Abstract
Study question What are the long term trends in the total (live births, fetal deaths, and terminations of pregnancy for fetal anomaly) and live birth prevalence of neural tube defects (NTD) in Europe, where many countries have issued recommendations for folic acid supplementation but a policy for mandatory folic acid fortification of food does not exist?
Methods This was a population based, observational study using data on 11 353 cases of NTD not associated with chromosomal anomalies, including 4162 cases of anencephaly and 5776 cases of spina bifida from 28 EUROCAT (European Surveillance of Congenital Anomalies) registries covering approximately 12.5 million births in 19 countries between 1991 and 2011. The main outcome measures were total and live birth prevalence of NTD, as well as anencephaly and spina bifida, with time trends analysed using random effects Poisson regression models to account for heterogeneities across registries and splines to model non-linear time trends.
Summary answer and limitations Overall, the pooled total prevalence of NTD during the study period was 9.1 per 10 000 births. Prevalence of NTD fluctuated slightly but without an obvious downward trend, with the final estimate of the pooled total prevalence of NTD in 2011 similar to that in 1991. Estimates from Poisson models that took registry heterogeneities into account showed an annual increase of 4% (prevalence ratio 1.04, 95% confidence interval 1.01 to 1.07) in 1995-99 and a decrease of 3% per year in 1999-2003 (0.97, 0.95 to 0.99), with stable rates thereafter. The trend patterns for anencephaly and spina bifida were similar, but neither anomaly decreased substantially over time. The live birth prevalence of NTD generally decreased, especially for anencephaly. Registration problems or other data artefacts cannot be excluded as a partial explanation of the observed trends (or lack thereof) in the prevalence of NTD.
What this study adds In the absence of mandatory fortification, the prevalence of NTD has not decreased in Europe despite longstanding recommendations aimed at promoting peri-conceptional folic acid supplementation and existence of voluntary folic acid fortification.
Funding, competing interests, data sharing The study was funded by the European Public Health Commission, EUROCAT Joint Action 2011-2013. HD and ML received support from the European Commission DG Sanco during the conduct of this study. No additional data available.
Introduction
Neural tube defects (NTD) are a major group of severe congenital anomalies that are associated with substantial mortality, morbidity, and long term disability, as well as emotional, psychological, and economic costs.1 2 Each year, approximately 5000 fetuses in Europe are affected with NTD. Most of these cases are diagnosed prenatally, and termination of pregnancy for fetal anomaly is by far the most common outcome for fetuses with NTD.3 4 5
Convincing evidence shows that peri-conceptional folic acid supplementation can substantially decrease the prevalence of NTD.6 7 8 Whereas many countries in Europe have issued recommendations for folic acid supplementation for women of reproductive age, or specifically for those who intend to become pregnant, mandatory fortification programmes do not yet exist in Europe.9 A previous study found that in the past these recommendations had not had an appreciable effect on the prevalence of NTD in European countries.10 A more recent but preliminary analysis of the pooled data on the prevalence of NTD in the European Surveillance of Congenital Anomalies (EUROCAT) network suggested that their overall prevalence may have slightly decreased in the period 2004-08.5
Most population based congenital anomaly registries in Europe belong to the EUROCAT network (www.eurocat-network.eu/), with a common database. In 2009 EUROCAT published a special report on NTD,9 which showed that important barriers continue to exist for successful implementation of the recommendations for folic acid supplementation. Hence, only a small minority of women take folic acid supplements in the peri-conceptional period as recommended.11 12
In this study, we assessed the trends in the total prevalence and live birth prevalence of NTD in Europe by using data from EUROCAT registries for the period 1991-2011. We examined trends for all NTD combined, as well as separately for anencephaly and spina bifida, the most common forms of NTD.
