Abstract
The purpose of this research is to examine the relationship between psychological distress and aspects of health insurance status, including lack of coverage, types of coverage, and disruption in coverage, among U.S. adults.
Data from the 2001-2010 National Health Interview Survey were used to conduct analyses representative of the U.S. adult population aged 18-64 years. Multivariate analyses regressed psychological distress on health insurance status while controlling for covariates.
Adults with private or no health insurance coverage had lower levels of psychological distress than those with public/other coverage. Adults who recently (≤1 year) experienced a change in health insurance status had higher levels of distress than those who had not recently experienced a change. An interaction effect indicated the relationship between recent change in health insurance status and distress was not dependent on whether an adult had private vs. public/other coverage. However, for adults who had not experienced a change in status in the past year, the average absolute level of distress is higher among those with no coverage vs. private coverage.
Although significant relationships between psychological distress and health insurance status were identified, their strength was modest, with other demographic and health condition covariates also being potential sources of distress.
Keywords: psychological distress, health insurance coverage, uninsured, United States
Introduction
A well-known finding is that stress is related to the mental well-being and physical health of individuals (Cohen, Janicki-Deverts, & Miller, 2007; Pearlin, 1989; Pearlin, Lieberman, Menaghan, & Mullan, 1981). However, studying stress is no easy task: sources of stress are numerous, whether they may be the occurrence of discrete events in an individual's life such as divorce or the loss of a child, or ongoing chronic strains such as unemployment and financial uncertainty (Pearlin, 1989; Pearlin et al., 1981). With this in mind, the following study examines the association between health insurance status – a potential stressor – and psychological distress (i.e., the occurrence of symptoms such as anxiety, depression, and somatic discomfort that foster “a general state of emotional arousal or upset;” Thoits, 2010, p. S49). To the authors’ knowledge there has been little to no focus on how health insurance status is associated with psychological distress. An examination of this association could have a variety of implications for researchers who are interested in better understanding how health insurance status may be correlated to mental health.
An important step in studying psychological distress and health insurance status is to hypothesize how these phenomena might be related. An obvious instance of health insurance status serving as a stressor would be in the case of a lack of health insurance coverage. However, classification as insured or uninsured may be an oversimplification (Olson, Tang, & Newacheck, 2005), and other aspects of one's health insurance status may be important to consider. For example, the length or duration of a particular coverage status could also be taken into consideration. The chronic strain (see Pearlin, 1989; Thoits, 1995) from lack of insurance coverage for a lengthy duration of time would leave an individual (and potentially his/her family) vulnerable to the high cost of medical care. As a prolonged period of time passes, the chronic strain of these demands may continually manifest as psychological distress.
An argument could also be made that the disruption of coverage itself – not the actual duration of coverage – may be a culprit of psychological distress. Research has argued that the creation of stress may be fostered indirectly, where the occurrence of an event may shift or alter usual social statuses, roles, and expected behaviors with which an individual identifies and/or exhibits (George, 1993). This shift in social roles could therefore be associated with the reallocation of these roles, demanding that individuals in a specific network adapt to new social roles. For example, take an individual who has a social role of the provider of health insurance coverage for his/her family. After a disruption in coverage, s/he would no longer be able to fulfill this role of provider, placing stress on oneself and his/her family as they are now forced to determine who will take over the role of provider, and the new provider is forced to determine what is needed to fulfill this role. In this instance, it is not necessarily the specific reason for the loss of coverage that fosters psychological distress (although this reason could very well serve as a stressor; for example, experiencing unemployment), nor is it being fostered by the duration of time during which one is uninsured. Instead it is the social consequence of the disruption in coverage, and being in a state of lacking of coverage, that is acting as a stressor and fostering psychological distress among the individuals in this social network.
In addition to lack and duration of coverage, another aspect that may be important to consider is the type of health insurance coverage possessed by an individual, specifically whether a person is covered by private insurance or a public health insurance program. Both types of health insurance have specific but distinct aspects that can potentially introduce psychological distress through various manners, and create disruptions in coverage. For example, the stressful experience of underinsurance (i.e., having coverage yet being at risk for substantial out-of-pocket medical costs relative to one's income; Lavarreda, Brown, & Bolduc, 2011; Schoen, Collins, Kriss, & Doty, 2008a) differs by type of health insurance coverage. Research has found adults with private coverage are more likely to be underinsured relative to those with public coverage through the U.S. Medicaid program (Magge, Cabral, Kazis, & Sommers, 2013). Also, for private health insurance the majority of this coverage is offered through an individual's employer, and loss of a job can also lead to loss of one's private coverage (Schoen, Davis, & Collins, 2008b). An act as simple as leaving one's current job to work at another job can create a temporary stoppage in coverage (Collins, Robertson, Garber, & Doty, 2012; Schoen et al., 2008b). Even if brief, this disruption could be stressful if medical or health-related issues arise that result in costly medical bills.
Individuals covered by public plans are also at risk for the manifestation of psychological distress, but for different reasons. For example, the qualification for certain public health insurance programs is dependent upon situations that past research has found to be stressful, such as unemployment (Pearlin, 1989; Pearlin et al., 1981) or disability. Once obtained, the renewal of public health insurance coverage can be a lengthy and ongoing process; one that could be quite stressful. There are also a plethora of factors that lend themselves to a loss of public coverage or create short-term gaps between coverage (Summer and Mann, 2006). The frequent number of renewals faced by individuals can result in temporary coverage disruptions. Learning new rules, regulations, and eligibility procedures of a public health insurance program is not only a stressful process itself, but can also create temporary periods of non-coverage. Thus, for both private and public types of health insurance, different aspects of each insurance type may introduce psychological distress through various situations, in addition to allowing persons to be susceptible to coverage disruption. These situations may not necessarily be long-term, but can involve the loss and reacquisition of coverage over a short period of time, known as “churning” (Summer & Mann, 2006), and can be a source of stress for an individual and his/her family.
The goal of this research is to examine the association between health insurance status and psychological distress among U.S. adults. It is expected that not only will a lack of health insurance coverage be associated with psychological distress, but so will insurance type (i.e., private vs. public/other) and experiencing a disruption in coverage. Furthermore, as different types of insurance may be related to different causes of disruption, it is also hypothesized that interaction effects exist related to these two dimensions of health insurance status. To test these assumptions, a more elaborate operationalization of health insurance status is used to provide a detailed description of this relationship.
