Genomic technologies have enabled personalized cancer treatments based on the unique molecular aberrations in each person's tumor. T-cell-based immunotherapies may expand the range of therapeutic options for personalized oncology. Here, we discuss the advantages of targeting T cells towards mutations, and the identification and potential therapeutic utilization of mutation-reactive T cells.
Keywords: immunotherapy, cancer, next-generation sequencing, personalized oncology, T cell, neoantigen
Abstract
Owing to recent advances in genomic technologies, personalized oncology is poised to fundamentally alter cancer therapy. In this paradigm, the mutational and transcriptional profiles of tumors are assessed, and personalized treatments are designed based on the specific molecular abnormalities relevant to each patient's cancer. To date, such approaches have yielded impressive clinical responses in some patients. However, a major limitation of this strategy has also been revealed: the vast majority of tumor mutations are not targetable by current pharmacological approaches. Immunotherapy offers a promising alternative to exploit tumor mutations as targets for clinical intervention. Mutated proteins can give rise to novel antigens (called neoantigens) that are recognized with high specificity by patient T cells. Indeed, neoantigen-specific T cells have been shown to underlie clinical responses to many standard treatments and immunotherapeutic interventions. Moreover, studies in mouse models targeting neoantigens, and early results from clinical trials, have established proof of concept for personalized immunotherapies targeting next-generation sequencing identified neoantigens. Here, we review basic immunological principles related to T-cell recognition of neoantigens, and we examine recent studies that use genomic data to design personalized immunotherapies. We discuss the opportunities and challenges that lie ahead on the road to improving patient outcomes by incorporating immunotherapy into the paradigm of personalized oncology.
introduction
We have entered an era in which personalized cancer interventions based on genomic data have great potential to improve patient outcomes. Proteins bearing somatic mutations represent ideal therapeutic targets, as they are often expressed exclusively by cancer cells. Recognizing this, many cancer centers are implementing personalized oncology programs that aim to use genomic approaches to identify optimal targeted therapies for individual patients. While this is an exciting and rational approach, it suffers from a major limitation: many cancer mutations are not easily ‘druggable’ by current pharmaceutical agents. T-cell-activating therapies are attractive alternatives, as in theory, T cells can recognize immunogenic mutations in any expressed protein, irrespective of the protein's biochemical function or subcellular location. Moreover, immunotherapies such as checkpoint blockade and adoptive T-cell therapy are yielding remarkable successes in the clinic. Intriguingly, genomic studies are revealing that mutated proteins are often the main target antigens underlying these successes [1, 2]. On the basis of such findings, we discuss the rationale and evidence for including mutation-targeted immunotherapeutic approaches in personalized oncology programs.
using next-generation sequencing to personalize cancer therapy
Next-generation sequencing (NGS), including whole-genome sequencing, whole-transcriptome sequencing, whole-exome sequencing, and targeted sequencing, has dramatically expanded our understanding of cancer. NGS can identify tumor-specific alterations in the genome and transcriptome that influence cancer development, progression, and response to treatment. Initially, it was hoped that sequencing tumors would reveal a circumscribed set of druggable, recurrently mutated genes responsible for the malignant phenotype (i.e. driver mutations). However, sequencing of the first tumor genome in 2008 [3] and the thousands of tumor genomes since has dampened these hopes. The majority of driver genes identified to date are mutated in at most a few percent of patients [4]. Indeed, large-scale sequencing projects like The Cancer Genome Atlas (TCGA) continue to identify new oncogenes as more tumors are sequenced [5, 6]. Moreover, most somatic tumor mutations are thought to be passengers and not implicated in tumorigenesis [4, 7, 8]. Furthermore, the mutational load differs by over three orders of magnitude within and between cancer types [4, 7, 8]. Collectively, the mutational diversity revealed by NGS emphasizes the need for personalized treatments that exploit the unique mutation profile of each tumor.
The first genomics-guided personalized cancer treatment was administered to a patient with adenocarcinoma of the tongue [9]. Integrated analysis of genome and transcriptome data revealed a putative driver mutation in the PTEN gene, as well as overexpression of the RET gene. Although tongue adenocarcinoma is not normally treated with RET inhibitors, on the basis of the NGS data, the patient was given the RET inhibitor Sunitinib, which led to temporary disease stabilization. In another study, NGS of a thyroid cancer identified a personal point mutation in mTOR that conferred resistance to the mTOR inhibitor everolimus [10]. Based on early case reports such as these, several centers have initiated personalized cancer therapy trials in which NGS data are used to inform treatment decisions [11–13]. One group sequenced a panel of 182–236 known driver genes in highly aggressive tumors from 34 patients [11]. Patients received one or more drugs tailored to their mutation profile. Of 11 assessable patients, 3 achieved a partial response and 4 achieved stable disease. While these results are encouraging, the majority of mutant gene products are not targetable with the current armamentarium of pharmaceuticals, thereby limiting the efficacy and broader applicability of personalized cancer therapy [14, 15]. Furthermore, there is limited financial incentive for pharmaceutical companies to develop drugs for rare driver mutations with niche markets. These factors severely limit pharmacological approaches to personalized cancer therapy.
recent advances in cancer immunotherapy
Several immunotherapies have yielded impressive results in the clinic. Recently, the immune modulatory antibodies ipilimumab (Yervoy) and pembrolizumab (Keytruda) received FDA approval for treatment of metastatic melanoma [16, 17], and nivolumab received FDA approval for melanoma and nonsmall-cell lung carcinoma (NSCLC) [18, 19]. These antibodies block signaling of inhibitory T-cell surface receptors cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) (for ipilimumab) and programmed cell death 1 (PD-1) (for pembrolizumab and nivolumab) [20, 21]. The net effect is to enhance T-cell reactivity toward tumors. The first published phase III clinical trial of nivolumab demonstrated a remarkable objective response rate of 40% in highly pre-treated metastatic melanoma patients [18]. Another strategy for inducing antitumor immunity is to use cancer vaccines to activate T cells specific for tumor antigens. Multiple formulations of cancer vaccines have yielded increased survival in phase II trials in prostate, breast, lung, and other cancers [22–24], and some have entered phase III clinical trials [25, 26]. A third form of immunotherapy is adoptive cell therapy (ACT), where tumor-infiltrating lymphocytes (TILs) are harvested from tumor tissue, expanded ex vivo, and transferred back to patients in large numbers [27]. Phase I and II clinical trials using ACT have resulted in response rates of over 50% in metastatic melanoma patients [28, 29]. More recently, ACT with T cells engineered to recognize the B-cell marker CD19 via chimeric antigen receptors have yielded response rates of 80% in acute lymphocytic leukemia [30]. These studies provide unequivocal evidence of the profound antitumor effects of T cells under specific circumstances. However, with the exception of a few lineage-specific targets like CD19, the antigens that underlie many successful antitumor immune responses have remained largely unknown due to the technical challenges associated with identifying T-cell antigens.