Methods
Data sources
Since 1980, the EUROCAT central database has held individual anonymised records of cases of congenital anomaly occurring for full member registries and aggregate data for associate member registries, including live births, fetal deaths from 20 weeks gestational age, and termination of pregnancy for fetal anomaly. Information on each of the registries, including methods of case ascertainment and local procedures regarding ethics approval for the registries’ activities and their collaborations with EUROCAT, are available on the EUROCAT website (www.eurocat-network.eu/ABOUTUS/MemberRegistries/MembersAndRegistryDescriptions/AllMembers) and in the publication by Greenlees et al.13 All registries use ICD-9 (international classification of diseases, 9th revision) or ICD-10 with BPA extension to code up to nine syndrome or malformation codes for each case.
All cases that were not associated with a chromosomal anomaly and had a diagnostic code corresponding to a neural tube defect (ICD-9 740 -742 and ICD-10 Q00, Q01, Q05) were included for full and associate EUROCAT registries that could provide data from both the 1990s and the 2000s; most registries provided data for the entire, or almost the entire, time period between 1991 and 2011 (table 1). We extracted data on 11 353 cases of NTD, including 4162 cases of anencephaly (ICD-9 740 and ICD-10 Q00), 5776 cases of spina bifida (ICD-9 741 and ICD-10 Q05), and 1415 cases of encephalocele (ICD-9 7420 and ICD-10 Q01), from 28 registries in 19 countries covering approximately 12.5 million births, in October 2013 for the analysis of time trends in total and live birth prevalence of NTD between 1991 and 2011.
Table 1.
Total and live birth prevalence of neutral tube defects in study population, European Surveillance of Congenital Anomalies (EUROCAT), 1991-2011
| Place | Time period | Total births | Total live births | Neural tube defects* | Anencephaly | Spina bifida | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No | Prevalence per 10 000 births | No | Prevalence per 10 000 births | No | Prevalence per 10 000 births | ||||||
| Austria, Styria | 1991-2009 | 216 196 | 215 388 | 166 | 7.68 | 40 | 1.85 | 98 | 4.53 | ||
| Belgium, Antwerp | 1991-2011 | 337 862 | 336 481 | 283 | 8.38 | 100 | 2.96 | 156 | 4.62 | ||
| Belgium, Hainaut | 1991-2011 | 263 703 | 262 493 | 247 | 9.37 | 82 | 3.11 | 135 | 5.12 | ||
| Czech Republic | 2000-09 | 1 029 247 | 1 026 352 | 769 | 7.47 | 245 | 2.38 | 410 | 3.98 | ||
| Croatia, Zagreb | 1991-2010 | 131 525 | 130 913 | 63 | 4.79 | 18 | 1.37 | 36 | 2.74 | ||
| Denmark, Odense | 1991-2011 | 115 846 | 115 231 | 127 | 10.96 | 44 | 3.80 | 68 | 5.87 | ||
| Finland | 1993-2010 | 1 070 940 | 1 066 986 | 928 | 8.67 | 314 | 2.93 | 436 | 4.07 | ||
| France, Paris | 1991-2011 | 666 353 | 660 950 | 801 | 12.02 | 347 | 5.21 | 331 | 4.97 | ||
| Germany, Mainz† | 1991-2011 | 71 627 | 71 343 | 134 | 18.72 | 28 | 3.91 | 85 | 11.87 | ||
| Germany, Saxony-Anhalt | 1991-2011 | 289 124 | 287 850 | 258 | 8.93 | 67 | 2.32 | 151 | 5.22 | ||
| Hungary | 1998-2010 | 1 260 719 | 1 254 111 | 847 | 6.72 | 256 | 2.03 | 498 | 3.95 | ||
| Ireland, Cork and Kerry | 1996-2010 | 131 168 | 130 443 | 159 | 12.13 | 65 | 4.96 | 83 | 6.33 | ||
| Ireland, Dublin | 1991-2011 | 470 231 | 467 901 | 411 | 8.74 | 149 | 3.17 | 201 | 4.28 | ||
| Ireland, south east | 1997-2011 | 101 348 | 101 269 | 97 | 9.58 | 30 | 2.96 | 63 | 6.22 | ||
| Italy, Emilia Romagna | 1991-2011 | 656 637 | 654 627 | 350 | 5.33 | 109 | 1.66 | 202 | 3.08 | ||