Method
Data
The 2001-2010 National Health Interview Survey (NHIS) restricted data files were used in the present study. The NHIS is a cross-sectional, multi-stage survey conducted continuously throughout the year, serves as a principal source of health data on the U.S. civilian, noninstitutionalized population (Schiller, Lucas, Ward, & Peregoy, 2012), and is the primary data source used to track health insurance coverage in the United States and progress toward the U.S. Department of Health and Human Service's (2013) Healthy People 2020 goals. The data analyzed in the present study were from 227,828 noninstitutionalized U.S. adults aged 18-64 years who completed the NHIS Sample Adult Core. The Sample Adult Core conditional response rates for these ten years (2001-2010) ranged from 74.2% in 2008 to 84.5% in 2003, while final response rates ranged from 60.8% in 2010 to 74.3% in 2002 (National Center for Health Statistics [NCHS], 2011). Ten years of NHIS data were appended together so that sample sizes for each health insurance status category would be large enough to yield reliable estimates, and economic contractions occurring during this time period were able to be accounted. Adults ≥65 years and over were excluded from the analyses in an attempt to remove the effects of changes in eligibility of various public health insurance programs due to age and/or retirement (e.g., Medicare), and to be consistent with other research on health insurance among U.S. adults that examines the <65 years and ≥65 years age groups as distinct subpopulations (Cohen & Martinez, 2013; Collins et al., 2012; Magge et al., 2013; Schoen et al., 2008a, 2008b). All adults in the sample with missing data for any of the variables of interest (with the exception of poverty status; see below) were removed (11.1% of cases). This created a final, standardized analytic sample of 202,663 used for all statistical analyses. A comparison of the standardized analytic sample to the full unstandardized sample revealed relatively small differences: all measures of interest differed by ≤0.6 percentage-points, with the exception of the measure for aerobic activity (1.1 percentage-point difference).
Measures
Psychological distress
To operationalize psychological distress in the present study, we used the K6 scale, a measure of non-specific psychological distress developed by Kessler and colleagues (2002). This scale was originally developed as a proxy for poor mental health (Colpe et al., 2001), and included in the NHIS in 1997. It was selected for inclusion because of an interest in capturing different dimensions (or severities) of distress as opposed to proportions of individuals above/below some specified threshold (Pearlin et al., 1981), a need for a measure that could be administered by laypersons in a structured interview setting, and restrictions on the time allotted in the NHIS to ask questions pertaining to psychological distress (Kessler et al., 2002). The K6 scale is used to identify individuals who are likely to meet formal definitions for certain types of mental illness (i.e., anxiety or depressive disorders), or those who may have a sub-clinical illness yet do not meet the formal definitions (e.g., ICD or DSM) for a specific disorder (Kessler et al., 2002; Myer, Stein, Grimsrud, Seedat, & Williams, 2008). Empirical testing has shown this scale to have good precision, and past research has validated its use for measuring psychological distress (Kessler et al., 2002). There is now a history of this scale appearing on the NHIS (Bratter & Eschbach, 2005; Dey & Lucas, 2006; Kessler et al., 2002), in addition to other U.S.-nationally representative health surveys (Colpe et al., 2010). Further details on the methodology and development of this scale can be found elsewhere (Kessler et al., 2002).
The K6 scale is created by combining six measures taken from survey questions that ask an adult “In the past 30 days, how often did you feel...” (a) so sad nothing could cheer you up; (b) nervous; (c) restless or fidgety; (d) hopeless; (e) that everything was an effort; and (f) worthless. Each of these items was categorized as: 0=none of the time; 1=a little of the time; 2=some of the time; 3=most of the time; 4=all of the time. The K6 scale had a possible range of 0-24, with higher scores indicating greater levels of psychological distress, and high internal consistency among our sample (α=.86).
The K6 scale was specifically designed to function similarly across various sociodemographic subgroups, and allows researchers the benefit of identifying distress levels ranging from mild to severe among national populations (Bratter & Eschbach, 2005; Kessler et al., 2002). To provide some context for interpreting the severity of distress captured by the scale, previous research has shown an optimal cut-point to balance “false-positive and false-negative results” for the prevalence of serious mental illness in the U.S. population as a score of 0-12 vs. ≥13 (Kessler et al., 2003, p. 188). Analysis using this cut-point shows that only a relatively small proportion (3.0%) of the U.S. adult population can be identified as having serious mental illness (Dey & Lucas, 2006), with the national prevalence varying only one percentage-point (i.e., 2.4%-3.4%) between the years 1997-2012 (Schiller, Ward, Freeman, & Peregoy, 2013). Research using the K6 shows low scores are not uncommon; for example, Bratter and Eschbach (2005) found a mean score of 2.52 among U.S. adults. When examining differences in distress among various racial/ethnic groups using the K6 scale, even small significant differences of approximately ±0.10 in mean scores and ±0.50 in linear regression coefficients are cited as being noteworthy to policy makers and health researchers (Bratter & Eschbach, 2005).
Health insurance status
Two measures were used to capture health insurance status. Both were created from survey questions asked in the NHIS family interview that precedes the Sample Adult Core; a family member other than the Sample Adult Core respondent may have answered these questions. The first was a series of questions that captured whether an adult currently had private health insurance coverage, public/other health insurance coverage, or no coverage. The public/other classification includes insurance from Medicare, Medicaid/Children's Health Insurance Program, a state-sponsored health plan, other government programs, or a military health plan. We did not differentiate between these various programs and instead placed them into a single category called “public/other health insurance,” as small sample sizes for certain programs would have been problematic when attempting to examine them individually. Note that adults with both private and public/other health insurance coverage were included in the category with adults who had private coverage (following the definition in Schiller et al., 2012).
The second measure of health insurance status was a determination whether there was a recent change in an individual's health insurance status, created by using two NHIS survey questions. In the NHIS, for currently insured adults, the respondent was asked “In the past 12 months, was there any time when {person} did not have any health insurance coverage?” For any uninsured adult, the respondent was asked “Not including Single Service Plans, about how long has it been since {person} last had health coverage?” These questions were used in our study to categorize if an adult's health insurance status had changed recently (≤1 year) or had not (>1 year). It is important to note that the variable for recent change in health insurance status refers to a change from insured to uninsured, or uninsured to insured. For currently insured adults this does not imply that one's coverage type (i.e., private or public/other) remained the same type of coverage throughout their most recent period of being insured. This was a limitation of the data.
Control variables
As demographic, health condition, and health behavior characteristics are related to the psychological distress experienced by an individual, a variety of measures were controlled for in this study; all found by past research to be related to stress and mental health (see citations listed after each control measure). Demographic characteristics controlled for in the analyses included dummy variables for whether or not a respondent was male (Hallman, Perski, Burell, Lisspers, & Setterlind, 2002; Schiller et al., 2013), U.S.-born (Dey & Lucas, 2006), currently married/cohabitating with a partner (Meyer & Paul, 2011), employed the week prior to the NHIS interview (Pearlin, 1989; Pearlin et al., 1981), and had one or more children (<18 years) living with the family/household (Angeles, 2010); and three series of dummy variables controlling for race/ethnicity (Hispanic, non-Hispanic white, non-Hispanic black, non-Hispanic other race; Dey & Lucas, 2006), age (18-24, 25-44, 45-64 years; Schiller et al., 2013), and education (less than high school, high school diploma/General Educational Development high school equivalency diploma [GED], some college, bachelor's degree or higher; Schiller et al., 2012). A series of dummy variables was also used for poverty status and included whether the respondent was poor (poverty ratio [PR]<100%), near poor (100≤PR<200%), or not poor (PR≥200%) (Schiller et al., 2012). The poverty ratio was calculated as: (family income/federal poverty threshold)*100. As is common in population surveys, the NHIS had a large number of missing values for its poverty and income variables, and multiply imputed income and poverty data made available with the NHIS were used to account for these missing values (Schenker et al., 2006).
