated with listwise deletion of cases with missing data. Fourth, at baseline 25% of participants were subthreshold for an anxiety diagnosis and all participants had mild to moderate symptoms. Therefore, the potential magnitude for improvement was limited, making the identification of significant changes over time difficult (22). However, rather than detracting from the significant findings reported here, inclusion of youth with subthreshold symptoms requires a greater effect size in order to detect group differences. Replication of this study with a sample including only children meeting full diagnostic criteria may result in even greater differences between groups. Fifth, data on potential confounding variables were not collected and thus not controlled for in the outcome analyses. For example, significant life stressors and levels of social support may have had an impact on the maintenance or reduction of anxiety symptoms. Findings of this study should be cautiously interpreted in light of these limitations. Finally, the generalizability of these results to culturally diverse groups is limited by including primarily middle-class Caucasian families. Future studies should include greater cultural diversity in the samples.
Summary.
The current study found evidence that, as documented with parent ratings, school-based CBT interventions may reduce the negative impact of anxiety in children over time. The parent CSR demonstrated that CBT interventions were superior to no-treatment control in reducing severity and impairment of child anxiety in a nonclinical sample across the entire 3-year LTFU period. Decline in parent-reported anxiety symptoms on the MASC and SCARED was initially more rapid and significant for the CBT interventions, compared with the control group. However, there was no significant group difference at the last assessment point. Child MASC and child CSR showed no group differences in rates of change over time. The results should be considered in the light of several methodological strengths including the use of a no-treatment control, a nonclinical sample, a longitudinal follow-up design, and latent piecewise growth curve modeling, as well as limitations including a small sample size. Replication in a larger sample is needed to confirm the findings.
Acknowledgements
This study was funded by grants from NIMH (MH065369) and University of Minnesota Academic Health Center (G.A.B.). The authors thank the families and schools who participated in the study.
Footnotes
Conflict of Interest: None for All Authors
Detailed data for the estimates comparing the two treatment conditions are available upon request to the first author.
References
- 1.Costello EJ, Egger HL, Angold A. Developmental epidemiology of anxiety disorders. In: Ollendick TH, March JS, editors. Phobic and Anxiety Disorders in Children and Adolescents. New York: Oxford University Press; 2004. [Google Scholar]
- 2.Vasey MW, Dadds MR. An introduction to the developmental psychopathology of anxiety. In: Vasey MW, Dadds MR, editors. The Developmental Psychopathology of Anxiety. New York: Oxford; 2001. pp. 1–26. [Google Scholar]
- 3.Connolly SD, Bernstein GA. Practice parameter for the assessment and treatment of children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry. 2007;46:267–283. doi: 10.1097/01.chi.0000246070.23695.06. [DOI] [PubMed] [Google Scholar]
- 4.Silverman WK, Pina AA, Viswesvaran C. Evidence-based psychosocial treatments for phobic and anxiety disorders in children and adolescents. Journal of Clinical Child & Adolescent Psychology. 2008;37:105–130. doi: 10.1080/15374410701817907. [DOI] [PubMed] [Google Scholar]
- 5.Walkup JT, Albano AM, Piacentini J, Birmaher B, Compton SN, Sherrill JT, et al. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. N Engl J Med. 2008;359:2753–2766. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barrett PM, Duffy AL, Dadds MR, Rapee RM. Cognitive-behavioral treatment of anxiety disorders in children: long-term (6-year) follow-up. J Consult Clin Psychol. 2001;69:135–141. [PubMed] [Google Scholar]
- 7.Barrett PM, Farrell LJ, Ollendick TH, Dadds M. Long-term outcomes of an Australian universal prevention trial of anxiety and depression symptoms in children and youth: an evaluation of the friends program. Journal of Clinical Child & Adolescent Psychology. 2006;35:403–411. doi: 10.1207/s15374424jccp3503_5. [DOI] [PubMed] [Google Scholar]