| Italy, Tuscany | 1991-2011 | 558 669 | 556 582 | 313 | 5.60 | 108 | 1.93 | 163 | 2.92 | ||
| Malta | 1991-2010 | 88 573 | 88 202 | 97 | 10.95 | 25 | 2.82 | 56 | 6.32 | ||
| Netherlands, northern | 1991-2011 | 401 404 | 399 055 | 338 | 8.42 | 108 | 2.69 | 197 | 4.91 | ||
| Norway | 1999-2011 | 775 060 | 769 293 | 718 | 9.27 | 282 | 3.64 | 360 | 4.65 | ||
| Poland, Wielkopolska | 1999-2010 | 440 163 | 437 966 | 407 | 9.25 | 71 | 1.61 | 290 | 6.59 | ||
| Portugal, southern | 1991-2010 | 316 853 | 315 491 | 150 | 4.73 | 62 | 1.96 | 76 | 2.40 | ||
| Spain, Basque Country | 1991-2010 | 361 416 | 359 810 | 356 | 9.85 | 189 | 5.23 | 141 | 3.90 | ||
| Switzerland, Vaud | 1991-2011 | 159 273 | 158 617 | 162 | 10.17 | 62 | 3.89 | 74 | 4.65 | ||
| United Kingdom, East Midlands and South Yorkshire | 1998-2011 | 922 288 | 916 786 | 1012 | 10.97 | 426 | 4.62 | 480 | 5.21 | ||
| UK, northern England | 2000-2011 | 382 973 | 380 843 | 522 | 13.63 | 214 | 5.59 | 251 | 6.56 | ||
| UK, Thames Valley | 1991-2011 | 291 827 | 290 307 | 337 | 11.55 | 155 | 5.31 | 156 | 5.35 | ||
| UK, Wales | 1998-2011 | 466 358 | 463 941 | 703 | 15.08 | 278 | 5.96 | 330 | 7.08 | ||
| UK, Wessex | 1994-2011 | 492 629 | 490 436 | 598 | 12.14 | 288 | 5.85 | 249 | 5.06 | ||
| Total (95% CI) | 1991-2011 | 12 470 012 | 12 409 667 | 11 353 | 9.105 (8.94 to 9.27) | 4162 | 3.34 (3.24 to 3.44) | 5776 | 4.63 (4.51 to 4.75) | ||
*Total number comprises cases of anencephaly, spina bifida, and encephalocele.
†Higher prevalence of neural tube defects (NTD), specifically spina bifida, has been consistent observation in Mainz; substantial fluctuations in prevalence of NTD in Mainz occurred over time, however (as in other registries), and no evidence was found that lack of clear downward trend in prevalence of NTD in overall data could be explained by any changes in Mainz.
Patient involvement
No patients were involved in setting the research question or the outcome measures; nor were they involved in design and implementation of the study. There are no plans to involve patients in dissemination.
Data analysis
We plotted the time trends, during the period 1991 to 2011, in the total and live birth prevalence of all non-chromosomal NTD and separately for anencephaly and spina bifida. We defined total prevalence of NTD as the total number of cases of NTD (live births plus fetal deaths after 20 weeks of gestational age plus termination of pregnancy for fetal anomaly) per 10 000 total births (live births plus fetal deaths). We defined live birth prevalence as the number of live births with NTD per 10 000 live births. We examined the plots of time trends in total and live birth prevalence of NTD by using restricted cubic splines,14 15 which can provide a flexible, semi-parametric, continuous model of the relation between prevalence of NTD and time.
Using the number of births as the “exposure” variable, we then used random effects Poisson regression models to examine the annual trends in the prevalence of NTD, for all NTD combined and separately for anencephaly and spina bifida. We used random effects models to take into account any heterogeneity that may exist across the registries.16 17 In the Poisson models, we used linear splines (or “piece-wise exponential models”) for modelling the time trends in the prevalence of NTD; we used splines with five equally spaced knots based on the quintiles of the distribution of the time period to estimate separately the annual trends for the following time periods: 1991-95, 1995-99, 1999-2003, 2003-07, and 2007-11. We used Stata software (versions 11 and 13) for all analyses.