Dummy control variables for health conditions included fair/poor respondent-assessed health status (Kaiser, Hartoonian, & Owen, 2010), physical disability (Turner & Noh, 1988) defined as having one or more activities of daily living (ADL) or instrumental activities of daily living (IADL) limitations, obesity (Grave, Calugi, Petroni, Di Domizio, & Marchesini, 2010) defined as a body mass index>30.0, or having one or more of the chronic conditions (Kaiser et al., 2010) considered by Goodman and colleagues (2013) (i.e., cancer, hypertension, coronary heart disease, stroke, chronic obstructive pulmonary disease, asthma, diabetes, arthritis, hepatitis, and/or weak or failing kidneys). Control variables that captured adults’ health behaviors included dummy variables for whether the respondent currently drank alcohol heavily (Foulds, Wells, Lacey, Adamson, Sellman, & Mulder, 2013), currently smoked (Ng & Jeffery, 2003), or engaged in sufficient aerobic physical activity (Ng & Jeffrey, 2003) defined as meeting the U.S. Department of Health and Human Service's physical activity guidelines (see Schoenborn & Stommel, 2011). Finally, as the data in our study span a ten year period that included two different U.S. economic recessions (March-November 2001 and December 2007- June 2009; National Bureau of Economic Research, 2010), a final dummy variable was used to identify if the NHIS interview occurred during a recession (Ayers et al., 2012).
Analytic procedures
All statistical analyses accounted for the additional covariance resulting from the complex cluster sampling design of the NHIS and used data weights to generate population estimates. As the NHIS data in this study originated from two distinct NHIS sample-design periods, variance estimates were adjusted to account for the statistically independent strata variables of each sample-design period (NCHS, 2012). Descriptive estimates were first examined for all study variables. Next, means and standard errors of psychological distress (K6) scores were examined by health insurance status measures. Two-tailed significance tests were used to determine if any significant differences existed. A series of multivariate models were then estimated using ordinary least squares (OLS) regression, each building upon the previous model by including additional control variables. The first model regressed the K6 scale score on both health insurance status measures. The second model regressed the K6 scale score upon both health insurance status and demographic characteristics. The third model added health condition variables, health behavior variables, and the control variable capturing if the interview occurred during a recession. In the final model, interaction terms between coverage type and recent change in health insurance status were included, and predicted marginals were calculated from the results of this final model. Diagnostic testing was performed for all multivariate analyses, and correlation coefficients (r≤.54) and variance inflation factors (VIF≤3.03) of the models provided no indication of multicollinearity.
Results
Descriptive characteristics
Among adults aged 18-64 years, 49.7% were male, 85.1% were U.S.-born, 64.1% were married/living with a partner, 73.9% were employed the week prior to the NHIS interview, and 44.1% had one or more children living with the family/household (Table I). The majority were non-Hispanic white (68.5%), followed by Hispanic (13.8%), non-Hispanic black (11.8%), and non-Hispanic other race (5.9%). Forty-five percent were aged 25-44 years, 39.5% were 45-64, and 15.5% were 18-24. Approximately one-third (31.1%) had completed some college, 27.4% had a high school diploma/GED, 27.7% a bachelor's degree or higher, and 13.8% less than a high school education. The majority (71.3%) were not poor, while 16.6% were near poor and 12.1% were in poverty. Four in ten adults (40.7%) had one or more chronic conditions, 26.0% were obese, 9.9% had fair/poor health status, and 2.4% had an ADL/IADL limitation. Forty-seven percent engaged in sufficient aerobic activity, 23.2% were current smokers, and 5.5% were current heavy alcohol drinkers. Approximately 23.6% of adults were interviewed during an economic recession.
Table I.
Descriptive Characteristics for demographic characteristics, health conditions, health behaviors, and economic climate among U.S. adults 18-64 years (unweighted n=202,663)
| % | (SE) | n | |
|---|---|---|---|
| Demographic characteristics | |||
| Male | 49.7 | (0.14) | 92,384 |
| Hispanic | 13.8 | (0.18) | 39,273 |
| Non-Hispanic white | 68.5 | (0.27) | 120,974 |
| Non-Hispanic black | 11.8 | (0.19) | 30,231 |
| Non-Hispanic other race | 5.9 | (0.13) | 12,185 |
| 18-24 yrs. | 15.5 | (0.18) | 26,247 |
| 25-44 yrs. | 45.0 | (0.17) | 95,672 |
| 45-64 yrs. | 39.5 | (0.19) | 80,744 |
| U.S.-born | 85.1 | (0.17) | 166,378 |
| Less than high school | 13.8 | (0.15) | 32,110 |
| High school diploma/GED | 27.4 | (0.18) | 54,078 |
| Some college | 31.1 | (0.17) | 62,481 |
| Bachelor's degree or higher | 27.7 | (0.23) | 53,994 |
| Married/living together | 64.1 | (0.21) | 110,200 |
| Child in family/household | 44.1 | (0.20) | 85,190 |
| Employed previous week | 73.9 | (0.15) | 148,276 |
| Poor (PR<100%)a | 12.1 | (0.16) | 32,409 |
| Near poor (100%≤PR<200%)a | 16.6 | (0.13) | 37,235 |
| Not poor (PR≥200%)a | 71.3 | (0.23) | 133,019 |
| Health conditions | |||
| Fair/poor health status | 9.9 | (0.10) | 22,590 |
| ADL/IADL limitation | 2.4 | (0.04) | 5,595 |
| Chronic condition(s) | 40.7 | (0.17) | 83,603 |
| Obese | 26.0 | (0.14) | 53,522 |
| Health behaviors | |||
| Current heavy alcohol drinker | 5.5 | (0.07) | 11,152 |
| Current smoker | 23.2 | (0.15) | 47,963 |
| Sufficient aerobic activity | 47.0 | (0.24) | 91,454 |
| Economic climate | |||
| Interviewed during recession | 23.6 | (0.21) | 43,382 |
Data source: National Health Interview Survey (NHIS), 2001-2010.
n = unweighted frequency; SE = standard error; GED = General Educational Development high school equivalency diploma; PR = poverty ratio; ADL = activity of daily living; IADL = instrumental activity of daily living.
Unweighted frequencies for poverty status obtained from the 2001-2010 NHIS imputed income files m=1.