a brief primer on T cells and antigen presentation
To understand how the immune system recognizes tumor cells, one needs to consider the basic mechanisms of antigen recognition by T cells. T-cells mature in the thymus, where somatic rearrangement of the T-cell receptor (TCR) locus creates a unique TCR for each T cell. Also within the thymus, self-reactive T cells are deleted through a process called negative-selection or central tolerance. The result is a mature T-cell repertoire with limited reactivity to self but strong reactivity to foreign antigens. The TCR on T cells recognizes antigens as short peptides (called epitopes) bound to the major histocompatibility complex (MHC) on the target cell surface. Only a few peptides from each protein have favorable biochemical characteristics to allow them to be proteolytically cleaved from the parent protein and bound to MHC. There are two types of MHC molecules encoded by human leukocyte antigen (HLA) genes: MHC class I (MHCI) and MHC class II (MHCII). Almost all nucleated cells express MHCI, which presents epitopes to ‘killer’ CD8+ T cells, also called cytotoxic T lymphocytes (CTLs). CTL can directly lyse cells that display cognate epitopes on MHCI, and this is thought to be the most important mechanism underlying antitumor immunity. Professional antigen-presenting cells (APCs) express MHCII, which presents epitopes to CD4+ T-helper cells (Th). Th cells can have multiple antitumor functions such as directly killing tumor cells, augmenting CD8+ T-cell responses, and activating innate antitumor immune cells [31]. Most commonly, T cells recognize antigens derived from pathogens; however, T cells can also recognize tumor antigens, if they are sufficiently different from self-proteins found in healthy tissue.
classes of tumor antigen
Tumor antigens fall into several major groups, each with distinct advantages and disadvantages as targets for cancer immunotherapy. First, cancers of viral origin express virus-derived proteins that can be recognized by the immune system. For example, the E6 and E7 proteins from human papillomavirus make ideal immunotherapy targets [32]. Second, many human cancers express cancer-testis antigens [33]. These proteins are normally expressed only in adult gametes, but can be aberrantly expressed in tumors due to hypomethylation and gene dysregulation [34]. While the tumor-restricted expression pattern of CT antigens makes them attractive targets for immunotherapy, typically they are expressed by only a portion of tumor cells and are dispensable for tumor cell survival [35]. Third, oncogenes with increased expression due to amplification or other mechanisms can give rise to ‘overexpressed’ T-cell antigens. Examples include human epidermal growth factor receptor 2 on breast and ovarian carcinomas [36–38], and mouse double minute 2 homolog in multiple cancers [39]. Fourth, proteins that are differentially expressed in the tissue of origin of the tumor can give rise to ‘differentiation’ antigens. For example, melanomas often express the differentiation antigens MART1, gp100, and tyrosinase [40, 41]. Since differentiation and overexpressed antigens are also present in healthy tissue, T-cells recognizing these classes of antigens are often low affinity as a result of thymic negative-selection [39, 42, 43]. Moreover, targeting such antigens with immunotherapy brings the risk of autoimmune toxicity [44]. Finally, as discussed next, mutations represent a unique class of tumor antigen that has recently become experimentally accessible as a result of NGS advances.
mutations can give rise to neoantigens that are recognized by T cells
Tumors develop tens to thousands of coding mutations during the process of tumorigenesis. A small proportion of mutations affect the extracellular domains of cell surface proteins, such as the EGFRvIII mutation, providing unique targets for antibody-based immunotherapies [45, 46]. However, to be recognized by T cells, mutations need to be processed and presented on MHCI or MHCII, giving rise to so-called neoantigens. Neoantigens can arise when mutations affect either TCR contact residues [47] or anchor residues in peptide epitopes with affinity for MHCI or II [48]. Even a single amino acid substitution can yield an epitope that is sufficiently different from self to mark tumor cells for T-cell-mediated destruction. The concept of neoantigens is not new. By screening tumor-derived cDNA libraries with tumor-reactive T-cell clones, several early studies provided anecdotal examples of immune system recognition of neoantigens [49–51]. Such studies demonstrated that neoantigens can be derived from both driver [52–54] and passenger genes [55, 56] and are present in many different types of tumors, including melanoma [57], renal cell carcinoma [58], oral squamous cell carcinoma [52], colorectal carcinoma [59], lung carcinoma [60], and chronic myelogenous leukemia [61]. Some studies have indicated that neoantigens can be the predominant class of antigen recognized by TIL [33, 62]. Furthermore, neoantigen-specific T-cell responses have been associated with complete or partial tumor regression either spontaneously or after therapy [63–65].
