Abstract
There is rare literature elaborating the complex total hip arthroplasty (THA) in patients with osteopetrosis who experienced malunion from femoral neck fracture. We have summarized the failure experience of the complex THA in osteopetrosis. Learned from the resurgery in the case reported by this paper, we recommend to highlight the initial stability of the prosthesis and not to overestimate the potency of fracture healing in the complex THA in osteopetrosis.
Keywords: Osteopetrosis, Albers-schonberg disease, complex THA, femoral neck fracture
Introduction
Osteopetrosis, discovered by a German radiologist Albers-schonberg in 1904 for the first time, is a rare genetic bone disease. In terms of the follow-up outcomes, complications and technical difficulties related to total hiparthroplasty (THA) in osteopetrosis patients, little is known. In fact, the hard brittle bone, abnormal bone marrow cavity, susceptibility to a variety of complications has become huge technical challenges to surgeons in the field. For this case, one patient of osteopetrosis with malunion after femoral neck fracture was intervened by THA in our department. More details regarding the surgery are as follows.
Case presentation
Human studies were approved by the appropriate ethics committee and performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its subsequent amendments. A 60-year-old man suffered from osteopetrosis for 52 years. He had already suffered four fractures during his medical history, left humerus fracture (8-year-old), right humerus fracture (12-year-old), left femur fracture (30-year-old), right tibia fracture (30-year-old) respectively. Conservative treatments helped him recovered from the fractures.
The patient suffered from femoral neck fracture resulted from a motorcycle accident in 2000, causing the right hip dysfunction and walked limply after conservative treatment. He felt right hip pain and limited mobility after a long walk in November 3, 2013, the X-ray showed the right femoral neck pathological old fracture, osteopetrosis. He could walk limply with crutches after conservative treatment in another hospital, and pain gradually eased. Then he transferred to our hospital, We carefully evaluated the patient’s condition based on examinations, his laboratory tests, imaging studies (Figures 1, 2, 3 and 4), then treated him with the right trochanter osteotomy and the right total hip arthroplasty (Figure 5) with ceramic femoral head and polyethylene cup, 13th Wagner Cone Prosthesis stem (Zimmer company). He received rehabilitation in bed for 2 months, but the patient had dysfunction and pain with weight-bearing walking. X-ray showed femoral fracture nonunion, loosening 1 month later (Figure 6), and situation got worse after 2 months (Figure 7). Then the patient received right femur fixation with Cable and Plate and bone grafting (Figure 8), and we found the fracture nonunion in surgery. X-ray showed the internal fixation well-fixed in 6 months later (Figure 9).
Figure 1.