Results
Trends in total prevalence of NTD
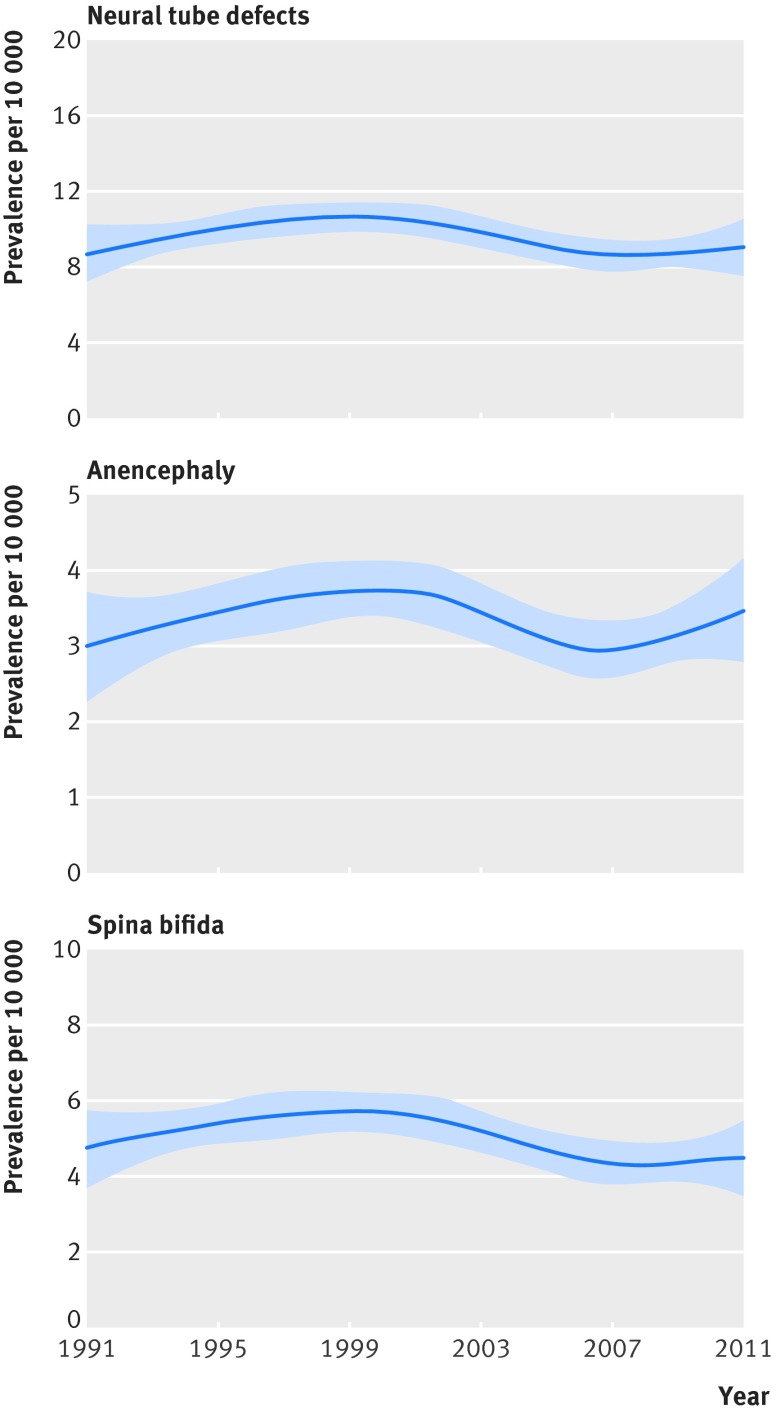
Figure 1 shows the time trend in the total prevalence of non-chromosomal NTD for the period 1991-2011, using pooled data from all of the EUROCAT registries included in the study and with time trends modelled with restricted cubic splines. The total prevalence of NTD was 9.1 (95% confidence interval 8.9 to 9.3) per 10 000 for 1991-2011 (table 1), fluctuating between a maximum of approximately 10.1 (highest) per 10 000 in the period 1999-2003 and 8.5 (lowest) per 10 000 in the period 2003-07 (fig 1). Overall, the total prevalence of NTD in 2011 was comparable to that in 1991. Time trend patterns in the pooled prevalence of anencephaly and spina bifida were comparable to those for all NTD combined.