As therapeutic targets, neoantigens have several advantages over other classes of tumor antigen. First, neoantigen-specific T cells are not subject to thymic or peripheral tolerance; therefore, high-affinity T-cell clones are available for immunotherapy [66]. Notably, T cells bearing TCRs with high affinity for their cognate antigens have greater cytotoxic capacity, longer persistence in the tumor environment, and decreased susceptibility to immune suppression [67]. Second, while differentiation and overexpressed antigens are expressed by nontumor tissues, neoantigens are exclusively expressed by tumor cells, reducing the potential for off-target toxicity. Third, while viral and CT antigens may be expressed in only a limited number of tumors, NGS has revealed that a large proportion of tumors express multiple mutant gene products that could potentially serve as T-cell targets [4]. However, as discussed next, it remains a major technical challenge to identify bona fide neoantigens from the tens to thousands of tumor mutations identified by NGS.
computational approaches facilitate identification of neoantigens
Until recently, the identification of personal neoantigens required highly labor-intensive techniques that precluded routine use in the clinic. Advances in NGS and epitope prediction are starting to address this feasibility issue. In addition to mutation profiles, a patient's HLA type can be extracted from NGS data with high accuracy [68], thereby enabling in silico epitope prediction to identify candidate neoantigens. Epitope prediction algorithms assign scores to queried peptide sequences based on similarity to known HLA-binding peptides [69]. Prediction accuracy is highest for common HLA alleles for which more training data are available [69]. Two complementary retrospective analyses have emphasized the ability of NGS and epitope prediction algorithms to identify targets of spontaneous, tumor-reactive T cells. One study found that epitope prediction correctly identified 87% of published neoantigens [63] (using the conventional IC50 cutoff of <500 nM [70]). The second study found that exome sequencing and epitope prediction correctly identified 76%–82% of published neoantigens [71]. Although these predictive algorithms demonstrate high sensitivity, their specificity is difficult to assess due in large part to the issue of antigen processing. While peptide binding to MHCI can be predicted with reasonable accuracy, only 15%–20% of predicted peptides are naturally processed, which is an essential precondition for MHCI presentation [72, 73]. Algorithms for antigen processing prediction have been developed and are continually improving [74], but their sensitivity is not yet adequate for clinical use [75]. Furthermore, it is estimated that the human T-cell repertoire can recognize only ∼50% of potential neoantigens [72, 73]. Thus, to identify tumor neoantigens recognized by patient T cells, predicted neoantigens must still undergo empirical validation.
An alternative to predicting epitopes is to use tandem minigenes to interrogate tumor mutations [76, 77]. In this approach, RNA encoding tumor-specific mutations and flanking sequences is transfected into autologous APCs. T-cell recognition of the APCs is then assessed by ELISPOT or upregulation of T-cell activation markers.
NGS and epitope prediction for interrogating T-cell responses to cancer
Despite current limitations of epitope prediction, NGS has been used successfully to identify tumor-specific T cells in the settings of conventional therapy, checkpoint blockade, vaccines, and ACT:
neoantigen-reactive T-cell responses arise during conventional therapies
Several studies have used NGS to identify and monitor neoantigen-specific T-cell responses during conventional therapies. In one study, T-cell responses to neoantigens were tracked during progression from primary to recurrent disease in a patient with high-grade serous ovarian cancer. Of 40 somatic mutations identified by whole-exome sequencing [78], one was recognized by a CD8+ T-cell clone present in ascites [79]. Interestingly, the mutation was at low abundance in the primary tumor, and the corresponding T-cell response was undetectable. By first recurrence, the mutation was abundant in the tumor, and the T-cell response first appeared. By second recurrence, the T-cell response became undetectable despite continued MHCI presentation of the mutant neoantigen by tumor cells. Thus, this provides an example of the immune system mounting a specific but ultimately unsuccessful response against the evolving tumor genome during standard treatment. In another study, neoantigen-specific CD8+ T-cell responses were detected in peripheral blood from two chronic lymphocytic leukemia patients who achieved long-term remission following allogeneic hematopoietic stem-cell transplantation [80]. In a melanoma study, neoantigen-specific CD4+ T-helper cells were identified in TIL from two of three patients [81]. Collectively, these studies show that neoantigen-specific CD8+ and CD4+ T-cell responses can occur spontaneously or during conventional cancer therapies.
predicted neoantigens are associated with patient survival
In a study analyzing data from TCGA, the potential immunogenicity of 22 758 missense mutations from 515 tumors across six cancer types was assessed in silico [82]. The study found that the number of predicted neoantigens was positively associated with CD8+ T-cell infiltration and patient survival. Moreover, a study of endometrial cancers found that patients with high numbers of immunogenic mutations due to dysfunctional DNA proofreading was associated with an increased cytotoxic immune signature, and improved survival [83]. These results were corroborated and extended by a study which revealed a positive relationship between mutational load and cytotoxic immune cell signatures within tumors [84]. Interestingly, the authors also found that the frequency of predicted highly immunogenic mutations was lower than expected in some tumor types, raising the possibility that T cells may have exerted selective pressure against tumor cells expressing neoantigens.
neoantigen-specific T cells in checkpoint blockade therapy
Several lines of evidence suggest that neoantigens are important for effective antitumor responses induced by immune checkpoint blockade. For example, patients with tumor types that harbor large mutational burdens—such as melanoma and NSCLC—experience the best response rates to PD-1 blocking antibodies [64, 85]. Moreover, colorectal cancer patients with large mutational burdens due to defects in mismatch repair proteins responded more favorably to PD-1 blockade [86]. Additionally, melanoma patients with high mutational loads respond more favorably to ipilimumab [65]. In this latter study, the authors proposed the intriguing concept that some neoantigens might mimic viral pathogens, although corroborating evidence has not been found in other studies [87]. Further evidence for the role of neoantigen-specific T cells in checkpoint blockade therapy was provided by a study of a murine sarcoma model [88]. After treating tumor-bearing mice with either PD-1 or CTLA-4 blocking antibodies, NGS was used to identify two neoantigen-specific T-cell responses in TIL. The neoantigen-specific T cells were activated strongly by checkpoint blockade and mediated a potent antitumor effect in vivo. Finally, in a case report of a melanoma patient who responded well to ipilimumab, T-cell responses against two neoantigens expanded fivefold during ipilimumab treatment in step with the clinical response to therapy [89]. These studies support the hypothesis that neoantigens are key T-cell targets underlying effective checkpoint blockade. Potentially, the number of mutations within a tumor may be useful for prospectively identifying patients who will respond favorably to checkpoint blockade (Figure 1).