Seven in ten (70.5%) adults had private health insurance, 10.9% had public/other, and 18.5% had no coverage (Table II). The majority of adults had not recently (>1 year) experienced a change in their health insurance status (90.8%), while 9.2% had recently (≤1 year) experienced a change. When looking at health insurance measures in combination, most adults (67.2%) were covered by private health insurance and had not recently experienced a change in status, while 9.7% were covered by public/other health insurance and had not recently experienced a change in status. The second largest health insurance category was adults who had no coverage and had not recently experienced a change in status (13.9%). Approximately 4.6% had no coverage and recently experienced a change in status, while 3.3% had private coverage and had recently experienced a change in status. Only 1.3% had public/other coverage and had recently experienced a change in status. The average score on the K6 scale was 2.5. Although this was at the lower end of the scale, it was similar to the average levels of psychological distress found in past research using the K6 scale with a large multi-purpose health survey (Bratter & Eschbach, 2005). Health insurance status measures and average score on the K6 scale were also estimated by demographic characteristics, health conditions, health behaviors, and economic climate, and are provided in Appendix Table A.
Table II.
Descriptive Characteristics for psychological distress and health insurance status among U.S. adults 18-64 years (unweighted n=202,663)
| Mean | % | (SE) | n | |
|---|---|---|---|---|
| Psychological distress | ||||
| K6 scale (range: 0-24)a | 2.5 | --- | (0.01) | 202,663 |
| During the past 30 days, how often did you feel (range: 0-4) | ||||
| So sad that nothing could cheer you up | 0.4 | --- | (<0.01) | 202,663 |
| Nervous | 0.6 | --- | (<0.01) | 202,663 |
| Restless or fidgety | 0.6 | --- | (<0.01) | 202,663 |
| Hopeless | 0.2 | --- | (<0.01) | 202,663 |
| That everything was an effort | 0.5 | --- | (<0.01) | 202,663 |
| Worthless | 0.2 | --- | (<0.01) | 202,663 |
| Health insurance status | ||||
| Coverage typeb | ||||
| Private | --- | 70.5 | (0.21) | 134,966 |
| Public/other | --- | 10.9 | (0.13) | 26,580 |
| No coverage | --- | 18.5 | (0.15) | 41,117 |
| Recent (≤1 year) change in status | ||||
| Yes | --- | 9.2 | (0.09) | 19,498 |
| No | --- | 90.8 | (0.09) | 183,165 |
| Coverage type and Recent (≤1 year) change in status | ||||
| Private coverage, experienced a recent change | --- | 3.3 | (0.05) | 6,745 |
| Public/other coverage, experienced a recent change | --- | 1.3 | (0.03) | 2,955 |
| No coverage, experienced a recent change | --- | 4.6 | (0.06) | 9,798 |
| Private coverage, did not experience a recent change | --- | 67.2 | (0.22) | 128,221 |
| Public/other coverage, did not experience a recent change | --- | 9.7 | (0.12) | 23,625 |
| No coverage, did not experience a recent change | --- | 13.9 | (0.13) | 31,319 |
Data source: National Health Interview Survey, 2001-2010.
n = unweighted frequency; SE = standard error; --- = not applicable.
Unweighted sample estimates for the K6 scale include a mean score of 2.6, SE of 0.01, and standard deviation of 3.99.
Percents do not add to 100.0% due to rounding.
K6 scores by health insurance status
Adults aged 18-64 years with public/other coverage (M=4.5) had the highest average score on the K6 scale, followed by those with no coverage (M=3.0), and those with private coverage (M=2.0) (Table III). Adults who had recently (≤1 year) experienced a change in status (M=3.5) had a significantly higher average K6 score than those who had not recently (>1 year) experienced a change (M=2.4). On average those with no coverage (regardless of whether a recent change had occurred) did not have the highest levels of psychological distress. It was those with public/other coverage who had not recently experienced a change in status (M=4.4) and those with public/other coverage who had recently experienced a change in status (M=5.1) who had the highest average levels of psychological distress. The lowest average score (M=1.9) on the K6 scale was among those adults who had private coverage and had not experienced a recent change in status, an average score more than 2.5 points lower than the score for those with public/other coverage (regardless of whether a recent change had occurred).
Table III.
Average psychological distress (K6 scale) by health insurance status among U.S. adults 18-64 years (unweighted n=202,663)
| Mean | (SE) | Sig. (p≤.01) | |
|---|---|---|---|
| Coverage type | |||
| Private | 2.0 | (0.01) | b, c |
| Public/other | 4.5 | (0.05) | a, c |
| No coverage | 3.0 | (0.03) | a, b |
| Recent (≤1 year) change in status | |||
| Yes | 3.5 | (0.04) | e |
| No | 2.4 | (0.01) | d |
| Coverage type and Recent (≤1 year) change in status | |||
| Private, experienced a recent change | 3.0 | (0.06) | g, h, i, j |
| Public/other, experienced a recent change | 5.1 | (0.13) | f, h, i, j, k |
| No coverage, experienced a recent change | 3.3 | (0.06) | f, g, i, j, k |
| Private, did not experience a recent change | 1.9 | (0.01) | f, g, h, j, k |
| Public/other, did not experience a recent change | 4.4 | (0.05) | f, g, h, i, k |
| No coverage, did not experience a recent change | 2.9 | (0.03) | g, h, i, j |
Data source: National Health Interview Survey, 2001-2010.
Significant differences between health insurance statuses were determined using a two-tailed significance test. SE = standard error.
Compared to “private coverage.”
Compared to “public/other coverage.”
Compared to “no coverage.”
Compared to “yes.”
Compared to “no.”
Compared to “private coverage, experienced a recent change.”
Compared to “public/other coverage, experienced a recent change.”
Compared to “no coverage, experienced a recent change.”
Compared to “private coverage, did not experience a recent change.”
Compared to “public/other coverage, did not experience a recent change.”
Compared to “no coverage, did not experience a recent change.”
Regression analyses of K6 on health insurance status
Table IV presents results of models that regressed the K6 scale upon health insurance status. In Model 1, relative to those with private health insurance coverage, adults aged 18-64 years with public/other coverage and no coverage had significantly higher average scores on the psychological distress (K6) scale. A similar OLS model was estimated that used no coverage as a reference category (table not shown), and showed those with public/other coverage were also more likely to have higher average levels of psychological distress compared to those with no coverage (b=1.60, SE=.057; p≤.01). The second health insurance status variable in Model 1 measured if a recent change in an adult's health insurance status had occurred. The results show that adults who recently (≤1 year) experienced a change in status had higher average scores on the K6 scale compared to adults who had not recently (>1 year) experienced a change in status.
Table IV.