Fig 1 Trends in total prevalence of non-chromosomal neural tube defects in Europe, 1991-2011: restrictive cubic spline estimates of pooled data in EUROCAT registries
Table 2 shows the results of random effects Poisson regression models that take into account heterogeneities across registries in estimating the time trends. Estimates are presented as prevalence ratios and can be interpreted as percentage increase (for ratios >1) or percentage decrease (for ratios <1). The estimates suggest that the total prevalence of NTD increased by about 4% a year between 1995 and 1999 (prevalence ratio 1.04, 95% confidence interval 1.01 to 1.07), decreased by 3% in 1999-2003 (0.97, 0.95 to 0.99), and was fairly stable thereafter.
Table 2.
Random effects Poisson regression models with splines (piece-wise exponential models) of trends in total and live birth prevalence of non-chromosomal neural tube defects, anencephaly, and spina bifida in 28 member registries in EUROCAT, 1991-2011
| Time period | Total prevalence | Live birth prevalence | |||
|---|---|---|---|---|---|
| Annual prevalence ratio (95% CI) | P value* | Annual prevalence ratio (95% CI) | P value* | ||
| All neural tube defects | |||||
| 1991-95 | 0.98 (0.95 to 1.02) | <0.001 | 0.93 (0.88 to 0.98) | <0.001 | |
| 1995-99 | 1.04 (1.01 to 1.07) | 0.97 (0.93 to 1.01) | |||
| 1999-2003 | 0.97 (0.95 to 0.99) | 0.96 (0.93 to 1.00) | |||
| 2003-07 | 0.99 (0.97 to 1.01) | 0.97 (0.93 to 1.00) | |||
| 2007-11 | 0.99 (0.97 to 1.01) | 0.98 (0.93 to 1.02) | |||
| Anencephaly | |||||
| 1991-95 | 1.01 (0.95 to 1.07) | <0.001 | 0.93 (0.80 to 1.09) | <0.001 | |
| 1995-99 | 1.03 (0.99 to 1.08) | 1.00 (0.89 to 1.13) | |||
| 1999-2003 | 0.98 (0.95 to 1.02) | 0.91 (0.82 to 1.00) | |||
| 2003-07 | 0.96 (0.93 to 0.99) | 0.99 (0.89 to 1.09) | |||
| 2007-11 | 1.01 (0.98 to 1.05) | 0.87 (0.76 to 1.00) | |||
| Spina bifida | |||||
| 1991-95 | 0.97 (0.92 to 1.02) | <0.001 | 0.94 (0.88 to 1.00) | <0.001 | |
| 1995-99 | 1.04 (1.00 to 1.07) | 0.96 (0.92 to 1.01) | |||
| 1999-2003 | 0.97 (0.94 to 1.00) | 0.97 (0.93 to 1.01) | |||
| 2003-07 | 0.99 (0.96 to 1.01) | 0.96 (0.93 to 1.00) | |||
| 2007-11 | 0.99 (0.96 to 1.03) | 1.00 (0.95 to 1.05) | |||
*P value tests statistical significance of any trend. In this case, significant P values indicate statistically significant non-monotonic trend for total prevalence and downward trend for live birth prevalence of neural tube defects, anencephaly, and spina bifida.
For non-chromosomal anencephaly, a slight increase was apparent in the 1990s, which was offset by a 4% decrease between 2003 and 2007 (prevalence ratio 0.96, 0.93 to 0.99), with stable rates afterwards until 2011. For non-chromosomal spina bifida, trends in the total prevalence mirrored those for overall NTD noted above (table 2).