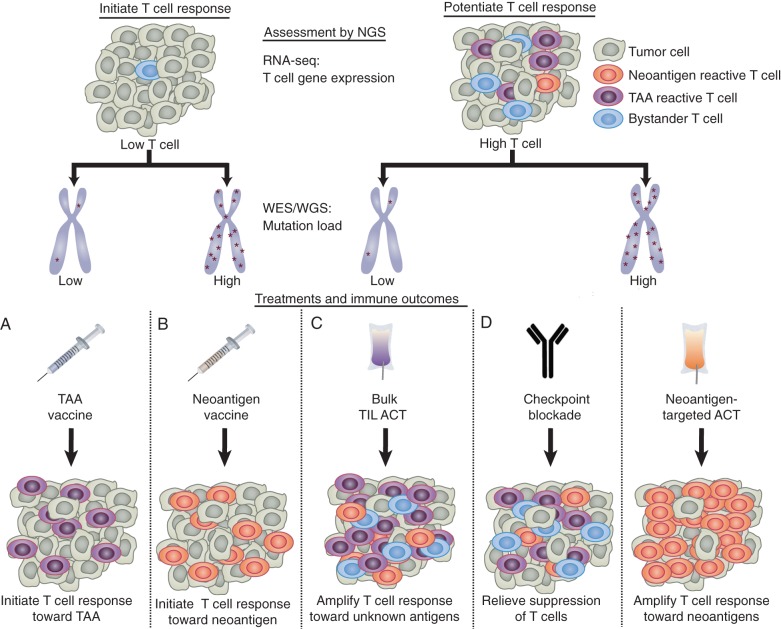
Figure 1.
Proposed use of NGS data to personalize immunotherapy. The goals of immunotherapy are to either potentiate pre-existing antitumor T-cell responses or initiate antitumor T-cell responses if antitumor immunity is low. The level of pre-existing tumor immunity can be assessed by measuring the level of T-cell markers in RNA-seq data [84]. The total mutation load can be determined using whole-genome or whole-exome sequencing (WGS/WES). (A) Patients with low T cells and low mutation load may benefit most from personalized tumor-associated antigen (TAA)-specific vaccines to activate T cells towards highly expressed TAA, which can be identified using RNA-seq data. (B) Patients with low T cells and a high mutation load may benefit most from neoantigen-specific vaccines. (C) Patients with high T cells but a low mutation load may benefit most from standard ACT, to amplify intratumoral T cells against undefined antigens. (D) Patients with high T cells and high mutation load may benefit most from either checkpoint blockade, to relieve T-cell suppression, or neoantigen-targeted ACT, to amplify the mutation-reactive T-cell response. Combination therapies can also be used.
neoantigens as vaccine targets
A compelling use of NGS is to guide the design of personalized, neoantigen-specific therapeutic cancer vaccines. In a preclinical study involving the murine melanoma cell line B16, NGS identified over 500 mutations, of which 50 with favorable epitope prediction and expression levels were targeted with peptide vaccines [90]. Two of these peptide vaccines extended the survival of mice bearing established B16 tumors. The authors subsequently extended these results and found that neoantigen-specific CD4 T-helper cells were important mediators of the antitumor responses, and combining several mutant targets in a single vaccine improved survival of tumor-bearing mice [91]. Additional studies have demonstrated the efficacy of mutation-specific peptide vaccines in mouse models of colon cancer and carcinogen-induced sarcoma [47, 48, 88]. Based on these preclinical successes, at least two personalized neoantigen-targeted trials using either mutant RNA or mutant peptides as antigens are currently recruiting melanoma patients [92, 93]. The first NGS-based neoantigen vaccine trial was recently published and involved three metastatic melanoma patients. Nine mutated peptides were found to induce activation of neoantigen-specific CD8 T cells, and these T-cell responses fell into three categories: (i) those detected before vaccination and subsequently expanded, (ii) those detected only after vaccination, and (iii) those activated toward neoantigens that were not naturally processed and therefore not useful for immunotherapy. These data demonstrate that neoantigen-specific T cells can be activated by vaccination in cancer patients [94].
neoantigen-specific T cells in ACT
Several studies suggest that neoantigens are important targets during successful ACT. In a study of three melanoma patients who responded favorably to ACT [95], NGS identified 264–574 nonsynonymous mutations per case. TIL products were assayed for recognition of predicted mutant peptides and found to recognize two to three neoantigens in each patient. For one patient, neoantigens accounted for the majority of the tumor-specific T-cell response, suggesting that neoantigen-specific T cells may be important effector cells during ACT. In another study by the same group, NGS was used to identify neoantigen-specific T-cell responses in two patients who had achieved durable responses to ACT [96]. These neoantigens were not identified when conventional screening methods were used on the same TIL product, indicating that NGS can identify neoantigens that are missed by other methods. The above findings were corroborated and extended in a study interrogating Th cells from two patients who responded favorably to ACT [81]. The study found that neoantigen-specific Th responses comprised a substantial proportion of the ACT product, yet these T cells were undetectable in peripheral blood before ACT. Together, these findings suggest that neoantigen-specific T cells are important mediators of successful ACT in melanoma.
Similar approaches are now being applied to other types of cancer, as illustrated by a recent case report involving a patient with metastatic cholangiocarcinoma [77]. The patient received ACT and experienced tumor stabilization for 13 months. NGS revealed that ∼25% of the TIL product used for ACT comprised a neoantigen-specific CD4+ T-cell clone recognizing a point mutation in the putative tumor suppressor ERBB2IP. On progression, exome sequencing showed that the tumor continued to express the mutation; therefore, a near clonal population of mutation-specific T cells was selected for infusion. Subsequently, the patient experienced tumor regression without new tumor growth for at least 6 months after ACT. Although speculative, continued expression of the mutation despite the severe immune pressure exerted by ACT suggests that mutant ERBB2IP may have been critical for tumor proliferation or survival. This study emphasizes the potential of using NGS to deliberately target mutations by ACT (Figure 1).
what proportion of mutations gives rise to neoepitopes?