Radiograph preoperative.
Figure 2.
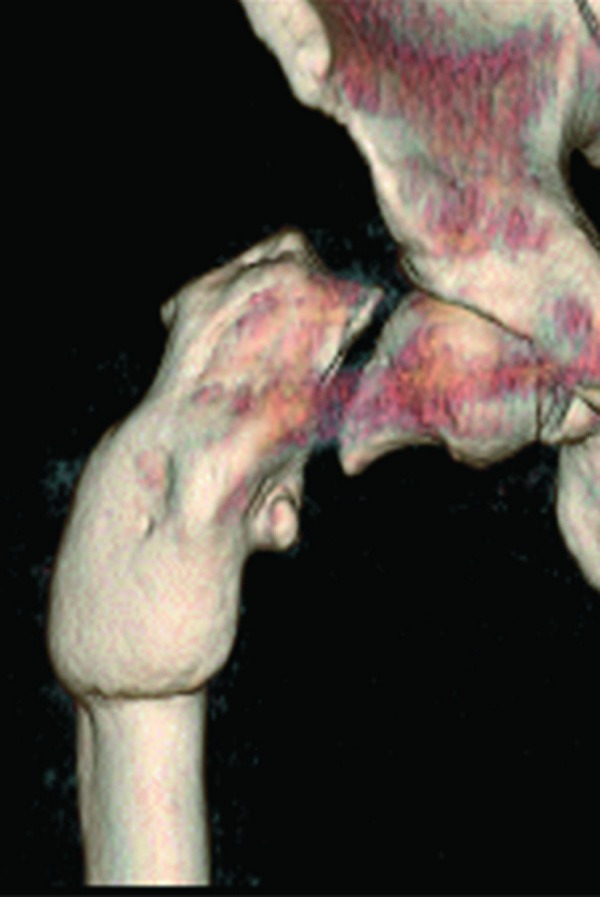
The front view of 3D CT.
Figure 3.
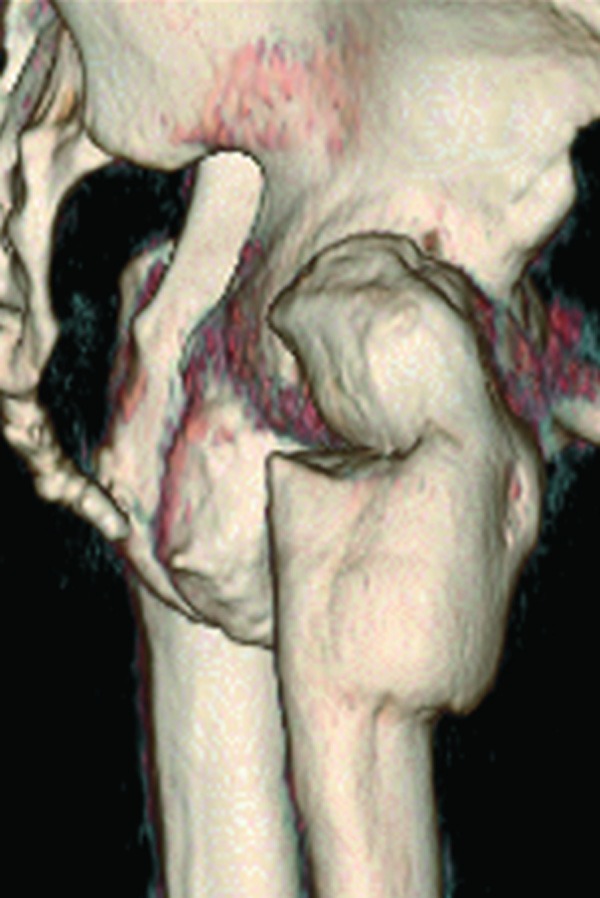
The lateral view of 3D CT.
Figure 4.

The posterior view of 3D CT.
Figure 5.

Radiograph after the THA.
Figure 6.

Radiograph after THA 1 month latter.
Figure 7.

Radiograph after THA 2 months latter.
Figure 8.

Radiograph after the reoperation.
Figure 9.