Trends in live birth prevalence of NTD
Live birth prevalence of NTD was less than half of all cases of NTD and decreased substantially over the study period (fig 2). Estimates from the random effects Poisson models suggested that the decrease occurred more during the 1990s (table 2), once heterogeneities across registries were taken into account. Estimates from the random effects Poisson models also suggested that trends in live birth prevalence of spina bifida were similar to those for all NTD, whereas for anencephaly greater decreases were seen in the live birth prevalence, including a large decrease in the most recent period of 2007-11 equivalent to a 13% annual decrease (prevalence ratio 0.87, 0.76 to 1.00), compared with a stable total prevalence of anencephaly during the same period.
Fig 2 Trends in live birth prevalence of non-chromosomal neural tube defects in Europe, 1991-2011: restrictive cubic spline estimates of pooled data in EUROCAT registries
Discussion
Using data for more than 11 000 cases of non-chromosomal neural tube defects from 28 population based registries in 18 countries covering approximately 12.5 million births in Europe over the period 1991 to 2011, we found that the overall (pooled) total prevalence of NTD in 2011 was fairly similar to that in 1991 (~9 per 10 000 births). This was also true for the two main types of NTD, anencephaly and spina bifida, each of which accounts for approximately half of the cases of NTD. Whereas estimates from mixed models that took into account heterogeneities across registries suggested that a small decrease (~3% per year) in total prevalence of NTD between 1999 and 2003, this decrease followed a period of a comparable increase between 1995 and 1999. Overall, we found no clear evidence of a downward trend over the 20 year study period. In contrast, as a result of prenatal diagnosis and termination of pregnancy for fetal anomaly of most NTD in Europe, their live birth prevalence substantially decreased over time, especially for anencephaly.
Strengths and limitations of study
This was a large study looking at long term trends in the prevalence of NTD based on data from a number of population based registries in Europe. We took into account heterogeneities across registries by using random effects models. Nevertheless, we cannot exclude the possibility that registration problems or other data artefacts may be a partial explanation of the observed trends (or lack thereof) in the prevalence of NTD. However, we had no a priori reason to believe that any changes in registrations would have occurred in specific periods of time in a way that would explain the observed, long term time trends in our study.
Comparisons with other studies
Our results are consistent with those of an older study of trends in the prevalence of NTD in Europe.10 The overall long term fluctuations in the total prevalence of NTD in our data cannot be due to mandatory fortification of food staples, as such a policy has not yet been implemented in European countries.9 Voluntary fortification or the various recommendations issued for folic acid supplementation for women of reproductive age in European countries may have had an effect,9 18 19 even if small and as yet very little documented, on the intake of folic acid and thereby the prevalence of NTD.9 12 18 However, the available evidence points to very low uptake of folic acid supplementation in European countries.11 12
In any case, this was an ecological study and, even if folic acid is known to be an important factor for explaining trends in NTD, it is not the only possible reason for any changes in NTD over time. Changes in other risk factors of NTD (for example, maternal smoking)20 21 22 and changes in the incidence and management of maternal chronic health conditions, such as obesity, diabetes, and epilepsy, or psychiatric illnesses treated with anti-epileptic drugs that are known to be associated with a higher risk of NTD,23 24 25 as well as any changes in population characteristics (for example, owing to immigration),2 must also be considered as possible explanations for the observed fluctuations in the prevalence of NTD.
Conclusions and policy implications
Our results underscore the fact that 20 years after publication of the Medical Research Council study,6 which provided definitive evidence for the efficacy of folic acid in preventing NTD, and years after various recommendations have been issued to promote folic acid supplementation to ensure adequate peri-conceptional folate concentrations for pregnant women, Europe has failed to implement an effective policy for prevention of NTD by folic acid.
NTD represent one of the most prevalent group of birth defects with serious consequences for newborns and their families. Although termination of pregnancy for fetal anomaly has considerably reduced the live birth prevalence of these anomalies, it is certainly not an optimal solution for a birth defect that is highly preventable with a readily available and low cost measure, as is the case for NTD with folic acid supplementation or food fortification. Consumption of adequate natural folates should also be encouraged but in many countries will not raise folate concentrations sufficiently and is likely to leave vulnerable populations unprotected.