For mutations to be of general utility as targets for immunotherapy, a reasonable proportion must give rise to bona fide MHCI- or MHCII-binding epitopes. However, at present, there is very little information regarding the proportion of mutations that meet this criterion. In the aforementioned studies involving TIL, ≤1% of tumor mutations elicited T-cell responses [80, 81, 89, 95]. However, these studies were designed to detect only pre-existing T-cell responses. What has yet to be quantified systematically is the proportion of mutant peptides that are presented by MHCI or MHCII but ignored by the immune system. Clinical trials have shown that vaccination can induce de novo T-cell responses to mutations in genes such as BCR-ABL, P53, and RAS [61, 94, 97, 98], lending support to the notion that neoantigens can be ignored by the immune system in the absence of intervention. Thus, an important area for future research is to develop methods to predict, quantify, and therapeutically target neoantigens that evade spontaneous immune recognition.
conclusions and future directions
As NGS plays an increasing role in the care of cancer patients, opportunities will arise for the rational design of targeted immunotherapies (Figure 1). Already, NGS has helped researchers discover that neoantigen-specific T-cell responses are implicated in the efficacy of checkpoint blockade and ACT. Building on these early findings, one can envision several clinical applications in the near term, including (i) stratifying patients for checkpoint blockade based on the number of predicted neoantigens in tumors; (ii) determining the effective dose and duration of checkpoint blockade by tracking neoantigen-specific T-cell responses over time; (ii) designing personalized vaccines encoding predicted neoantigens [94]; and (iv) generating neoantigen-specific T-cell products for ACT [77] (Figure 1). To fully realize these possibilities, we require improved methods to reliably identify authentic neoantigens from among the tens to thousands of mutations found in human tumors. NGS can identify mutations with high sensitivity, and epitope prediction algorithms can accurately predict MHCI binding of mutant peptides. However, three major remaining challenges are (i) to predict accurately which neoantigens are naturally processed to yield MHCI-binding peptides presented by tumor cells; (ii) to identify and track neoantigen-reactive T cells in a high-throughput manner; and (iii) to develop immunotherapies that effectively mobilize neoantigen-reactive T cells in cancer patients. Based on the evidence provided by the studies reviewed here, efforts applied on these fronts will facilitate the advancement of immunotherapy as a central modality of NGS-guided personalized oncology.
funding
This work was supported by the British Columbia Cancer Foundation to (SDM, RAH, and BHN); Canadian Institutes of Health Research to (SDM, RAH, and BHN) grant (MOP 84463); Canadian Breast Cancer Foundation to (SDM and BHN); Genome BC to (RAH and BHN); Genome Canada to (RAH); the US Department of Defense to (BHN and RAH) grant (W81XWH); the National Institutes of Health to (GC) grant (R01CA156695); the Ludwig Institute for Cancer Research to (GC); the Ovarian Cancer Research Fund to (GC); and the European Research Council to (GC) grant (1400206AdG-322875).
disclosure
The authors have declared no conflicts of interest.
acknowledgements
We thank Scott Brown, Julie Nielsen and Kwame Twumasi-Boateng for reviewing drafts of this article.
references
- 1.Heemskerk B, Kvistborg P, Schumacher TN. The cancer antigenome. EMBO J 2013; 32: 194–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schumacher TN, Schreiber RD. Neoantigens in cancer immunotherapy. Science 2015; 348: 69–74. [DOI] [PubMed] [Google Scholar]
- 3.Ley TJ, Mardis ER, Ding L et al. . DNA sequencing of a cytogenetically normal acute myeloid leukaemia genome. Nature 2008; 456: 66–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lawrence MS, Stojanov P, Mermel CH et al. . Discovery and saturation analysis of cancer genes across 21 tumour types. Nature 2014; 505: 495–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cancer Genome Atlas Research Network. Comprehensive molecular characterization of urothelial bladder carcinoma. Nature 2014; 507: 315–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tamborero D, Gonzalez-Perez A, Perez-Llamas C et al. . Comprehensive identification of mutational cancer driver genes across 12 tumor types. Sci Rep 2013; 3: 2650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lawrence MS, Stojanov P, Polak P et al. . Mutational heterogeneity in cancer and the search for new cancer-associated genes. Nature 2013; 499: 214–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kandoth C, McLellan MD, Vandin F et al. . Mutational landscape and significance across 12 major cancer types. Nature 2013; 502: 333–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jones SJ, Laskin J, Li YY et al. . Evolution of an adenocarcinoma in response to selection by targeted kinase inhibitors. Genome Biol 2010; 11: R82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wagle N, Grabiner BC, Van Allen EM et al. . Response and acquired resistance to everolimus in anaplastic thyroid cancer. N Engl J Med 2014; 371: 1426–1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schwaederle M, Parker BA, Schwab RB et al. . Molecular tumor board: the University of California-San Diego Moores Cancer Center experience. Oncologist 2014; 19: 631–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tran B, Brown AM, Bedard PL et al. . Feasibility of real time next generation sequencing of cancer genes linked to drug response: results from a clinical trial. Int J Cancer 2013; 132: 1547–1555. [DOI] [PubMed] [Google Scholar]
- 13.Arnedos M, Andre F, Farace F et al. . The challenge to bring personalized cancer medicine from clinical trials into routine clinical practice: the case of the Institut Gustave Roussy. Mol Oncol 2012; 6: 204–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goncalves R, Warner WA, Luo J, Ellis MJ. New concepts in breast cancer genomics and genetics. Breast Cancer Res 2014; 16: 460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen Y, McGee J, Chen X et al. . Identification of druggable cancer driver genes amplified across TCGA datasets. PLoS One 2014; 9: e98293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.US Food and Drug Administration. FDA.gov. 2014. http://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm412861.htm (1 August 2015, date last accessed).
- 17.Hodi FS, O'Day SJ, McDermott DF et al. . Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med 2010; 363: 711–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Robert C, Long GV, Brady B et al. . Nivolumab in previously untreated melanoma without BRAF mutation. N Engl J Med 2015; 372: 320–330. [DOI] [PubMed] [Google Scholar]
- 19.US Food and Drug Administration. FDA.gov. 2015. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm436534.htm (15 March 2015, date last accessed).