Ordinary least squares regression of psychological distress (K6 scale) on health insurance status and control variables (unweighted n=202,663)
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|---|---|
| b | (SE) | b | (SE) | b | (SE) | b | (SE) | |
| Health insurance status | ||||||||
| Public/other coverage* | 2.46** | (.051) | 1.43** | (.050) | 0.65** | (.046) | 0.64** | (.048) |
| No coverage* | 0.86** | (.032) | 0.47** | (.035) | 0.38** | (.033) | 0.47** | (.036) |
| Recent (≤1 year) change in status | 0.73** | (.042) | 0.68** | (.042) | 0.61** | (.040) | 0.80** | (.055) |
| Demographic characteristics | ||||||||
| Male | -0.42** | (.020) | -0.47** | (.019) | -0.47** | (.019) | ||
| Hispanicb | -0.44** | (.038) | -0.30** | (.036) | -0.31** | (.036) | ||
| Non-Hispanic blackb | -0.58** | (.035) | -0.57** | (.033) | -0.56** | (.033) | ||
| Non-Hispanic other raceb | -0.01 | (.050) | -0.05 | (.046) | -0.05 | (.046) | ||
| 18-24 yrs.c | -0.67** | (.038) | 0.35** | (.036) | 0.34** | (.036) | ||
| 25-44 yrs.c | 0.04 | (.023) | 0.48** | (.023) | 0.48** | (.023) | ||
| U.S.-born | 0.70** | (.035) | 0.32** | (.033) | 0.32** | (.033) | ||
| Less than high schoold | 0.40** | (.043) | 0.17** | (.040) | 0.17** | (.040) | ||
| Some colleged | 0.04 | (.028) | 0.14** | (.026) | 0.14** | (.026) | ||
| Bachelor's degree or higherd | -0.39** | (.027) | -0.01 | (.026) | -0.01 | (.026) | ||
| Married/living together | -0.47** | (.024) | -0.36** | (.023) | -0.36** | (.023) | ||
| Child in family/household | -0.23** | (.023) | -0.03 | (.021) | -0.03 | (.022) | ||
| Employed previous week | -1.02** | (.029) | -0.51** | (.026) | -0.51** | (.026) | ||
| Poor (PR<100%)e | 0.93** | (.048) | 0.63** | (.042) | 0.61** | (.043) | ||
| Near poor (100%≤PR<200%)e | 0.56** | (.034) | 0.31** | (.032) | 0.30** | (.032) | ||
| Health conditions | ||||||||
| Fair/poor health status | 2.76** | (.053) | 2.76** | (.053) | ||||
| ADL/IADL limitation | 2.78** | (.115) | 2.78** | (.115) | ||||
| Chronic condition(s) | 0.86** | (.022) | 0.86** | (.022) | ||||
| Obese | 0.17** | (.023) | 0.17** | (.023) | ||||
| Health behaviors | ||||||||
| Current heavy alcohol drinker | 0.56** | (.046) | 0.56** | (.046) | ||||
| Current smoker | 0.84** | (.026) | 0.84** | (.026) | ||||
| Sufficient aerobic activity | 0.05* | (.020) | 0.05* | (.020) | ||||
| Economic climate | ||||||||
| Interviewed during recession | 0.16** | (.025) | 0.16** | (.025) | ||||
| Health insurance status interactions | ||||||||
| Public/other coverage × Recent changef | 0.04 | (.132) | ||||||
| No coverage × Recent changef | -0.46** | (.079) | ||||||
| Intercept | 1.96** | (.013) | 2.96** | (.055) | 1.47** | (.054) | 1.46** | (.054) |
| R2 | 0.048 | 0.091 | 0.185 | 0.185 | ||||
Data source: National Health Interview Survey, 2001-2010.
p≤05
p≤.01. b = unstandardized coefficient; SE = standard error; PR = poverty ratio; ADL = activity of daily living; IADL = instrumental activity of daily living.
Reference category is “private coverage.”
Reference category is “non-Hispanic white.”
Reference category is “45-64 yrs.”
Reference category is “high school diploma/General Educational Development high school equivalency diploma.”
Reference category is “not poor (PR≥200%).”
Reference category is “private coverage × recent change.”
In the next model demographic characteristics were controlled. Here the nature of the effect of coverage type and recent change in health insurance status on psychological distress remained, but the magnitude decreased. When controlling for demographics, again relative to adults with private health insurance those with public/other insurance and no coverage had higher average K6 scores. Using no coverage as a reference category (table not shown), adults with public/other coverage had a score of 0.96 higher on average (SE=.053; p≤.01). The coefficient for recent change in health insurance status remained positive and relatively unchanged in size between Models 1 and 2. A number of demographic control variables had significant relationships with the K6 scale: those who were employed had less psychological distress on average compared to those not employed, and those adults who were a member of a family in poverty had higher average levels of psychological distress than those adults who were in a family that was not poor.
Model 3 added health conditions, health behaviors, and the control variable capturing if the NHIS interview occurred during a recession. Relative to those with private coverage, the coefficients for those with public/other coverage and no coverage remained significant, yet further decreased in magnitude. When using no coverage as the reference category (table not shown) a similar decrease was found: those with public/other coverage had higher average levels of psychological distress (b=0.27, SE=.049; p≤.01). Unlike these decreases in coefficient size for coverage type, the coefficient for recent change in health insurance status remained stable; those who had recently experienced a change in status had higher average levels of psychological distress compared to those who had not recently experienced a change. Two health condition measures were found to have substantial relationships with psychological distress. Those with fair/poor health had a higher average score on the K6 scale compared to those with good to excellent health, while those with an ADL/IADL limitation had a higher average score on the K6 scale compared to those without a limitation. Two health behavior measures also had modest, significant relationships: adults who were current heavy drinkers had higher K6 scores on average compared to those who were not current heavy drinkers, and adults who currently smoked had higher K6 scores on average compared to those who did not. A small, positive, and statistically significant relationship was found for those adults interviewed during a recession period.
Finally, a fourth model was estimated with interaction terms for coverage type and experiencing a recent (≤1 year) change in health insurance status. In this model, relative to adults with private coverage, those with public/other coverage had higher levels of psychological distress. The interaction term for coverage type (private or public/other coverage) and recently experiencing a change in health insurance status was not significant, indicating the relationship between recent change in health insurance status and psychological distress was not dependent on whether an adult had private vs. public/other health insurance coverage.
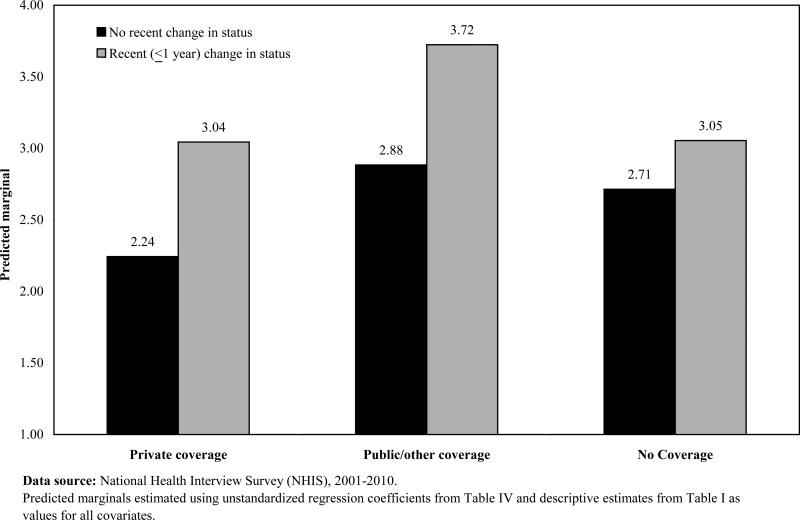
Model 4 also showed that adults with no coverage had a higher level of psychological distress relative to those with private coverage. The interaction term for coverage type (private or no coverage) and recently experiencing a change in status was statistically significant. Note that the interaction term is negative, and taking both the main and interaction effects into consideration, these results indicate that for adults who had not experienced a change status in the past year, the average absolute level of psychological distress remains higher among those with no coverage compared to those with private coverage. However, as Figure I shows, for adults who had experienced a change status in the past year, the difference associated with coverage type is much smaller. The average absolute level of psychological distress is nearly the same (a difference of 0.1) among adults with no coverage (i.e., adults who have recently lost coverage) compared to those with private coverage (i.e., adults who have recently obtained coverage).