Our data suggest that recommendations, voluntary fortification, or both have not been effective in decreasing the prevalence of NTD in Europe. Hence, policies for mandatory fortification of food staples with folic acid should be considered as an important and more effective means for prevention of NTD,8 26 27 while weighing the evidence for its proven benefits and possible risks.2 19
What is already known on this topic
Peri-conceptional supplementation with folic acid can greatly reduce the risk of neural tube defects (NTD)
Although various recommendations for folic acid supplementation have been issued in Europe and elsewhere, important barriers exist for effective implementation of these recommendations
In contrast, mandatory fortification of food staples with folic acid has proved very effective in decreasing the prevalence of NTD
Up to date, population based data on the long term trends of the prevalence of NTD in Europe, where policies for mandatory fortification do not exist, are not available and could help to inform future policies
What this study adds
The prevalence of NTD has not decreased in Europe despite longstanding recommendations aimed at promoting peri-conceptional folic acid supplementation and the existence of voluntary folic acid fortification
Policies for mandatory fortification of food staples with folic acid should be considered as an important and more effective means for prevention of NTD in Europe
Contributors: BK, HdW, ML, and HD conceived the study. BK did the statistical analysis, with the assistance of ML, and wrote the first draft of the article. HD, ML, and HdW made substantial contributions to interpretation of results and revision of the manuscript. All other co-authors were registry representatives from EUROCAT participating registries. They contributed and validated their data and participated in the interpretation of results and critical revision of manuscript. BK and ML are the guarantors.
Funding: The study was funded by the European Public Health Commission, EUROCAT Joint Action 2011-2013 (grant No 2010 22 04). The funding body had no role in study design, analysis, or reporting.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf (available on request from corresponding author) and declare: HD and ML received support from the European Commission DG Sanco during the conduct of this study; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Data sharing: No additional data available.
Transparency: The lead authors (the manuscript’s guarantors) affirm that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Cite this as: BMJ 2015;351:h5949
References
- 1.Botto LD, Moore CA, Khoury MJ, Erickson JD. Neural-tube defects. N Engl J Med 1999;341:1509-19. [DOI] [PubMed] [Google Scholar]
- 2.Dunlap B, Shelke K, Salem SA, Keith LG. Folic acid and human reproduction—ten important issues for clinicians. J Exp Clin Assist Reprod 2011;8:2. [PMC free article] [PubMed] [Google Scholar]
- 3.Garne E, Loane M, Dolk H, et al. Prenatal diagnosis of severe structural congenital malformations in Europe. Ultrasound Obstet Gynecol 2005;25:6-11. [DOI] [PubMed] [Google Scholar]
- 4.Boyd PA, Devigan C, Khoshnood B, Loane M, Garne E, Dolk H. Survey of prenatal screening policies in Europe for structural malformations and chromosome anomalies, and their impact on detection and termination rates for neural tube defects and Down’s syndrome. BJOG 2008;115:689-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khoshnood B, Greenlees R, Loane M, Dolk H. Paper 2: EUROCAT public health indicators for congenital anomalies in Europe. Birth Defects Res A Clin Mol Teratol 2011;91(suppl 1):S16-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.MRC Vitamin Study Research Group. Prevention of neural tube defects: results of the Medical Research Council Vitamin Study. Lancet 1991;338:131-7. [PubMed] [Google Scholar]
- 7.Czeizel AE, Dudas I. Prevention of the first occurrence of neural-tube defects by periconceptional vitamin supplementation. N Engl J Med 1992;327:1832-5. [DOI] [PubMed] [Google Scholar]
- 8.Oakley GP Jr. The scientific basis for eliminating folic acid-preventable spina bifida: a modern miracle from epidemiology. Ann Epidemiol 2009;19:226-30. [DOI] [PubMed] [Google Scholar]
- 9.EUROCAT Folic Acid Working Group. EUROCAT special report: prevention of neural tube defects by folic acid supplementation in Europe. 2009. www.eurocat-network.eu/content/Special-Report-NTD-3rdEd-Part-I.pdf.