Radiograph after the reoperation 6 months latter.
Discussion
Generally, there are three kinds of genotypes osteopetrosis, in which two kinds were fatal autosomal recessive inheritance types and one kind was benign autosomal dominant type [1]. The latter autosomal dominant type can furtherly be subdivided into type I and type II [2,3]. All three kinds of hereditary osteopetrosis can result in increased cortical bone and calcified cartilage due to poor osteoclast function that leads to the blocking of bone resorption. The type II osteopetrosis is deemed to be the classic Albers-Schonberg disease [4]. In such condition, although life of patients may not be threatened, however, there will still be a variety of orthopedic problems, including frequent fractures, coxa vara, long-bone bowing, osteomyelitis, osteoarthritis and fracture nonunion [5-9].
Osteosclerotic patients with hip fracture or arthritis are frequently advised to receive total hip arthroplasty to avoid complications such as osteoarthritis, poor fracture healing and other complications [4]. However, there are few clinical reports regarding THA in osteosclerotic patients, thus, experience in such type of surgery was limited so far which made it a challenge for the clinician. THA in osteosclerotic patients has stricter requirement compared with THA in common people. Successful THA in osteosclerotic patients commonly requires team work, experienced THA surgeon, appropriate prosthesis selection, detailed preoperative assessment of the patient’s condition, intraoperative emergency preparedness, rehabilitation, etc.
Initial stability is essential for THA in osteosclerotic patients. The feature of bone in osteopetrosis can affect the adhesion between cement and bone, thus prevent the stability between prosthesis and bone. In both cemented anduncemented prosthesis, favorable initial stability is important. Previous reports have also confirmed that stable fixation can be achieved through surgery. According to Justin P. Strickland [4], in six osteosclerotic cases (nine hips) received THA, four cases with cemented prosthesises and two cases with uncemented prosthesises showed no loosening after midterm follow-up. As for the reoperation in our case, poor initial stability, alone with malunion fracture may explain the failure in the primary THA.
As is known, digging a suitable bone marrow cavity is a key step in THA. However, the marrow cavity inosteopetrosisis irregular or even completely closed, considering the hard and brittle bone, digging a proper marrow cavity seems particularly difficult [5]. To solve this problem, we prepared high-speed burrs and power drills preoperatively, and operated carefully to avoid drilling through the femoral cortex. Unneglectable, thereamer that is used routinely in conventional THA may not be suitable in osteosclerotic cases. As to the prosthesis selection, small and short prosthesis will greatly reduce the surgery difficulty and duration, however, which still significantly outstands ordinary THA.
Theoretically, owing to the hard brittle bone, the risk of periprosthetic fracture and prosthesis fracture in osteosclerotic patients received THA will rise [6], although without previous literature supported. Osteomyelitis may be the other complication secondary to decreased bone vascularity and impaired white cellfunction [8,9]. However, no infections have been reported in the 14 cases of total joint arthroplasty now reported in the English literature [4].
In summary, since osteosclerotic patients that needs THA are rare, there existed limited literature reference to learn from, which makes the clinicians lack of experience in the field. Also, THA carried on such kind of patients is tougher compared to the common one, thus, it requires operators to pay more patience and train better surgical skills. In another aspect, there are more complications that could happen during or after the surgery, so establishing detailed preoperative plan, fully mental preparation to what may happen intraoperatively, as well as corresponding countermeasures, will possibly lead to favorable surgical outcome. Drawing from the resurgery in the case reported in this paper, we recommend to highlight the initial stability of the prosthesis and not to overestimate the potency of fracture healing in the complex THA in osteopetrosis.
Acknowledgements
It was funded by National Natural Science Foundation of China (81373655).
Disclosure of conflict of interest
None.
References
- 1.Carolino J, Perez JA, Popa A. Osteopetrosis. Am Fam Physician. 1998;57:1293–1296. [PubMed] [Google Scholar]
- 2.Bollerslev J, Andersen PE Jr. Fracture patterns in two types of autosomal dominant osteopetrosis. Acta Orthop Scand. 1989;60:110–112. doi: 10.3109/17453678909150106. [DOI] [PubMed] [Google Scholar]
- 3.Bollerslev J, Mosekilde L. Autosomal dominantosteopetrosis. Clin Orthop. 1993;294:45–51. [PubMed] [Google Scholar]
- 4.Strickland JP, Berry DJ. Total Joint Arthroplasty in Patients with Osteopetrosis: a report of 5 cases and review of the literature. J Arthroplasty. 2005;20:815–820. doi: 10.1016/j.arth.2004.11.015. [DOI] [PubMed] [Google Scholar]
- 5.Armstrong DG, Newfield JT, Gillespie RMB. Orthopedicmanagement of osteopetrosis: results of asurvey and review of the literature. J Pediatr Orthop. 1999;19:122–132. [PubMed] [Google Scholar]
- 6.Ashby ME. Total hip arthroplasty in osteopetrosis: areport of two cases. Clin Orthop. 1992;276:214–221. [PubMed] [Google Scholar]
- 7.Gupta R, Gupta N. Femoral fractures in osteopetrosis:case reports. J Trauma. 2001;51:997–999. doi: 10.1097/00005373-200111000-00027. [DOI] [PubMed] [Google Scholar]
- 8.Milgram JW, Jasty M. Osteopetrosis: a morphologicstudy of twenty-one cases. J Bone Joint Surg. 1982;64A:912–929. [PubMed] [Google Scholar]
- 9.Shapiro F. Osteopetrosis: current clinical considerations. Clin Orthop. 1993;294:34–44. [PubMed] [Google Scholar]