Figure I.
Predicted marginals for psychological distress (K6 scale) among U.S. adults 18-64 years, by coverage type and change in health insurance status
Using no coverage as the reference category (table not shown), those with public/other coverage had significantly higher levels of psychological distress than those with no coverage (b=0.17; p≤.01). The interaction term for coverage type (public/other or no coverage) and recently experienced a change in status was also statistically significant (b=0.49; p≤.01). Thus, not only did adults with public/other coverage have higher absolute levels of psychological distress relative to those with no coverage, but recently experiencing a change in status was associated with an even higher level of psychological distress among those with public/other coverage compared to those with no coverage.
Discussion
This study examined the association between health insurance status and psychological distress. It was hypothesized that coverage type and experiencing a disruption in coverage could significantly impact psychological distress experienced by U.S. adults, and that an interaction effect exists among these measures of health insurance status. The first important finding was that psychological distress varied by type of health insurance coverage. Adults aged 18-64 years who had public/other coverage had the highest average levels of psychological distress, followed by those with no coverage, and then by adults with private coverage. The magnitude of these differences decreased noticeably as additional covariates were included in the model, where the greatest stressors appeared to be nativity, employment, poverty status, health status, and physical limitations. In absolute terms, irrespective of coverage type these levels of distress among U.S. adults are rather mild, with the mildest levels among those with private coverage. While the average differences in distress found in this study may not have clinical implications, previous research (Bratter & Eschbach, 2005) has considered K6 scores similar to the magnitude we found in our study, and the magnitude of the differences we found between them, to be noteworthy for researchers and policy makers.
Another finding in this study was that adults having faced a recent change in health insurance status (≤1 year) experienced higher levels of psychological distress on average compared to adults who had not recently (>1 year) experienced a change. Unlike type of coverage, the modest relationship between recent change in status and psychological distress remained as control variables were added to the model; no real decrease in magnitude occurred. One of the most interesting findings of this study was the interaction term showing that experiencing a recent change in status was associated with a greater difference in psychological distress for adults with private or public/other coverage relative to those with no coverage. Contrary to what was expected, this term implies that recent movement from being uninsured to having health insurance coverage (i.e., gaining coverage) is associated with experiencing higher levels of distress relative to movement from having coverage to becoming uninsured (i.e., losing coverage).
Although an interaction effect was found, its direction was unexpected based on our review of the theoretical and empirical literature. This finding that recently gaining insurance is associated with higher levels of psychological distress raises questions as to what may be driving this relationship. We can only speculate about the reasons. Among recently uninsured adults who had gained private coverage, this association may stem from beginning a new job. New employment can be stressful not only for the individual himself/herself, but may subsequently manifest as distress among other family members through the shifting of social roles (George, 1993) or having to move residences and relocate to another geographical area (Riemer, 2000). Recent acquisition of public coverage through a program such as Medicaid can correspond to the loss of employment or experiencing a physical/mental disability, both experiences that our analyses and those of others (Pearlin, 1989; Pearlin et al., 1981; Turner & Noh, 1988) have shown to increase psychological distress among adults. A gain in public insurance may also be the result of churning (Summer & Mann, 2006), with this gain being one stage in a string of disruptions in coverage.
Perhaps the biggest limitation of our study was that NHIS data are not longitudinal in nature. This would have allowed for us to gain an even better understanding of the relationship between psychological distress and health insurance status, especially when examining recent change in one's health insurance status and the amount of time spent with a specific coverage type. Longitudinal data would have also allowed for causal inference and helped to account for the possibility of a two-directional relationship between psychological distress and health insurance status. Furthermore, it would have allowed us to use more consistent timeframes of reference among variables measuring psychological distress and health insurance status. This inconsistency among our timeframes was a clear limitation of our study, as it not only prevented us from knowing whether one's current coverage was the same prior to the 30-day reference period used for the K6 scale, but also from knowing if one's change in health insurance status occurred within this 30-day reference period, or exactly how close to this reference period it did occur.
As cross-sectional data from 2001-2010 were appended together, another limitation was having to make the assumption that the relationships between variables remained consistent over this time period. Our study focused on adults 18-64 years, and the results cannot be generalized to those ≥65 years. To make such generalizations, future research would need to focus explicitly on this subpopulation. In addition, this study was limited to measures available in the NHIS. Additional measures of health insurance status and change in health insurance status (including the reasons behind having one type of coverage vs. another, and the reasons behind experiencing a specific change) could have yielded further understanding of the relation to psychological distress. It would have also been beneficial if our study was able to account for change in employment status, a source of stress (Pearlin et al., 1981) that is related to health insurance coverage (Schoen et al., 2008b). Finally, although the K6 is a reliable (Kessler et al., 2002) and a relatively well-known measure (Colpe et al., 2010) of psychological distress, a number of other measures that can capture various manifestations of stress have since been developed (Thoits, 2010) and may have yielded additional understanding of this association had they been available.
In spite of these limitations, this exploratory study provides a basis upon which future research can build. Additional analyses that attempt to better understand the interaction between health insurance type and recent change in coverage on psychological distress may be warranted. To our knowledge this exploratory study was the first to examine the association between health insurance and psychological distress, and provides initial insights to this association for U.S. adults aged 18-64 years. Its results imply that studies seeking to examine psychological distress may benefit from considering the multi-faceted and complex relationship between health insurance status, correlates of health insurance and psychological distress, and how these relationships might change as health insurance coverage changes in the United States (Cohen & Martinez, 2013). Of course, changes in health insurance coverage may be related to some (but certainly not all) of the stressors a person experiences, and alone it will not fully explain the psychological distress experienced by an individual. However, accounting for this particular variable may assist in developing a more comprehensive understanding of stress, the stress process, and the relationship between stress and health.
Acknowledgements
No financial support was received for this paper. All views expressed in this manuscript belong to the authors and do not necessarily represent the official views of the National Center for Health Statistics, Centers for Disease Control and Prevention, or U.S. Department of Health and Human Services.
Appendix
Table A.