- 10.Busby A, Abramsky L, Dolk H, Armstrong B. Preventing neural tube defects in Europe: population based study. BMJ 2005;330:574-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bestwick JP, Huttly WJ, Morris JK, Wald NJ. Prevention of neural tube defects: a cross-sectional study of the uptake of folic acid supplementation in nearly half a million women. PLoS One 2014;9:e89354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tort J, Lelong N, Prunet C, Khoshnood B, Blondel B. Maternal and health care determinants of preconceptional use of folic acid supplementation in France: results from the 2010 National Perinatal Survey. BJOG 2013;120:1661-7. [DOI] [PubMed] [Google Scholar]
- 13.Greenlees R, Neville A, Addor MC, et al. Paper 6: EUROCAT member registries: organization and activities. Birth Defects Res A Clin Mol Teratol 2011;91(suppl 1):S51-100. [DOI] [PubMed] [Google Scholar]
- 14.Royston P. A strategy for modelling the effect of a continuous covariate in medicine and epidemiology. Stat Med 2000;19:1831-47. [DOI] [PubMed] [Google Scholar]
- 15.Sauerbrei W, Royston P, Binder H. Selection of important variables and determination of functional form for continuous predictors in multivariable model building. Stat Med 2007;26:5512-28. [DOI] [PubMed] [Google Scholar]
- 16.Rankin J, Pattenden S, Abramsky L, et al. Prevalence of congenital anomalies in five British regions, 1991-99. Arch Dis Child Fetal Neonatal Ed 2005;90:F374-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Loane M, Dolk H, Garne E, Greenlees R, EUROCAT Working Group. Paper 3: EUROCAT data quality indicators for population-based registries of congenital anomalies. Birth Defects Res A Clin Mol Teratol 2011;91(suppl 1):S23-30. [DOI] [PubMed] [Google Scholar]
- 18.Hoey L, McNulty H, Askin N, et al. Effect of a voluntary food fortification policy on folate, related B vitamin status, and homocysteine in health adults. Am J Clin Nutr 2007;86:1405-13. [DOI] [PubMed] [Google Scholar]
- 19.Flynn MA, Anderson WA, Burke SJ, Reilly A. Session 1: Public health nutrition. Folic acid food fortification: the Irish experience. Proc Nutr Soc 2008;67:381-9. [DOI] [PubMed] [Google Scholar]
- 20.Hackshaw A, Rodeck C, Boniface S. Maternal smoking in pregnancy and birth defects: a systematic review based on 173 687 malformed cases and 11.7 million controls. Hum Reprod Update 2011;17:589-604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mladovsky P, Allin S, Masseria C, Hernandez-Quevedo, McDaid D, Mossialos E. Health in the European Union: trends and analysis. World Health Organization, 2009: 76-81 (Observaotry Studies Series No 19).
- 22.Lelong N, Blondel B, Kaminski M. [Smoking during pregnancy in France between 1972 to 2003: results from the national perinatal surveys]. J Gynecol Obstet Biol Reprod (Paris) 2011;40:42-9. [DOI] [PubMed] [Google Scholar]
- 23.Jentink J, Bakker MK, Nijenhuis CM, Wilffert B, de Jong-van den Berg LT. Does folic acid use decrease the risk for spina bifida after in utero exposure to valproic acid? Pharmacoepidemiol Drug Saf 2010;19:803-7. [DOI] [PubMed] [Google Scholar]
- 24.Jentink J, Loane MA, Dolk H, et al. Valproic acid monotherapy in pregnancy and major congenital malformations. N Engl J Med 2010;362:2185-93. [DOI] [PubMed] [Google Scholar]
- 25.Jentink J, Dolk H, Loane MA, et al. Intrauterine exposure to carbamazepine and specific congenital malformations: systematic review and case-control study. BMJ 2010;341:c6581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Honein MA, Paulozzi LJ, Mathews TJ, Erickson JD, Wong LY. Impact of folic acid fortification of the US food supply on the occurrence of neural tube defects. JAMA 2001;285:2981-6. [DOI] [PubMed] [Google Scholar]
- 27.Oakley GP, Mandel JS. Folic acid fortification remains an urgent health priority. BMJ 2004;329:1376. [DOI] [PMC free article] [PubMed] [Google Scholar]