- 20.Krummel MF, Allison JP. CD28 and CTLA-4 have opposing effects on the response of T cells to stimulation. J Exp Med 1995; 182: 459–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Freeman GJ, Long AJ, Iwai Y et al. . Engagement of the PD-1 immunoinhibitory receptor by a novel B7 family member leads to negative regulation of lymphocyte activation. J Exp Med 2000; 192: 1027–1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kantoff PW, Schuetz TJ, Blumenstein BA et al. . Overall survival analysis of a phase II randomized controlled trial of a Poxviral-based PSA-targeted immunotherapy in metastatic castration-resistant prostate cancer. J Clin Oncol 2010; 28: 1099–1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mittendorf EA, Clifton GT, Holmes JP et al. . Clinical trial results of the HER-2/neu (E75) vaccine to prevent breast cancer recurrence in high-risk patients: from US Military Cancer Institute Clinical Trials Group Study I-01 and I-02. Cancer 2012; 118: 2594–2602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brunsvig PF, Kyte JA, Kersten C et al. . Telomerase peptide vaccination in NSCLC: a phase II trial in stage III patients vaccinated after chemoradiotherapy and an 8-year update on a phase I/II trial. Clin Cancer Res 2011; 17: 6847–6857. [DOI] [PubMed] [Google Scholar]
- 25.US National Library of Medicine. clinicaltrials.gov/show/NCT01322490 2014. http://www.clinicaltrials.gov/show/NCT01322490 (17 October 2014, date last accessed). [DOI] [PubMed]
- 26.US National Library of Medicine. clinicaltrials.gov/show/NCT01579188 2012. http://www.clinicaltrials.gov/show/NCT01579188 (17 October 2014, date last accessed). [DOI] [PubMed]
- 27.Hinrichs CS, Rosenberg SA. Exploiting the curative potential of adoptive T-cell therapy for cancer. Immunol Rev 2014; 257: 56–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rosenberg SA, Yang JC, Sherry RM et al. . Durable complete responses in heavily pretreated patients with metastatic melanoma using T-cell transfer immunotherapy. Clin Cancer Res 2011; 17: 4550–4557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Radvanyi LG, Bernatchez C, Zhang M et al. . Specific lymphocyte subsets predict response to adoptive cell therapy using expanded autologous tumor-infiltrating lymphocytes in metastatic melanoma patients. Clin Cancer Res 2012; 18: 6758–6770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Maus MV, Grupp SA, Porter DL, June CH. Antibody-modified T cells: CARs take the front seat for hematologic malignancies. Blood 2014; 123: 2625–2635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Haabeth OA, Tveita AA, Fauskanger M et al. . How do CD4(+) T cells detect and eliminate tumor cells that either lack or express MHC class II molecules? Front Immunol 2014; 5: 174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wick DA, Webb JR. A novel, broad spectrum therapeutic HPV vaccine targeting the E7 proteins of HPV16, 18, 31, 45 and 52 that elicits potent E7-specific CD8T cell immunity and regression of large, established, E7-expressing TC-1 tumors. Vaccine 2011; 29: 7857–7866. [DOI] [PubMed] [Google Scholar]
- 33.Coulie PG, Van den Eynde BJ, van der Bruggen P, Boon T. Tumour antigens recognized by T lymphocytes: at the core of cancer immunotherapy. Nat Rev Cancer 2014; 14: 135–146. [DOI] [PubMed] [Google Scholar]
- 34.Whitehurst AW. Cause and consequence of cancer/testis antigen activation in cancer. Annu Rev Pharmacol Toxicol 2014; 54: 251–272. [DOI] [PubMed] [Google Scholar]
- 35.Jungbluth AA, Stockert E, Chen YT et al. . Monoclonal antibody MA454 reveals a heterogeneous expression pattern of MAGE-1 antigen in formalin-fixed paraffin embedded lung tumours. Br J Cancer 2000; 83: 493–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fisk B, Blevins TL, Wharton JT, Ioannides CG. Identification of an immunodominant peptide of HER-2/neu protooncogene recognized by ovarian tumor-specific cytotoxic T lymphocyte lines. J Exp Med 1995; 181: 2109–2117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zsiros E, Duttagupta P, Dangaj D et al. . The ovarian cancer chemokine landscape is conducive to homing of vaccine-primed and CD3/CD28-costimulated T cells prepared for adoptive therapy. Clin Cancer Res 2015; 21: 2840–2850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mittendorf EA, Clifton GT, Holmes JP et al. . Final report of the phase I/II clinical trial of the E75 (nelipepimut-S) vaccine with booster inoculations to prevent disease recurrence in high-risk breast cancer patients. Ann Oncol 2014; 25: 1735–1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bendle GM, Holler A, Downs AM et al. . Broadly expressed tumour-associated proteins as targets for cytotoxic T lymphocyte-based cancer immunotherapy. Expert Opin Biol Ther 2005; 5: 1183–1192. [DOI] [PubMed] [Google Scholar]
- 40.Kawakami Y, Eliyahu S, Sakaguchi K et al. . Identification of the immunodominant peptides of the MART-1 human melanoma antigen recognized by the majority of HLA-A2-restricted tumor infiltrating lymphocytes. J Exp Med 1994; 180: 347–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wolfel T, Van Pel A, Brichard V et al. . Two tyrosinase nonapeptides recognized on HLA-A2 melanomas by autologous cytolytic T lymphocytes. Eur J Immunol 1994; 24: 759–764. [DOI] [PubMed] [Google Scholar]
- 42.Rolla S, Nicolo C, Malinarich S et al. . Distinct and non-overlapping T cell receptor repertoires expanded by DNA vaccination in wild-type and HER-2 transgenic BALB/c mice. J Immunol 2006; 177: 7626–7633. [DOI] [PubMed] [Google Scholar]
- 43.Aleksic M, Liddy N, Molloy PE et al. . Different affinity windows for virus and cancer-specific T-cell receptors: implications for therapeutic strategies. Eur J Immunol 2012; 42: 3174–3179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Morgan RA, Chinnasamy N, Abate-Daga D et al. . Cancer regression and neurological toxicity following anti-MAGE-A3 TCR gene therapy. J Immunother 2013; 36: 133–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Klausz K, Berger S, Lammerts van Bueren JJ et al. . Complement-mediated tumor-specific cell lysis by antibody combinations targeting epidermal growth factor receptor (EGFR) and its variant III (EGFRvIII). Cancer Sci 2011; 102: 1761–1768. [DOI] [PubMed] [Google Scholar]
- 46.Morgan RA, Johnson LA, Davis JL et al. . Recognition of glioma stem cells by genetically modified T cells targeting EGFRvIII and development of adoptive cell therapy for glioma. Hum Gene Ther 2012; 23: 1043–1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yadav M, Jhunjhunwala S, Phung QT et al. . Predicting immunogenic tumour mutations by combining mass spectrometry and exome sequencing. Nature 2014; 515: 572–576. [DOI] [PubMed] [Google Scholar]
- 48.Duan F, Duitama J, Al Seesi S et al. . Genomic and bioinformatic profiling of mutational neoepitopes reveals new rules to predict anticancer immunogenicity. J Exp Med 2014; 211: 2231–2248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mendoza LM, Malarkannan S, Shastri N. Identification of CD8+ T-cell-stimulating antigen genes in cDNA libraries. Methods Mol Biol 2001; 156: 255–263. [DOI] [PubMed] [Google Scholar]
- 50.Sharma G, Holt RA. T-cell epitope discovery technologies. Hum Immunol 2014; 75: 514–519. [DOI] [PubMed] [Google Scholar]
- 51.Cancer Immunity. CancerImmunity.org. 2013. http://www.cancerimmunity.org/peptide/mutations (18 October 2014, date last accessed).