Health insurance status and psychological distress (K6 scale) by control variables among U.S. adults 18-64 years (unweighted n=202,663)
| Private coverage | Public/other coverage | No coverage | Recent (≤1 yr.) change in status | Psychological distress (K6) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| % | (SE) | % | (SE) | % | (SE) | % | (SE) | Mean | (SE) | |
| Demographic characteristics | ||||||||||
| Male | 70.8 | (0.25) | 8.8 | (0.14) | 20.4 | (0.20) | 8.8 | (0.12) | 2.1 | (0.02) |
| Hispanic | 45.8 | (0.46) | 13.8 | (0.28) | 40.4 | (0.46) | 11.1 | (0.21) | 2.3 | (0.03) |
| Non-Hispanic white | 77.7 | (0.23) | 8.7 | (0.15) | 13.6 | (0.15) | 8.4 | (0.11) | 2.5 | (0.02) |
| Non-Hispanic black | 57.3 | (0.44) | 20.4 | (0.37) | 22.3 | (0.32) | 11.7 | (0.23) | 2.5 | (0.03) |
| Non-Hispanic other race | 71.3 | (0.62) | 11.2 | (0.41) | 17.5 | (0.49) | 8.7 | (0.33) | 2.2 | (0.04) |
| 18-24 yrs. | 58.2 | (0.55) | 13.9 | (0.33) | 27.9 | (0.44) | 16.6 | (0.30) | 2.5 | (0.03) |
| 25-44 yrs.a | 70.0 | (0.26) | 9.5 | (0.15) | 20.6 | (0.21) | 10.2 | (0.12) | 2.4 | (0.02) |
| 45-64 yrs.a | 76.1 | (0.23) | 11.5 | (0.17) | 12.5 | (0.16) | 5.1 | (<0.01) | 2.5 | (0.02) |
| U.S.-born | 73.6 | (0.22) | 11.1 | (0.15) | 15.3 | (0.14) | 9.2 | (<0.01) | 2.5 | (0.02) |
| Less than high schoola | 36.8 | (0.41) | 23.5 | (0.36) | 39.8 | (0.41) | 11.4 | (0.23) | 3.3 | (0.04) |
| High school diploma/GED | 64.0 | (0.31) | 13.3 | (0.21) | 22.7 | (0.25) | 10.2 | (0.16) | 2.6 | (0.03) |
| Some college | 74.5 | (0.26) | 9.6 | (0.18) | 15.9 | (0.19) | 10.3 | (0.15) | 2.5 | (0.02) |
| Bachelor's degree or highera | 89.5 | (0.18) | 3.9 | (0.11) | 6.7 | (0.14) | 5.9 | (0.13) | 1.8 | (0.02) |
| Married/living togethera | 76.6 | (0.22) | 8.2 | (0.14) | 15.3 | (0.17) | 7.6 | (0.10) | 2.2 | (0.02) |
| Child in family/householda | 67.9 | (0.28) | 12.5 | (0.19) | 19.7 | (0.22) | 9.9 | (0.13) | 2.3 | (0.02) |
| Employed previous week | 78.3 | (0.18) | 5.3 | (<0.01) | 16.4 | (0.16) | 8.2 | (<0.01) | 2.0 | (0.01) |
| Poor (PR<100%)b | 25.7 | (0.91) | 36.5 | (0.63) | 37.8 | (0.60) | 15.1 | (0.33) | 4.2 | (0.06) |
| Near poor (100%≤PR<200%)b | 42.3 | (0.40) | 19.8 | (0.33) | 37.9 | (0.39) | 15.3 | (0.26) | 3.3 | (0.04) |
| Not poor (PR≥200%)b | 84.6 | (0.16) | 4.6 | (0.10) | 10.8 | (0.13) | 7.5 | (0.11) | 2.1 | (0.01) |
| Health conditions | ||||||||||
| Fair/poor health status | 43.0 | (0.46) | 34.7 | (0.45) | 22.3 | (0.37) | 10.4 | (0.26) | 6.2 | (0.06) |
| ADL/IADL limitation | 35.2 | (0.87) | 54.0 | (0.89) | 10.8 | (0.50) | 8.1 | (0.44) | 7.9 | (0.12) |
| Chronic condition(s) | 70.2 | (0.26) | 15.1 | (0.19) | 14.7 | (0.17) | 8.5 | (0.12) | 3.3 | (0.02) |
| Obese | 66.9 | (0.30) | 14.5 | (0.22) | 18.6 | (0.23) | 9.8 | (0.16) | 3.0 | (0.03) |
| Health behaviors | ||||||||||
| Current heavy alcohol drinker | 67.9 | (0.60) | 8.7 | (0.32) | 23.4 | (0.54) | 11.7 | (0.39) | 3.3 | (0.05) |
| Current smoker | 56.8 | (0.35) | 15.7 | (0.24) | 27.5 | (0.28) | 13.3 | (0.21) | 3.6 | (0.03) |
| Sufficient aerobic activitya | 77.8 | (0.22) | 7.2 | (0.13) | 15.1 | (0.17) | 9.0 | (0.12) | 2.2 | (0.02) |
| Economic climate | ||||||||||
| Interviewed during recession | 70.8 | (0.36) | 11.0 | (0.23) | 18.2 | (0.27) | 9.5 | (0.19) | 2.6 | (0.03) |
Data source: National Health Interview Survey (NHIS), 2001-2010.
n = unweighted frequency; SE = standard error; GED = General Educational Development high school equivalency diploma; PR = poverty ratio; ADL = activity of daily living; IADL = instrumental activity of daily living.
Prevalence of private, public/other, and no coverage across this attribute do not add to 100.0% due to rounding.
Estimates by poverty status categories generated from the 2001-2010 NHIS imputed income files m=1.