- 8.Dadds MR, Holland DE, Laurens KR, Mullins M, Barrett PM, Spence SH. Early intervention and prevention of anxiety disorders in children: results at 2-year follow-up. J Consult Clin Psychol. 1999;67:145–150. doi: 10.1037//0022-006x.67.1.145. [DOI] [PubMed] [Google Scholar]
- 9.Garcia-Lopez LJ, Olivares J, Beidel D, Albano AM, Turner S, Rosa AI. Efficacy of three treatment protocols for adolescents with social anxiety disorder: a 5-year follow-up assessment. J Anxiety Disord. 2006;20:175–191. doi: 10.1016/j.janxdis.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 10.Kendall PC, Safford S, Flannery-Schroeder E, Webb A. Child anxiety treatment: outcomes in adolescence and impact on substance use and depression at 7.4-year follow-up. J Consult Clin Psychol. 2004;72:276–287. doi: 10.1037/0022-006X.72.2.276. [DOI] [PubMed] [Google Scholar]
- 11.Kendall PC, Southam-Gerow MA. Long-term follow-up of a cognitive-behavioral therapy for anxiety-disordered youth. J Consult Clin Psychol. 1996;64:724–730. doi: 10.1037//0022-006x.64.4.724. [DOI] [PubMed] [Google Scholar]
- 12.Manassis K, Avery D, Butalia S, Mendlowitz S. Cognitive-behavioral therapy with childhood anxiety disorders: functioning in adolescence. Depress Anxiety. 2004;19:209–216. doi: 10.1002/da.10133. [DOI] [PubMed] [Google Scholar]
- 13.Ginsburg GS, Becker EM, Keeton CP, Sakolsky D, Piacentini J, Albano AM, et al. Naturalistic follow-up of youths treated for pediatric anxiety disorders. JAMA Psychiatry. 2014;71:310–318. doi: 10.1001/jamapsychiatry.2013.4186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nevo GA, Manassis K. Outcomes for treated anxious children: a critical review of Long-Term-Follow-Up studies. Depress Anxiety. 2009;26:650–660. doi: 10.1002/da.20584. [DOI] [PubMed] [Google Scholar]
- 15.Mifsud C, Rapee RM. Early intervention for childhood anxiety in a school setting: outcomes for an economically disadvantaged population. J Am Acad Child Adolesc Psychiatry. 2005;44:996–1004. doi: 10.1097/01.chi.0000173294.13441.87. [DOI] [PubMed] [Google Scholar]
- 16.Armbruster P. The administration of school-based mental health services. Child Adolesc Psychiatr Clin N Am. 2002;11:23–41. doi: 10.1016/s1056-4993(03)00059-2. [DOI] [PubMed] [Google Scholar]
- 17.Dadds MR, Spence SH, Holland DE, Barrett PM, Laurens KR. Prevention and early intervention for anxiety disorders: a controlled trial. J Consult Clin Psychol. 1997;65:627–635. doi: 10.1037//0022-006x.65.4.627. [DOI] [PubMed] [Google Scholar]
- 18.Masia Warner C, Fisher PH, Shrout PE, Rathor S, Klein RG. Treating adolescents with social anxiety disorder in school: an attention control trial. J Child Psychol Psychiatry. 2007;48:676–686. doi: 10.1111/j.1469-7610.2007.01737.x. [DOI] [PubMed] [Google Scholar]
- 19.Masia-Warner C, Klein RG, Dent HC, Fisher PH, Alvir J, Albano AM, et al. School-based intervention for adolescents with social anxiety disorder: results of a controlled study. J Abnorm Child Psychol. 2005;33:707–722. doi: 10.1007/s10802-005-7649-z. [DOI] [PubMed] [Google Scholar]
- 20.Stallard P. School-based interventions for depression and anxiety in children and adolescents. Evid Based Ment Health. 2013;16:60–61. doi: 10.1136/eb-2013-101242. [DOI] [PubMed] [Google Scholar]
- 21.Bernstein GA, Layne AE, Egan EA, Tennison DM. School-based interventions for anxious children. J Am Acad Child Adolesc Psychiatry. 2005;44:1118–1127. doi: 10.1097/01.chi.0000177323.40005.a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bernstein GA, Bernat DH, Victor AM, Layne AE. School-based interventions for anxious children: 3-, 6-, and 12-month follow-ups. J Am Acad Child Adolesc Psychiatry. 2008;47:1039–1047. doi: 10.1097/CHI.ob013e31817eecco. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.March JS, Parker JD, Sullivan K, Stallings P, Conners CK. The Multidimensional Anxiety Scale for Children (MASC): factor structure, reliability, and validity. J Am Acad Child Adolesc Psychiatry. 1997;36:554–565. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- 24.Barrett P, Webster H, Turner C. FRIENDS Prevention of Anxiety and Depression for Children Group Leader's Manual. Bowen Hills, Australia: Australian Academic Press; 2000. [Google Scholar]
- 25.Barrett PM. Group Coping Koala Workbook. Mt. Gravatt, Australia: Griffith University School of Applied Psychology; 1995. [Google Scholar]
- 26.Kendall PC. Coping Cat Manual. Ardmore, PA: Workbook Publishing; 1990. [Google Scholar]