- 52.Mandruzzato S, Brasseur F, Andry G et al. . A CASP-8 mutation recognized by cytolytic T lymphocytes on a human head and neck carcinoma. J Exp Med 1997; 186: 785–793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Robbins PF, El-Gamil M, Li YF et al. . A mutated beta-catenin gene encodes a melanoma-specific antigen recognized by tumor infiltrating lymphocytes. J Exp Med 1996; 183: 1185–1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wolfel T, Hauer M, Schneider J et al. . A p16INK4a-insensitive CDK4 mutant targeted by cytolytic T lymphocytes in a human melanoma. Science 1995; 269: 1281–1284. [DOI] [PubMed] [Google Scholar]
- 55.Echchakir H, Mami-Chouaib F, Vergnon I et al. . A point mutation in the alpha-actinin-4 gene generates an antigenic peptide recognized by autologous cytolytic T lymphocytes on a human lung carcinoma. Cancer Res 2001; 61: 4078–4083. [PubMed] [Google Scholar]
- 56.Chiari R, Foury F, De Plaen E et al. . Two antigens recognized by autologous cytolytic T lymphocytes on a melanoma result from a single point mutation in an essential housekeeping gene. Cancer Res 1999; 59: 5785–5792. [PubMed] [Google Scholar]
- 57.Sharkey MS, Lizee G, Gonzales MI et al. . CD4(+) T-cell recognition of mutated B-RAF in melanoma patients harboring the V599E mutation. Cancer Res 2004; 64: 1595–1599. [DOI] [PubMed] [Google Scholar]
- 58.Gaudin C, Kremer F, Angevin E et al. . A hsp70-2 mutation recognized by CTL on a human renal cell carcinoma. J Immunol 1999; 162: 1730–1738. [PubMed] [Google Scholar]
- 59.Linnebacher M, Gebert J, Rudy W et al. . Frameshift peptide-derived T-cell epitopes: a source of novel tumor-specific antigens. Int J Cancer 2001; 93: 6–11. [DOI] [PubMed] [Google Scholar]
- 60.Karanikas V, Colau D, Baurain JF et al. . High frequency of cytolytic T lymphocytes directed against a tumor-specific mutated antigen detectable with HLA tetramers in the blood of a lung carcinoma patient with long survival. Cancer Res 2001; 61: 3718–3724. [PubMed] [Google Scholar]
- 61.Yotnda P, Firat H, Garcia-Pons F et al. . Cytotoxic T cell response against the chimeric p210 BCR-ABL protein in patients with chronic myelogenous leukemia. J Clin Invest 1998; 101: 2290–2296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lennerz V, Fatho M, Gentilini C et al. . The response of autologous T cells to a human melanoma is dominated by mutated neoantigens. Proc Natl Acad Sci USA 2005; 102: 16013–16018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fritsch EF, Rajasagi M, Ott PA et al. . HLA-binding properties of tumor neoepitopes in humans. Cancer Immunol Res 2014; 2: 522–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rizvi NA, Hellmann MD, Snyder A et al. . Mutational landscape determines sensitivity to PD-1 blockade in non–small cell lung cancer. Science 2015; 348: 124–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Snyder A, Makarov V, Merghoub T et al. . Genetic basis for clinical response to CTLA-4 blockade in melanoma. N Engl J Med 2014; 371: 2189–2199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kessels HW, de Visser KE, Tirion FH et al. . The impact of self-tolerance on the polyclonal CD8+ T cell repertoire. J Immunol 2004; 172: 2324–2331. [DOI] [PubMed] [Google Scholar]
- 67.Bos R, Marquardt KL, Cheung J, Sherman LA. Functional differences between low- and high-affinity CD8(+) T cells in the tumor environment. Oncoimmunology 2012; 1: 1239–1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Warren RL, Choe G, Freeman DJ et al. . Derivation of HLA types from shotgun sequence datasets. Genome Med 2012; 4: 95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zhang GL, Ansari HR, Bradley P et al. . Machine learning competition in immunology—prediction of HLA class I binding peptides. J Immunol Methods 2011; 374: 1–4. [DOI] [PubMed] [Google Scholar]
- 70.Sette A, Vitiello A, Reherman B et al. . The relationship between class I binding affinity and immunogenicity of potential cytotoxic T cell epitopes. J Immunol 1994; 153: 5586–5592. [PubMed] [Google Scholar]
- 71.van Buuren MM, Calis JJ, Schumacher TN. High sensitivity of cancer exome-based CD8T cell neo-antigen identification. Oncoimmunology 2014; 3: e28836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Yewdell JW, Bennink JR. Immunodominance in major histocompatibility complex class I-restricted T lymphocyte responses. Annu Rev Immunol 1999; 17: 51–88. [DOI] [PubMed] [Google Scholar]
- 73.Assarsson E, Sidney J, Oseroff C et al. . A quantitative analysis of the variables affecting the repertoire of T cell specificities recognized after vaccinia virus infection. J Immunol 2007; 178: 7890–7901. [DOI] [PubMed] [Google Scholar]
- 74.Nielsen M, Lundegaard C, Lund O, Kesmir C. The role of the proteasome in generating cytotoxic T-cell epitopes: insights obtained from improved predictions of proteasomal cleavage. Immunogenetics 2005; 57: 33–41. [DOI] [PubMed] [Google Scholar]
- 75.Tenzer S, Peters B, Bulik S et al. . Modeling the MHC class I pathway by combining predictions of proteasomal cleavage, TAP transport and MHC class I binding. Cell Mol Life Sci 2005; 62: 1025–1037. [DOI] [PubMed] [Google Scholar]