References
- Altman B, Bernstein A. Disability and health in the United States, 2001-2005. National Center for Health Statistics; Hyattsvile: 2008. [Google Scholar]
- Angeles L. Children and life satisfaction. Journal of Happiness Studies. 2010;11:523–538. [Google Scholar]
- Ayers JW, Althouse BM, Allem JP, Childers MA, Zafar W, Ribisl KM, Brownstein JS. Novel surveillance of psychological distress during the great recession. Journal of Affective Disorders. 2012;142:323–330. doi: 10.1016/j.jad.2012.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bratter JL, Eschbach K. Race/ethnic differences in nonspecific psychological distress: evidence from the National Health Interview Survey. Social Science Quarterly. 2005;86:620–644. [Google Scholar]
- Cohen RA, Martinez ME. Health insurance coverage: early release of estimates from the National Health Interview Survey, 2012. National Center for Health Statistics; Hyattsville: 2013. [Google Scholar]
- Cohen S, Janicki-Deverts D, Miller GE. Psychological stress and disease. JAMA. 2007;298:1685–1687. doi: 10.1001/jama.298.14.1685. [DOI] [PubMed] [Google Scholar]
- Collins SR, Robertson R, Garber T, Doty MM. Gaps in health insurance: why so many Americans experience breaks in coverage and the how the Affordable Care Act will help. The Commonwealth Fund; New York: 2012. [PubMed] [Google Scholar]
- Colpe LJ, Freeman EJ, Strine TW, Dhingra S, McGuire LC, Elam-Evans LD, Perry GS. Public health surveillance for mental health. Preventing Chronic Disease. 2010;7:A1–A7. [PMC free article] [PubMed] [Google Scholar]
- Dey AN, Lucas JW. Physical and mental health characteristics of U.S.- and foreign-born adults: United States, 1998-2003. Advance Data. 2006;369:1–20. [PubMed] [Google Scholar]
- Foulds JA, Wells JE, Lacey CJ, Adamson SJ, Sellman JD, Mulder RT. A comparison of alcohol measures as predictors of psychological distress in the New Zealand population. International Journal of Alcohol and Drug Research. 2013;2:59–67. [Google Scholar]
- George LK. Sociological perspectives on life transitions. Annual Review of Sociology. 1993;19:353–373. [Google Scholar]
- Goodman RA, Posner SF, Huang ES, Parekh AK, Koh HK. Defining and measuring chronic conditions: imperatives for research, policy, program, and practice. [June 19, 2013];Preventing Chronic Disease. 2013 10 doi: 10.5888/pcd10.120239. from: http://www.cdc.gov/pcd/issues/2013/12_0239.htm. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grave RD, Calugi S, Petroni ML, Di Domizio S, Marchesini G. Weight management, psychological distress and binge eating in obesity: a reappraisal of the problem. Appetite. 2010;54:269–273. doi: 10.1016/j.appet.2009.11.010. [DOI] [PubMed] [Google Scholar]
- Hallman T, Perski A, Burell G, Lisspers J, Setterlind S. Perspectives on differences in perceived external stress: a study of women and men with coronary heart disease. Stress and Health. 2002;18:105–118. [Google Scholar]
- Kaiser NC, Hartoonian N, Owen JE. Toward a cancer-specific model of psychological distress: population data from the 2003-2005 National Health Interview Surveys. Journal of Cancer Survivorship. 2010;4:291–302. doi: 10.1007/s11764-010-0120-3. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand S-LT, Walters EE, Zaslavsky AM. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine. 2002;32:959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Howes MJ, Normand SLT, Manderscheid RW, Walters EE, Zaslavsky AM. Screening for serious mental illness in the general population. Archives of General Psychiatry. 2003;60:184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- Lavarreda SA, Brown ER, Bolduc CD. Underinsurance in the United States: an interaction of costs to consumers, benefit design, and access to care. Annual Review of Public Health. 2011;32:471–482. doi: 10.1146/annurev.publhealth.012809.103655. [DOI] [PubMed] [Google Scholar]
- Magge H, Cabral HJ, Kazis LE, Sommers B. Prevalence and predictors of underinsurance among low-income adults. Journal of General Internal Medicine. 2013 doi: 10.1007/s11606-013-2354-z. doi:10.1007/s11606-013-2354-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer D, Paul R. A cross-national examination of marriage and early life stressors as correlates of depression, anxiety, and stress. The Family Journal. 2011;19:274–280. [Google Scholar]
- Myer L, Stein DJ, Grimsrud A, Seedat S, Williams DR. Social determinants of psychological distress in a nationally-representative sample of South African adults. Social Science and Medicine. 2008;66:1828–1840. doi: 10.1016/j.socscimed.2008.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Bureau of Economic Research . US Business cycle expansions and contractions. National Bureau of Economic Research; Cambridge: 2010. [March 12, 2012]. from: http://www.nber.org/cycles.html. [Google Scholar]
- National Center for Health Statistics . 2010 National Health Interview Survey (NHIS) public use data release: NHIS survey description. National Center for Health Statistics; Hyattsville: 2011. [Google Scholar]
- National Center for Health Statistics . Variance estimation and other analytic issues, NHIS 2006-2011. National Center for Health Statistics; Hyattsville: 2012. [June 19, 2013]. from: http://www.cdc.gov/nchs/data/nhis/2006var.pdf. [Google Scholar]
- Ng DM, Jeffrey RW. Relationships between perceived stress and health behaviors in a sample of working adults. Health Psychology. 2003;22:638–642. doi: 10.1037/0278-6133.22.6.638. [DOI] [PubMed] [Google Scholar]
- Olson LM, Tang SF, Newacheck PW. Children in the United States with discontinuous health insurance coverage. New England Journal of Medicine. 2005;353:382–391. doi: 10.1056/NEJMsa043878. [DOI] [PubMed] [Google Scholar]
- Pearlin LI. The sociological study of stress. Journal of Health and Social Behavior. 1989;30:241–256. [PubMed] [Google Scholar]
- Pearlin LI, Lieberman MA, Menaghan EG, Mullan JT. The stress process. Journal of Health and Social Behavior. 1981;22:337–356. [PubMed] [Google Scholar]
- Riemer JW. Job relocation, sources of stress, and sense of home. Community, Work, & Family. 2000;3:205–217. [Google Scholar]
- Schenker N, Raghunathan TE, Chiu P-L, Makuc DM, Zhang G, Cohen AJ. Multiple imputation of missing income data in the National Health Interview Survey. Journal of the American Statistical Association. 2006;101:924–933. [Google Scholar]
- Schiller JS, Lucas JW, Ward BW, Peregoy JA. Summary health statistics for U.S. adults: National Health Interview Survey, 2010. Vital and Health Statistics. 2012;10:1–207. [PubMed] [Google Scholar]
- Schiller JS, Ward BW, Freeman G, Peregoy JA. Early release of select estimates based on data from the 2012 National Health Interview Survey. National Center for Health Statistics; Hyattsville: 2013. [Google Scholar]
- Schoen C, Collins SR, Kriss JL, Doty MM. How many are underinsured? Trends among U.S. adults, 2003 and 2007. Health Affairs. 2008a;27:w298–w309. doi: 10.1377/hlthaff.27.4.w298. [DOI] [PubMed] [Google Scholar]
- Schoen C, Davis K, Collins SR. Building blocks for reform: achieving universal coverage with private and public group health insurance. Health Affairs. 2008b;27:646–657. doi: 10.1377/hlthaff.27.3.646. [DOI] [PubMed] [Google Scholar]
- Schoenborn CA, Stommel M. Adherence to the 2008 adult physical activity guidelines and mortality risk. American Journal of Preventive Medicine. 2011;40:514–521. doi: 10.1016/j.amepre.2010.12.029. [DOI] [PubMed] [Google Scholar]
- Summer L, Mann C. Instability of public health insurance coverage for children and their families: causes, consequences, and remedies. Georgetown University Health Policy Institute; Washington: 2006. [Google Scholar]
- Thoits PA. Stress, coping, and social support processes: where are we? what next? Journal of Health and Social Behavior. 1995;35:53–79. [PubMed] [Google Scholar]
- Thoits PA. Stress and health: major findings and policy implications. Journal of Health and Social Behavior. 2010;51:S41–S53. doi: 10.1177/0022146510383499. [DOI] [PubMed] [Google Scholar]
- Turner RJ, Noh S. Physical disability and depression: a longitudinal analysis. Journal of Health and Social Behavior. 1988;29:23–37. [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services . Healthy People 2020. Department of Health and Human Services; Washington: U.S.: 2013. [June 19, 2013]. from: http://www.healthypeople.gov/2020/default.aspx. [Google Scholar]