- 27.Hollingshead AB. Four Factor Index of Social Status. New Haven, CT: Yale University Department of Sociology; 1975. [Google Scholar]
- 28.Lyneham HJ, Abbott MJ, Rapee RM. Interrater reliability of the Anxiety Disorders Interview Schedule for DSM-IV: Child and parent version. J Am Acad Child Adolesc Psychiatry. 2007;46:731–736. doi: 10.1097/chi.0b013e3180465a09. [DOI] [PubMed] [Google Scholar]
- 29.Wood JJ, Piacentini JC, Bergman RL, McCracken J, Barrios V. Concurrent validity of the anxiety disorders section of the Anxiety Disorders Interview Schedule for DSM-IV: Child and parent versions. Journal of Clinical Child & Adolescent Psychology. 2002;31:335–342. doi: 10.1207/S15374424JCCP3103_05. [DOI] [PubMed] [Google Scholar]
- 30.Baldwin JS, Dadds MR. Reliability and validity of parent and child versions of the Multidimensional Anxiety Scale for Children in community samples. J Am Acad Child Adolesc Psychiatry. 2007;46:252–260. doi: 10.1097/01.chi.0000246065.93200.a1. [DOI] [PubMed] [Google Scholar]
- 31.March JS. Manual for the Multidimensional Anxiety Scale for Children (MASC) Toronto, Canada: Multi-Health Systems; 1998. [Google Scholar]
- 32.Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): a replication study. J Am Acad Child Adolesc Psychiatry. 1999;38:1230–1236. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- 33.Muthen LK, Muthen BO. Mplus user's guide. 6th ed. Los Angeles, CA: 2010. [Google Scholar]
- 34.Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 35.Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Newbury Park, CA: Sage; 1993. [Google Scholar]
- 36.Hu L-T, Bentler PM. Cutoff criteria for fit indexes convariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- 37.Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 38.Cobham VE, Dadds MR, Spence SH, McDermott B. Parental anxiety in the treatment of childhood anxiety: a different story three years later. Journal of Clinical Child & Adolescent Psychology. 2010;39:410–420. doi: 10.1080/15374411003691719. [DOI] [PubMed] [Google Scholar]
- 39.Barmish AJ, Kendall PC. Should parents be co-clients in cognitive-behavioral therapy for anxious youth? J Clin Child Adolesc Psychol. 2005;34:569–581. doi: 10.1207/s15374424jccp3403_12. [DOI] [PubMed] [Google Scholar]
- 40.Miller LD, Martinez YJ, Shumka E, Baker H. Multiple informant agreement of child, parent, and teacher ratings of child anxiety within community samples. Can J Psychiatry. 2014;59:34–39. doi: 10.1177/070674371405900107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Grills AE, Ollendick TH. Issues in parent-child agreement: the case of structured diagnostic interviews. Clin Child Fam Psychol Rev. 2002;5:57–83. doi: 10.1023/a:1014573708569. [DOI] [PubMed] [Google Scholar]
- 42.Rapee RM, Barrett PM, Dadds MR, Evans L. Reliability of the DSM-III-R childhood anxiety disorders using structured interview: interrater and parent-child agreement. J Am Acad Child Adolesc Psychiatry. 1994;33:984–992. doi: 10.1097/00004583-199409000-00008. [DOI] [PubMed] [Google Scholar]
- 43.Vasey MW, MacLeod C. Information-processing factors in childhood anxiety: a review and develomental perspective. In: Vasey MW, Dadds MR, editors. The Developmental Psychopathology of Anxiety. New York: Oxford University Press; 2001. pp. 253–277. [Google Scholar]
- 44.Comer JS, Kendall PC. A symptom-level examination of parent-child agreement in the diagnosis of anxious youths. J Am Acad Child Adolesc Psychiatry. 2004;43:878–886. doi: 10.1097/01.chi.0000125092.35109.c5. [DOI] [PubMed] [Google Scholar]
- 45.Dadds MR, Perrin S, Yule W. Social desirability and self-reported anxiety in children: an analysis of the RCMAS Lie scale. J Abnorm Child Psychol. 1998;26:311–317. doi: 10.1023/a:1022610702439. [DOI] [PubMed] [Google Scholar]
- 46.Engel NA, Rodrigue JR, Geffken GR. Parent-child agreement on ratings of anxiety in children. Psychol Rep. 1994;75:1251–1260. doi: 10.2466/pr0.1994.75.3.1251. [DOI] [PubMed] [Google Scholar]
- 47.Jensen PS, Xenakis SN, Davis H, Degroot J. Child psychopathology rating scales and interrater agreement: II. Child and family characteristics. J Am Acad Child Adolesc Psychiatry. 1988;27:451–461. doi: 10.1097/00004583-198807000-00013. [DOI] [PubMed] [Google Scholar]
- 48.Curran PJ, Obeidat K, Losardo D. Twelve Frequently Asked Questions About Growth Curve Modeling. J Cogn Dev. 2010;11:121–136. doi: 10.1080/15248371003699969. [DOI] [PMC free article] [PubMed] [Google Scholar]