- 76.Nielsen JS, Wick DA, Tran E et al. . An in vitro-transcribed-mRNA polyepitope construct encoding 32 distinct HLA class I-restricted epitopes from CMV, EBV, and Influenza for use as a functional control in human immune monitoring studies. J Immunol Methods 2010; 360: 149–156. [DOI] [PubMed] [Google Scholar]
- 77.Tran E, Turcotte S, Gros A et al. . Cancer immunotherapy based on mutation-specific CD4+ T cells in a patient with epithelial cancer. Science 2014; 344: 641–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Castellarin M, Milne K, Zeng T et al. . Clonal evolution of high-grade serous ovarian carcinoma from primary to recurrent disease. J Pathol 2013; 229: 515–524. [DOI] [PubMed] [Google Scholar]
- 79.Wick DA, Webb JR, Nielsen JS et al. . Surveillance of the tumor mutanome by T cells during progression from primary to recurrent ovarian cancer. Clin Cancer Res 2014; 20: 1125–1134. [DOI] [PubMed] [Google Scholar]
- 80.Rajasagi M, Shukla SA, Fritsch EF et al. . Systematic identification of personal tumor-specific neoantigens in chronic lymphocytic leukemia. Blood 2014; 124: 453–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Linnemann C, van Buuren MM, Bies L et al. . High-throughput epitope discovery reveals frequent recognition of neo-antigens by CD4+ T cells in human melanoma. Nat Med 2015; 21: 81–85. [DOI] [PubMed] [Google Scholar]
- 82.Brown SD, Warren RL, Gibb EA et al. . Neo-antigens predicted by tumor genome meta-analysis correlate with increased patient survival. Genome Res 2014; 24: 743–750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.van Gool IC, Eggink FA, Freeman-Mills L et al. . POLE proofreading mutations elicit an anti-tumor immune response in endometrial cancer. Clin Cancer Res 2015; 21: 3347–3355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Rooney MS, Shukla SA, Wu CJ et al. . Molecular and genetic properties of tumors associated with local immune cytolytic activity. Cell 2015; 160: 48–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Champiat S, Ferte C, Lebel-Binay S et al. . Exomics and immunogenics: bridging mutational load and immune checkpoints efficacy. Oncoimmunology 2014; 3: e27817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Le DT, Uram JN, Wang H et al. . PD-1 blockade in tumors with mismatch-repair deficiency. N Engl J Med 2015; 372: 2509–2520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Schumacher TN, Kesmir C, van Buuren MM. Biomarkers in cancer immunotherapy. Cancer Cell 2015; 27: 12–14. [DOI] [PubMed] [Google Scholar]
- 88.Gubin MM, Zhang X, Schuster H et al. . Checkpoint blockade cancer immunotherapy targets tumour-specific mutant antigens. Nature 2014; 515: 577–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.van Rooij N, van Buuren MM, Philips D et al. . Tumor exome analysis reveals neoantigen-specific T-cell reactivity in an ipilimumab-responsive melanoma. J Clin Oncol 2013; 31: e439–e442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Castle JC, Kreiter S, Diekmann J et al. . Exploiting the mutanome for tumor vaccination. Cancer Res 2012; 72: 1081–1091. [DOI] [PubMed] [Google Scholar]
- 91.Kreiter S, Vormehr M, van de Roemer N et al. . Mutant MHC class II epitopes drive therapeutic immune responses to cancer. Nature 2015; 520: 692–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.US National Library of Medicine. clinicaltrials.gov/show/NCT02035956 2014. http://www.clinicaltrials.gov/show/NCT02035956 (18 October 2014, date last accessed). [DOI] [PubMed]
- 93.US National Library of Medicine. clinicaltrials.gov/ct2/show/NCT01970358 2014. http://www.clinicaltrials.gov/ct2/show/NCT01970358 (18 October 2014, date last accessed). [DOI] [PubMed]
- 94.Carreno BM, Magrini V, Becker-Hapak M et al. . Cancer immunotherapy. A dendritic cell vaccine increases the breadth and diversity of melanoma neoantigen-specific T cells. Science 2015; 348: 803–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Robbins PF, Lu YC, El-Gamil M et al. . Mining exomic sequencing data to identify mutated antigens recognized by adoptively transferred tumor-reactive T cells. Nat Med 2013; 19: 747–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lu YC, Yao X, Crystal JS et al. . Efficient identification of mutated cancer antigens recognized by T cells associated with durable tumor regressions. Clin Cancer Res 2014; 20: 3401–3410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ito D, Visus C, Hoffmann TK et al. . Immunological characterization of missense mutations occurring within cytotoxic T cell-defined p53 epitopes in HLA-A*0201+ squamous cell carcinomas of the head and neck. Int J Cancer 2007; 120: 2618–2624. [DOI] [PubMed] [Google Scholar]
- 98.Gjertsen MK, Bjorheim J, Saeterdal I et al. . Cytotoxic CD4+ and CD8+ T lymphocytes, generated by mutant p21-ras (12Val) peptide vaccination of a patient, recognize 12Val-dependent nested epitopes present within the vaccine peptide and kill autologous tumour cells carrying this mutation. Int J Cancer 1997; 72: 784–790. [DOI] [PubMed] [Google Scholar]